Abstract
Removable dentures made of poly (methyl methacrylate) (PMMA) are prone to bacterial adherence and dental plaque formation, which is called denture plaque. Denture plaque-associated infection is a source of serious dental and medical complications in the elderly. 2-Methacryloyloxyethyl phosphorylcholine (MPC) is a well-known biomedical material that exhibits marked antithrombogenicity and tissue compatibility because of its high resistance to protein adsorption and cell adhesion. Therefore, MPC polymer coatings are suggested to have the potential to inhibit plaque deposition on the surface of PMMA dentures. However, coating MPC polymer on the surface of a PMMA denture is a complex procedure that requires specialized equipment, which is regarded as a major barrier to its clinical application.
Here, we introduce a new MPC polymer treatment procedure that uses poly (MPC-co-BMA-co-MPAz) (PMBPAz) to prevent denture plaque deposition on removable dentures. This procedure enables the MPC coating of PMMA denture surfaces in a simple and stable manner that is resistant to various chemical and mechanical stresses due to the MPC layer of PMBPAz that is covalently bound to the PMMA surface by ultraviolet light irradiation. In addition, the procedure does not require any specialized equipment and can be completed by clinicians within 2 min. We applied this procedure in a clinical setting and demonstrated its clinical utility and efficacy in inhibiting plaque deposition on removable dentures.
Keywords: Medicine, Issue 118, MPC polymer, PMBPAz, biofilm formation, complete denture, PMMA, plaque inhibition, oral health
Introduction
Oral healthcare plays an important role in the prevention of opportunistic infections and aspiration pneumonia in the physically vulnerable elderly. Oral healthcare, consisting of brushing after each meal, cleaning dentures, and receiving professional oral health care, plays a vital role in reducing the incidence of such diseases1-3. In particular, poor oral hygiene is strongly associated with aspiration pneumonia in the physically vulnerable elderly. Therefore, more attention should be paid to the oral health care of elderly patients, who have limited ability to clean their dentures by themselves4.
Even in developed countries, the use of acrylic, resin-based removable dentures remains the most common treatment option for edentulous elderly patients5. Given their high water absorption capacity, microporous surface, and hydrophobic nature, acrylic denture bases constructed from polymethyl methacrylate (PMMA) easily accumulate dental plaque on their surfaces, which is called denture plaque.
2-Methacryloyloxyethyl phosphorylcholine (MPC) polymers are well-known biomedical polymeric materials6 that have remarkable antithrombogenicity and tissue compatibility because of their high resistance to protein adsorption and cell adhesion7-11. MPC polymer coatings have been applied in various medical devices to prevent infection12 and have been suggested to have the potential to prevent denture plaque accumulation on PMMA denture surfaces13. The challenge in the clinical application of MPC polymers to PMMA dentures is to reliably bind them to PMMA surfaces in a simple and stable manner. Previously, MPC polymers were reported to be stably bound to PMMA surfaces by a grafting technique and to have the potential to inhibit plaque accumulation. However, the grafting technique is not simple and requires specialized equipment, which makes its clinical application challenging. Here, we describe a new MPC coating procedure that utilizes photoreactive phospholipid polymers-specifically, a photoreactive methacrylate derivative, 2-methacryloyloxyethyl-4-azidobenzoate (MPAz)-synthesized to accomplish a variety of surface modifications of different types of materials. MPAz was co-polymerized with MPC polymers and n-butyl methacrylate (BMA) to yield poly (MPC-co-BMA-co-MPAz) (PMBPAz). PMBPAz can covalently bind to the surfaces of PMMA dentures via activation of the azide groups in MPAz under ultraviolet (UV) light irradiation14. The procedure does not require any specialized equipment and can be completed by clinicians within 2 min. We also applied this procedure in a clinical setting and demonstrated its clinical utility and efficacy in inhibiting plaque deposition on removable dentures.
Protocol
1. Preparation of PMBPAz Solution (Figure 1)
Synthesize MPC following a previously reported industrial procedure15.
Synthesize the photoreactive MPC polymer PMBPAz using conventional radical polymerization of MPC, BMA, and MPAz in ethanol, as previously described14. NOTE: PMBPAz should contain 60%, 30%, and 10% (mol %) of the aforementioned monomer units, respectively. Refrigerate the PMBPAz dissolved in ethanol to prepare a 0.5 wt% solution before use.
Before treating the PMMA surface, allow the PMBPAz ethanol solution to stand for 30 min at room temperature.
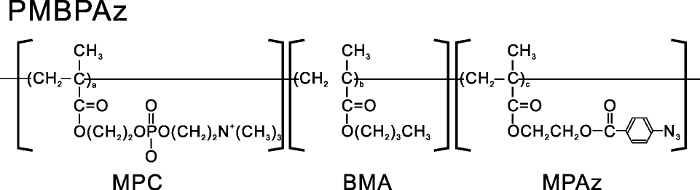 Figure 1. Chemical structural formula of the photoreactive MPC polymer PMBPAz. PMBPAz was constructed using an MPC unit, a BMA unit, and an MPAz unit. Please click here to view a larger version of this figure.
Figure 1. Chemical structural formula of the photoreactive MPC polymer PMBPAz. PMBPAz was constructed using an MPC unit, a BMA unit, and an MPAz unit. Please click here to view a larger version of this figure.
2. PMBPAz Treatment of a Complete PMMA Denture (Figure 2)
Mechanically clean the denture for 3 min using a denture brush.
Chemically clean the denture for 5 min in an ultrasonic bath sonicator with a denture cleaner including 2.0% sodium hypochlorite and under the following sonication conditions: frequency, 50/60 Hz; phase number, 1φ; and oscillating frequency, 28 kHz.
Before performing the surface modification with PMBPAz, wash the denture surface by immersion in ethanol. After the ethanol wash, let the denture surface dry by itself, as ethanol is a volatile compound.
Apply 1 ml of PMBPAz ethanol solution directly to the entire surface of the denture using a brush applicator. Subsequently, keep the denture at room temperature and atmospheric pressure for 10 min to allow the solvent to evaporate in an ethanol vapor atmosphere. Allow it to dry. Repeat these steps twice.
Irradiate the denture surface with UV light for 2 min (at 254 nm).
Immerse the PMBPAz-treated denture in distilled water for 5 min before use.
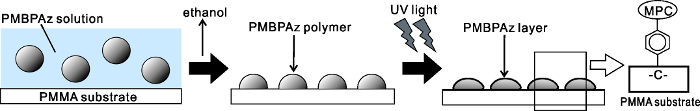 Figure 2. Fabrication of a surface modified using the photoreactive MPC polymer PMBPAz. The PMBPAz polymer can covalently bind to PMMA by applying UV irradiation. Please click here to view a larger version of this figure.
Figure 2. Fabrication of a surface modified using the photoreactive MPC polymer PMBPAz. The PMBPAz polymer can covalently bind to PMMA by applying UV irradiation. Please click here to view a larger version of this figure.
3. Evaluation of Denture Plaque Deposition
Use the PMBPAz-treated denture at home for 2 weeks. As a control, repeat the same procedure, excluding the treatment with the PMBPAz.
After a patient has used the denture for 2 weeks (used about 12 to 14 hr per day), rinse it with tap water to remove any loose food particles, and then stain it with a 0.25% methylene blue disclosing solution for 1 min.
Clean any stains present on the denture surface in distilled water using an ultrasonic bath sonicator for 30 sec.
Capture images at a 90° angle on a wax seat with a digital camera by using a white-light system. Capture images with the same focal object distance, exposure time, and intensity of illumination. Capture images from 3 different directions to get mucosal, right, and left polished surface images.
- Calculate the stained area and quantify it using an image analysis software for the entire denture surface16.
- Select the denture area using the "magnetic lasso" tool from the captured denture image. Subsequently, change the red-colored channel to highlight the plaque area from the denture area image. Select all plaque areas using the "magic wand" tool (tolerance level 8) and the "select similar" tool from the denture area.
- Count the total number of pixels for each image. Thereafter, calculate the percentage plaque index of the area covered on the denture from the pixel count of these images (total plaque pixels/total denture surface pixels). Evaluate the statistical differences between the stained areas on the PMBPAz-treated and untreated dentures (ANOVA, p <0.05).
Representative Results
PMBPAz treatment enables the MPC coating of PMMA surfaces through a simple and short method and maintains the plaque inhibition effect of the MPC polymer. This procedure does not require any specialized equipment and can be performed chair-side by clinicians within 2 min. Following protocol step 2, the PMBPAz treatment of removable complete dentures from 11 edentulous patients was successfully conducted in a clinical setting without any substantial problems. The mean percentage plaque indexes on the mucosal and polished surfaces of the control dentures were 40.7% ± 19.9% and 28.0% ± 16.8%, respectively, while those of PMBPAz-treated dentures were 17.4% ± 12.0% and 15.0% ± 9.9%, respectively. The PMBPAz treatment of PMMA denture surfaces significantly inhibited the deposition of denture plaque for at least 2 weeks (n = 11, p <0.05; Figure 3A, 3B, and 3C).
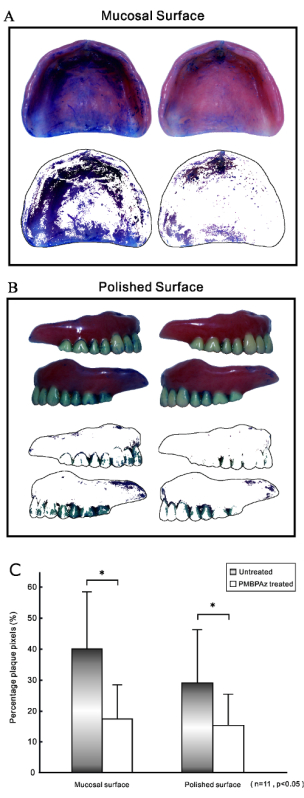 Figure 3. Assessment of plaque deposition on maxillary complete dentures after use in patients for 2 weeks. (A) The total denture area of the mucosal surface after staining and digitization (left: untreated, right: PMBPAz-treated) and the plaque area of the mucosal surface after selection. Visual inspection of the control denture images revealed that the stained plaque was concentrated in the areas corresponding to the mucosal surfaces of the alveolar ridge and that the stained plaque areas were consistently and markedly decreased by PMBPAz treatment. (B) Total denture area of the polished surfaces after staining and digitization (left: untreated, right: PMBPAz-treated) and plaque area of the polished surfaces after selection. Visual inspection of the control denture images revealed that the stained plaque was concentrated in the areas corresponding to the interdental papilla regions of the polished surfaces and that the stained plaque areas were consistently and markedly decreased by PMBPAz treatment. (C) The mean percentage plaque pixels on the mucosal and polished surfaces of untreated and PMBPAz-treated dentures. The PMBPAz treatment of the mucosal and polished surfaces significantly inhibited the deposition of denture plaque. The data shows the mean ± standard deviation. (n = 11, p <0.05). Please click here to view a larger version of this figure.
Figure 3. Assessment of plaque deposition on maxillary complete dentures after use in patients for 2 weeks. (A) The total denture area of the mucosal surface after staining and digitization (left: untreated, right: PMBPAz-treated) and the plaque area of the mucosal surface after selection. Visual inspection of the control denture images revealed that the stained plaque was concentrated in the areas corresponding to the mucosal surfaces of the alveolar ridge and that the stained plaque areas were consistently and markedly decreased by PMBPAz treatment. (B) Total denture area of the polished surfaces after staining and digitization (left: untreated, right: PMBPAz-treated) and plaque area of the polished surfaces after selection. Visual inspection of the control denture images revealed that the stained plaque was concentrated in the areas corresponding to the interdental papilla regions of the polished surfaces and that the stained plaque areas were consistently and markedly decreased by PMBPAz treatment. (C) The mean percentage plaque pixels on the mucosal and polished surfaces of untreated and PMBPAz-treated dentures. The PMBPAz treatment of the mucosal and polished surfaces significantly inhibited the deposition of denture plaque. The data shows the mean ± standard deviation. (n = 11, p <0.05). Please click here to view a larger version of this figure.
Discussion
Mechanism of the PMBPAz Coating
It is challenging to bind MPC polymers to a PMMA surface in a simple and stable manner. Here, we used a new photoreactive monomer bearing a phenylazide group, MPAz, which polymerizes with other monomers through a conventional free-radical polymerization procedure, resulting in a polymer with phenylazide side chains. The phenylazide groups are decomposed by UV irradiation to form nitrene groups, which are highly reactive radical groups that can covalently bind to alkyl groups. Thus, MPC-based polymers containing MPAz units can be bound to the surfaces of various materials by UV irradiation. The advantages of PMBPAz coating include a short reaction time and efficient reaction conversion. In addition, photoirradiation does not have any significant adverse effects on the bulk properties of the surface of materials when used at appropriate wavelengths17,18.
PMBPAz Coating Procedure
Previously, we reported that the surface modification layer formed on a PMMA surface by the MPC-polymer grafting technique was resistant to mechanical stress19. However, the clinical application of this technique may not be possible due to its technical complexity because the procedure includes several steps and the polymerization efficiency is low. Moreover, it requires highly specialized experimental equipment, which is currently unavailable in clinical settings19.
Against this background, as an effective alternative, the PMBPAz coating procedure only required the dentures to be painted and exposed and could thus be completed within 2 min in a clinical setting. The only additional equipment required is a UV irradiation unit, which is easy to operate and is also inexpensive. These characteristics of the PMBPAz treatment procedure described in this paper allow for the easier application of the MPC coating in clinical settings.
Effectiveness
Dental plaque, which adheres to denture surfaces, was visualized by staining with methylene blue. The uneven surface area of a denture that has not been polished is prone to denture plaque accumulation; such surfaces are difficult for patients to clean thoroughly, as demonstrated by the staining of the denture surface (Figure 3). However, the PMBPAz treatment of PMMA denture surfaces controlled the formation of biofilm after clinical usage for 2 weeks. This suggests that the MPC coating method introduced in this study is durable and resistant to the clinical usage of dentures for at least 2 weeks.
Conclusion and Lingering Questions
The protocol described in this paper for PMBPAz treatment of PMMA denture surfaces is feasible in clinical settings and effectively inhibits denture plaque deposition. Therefore, it has the potential to improve denture hygiene in the elderly. This method has a distinct advantage over conventional denture cleaning procedures because it aims to prevent denture plaque accumulation. In general, a majority of strategies to improve denture hygiene are associated with technical complexity because they address the removal of plaque already adhered to denture surfaces through the use of mechanical brushing along with denture cleaning agents. The present method might be particularly useful in long-term healthcare facilities and for individuals who are not able to take care of their dentures, such as those suffering from post-stroke hemiparesis.
We twice applied a PMBPAz-ethanol solution directly to denture surfaces using a brush applicator and then irradiated the surfaces with UV light for 2 min. In the future, this protocol needs to be re-evaluated to identify the optimal conditions that maximize the effects of the PMBPAz treatment. Subsequently, the optimum wavelength of UV irradiation, the treatment interval, and the method of coating the dentures with the MPC solution should also be determined. In this study, we found that the effects of the PMBPAz treatment lasted for at least 2 weeks, but no long-term observations were conducted, which should be included in future studies.
Disclosures
We have no disclosures or financial support.
Acknowledgments
The authors wish to thank all of the participants, dentists, and assistants for their participation in this study. We sincerely thank Professor Hirotaka Kuwata and Assistant Professor Hirobumi Morisaki, Department of Oral Microbiology and Immunology, Showa University School of Dentistry, for their support.
References
- Watando A, et al. Daily oral care and cough reflex sensitivity in elderly nursing home patients. Chest. 2004;126:1066–1070. doi: 10.1378/chest.126.4.1066. [DOI] [PubMed] [Google Scholar]
- Bassim CW, Gibson G, Ward T, Paphides BM, DeNucci DJ. Modification of the risk of mortality from pneumonia with oral hygiene care. J. Am. Geriatr. Soc. 2008;56:1601–1607. doi: 10.1111/j.1532-5415.2008.01825.x. [DOI] [PubMed] [Google Scholar]
- Ishikawa A, Yoneyama T, Hirota K, Miyake Y, Miyatake K. Professional oral health care reduces the number of oropharyngeal bacteria. J. Dent. Res. 2008;87:594–598. doi: 10.1177/154405910808700602. [DOI] [PubMed] [Google Scholar]
- Hosokawa R. Prosthodontic interventions for special-needs patients. J Prosthodont Res. 2014;58:69–70. doi: 10.1016/j.jpor.2014.03.004. [DOI] [PubMed] [Google Scholar]
- Parvizi A, Lindquist T, Schneider R, Williamson D, Boyer D, Dawson DV. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J. Prosthodont. 2004;13:83–89. doi: 10.1111/j.1532-849X.2004.04014.x. [DOI] [PubMed] [Google Scholar]
- Ishihara K, Ueda T, Nakabayashi N. Preparation of phospholipid polylmers and their properties as polymer hydrogel membranes. Polym. J. 1990;22:355–360. [Google Scholar]
- Ishihara K, Aragaki R, Ueda T, Watenabe A, Nakabayashi N. Reduced thrombogenicity of polymers having phospholipid polar groups. J. Biomed. Mater. Res. 1990;24(8):1069–1077. doi: 10.1002/jbm.820240809. [DOI] [PubMed] [Google Scholar]
- Ishihara K, Ziats NP, Tierney BP, Nakabayashi N, Anderson JM. Protein adsorption from human plasma is reduced on phospholipid polymers. J. Biomed. Mater. Res. 1991;25(11):1397–1407. doi: 10.1002/jbm.820251107. [DOI] [PubMed] [Google Scholar]
- Ishihara K, Nomura H, Mihara T, Kurita K, Iwasaki Y, Nakabayashi N. Why do phospholipid polymers reduce protein adsorption? J. Biomed. Mater. Res. 1998;39(2):323–330. doi: 10.1002/(sici)1097-4636(199802)39:2<323::aid-jbm21>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Ishihara K. Bioinspired phospholipid polymer biomaterials for making high performance artificial organs. Sci. Technol. Adv. Mater. 2000;1(3):131–138. [Google Scholar]
- Iwasaki Y, Ishihara K. Cell membrane-inspired phospholipid polymers for developing medical devices with excellent biointerfaces. Sci. Technol. Adv. Mater. 2012;13(6):064101 (10pp). doi: 10.1088/1468-6996/13/6/064101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N, Chen C, Melo MA, et al. A novel protein-repellent dental composite containing 2-methacryloyloxyethyl phosphorylcholine. Int J Oral Sci. 2015;7:103–109. doi: 10.1038/ijos.2014.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirota K, Yumoto H, Miyamoto K, et al. MPC-polymer reduces adherence and biofilm formation by oral bacteria. J Dent Res. 2011;90:900–905. doi: 10.1177/0022034511402996. [DOI] [PubMed] [Google Scholar]
- Fukazawa K, Ishihara K. Synthesis of photoreactive phospholipid polymers for use in versatile surface modification of various materials to obtain extreme wettability. ACS Appl. Mater. Interfaces. 2013;5(15):6832–6836. doi: 10.1021/am402051e. [DOI] [PubMed] [Google Scholar]
- Ishihara K, Ueda T, Nakabayashi N. Preparation of phospholipid polymers and their properties as polymer hydrogel membranes. Polym. J. 1990;22(5):355–360. [Google Scholar]
- Coulthwaite L, Verran J. Evaluation of in vivo denture plaque assessment methods. Br Dent J. 2009;207(E12):282–283. doi: 10.1038/sj.bdj.2009.854. [DOI] [PubMed] [Google Scholar]
- He D, Susanto H, Ulbricht M. Photo-irradiation for preparation, modification and stimulation of polymeric membranes. Prog Polym Sci. 2009;34:62–98. [Google Scholar]
- Nakayama Y. Surface macromolecular architectural designs using photo-graft copolymerization based on photochemistry of benzyl N,N-diethyldithiocarbamate. Macromolecules. 1996;29:8622–8630. [Google Scholar]
- Takahashi N, Iwasa F, Inoue Y, Morisaki H, Ishihara K, Baba K. Evaluation of the durability and antiadhesive action of 2-methacryloyloxyethyl phosphorylcholine grafting on an acrylic resin denture base. J. Prosthet. Dent. 2014;112(2):194–203. doi: 10.1016/j.prosdent.2013.08.020. [DOI] [PubMed] [Google Scholar]


