Abstract
Background:
Scars over the face are cosmetically and psychologically disturbing. Various techniques have been described and are being practiced in the management of these scars.
Aims and Objectives:
This study was undertaken to study the safety, effectiveness of using dermal grafts as fillers in the management of facial scars due to acne, chickenpox, trauma or any others.
Materials and Methods:
Fifteen patients with atrophic facial scars of varied aetiology and willing for surgery were considered for dermal graft technique. After pre-operative workup, subcision was done 2 weeks before planned surgery. Depending on the type of scar, grafts were inserted using pocket or road railing techniques. Scar improvement was assessed based on patient satisfaction.
Results:
Linear scars showed excellent improvement. Acne, varicella and traumatic scars also showed good improvement. However, two patients did not appreciate improvement due to marked surface irregularities as the scars were elevated. They were further subjected to LASER and chemical peel resurfacing.
Conclusion:
Dermal grafting can be used in the management of any round to oval facial scar which is soft, prominent and at least 4–5 mm across; linear scars at least 2–3 mm across and 3–4 cm in length. However, scars with prominent surface irregularities need further resurfacing techniques along with dermal grafting.
Limitations:
Limitations of the study include small sample size, and only subjective assessment of the scar has been taken into consideration to assess the outcome.
KEYWORDS: Atrophic scar, dermal graft, pocket technique, railroad technique
INTRODUCTION
Scar formation is an inevitable result of surgery and trauma that results in full thickness epidermal loss. Acne and other inflammatory, infectious conditions such as varicella, odontogenic sinus, surgery and trauma can result in atrophic scars over the face. Scars over the face and other exposed parts can be cosmetically, psychologically and socially disturbing.[1] Various techniques such as subcision, microneedling, fillers, peels, autologous fat transplant, dermal graft and LASER resurfacing are being practiced in the management of atrophic scars. An ideal technique which is free of allergic reaction or irritation, economical, less time-consuming and easily available, which gives a permanent correction with no rejection or resorption, is still very far from reality. This study was undertaken to evaluate the effectiveness and safety of dermal grafting technique in the management of atrophic facial scars.
MATERIALS AND METHODS
Fifteen patients with atrophic facial scars of varied aetiology such as acne, varicella, traumatic or surgical linear scars, who had not responded to minor procedures such as subcision and microneedling and were willing for surgery, were considered for dermal grafting. Subcision was done about 2 weeks before the planned surgery. Proper counselling regarding the procedure, possible outcome, side effects and alternate modes of treatment was done. Required pre-operative investigations were done. After obtaining written informed consent, participants were posted for surgery. Pre-procedure photographs were taken. Retroauricular area was chosen as donor area. Under aseptic precautions, donor area was dermabraded with motorised dermabraders using dental burrs till there was pinpoint bleeding which ensured complete removal of epidermis [Figure 1a]. Depending on the type of scar, dermal grafts were harvested. For linear scars, a linear strip of appropriate length and breadth of dermal graft [Figure 1c and d] was obtained and wound closed using continuous sutures with 3-0 vicryl. For irregular and circular scars, dermal grafts were obtained using 6 mm punches [Figure 1b] and wound closed with simple sutures and dressed. The grafts so obtained were washed in normal saline and transferred to a Petri dish containing trypsin and incubated at 37 C for 45 min. Then, the grafts were again washed with normal saline and the action of trypsin neutralised with patients serum.
Figure 1.

Linear and circular graft harvesting from retroauricular area (a) retro auricular area dermabraded till there is pinpoint bleeding (b) circular grafts taken with 6mm punches (c) a linear dermal grafts taken from retro auricular area (d) linear dermal graft obtained
In the recipient area, for circular or irregular scar, grafts were placed below the scar using a pocket technique [Figure 2]. For linear scar, grafts were inserted using railroading technique[2] [Figure 3a–d]. In pocket technique, a pocket was created below the scar by doing subcision using 18-G needle. A small nick was made on either side of the needle [Figure 2]. The prepared grafts were inserted into the pocket using Jeweler's forceps. Multiple grafts are similarly placed till the scar is elevated. Entry wound was closed with 5-0 ethilon. In railroad technique, tunnelling was done beneath the scar using 18-G needle [Figure 3a–d]. A small nick on either side of needle was put to create an entry wound. From the bevelled edge, a suture was passed through the needle, the other end of which was tied to the one end of the linear graft previously prepared. Then, the needle was slowly withdrawn; at the same time, traction was given to the graft by pulling the suture and pushing the graft into the tunnel till it reached the other end of the tunnel. Entry wound was closed with 5-0 Prolene. Steri-Strips were applied. Immediate elevation of the scar was noted. Patients were reviewed after 3rd day for donor area, dressing and suture removal of recipient area was done on the 5th day. Patients were followed up again at 6 months, and results were assessed using visual analogue scale ranging from 1 (least satisfied) to 10 (most satisfied).
Figure 2.

Pocket technique of graft insertion
Figure 3.
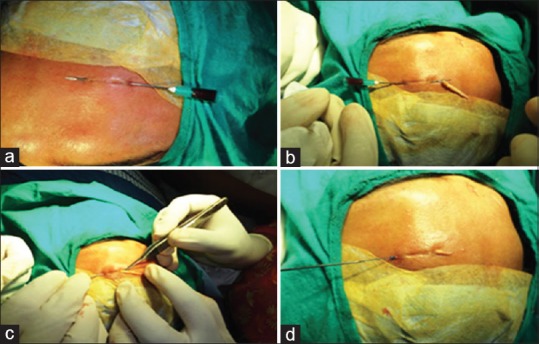
Railroad technique of graft insertion (a) a needle inserted just beneath the linear scar (b) a suture thread tied to the graft is made to pass through the bevel of the needle till it comes out of the hub (c) slow traction being given to the thread simultaneously pushing the graft below the scar (d) graft completely placed below the scar
RESULTS
Among fifteen patients recruited for surgery, eight were males and seven females. Mean age of patients was 35 years. Out of them, eight scars were secondary to trauma, two were post to varicella scar, three post acne scars, one due to branding and one due to healed odontogenic sinus scar. Five were linear scars with width ranging between 3 and 5 mm, length 1–3 cm, seven were circular with diameter ranging between 4–13 mm and three were irregular scars. Surface changes were minimal or absent in thirteen patients. Two patients had surface irregularities. All the fifteen patients tolerated the procedure well. There was definite improvement in all the scars with immediate elevation. Patient's satisfaction was analysed using visual analogue scale which showed an average value of 8.4 [Table 1]. Linear scars showed excellent improvement [Figure 4]. Acne, varicella and traumatic scars improved significantly [Figures 5–8]. Scar due to pilonidal sinus showed moderate improvement due to skin tethering [Figure 9]. However, two patients did not appreciate any difference in the scar due to altered skin texture over the scars though there was elevation of the scar. They were further subjected to Q-switched Nd-YAG laser therapy to improve surface irregularities. Transient oedema and bruise were noted in two patients. Tip necrosis [Figure 11] which healed with hyperpigmentation was observed in one patient [Figure 10]. Donor areas also healed uneventfully in all patients.
Table 1.
Patient satisfaction on visual analogue scale
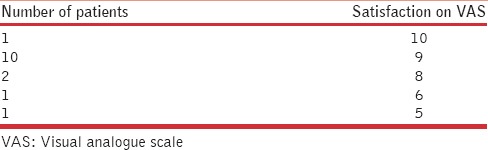
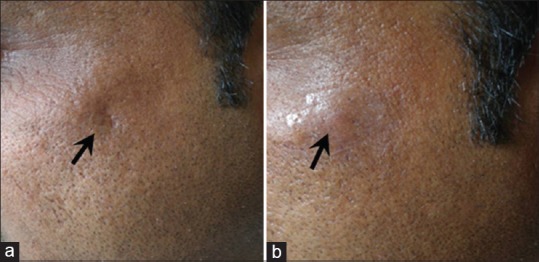
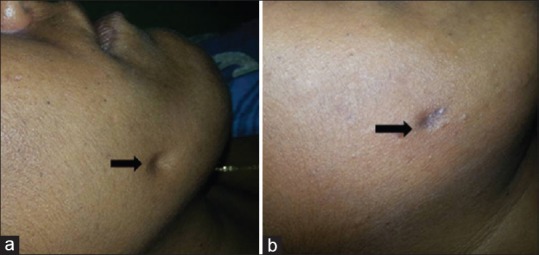
Figure 4.

Linear scar due to branding on the forehead (a) after dermal grafting with hyperpigmentation at entry points (b)
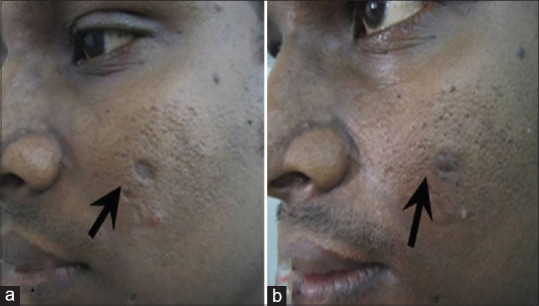
Figure 5.
Traumatic scar on left upper cheek (a) and after (b) dermal grafting
Figure 8.
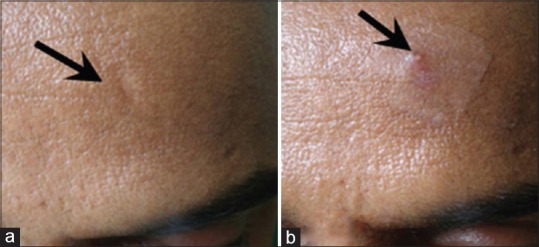
Traumatic scar on the forehead (a) and after (b) dermal grafting
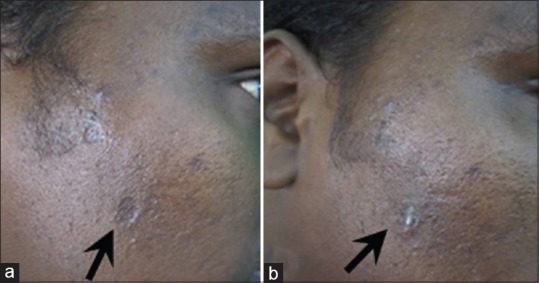
Figure 9.
Healed odontogenic sinus scar on the right cheek (a) with partial improvement with dermal grafting (b)
Figure 11.

Tip necrosis seen on the right after dermal grafting in a linear scar
Figure 10.
Atrophic acne scar on left cheek (a) after dermal grafting (b)
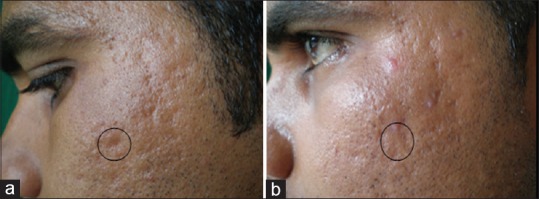
Figure 6.
(a and b) Varicella scar on the left cheek
Figure 7.
(a and b) Varicella scar in the right cheek
DISCUSSION
An effective, permanent therapy of broad, depressed scar has posed a real challenge for surgeons treating atrophic scars of the face. An ideal technique which is free of allergic reaction or irritation, economical, less time-consuming and easily available and which gives a permanent correction with no rejection or resorption, is still very far from reality. Dermal grafts have been in use for many years. In the past, surgeons have focussed on their use in ophthalmology and correction of defects in other organ systems. Previous problems encountered with these grafts include persistence of the epithelium, cyst formation and unpredictable behaviour. However, with improved surgical technique, complications with dermal grafts have reduced. In our study, removal of epidermis by dermabrasion has prevented the formation of epidermal cyst as seen in earlier studies. Fournier has utilised solid bits of dermis and fat, for implantations into facial rhytides.[3] Dermal grafting is the implantation of appropriately dissected deep dermis into corresponding recipient areas such as atrophic scars or other soft tissue defects.[4] Selection of patient is very important for this procedure. Any acne scar which is prominent and soft, at least 4–5 mm across, can be considered for dermal grafting.[3] At the same time, patients should also be counselled for the need for other procedures such as dermabrasion, peels or LASER if they have irregular or pigmented surface. As the results may not be evident in scars with surface irregularities as in two of our case, choosing patients with normal skin texture is important while selecting the patient for dermal graft. The subcision releases fibrous anchoring of dermis and also produces trauma at microscopic level within scar tissues. Newer matrix and collagen tissue are laid down[5] and establish a well-vascularised bed of granulation tissue to accept the grafts once they are inserted one and half to 2 weeks after the undermining.[3] Therefore, all the patients were advised to undergo a procedure of undermining or subcision 2 weeks before dermal graft insertion. A commonly selected and convenient donor site is the crease behind one or both ears in an area devoid of appendages.[3] Depending on the scar shape and size, grafts are obtained and implanted as explained above. Two different techniques can be used to harvest the dermal grafts. One is conventional technique and the other is enzymatic technique. In conventional technique, the donor tissue is harvested using any conventional dermatomes or using biopsy punches from the post-auricular site. Epidermal part is trimmed using a fine scissors. Alternatively, dermal tissue can also be harvested from a dermabraded area where the whole of epidermis is completely removed. Excess of fat tissue is trimmed off. The punch grafts or narrow strip of dermis is transferred to saline and then inserted into the recipient area. In enzymatic technique, similarly obtained dermal tissue is transferred into a Petri dish containing 0.25% of trypsin in ethylenediaminetetraacetic acid solution. This is incubated at 37C for 75 min. After which, the tissue is transferred to phosphate-buffered saline. This technique makes dermal graft soft, flexible and easily mouldable as compared to grafts obtained via conventional technique.[6] After preparing the graft, they can be inserted either by pocket grafting technique or railroad technique.
Advantages of dermal grafts are it is readily available, there are no allergic or hypersensitivity reactions, its inexpensive, not susceptible to infections, can be accurately tailored for different types of atrophic scars and acts as a permanent spacer between the skin and underlying fibrous band of tissue.[6]
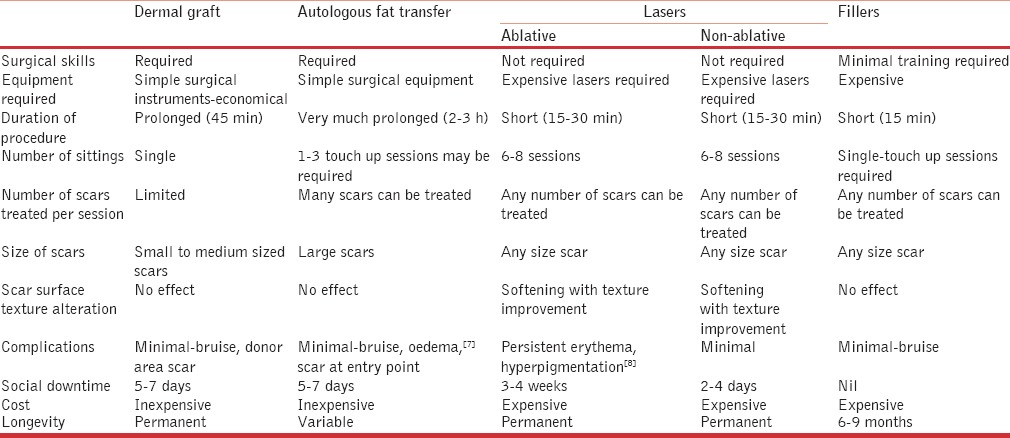
However, the drawbacks of dermal graft is that it may not be an ideal solution for large depressed scars where multiple sittings may be required and in scars with significant skin texture alteration where it may have to be combined with resurfacing techniques. The advantages and disadvantages of dermal graft in comparison with other modalities such as LASERs, fillers and autologous fat transfer have been tabulated in Table 2. Limitations of the study include small sample size, and subjective assessment of the scar to assess the outcome.
Table 2.
Advantages and disadvantages of dermal graft in comparison with other techniques
CONCLUSION
To conclude dermal graft can serve as natural, permanent and inexpensive filler in the management of facial scars such as acne scars, varicella scars and linear scars of varied aetiology. However, large-scale studies are required to confirm the same.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lee KK, Gorman AK, Swanson NA. In: Scar revision. Surgery of the Skin-Procedural Dermatology. 1st ed. Robinson JK, Hanke CW, Sengelmann RD, Siegel DM, editors. Philadelphia: Mosby; 2005. pp. 1–10. [Google Scholar]
- 2.Nirmal B, Somiah S, Sacchidanand SA. Railroading technique of dermal grafting for linear atrophic scarring. J Cutan Aesthet Surg. 2014;7:224–6. doi: 10.4103/0974-2077.150781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swinehart JM. Pocket grafting with dermal graft: Autologous collagen implants for permanent correction of cutaneous depressions. Am J Cosmet Surg. 1995;12:321–31. [Google Scholar]
- 4.Swinehart JM. In: Dermal grafting. Tissue Augmentation in Clinical Practice. 2nd ed. Klein AW, editor. New York: Taylor and Francis Group; 2006. pp. 21–54. [Google Scholar]
- 5.Vaishnani JB. Subcision in rolling acne scars subcision with 24G needle. Indian J Dermatol Venereol Leprol. 2008;74:677–9. doi: 10.4103/0378-6323.45133. [DOI] [PubMed] [Google Scholar]
- 6.Salim T, Ghiya R. In: Surgical management of acne scars. ACS (I) Textbook on Cutaneous and Aesthetic Surgery. 1st ed. Venkataram M, editor. New Delhi: Jaypee Brothers Medical Publications; 2012. pp. 393–406. [Google Scholar]
- 7.Piombino P, Marenzi G, Dell’Aversana Orabona G, Califano L, Sammartino G. Autologous fat grafting in facial volumetric restoration. J Craniofac Surg. 2015;26:756–9. doi: 10.1097/SCS.0000000000001663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harithy RA, Pon K. Scar treatment with lasers: A review and update. Curr Dermatol Rep. 2012;1:69–75. [Google Scholar]


