Abstract
Introduction
We aimed to assess the current scope of handoff education and practice among resident physicians in academic centers and to propose a standardized handoff algorithm for the transition of care from the emergency department (ED) to an inpatient setting.
Methods
This was a cross-sectional survey targeted at the program directors, associate or assistant program directors, and faculty members of emergency medicine (EM) residency programs in the United States (U.S.). The web-based survey was distributed to potential subjects through a listserv. A panel of experts used a modified Delphi approach to develop a standardized algorithm for ED to inpatient handoff.
Results
121 of 172 programs responded to the survey for an overall response rate of 70.3%. Our survey showed that most EM programs in the U.S. have some form of handoff training, and the majority of them occur either during orientation or in the clinical setting. The handoff structure from ED to inpatient is not well standardized, and in those places with a formalized handoff system, over 70% of residents do not uniformly follow it. Approximately half of responding programs felt that their current handoff system was safe and effective. About half of the programs did not formally assess the handoff proficiency of trainees. Handoffs most commonly take place over the phone, though respondents disagree about the ideal place for a handoff to occur, with nearly equivalent responses between programs favoring the bedside over the phone or face-to-face on a computer. Approximately two-thirds of responding programs reported that their residents were competent in performing ED to inpatient handoffs. Based on this survey and on the review of the literature, we developed a five-step algorithm for the transition of care from the ED to the inpatient setting.
Conclusion
Our results identified the current trends of education and practice in transitions of care, from the ED to the inpatient setting in U.S. academic medical centers. An algorithm, which guides this process, is proposed to address the current gap in the standardized approach to ED to inpatient handoffs that were identified in the survey’s assessment of needs.
INTRODUCTION
The handoff was defined as “the exchange between health professionals of information about a patient accompanying either a transfer of control over or of responsibility for the patient.”1 Patient handoffs were found to be responsible for medical errors and harmful to the patient, and the Institute of Medicine’s report, “To Err is Human,” highlighted handoffs as a potential area of improvement.2 The Joint Commission and the Accreditation Council for Graduate Medical Education (ACGME) recommended that sponsoring programs ensure and monitor an effective and structured handoff process. 3,4,5
Several studies reported the current practice of transition of care within the emergency department (ED), including previous studies by the Council of Residency Directors (CORD). 6 7 8 The CORD survey showed that over half of the respondents from academic EDs indicated that their EDs use a standardized handoff. 9 However, it is not known how emergency medicine (EM) residency programs are providing training around care transitions from the ED to inpatient settings.
The authors aimed to assess the current scope of handoff education and practices among resident physicians and to propose a standardized handoff algorithm to improve the transition of care from the ED to the inpatient setting.
METHODS
Survey Content
The authors conducted a cross-sectional survey targeted at EM residency programs in the United States. The survey was developed to address the initial two steps of the Kern model for medical curriculum development: 1) problem identification and general needs assessment; and 2) needs assessment for targeted learners.10 Content experts created a web-based survey to assess the current handoff practice from the ED to inpatient providers (Appendix 1. Survey questions).
Survey Administration
We piloted surveys among the CORD Transition of Care (TOC) task force members and revised them before final administration. The survey was designed using the SurveyMonkey® platform (SurveyMonkey Inc., Palo Alto, California, USA. www.surveymonkey.com) and distributed to all members through the CORD listserv. The validity of using the CORD listserv as sample population has been described elsewhere.7,11,12 The responses were collected, and duplicated responses were removed and compiled for data analysis.
Transition of Care Algorithm
Given the identified needs and opportunities in the transition of care, authors performed a review of the literature (Appendix 2. Search strategy). We used a modified Delphi technique to develop an algorithmic approach to conducting efficient handoffs from the ED to the inpatient setting, which served as a primer for the following two steps of the six-step Kern model: 3) goals and objectives, and 4) educational strategies.10,13 The algorithm was initially derived from the CORD TOC EM to EM handoff by Kessler et al.7 and implemented based on the literature review.5,7,8,14–29 The algorithm was modified and approved by seven experts.
Statistical Analysis
Sample size calculations demonstrated that of the 172 programs surveyed as the true target population, 121 responses would give a 95% confidence interval with a 5% margin of error. We reported data using descriptive statistics and analyzed them by a two-sample test of proportion or Fisher’s exact test, as appropriate. We completed statistical analysis with JMP®, Version <10.0> (SAS Institute Inc., Cary, NC), and we reported p-values.
This study was declared exempt by the Alameda Health System.
RESULTS
Response Rate
A survey response was obtained from 121 out of 172 programs with the overall response rate being 70.3%.
Transition of Care Curriculum, Handoff Structure and Safety Perception
Most programs offer handoff training to their resident physicians (Table 1). The type of training varied, with the most common form being instruction in the clinical setting, followed by handoff training during orientation, structured workshop/classes, educational packets or guides, and other methods. Less than half of the programs responded that they have a structured formal handoff process, yet the compliance among residents was variable. About half of responding programs responded that their current handoff system was safe and effective (Table 1).
Table 1.
Transition of care curriculum, handoff structure, and safety perception in emergency medicine training programs.
| Response choices | Response rate/total, (%)* |
|---|---|
| Transition of care curriculum | |
| Attendings or senior residents provide handoff instruction in the clinical environment | 90/121 (74.4) |
| Handoff training offered during the initial orientation | 87/121 (71.9) |
| Structured workshop/classes to teach proper handoff procedure | 27/121 (22.3) |
| Educational packets or guides for handoff | 14/121 (11.6) |
| Other methods (simulation, policy and online instructions) | 7/121 (5.8) |
| Handoff structure | |
| Structured handoff for ED to inpatient providers in place | 45/119 (37.2) |
| How often do residents use a structured handoff? | |
| Always | 9/45 (20) |
| Usually | 13/45 (29) |
| Sometimes | 19/45 (42) |
| Rarely | 3/45 (6.7) |
| Safety perception | |
| Current handoff process is: | |
| Extremely safe and effective | 2/121 (1.7) |
| Safe and effective | 57/121 (47.1) |
| Somewhat safe and effective | 56/121 (42.3) |
| Not safe or effective | 6/121 (5.0) |
Multiple choices were allowed.
Handoff Assessment
Nearly half of responding programs stated that they do not formally assess handoff proficiency in resident physicians (Table 2). Otherwise, Table 2 shows the types of formal assessment methods of handoff proficiency in trainees.
Table 2.
Do you formally assess the handoff proficiency of your residents? If yes, how?
| Response choices | Response rate/total, (%) |
|---|---|
| No, I do not formally assess the handoff of the residents. | 59/121 (48.8) |
| Yes, assessment is done through scheduled one-on-one discussion with each resident. | 7/121 (5.8) |
| Yes, assessment is done through regular written feedback/evaluation from EM personnel. | 31/121 (25.6) |
| Yes, I ask the senior EM residents to assess the handoff proficiency of the junior residents. | 15/121 (12.4) |
| Yes, residents/faculty from other services provide informal feedback on the quality of admission handoffs. | 26/121 (21.5) |
| Yes, residents/faculty from other services provide regular formalized feedback on the quality of admission handoff. | 3/121 (2.5) |
| Other methods | 16/121 (13.2) |
Current mode of Handoff and Recommended Handoff
Eighty-nine programs responded to the question of which mode of handoff process was used, and a handoff via phone was most common (Figure). On the other hand, of the 116 programs that responded to where the formal handoff should occur, answers were variable (Figure).
Figure.
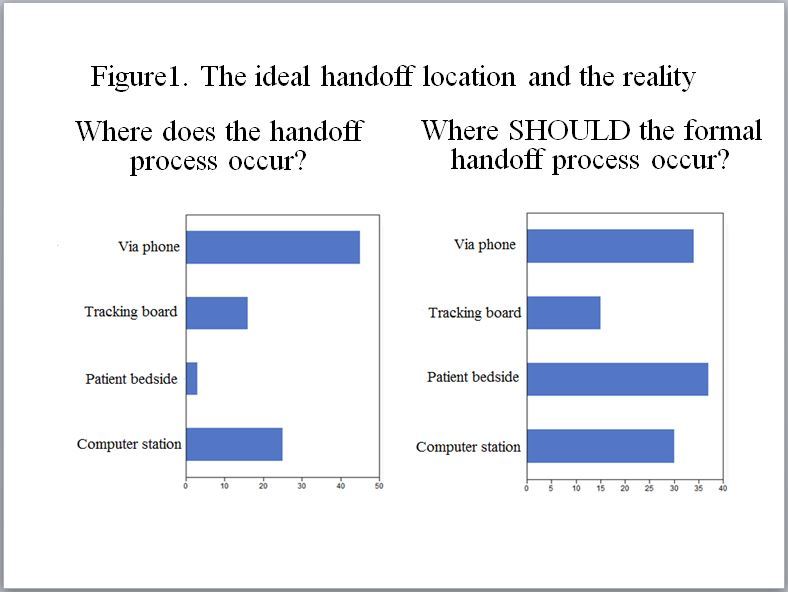
The ideal handoff location and the reality.
Handoff Competency Assessment
Lastly, two-thirds of programs responded that their residents were extremely competent to competent in giving ED to inpatient handoffs (extremely competent 8/121, 6.6%; competent 71/121, 58.7%; somewhat competent, 41/121, 33.9%; incompetent, 1/121, 0.8%). There was a statistically significant association between achieving competency and instruction offered by attending or senior resident at clinical setting (p=0.006), but not with the handoff training during initial orientation (p=0.23), structured workshop (p=0.12), or educational packet (p=0.5).
Handoff Algorithm
Given the identified need for handoff education and existing literature, authors developed a handoff algorithm ‘Prep-4Cs.’8,15–18,30 The handoff algorithm consists of five steps (Table 3).
Table 3.
EM-IM transition of care algorithm “PREP-4Cs.”
| PREP-4Cs |
| Step 1. Preparation Immediate access to patient information, assessment, access to images, labs and medical record. Time commitment (2–5min) Space with minimal interruption |
| Step 2. Contact Sender and receiver identify themselves, including name and service “Face to face or voice to voice” to share real time information |
Step 3. Communicate patient information
|
Step 4. Closing the loop
|
Step 5. Conclusion
|
DISCUSSION
Statement of Principal Findings
Our survey showed that most EM programs in the U.S. have some form of handoff training, the majority of them occurring during clinical setting. However, the handoff structure from ED to inpatient is neither well standardized nor followed. Only half of responding programs felt that their current handoff system was safe and effective. About half of the programs did not have a formal assessment. Handoffs most commonly take place over the phone, though respondents disagreed about the ideal place for a handoff to occur.
Interpretation of Results Compared to Other Studies
The majority of EM programs in the U.S. now have some form of handoff training, which is in compliance with the ACGME common program requirement.3 The overall rate of the handoff education has now increased to 94% from 13% in 2013, reflecting the successful dissemination of handoff education.7 Hern et al. surveyed the trend of EM providers and concluded that there is an insufficient level of mandatory handoff training with varying results.9 Our study supports this finding and implies a further need for an effective handoff education.
This study demonstrates that handoff practice from ED to inpatient is not standardized, and even in places where a formal system exists, the compliance rate is not high. This is consistent with the existing literature, which showed that less than half of EM programs had a standardized handoff practice in 2013.12 A standardized handoff practice has been introduced to several inter-unit handoff processes, namely using mnemonics and checklists.14,31 A recent study showed that the use of communication training, mnemonics, and handoff structures decreased medical error in the pediatric inpatient setting.32,33 It implies that the introduction of standard mnemonics can be a starting point, yet programs may have to expand their curriculum into a handoff bundle tailored for ED to inpatient transition of care.
Only approximately half of the responding programs felt that their current handoff system was safe and effective, and about half of programs reported using a formal evaluation process for trainee proficiency. The existing literature identified a knowledge gap and the potential benefit of evaluation tools.34,35 It is prudent to develop validated evaluation tools to accurately assess the effectiveness and safety of handoffs.
About half of the respondents reported that the handoff occurred over the phone, yet there was no consensus on what mode of handoff would be ideal (Figure). A previous survey study demonstrated that ED to ED end of shift handoffs should ideally occur at the patient bedside, although many found that the handoffs actually occurred at the computer station.7 The most effective and safest practice model needs to be elucidated.
Lastly, while approximately two-thirds of programs reported that their residents were competent, this still leaves room for improvement either in training or assessment. Our analysis showed that only the presence of handoff training during clinical setting was associated with competency. Currently, there is no universally accepted competency assessment.36 As the program requirement includes the milestones for resident education, the level of competency needs to be accurately evaluated.
Proposed Handoff Algorithm
The proposed algorithm “Prep-4Cs” (Table 3) is meant to provide some standardization while still allowing flexibility so institutions/programs ensure that their unique needs are met. Some institutions may already use a handoff mnemonic or template that can be incorporated into this algorithm. Prospective validation of this algorithm is required.
LIMITATIONS
The study has several limitations. First, the response was based on each responder’s perception of the transition of care. Second, construct underrepresentation and construct-irrelevant variance could have affected the validity of the survey questions.37 Third, rater and recall bias need to be considered in the results, as the responder was anonymous in the survey.
CONCLUSION
This study identified current trends of transitions of care from the ED to inpatient settings among academic medical centers in the U.S. and developed an algorithm to provide a foundation and springboard for educational strategies.
Supplementary Information
Footnotes
Section Editor: Jeffrey Love, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010;19(6):493–7. doi: 10.1136/qshc.2009.033480. [DOI] [PubMed] [Google Scholar]
- 2.Kohn LT, CJM, Donaldson MS Institute of Medicine. To err is human: building a safer health system. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. Common Program Requirements, Section VI.B.2. [Accessed Nov 9, 2015]. Available at: http://www.acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx.
- 4.Joint Commission. 2006 Critical Access Hospital and Hospital National Patient Safety Goals #2E. 2006. [Accessed Nov 9, 2015]. [Accessed on 10/20/2015]. Available at: http://www.neodevices.com/resources/CR_NationalPatientSafetyGoals.pdf.
- 5.Riesenberg LA. Shift-to-Shift Handoff Research: Where Do We Go From Here? J Grad Med Educ. 2012;4(1):4–8. doi: 10.4300/JGME-D-11-00308.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ye K, Mc DTD, Knott JC, et al. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas. 2007;19(5):433–41. doi: 10.1111/j.1742-6723.2007.00984.x. [DOI] [PubMed] [Google Scholar]
- 7.Kessler C, Shakeel F, Hern HG, et al. An algorithm for transition of care in the emergency department. Acad Emerg Med. 2013;20(6):605–10. doi: 10.1111/acem.12153. [DOI] [PubMed] [Google Scholar]
- 8.Riesenberg LA, Leitzsch J, Little BW. Systematic review of handoff mnemonics literature. Am J Med Qual. 2009;24(3):196–204. doi: 10.1177/1062860609332512. [DOI] [PubMed] [Google Scholar]
- 9.Hern HG, Jr, Gallahue FE, Burns BD, et al. Handoff Practices in Emergency Medicine: Are We Making Progress? Acad Emerg Med. 2016;23(2):197–201. doi: 10.1111/acem.12867. [DOI] [PubMed] [Google Scholar]
- 10.Kern D. Curriculum development for medical education: a six step approach. Baltimore, MD: Johns Hopkins University Press; 1998. [Google Scholar]
- 11.Downing SM. Validity: on meaningful interpretation of assessment data. Med Educ. 2003;37(9):830–7. doi: 10.1046/j.1365-2923.2003.01594.x. [DOI] [PubMed] [Google Scholar]
- 12.Kessler C, Shakeel F, Hern HG, et al. A survey of handoff practices in emergency medicine. Am J Med Qual. 2014;29(5):408–14. doi: 10.1177/1062860613503364. [DOI] [PubMed] [Google Scholar]
- 13.Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15. [PubMed] [Google Scholar]
- 14.Kessler CS, Kalapurayil PS, Yudkowsky R, et al. Validity evidence for a new checklist evaluating consultations, the 5Cs model. Acad Med. 2012;87(10):1408–12. doi: 10.1097/ACM.0b013e3182677944. [DOI] [PubMed] [Google Scholar]
- 15.Kessler CS, Afshar Y, Sardar G, et al. A prospective, randomized, controlled study demonstrating a novel, effective model of transfer of care between physicians: the 5 Cs of consultation. Acad Emerg Med. 2012;19(8):968–74. doi: 10.1111/j.1553-2712.2012.01412.x. [DOI] [PubMed] [Google Scholar]
- 16.Brannen ML, Cameron KA, Adler M, et al. Admission handoff communications: clinician’s shared understanding of patient severity of illness and problems. J Patient Saf. 2009;5(4):237–42. doi: 10.1097/PTS.0b013e3181c029e5. [DOI] [PubMed] [Google Scholar]
- 17.Apker J, Mallak LA, Gibson SC. Communicating in the “gray zone”: perceptions about emergency physician hospitalist handoffs and patient safety. Acad Emerg Med. 2007;14(10):884–94. doi: 10.1197/j.aem.2007.06.037. [DOI] [PubMed] [Google Scholar]
- 18.Collins SA, Stein DM, Vawdrey DK, et al. Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. J Biomed Inform. 2011;44(4):704–12. doi: 10.1016/j.jbi.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maughan BC, Lei L, Cydulka RK. ED handoffs: observed practices and communication errors. Am J Emerg Med. 2011;29(5):502–11. doi: 10.1016/j.ajem.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Apker J, Mallak LA, Applegate EB, 3rd, et al. Exploring emergency physician-hospitalist handoff interactions: development of the Handoff Communication Assessment. Ann Emerg Med. 2010;55(2):161–170. doi: 10.1016/j.annemergmed.2009.09.021. [DOI] [PubMed] [Google Scholar]
- 21.Patterson ES, Roth EM, Woods DD, et al. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16(2):125–132. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- 22.Cheung DS, Kelly JJ, Beach C, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171–180. doi: 10.1016/j.annemergmed.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 23.Telem DA, Buch KE, Ellis S, et al. Integration of a formalized handoff system into the surgical curriculum: resident perspectives and early results. Arch Surg. 2011;146(1):89–93. doi: 10.1001/archsurg.2010.294. [DOI] [PubMed] [Google Scholar]
- 24.Arora VM, Manjarrez E, Dressler DD, et al. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–40. doi: 10.1002/jhm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sinha M, Shriki J, Salness R, et al. Need for standardized sign-out in the emergency department: a survey of emergency medicine residency and pediatric emergency medicine fellowship program directors. Acad Emerg Med. 2007;14(2):192–6. doi: 10.1197/j.aem.2006.09.048. [DOI] [PubMed] [Google Scholar]
- 26.Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84(12):1775–87. doi: 10.1097/ACM.0b013e3181bf51a6. [DOI] [PubMed] [Google Scholar]
- 27.Wayne JD, Tyagi R, Reinhardt G, et al. Simple standardized patient handoff system that increases accuracy and completeness. J Surg Educ. 2008;65(6):476–85. doi: 10.1016/j.jsurg.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 28.Wohlauer MV, Arora VM, Horwitz LI, et al. The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med. 2012;87(4):411–8. doi: 10.1097/ACM.0b013e318248e766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hinami K, Farnan JM, Meltzer DO, et al. Understanding communication during hospitalist service changes: a mixed methods study. J Hosp Med. 2009;4(9):535–40. doi: 10.1002/jhm.523. [DOI] [PubMed] [Google Scholar]
- 30.Kessler C, Scott NL, Siedsma M, et al. Interunit handoffs of patients and transfers of information: a survey of current practices. Ann Emerg Med. 2014;64(4):343–9 e345. doi: 10.1016/j.annemergmed.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 31.Boat AC, Spaeth JP. Handoff checklists improve the reliability of patient handoffs in the operating room and postanesthesia care unit. Paediatric anaesthesia. 2013;23(7):647–54. doi: 10.1111/pan.12199. [DOI] [PubMed] [Google Scholar]
- 32.Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262–70. doi: 10.1001/jama.2013.281961. [DOI] [PubMed] [Google Scholar]
- 33.Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. The New England journal of medicine. 2014;371(19):1803–12. doi: 10.1056/NEJMsa1405556. [DOI] [PubMed] [Google Scholar]
- 34.Tapia NM, Fallon SC, Brandt ML, et al. Assessment and standardization of resident handoff practices: PACT project. J Surg Res. 2013;184(1):71–7. doi: 10.1016/j.jss.2013.04.063. [DOI] [PubMed] [Google Scholar]
- 35.Smith CJ, Britigan DH, Lyden E, et al. Interunit handoffs from emergency department to inpatient care: A cross-sectional survey of physicians at a university medical center. J Hosp Med. 2015 doi: 10.1002/jhm.2431. [DOI] [PubMed] [Google Scholar]
- 36.Doty CI, Roppolo LP, Asher S, et al. How Do Emergency Medicine Residency Programs Structure Their Clinical Competency Committees? A Survey. Acad Emerg Med. 2015 doi: 10.1111/acem.12804. [DOI] [PubMed] [Google Scholar]
- 37.Downing SM. Threats to the validity of locally developed multiple-choice tests in medical education: construct-irrelevant variance and construct underrepresentation. Adv Health Sci Educ Theory Pract. 2002;7(3):235–41. doi: 10.1023/a:1021112514626. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


