Abstract
Background
Eliciting cancer survivors’ priorities is essential to address the specific needs of cancer survivor subgroups.
Objective
To describe long-term rectal cancer survivors’ greatest challenges related to treatment.
Design
Observational study with cross-sectional survey.
Setting
Members of Kaiser Permanente, Northern California and Northwest health plans.
Patients
A survey was mailed to long-term (≥5 years post diagnosis) rectal cancer survivors who had an anastomosis, temporary ostomy, or permanent ostomy.
Main Outcome Measures
An open-ended question about the greatest challenge related to cancer surgery. We categorized responses using a grounded theory approach with double coding for reliability. Bonferroni-adjusted X2 values were used to assess differences in the proportions of subgroups who mentioned challenges within each response category.
Results
The survey completion rate was 61% (577/953); 76% (440/577) of participants responded to the greatest challenge question. Respondents’ greatest challenges were bowel/ostomy management (reported by 44%), negative psychosocial effects (37%), late effects of treatment (21%), comorbidities and aging (13%), postoperative recovery (5%), and negative health care experiences (5%). Survivors with temporary ostomy or anastomosis were more likely than survivors with permanent ostomy to report late effects (p<0.0001 and p=0.01, respectively). Survivors with anastomosis were less likely than survivors with permanent ostomy to report negative psychosocial impacts (p=0.0001).
Conclusions
Our results reveal the need for bowel/ostomy management, psychosocial services and surveillance for late effects in survivorship and supportive care services for all rectal cancer survivors, regardless of ostomy status. The perspective of long-term survivors with anastomosis reveals challenges that may not be anticipated during treatment decision-making.
Limitations
Generalizability is restricted by the lack of ethnically and racially diverse, uninsured (non-Medicare-eligible population), and non-English-speaking participants. Because the survey was cross-sectional and included respondents at different times since diagnosis, we could not adequately address changes in the greatest challenges over time.
Keywords: Rectal cancer, survivors, unmet needs, survey, patient-centered outcomes
INTRODUCTION
Fourteen and a half million Americans are cancer survivors, and most are >5 years past their cancer diagnosis.1–3. However, survival does not represent a return to the life prior to cancer, since most survivors experience changes in quality of life related to long-term and late effects from the disease and its treatment. Understanding survivors’ enduring difficulties and perspectives on cancer survivorship’s greatest challenges is essential for identifying and planning for the specific needs of cancer survivor subgroups.4
Research on rectal cancer survivorship has focused on health-related quality of life (HRQOL) as well as comparisons between survivors with or without a permanent ostomy.5–9 While systematic reviews and a meta-analysis have not shown a clear HRQOL difference in patients with or without a permanent colostomy, most patients and health care providers presume that living with an ostomy is dramatically different and more difficult than living without one.10–12 Research directly comparing the HRQOL impacts of various rectal cancer surgical approaches has not relied directly on patients’ narrative appraisals of their experiences. This approach can complement HRQOL measures because it allows patients to report, in their own words, the outcomes that are most meaningful to them. Well-documented and systematically collected information about patients’ experiences after cancer surgery could also optimize treatment decisions that are driven in part by an unrealistic appraisal of what life is like with or without an ostomy.13
In our previous report of the greatest challenges experienced by long-term colorectal cancer survivors with ostomies (88% rectal cancer survivors),14,15 we identified ongoing concerns, including adjustment problems that endured beyond the postoperative period and a continued need for education, skill building, and emotional support. Survivors also noted a need for good, safe, and economical ostomy equipment and a lack of awareness among healthcare professionals about ostomies and available ostomy supplies. Finally, survivors reported that comorbidities had a strong effect on HRQOL, ostomy function, and ostomy self-care.
The current analysis is based on a study of rectal cancer survivors with or without permanent ostomy, including those who had a temporary ostomy. Among colorectal cancer survivors, rectal cancer survivors—particularly those with low tumors—may experience the most challenges with HRQOL after treatment.16,17 We directly and systematically compare the greatest challenges reported by rectal cancer survivors whose surgeries resulted in anastomosis, temporary ostomy, or permanent ostomy. Our goal was to garner information that could guide treatment decision making and to identify patient-centered concerns that could be mitigated through improved survivorship care and advances in research.
METHODS
Study Participants
We mailed a one-time survey to all rectal cancer survivors ≥5 years post diagnosis, enrolled in the Kaiser Permanente integrated health care system in Northern California or Northwest (Oregon/Southwest Washington).18 All participants had a history of abdominal surgery to treat rectal cancer that resulted in an anastomosis or permanent ostomy. We identified participants who had a temporary ostomy, a subset of the anastomosis group, using medical records data. Our study activities were approved by the institutional review boards at Kaiser Permanente Northwest, Kaiser Permanente Northern California, and the University of Arizona.
Measures
Our survey included questions about HRQOL, bowel function, dietary and behavioral adaptations related to rectal cancer, and other elements of cancer survivorship, which are reported elsewhere and summarized in Table 1.18,19 We concluded the survey with an open-ended question. For survivors with permanent ostomy, the question was: “Many people have shared stories about their lives with an ostomy. Please share with us the greatest challenge you have encountered in having an ostomy.” For survivors with an anastomosis or a temporary ostomy, the survey question was: “Many people have shared stories about their lives after rectal or colon cancer surgery. Please share with us the greatest challenge(s) you have encountered since your cancer surgery.” All participants were provided with a full page in which to write their response.
TABLE 1.
Survey Measures
| Topic area | Sources/Details |
|---|---|
| Health-related quality of life (condition specific) |
City of Hope Quality of Life Colorectal Cancer (COH-QOL-CRC)15,20 |
| Health-related quality of life (general) |
SF-12.221 |
| Social support | Duke-UNC Functional Social Support Questionnaire22 |
| Bowel function | Bowel Function Index (adapted to patients with and without ostomy)18,23 |
| Ostomy-specific questions | Developed questions about ostomy location, problems with ostomy equipment, self-care |
| Sexual activity | Developed questions about sexual activity, satisfaction, body image, functional problems. Adapted from COH-QOL-CRC and American Cancer Society’s Study of Cancer Survivors24 |
| Diet & Behavioral Modifications |
Developed questions on typical eating patterns, adjustments since surgery Adapted from COH-QOL-CRC Developed questions asking what foods and beverages as well as other dietary behaviors help with bowel function Developed questions asking what supplements, medications or other products help with bowel function. Developed questions asking what exercises or activities help with bowel function. |
| Exercise | Physical activity Adapted from the Leisure Score Index from the Godin Leisure-Time Exercise Questionnaire25 |
| Smoking | Current smoking status, quit date, pack years, use of other tobacco products |
| Work | Adapted from the American Cancer Society’s Study of Cancer Survivors and COH-QOL-CRC |
| Demographics | Education, current height and weight, weight at time of surgery, race/ethnicity, household income, marital status |
| Greatest challenge | Open-ended question (reported in this manuscript) |
Electronic data on rectal cancer history, surgery type, and comorbidity burden (as measured with the Charlson-Deyo comorbidity index score)26 were extracted from the tumor registries and clinical databases at each study site.
Data Analysis
Qualitative analysis
Free-text survey responses were transcribed into a spreadsheet to facilitate our mixed-method analysis. Using a qualitative, grounded theory approach, several co-authors reviewed all survey responses and created a list of unique topics in our data.27 Codes were created from the topics and then grouped into higher level categories. These codes and categories were used in a content analysis. Every challenge mentioned received a code. All responses were double-coded by pairs of researchers who first coded responses individually and then met to resolve any discrepancies. Problems with the codebook or specific participant responses were shared among the entire group of coders (CM, JB, RK, MG, MH, AA, VS) to ensure the codebook was applied consistently. Participant responses were given as many different codes as were applicable, so the number of codes exceeded the number of respondents in our dataset.
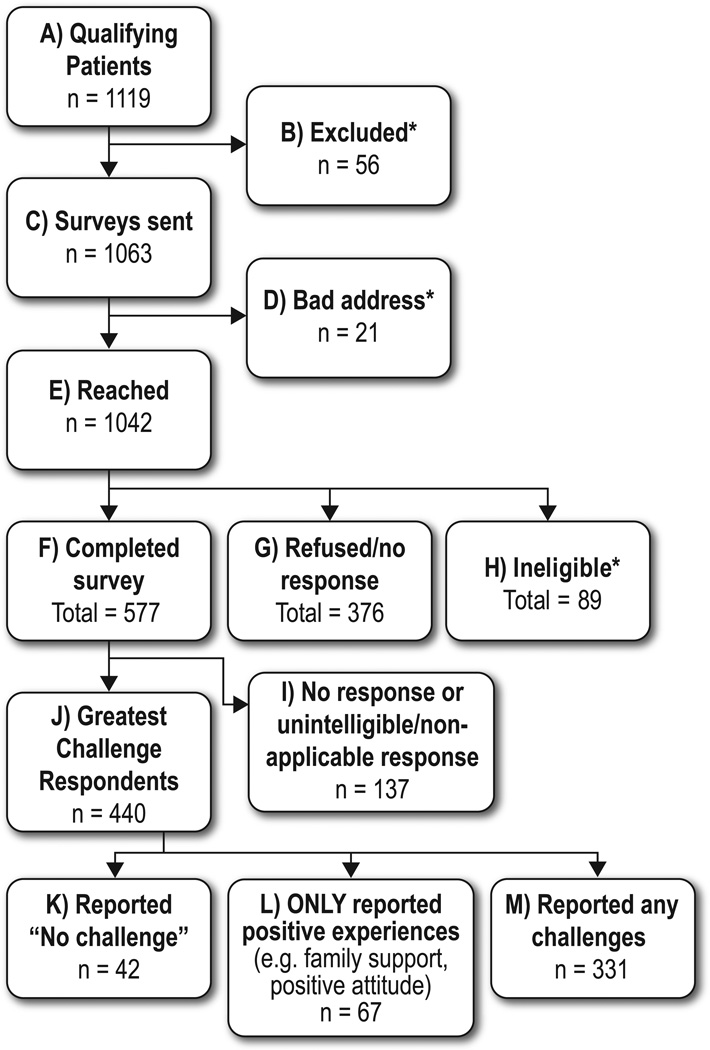
We did not include in this analysis codes that referred to positive aspects of survivorship, such as faith and family support, because we aimed to describe reported challenges. Individuals who mentioned only positive aspects of survivorship were included in the denominator (Fig 1).
FIGURE 1.
Survey response rates. *Found to be ineligible (dead, not rectal cancer, etc) after initial search (B), after wrong address and phone number (D), or after return of survey if patient reported no rectal cancer, no intra-abdominal surgery, and so forth (H).
Quantitative analysis of coded, qualitative data
We compared the proportion of respondents who mentioned challenges in each category by surgery type, time since surgery, and sex. Time since surgery was dichotomized at a cut off of 12 years, the median length of time since surgery among respondents. We compared the means of continuous variables using Student’s t-test and the proportions of categorical variables using the X2 test. We performed Bonferroni adjustment for 3 pairwise comparisons (anastomosis vs permanent ostomy, anastomosis vs temporary ostomy, and permanent ostomy vs temporary ostomy) by using an alpha of .05/3; thus a p-value less than .0167 was considered statistically significant.
RESULTS
The survey response rate was 61% (Figure 1: F/(A-B-D-H)), with a higher response among participants with permanent ostomy compared to anastomosis (66.8% vs. 58.6%, p. 0.02). Participants and non-participants differed according to several socio-demographic factors, but not by stage at diagnosis.18 Among survey respondents, seventy-six percent (440/577) wrote an answer to the greatest challenge question. The mean age of respondents and nonrespondents to the greatest challenge question was similar (73.3 ± 10.6 vs 73.0 ± 11.6, P =0.82), as was the number of years between cancer surgery and the survey (13.3 ± 6.5 vs 12.6 ± 6.0, p=0.30). Respondents to the question had a significantly lower comorbidity burden (P=0.003) and higher education level (P=0.02) than nonrespondents did; otherwise, these two groups did not differ significantly (Table 2). Responses came from 241 (55%) survey respondents with anastomosis, 145 (33%) with permanent ostomy, and 54 (12%) with temporary ostomy. Percentages reported for the categories of challenges described below are based on the 440 respondents who provided an answer to our question in English. Of these, 42 (10%) responded that they had not experienced any challenges.
TABLE 2.
Demographic and Clinical Characteristics of Survey Participants Who Did or Did Not Respond to the Greatest Challenge Question (N=577)
| Provided Greatest Challenge Response (n=440) |
Did Not Provide a Greatest Challenge Response (n=137) |
P | |
|---|---|---|---|
| Age (mean ± SD) | 73.3 ± 10.6 | 73.0 ± 11.6 | .82 |
| Male (%) | 58.9 | 59.9 | .84 |
| Hispanic ethnicity (%) | 7.3 | 4.4 | .23 |
| White race (%) | 85.6 | 80.9 | .18 |
| Received college degree (%) | 40.9 | 28.8 | .02 |
| Income >$50,000 per year (%) | 46.0 | 37.6 | .10 |
| Married or partnered (%) | 66.7 | 58.2 | .07 |
| Employed (%) | 34.2 | 38.6 | .35 |
| Retired (%) | 63.8 | 57.6 | .20 |
| Charlson-Deyo comorbidity score >2 | 18.9 | 30.7 | .003 |
| Surgery type (%) | |||
| Permanent ostomy | 33.0 | 27.7 | .25 |
| Temporary ostomy | 12.3 | 9.5 | |
| Anastomosis | 54.8 | 62.8 | |
| Received radiotherapy (%) | 38.2 | 43.8 | .24 |
| Received chemotherapy (%) | 50.5 | 53.3 | .56 |
| Years from cancer surgery to survey (mean ± SD) |
13.3 ± 6.5 | 12.6 ± 6.0 | .30 |
| Tumor stage (%) | |||
| Localized | 52.3 | 46.5 | .17 |
| Regional | 46.3 | 53.5 | |
| Distant | 1.4 | 0 | |
Categories of Survivorship Challenges
Our taxonomy included 6 higher-order categories of challenges, which encompassed 43 specific topics. On average, respondents who mentioned any challenge reported 1.88 categories of challenges in their response. Illustrative quotes of responses for each category are presented in Table 3.
TABLE 3.
Illustrative Survivor Quotes for Each Category of Challenges
| Category of Challenge | Quote |
|---|---|
| Negative psychosocial effects from surgery or ostomy |
“I was a middle school teacher when I became ill… I often had to run to the bathroom between classes and sometimes during class. I retired early in part because the work-related stress became overwhelming.” (survivor with anastomosis) “My ostomy is a permanent fixture attached to my body. Having the thought I will never be normal again, and feeling I no longer really have control over a body function…. Constantly thinking of [the stoma] and worry what would happen next….” (survivor with ostomy) |
| Bowel and ostomy management |
“If I’m going to a major league baseball game, I eat very little the day of the game—towards the end of a game, the beer drinkers are standing in a line to use the bathroom—I can’t take the chance to have to wait in a line.” (survivor with anastomosis) “Odor control is probably the biggest challenge. It requires frequent emptying when in social environments—taking care of what you eat and when you eat it as a control measure—using a fresh bag/wafer to minimize odor prior to a social event—having a bag break or split, or having the clip come undone is never fun in a public place.” (survivor with ostomy) |
| Late effects of cancer treatments |
“Both my intestines and vagina were greatly affected by the radiation I had after surgery…. It’s possible to have a busy life, just not eating much during the day. That and a good attitude goes a long way.” (survivor with anastomosis) “I regret that my hernia, not my stoma, is obvious.” (survivor with ostomy) |
| Comorbidities and aging (other than rectal cancer) |
“I am a self-employed artist, selling my products… at street fairs, markets and festivals. The most difficult problem I’ve had to deal with is incontinence. I can no longer work all day in my booth… and I’m often tired. Much of this difficulty may just be a function of getting older and I could blame my condition on the cancer operation but honestly I don’t know.” (survivor with temporary ostomy) “The greatest health challenges for me are related to diabetes, cardiovascular disease, and bilateral hip and spinal problems. The cancer is just another chronic condition along with the above.” (survivor with temporary ostomy) |
| Postoperative recovery | “Had a bad start, spent 8 days in hospital. Learned nothing about taking care of myself after surgery. Was sent to care home to learn more about things. No one knew anything about my condition. Had a meltdown. Couldn’t stop crying. A doctor… talked to me and got me out and sent me to an ostomy nurse (2 days later)… Finally got someone to take my stitches out so I could sit… had a lot of ups and downs but I’m still here.” (survivor with ostomy) “One of the biggest problems I had was the recovery time for healing and the amount of pain I had after surgery… I believe my recovery time was lengthened due to the fact that I returned to work too soon… but I could not afford to stay off work any longer.” (survivor with anastomosis) |
| Negative experiences in health care |
“… The medical crew gave me no clue as to what to expect after surgery.” (survivor with temporary ostomy) “The greatest challenge I think is to get the attention of medical professionals and staff to see that quality of life issues are almost as important as the diagnosis/surgery/treatment/cure and recurrence of cancer.” (survivor with temporary ostomy) |
Bowel/Ostomy Management
Forty-four percent of survey respondents mentioned bowel and ostomy management as one of their greatest challenges. Topics included the consequences of living with bowel dysfunction, such as planning around problems or not adequately predicting problems (e.g., constipation, diarrhea, gas, odor, incomplete evacuation, incontinence, urgency). Other comments related to strategies for regulating bowel function, such as altering diet, adjusting the timing of meals and activities, changing physical activity, and consuming medications. Survivors with ostomies also reported self-care challenges, such as the time and effort required for ostomy care and problems with ostomy equipment that could result in leaks. Pain or discomfort associated with bowel movements was included in this domain.
Negative Psychosocial Effects from Surgery or Ostomy
This category included responses that explicitly referred to negative emotional or social consequences of the surgery. Thirty-seven percent of participants reported negative psychosocial challenges, including fear and anxiety regarding gas, odor, incontinence, or leakage of stool or ostomy bag contents; not returning to “normal” after cancer; constraints on valued activities; relationship and intimacy problems; and other emotional and mental health issues beyond bowel function. Survivors described challenges during their initial adaptation after treatment as well as ongoing struggles with psychological and social issues.
Late Effects of Cancer Treatments
Twenty-one percent of respondents mentioned challenges relating to late effects of chemotherapy, radiotherapy, or surgery (other than bowel dysfunction or ostomy-specific challenges). Primary challenges related to surgery included hernias, bowel obstruction or blockage, and urinary incontinence and fistulas. Survivors attributed fatigue, concentration, and stamina problems to all treatment modalities (surgery, chemotherapy, and radiotherapy). Some enduring pain and discomfort was attributed to the effects of cancer treatment. Radiation-induced scarring, infertility, and sexual dysfunction among women were particularly problematic. Survivors with anastomosis wrote about bowel obstructions, strictures, and narrowing of the rectum, and survivors who received chemotherapy wrote about neuropathy. Issues relating to cancer recurrence and problems experienced during ongoing surveillance were included in this category.
Comorbidities and Aging (Other than Rectal Cancer)
Thirteen percent of respondents commented on challenges they attributed to aging or specific conditions (e.g., arthritis, heart disease, or other cancers). Although these issues were not predominant challenges for most participants, for some these types of challenges were more significant than any directly related to rectal cancer. Preexisting conditions before rectal cancer shaped the survivorship experience for some respondents (e.g., those with Crohn’s disease noted relief after bowel resection). Survivors expressed some difficulty in attributing their current difficulties to “old age,” comorbidities, or rectal cancer and its treatment and questioned their ability to clearly assess their rectal cancer-specific HRQOL.
Postoperative Recovery
Postoperative recovery was mentioned by 5% of respondents as one of their greatest challenges. This category included comments about significant challenges soon after the initial rectal cancer surgery, such as readmission to the hospital, a painful or lengthy recovery, or postoperative infection. We placed these comments in a separate category to distinguish them from enduring and later-onset effects of cancer treatment.
Negative Experiences in Health Care
A few respondents (5%) described negative experiences with health care, including problems experienced during initial cancer treatment or subsequent health care encounters. Experiences included lack of attention by health care providers to quality-of-life issues, other unmet needs (e.g., lack of ostomy checkups, or updates about recommendations for survivorship care), the cost of ostomy supplies, and lack of options for ostomy equipment. They also reported problems with the quality of care or service (e.g., delayed diagnosis or unnecessary treatment) and having been given inappropriate or false expectations about recovery and late or long-term effects.
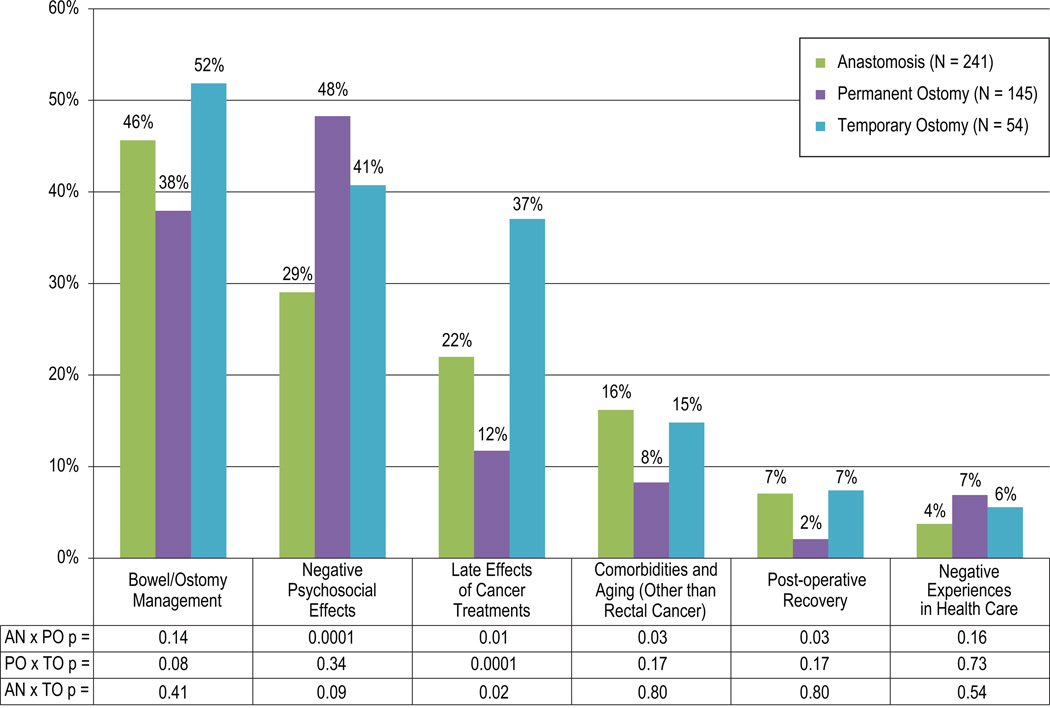
Challenges by Surgery Type
All 6 categories of challenges were reported by survivors in each surgical group (anastomosis, temporary ostomy, and permanent ostomy). The 2 most commonly reported problems in each group were bowel/ostomy management and negative psychosocial effects. Survivors with temporary ostomy or anastomosis were more likely than survivors with permanent ostomy to report late effects (p<0.0001 and p=0.01, respectively). Survivors with anastomosis were less likely to report negative psychosocial effects than were survivors with permanent ostomy (29% vs 48%, P=0.0001) (Fig. 2).
FIGURE 2.
Survivor reports. P values are shown after Bonferroni adjustment. AN = anastomosis; PO = permanent ostomy; TO = temporary ostomy.
Qualitative review of the codes and comments within each category revealed many issues shared across the surgical groups, such as managing bowel function and avoiding incontinence (or equipment failures) through medication and diet, activity restrictions, and travel accommodations. There were some notable surgery-specific differences. Ostomy patients reported difficulty in managing equipment, pronounced forms of psychological distress, and good support from ostomy nurses or ostomy support groups. In contrast, anastomosis patients reported concern about the effects of radiotherapy and the lack of support resources.
Challenges by Time Since Diagnosis and Sex
There were no statistically significant differences in the frequency of reported challenges in different categories by sex or time since surgery.
DISCUSSION
By surveying long-term rectal cancer survivors with or without a permanent ostomy and asking them a single nondirective and open-ended question, we gained a unique perspective on survivors’ greatest cancer-related challenges ≥5 years after diagnosis. The most frequent problems mentioned were related to bowel/ostomy management and negative psychosocial impacts. The proportion of respondents mentioning types of challenges varied by surgical group in only two categories of challenges (negative psychosocial effects and late effects of cancer treatment). Categories of challenges reported did not vary by sex or time since surgery. Our content analysis findings reflect the presence or absence of a domain as a major challenge during survivorship rather than the amount of distress experienced within a given domain. Thus, our findings related to sex and time since surgery do not directly contradict comparative studies using disease-specific HRQOL measures that have found, for example, that women and survivors with ostomies have worse HRQOL outcomes in certain domains or that the effect of an ostomy on HRQOL is attenuated by increased age.9,28
Our results resemble those of a population-level survey of British colorectal cancer survivors (N=21,802)5 and highlight the notable challenges reported by rectal cancer survivors after sphincter-sparing surgery. Thirty percent of British rectal cancer survivors without permanent ostomy experienced moderate to severe problems with bowel dysfunction in the first 3 years after diagnosis.5 In our study, 44% of rectal cancer reported bowel management as their greatest challenge. Anastomosis patients in our study perceived a lack of clinical and emotional support, whereas ostomy patients praised the specialized nursing care and peer support they received, indicating that survivors without an ostomy have unrecognized ongoing care needs. Despite a much larger population of survivors with anastomosis than with permanent ostomy, health care providers seem to be neglecting the needs of anastomosis patients, perhaps due to an implicit assumption that these patients have fewer problems because bowel continuity is preserved or because there are too few specialized nursing or other resources for this population. The American Cancer Society’s Study of Cancer Survivors II found that 19% of colorectal cancer survivors reported unmet needs relating to education and information,4 and our results suggest that interventions should be targeted at managing bowel/ostomy function as well as psychosocial distress.
Patients who had a temporary ostomy reported the highest levels of bowel/ostomy concerns and levels of psychosocial challenges that are similar to patients with permanent ostomy. This pattern may be due to temporary ostomy patients having experienced two adjustment processes (receiving the ostomy, then its reversal). Other patient factors, including tumor location, may also result in worse bowel function and thus psychosocial distress. Further exploration of the unique challenges and solutions for patients with temporary ostomy is needed.5,29
Across surgery types, psychosocial distress was mentioned as one of the top two challenges of survivorship by 37% of patients in our study (162/440). In 2011, the US Medical Expenditures Panel Survey showed that for nearly half of elderly cancer survivors with Medicare insurance only, providers did not discuss social and emotional needs at any time after treatment, and in a study of follow-up care priorities expressed by colorectal patients and surgeons in Italy, addressing emotional concerns during follow-up care was important for 26% of patients but was not a priority for surgeons (P=0.03).30,31 The American Society for Clinical Oncology (ASCO) and the National Comprehensive Cancer Center Network (NCCN) follow-up/survivorship care guidelines for colorectal cancer do not mention psychosocial services as part of recommended follow-up care.32,33 However, the more general NCCN Survivorship Care Guidelines recommend screening for anxiety and depression at regular intervals, particularly when disease status or treatment has changed.34 The discrepancy between patient-reported priorities and clinical priorities indicate that assessment and intervention for psychosocial challenges warrant more systematic attention in rectal cancer survivorship care guidelines and service delivery.
The generalizability of our study results is restricted by the lack of ethnically diverse, racially diverse, uninsured (non-Medicare-eligible population), and non-English-speaking participants. Because the survey was cross-sectional and included respondents at different times since diagnosis, we could not adequately address changes in the greatest challenges over time. We were not able to compare responses by patterns of chemotherapy or radiotherapy, by tumor location, or by recurrence status. However, we had a large, population-based sample (derived from a health plan membership of approximately 4 million individuals) and identified cases using high-quality tumor registry data. Our method of data elicitation allowed patients to describe their experience using their own terms, and our use of a grounded theory approach to codifying responses in a large, qualitative data set that was rigorously quantified using content analysis resulted in sufficient numbers of respondents by surgical group to permit statistical analysis of subgroup differences.
Conclusion and Next Steps
Our results revealed the need for bowel/ostomy management, psychosocial services and surveillance for late effects in survivorship and supportive care services for all rectal cancer survivors, regardless of ostomy status. The perspective of long-term survivors with anastomosis about life after treatment reveals challenges that may not be anticipated during treatment decision-making. Our findings suggest several messages that could help rectal cancer patients make decisions about surgery and/or optimize survivorship:
Counter to prevailing ideas that influence surgical decision-making, patients with anastomosis or temporary ostomy report as frequently as patients with permanent ostomy that their greatest challenges in survivorship relate to bowel management.
In accordance with previous HRQOL studies, patients with permanent ostomy report negative psychosocial impacts more often than those with anastomosis do.
Patients with a permanent ostomy are least likely to report that the late effects of cancer treatments present a significant survivorship challenge.
The enduring concerns (particularly negative psychosocial impacts, bowel dysfunction, and late effects) of rectal cancer survivors need to be addressed through improved surveillance and supportive care. Subsequent studies could explore whether patient-reported challenges vary by tumor location, chemotherapy, radiotherapy, recurrence, or patterns of follow-up care. Next steps include developing and testing support approaches for rectal cancer survivors, focusing on the common and unique aspects by surgery group and the personnel and resources needed to address those needs.
Supplementary Material
Acknowledgments
This research was made possible by Grant Number R01 CA106912, HRQOL in Colorectal Cancer Survivors with Stomas, and the University of Arizona Cancer Center Support Grant CA023074, from the National Cancer Institute, National Institutes of Health.
Dr. Hornbrook has a research contract with Medial Research Inc., Israel.
Footnotes
Conflicts of Interest:
The other authors have no conflicts of interest to disclose.
Disclaimer
The views expressed in this report are those of the authors and do not necessarily represent the views of Kaiser Permanente or the Department of Veterans Affairs.
Previous Presentation of Findings
An abstract based on a poster presenting preliminary analysis of this data has been published as part of proceedings of the AACR 106th Annual Meeting, April 18–22, 2015; Philadelphia, PA (Krouse RS, Bulkley JE, Altshuler A, Wendel CS, Grant M, Hornbrook MC, Sun V, McMullen CK. Abstract 3431: What are the greatest challenges of rectal cancer survivors? Results of a population-based survey. Cancer Research 08/2015; 75(15 Supplement):3431.).
Author Contributions
Carmit McMullen, Joanna Bulkley, Andrea Altschuler, Christopher Wendel, Marcia Grant, Mark Hornbrook, and Robert Krouse contributed to the conceptualization and design of the study, acquisition of data, analysis and interpretation of the data, drafting the article and reviewing the article. Virginia Sun participated in all the steps mentioned above with the exception of conceptualization and design of the study and the acquisition of data. All authors have all provided final approval of this manuscript.
REFERENCES
- 1.DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64(4):252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 2.National Cancer Institute. [Accessed 2006];SEER Cancer Statistics Review, 1975–2003. http://seer.cancer.gov/csr/1975_2003.
- 3.de Moor J, Mariotto A, Parry C, et al. Cancer survivors in the United States: Prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561–570. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burg MA, Adorno G, Lopez ED, et al. Current unmet needs of cancer survivors: Analysis of open-ended responses to the American Cancer Society Study of Cancer Survivors II. Cancer. 2015;121(4):623–630. doi: 10.1002/cncr.28951. [DOI] [PubMed] [Google Scholar]
- 5.Downing A, Morris EJ, Richards M, et al. Health-Related Quality of Life After Colorectal Cancer in England: A Patient-Reported Outcomes Study of Individuals 12 to 36 Months After Diagnosis. J Clin Oncol. 2015;33(6):616–624. doi: 10.1200/JCO.2014.56.6539. [DOI] [PubMed] [Google Scholar]
- 6.Mrak K, Jagoditsch M, Eberl T, Klingler A, Tschmelitsch J. Long-term quality of life in pouch patients compared with stoma patients following rectal cancer surgery. Colorectal Dis. 2011;13(12):e403–e410. doi: 10.1111/j.1463-1318.2011.02740.x. [DOI] [PubMed] [Google Scholar]
- 7.Otto S, Kroesen AJ, Hotz HG, Buhr HJ, Kruschewski M. Effect of anastomosis level on continence performance and quality of life after colonic J-pouch reconstruction. Dig Dis Sci. 2008;53(1):14–20. doi: 10.1007/s10620-007-9815-3. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt CE, Bestmann B, Kuchler T, Longo WE, Kremer B. Prospective evaluation of quality of life of patients receiving either abdominoperineal resection or sphincter-preserving procedure for rectal cancer. Ann Surg Oncol. 2005;12(2):117–123. doi: 10.1245/ASO.2005.12.036. [DOI] [PubMed] [Google Scholar]
- 9.Krouse RS, Herrinton LJ, Grant M, et al. Health-related quality of life among long-term rectal cancer survivors with an ostomy: Manifestations by sex. J Clin Oncol. 2009;27(28):4664–4670. doi: 10.1200/JCO.2008.20.9502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pachler J, Wille-Jorgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev. 2005;(2):CD004323. doi: 10.1002/14651858.CD004323.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW, Tekkis PP. A meta-analysis of quality of life for abdominoperineal excision of rectum versus anterior resection for rectal cancer. Ann Surg Oncol. 2007;14(7):2056–2068. doi: 10.1245/s10434-007-9402-z. [DOI] [PubMed] [Google Scholar]
- 12.Fish D, Temple LK. Functional consequences of colorectal cancer management. Surg Oncol Clin N Am. 2014;23(1):127–149. doi: 10.1016/j.soc.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Zolciak A, Bujko K, Kepka L, Oledzki J, Rutkowski A, Nowacki MP. Abdominoperineal resection or anterior resection for rectal cancer: Patient preferences before and after treatment. Colorectal Dis. 2006;8(7):575–580. doi: 10.1111/j.1463-1318.2006.01000.x. [DOI] [PubMed] [Google Scholar]
- 14.McMullen CK, Hornbrook MC, Grant M, et al. The greatest challenges reported by long-term colorectal cancer survivors with stomas. J Support Oncol. 2008;6(4):175–182. [PubMed] [Google Scholar]
- 15.Mohler MJ, Coons SJ, Hornbrook MC, et al. The health-related quality of life in long-term colorectal cancer survivors study: Objectives, methods and patient sample. Curr Med Res Opin. 2008;24(7):2059–2070. doi: 10.1185/03007990802118360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziv Y, Zbar A, Bar-Shavit Y, Igov I. Low anterior resection syndrome (LARS): Cause and effect and reconstructive considerations. Tech Coloproctol. 2013;17(2):151–162. doi: 10.1007/s10151-012-0909-3. [DOI] [PubMed] [Google Scholar]
- 17.Pucciani F. A review on functional results of sphincter-saving surgery for rectal cancer: the anterior resection syndrome. Updates Surg. 2013;65(4):257–263. doi: 10.1007/s13304-013-0220-5. [DOI] [PubMed] [Google Scholar]
- 18.Wendel CS, Grant M, Herrinton L, et al. Reliability and validity of a survey to measure bowel function and quality of life in long-term rectal cancer survivors. Qual Life Res. 2014;23(10):2831–2840. doi: 10.1007/s11136-014-0724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chongpison Y, Hornbrook MC, Harris RB, et al. Self-reported depression and perceived financial burden among long-term rectal cancer survivors. Psychooncology. 2015 doi: 10.1002/pon.3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grant M, Ferrell B, Dean G, Uman G, Chu D, Krouse R. Revision and psychometric testing of the City of Hope Quality of Life-Ostomy Questionnaire. Qual Life Res. 2004;13(8):1445–1457. doi: 10.1023/B:QURE.0000040784.65830.9f. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 22.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26(7):709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Temple LK, Bacik J, Savatta SG, et al. The development of a validated instrument to evaluate bowel function after sphincter-preserving surgery for rectal cancer. Dis Colon Rectum. 2005;48(7):1353–1365. doi: 10.1007/s10350-004-0942-z. [DOI] [PubMed] [Google Scholar]
- 24.Smith T, Stein KD, Mehta CC, et al. The rationale, design, and implementation of the American Cancer Society's studies of cancer survivors. Cancer. 2007;109(1):1–12. doi: 10.1002/cncr.22387. [DOI] [PubMed] [Google Scholar]
- 25.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–146. [PubMed] [Google Scholar]
- 26.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with IDC-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 27.Ryan G, Bernard H. Techniques to Identify Themes. Field Methods. 2003;15(1):85–109. [Google Scholar]
- 28.Orsini RG, Thong MS, van de Poll-Franse LV, et al. Quality of life of older rectal cancer patients is not impaired by a permanent stoma. Eur J Surg Oncol. 2013;39(2):164–170. doi: 10.1016/j.ejso.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Phatak UR, Kao LS, You YN, et al. Impact of ileostomy-related complications on the multidisciplinary treatment of rectal cancer. Ann Surg Oncol. 2014;21(2):507–512. doi: 10.1245/s10434-013-3287-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soni A. STATISTICAL BRIEF #451: Experiences with Health Care Providers among Cancer Survivors, U.S. Civilian Noninstitutionalized Population, 2011. [Accessed 10/2014];2011 http://meps.ahrq.gov/mepsweb/data_files/publications/st451/stat451.shtml. [PubMed]
- 31.Di Fabio F, Koller M, Nascimbeni R, Talarico C, Salerni B. Long-term outcome after colorectal cancer resection. Patients' self-reported quality of life, sexual dysfunction and surgeons' awareness of patients' needs. Tumori. 2008;94(1):30–35. doi: 10.1177/030089160809400107. [DOI] [PubMed] [Google Scholar]
- 32.Meyerhardt JA, Mangu PB, Flynn PJ, et al. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol. 2013;31(35):4465–4470. doi: 10.1200/JCO.2013.50.7442. [DOI] [PubMed] [Google Scholar]
- 33.National Comprehensive Cancer Network. [Accessed October 26, 2015];NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Rectal Cancer, Version 2. 2015 http://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf. [Google Scholar]
- 34.National Comprehensive Cancer Network. [Accessed October 31, 2015];NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Survivorship, Version 2. 2015 http://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.