Abstract
Anterior cruciate ligament (ACL) tears are common knee injuries sustained by athletes during sports participation. A devastating complication of returning to sport following ACL reconstruction (ACLR) is a second ACL injury. Strong evidence now indicates that younger, more active athletes are at particularly high risk for a second ACL injury and this risk is greatest within the first two years following ACLR. Nearly one-third of the younger cohort that resumes sports participation will sustain a second ACL injury within the first two years after ACLR. The evidence indicates that the risk of second injury may abate over this time period. The incidence rate of second injuries in the first year after ACLR is significantly greater than the rate in the second year. The lower relative risk in the second year may be related to athletes achieving baseline joint health and function well after the current expected timeline (6 to 12 months) to be released to unrestricted activity. This highlights a considerable debate in the return to sport decision process as to whether an athlete should wait until two years after ACLR to return to unrestricted, sports activity. In this review, we present evidence in the literature that athletes achieve baseline joint health and function approximately two years after ACLR. We postulate that delay in returning to sports for nearly two years will significantly reduce the incidence of second ACL injuries.
1. Introduction
Anterior cruciate ligament (ACL) tears are common musculoskeletal injuries sustained by athletes who participate in landing and pivoting sports. ACL reconstruction (ACLR) is the current clinical standard to provide mechanical stability to the joint and return to sports (RTS) in a timely manner.[1] One of the most devastating, and all too common, complications following a return to activity is a second ACL injury. A systematic review of prospective studies with a minimum follow-up time of 5 years found that the pooled percentage of autograft failure rates and contralateral ACL tears to be 5.8% and 11.8%, respectively.[2] Long-term follow-ups of 10 years or more have reported second injury rates between 23% and 27%.[3–5] Several factors have been implicated in second ACL injury risk, including graft placement,[6–8] graft type,[9–13] sex,[14–16] age,[5, 14, 17–19] time from surgery,[10, 20, 21] activity level,[22, 23] and aberrant neuromuscular and biomechanical adaptations.[24]
The active, young athlete who resumes activity following ACLR has a greater propensity for a second ACL injury.[8, 9, 13, 14, 17–19, 25, 26] The probability of a second injury increases 3- to 6-fold when the athlete is less than 20 years of age.[19] Injury rates in this younger cohort have been reported almost as high as 30% in the literature.[5, 17, 20, 24] In addition, the increased risk in this group is apparent immediately upon returning to sports. The evidence strongly indicates that second ACL injury risk is greatest within the first 2 years after ACLR for young athletes returning back to high level sports.[15, 19, 20, 22, 24, 26] A young athlete who returns to sport within 1 year is 15 times more likely to suffer a second ACL injury than a healthy athlete with no medical history of a knee injury.[15] This elevated risk remains evident within two years of returning to activity, when an athlete is approximately 6 times more likely to sustain a second injury than an uninjured counterpart.[20] While the risk in this young cohort is high initially, this evidence indicates that the risk may be abated over time as athletes are still recovering baseline joint health and function. These athletes are at a disproportionately higher risk of second ACL injury within the first two years after ACLR. Therefore, waiting to reintegrate in high level sports activity will significantly benefit the ACLR athlete.
The high secondary injury rates within two years after ACLR in the young, active cohort highlight the significant impact of returning to sport too early. The marked increase in early second ACL injuries also correspond with the shift from a more conservative post-operative treatment of ACLR athletes as described by Paulos et al.[27] to the accelerated rehabilitation program suggested by Shelbourne and Nitz.[28] The lower relative risk of second ACL injuries in athletes who delay a return to activity after ACLR may be related to graft healing, recovering knee joint homeostasis, and restoring normal joint motion prior to be released to unrestricted, sports activity. A complete resolution of symptoms and deficits after ACLR may be directly related to the biological and functional recovery of the knee joint. In this review, we present the evidence that athletes achieve baseline joint health and function at approximately two years after ACLR. The postulate outlined below is that a delay in return to unrestricted, high level sports participation for at least two years will significantly reduce the incidence of second ACL injuries.
2. Biological Recovery of the Knee
Athletes may require a longer post-operative recovery period than the typically advocated 6 to 12 months to facilitate the biological recovery of the joint.[29] The ACL graft must undergo repopulation and proliferation of cells, re-vascularization, and re-innervation to successfully restore the native properties of the ligament.[30] In addition, ACL graft maturation, through assimilation and re-ligamentization, is critical to reinstate ACL integrity.[31, 32] These innate properties may be regained, but the current evidence indicates that this healing occurs at a slower rate than the time frame in which athletes commonly return to activity.[33–36] Furthermore, the trauma from the injury is not restricted to the ligament alone but also the surrounding joint tissues. A majority of ACL tears occur as non-contact episodes that involve the knee absorbing a high external load causing substantial trauma to the articular cartilage and subchondral bone.[37–40] Partial recovery of the joint is deleterious and may lead to a knee joint environment that is unable to endure the forces associated with a return to activity. Therefore, if time from ACLR is utilized among the RTS criteria in determining whether an athlete is ready to RTS, it should ensure that the ACL graft and surrounding knee joint tissue are completely recovered prior to returning to sport. Ideally, an athlete returns to sport once ACL and whole joint integrity is re-established.
2.1 Bone Bruises
The prevalence of bone bruises concomitant with ACL injuries is high, as approximately 80% of individuals present with subchondral lesions and bone marrow edema.[38, 41, 42] These occult osseous lesions are identifiable by magnetic resonance imaging (MRI) as alterations in signal intensity.[43, 44] Despite conflicting evidence of their clinical relevance and an absence of association with second ACL injury risk, [45–48] the presence of bone bruises at follow-ups may indicate that the knee has not normalized.
A recent systematic review[49] investigated the characteristics of bone bruises associated with ACL tears, their clinical relevance, and their progression over time. The studies that included follow-up imaging observed that chondral defects were still present at one year after ACL injury.[49] One limitation of the studies that were included in the review was the relative short-term follow-up period of less than 2 years.[49] Hence, it is not clear whether these effects persisted at two years post injury. Boks and colleagues[50] performed a systematic review of follow-up studies to examine the natural course of posttraumatic occult bone lesions as detected by MRI imaging. A review of 13 studies demonstrated that a natural healing response may be observed for bone bruises after acute trauma but the time to recover may depend on the extent of disturbance.[51] At follow-up imaging, the percentage of complete resolutions of bone bruises in the knee ranged from 88% after 11–16 months of follow-up to 100% after 5–12 months of follow-up.[51] The course of healing was variable and possibly related to the severity and location of the bone bruise.
Costa-Paz et al.[47] conducted a follow-up study of bone bruises associated with ACL ruptures. Preoperative MRIs verified the presence of bone bruises and were used to develop a 3-level classification system based on severity and location.[47] The more severe a bone bruise the higher classification it received. Follow-up MRIs were done at an average of 34 months following ACLR and revealed the resolution of all type I and type II bone bruises, except one type II.[47] However, all type III lesions had persistent evidence of abnormality on MRI scans that was consistent with cartilage thinning or cortical depression, indicating that recovery was not complete.[47] Bone bruises may be recovering up to one year following ACLR and require a longer recovery period than the standard timeline according to which athletes are returning to activity.
Bone scans are important tools to evaluate both osseous metabolic activity of the joint and potential bone loss resultant from the trauma of the injury.[52] Bone loss is not directly implicated in second ACL injury, but a metabolically active joint and substantial bone loss are signs of a degenerative joint environment and a knee that is not prepared for unrestricted, sports activity. In addition, ACLR may slow the process of knee joint homeostasis, further delaying its full recovery.[53] Nyland et al.[54] conducted a systematic review of osseous deficits after ACL injury and ACLR. A review of the literature indicated that involved limb bone integrity is decreased after ACL injury and that premorbid bone integrity is not re-established after ACLR and accelerated rehabilitation.[54] Zerahn et al.[55] conducted a two-year prospective cohort study that evaluated the relationship of subjective knee function (IKDC score), self-reported signs of instability (Lysholm score), and bone mineral density (BMD). There was a significant decline in BMD in the proximal tibia of the ACLR limb at the 4 and 12 month follow-up compared to controls and the uninjured contralateral limb.[55] The BMD of the medial tibia had returned to normal levels at 24 months, but the lateral tibia had significantly lower BMD compared to the uninjured limb and healthy controls.[55] Also, there was a significant improvement in Lysholm score, level of activity, and knee function at 24 months.[55] The improvement in self-reported knee function at 24 months was also associated with an increase in BMD in the ACLR limb.[55] In summary, the recovery of bone to that of the baseline level may requisite a significant delay in a RTS of nearly two years.[56–58]
2.2 Mechanoreceptors and Sensory Afferents
Sensory nerve fibers and mechanoreceptors (Golgi tendon organs, Pacinian corpuscles, and Ruffini nerve endings) comprise nearly 3% of the ACL’s tissue volume and account for the sensory function of the ligament.[59, 60] In addition, a reflex loop between these sensory constituents and the surrounding musculature is involved in dynamic joint stability and proprioception.[61, 62] However, once the ACL is disrupted, the native sensory function is lost and re-innervation is not fully restored, regardless of ACLR.[63–65] In order to compensate, ACLR athletes must develop extra-articular sensation and control of the joint through the mechanoreceptors and sensory nerve fibers in peri-articular tissue. This loss in sensory function is strongly indicated by proprioceptive deficits following ACL injury and ACLR.[66, 67] Because proprioception of the knee is not objectively defined and can be measured in several ways, we limit our discussion in this current opinion article to tasks of joint position matching and threshold to detection of passive moments, which are commonly measured for joint kinesthesia; however, we have reviewed alternative, more sensitive and specific methodologies in a separate review.[67]
This proprioceptive compensation strategy is not immediately developed, but is slowly gained long after ACLR and a release from sports participation. Iwasa et al.[68] evaluated 38 patients following a hamstrings tendon (HT) ACLR in joint position tasks from 3 to 24 months at every 3 month interval. Thirty of the patients had improved joint position sense up until the final follow-up at 24 months.[68] Eight of the patients did not have any improvement in proprioception at any time in the course of the study.[68] This study indicated that a longer postoperative recovery may be required for a complete resolution of proprioceptive deficits. MacDonald et al.[69] conducted threshold to detection of passive movement testing of ACL-deficient, ACLR with HT autograft, and ACLR with patellar tendon (PT) autograft at an average follow-up of 31 months. No statistically significant differences were observed during testing between the three groups at follow-up.[69]
Deficits in proprioception are not exclusive to the ACL-injured and ACLR limb, but have been widely reported in the uninjured limb, but to a lesser extent.[70] While symmetry is important, the assessment of proprioception using the contralateral limb is a fundamental issue that should be controlled. Roberts et al.[71] compared bilateral proprioceptive deficits in ACLR and healthy volunteers at a mean of 2 years from surgery. There were no observed differences at two years within or between groups during the active and visual reproduction tests.[71] Risberg et al.[72] investigated proprioception in ACLR and control cohorts with and without bracing. After controlled rehabilitation, the cohorts were studied at a mean follow-up of two years. No significant differences were observed during the threshold to detection of passive moments between the ACLR knees and the contralateral uninjured knees.[72] Further, there were no significant differences during the same task between the ACLR and control group or the uninjured contralateral limbs and the control group.[72] These studies indicate that continued improvement in proprioceptive function is observed up to two years after ACLR.
The current evidence regarding proprioception presents conflicting results. There is limited evidence to indicate that proprioceptive function can be fully restored to baseline levels. However, the longitudinal evidence indicates an improvement of proprioceptive function over time and a recovery to not significantly different from baseline well after athletes are commonly released to sports activity. A recent review by Gokeler et al.[73] examined the literature to evaluate the clinical relevance of proprioceptive deficits. Limited evidence was found to indicate that proprioceptive deficits detected by the current measurement techniques adversely affect function in ACL-deficient and ACLR athletes.[73] Further research is needed to develop more sensitive and relevant measurements for proprioception and sensorimotor function. However, it is unclear what the relative contribution of the loss of ACL sensory information is to chronic joint dysfunction and second ACL injury risk.
2.3 Graft Maturation
The restoration of normal knee function may depend on ACL graft maturation toward a biologic structure similar to that of the native ACL. The healing and metaplasia of the ACL graft commonly became known as ligamentization.[31] Histological analysis of graft tissue from animal models is commonly used to study the early, remodeling, and mature phases of the ACL graft ligamentization sequence.[32, 74] The biomechanical properties of the ACL graft are significantly influenced by the remodeling phase, the phase in which the graft is mechanically the weakest and most susceptible to injury.[30, 75] A systematic review by Claes et al.[33] studied the current literature on the ligamentization process in humans. A key finding from the review is that humans undergo the same ligamentization sequence as animals, but the timeline of healing is substantially different.[33] The ligamentization processes occurs in humans over a much longer duration than what is originally observed in animal studies, specifically with humans having a much slower remodeling phase.[33]
A recent systematic review examined the literature on the ligamentization process in hamstrings tendon (HT) autograft used in human ACLR.[34] Within this review, the results of the ligamentization process in HT autografts were compared to the other commonly used graft in ACLR, the patellar tendon (PT) autograft.[34] Comparison of the results indicated that the HT autograft has a significantly delayed remodeling phase, which occurs between 12–24 months.[34] Alternatively, PT autografts undergo the remodeling phase during the 6–12 month timeline.[34] These time periods correspond not only to the time that athletes are returning to sport, but also the time when athletes are at a greater risk for a second ACL injury.
A non-invasive approach to examine the ACL graft and its stages of healing in humans is achieved through various imaging modalities that are now clinically available.[76] A recovery to nearly native ACL properties in imaging studies is indicated approximately two years after ACLR. Vogl et al.[77] conducted a two-year prospective study that evaluated the ACL graft healing process using contrast-enhanced magnetic resonance imaging (MRI). Revascularization of the ACL graft closely resembled that of the native ACL at the two-year follow-up.[77] Zaffagnini et al.[78] studied the histological ligamentization changes in PT autograft at 6, 12, 24, 48, and 120 months following ACLR using transmission electron microscopy (TEM). The results of the study indicated that progressive ultrastructural changes towards the normal ACL were observed for up to 24 months.[78] Notably, no further changes were observed in the TEM imaging after the 24 month time point after ACLR.[78] Variability in healing was observed in these studies but longer follow-ups indicated a complete structural and morphological resemblance to the native ACL.[79–82] A significant delay in returning to sport following ACLR to nearly two years may allow complete healing of the ACL graft and possibly the prevention of early failure in ACLR knees.
3. Functional Recovery of the Knee
Restoring mechanical stability after ACL injury by electing to undergo ACLR does not address residual functional deficits.[83–85] Post-operative rehabilitation protocols treat the localized dysfunction and related symptoms, including joint effusion, limited range of motion, and deficits in quadriceps muscle strength and activation. Functional impairments that are implicated in second ACL injury continue to persist when athletes are returning to sport and are measurable for several months afterwards.[84–87] The evidence in the literature indicates that the recovery of knee function is the last of the remaining sequelae to normalize following ACLR.[88–91] Specifically, ACLR athletes demonstrate characteristic deficits in neuromuscular control and knee extension strength that do not begin to reach baseline levels until at least two years after ACLR.
3.1 Neuromuscular Control
Similar to primary ACL injury, the majority of second ACL injuries occur as non-contact episodes,[92] and failure to actively control the knee during multi-planar movements may lead to an increased risk of second ACL injury. A recent prospective study[24] screened 56 high-risk ACLR athletes at the time they were medically cleared to resume sports participation. One year after the initial assessment and actively participating in sport, 13 of the athletes sustained a second ACL injury.[24] A combination of neuromuscular and biomechanical factors, including transverse plane hip moments, frontal plane knee angles, sagittal plane knee moments, and deficits in postural stability predicted second injury with 92% sensitivity and 88% specificity.[24] These findings are important because they demonstrated that residual deficits in neuromuscular control are highly predictive of a second ACL injury after athletes resume sports participation.
Persistent, faulty neuromuscular characteristics are evident in even basic biomechanical tasks such as walking. The authors of a recent systematic review[88] conducted a comprehensive overview of kinematic and kinetic variables present during gait in athletes following ACLR. A review of over twenty studies with a mean gait analysis at 29.3 months (range between 3 weeks to 5.7 years) observed that altered biomechanics in all three planes are common after ACLR and may persist up to five years after ACLR.[88] A more recent systematic review and meta-analysis[89] compared the knee kinematic and kinetics during walking of ACLR knees to healthy controls and uninjured contralateral limbs. The analysis of thirty-four studies identified lower peak flexion moments during 6–12 months post-ACLR and lower peak flexion angles during 1–3 years and ≥3 years after ACLR.[89] However, the pooled data provided evidence of no significant difference between peak knee adduction moments after 3 years following ACLR.[89] The recovery of normal neuromuscular control during daily activities such as gait may be significantly delayed after ACLR.
To date, two studies have reported the progressive recovery of neuromuscular control during gait 2 years or later following ACLR. Roewer and colleagues[84] recruited a cohort of high-risk athletes and assessed knee strength and biomechanics during gait, initially at 6 months and then again at 2 years after ACLR. The acute post-injury assessment revealed asymmetrical knee angles, knee moments, and hip and knee power that also persisted to 6 months after ACLR.[84] Two years after surgery, quadriceps strength continued to improve and the kinematic and kinetic asymmetries that were present at 6 months were resolved, which indicated that athletes have the capability to functionally improve up to two-years after ACLR.[84] Webster et al.[93] also assessed longitudinal changes in knee biomechanics during gait at an initial assessment of 10 months and then again at 3 years after ACLR. An improvement in knee extension and internal rotation was documented over time.[93] Primarily, knee biomechanics remained relatively unchanged from the initial and final assessment.[93] However, the results indicated that normal gait may recover over the longer time frames, past the one year time point.[93]
Altered neuromuscular control is also commonly reported during sports-related, high demand activities following ACLR. Sports-specific jumping tasks have revealed alterations in force generation and attenuation at the ACLR knee up to two years after ACLR and beyond.[94–96] Performance during functional hop testing is a common assessment for clearance of athletes for unrestricted sports activities. A recent systematic review[97] reported the results of functional performance testing at differing time points following ACLR. A review of 88 studies and nearly 5,000 patients observed that the 4 standard hop tests (single-leg, cross-over, triple, and timed 6-meter hop tests) were the common functional assessments.[97] The results indicated that athletes reach 90% limb symmetry index (LSI) at 6 to 9 months postoperatively.[97] However, when more demanding functional tasks, such as endurance hop testing, are utilized, the results indicated larger deficits over the same 6 to 9-month time points.[97] These deficits appeared to normalize at 24 months post-ACLR, with reported LSI in the mid 90’s, which are comparable to the standard hop tests.[97]
More recently, groups have utilized more invasive techniques to study in vivo, dynamic knee function after ACLR.[98] Dual fluoroscopy and dynamic stereo-radiography is becoming more widely accessible because it provides better precision and more reliability than the use of high-speed cameras or marker based motion capture systems.[98] Hoshino and colleagues[99] investigated whether knee kinematics and joint contact mechanics can be restored after ACLR with a double-bundle or single-bundle graft using dynamic stereo x-ray to capture biplane radiographic images. The athletes were on average a little more than one year out from ACLR and were performing downhill treadmill running.[99] The study concluded that neither ACLR procedure restored normal knee kinematics or medial joint sliding.[99] In addition, developments in quantitative magnetic resonance imaging (MRI) have allowed researchers to evaluate the composition and structures within the knee. A recent study used volumetric dynamic imaging to assess contact patterns during an active knee flexion/extension task in athletes an average of 2 years post-ACLR.[100] There were no reported significant differences in cartilage thickness between the ACLR group and healthy control group.[100] However, the ACLR group demonstrated a greater reduction in the fraction of water bound by proteoglycan and greater contact in the medial and posterior portion of the knee compared to the control group.[100] In contrast to the commonly used high-speed cameras, these systems are far more expensive, expose the patient to more radiation, and highly complex. Regardless of technique used to assess kinematics and kinetics, athletes are still presenting with large deficits in the 6–12 month time frame, but normalizing closer to 2 years after ACLR.
Failure to recover normal knee function may be related to the inability to restore intrinsic properties of the native ACL. Although functional asymmetries may abate over time, normal neuromuscular control may never fully recover following ACLR.[88] A new standard of neuromuscular control that involves deficits not significantly different from baseline function may be inevitable in some athletes.
3.2 Quadriceps Strength
Lower extremity muscle weakness is a debilitating and ubiquitous impairment resulting from ACL injury. Although the relative ratio between quadriceps and hamstring strengths has been implicated in primary ACL injury risk,[101] the direct relationship of knee extensor and flexor strength to second ACL has not been assessed. The majority of sports medicine clinicians and physical therapists advocate a recovery of quadriceps and hamstring torque production equivalent to the contralateral limb prior to participating in high level, sports activity. However, the evidence in the literature strongly indicates that quadriceps strength deficits are commonly observed for several months and years following ACLR, in spite of formal rehabilitation focusing on rebuilding muscle strength.[91] A systematic review and meta-analysis investigated the influence of graft choice on isokinetic muscle strength 4 to 24 months following ACLR.[90] The study observed athletes who elect to receive a patellar tendon autograft demonstrated a greater knee extensor deficit and lower knee flexor deficits than patients with a hamstring tendon autograft.[90] Importantly, the strength deficits were unresolved up to two years following ACLR.[90] The impact of lower extremity muscle weakness has significant functional implications as athletes with greater strength deficits demonstrate decreased functional performance and landing strategies that increase risk of second ACL injury.[102, 103]
Recovery of quadriceps and hamstring strength is commonly observed over time. However, the evidence clearly indicates that athletes consistently demonstrate significant knee extensor and flexor strength deficits during the expected time frame to RTS, but these deficits begin to normalize approximately two years after ACLR. A few studies that demonstrate a recovery of knee strength at two years are highlighted below. Aune et al.[104] longitudinally compared isokinetic knee extensor and flexor strength between athletes who received two different autografts for ACLR. Twenty-four months after surgery, nearly symmetrical knee extensor and flexor strength measurements were reported within the groups, and significant differences between the two cohorts were not observed.[104] Further, Inagaki and associates[105] assessed clinical outcomes two years following ACLR. This study documented that average peak isokinetic knee extensor and flexor measurements at two years demonstrated comparable symmetry to an uninjured population (<15% deficit).[105]
Longitudinal prospective, randomized clinical trials may provide valuable insight on trends in clinical outcomes. In one such study, Aglietti et al.[106] assessed 120 athletes in a prospective, randomized study to compare 2 unique autografts fixed with modern devices at 4 months, 12 months, and 24 months. An isokinetic dynamometer was used to measure concentric knee extensors and flexors muscle at 60, 120, and 180 degrees/second.[106] At the two-year follow-up evaluation, knee extensor and flexor strength of the involved limb was comparable with the contralateral side, and in some instances even greater.[106] Furthermore, a marked improvement in extensor strength was observed over time regardless of the graft type, and only became symmetrical with the contralateral side at two years post-operative.[106] In addition, Maletis and colleagues[107] also conducted a similar prospective, randomized study using similar autografts and assessment time points. Isokinetic knee extension/flexion measurements were also conducted at 60, 180, and 300 degrees/second.[107] Similarly, at the two-year follow-up, clinically meaningful significant differences were not observed in knee extension and flexion strength.[107] Extensor muscle strength once again significantly improved over time, and became comparable to the contralateral side at two years.[107] It is common to measure variable measures of knee strength following ACLR, but the recovery of strength seems to be sustained beyond the two-year time point.
Longitudinal studies of more than two years have also demonstrated the sustained recovery of knee strength. Studies that evaluated athletes for over five years after ACLR reported quadriceps strength measurements comparable to a healthy athlete population, with minimal deficits between 6% and 10%.[108–110] Another benefit of delay of return to pre-injury level of activity for up to two years after ACLR is the recovery of baseline knee strength and a potential reduction of second ACL injury risk.
3.3 Effect of Surgical Techniques and Post-Operative Rehabilitation
In addition, functional recovery of the knee after ACLR may be related to surgical techniques utilized in ACLR and post-operative rehabilitation programs. These are highly researched and discussed topics in sports medicine that have minimal consensus. Here, we give a brief overview of the recent evidence and how these factors may affect early failures. In particular, femoral tunnel placement during ACLR has highlighted the impact of surgical techniques on second ACL injury risk. A recent report has observed that femoral tunnel malposition was the most commonly cited reason for a graft failure in a large ACLR cohort.[111] Also, the Danish Knee Ligament Registry observed an increased risk of revision after anteromedial femoral tunnel placement compared with a transtibial approach.[112] Current techniques in ACLR over the past several years have focused on reproducing more anatomical tunnel placement and graft geometry to restore knee kinematics.[98] Xu et al.[113] demonstrated in a cadaveric study that an anatomic anteromedial tunnel placement can lead to biomechanical advantages when compared to a non-anatomic placement, and the anatomic placement better restores knee kinematics to the native intact ACL state.[113] However, the anatomic placement had significantly greater in situ forces than the non-anatomic placement making it more vulnerable to graft failure.[113] Therefore, delaying a return to activity longer than the expected timeline may significantly help the recovering knee withstand the forces of returning to sport. It is likely that misplaced tunnels are responsible for early traumatic failures, but also may predispose a graft to aberrant biomechanics causing it to rupture at a later time.[114] Although differences in outcomes may be reported, it is generally thought that the recent trend in surgical practice of a more anatomic placement to resemble the native ligament is better for the outcome of the graft as long as it is allowed to heal completely.[115, 116] Because the significant majority of athletes undergo ACLR, it is also important to understand how surgery and rehabilitation together can be utilized to optimize patient knee outcomes.
Post-operative rehabilitation programs are considered essential for rebuilding lower extremity muscle strength and restoring joint mobility and neuromuscular control with the goal of returning to pre-injury levels of activity. Currently, there is little consensus regarding an optimal rehabilitation program to return athletes back to their pre-injury level of sport in a safe, effective manner. A systematic review of 33 randomized clinical trials observed that several of the studies had significant flaws and little evidence could be derived from them.[117] The authors concluded that there was evidence for high intensity neuromuscular electrical stimulation, volitional exercises, and neuromuscular training.[117] More recently, in a randomized control trial, 74 ACLR patients were assigned to either a neuromuscular training program or a traditional strength training program and followed for 2 years after ACLR.[118] The neuromuscular training group reported greater global knee function and reduced pain during activity, while the strength training group demonstrated greater hamstring strength at 2 years post-ACLR.[118] However, there were no significant differences between the two groups in Cincinnati knee score at 1 and 2 years.[118] Grindem et al.[119] compared the preoperative and 2 year postoperative self-reported outcomes of ACLR patients who underwent a progressive preoperative and postoperative rehabilitation compared with the institution’s standard of care. The patients that were enrolled in the preoperative and postoperative rehabilitation program demonstrated significantly greater Knee Injury and Osteoarthritis Outcome Score (KOOS) in all subscales preoperatively and 2 years postoperatively than the patients in the standard of care group.[119] Furthermore, a group investigated whether there were any long-term differences (at 2 to 4 years after ACLR) in athletes who underwent a home-based or physical therapist-supervised rehabilitation program in the first 3 months after ACLR.[120] The home-based group had a significantly higher ACL quality of life questionnaire at a mean of 38 months after ACLR, but there were no significant differences in knee extension/flexion range of motion, knee laxity, lower extremity strength, and International Knee Documentation Committee score.[120] The optimal rehabilitation program is still unknown, and the lack of a standard rehabilitation treatment protocol is a major limitation to returning athletes back to sport safely. Regardless of the post-operative rehabilitation protocol, the outcomes following ACLR begin to normalize nearly two years or later. The combination of time and comprehensive functional criteria is critical to return to high demand activity, but the current approach of accelerated rehabilitation and timeline to recover is detrimental to the athlete.
Surgical techniques and post-operative rehabilitation programs are certainly a topic of ongoing debate and research studies. Importantly, regardless of surgical techniques and rehabilitation protocols, athletes returning to activity too early, prior to recovering baseline knee joint health and function, increase their risk for a subsequent ACL injury. The evidence in the literature indicates that significantly delaying a return to high level sports until nearly two years will benefit the athlete.
4. Conclusion
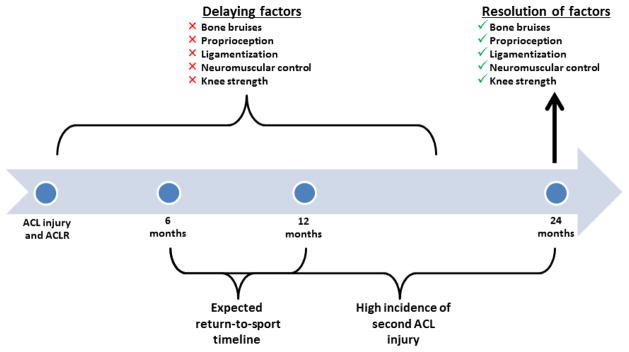
Deficits in knee function and biological health of the knee joint are all common up to one year following ACLR. A marked improvement in joint health and function and a resolution of symptoms is strongly indicated at two years and beyond following ACLR. The two-year time point post-ACLR is not arbitrary, but is evident based on a discerning review of the current evidence. A timeline of recovery that is strongly indicated by the current literature and presented here in this current opinion article is displayed in Figure 1. The sports medicine community has made significant advances in surgical techniques, post-operative rehabilitation, and identification of risk factors for second injury, but this has not translated to a reduction in secondary ACL injury risk. The recovery of baseline knee health and function should be a fundamental requisite prior to returning to sport following ACLR.
Figure 1.
A timeline of recovery that is indicated in the literature and presented in this current opinion article. Recovery of baseline, or not significantly different from baseline, joint health and function is not indicated until two-years after ACLR. We advocate significantly delaying returning to sport to at least two years after ACLR. Anterior cruciate ligament (ACL) reconstruction (ACLR).
In summary, the young, active athlete who returns to high level landing, pivoting sports is at significantly greater risk for a second ACL injury.[17, 19] These injuries are also most frequent in the first 2 years after ACLR.[22, 26] Several risk factors are implicated in this increased risk of second ACL injury, including surgical factors (graft placement and type),[6, 7] demographics (sex and age),[121] activity level,[17] sport,[16] and neuromuscular and biomechanical factors.[24] Also, there are anatomical and intrinsic risk factors that have not been discussed in this article because these factors are not subject to change by delaying a RTS.[122] We have presented the evidence in the literature showing that at 2 years after ACLR, biological healing (absence of bone bruises, ACL graft maturation, and sensory restoration) has occurred and functional recovery (biomechanical and neuromuscular control and quadriceps strength) of the knee has normalized or is not significantly different from baseline. Therefore, delaying a return to high level activity for high-risk athletes until two years after ACLR will restore knee joint homeostasis and significantly reduce the risk of subsequent injury.
One of the challenges to be faced with a new paradigm such as that advocated in the current article relates to the differential recovery of athletes following ACLR. There are some young, active athletes who recover more quickly and successfully transition back to sports, as the majority of athletes safely return to some form of activity following ACLR. In addition, waiting two years after ACLR to return to pre-injury level of activity means that the athlete themselves, their coaches, and their parents must be willing to potentially not return at the same level of sport and miss up to two seasons of their respective sport. This may have serious consequences on the immediate career for the athletes and depending on the athlete’s potential, their future long-term career. However, the current approach of early, accelerated rehabilitation programs and the expected timeline to recover in 6 to 12 months is deleterious because the athlete is not completely recovered which predisposes them to an increased risk for a second ACL injury. The young, active athlete who attempts to resume sports participation at the same competitive level has a nearly 1 in 3 chance of going on to a second ACL injury within the first or second year post-ACLR. Therefore, the evidence advocates that these athletes delay a return to sports for two-years to mitigate the unacceptably high risk for a second ACL injury, especially in those under 20 years of age.
Key Points.
Young, active anterior cruciate ligament (ACL) reconstructed (ACLR) athletes who return to high level sports sustain a disproportionately greater incidence of second ACL injuries within the first two years after ACLR.
The evidence in the literature indicates that the ACLR athletes do not regain baseline, or not significantly different from baseline, knee joint biological health and function until approximately two years after ACLR.
The incidence of second ACL injuries will significantly decrease if ACLR athletes delay a return to high level activity until two years after ACLR.
Acknowledgments
Funding
The authors acknowledge funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases: R01-AR049735, R01-AR055563, and R01AR056259 to TEH.
The authors would like to thank Drs. Stephanie Di Stasi, Wendy Hurd, and Kate Webster for their input, clinical expertise, editorial work, and conversations regarding the topic presented in this article.
Footnotes
Compliance with Ethical Standards
Conflicts of Interest
Christopher Nagelli and Timothy Hewett declare that they have no conflicts of interest relevant to the content of this review.
References
- 1.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014 Oct;42(10):2363–70. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 2.Wright RW, Magnussen RA, Dunn WR, et al. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction a systematic review. J Bone Joint Surg Am. 2011 Jun;93A(12):1159–65. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourke HE, Salmon LJ, Waller A, et al. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012 Sep;40(9):1985–92. doi: 10.1177/0363546512454414. [DOI] [PubMed] [Google Scholar]
- 4.Drogset JO, Grontvedt T, Robak OR, et al. A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 2006 May;88(5):944–52. doi: 10.2106/JBJS.D.02876. [DOI] [PubMed] [Google Scholar]
- 5.Morgan MD, Salmon LJ, Waller A, et al. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016 Feb;44(2):384–92. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- 6.Brophy RH, Selby RM, Altchek DW. Anterior cruciate ligament revision: double-bundle augmentation of primary vertical graft. Arthroscopy. 2006 Jun;22(6):683, e1–5. doi: 10.1016/j.arthro.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 7.Marchant BG, Noyes FR, Barber-Westin SD, et al. Prevalence of nonanatomical graft placement in a series of failed anterior cruciate ligament reconstructions. Am J Sports Med. 2010 Oct;38(10):1987–96. doi: 10.1177/0363546510372797. [DOI] [PubMed] [Google Scholar]
- 8.Hui C, Salmon LJ, Kok A, et al. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med. 2011 Jan;39(1):89–98. doi: 10.1177/0363546510379975. [DOI] [PubMed] [Google Scholar]
- 9.Leys T, Salmon L, Waller A, et al. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012 Mar;40(3):595–605. doi: 10.1177/0363546511430375. [DOI] [PubMed] [Google Scholar]
- 10.Laboute E, Savalli L, Puig P, et al. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med. 2010 Dec;53(10):598–614. doi: 10.1016/j.rehab.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014 Oct;42(10):2319–28. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 12.Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med. 2014 Feb;42(2):285–91. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 13.Maletis GB, Inacio MC, Desmond JL, et al. Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Joint J. 2013 May;95-B(5):623–8. doi: 10.1302/0301-620X.95B5.30872. [DOI] [PubMed] [Google Scholar]
- 14.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009 Feb;37(2):246–51. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 15.Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012 Mar;22(2):116–21. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016 Jun 3; doi: 10.1177/0363546516648439. [DOI] [PubMed] [Google Scholar]
- 17.Kamien PM, Hydrick JM, Replogle WH, et al. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013 Aug;41(8):1808–12. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 18.Magnussen RA, Lawrence JT, West RL, et al. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012 Apr;28(4):526–31. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 19.Webster KE, Feller JA, Leigh WB, et al. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014 Mar;42(3):641–7. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- 20.Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014 Apr 21;42(7):1567–73. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maletis GB, Inacio MC, Reynolds S, et al. Incidence of postoperative anterior cruciate ligament reconstruction infections: graft choice makes a difference. Am J Sports Med. 2013 Aug;41(8):1780–5. doi: 10.1177/0363546513490665. [DOI] [PubMed] [Google Scholar]
- 22.Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005 Aug;21(8):948–57. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 23.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009 Dec;37(12):2362–7. doi: 10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 24.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010 Oct;38(10):1968–78. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fauno P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the Danish registry of knee ligament reconstruction. Orthop J Sports Med. 2014 Oct;2(10):2325967114552405. doi: 10.1177/2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012 Jul;40(7):1551–7. doi: 10.1177/0363546512446000. [DOI] [PubMed] [Google Scholar]
- 27.Paulos L, Noyes FR, Grood E, et al. Knee rehabilitation after anterior cruciate ligament reconstruction and repair. Am J Sports Med. 1981 May-Jun;9(3):140–9. doi: 10.1177/036354658100900303. [DOI] [PubMed] [Google Scholar]
- 28.Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1992;15(6):256–64. doi: 10.2519/jospt.1992.15.6.256. [DOI] [PubMed] [Google Scholar]
- 29.Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016 May 9; doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scheffler SU, Unterhauser FN, Weiler A. Graft remodeling and ligamentization after cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008 Sep;16(9):834–42. doi: 10.1007/s00167-008-0560-8. [DOI] [PubMed] [Google Scholar]
- 31.Amiel D, Kleiner JB, Roux RD, et al. The phenomenon of “ligamentization”: anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orthop Res. 1986;4(2):162–72. doi: 10.1002/jor.1100040204. [DOI] [PubMed] [Google Scholar]
- 32.Arnoczky SP, Tarvin GB, Marshall JL. Anterior cruciate ligament replacement using patellar tendon. An evaluation of graft revascularization in the dog. J Bone Joint Surg Am. 1982 Feb;64(2):217–24. [PubMed] [Google Scholar]
- 33.Claes S, Verdonk P, Forsyth R, et al. The “ligamentization” process in anterior cruciate ligament reconstruction what happens to the human graft? a systematic review of the literature. Am J Sports Med. 2011 Nov;39(11):2476–83. doi: 10.1177/0363546511402662. [DOI] [PubMed] [Google Scholar]
- 34.Pauzenberger L, Syre S, Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013 Oct;29(10):1712–21. doi: 10.1016/j.arthro.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 35.Abe S, Kurosaka M, Iguchi T, et al. Light and electron microscopic study of remodeling and maturation process in autogenous graft for anterior cruciate ligament reconstruction. Arthroscopy. 1993;9(4):394–405. doi: 10.1016/s0749-8063(05)80313-5. [DOI] [PubMed] [Google Scholar]
- 36.Rougraff B, Shelbourne KD, Gerth PK, et al. Arthroscopic and histologic analysis of human patellar tendon autografts used for anterior cruciate ligament reconstruction. Am J Sports Med. 1993 Mar-Apr;21(2):277–84. doi: 10.1177/036354659302100219. [DOI] [PubMed] [Google Scholar]
- 37.Borchers JR, Kaeding CC, Pedroza AD, et al. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011 Sep;39(9):1889–93. doi: 10.1177/0363546511406871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spindler KP, Schils JP, Bergfeld JA, et al. Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med. 1993 Jul-Aug;21(4):551–7. doi: 10.1177/036354659302100412. [DOI] [PubMed] [Google Scholar]
- 39.Boden BP, Dean GS, Feagin JA, Jr, et al. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000 Jun;23(6):573–8. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 40.Rosen MA, Jackson DW, Berger PE. Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy. 1991;7(1):45–51. doi: 10.1016/0749-8063(91)90077-b. [DOI] [PubMed] [Google Scholar]
- 41.Dunn WR, Spindler KP, Amendola A, et al. Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. Am J Sports Med. 2010 Sep;38(9):1778–87. doi: 10.1177/0363546510370279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vellet AD, Marks PH, Fowler PJ, et al. Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology. 1991 Jan;178(1):271–6. doi: 10.1148/radiology.178.1.1984319. [DOI] [PubMed] [Google Scholar]
- 43.Mink JH, Deutsch AL. Occult cartilage and bone injuries of the knee: detection, classification, and assessment with MR imaging. Radiology. 1989 Mar;170(3 Pt 1):823–9. doi: 10.1148/radiology.170.3.2916038. [DOI] [PubMed] [Google Scholar]
- 44.Roemer FW, Frobell R, Hunter DJ, et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage. 2009 Sep;17(9):1115–31. doi: 10.1016/j.joca.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 45.Johnson DL, Bealle DP, Brand JC, Jr, et al. The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med. 2000 Mar-Apr;28(2):152–5. doi: 10.1177/03635465000280020301. [DOI] [PubMed] [Google Scholar]
- 46.Boks SS, Vroegindeweij D, Koes BW, et al. Clinical consequences of posttraumatic bone bruise in the knee. Am J Sports Med. 2007 Jun;35(6):990–5. doi: 10.1177/0363546506297059. [DOI] [PubMed] [Google Scholar]
- 47.Costa-Paz M, Muscolo DL, Ayerza M, et al. Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy. 2001 May;17(5):445–9. doi: 10.1053/jars.2001.23581. [DOI] [PubMed] [Google Scholar]
- 48.Hanypsiak BT, Spindler KP, Rothrock CR, et al. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008 Apr;36(4):671–7. doi: 10.1177/0363546508315468. [DOI] [PubMed] [Google Scholar]
- 49.Papalia R, Torre G, Vasta S, et al. Bone bruises in anterior cruciate ligament injured knee and long-term outcomes. A review of the evidence. Open Access J Sports Med. 2015;6:37–48. doi: 10.2147/OAJSM.S75345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boks SS, Vroegindeweij D, Koes BW, et al. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: prevalence and associations with traumatic history in general practice. Am J Sports Med. 2006 Dec;34(12):1984–91. doi: 10.1177/0363546506290189. [DOI] [PubMed] [Google Scholar]
- 51.Boks SS, Vroegindeweij D, Koes BW, et al. Follow-up of posttraumatic ligamentous and meniscal knee lesions detected at MR imaging: systematic review. Radiology. 2006 Mar;238(3):863–71. doi: 10.1148/radiol.2382050063. [DOI] [PubMed] [Google Scholar]
- 52.Dye SF, Chew MH. The use of scintigraphy to detect increased osseous metabolic activity about the knee. Instr Course Lect. 1994;43:453–69. [PubMed] [Google Scholar]
- 53.Leppala J, Kannus P, Natri A, et al. Effect of anterior cruciate ligament injury of the knee on bone mineral density of the spine and affected lower extremity: a prospective one-year follow-up study. Calcif Tissue Int. 1999 Apr;64(4):357–63. doi: 10.1007/s002239900632. [DOI] [PubMed] [Google Scholar]
- 54.Nyland J, Fisher B, Brand E, et al. Osseous deficits after anterior cruciate ligament injury and reconstruction: a systematic literature review with suggestions to improve osseous homeostasis. Arthroscopy. 2010 Sep;26(9):1248–57. doi: 10.1016/j.arthro.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 55.Zerahn B, Munk AO, Helweg J, et al. Bone mineral density in the proximal tibia and calcaneus before and after arthroscopic reconstruction of the anterior cruciate ligament. Arthroscopy. 2006 Mar;22(3):265–9. doi: 10.1016/j.arthro.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 56.Sievanen H, Kannus P, Heinonen A, et al. Bone mineral density and muscle strength of lower extremities after long-term strength training, subsequent knee ligament injury and rehabilitation: a unique 2-year follow-up of a 26-year-old female student. Bone. 1994 Jan-Feb;15(1):85–90. doi: 10.1016/8756-3282(94)90896-6. [DOI] [PubMed] [Google Scholar]
- 57.Dye SF, Chew MH. Restoration of osseous homeostasis after anterior cruciate ligament reconstruction. Am J Sports Med. 1993 Sep-Oct;21(5):748–50. doi: 10.1177/036354659302100521. [DOI] [PubMed] [Google Scholar]
- 58.van Meer BL, Waarsing JH, van Eijsden WA, et al. Bone mineral density changes in the knee following anterior cruciate ligament rupture. Osteoarthritis Cartilage. 2014 Jan;22(1):154–61. doi: 10.1016/j.joca.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 59.Zimny ML, Schutte M, Dabezies E. Mechanoreceptors in the human anterior cruciate ligament. Anat Rec. 1986 Feb;214(2):204–9. doi: 10.1002/ar.1092140216. [DOI] [PubMed] [Google Scholar]
- 60.Schultz RA, Miller DC, Kerr CS, et al. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am. 1984 Sep;66(7):1072–6. [PubMed] [Google Scholar]
- 61.Solomonow M, Baratta R, Zhou BH, et al. The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. Am J Sports Med. 1987 May-Jun;15(3):207–13. doi: 10.1177/036354658701500302. [DOI] [PubMed] [Google Scholar]
- 62.Dyhre-Poulsen P, Krogsgaard MR. Muscular reflexes elicited by electrical stimulation of the anterior cruciate ligament in humans. J Appl Physiol. 2000 Dec;89(6):2191–5. doi: 10.1152/jappl.2000.89.6.2191. [DOI] [PubMed] [Google Scholar]
- 63.Krogsgaard MR, Fischer-Rasmussen T, Dyhre-Poulsen P. Absence of sensory function in the reconstructed anterior cruciate ligament. J Electromyogr Kinesiol. 2011 Feb;21(1):82–6. doi: 10.1016/j.jelekin.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 64.Ochi M, Iwasa J, Uchio Y, et al. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999 Sep;81(5):902–6. doi: 10.1302/0301-620x.81b5.9202. [DOI] [PubMed] [Google Scholar]
- 65.Ochi M, Iwasa J, Uchio Y, et al. Induction of somatosensory evoked potentials by mechanical stimulation in reconstructed anterior cruciate ligaments. J Bone Joint Surg Br. 2002 Jul;84(5):761–6. doi: 10.1302/0301-620x.84b5.12584. [DOI] [PubMed] [Google Scholar]
- 66.Nyland J, Brosky T, Currier D, et al. Review of the afferent neural system of the knee and its contribution to motor learning. J Orthop Sports Phys Ther. 1994 Jan;19(1):2–11. doi: 10.2519/jospt.1994.19.1.2. [DOI] [PubMed] [Google Scholar]
- 67.Hewett TE, Paterno MV, Myer GA. Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res. 2002 Sep;(402):76–94. doi: 10.1097/00003086-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 68.Iwasa J, Ochi M, Adachi N, et al. Proprioceptive improvement in knees with anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000 Dec;(381):168–76. doi: 10.1097/00003086-200012000-00020. [DOI] [PubMed] [Google Scholar]
- 69.MacDonald PB, Hedden D, Pacin O, et al. Proprioception in anterior cruciate ligament-deficient and reconstructed knees. Am J Sports Med. 1996 Nov-Dec;24(6):774–8. doi: 10.1177/036354659602400612. [DOI] [PubMed] [Google Scholar]
- 70.Negahban H, Mazaheri M, Kingma I, et al. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014 Jul;22(7):1491–504. doi: 10.1007/s00167-013-2501-4. [DOI] [PubMed] [Google Scholar]
- 71.Roberts D, Friden T, Stomberg A, et al. Bilateral proprioceptive defects in patients with a unilateral anterior cruciate ligament reconstruction: a comparison between patients and healthy individuals. J Orthop Res. 2000 Jul;18(4):565–71. doi: 10.1002/jor.1100180408. [DOI] [PubMed] [Google Scholar]
- 72.Risberg MA, Beynnon BD, Peura GD, et al. Proprioception after anterior cruciate ligament reconstruction with and without bracing. Knee Surg Sports Traumatol Arthrosc. 1999;7(5):303–9. doi: 10.1007/s001670050168. [DOI] [PubMed] [Google Scholar]
- 73.Gokeler A, Benjaminse A, Hewett TE, et al. Proprioceptive deficits after ACL injury: are they clinically relevant? Br J Sports Med. 2012 Mar;46(3):180–92. doi: 10.1136/bjsm.2010.082578. [DOI] [PubMed] [Google Scholar]
- 74.Sanchez M, Anitua E, Azofra J, et al. Ligamentization of tendon grafts treated with an endogenous preparation rich in growth factors: gross morphology and histology. Arthroscopy. 2010 Apr;26(4):470–80. doi: 10.1016/j.arthro.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 75.Weiler A, Peters G, Maurer J, et al. Biomechanical properties and vascularity of an anterior cruciate ligament graft can be predicted by contrast-enhanced magnetic resonance imaging. A two-year study in sheep. Am J Sports Med. 2001 Nov-Dec;29(6):751–61. doi: 10.1177/03635465010290061401. [DOI] [PubMed] [Google Scholar]
- 76.Rabuck SJ, Baraga MG, Fu FH. Anterior cruciate ligament healing and advances in imaging. Clin Sports Med. 2013 Jan;32(1):13–20. doi: 10.1016/j.csm.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 77.Vogl TJ, Schmitt J, Lubrich J, et al. Reconstructed anterior cruciate ligaments using patellar tendon ligament grafts: diagnostic value of contrast-enhanced MRI in a 2-year follow-up regimen. Eur Radiol. 2001;11(8):1450–6. doi: 10.1007/s003300100870. [DOI] [PubMed] [Google Scholar]
- 78.Zaffagnini S, De Pasquale V, Marchesini Reggiani L, et al. Neoligamentization process of BTPB used for ACL graft: histological evaluation from 6 months to 10 years. Knee. 2007 Mar;14(2):87–93. doi: 10.1016/j.knee.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 79.Gohil S, Annear PO, Breidahl W. Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br. 2007 Sep;89(9):1165–71. doi: 10.1302/0301-620X.89B9.19339. [DOI] [PubMed] [Google Scholar]
- 80.Ge Y, Li H, Tao H, et al. Comparison of tendon-bone healing between autografts and allografts after anterior cruciate ligament reconstruction using magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):954–60. doi: 10.1007/s00167-013-2755-x. [DOI] [PubMed] [Google Scholar]
- 81.Li H, Tao H, Cho S, et al. Difference in graft maturity of the reconstructed anterior cruciate ligament 2 years postoperatively: a comparison between autografts and allografts in young men using clinical and 3.0-T magnetic resonance imaging evaluation. Am J Sports Med. 2012 Jul;40(7):1519–26. doi: 10.1177/0363546512443050. [DOI] [PubMed] [Google Scholar]
- 82.Suomalainen P, Moisala AS, Paakkala A, et al. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med. 2011 Aug;39(8):1615–22. doi: 10.1177/0363546511405024. [DOI] [PubMed] [Google Scholar]
- 83.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–6. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 84.Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011 Jul 7;44(10):1948–53. doi: 10.1016/j.jbiomech.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Di Stasi S, Hartigan EH, Snyder-Mackler L. Sex-specific gait adaptations prior to and up to 6 months after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015 Mar;45(3):207–14. doi: 10.2519/jospt.2015.5062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Di Stasi SL, Logerstedt D, Gardinier ES, et al. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013 Jun;41(6):1310–8. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xergia SA, Pappas E, Zampeli F, et al. Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2013 Mar;43(3):154–62. doi: 10.2519/jospt.2013.3967. [DOI] [PubMed] [Google Scholar]
- 88.Gokeler A, Benjaminse A, van Eck CF, et al. Return of normal gait as an outcome measurement in acl reconstructed patients. A systematic review. Int J Sports Phys Ther. 2013 Aug;8(4):441–51. [PMC free article] [PubMed] [Google Scholar]
- 89.Hart HF, Culvenor AG, Collins NJ, et al. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2016 May;50(10):597–612. doi: 10.1136/bjsports-2015-094797. [DOI] [PubMed] [Google Scholar]
- 90.Xergia SA, McClelland JA, Kvist J, et al. The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011 May;19(5):768–80. doi: 10.1007/s00167-010-1357-0. [DOI] [PubMed] [Google Scholar]
- 91.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008 Jul;27(3):405–24. vii–ix. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 92.Wright RW, Huston LJ, Spindler KP, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010 Oct;38(10):1979–86. doi: 10.1177/0363546510378645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Webster KE, Feller JA, Wittwer JE. Longitudinal changes in knee joint biomechanics during level walking following anterior cruciate ligament reconstruction surgery. Gait Posture. 2012 Jun;36(2):167–71. doi: 10.1016/j.gaitpost.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 94.Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012 Jan;30(1):72–8. doi: 10.1002/jor.21504. [DOI] [PubMed] [Google Scholar]
- 95.Delahunt E, Prendiville A, Sweeney L, et al. Hip and knee joint kinematics during a diagonal jump landing in anterior cruciate ligament reconstructed females. J Electromyogr Kinesiol. 2012 Aug;22(4):598–606. doi: 10.1016/j.jelekin.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 96.Paterno MV, Ford KR, Myer GD, et al. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007 Jul;17(4):258–62. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 97.Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014 Jan;2(1):2325967113518305. doi: 10.1177/2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tashman S, Araki D. Effects of anterior cruciate ligament reconstruction on in vivo, dynamic knee function. Clin Sports Med. 2013 Jan;32(1):47–59. doi: 10.1016/j.csm.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hoshino Y, Fu FH, Irrgang JJ, et al. Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2013 Sep;471(9):2924–31. doi: 10.1007/s11999-012-2761-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kaiser J, Vignos MF, Liu F, et al. American Society of Biomechanics Clinical Biomechanics Award 2015: MRI assessments of cartilage mechanics, morphology and composition following reconstruction of the anterior cruciate ligament. Clin Biomech (Bristol, Avon) 2016 May;34:38–44. doi: 10.1016/j.clinbiomech.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Myer GD, Ford KR, Barber Foss KD, et al. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009 Jan;19(1):3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012 Sep;42(9):750–9. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schmitt LC, Paterno MV, Ford KR, et al. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015 Jul;47(7):1426–34. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Aune AK, Holm I, Risberg MA, et al. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction - A randomized study with two-year follow-up. Am J Sports Med. 2001 Nov-Dec;29(6):722–8. doi: 10.1177/03635465010290060901. [DOI] [PubMed] [Google Scholar]
- 105.Inagaki Y, Kondo E, Kitamura N, et al. Prospective clinical comparisons of semitendinosus versus semitendinosus and gracilis tendon autografts for anatomic double-bundle anterior cruciate ligament reconstruction. J Orthop Sci. 2013 Sep;18(5):754–61. doi: 10.1007/s00776-013-0427-9. [DOI] [PubMed] [Google Scholar]
- 106.Aglietti P, Giron F, Buzzi R, et al. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004 Oct;86-A(10):2143–55. [PubMed] [Google Scholar]
- 107.Maletis GB, Cameron SL, Tengan JJ, et al. A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007 Mar;35(3):384–94. doi: 10.1177/0363546506294361. [DOI] [PubMed] [Google Scholar]
- 108.Keays SL, Bullock-Saxton JE, Keays AC, et al. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med. 2007 May;35(5):729–39. doi: 10.1177/0363546506298277. [DOI] [PubMed] [Google Scholar]
- 109.Lautamies R, Harilainen A, Kettunen J, et al. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2008 Nov;16(11):1009–16. doi: 10.1007/s00167-008-0598-7. [DOI] [PubMed] [Google Scholar]
- 110.Moisala AS, Jarvela T, Kannus P, et al. Muscle strength evaluations after ACL reconstruction. Int J Sports Med. 2007 Oct;28(10):868–72. doi: 10.1055/s-2007-964912. [DOI] [PubMed] [Google Scholar]
- 111.Morgan JA, Dahm D, Levy B, et al. Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012 Nov;25(5):361–8. doi: 10.1055/s-0031-1299662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rahr-Wagner L, Thillemann TM, Pedersen AB, et al. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013 Jan;29(1):98–105. doi: 10.1016/j.arthro.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 113.Xu Y, Liu J, Kramer S, et al. Comparison of in situ forces and knee kinematics in anteromedial and high anteromedial bundle augmentation for partially ruptured anterior cruciate ligament. Am J Sports Med. 2011 Feb;39(2):272–8. doi: 10.1177/0363546510383479. [DOI] [PubMed] [Google Scholar]
- 114.Kato Y, Maeyama A, Lertwanich P, et al. Biomechanical comparison of different graft positions for single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013 Apr;21(4):816–23. doi: 10.1007/s00167-012-1951-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fu FH, van Eck CF, Tashman S, et al. Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc. 2015 Mar;23(3):640–8. doi: 10.1007/s00167-014-3209-9. [DOI] [PubMed] [Google Scholar]
- 116.Middleton KK, Hamilton T, Irrgang JJ, et al. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014 Jul;22(7):1467–82. doi: 10.1007/s00167-014-2846-3. [DOI] [PubMed] [Google Scholar]
- 117.Risberg MA, Lewek M, Snyder-Mackler L. A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Phys Ther Sport. 2004 Aug;5(3):125–45. [Google Scholar]
- 118.Risberg MA, Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009 Oct;37(10):1958–66. doi: 10.1177/0363546509335196. [DOI] [PubMed] [Google Scholar]
- 119.Grindem H, Granan LP, Risberg MA, et al. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2015 Mar;49(6):385–9. doi: 10.1136/bjsports-2014-093891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Grant JA, Mohtadi NG. Two- to 4-year follow-up to a comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction. Am J Sports Med. 2010 Jul;38(7):1389–94. doi: 10.1177/0363546509359763. [DOI] [PubMed] [Google Scholar]
- 121.Wiggins AJ, Grandhi RK, Schneider DK, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016 Jan 15; doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Christensen JJ, Krych AJ, Engasser WM, et al. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015 Oct;43(10):2510–4. doi: 10.1177/0363546515597664. [DOI] [PubMed] [Google Scholar]