Dear Editor,
Extraoral skin fistula with odontogenic source should be considered in differential diagnosis of cervicofacial fistula. Occasionally, these fistulas have been treated with the false diagnosis of acne, folliculitis, and basal cell carcinoma.[1,2,3]
The dominant opinion is that after correct diagnosis and resolution of the odontogenic source of infection, the extraoral fistula will disappear spontaneously without the need for any surgical intervention.[4] This concept is almost always true; however, in our practice, we have confronted with two cases that need to local skin flaps for solving the problem of depressed scar on the face several months after resolution of odontogenic source of infection.
The first patient was 26-year-old male with depressed scar on the right cheek. The responsible tooth was maxillary right first permanent molar that had been treated endodontically a year ago. In obtained periapical radiography, there was not any problem with treatment, but a fibrotic band was palpable in the vestibule. An unsightly depressed scar was remained on the cheek. Squeezing this scar expressed any secretion. The scar was excised and the fibrotic band was removed through intraoral incision. The skin defect was reconstructed by O to Z flap [Figure 1].
Figure 1.

(a) Depressed scar after resolution of odontogenic source of infection, (b) depression aggravates with mouth opening, (c) Z-shaped linear scar after O to Z flap, (d) result 3 months after operation
Another patient was 17-year-old boy with depressed scar in submandibular region near the anterior border of sternocleidomastoid muscle. He had been admitted to the hospital with a large fluctuant submandibular abscess 8 months ago. Extraoral incision and drainage and removal of the left mandibular wisdom tooth were done under local anesthesia. He was referred to solve the problem of unsightly depressed scar in the upper neck previous surgical incision.
The infection had been resolved completely, but a depressed scar with atrophied skin in the center was flaunted. Under local anesthesia, the scar was excised, the skin was undermined below the platysma muscle, and the defect was closed by O to Z flap [Figure 2].
Figure 2.
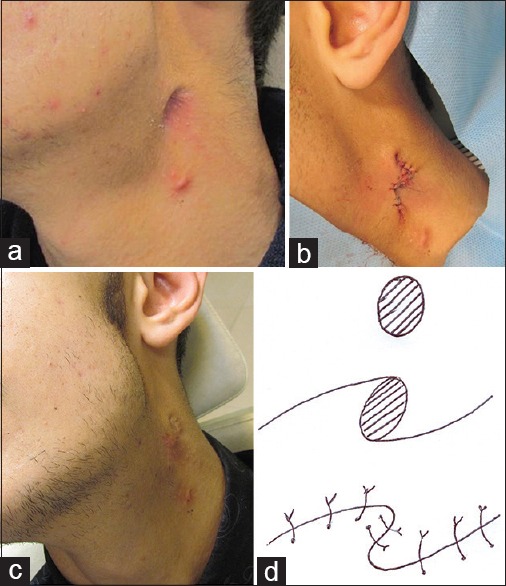
(a) Depressed scar in submandibular region, (b) O to Z flap is used to manage this problem, (c) 3-month follow-up photograph, (d) schematic picture of O to Z flap
Extraoral skin fistula from odontogenic infections often heal satisfactorily, after eliminating the odontogenic source of infection through root canal therapy of severely decayed tooth, extraction of hopeless teeth, or enucleation of the infected cyst.
However, in long-standing lesions, fibrosis surrounds sinus tract and prohibits healing even after eliminating odontogenic source of infection.
Slightly depressed scar can be managed with subcision but severe forms need surgical intervention.[5] O to Z flap is a good option in if the shape of defect is oval or circular.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Herd MK, Aldridge T, Colbert SD, Brennan PA. Odontogenic skin sinus: A commonly overlooked skin presentation. J Plast Reconstr Aesthet Surg. 2012;65:1729–30. doi: 10.1016/j.bjps.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Peermohamed S, Barber D, Kurwa H. Diagnostic challenges of cutaneous draining sinus tracts of odontogenic origin: A case report. Dermatol Surg. 2011;37:1525–7. doi: 10.1111/j.1524-4725.2011.02107.x. [DOI] [PubMed] [Google Scholar]
- 3.Gupta SK, Saxena P. Cutaneous manifestation of odontogenic infection misdiagnosed as having dermatologic etiology: A report of two cases. Quintessence Int. 2011;42:455–8. [PubMed] [Google Scholar]
- 4.Kumar U, Dharmani CK, George BJ, Abraham S. Conservative management of persistent facial cutaneous sinus tract with a dental origin. BMJ Case Rep 2014. 2014:pii: Bcr2014204347. doi: 10.1136/bcr-2014-204347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahpeyma A, Khajehahmadi S. Needle subcision: A conservative treatment for facial dimpling after elimination of odontogenic infection source: A technical note. Oral Maxillofac Surg. 2014;18:415–8. doi: 10.1007/s10006-013-0429-y. [DOI] [PubMed] [Google Scholar]


