Abstract
Introduction
Elastofibromas are rare, pseudo-tumours arising at the inferior pole of the scapula that have a characteristic presentation. Due to their tissue of origin and size, they may often be mistaken for soft tissue sarcomas. We present the management of patients diagnosed with elastofibroma at a single institution.
Methods
Patients diagnosed with elastofibroma between January 1995 and January 2015 were identified from a prospectively maintained histopathology database. Electronic patient records, imaging and pathology reports were retrieved and reviewed.
Results
Thirty seven patients were identified, with a median age of 66 years and a male-to-female ratio of 1:1.6. All tumours occurred in the characteristic subscapular location. The median maximum tumour diameter was 8.2cm. A synchronous contralateral lesion (15.8%) was found in six patients. Cross-sectional imaging was performed in 29 patients, with magnetic resonance imaging the most common modality (59.5%). Diagnosis was confirmed with percutaneous biopsy in all but one patient, who proceeded directly to surgery. Eighteen patients were managed non-operatively; 19 opted for surgical excision due to significant symptoms. Excision was performed in a marginal fashion and, at a median follow-up of 5 months, no functional impairment or local recurrences were observed.
Conclusions
Soft tissue masses greater than 5cm in diameter should prompt the clinician to exclude soft tissue sarcoma. The diagnosis of elastofibroma may be alluded to by its typical presentation and can be confirmed by percutaneous biopsy. After excluding malignancy, these lesions can be safely managed non-operatively, with surgery reserved for symptomatic patients.
Keywords: Elastofibroma dorsi, Soft tissue sarcoma, Scapula
Elastofibromas are rare pseudotumours originating from the soft tissues, which were first described by Jarvi and Saxen in 1959.1 Although there have been reports of elastofibromas occurring at other sites,2–4 they are most commonly found at the inferior pole of the scapula, deep to the serratus anterior muscle.5–7 This site gives rise to the typical clinical presentation of a ‘clunking’ sensation on abduction and adduction of the arm, as the mass appears and disappears beneath the scapula.8,9
The aetiology of elastofibromas remains unclear. There is some evidence to suggest that they result from the degeneration of collagen fibres secondary to repetitive trauma or mechanical stresses.1,10,11 This may account for their typical subscapular location. The fibro-elastic tissue at the inferior pole of the scapula is thought to act as a shock-absorber, transmitting force from the upper limb through the shoulder girdle.6 An autopsy series suggested that elastofibromas are twice as common in women than men, and rarely occur in those younger than 55 years of age.12
Given their size and tendency to present in an elderly population,5,13 it is not uncommon for an elastofibroma to be mistaken for a soft tissue sarcoma. The diagnosis may be indicated by a typical clinical presentation or the presence of a contralateral lesion, which reassuringly almost certainly excludes a malignant process. Once the benign nature of these lesions has been confirmed with concordant cross-sectional imaging and percutaneous biopsy, operative management may be reserved for patients with significant symptoms.
Due to the rarity of these tumours, much of the evidence for their management is based on small case series. We present the largest surgical series to date of patients with elastofibroma dorsi managed at a single tertiary referral centre for soft tissue tumours.
Methods
All patients diagnosed with an elastofibroma at our institution between January 1995 and January 2015 were identified from a prospectively maintained histopathological database. No exclusion criteria were applied. Data regarding clinical presentation, diagnostic work-up, management and outcomes were retrieved from electronic patient records.
The patients were divided into those managed operatively and non-operatively, and differences in age at presentation were analysed using a two-tailed unpaired t-test. Statistical significance was defined as p <0.05. The analyses were performed using Graphpad version 6.0 (Graphpad Software, San Diego, USA).
Results
Patient demographics and clinical features
Over a 20-year period, 37 patients were diagnosed with an elastofibroma at our institution. The median age at presentation was 66 years (range 43–93 years). A female preponderance was noted, at a male-to-female ratio of 1:1.6. An employment history was available for 33 patients: 15 patients were still employed (40.5%), of whom five (13.5%) had a history of manual labour. Seventeen (45.9%) were retired and one (2.7%) was unemployed.
All of the lesions occurred in the typical subscapular location. A contralateral lesion was found in six patients (15.8%). The median maximum tumour diameter was 8.2cm (range 2–12cm). Each patient had been aware of a mass for some time, at a median symptom duration of 6 months (range 1–60 months). Eight patients were otherwise asymptomatic (21.6%). The typical ‘clunking’ sensation was present in 22 (59.5%) patients, and 15 (40.5%) patients reported pain.
The diagnosis of elastofibroma was suspected by the referring clinician in 10 cases (27.0%). In all other cases, the working diagnosis on referral was that of a soft tissue sarcoma (73.0%).
Diagnostic work-up
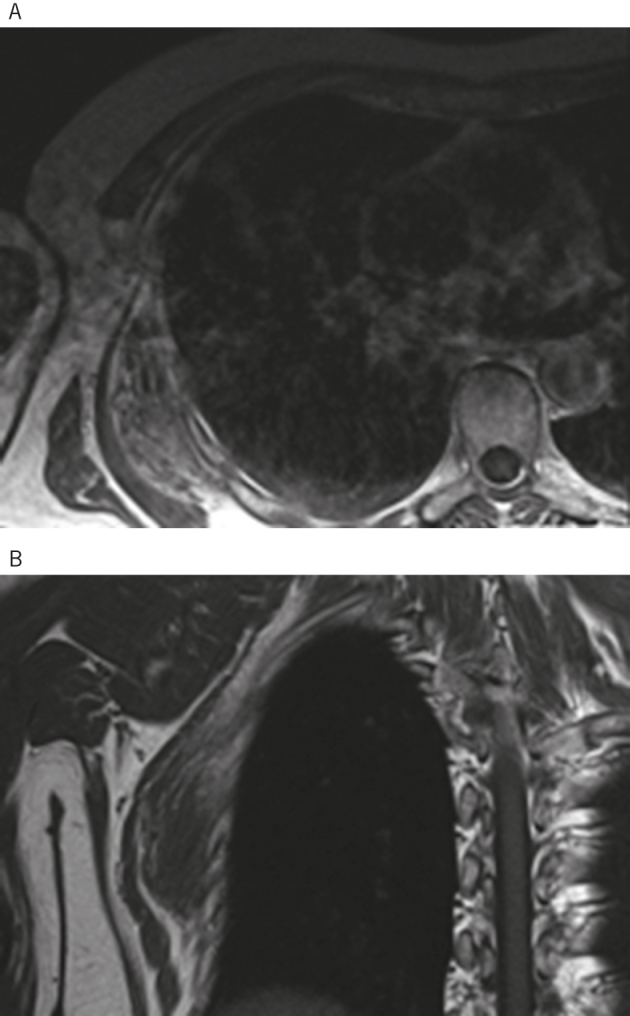
Thirty-two patients underwent some form of imaging as part of their diagnostic work-up. The most commonly used modalities were magnetic resonance imaging (MRI) (59.5%), computed tomography (CT) (29.8%) and ultrasound (10.8%). With MRI, the diagnosis of elastofibroma could be confidently made in 16 patients (69.7%), and a malignant process excluded in a further three (13.0%) patients. The sensitivity of MRI for elastofibroma was 85.7%. The characteristics appearances of elastofibroma on MRI are shown in Figure 1. With CT, the diagnosis of elastofibroma could be confidently made in seven patients (63.6%), and a malignant process excluded in a further patient (9.1%). The sensitivity of CT for elastofibroma was 80.0%. Ultrasound was performed prior to referral and, as a result, a specialist radiologist could not review the images. Based on the reports of these investigations, one patient could be diagnosed with elastofibroma (20%). Six patients did not have any imaging performed, with the diagnosis based on clinical examination and percutaneous biopsy.
Figure 1.
The typical appearances of elastofibroma as seen on magnetic resonance imaging (MRI). Axial (A) and coronal (B) T1-weighted MRI demonstrate a heterogeneous soft tissue mass deep to the serratus anterior, which is isointense to skeletal muscle and interlaced with strands of fat.
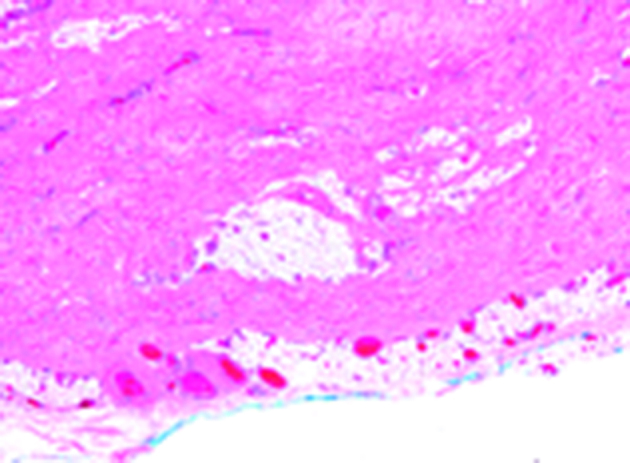
A percutaneous biopsy was obtained in all but one patient (97.4%). This patient presented with characteristic bilateral lesions and proceeded directly to surgery. All biopsies were obtained without image guidance under local anaesthetic at the time of the initial consultation. The typical histological appearance of elastofibroma is shown in Figure 2.
Figure 2.
The characteristic histological appearance of elastofibromas. These are sparsely cellular lesions, composed of densely collagenous tissue that contains patternless distributions of bland spindle cells with ovoid nuclei and even chromatin and fibrillary cytoplasm. The lesions are often relatively ill-defined, and typically entrap the surrounding mature adipose tissue (haematoxylin and eosin).
Management
Once the diagnosis had been, the decision to proceed to surgery was made jointly between the patient and the surgeon. Nineteen patients experienced significant symptoms that were attributable to the lesion and thus opted for surgical excision (51.4%). Thirteen of these patients reported significant pain as the predominant feature, with the remaining six distressed by the ‘clunking’ sensation. Four patients who opted for surgical excision had bilateral lesions. In these cases, staggered excisions were performed, with the largest, symptomatic lesion excised first. The contralateral lesion was excised once it had become symptomatic, at a median of 29 months (range 23–29 months) after the initial operation.
Eighteen patients decided against surgical intervention (48.6%). Eight of these patients were asymptomatic, while eight reported ‘clunking’ as their predominant symptom. Although the remaining two patients reported pain attributable to the tumour, they did not feel it was sufficient to warrant intervention.
The patients undergoing surgery were significantly younger than those opting for non-operative management, with median ages of 61 years and 77 years, respectively (p=0.0004).
Operative procedure and morbidity
All operations were performed under general anaesthetic. The patient was placed in the lateral position, with the ipsilateral arm extended to expose the mass. Following an incision made over the dome of the tumour, the lattisimus dorsi and serratus anterior muscles were split in the direction of their fibres. Once exposed, the tumour was excised from the chest wall in a marginal fashion. After haemostasis had been secured, a suction drain was placed within the cavity and the muscle layers were closed with absorbable sutures.
The median duration of hospital stay was 3 days (range 2–9 days). The morbidity associated with this procedure was modest. A postoperative haematoma developed in two patients (10.5%), requiring a return to theatre for evacuation. Postoperative seromas occurred in five patients (26.3%), which were drained percutaneously in the outpatient clinic.
Follow-up and outcomes
Our institution operates an ‘open door’ policy for follow-up of elastofibromas, in which patients and their general practitioners are encouraged to contact the department if they have any concerns. Once the diagnosis had been confirmed, those patients with minimal symptoms opting for conservative management were discharged from clinic. Those undergoing surgery were discharged once they had fully recovered and their wounds had healed.
The median duration of active follow-up was 5 months (range 0–121 months). By this time, none of the patients who had undergone surgery had experienced any functional morbidity or developed a local recurrence. Two patients represented with pain on the ipsilateral side to surgery. An MRI was performed in both cases, which excluded recurrent disease. The median follow-up from diagnosis at the time of writing was 52.5 months (range 2–234 months), with no local recurrences reported.
Discussion
Elastofibromas are rare pseudo-tumours arising from the deep soft tissues, which may be mistaken for soft tissue sarcomas. They tend to be of a significant size and often occur in elderly people. The median tumour diameter of 8.2cm and median age at presentation of 66 years in our cohort mirrors that of previous case series.5,13 The diagnosis of elastofibroma may be suggested by the characteristic symptom of ‘clunking’ on abduction and adduction of the arm. This was present in less than 60% of our patients, however. The subscapular location of these tumours is also typical, although it is not uncommon for soft tissue sarcomas to present at this site. In light of this, a comprehensive assessment of patients presenting with these lesions is vital to ensure a malignant diagnosis is not overlooked.
Current guidelines recommend that suspicious soft tissue masses be investigated by means of clinical history, imaging and biopsy at a specialist centre.14 In this series, MRI was superior to CT in the imaging of these lesions. It was possible to exclude a malignant process based on MRI appearance on in 82.7% of cases versus 72.7% with CT. These modalities have the further benefit of detecting subclinical contralateral lesions, whose presence virtually excludes malignant pathology. Ultrasound provides limited information and was not routinely used in this series.
Some may argue that, with advances in cross-sectional imaging, the typical appearance of elastofibroma on MRI or CT is sufficient to confirm the diagnosis and precludes the need for biopsy.15–17 At our institution, it is standard practice to obtain a histological diagnosis in patients presenting with a probable elastofibroma, unless a clinically detectable contralateral lesion is present. A percutaneous biopsy may be performed with minimal discomfort under local anaesthetic at the time of the initial consultation. The benefits of obtaining a histological diagnosis are two-fold. First, if a policy of non-operative management is to be pursued, a histological diagnosis provides reassurance to the patient and clinician alike, and allows the patient to be discharged from the clinic without active follow-up. Second, if a surgical intervention is planned, a histological diagnosis confirms that marginal excision is the correct operation to perform. The consequences of inadvertently resecting a sarcoma are substantial. Local recurrence rates in such patients are significantly higher than those undergoing a planned wide excision, even following re-excisions and radiotherapy.18
The decision to excise an elastofibroma should be made jointly by the patient and surgeon. In the absence of significant symptoms, there is no benefit in removing these lesions, and non-operative management should be pursued. None of the patients managed non-operatively in this series represented with worsening symptoms, suggesting long-term follow-up of such patients is unwarranted. Those with significant symptoms should be offered an excision and be made aware of the risks of surgery. The most common postoperative complications in previous series have been haematomas and seromas, at rates of up to 40% and 86%, respectively.7,13,19,20 The complication rates in our series were lower (10.5% and 26.3%), although an apparently larger rate in other series may be related to the smaller patient numbers. Elastofibromas should be excised in a marginal fashion, and our institution has no experience of local recurrence following excision.
Conclusions
In summary, elastofibromas may be easily mistaken for soft tissue sarcomas. The diagnostic work-up of such patients should include clinical history, cross-sectional imaging and biopsy. Surgery should be reserved for those patients with significant symptoms and may be performed in a marginal fashion with minimal morbidity.
References
- 1.Jarvi O, Saxen E. Elastofibroma dorse. Acta pathologica et microbiologica Scandinavica Supplement 1961; : 83–84. [PubMed] [Google Scholar]
- 2.Chen F, Lu D, Tang Y, Peng JJ, Yang H. An unusual case of elastofibroma in the neck. The West Indian medical journal 2014; : 189–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Darling MR, Kutalowski M, MacPherson DG, Jackson-Boeters L, Wysocki GP. Oral elastofibromatous lesions: a review and case series. Head and neck pathology 2011; : 254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McPherson FC, Norman LS, Truitt CA, Morgan MB. Elastofibroma of the foot: uncommon presentation: a case report and review of the literature. Foot & ankle international 2000; : 775–777. [DOI] [PubMed] [Google Scholar]
- 5.Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Davies AM et al. Elastofibroma dorsi: an uncommon benign pseudotumour. Sarcoma 2008; : 756565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayes AJ, Alexander N, Clark MA, Thomas JM. Elastofibroma: a rare soft tissue tumour with a pathognomonic anatomical location and clinical symptom. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 2004; : 450–453. [DOI] [PubMed] [Google Scholar]
- 7.Parratt MT, Donaldson JR, Flanagan AM, Saifuddin A, Pollock RC, Skinner JA, et al. Elastofibroma dorsi: management, outcome and review of the literature. The Journal of bone and joint surgery British volume 2010; : 262–266. [DOI] [PubMed] [Google Scholar]
- 8.Brown RK, Clearkin KP, Nakachi K, Burdick CO. Elastofibroma dorsi. The New England journal of medicine 1966; : 154–155. [DOI] [PubMed] [Google Scholar]
- 9.Jarvi OH, Saxen AE, Hopsu-Havu VK, Wartiovaara JJ, Vaissalo VT. Elastofibroma – a degenerative pseudotumor. Cancer 1969; : 42–63. [DOI] [PubMed] [Google Scholar]
- 10.Stemmermann GN, Stout AP. Elastofibroma dorsi. American journal of clinical pathology 1962; : 499–506. [DOI] [PubMed] [Google Scholar]
- 11.Tighe JR, Clark AE, Turvey DJ. Elastofibroma dorsi. Journal of clinical pathology 1968; : 463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jarvi OH, Lansimies PH. Subclinical elastofibromas in the scapular region in an autopsy series. Acta pathologica et microbiologica Scandinavica Section A, Pathology 1975; : 87–108. [DOI] [PubMed] [Google Scholar]
- 13.Nagano S, Yokouchi M, Setoyama T, Sasaki H, Shimada H, Kawamura I et al. Elastofibroma dorsi: Surgical indications and complications of a rare soft tissue tumor. Molecular and clinical oncology 2014; : 421–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grimer R, Judson I, Peake D, Seddon B. Guidelines for the management of soft tissue sarcomas. Sarcoma 2010; : 506182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Battaglia M, Vanel D, Pollastri P, Balladelli A, Alberghini M, Staals EL et al. Imaging patterns in elastofibroma dorsi. European journal of radiology 2009; : 16–21. [DOI] [PubMed] [Google Scholar]
- 16.Faccioli N, Foti G, Comai A, Cugini C, Guarise A, Mucelli RP. MR imaging findings of elastofibroma dorsi in correlation with pathological features: our experience. La Radiologia medica 2009; : 1283–1291. [DOI] [PubMed] [Google Scholar]
- 17.Tamimi Marino I, Sesma Solis P, Perez Lara A, Martinez Malo J, Vazquez ML, Tamimi F. Sensitivity and positive predictive value of magnetic resonance imaging in the diagnosis of elastofibroma dorsi: review of fourteen cases. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al] 2013; : 57–63. [DOI] [PubMed] [Google Scholar]
- 18.Qureshi YA, Huddy JR, Miller JD, Strauss DC, Thomas JM, Hayes AJ. Unplanned excision of soft tissue sarcoma results in increased rates of local recurrence despite full further oncological treatment. Annals of surgical oncology 2012; : 871–877. [DOI] [PubMed] [Google Scholar]
- 19.Daigeler A, Vogt PM, Busch K, Pennekamp W, Weyhe D, Lehnhardt M et al. Elastofibroma dorsi – differential diagnosis in chest wall tumours. World journal of surgical oncology 2007; : 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muramatsu K, Ihara K, Hashimoto T, Seto S, Taguchi T. Elastofibroma dorsi: diagnosis and treatment. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al] 2007; : 591–595. [DOI] [PubMed] [Google Scholar]


