Highlights
-
•
Giant cystic pheochromocytoma is a rare entity.
-
•
Preoperative diagnosis is very difficult to obtain.
-
•
Open surgery is the gold standard to treat these giant masses, but comparison studies are lacking.
-
•
Posterior retroperitoneoscopic approach has advantages over transperitoneal laparoscopic method.
-
•
This is the first report of a giant cystic pheochromocytoma treated by posterior retroperitoneoscopic adrenalectomy.
Keywords: Adrenal, Giant cystic pheochromocytoma, Retroperitoneoscopic adrenalectomy, Posterior retroperitoneoscopy
Abstract
Introduction
Giant cystic pheochromocytoma (>10 cm) is rare with only a few cases described in the literature. Preoperative diagnosis is very difficult because clinical, biochemical and radiologic finds are usually not consistent with a pheochromocytoma. Open surgery is traditionally the gold standard.
Case presentation
A 51 year-old male patient resorted to surgery department with an adrenal cystic incidentaloma. He was asymptomatic, mild hypertension easily controlled, with increased plasma fractionated metanephrines. MRI and MIBG scans confirmed the presence of a right adrenal giant cystic pheochromocytoma (14 cm). A right posterior retroperitoneoscopic adrenalectomy was performed, complicated with an unintended disruption. At follow-up he was asymptomatic and with plasma fractionated metanephrines normalized.
Discussion
Although laparoscopic surgery is effective and safe, traditional open surgery is the gold standard in the presence of adrenal tumours with suspicion of malignancy, like masses larger than 8 cm (including giant cystic pheochromocytomas). Minimal invasive techniques have the advantages of less postoperative pain and ileus, less morbidity, improved cosmetics, and faster recovery, but with the negative impact in R0 resection and probably a higher risk of cystic rupture. However comparisons between open and minimally invasive surgery are lacking. Additionally posterior retroperitoneoscopic approach has several advantages over laparoscopic transperitoneal method.
Conclusion
This is the first case report of a giant cystic pheochromocytoma treated by posterior retroperitoneoscopic adrenalectomy, but the occurrence of the unintended rupture may be a factor against this approach. More studies are needed to compare open and minimally invasive techniques in terms of resectability and cystic rupture rate.
1. Introduction
Cystic adrenal neoplasms are rare and can be discovered incidentally or because of symptoms. Although adrenal cysts can be associated with neoplasms of the adrenal, they should be differentiated from adrenal neoplasms with foci of cystic or degenerative changes. A haemorrhage or degeneration within a pheochromocytoma can result in a pseudocyst. Triggering mechanism could be the tumour outgrowing its vascular supply [1], [2]. Cystic lesions of the adrenal can be huge with more than 20 cm [1]. Cystic pheochromocytoma is a rare neuro-endocrine catecholamine-producing tumour arising from chromaffin cells. The majority are asymptomatic, often diagnosed incidentally, and are rarely malignant. Giant cystic pheochromocytoma (>10 cm) is even more rare with only a few cases described in the literature [2], [3], [4], [5]. Preoperative suspicion and intraoperative crisis management are the key factors for a successful treatment [6]. However the preoperative diagnosis of a cystic pheochromocytoma is very difficult because many times the clinical, biochemical and radiologic finds are not consistent with a pheochromocytoma [2], [7], [8].
Resection is indicated for all functioning adrenal incidentalomas and those suspected of harbouring a cancer. Adrenal lesions larger than 5–6 cm (25% incidence of malignancy) and smaller lesions with suspicious criteria on imaging should also be resected [6], [7]. Nowadays large adrenal masses and those that may harbour malignancy should be resected by anterior approach to gain sufficient exposure for safe resection. Additionally, several studies have shown the efficacy and safety of laparoscopy for tumours only up to 6 cm [7]. Posterior retroperitoneoscopic approach has advantages over laparoscopic transperitoneal method, although both have a size limit up to 8–10 cm according to Lee et al. [9]. To treat bigger lesions open surgery is usually the preferred approach [4], [5] because of the potential of malignancy and to allow a secure R0 resection. The authors present the first case of a giant (14 cm) adrenal pheochromocytoma with cystic degeneration treated by posterior retroperitoneoscopic adrenalectomy in an Academic Hospital.
2. Case presentation
A 51 year-old male patient was sent to General Surgery appointment presenting a right adrenal incidentaloma found on an abdominal CT scan, described as a cystic lesion with 13 × 11 × 10 cm causing deviation of adjacent structures, without hepatic nor contralateral adrenal lesions. Patient was asymptomatic and with no tachycardia, diaphoresis or headache, presenting only mild hypertension controlled with perindopril plus amlodipine. No other past medical or surgical history.
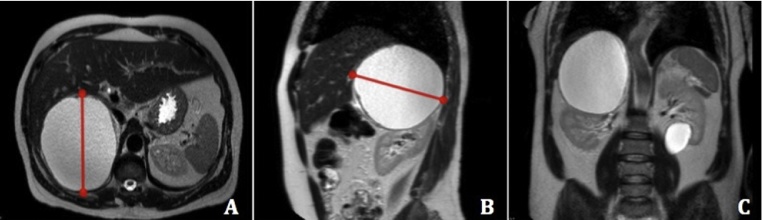
Biochemical functional tests revealed a pheochromocytoma with increased plasma fractionated metanephrines: metanephrine 3643.9 pg/mL (<60 pg/mL), normetanephrine 3001.5 pg/mL (<120 pg/mL). Serum potassium, plasma aldosterone, renine and urinary cortisol were normal. Since the initial CT scan couldn’t individualize the right adrenal gland, a MRI was performed in order to clarify the cyst aetiology. Resonance images confirmed a large well-delimited lesion at the hepato-renal space measuring 14 cm, hyperintense in T1- and T2- weighted images, suggesting high protein/hematic content, and although the right adrenal was not identified this gland was pointed out as the origin of the giant cyst (Fig. 1). MIBG scintigraphy was also performed, showing hypercaptation on the known giant lesion in the topography of the right adrenal gland, supporting the diagnosis of a pheochromocytoma in that level.
Fig. 1.
MRI images. A right adrenal giant cystic pheochromocytoma is evident. Red line represents the biggest diameter (14 cm). A. Transverse plane. B. Sagittal plane showing cystic lesion pushing down the right kidney. C. Coronal plane with kidney being compressed by the giant cystic pheochromocytoma.
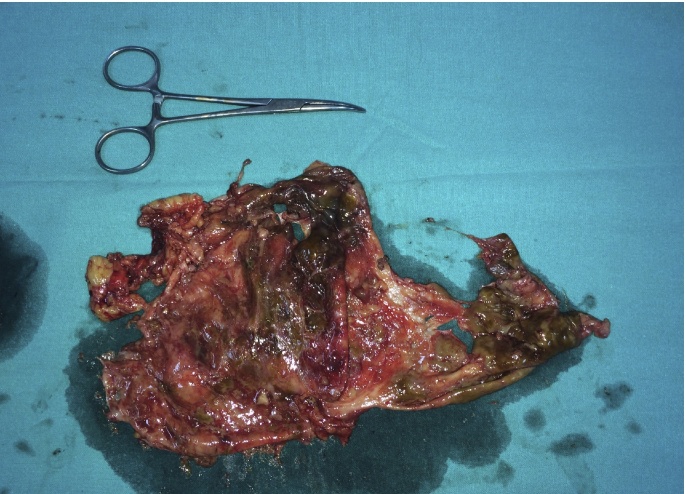
Prior to surgery, a 3-week treatment with phenoxybenzamine 10 mg a day was accomplished, and at the time of surgery the patient was hemodynamically stable with systolic blood pressure around 120 mm Hg. A right posterior retroperitoneoscopic adrenalectomy was performed. During lesion’s dissection with LigaSure 5 mm, a small disruption occurred with spillage of a dark brown fluid. In order to prevent dissemination of any potential malignant cells (since pathology was unknown at time of surgery), iodine solution was instilled in the entire surgical site. Lesion was extracted within a bag (Fig. 2). During the whole surgery there wasn’t any significant hemodynamic instability, with the systolic blood pressure reaching 230 mm Hg only in an isolated instant. Surgical operation lasted 70 min. Pathology confirmed the diagnosis of a giant cystic pheochromocytoma with a PASS score of three (no metastatic potential). Immunohistochemistry analysis found positivity of neoplastic cells for chromogranin A, synaptophysin and CD56.
Fig. 2.
Giant cystic pheochromocytoma extracted.
Patient completed a 24 h period at the Intensive Care Unit, where he was hemodynamically normal. Next day in the morning (20 h after surgery) initiated oral intake. During post-op in-hospital stay he remained hemodynamically normal, with blood pressure around 120/70 mm Hg. No pain or surgical site infection (SSI). Patient was discharged home at 4th postoperative day. After 3 months of follow-up patient is asymptomatic, blood pressure easily controlled with medication, and with plasma fractionated metanephrines normalized: metanephrine 33.4 pg/mL (<60 pg/mL), normetanephrine 64.7 pg/mL (<120 pg/mL).
3. Discussion
Cystic masses account for only 4–22% of all adrenal incidentalomas [2], [6]. The prevalence of pheochromocytoma in the hypertensive population is 0,1–0,6% [2]. In the general population the incidence of pheochromocytoma is about 0,005–0,1% [3], [4]. Cystic pheochromocytoma is even more rare with only a few cases reported worldwide [4], [8]. Although the cystic pheochromocytoma is a rare entity, its possibility must be considered for any adrenal mass because of the high risk of surgery on unsuspected patients. Clinical manifestations of a cystic pheochromocytoma are varied, and it may not demonstrate the clinical (tachycardia, headache, sweating), radiological and biochemical features of a pheochromocytoma [2], [6], [7], [8]. Although abdominal pain as been reported in several case reports, most of the times cystic pheochromocytomas are asymptomatic, and yield normal plasma and urinalysis because secreted cathecolamines are metabolized within the neoplasm, with only a small amount being release into circulation [2], [3], [4], [8]. However, this small amount can be sufficient to cause hypertension [2]. In several worldwide publications, cystic pheochromocytoma has been wrongly diagnosed as renal tumour, liver abscess, hepatic cyst, and liver or pancreatic tumour, with the correct diagnosis being confirmed only during surgery due to hemodynamic instability [3], [4], [6], [7], [10], [11], [12]. Abdominal enhanced CT scan will show rim enhancement and areas of low attenuation. MRI will be of good help in identifying the nature of the cystic lesion; with haemorrhage hypointense in both T1- and T2- weighted images and necrosis hyperintense in T2 images. Metaiodobenzylguanidine (MIBG) scan will be especially helpful in identifying an atypical pheochromocytoma like the cystic pheochromocytoma, and to differentiate it from benign adrenal cysts [6], [13].
In the case presented, adrenal incidentaloma was found on a hypertensive patient, easily controlled with medication, but with no other signs or symptoms of pheochromocytoma, matching other studies data. Increased plasma fractionated metanephrines made the diagnosis of a pheochromocytoma. MRI was very helpful in our case because the origin of the cystic lesion was uncertain in the CT scan. Although resonance images described the lesion as filled with protein/hematic liquid and pointed out the right adrenal gland as the origin of the giant cyst, the lesion was hyperintense in T1- and T2- weighted images rising doubts about the real location of the pheochromocytoma. It was the MIBG scan that confirmed the presence of a pheochromocytoma in the location of the right adrenal giant cyst, leading the surgical team to the diagnosis of a giant cystic pheochromocytoma.
Surgical excision of adrenal masses is indicated in the presence of symptoms, endocrine abnormalities (even when subclinical), complications, suspicion of malignancy and/or large size (>6 cm) [6], [7]. Surgery is the curative treatment for a pheochromocytoma because if left untreated it can lead to several complications like myocardial infarction, cardiac arrhythmias, heart failure, hypertensive encephalopathy, cerebrovascular accident and sudden death [2], [4]. It is very difficult to distinguish a benign pheochromocytoma from a malignant one from histopathological evaluation [4], [5], [8]. Malignancy can be indicated by radiological and intraoperative findings like invasion of adjacent organs or structures, regional adenopathy, or the presence of metastasis [5], [6], [8], [9]. Although malignant tumours tend to be larger, size is not an absolute criterion for malignancy [5]. Additionally, during surgery cystic rupture must be avoided in order to decrease spillage of potentially malignant cells [7]. Although laparoscopic surgery is effective and safe, traditional open surgery is the gold standard in the presence of adrenal tumours with suspicion of malignancy, like masses larger than 8 cm (including giant cystic pheochromocytomas), because open surgery can increase R0 resection rate in case of malignancy [4], [6], [9]. Minimal invasive techniques (laparoscopy and retroperitoneoscopy) have the advantages of less postoperative pain and ileus, less morbidity, improved cosmetics, and faster recovery, but with the negative impact in R0 resection and probably easier to cystic rupture occurrence [7], [9]. In 1992 laparoscopic adrenalectomy was first described by Gagner, and since then is has become the gold standard of care for adrenal tumours (size limit up to 6–8 cm, without malignancy suspicion) [9]. Comparisons have been made between transperitoneal laparoscopic method and the posterior retroperitoneoscopic (PR) approach. Lee and Walz published a study where they concluded that PR adrenalectomy has shorter operative time, decreased abdominal viscera lesions because there is no incursion into the peritoneal cavity, less post-operative pain, and shorter time to first oral intake comparing to transperitoneal laparoscopic method [9]. Direct access to adrenal gland is probably the reason for these advantages.
The authors use PR adrenalectomy as the standard method to treat adrenal masses less than 6–8 cm and without suspicion of malignancy. The option to use the same approach in the case presented (14 cm cystic mass) was based in the absence of both metastasis and organs invasion, size is not an absolute criterion for malignancy [5], and in the intent to perform a controlled aspiration of cyst content after dissection and protection with a bag. However, it revealed to be very difficult to isolate and an unintended rupture occurred. Thankfully pathology concluded it was a benign pheochromocytoma with PASS score of three (metastatic potential if PASS score ≥4). This complication is probably a factor against the authors’ surgical option, since spillage of cancer cells would be a possibility in case of malignancy. However there are no studies comparing cystic pheochromocytoma rupture rates between minimally invasive surgery and open surgery. The authors performed a review of literature and found only 20 case reports of giant cystic pheochromocytoma. Of those none was treated by PR approach, one was resected by laparoscopy, and at least 17 were submitted to open surgery (Table 1). The case presented is the first worldwide description of a giant cystic pheochromocytoma treated by posterior retroperitoneoscopic adrenalectomy.
Table 1.
Surgical approach to adrenal giant cystic pheochromocytoma reported in published cases. None was treated by posterior retroperitoneoscopy. (N/A – not available).
| Surgical approach to Adrenal Giant Cystic Pheochromocytoma | |||||
|---|---|---|---|---|---|
| Author | N | Size (cm) | Surgery | ||
| Open | Laparoscopic | Retroperitoneoscopic | |||
| Grissom JR et al. [19] | 1 | “huge” | 1 | – | – |
| Wu JS et al. [12] | 1 | 15,0 | 1 | – | – |
| Suga K et al.[17] | 1 | “huge” | 1 | – | – |
| Mishra AK et al. [14] | 1 | 12,8 | – | 1 | – |
| Minei S et al. [16] | 1 | 11,6 | 1 | – | – |
| Erickson LA et al.[1] | 1 | 25,0 | N/A | N/A | N/A |
| Antedomenico E et al. [11] | 1 | 10,5 | 1 | – | – |
| Andreoni C et al. [2] | 1 | 11,0 | 1 | – | – |
| Costa SR et al.[5] | 2 | 30,0/16,0 | 2 | – | – |
| Pan Z et al. [15] | 1 | 18,0 | 1 | – | – |
| Santarone M et al. [22] | 1 | 13,0 | N/A | N/A | N/A |
| Basiri A et al. [20] | 1 | “huge” | 1 | – | – |
| Goldberg A et al.[21] | 1 | 10,6 | 1 | – | – |
| Soufi M et al. [8] | 1 | 20,0 | 1 | – | – |
| Li C et al. [13] | 1 | 12,7 | 1 | – | – |
| Sarveswaran V et al. [6] | 1 | 11,2 | 1 | – | – |
| Wang et al. [3] | 1 | 10,3 | 1 | – | – |
| Uysal E et al. [18] | 1 | 18,0 | 1 | – | – |
| Gupta A et al. [4] | 1 | 25,0 | 1 | – | – |
| Total | 20 | – | 17 | 1 | 0 |
An important reason to the good outcome of the case presented was the preoperative diagnosis of adrenal giant cystic pheochromocytoma. In several case reports published worldwide the correct diagnosis was only confirmed due to intraoperative hemodynamic instability [3], [4], [6], [7], [10], [11], [12], and the capability to tackle it was a major factor for good outcome [6], [7]. Having the correct diagnosis before surgery can anticipate such intraoperative events, and improve the outcome of the surgery. Since we had the correct diagnosis of a cystic pheochromocytoma before surgery, we could administrate phenoxybenzamine for 3 weeks before surgery, be aware to do not touch the lesion before vascular control, and the anaesthesiologist was prepared for any intraoperative instability. Since the cystic pheochromocytoma pose clinical, radiological and biochemical difficulties in making a correct preoperative diagnosis [2], the possibility of cystic pheochromocytoma should be considered for any peri-adrenal cystic lesion even though investigations are not suggestive of pheochromocytoma [2], [6], [20].
4. Conclusion
Giant cystic pheochromocytoma is rare and pose clinical, radiological and biochemical difficulties in making a correct preoperative diagnosis. Cystic rupture must be avoided when dealing with these lesions because of the risk of malignant cells spillage. To allow a secure R0 resection, open surgery is the gold standard of care for adrenal lesions bigger than 8 cm. However, studies comparing open and minimally invasive techniques for large adrenal masses are lacking. In fact, this is the first case report of a giant cystic pheochromocytoma treated by posterior retroperitoneoscopic adrenalectomy, but the occurrence of the unintended rupture may be a factor against this approach. More studies are needed to compare open and minimally invasive techniques in terms of resectability and cystic rupture rate.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
C.E. Costa Almeida – study concept and design, data collection and analysis, writing the paper, review.
M. Silva – data analysis, writing the paper, review.
L. Carvalho – review.
Funding
None.
Ethical approval
Ethical approval was not needed since this paper describes the use of a well-known technique. Posterior retroperitoneoscopic approach is a valid option to treat adrenal tumours. The novelty of this case report is the huge size of the lesion.
Conflicts of interest
Authors declare no conflicts of interest.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
Adrenal giant cystic pheochromocytoma treated by posterior retroperitoneoscopic adrenalectomy.
UIN – researchregistry1705.
Guarantor
C.M. Costa Almeida, MD, PhD.
Contributor Information
Carlos E. Costa Almeida, Email: carloscostaalmeida@yahoo.com.
Marta Silva, Email: mafr.silva@gmail.com.
Luis Carvalho, Email: luisfcarvalho@netcabo.pt.
Carlos Manuel Costa Almeida, Email: c.m.costa.almeida@gmail.com.
References
- 1.Erickson L.A., Lloyd R.V., Hartman R., Thompson G. Cystic adrenal neoplasms. Cancer. 2005;101(7):1537–1544. doi: 10.1002/cncr.20555. [DOI] [PubMed] [Google Scholar]
- 2.Andreoni C., Krebs R., Bruna P., Goldman S., Katert C., Alves M. Cystic phaeochromocytoma is a distinctive subgroup with special clinical, imaging and histological features that might mislead diagnosis. BJU Int. 2007;101:345–350. doi: 10.1111/j.1464-410X.2007.07370.x. [DOI] [PubMed] [Google Scholar]
- 3.Wang H.L., Sun B.Z., Xu Z.J., Lei F.U., Wang X.S. Undiagnosed giant cystic pheochromocytoma: a case report. Oncol. Lett. 2015;10:1444–1446. doi: 10.3892/ol.2015.3484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta A., Bains L., Agarwal M.K., Gupta R. Giant cystic pheochromocytoma: a silent entity. Urol. Ann. 2016;8(3):384–386. doi: 10.4103/0974-7796.184886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa S.R., Cabral N.M., Abhrão A.T., Costa R.B., Silva L.M., Lupinacci R.A. Giant cystic malignant pheochromocytoma invading right hepatic lobe: report on two cases. Sao Paulo Med. J. 2008;126(4):229–231. doi: 10.1590/S1516-31802008000400008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarveswaran V., Kumar S., Kumar A., Vamseedharan M. A giant cystic pheochromocytoma mimicking liver abscess an unusual presentation–a case report. Clin. Case Rep. 2015;3(1):64–68. doi: 10.1002/ccr3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olson J.A., Jr. Adrenal glands. In: Mulholland M.W., Lillemoe K.D., editors. 4th edition. vo. 79. Lippincott Williams & Wilkins; 2006. pp. 1334–1354. (Greenfield’s Surgery: Scientific Principles & Practice). [Google Scholar]
- 8.Soufi M., Lahlou M., Benamr S., Massrouri R., Mdaghri J., Essadel A. Giant malignant cystic pheochromocytoma: a case report. Indian J. Surg. 2012;74(6):504–506. doi: 10.1007/s12262-012-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee C.R., Walz M.K., Park S., Park J.H., Jeong J.S., Lee S.H. A comparative study of the transperitoneal and posterior retroperitoneal approaches for laparoscopic adrenalectomy for adrenal tumors. Ann. Surg. Oncol. 2012;19:2629–2634. doi: 10.1245/s10434-012-2352-0. [DOI] [PubMed] [Google Scholar]
- 10.Bellantone R., Ferrante A., Raffaelli M., Boscherini M., Lombardi C.P., Crucitti F. Adrenal cystic lesions: report of 12 surgically treated cases and review of the literature. J. Endocrinol. Invest. 1998;21:109–114. doi: 10.1007/BF03350324. [DOI] [PubMed] [Google Scholar]
- 11.Antedomenico E., Wascher R.A. A case of mistaken identity: giant cystic pheochromocytoma. Curr. Surg. 2005;62:193–198. doi: 10.1016/j.cursur.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 12.Wu J.S., Ahya S.N., Reploeg M.D., Singer G.G., Brennan D.C., Howard T.K. Pheochromocytoma presenting as a giant cystic tumor of the liver. Surgery. 2000;128:482–484. doi: 10.1067/msy.2000.104113. [DOI] [PubMed] [Google Scholar]
- 13.Li C., Chen Y., Wang W., Teng L. A case of clinically silent giant right pheochromocytoma and review of literature. Can. Urol. Assoc. J. 2012;6(6):E267–E269. doi: 10.5489/cuaj.11195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mishra A.K., Agarwal G., Agarwal A., Mishra S.K. Laparoscopic adrenalectomy of large cystic pheochromocytoma. Surg. Endosc. 2001;15(2):220. doi: 10.1007/s004640040036. [DOI] [PubMed] [Google Scholar]
- 15.Pan Z., Repertinger S., Deng C., Sharma P. A giant cystic pheochromocytoma of the adrenal gland. Endocr. Pathol. 2008;19(2):133–138. doi: 10.1007/s12022-008-9016-4. [DOI] [PubMed] [Google Scholar]
- 16.Minei S., Yamashita H., Koh H., Satoh T., Kobayashi S., Furuhata M. Giant cystic pheochromocytoma: a case report. Hinyokika Kiyo. 2001;47(8):561–563. [PubMed] [Google Scholar]
- 17.Suga K., Motoyama K., Hara A., Kume N., Ariga M., Matsunaga N. Tc-99 m MIBG imaging in a huge clinically silent pheochromocytoma with cystic degeneration and massive hemorrhage. Clin. Nucl. Med. 2000;25:796–800. doi: 10.1097/00003072-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Uysal E., Kirdak T., Gürer A.O., Ikidag M.A. Giant multicystic malignant pheochromocytoma. Turk. J. Surg. 2015 doi: 10.5152/UCD.2015.3011. Ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grissom J.R., Yamase H.T., Prosser P.R. Giant pheochromocytoma with sarcoidosis. South Med. J. 1979;72:1605–1607. doi: 10.1097/00007611-197912000-00035. [DOI] [PubMed] [Google Scholar]
- 20.Basiri A., Radfar M.H. Giant cystic pheochromocytoma. Urol. J. 2010;7:16. [PubMed] [Google Scholar]
- 21.Goldberg A., Pautler S.E., Harle C., Dennis A., Rachinsky I., Dhir A. Giant cystic pheochromocytoma containing high concentrations of catecholamines and metanephrines. J. Clin. Endocrinol. Metab. 2011;96(8):2308–2309. doi: 10.1210/jc.2011-0465. [DOI] [PubMed] [Google Scholar]
- 22.Santarone M., Borghi C., Miglierina E., Senatore S., Corrado G. Giant cystic pheochromocytoma. J. Cardiovasc. Med. 2008;9(9):971–972. doi: 10.2459/JCM.0b013e328303698b. [DOI] [PubMed] [Google Scholar]