Introduction
Gastric cancer remains a common problem in Japan. Until recently, the primary approach to reducing the burden of disease has been surveillance (regular gastroscopic evaluations) programs with the goal of identifying early and still curable lesions. Surveillance s is designed to discover incidence cases and as such is not preventative. Whenever possible primary prevention is preferred over surveillance as prevention is more efficient and always less expensive.
Surveillance
For more than 100 years gastric cancer has been known to be tightly associated with atrophic gastritis and this understanding was responsible for considerable research efforts aimed at identifying the cause of gastritis 1). The discovery of Helicobacter pylori and proof that it was the cause of gastritis suggested that it might be possible to heal or even prevent gastritis and thus prevent gastric cancer. The data are now sufficient to recommend a change in the approach to gastric cancer from surveillance to a strategy that emphasizes prevention with targeted surveillance.
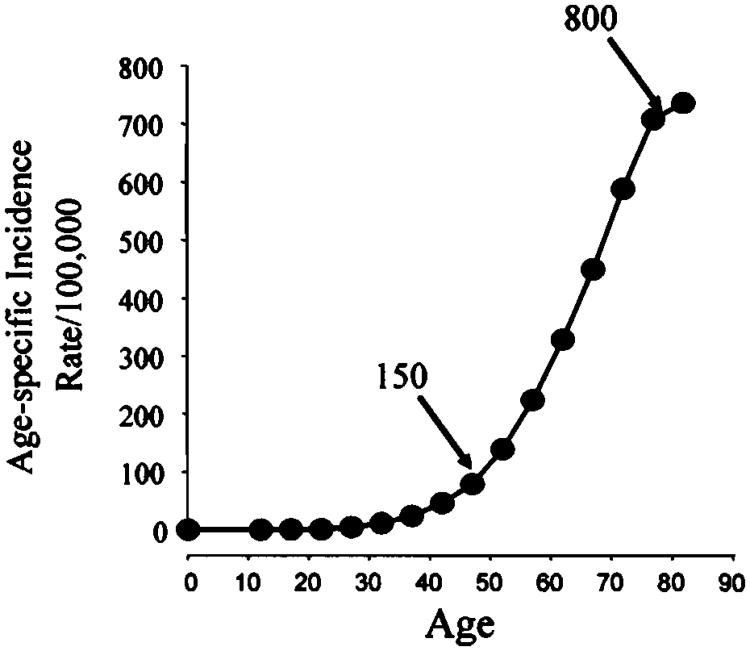
Because gastric cancer is closely linked with atrophic gastritis it is possible to risk stratify patients based on the extent and severity of atrophic gastritis. The cancer risk associated with a normal uninflamed stomach is essentially zero. The risk increases with the extent and severity of gastritis (ie. it is very low in non-atrophic gastritis and with antral restricted gastritis and increases in proportion to the extent and severity of atrophic corpus gastritis). Risk is highest when the stomach is atrophic and achlorhydria is present 2-4). Although atrophy typically develops gradually, the rate of progression varies among population and even among birth cohorts. The cancer risk increases with age and the shape gastric cancer incidence plot shows that after a relatively long latent period the risk increases exponentially after about age 50 (Figure 1). This rapid increase in incidence has resulted in age being used as a criteria for starting surveillance programs with the idea that screening during the latent period would not be cost effectiveness. While the risk can be identified for each birth cohort (eg, those age 50), it is important to remember that the published risk is actually the average risk made up of patients with risks averaging from none to very high. As such, annual surveillance as practiced is inefficient as it only examines a small proportion of those at risk, it includes both those that can and cannot benefit, allows progression of risk, and has a limited or no “preventive” role. For example, if we consider what happens in a surveillance program based on the data from Figure 1. In this model annual surveillance begins at age 50 (incidence approximately 150/100,000/yr) and continues until age 85 (incidence approximately 800/100,000/yr). We will assume that all incident cancers are discovered at each procedure. At age 50, one would identify approximately 1 cancer per 700 procedures and the number would increase yearly; at age 85 one would identify 1 gastric cancer for every 125 procedures.
Figure 1.
Illustrative age-specific gastric cancer incidence for Japanese men.
Limitations of surveillance
Although such a program would identify many early cancers and save many lives, because the age-specific incidence includes the full range of patients (ie, those with no infection and no risk and those with high risk) it is very inefficient. If it were risk stratified and limited to those at high risk and excluded those with no possible chance to benefit (ie, no infection, no gastritis) and those with very low yield (ie, nonatrophic gastritis), the yield would be high independent of the age group. We define this as targeted surveillance. The second problem is that standard surveillance has no effect on the natural history of the disease and the patients enter the program with an average risk of 150/100,000 cancers/year and that risk increases 533% despite the fact that that are undergoing annual surveillance. Until recently, this was probably the best one could do to reduce cancer deaths.
Prevention plus targeted surveillance
Cancer prevention hinges on prevention of atrophic gastritis and gastric atrophy 5, 6). We now recognize that Helicobacter pylori eradication done before the development of atrophy results in healing of the gastritis, elimination of inflammation, and prevention of the progressive mucosal damage thus development of atrophy. Helicobacter pylori eradication after the onset of mild to moderate atrophy promotes some return of function, prevents further increases in atrophy, and eliminates or reduces the age-related increase in risk. It seems likely that because it is associated with some return of function, the risk not only stabilizes but also actually decreases 7). The risk may further decrease over time. If in our model with screening beginning at age 50 we now include an evaluation of Helicobacter pylori status, we can divide the patient population into risk groups and manage them accordingly (Table 1). At age 50 most would likely fall into the low risk groups and require no follow-up after successful Helicobacter pylori eradication. After Helicobacter pylori eradication surveillance could be limited to the higher risk populations (ie, prevention plus targeted surveillance).
Table 1. Risk stratification and need for surveillance after H. pylori eradication.
| Group | Risk | Surveillance needed? |
|---|---|---|
| Never infected | None | No |
| Infected | ||
| Non-atrophic gastritis | None | No |
| Mild atrophic gastritis | Slight | No |
| Moderate atrophy | Moderate | Probably yes |
| Severe atrophy | High | Yes |
Because we expect that Helicobacter pylori eradication to prevent the subsequent age-related increases in risk and likely to actually reduce risk, those patients should be entered into clinical trials to define the appropriate surveillance intervals for each of the groups as well as how long surveillance would be needed. Other trials could examine whether additional risk reductions could be obtained over and above that accursed with Helicobacter pylori eradication. For example, risk reduction programs might include smoking cessation programs, changes in the diet (ie, less salt, more fresh fruits and vegetables), and drugs such as gastroprotectives or anti-inflammatory agents. The fact that the risk stratification would identify populations with similar risks would allow such research to be conducted efficiently.
Risk stratification
Risk stratification is related to identification of the severity and extent of atrophy. Approaches to identify risk range from identification of the atrophic border at endoscopy, histologically examination of directed gastric biopsy, and noninvasively by measuring serum pepsinogen levels and pepsinogen I/II ratios 8, 9). If endoscopy is done, we recommend biopsy of both the antrum and corpus (Figure 2). This approach uses two more specimens (CL1 and CG3 in Figure 2) than recommended by the Sydney system 10 which ensure that less extensive atrophy is identified as the Sydney system recommendations systematically underestimate the presence of atrophy 11, 12). This is called the Houston or the Baylor System 11). The corpus biopsies should be separated from the antral biopsies and because the proximal extent of atrophy determines risk, greater and lesser curvature biopsies should be also kept separate. The finding of intestinal metaplasia identifies the presence of atrophy but the most common manifestation of atrophy is not intestinal metaplasia but is pseudopyloric or mucus metaplasia where the corpus mucosa takes on the appearance of antral mucosa. If the corpus biopsies are not separated from the antral biopsies, the pathologist may mistake them for antrum and mischaracterize the extent of atrophy. Clues to allow the appropriate characterization are knowledge of the location (ie, corpus instead of antrum) and staining for pepsinogen I which if positive would identify that they were actually corpus instead of antrum (Figure 3) 11-13). Antral biopsies would usually stain positive for gastrin but that level of conformation is generally not needed. For practical purposes all of the antral specimens can be placed into one bottle but the lesser and greater curve corpus biopsies should be kept separate and labeled as to site. It is not necessary to separate the two lesser curvature or two greater curvature specimens because if one shows atrophy and other does not, the atrophic one is always the more distal one. Thus, one should provide the pathology department with a minimum of 3 specimen contains (antral, lesser curve corpus, greater curve corpus). After grading the various histologic features, we recommend the results be entered into the OLGA histology-based staging system. It is preferred as it provides the clinician an estimate of cancer risk based on the extent and severity of atrophy 14).
Figure 2. Recommended sites for gastric biopsy for identification of the extent of atrophy.
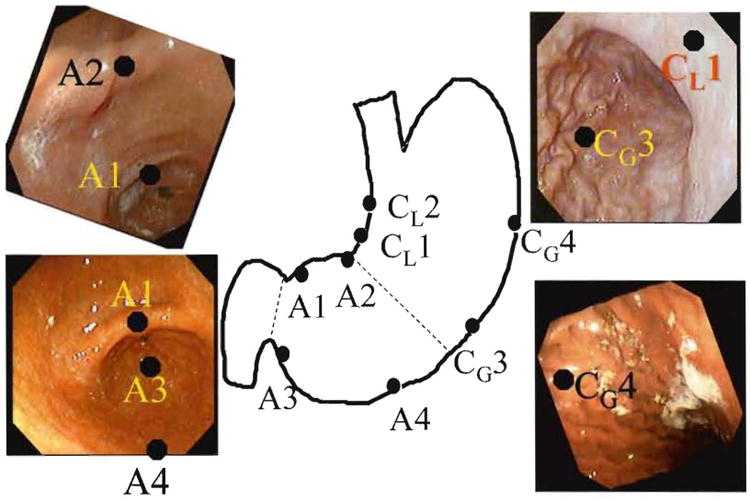
Recommended antral (A) sites and corpus (C) biopsy sites are shown in the schematic and in endoscopic photographs (note Cl3 is not shown in the photo). It is important that antrum and corpus be submitted separately and that lesser and greater curvature corpus sites be separately identified (see test for details). All specimens can be embedded in the same block of compartmental embedding blocks are used.
Figure 3. Pseudopyloric metaplasia.
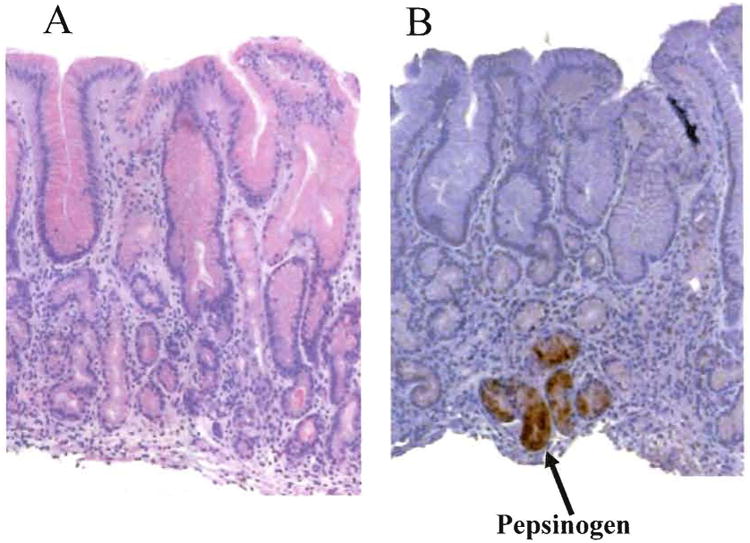
Corpus biopsies with pseudopyloric metaplasia. A shows mucosa that without knowledge of its source as corpus mucosa would likely be identified as antrum by the pathologist. B. Immunohistochemical staining for pepsinogen I showing positive staining confirming that the tissue is actually atrophic corpus mucosa (courtesy of the Gastrointestinal mucosal pathology laboratory, Baylor College of Medicine, Hala El-Zimaity director).
For large scale screening, non-invasive testing is preferred as it is more efficient and more cost effective. Non-invasive testing would likely employ tests for active infection such as the urea breath or fecal Helicobacter pylori antigen testing for testing for Helicobacter pylori infection status and pepsinogen testing for risk stratification for the presence, absence, and degree of mucosal atrophy. Only those with some degree of atrophy would be considered for endoscopy and only after Helicobacter pylori eradication. All Helicobacter pylori infected would receive Helicobacter pylori eradication and confirmatory Helicobacter pylori eradication testing.
Country-wide instead of age-related screening
Because Helicobacter pylori eradication done before atrophic gastritis develops heals gastritis and prevents the development of atrophic gastritis and gastric cancer, the earlier in the natural history of the disease it is done, the higher will be the proportion of those in whom the cancer risk is eliminated. It follows that countrywide Helicobacter pylori testing should be done in all adults to find and eliminate Helicobacter pylori infections If one desires, one can also check the Helicobacter pylori status of children but this would be restricted to the children of infected parents. Such a program of Helicobacter pylori eradication would result a rapidly falling incidence of gastric cancer and it elimination of gastric cancer in Japan within a few decades.
Gastric cancer surveillance programs are now obsolete
Screening for gastric cancer based on identifying the population at risk using indirect testing (ie, hypo chlorhydria/achlorhydria – a pepsinogen surrogate) followed by radiographic studies was suggested more than 50 years ago 15, 16. Although surveillance is now done using more modern and effective methods, the approach can not prevent cancer but can only reduce cancer deaths. Helicobacter pylori eradication and targeted surveillance can do both. I recommend that Japan abandon currently constructed gastric cancer surveillance programs and substitute cancer prevention plus targeted surveillance programs. Targeted surveillance could also probably be discontinued within 20 years and the health care resources currently directed to gastric cancer could be redirected elsewhere.
Support and Potential Conflicts of Interest
This material is based upon work supported in part by the Office of Research and Development Medical Research Service Department of Veterans Affairs and by Public Health Service grant DK56338 which funds the Texas Medical Center Digestive Diseases Center and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the VA or NIH. We also thank Dr. Claudia A. Kozinetz for the assistance with study designs.
In the last 3 years, Dr. Graham has received small amounts of grant support and/or free drugs or urea breath tests from Meretek, Jannsen/Eisai, and TAP, and BioHit for investigator initiated and completely investigator controlled research. Dr. Graham is a consultant for Novartis in relation to vaccine development for treatment or prevention of Helicobacter pylori infection. Dr. Graham is a also paid consultant for Otsuka Pharmaceuticals and until July 2007 was member of the Board of Directors of Meretek, Diagnostics, the manufacturer of the 13C-urea breath test. Dr. Graham also receives royalties on the Baylor College of Medicine patent covering materials related to 13C-urea breath test.
References
- 1.Howson CP, Hiyama T, Wynder EL. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev. 1986;8:1–27. doi: 10.1093/oxfordjournals.epirev.a036288. [DOI] [PubMed] [Google Scholar]
- 2.Graham DY. Helicobacter pylori infection is the primary cause of gastric cancer. J Gastroenterol. 2000;35(12):90–97. [PubMed] [Google Scholar]
- 3.Graham DY, Shiotani A. The time to eradicate gastric cancer is now. Gut. 2005;54:735–738. doi: 10.1136/gut.2004.056549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham DY, Uemura N. Natural history of gastric cancer after Helicobacter pylori eradication in Japan: after endoscopic resection, after treatment of the general population, and naturally. Helicobacter. 2006;11:139–143. doi: 10.1111/j.1523-5378.2006.00391.x. [DOI] [PubMed] [Google Scholar]
- 5.Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, Taniyama K, Sasaki N, Schlemper RJ. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–789. doi: 10.1056/NEJMoa001999. [DOI] [PubMed] [Google Scholar]
- 6.Wong BC, Lam SK, Wong WM, Chen JS, Zheng TT, Feng RE, Lai KC, Hu WH, Yuen ST, Leung SY, Fong DY, Ho J, Ching CK, Chen JS. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004;291:187–194. doi: 10.1001/jama.291.2.187. [DOI] [PubMed] [Google Scholar]
- 7.Graham DY, Shiotani A, El-Zimaity HM. Chromoendoscopy points the way to understanding recovery of gastric function after Helicobacter pylori eradication. Gastrointest Endosc. 2006;64:686–690. doi: 10.1016/j.gie.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Miki K, Urita Y. Using serum pepsinogens wisely in a clinical practice. J Dig Dis. 2007;8:8–14. doi: 10.1111/j.1443-9573.2007.00278.x. [DOI] [PubMed] [Google Scholar]
- 9.nis-Ribeiro M, Yamaki G, Miki K, Costa-Pereira A, Matsukawa M, Kurihara M. Meta-analysis on the validity of pepsinogen test for gastric carcinoma, dysplasia or chronic atrophic gastritis screening. J Med Screen. 2004;11:141–147. doi: 10.1258/0969141041732184. [DOI] [PubMed] [Google Scholar]
- 10.Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis The updated Sydney System International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–1181. doi: 10.1097/00000478-199610000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Graham DY, Nurgalieva ZZ, El-Zimaity HMT, Opekun AR, Campos A, Guerrero L, Chavez A, Cardenas V. Noninvasive versus histologic detection of gastric atrophy in a Hispanic population in North America. Clinical Gastroenterology and Hepatology. 2006;4:306–314. doi: 10.1016/j.cgh.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Ricuarte O, Gutierrez O, Cardona H, Kim JG, Graham DY, El-Zimaity HM. Atrophic gastritis in young children and adolescents. J Clin Pathol. 2005;58:1189–1193. doi: 10.1136/jcp.2005.026310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Zimaity HM, Ota H, Graham DY, Akamatsu T, Katsuyama T. Patterns of gastric atrophy in intestinal type gastric carcinoma. Cancer. 2002;94:1428–1436. doi: 10.1002/cncr.10375. [DOI] [PubMed] [Google Scholar]
- 14.Rugge M, Correa P, Di MF, el-Omar E, Fiocca R, Geboes K, Genta RM, Graham DY, Hattori T, Malfertheiner P, Nakajima S, Sipponen P, Sung J, Weinstein W, Vieth M. OLGA staging for gastritis: a tutorial. Dig Liver Dis. 2008;40:650–658. doi: 10.1016/j.dld.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 15.Comfort MW. Gastric acidity before and after development of gastric cancer: its etiologic, diagnostic and prognostic significance. Ann Intern Med. 1951;36:1331–13348. doi: 10.7326/0003-4819-34-6-1331. [DOI] [PubMed] [Google Scholar]
- 16.Ivy AC. Discussion. J Natl Cancer Inst. 1947;7:404–407. [Google Scholar]