Abstract
Background
Effective postoperative pain control for thoracic surgery is very important, not only because it reduces pulmonary complications but also because it accelerates the pace of recovery. Moreover, it increases patients’ satisfaction with the surgery. In this study, we present a simple approach involving the safe placement of intercostal catheter (ICC) after single port video-assisted thoracoscopic surgery (VATS) anatomic resection and we evaluate postoperative analgesic function with and without it.
Methods
We identified patients who underwent single port anatomic resection with ICC placed intraoperatively as a route for continuous postoperative levobupivacaine (0.5%) administration and retrospectively compared them with a group of single port anatomic resection patients without ICC. The operation time, postoperative day 0, 1, 2, 3 and discharge day pain score, triflow numbers, narcotic requirements, drainage duration and post-operative hospital stay were compared.
Results
In total, 78 patients were enrolled in the final analysis (39 patients with ICC and 39 without). We found patients with ICC had less pain sensation numerical rating scale (NRS) on postoperative day 0, 1 (P=0.023, <0.001) and better triflow performance on postoperative day 1 and 2 (P=0.015, 0.032). In addition, lower IV form morphine usage frequency and dosage (P=0.009, 0.017), shorter chest tube drainage duration (P=0.001) and postoperative stay (P=0.005) were observed in the ICC group.
Conclusions
Continuous intercostal nerve blockade by placing an ICC intraoperatively provides effective analgesia for patients undergoing single port VATS anatomic resection. This may be considered a viable alternative for postoperative pain management.
Keywords: Single port VATS, anatomic resection, intercostal nerve block
Introduction
For acute stage postoperative pain control, various modalities including oral analgesic agents, intramuscular morphine injection, intercostal nerve blockade, and epidural analgesia have been used in thoracotomy and video-assisted thoracoscopic surgery (VATS) patients (1-3). Effective pain control can reduce not only postoperative pulmonary complications but also patients’ fear of surgery. However, high potency opioid drugs may bring about gastrointestinal dysfunction while epidural analgesia might carry considerable risks of epidural hematoma, dural perforation, urinary retention and increase the risk of adverse cardiovascular outcomes in high risk patients (4). The complications mentioned above, though rare, prompt us to improve currently existing postoperative analgesia. With the improvement of endoscopic surgical instruments and skills, comparable therapeutic results have been achieved in selected patients with a smaller incision wound (5-8). Single port thoracoscopic surgery has been reported since 2004 (9), and, although it is still controversial with regard to postoperative pain outcome when compared with conventional VATS (10), it does allow for a smaller intercostal incision wound and nerve injury area. Intercostal nerve block has been proven useful in thoracotomy and VATS patients (11-12). We hypothesized that a targeted local analgesic technique aimed at the location of pain generation could eliminate postoperative pain, and that continuous single intercostal nerve block might be effective in single port VATS patients. In this study, we present a simple approach involving the placement of an intercostal catheter (ICC) in the sub pleural space during single port VATS anatomic resection to determine its utility in post operation pain control.
Methods
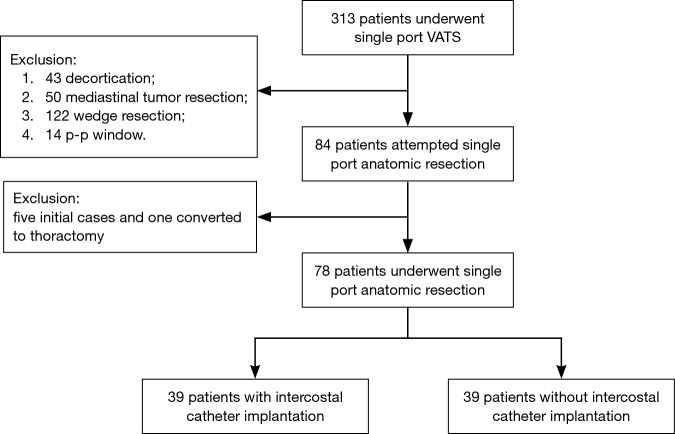
The study was approved by the institutional review board of Chang Gung Memorial Hospital (IRB No. 104-1204 B). Preoperative examinations included blood routine, pulmonary function test, bronchoscope, chest radiography, chest computed tomography, positron emission tomography, and brain computed tomography or brain magnetic resonance. A retrospective database of all patients who received single port VATS between March 2014 and January 2016 was used to identify patients who underwent single port VATS anatomic resections. Starting from May 2015, we began to place an ICC intraoperatively as a route for postoperative levobupivacaine (0.5%) administration. Exclusion criteria for single port VATS with ICC insertion included (I) empyema; (II) patients’ pleural surface having tumor seeding; (III) patients having allergy history to amide-type local anesthetic. Originally, 84 patients were slated to receive single port VATS anatomic resection during this period, however, one case converted to thoracotomy due to catastrophic intraoperative bleeding, while initial five cases had to be excluded due to the learning curve effect. In total, seventy-eight cases were enrolled in the final analysis. Thirty-nine patients received single port VATS anatomic resections without ICC insertion, while the remaining thirty-nine patients received single port VATS anatomic resections with ICC insertion in the period since May 2015 (Figure 1). Age, gender, body mass index, operation time, blood loss, postoperative complications, average daily numerical rating scale (NRS), incentive spirometry numbers (triflow ball numbers), and pathological report were collected from the hospital information system. Surgical mortality was defined as death occurring during the same hospitalization or within 30 days after the operation.
Figure 1.
Flowchart of the study enrollment. VATS, video-assisted thoracoscopic surgery.
Surgical techniques of single port video assisted thoracoscopic anatomic resections
A single operation surgeon (Ching Feng Wu) and two fixed assistants (Ming Ju Hsieh, Ching Yang Wu) completed the whole single port VATS anatomic resections. After intravenous induction, double lumen endotracheal tube was intubated to accomplish one lung ventilation with patients was placed in the lateral decubitus position. In single port VATS anatomic resections, a 3–4 cm incision was created in the fourth or fifth intercostal space at the anterior axillary line. For upper lobe lesions, the incisions were created at the fourth intercostal space. For middle or lower lobe lesions, the incisions were made at the fifth intercostal space. Then a plastic wound protector (Alexis®, USA) was applied in the wound without rib-spreading. A 30-degree 10 mm thoracoscope was placed at the top of the incision wound. The endoscope instruments (Scanlan®, USA) and curved electric hook were used for tissue dissection using techniques learned from Gonzalez-Rivas D. The vein, artery and bronchus were divided separately by using endoscopic staplers (Covidien, USA, or Ethicon, USA). The division order varied case by case. For upper lobe lesions, the artery was divided first, then the bronchus, and finally the vein. In cases of middle or lower lobe lesions, the dissection order was vein, artery and then bronchus. The specimen was retrieved with a plastic bag through the incision wound. After removal of the specimen, systemic lymph dissection was performed. At the end of the operation, one Fr 20 chest tube was inserted and not removed until there was no air leakage and the drainage amount was below 200 mL per day.
Analgesia techniques
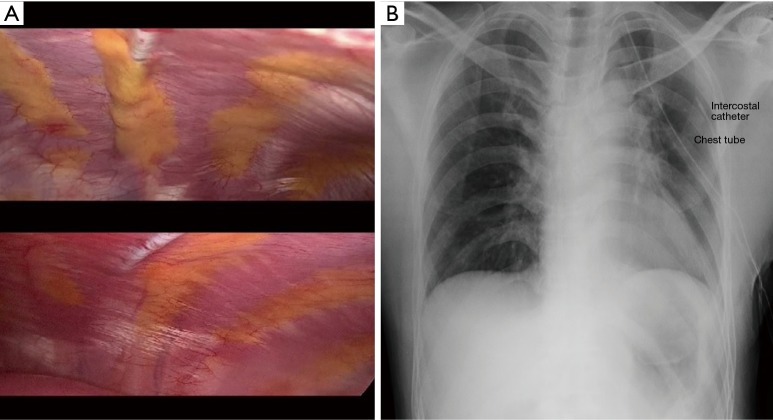
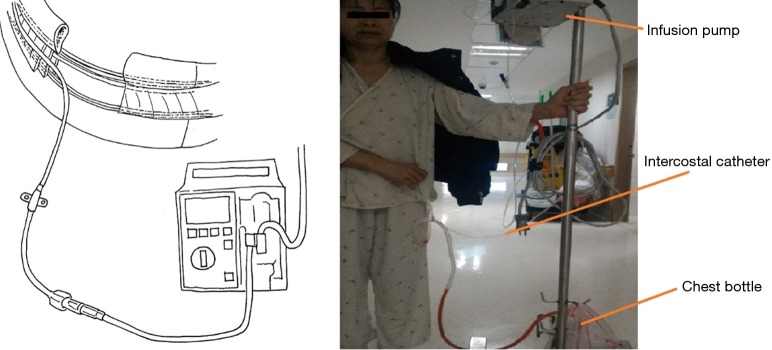
Before the Fr 20 chest tube was placed in the chest cavity, a dilating catheter (8 Fr Angiotech) was used to dissect the wound associated sub pleural space, and then a guidewire was passed through the dilating catheter. After we removed the dilating catheter, a 7 F, 20-cm-length radio-opaque polyurethane catheter with side holes was passed over the guidewire and fixed at 15 cm (Figure 2). Finally, 10 mL levobupivacaine (0.5%) was injected through the catheter into the sub pleural space (Figure 3). All procedures were done under endoscope. When the patients were returned to the ordinary ward or intensive care unit, the ICC was connected to an infusion pump with levobupivacaine (0.5%) 2.5 mL/hour (Figure 4), a dosage suggested by the anesthesiologist (Hung Pin Liu); this dose is about one third of the maximum dose. The duration of ICC depends on patients. We removed ICC and chest tube at the same time when the chest tube drainage was smaller than 200 mL/day.
Figure 2.
ICC was placed in the sub-pleural space, which was the same intercostal space of wound. ICC, intercostal catheter.
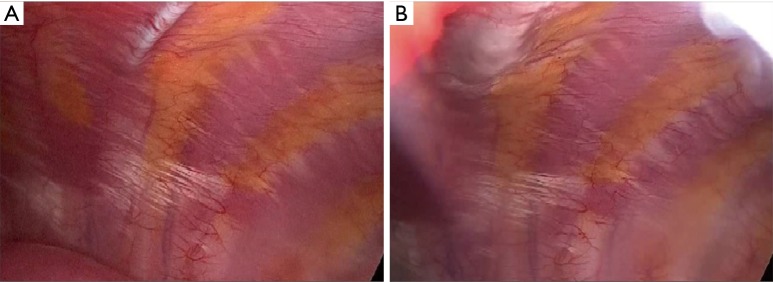
Figure 3.
Injection levobupivacaine before and after ICC was inserted through subpleural space. (A) Before and (B) after 10 mL levobupivacaine (0.5%) was injected through the catheter into the sub-pleural space. ICC, intercostal catheter.
Figure 4.
With the help of continuous intercostal nerve block, patients could easily ambulate in the ward on postoperative day 1.
For patients without ICC insertion, 10 mL levobupivacaine (0.5%) was injected into the intercostal space at the end of the operation. All analyzed patients took Ultracet® Q6H (Tramadol 37.5 mg + acetaminophen 325 mg, Johnson, USA) as postoperative oral anodyne. IV form morphine (0.1 mg/kg) was given on request if patients’ NRS was >3 at rest or NRS >5 during activity.
NRS and triflow numbers
Triflow numbers of all patients were recorded by the same observer (Ching Feng Wu) before operation and on postoperative day 1, 2, 3 and discharge day. At the same time Dr. Wu also educated patients on how to use triflow correctly. Pain assessments were made regularly by nursing staff at least once on each shift (3 times/24 hrs) and on physician rounds (Ching Feng Wu). A chart card containing a 10-cm horizontal line with word anchors at each end, ranging from 0= “no pain” to 10= “worst pain” was used to query patients about the degree of pain they had on postoperative day 0, 1, 2, 3 and discharge day. Finally, we took nursing records and physician‘s records to express the average daily NRS.
Analysis
Continuous data are expressed as mean value with a range of one standard deviation (SD). Before comparison, two groups’ continuous variables were examined by Levene test. If the variances were not equal, we used the Brown-Forsythe test to detect any significant difference between the two groups. If the variances were equal, one way ANOVA was used to examine the variables. All data analysis was done by SPSS version 19 (IBM, USA). A P value <0.05 was considered statistically significant.
Results
Between March 2014 and January 2016, a total of 84 patients were scheduled to receive single port VATS anatomic resections. After exclusion of the initial five cases and one who converted to thoracotomy, seventy eight patients (39 patients with continuous intercostal nerve block and 39 patients without continuous intercostal nerve block) were enrolled in the final analysis. The clinical features of the seventy eight patients are listed in Table 1. The average wound length, operation time and blood loss were similar in both ICC and no ICC group (P=0.139, 0.104, 0.299 respectively). The comparison of perioperative results is shown in Table 2.
Table 1. Clinical features of analyzed patients.
| Clinical features | ICC (n=39) | No ICC (n=39) | P value | Total (n=78) |
|---|---|---|---|---|
| Age | 60.87±12.33 | 60.21±10.38 | 0.797 | 60.54±11.32 |
| Gender | 0.645 | |||
| Male | 24 | 22 | 46 (59.0) | |
| Female | 15 | 17 | 32 (41.0) | |
| Body mass index | 23.86±2.12 | 23.91±3.15 | 0.932 | 23.89±2.67 |
| FEV1 | 2.17±0.64 | 2.26±0.60 | 0.561 | 2.21±0.62 |
| Smoking history | 1.000 | |||
| Yes | 13 | 13 | 26 (33.3) | |
| No | 26 | 26 | 52 (66.7) | |
| APM history* | 0.467 | |||
| Yes | 14 | 11 | 25 (32.1) | |
| No | 25 | 28 | 53 (67.9) | |
| Tumor location | – | |||
| Right upper lobe | 10 | 10 | 20 (25.6) | |
| Right middle lobe | 5 | 4 | 9 (11.5) | |
| Right lower lobe | 7 | 13 | 20 (25.6) | |
| Left upper lobe | 8 | 8 | 16 (20.5) | |
| Left lower lobe | 8 | 5 | 13 (16.7) | |
| Histology | – | |||
| AD | 23 | 23 | 46 (59.0) | |
| SC | 2 | 3 | 5 (6.4) | |
| Other* | 14 | 13 | 27 (34.6) | |
| Tumor size (cm) | 2.39±1.24 | 2.43±1.52 | 0.883 | 2.41±1.38 |
| Fissure | 0.495 | |||
| Development | 16 | 19 | 35 (44.9) | |
| No development | 23 | 20 | 43 (55.1) |
Continuous data are expressed as mean ± SD (interquartile range). *, including metastatic malignancy, Centro located benign lesions. FEV1, forced expiratory volume in the first second; APM, additional primary malignancy; SC, squamous cell cancer; AD, adenocarcinoma; ICC, intercostal catheter; SD, standard deviation.
Table 2. Comparison of perioperative outcomes and postoperative pain evaluation.
| Perioperative and postoperative parameters | ICC (n=39) | No ICC (n=39) | P value | Total (n=78) |
|---|---|---|---|---|
| Operation time | 167.64±48.50 | 185.53±47.43 | 0.104 | 176.58±48.50 |
| Wound size (cm) | 3.29±0.54 | 3.47±0.51 | 0.139 | 3.38±0.53 |
| Operation method | ||||
| Segmentectomy | 14 | 10 | 24 (30.8) | |
| Lobectomy | 23 | 27 | 50 (64.1) | |
| Bilobectomy | 2 | 2 | 4 (5.1) | |
| Blood loss (mL) | 68.33±110.06 | 48.97±35.59 | 0.299 | 58.65±81.84 |
| Numbers of N1 lymph node | 8.09±5.29 | 7.42±4.80 | 0.594 | 7.75±5.02 |
| Numbers of N2 lymph node | 13.28±6.76 | 13.37±9.37 | 0.964 | 13.32±8.11 |
| NRS | ||||
| Day 0 | 2.94±1.77 | 3.84±1.64 | 0.023 | 3.39±1.76 |
| Day 1 | 1.53±1.14 | 2.89±1.90 | <0.001 | 2.21±1.70 |
| Day 2 | 1.30±1.02 | 1.46±0.88 | 0.481 | 1.38±0.95 |
| Day 3 | 0.63±0.78 | 0.73±0.92 | 0.594 | 0.68±0.85 |
| Discharge day | 0.35±0.58 | 0.43±0.71 | 0.531 | 0.38±0.65 |
| Triflow numbers | ||||
| Pre operation | 2.71±0.45 | 2.89±1.90 | 0.175 | 2.78±0.41 |
| Day 1 | 2.30±0.65 | 1.89±0.78 | 0.015 | 2.10±0.74 |
| Day 2 | 2.58±0.49 | 2.28±0.72 | 0.032 | 2.43±0.63 |
| Day 3 | 2.66±0.47 | 2.64±0.48 | 0.815 | 2.65±0.47 |
| Discharge day | 2.71±0.46 | 2.69±0.46 | 0.864 | 2.69±0.46 |
| IV form morphine usage frequency (times) | 0.43±0.55 | 0.97±1.13 | 0.009 | 0.70±0.92 |
| IV form morphine dose (mg) | 2.61±3.55 | 5.48±6.39 | 0.017 | 4.05±5.33 |
| Chest tube drainage duration | 3.20±1.80 | 5.02±2.86 | 0.001 | 4.11±2.55 |
| Postoperative hospital stay | 4.23±1.93 | 6.30±4.04 | 0.005 | 5.26±3.31 |
Continuous data are expressed as mean ± SD (interquartile range). ICC, intercostal catheter; NRS, numerical rating scale; SD, standard deviation.
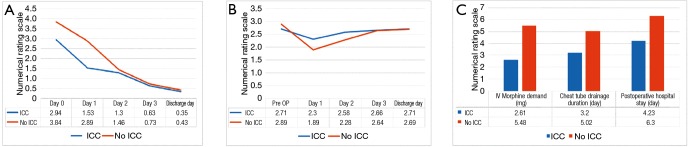
We further analyzed postoperative day 0, 1, 2, 3, and discharge day NRS and postoperative day 1, day 2, day 3, and discharge day triflow numbers, chest tube drainage duration, and postoperative hospital stay. We found patients with ICC had less pain sensation (NRS) on postoperative day 0, 1 (P=0.023, <0.001) and similar pain sensation on postoperative day 2, 3, and discharge day (P=0.481, 0.594, 0.531, Figure 5A). In addition, patients with ICC had better triflow performance on postoperative day 1 and 2 (P=0.015, 0.032) and similar triflow performance on postoperative day 3 and discharge day (P=0.815, 0.864, Figure 5B). IV form morphine use frequency and dose were lower in the ICC group (P=0.009, 0.017, Figure 5C). The average chest tube drainage duration and postoperative hospital stay was 3.20±1.80 and 4.23±1.93 days in the ICC group and 5.02±2.86 and 6.30±4.04 days in the non-ICC group (P=0.001, 0.005, Figure 5C). No mortality was recorded in either group. However, a total of six patients suffered from complications (three each in the ICC and non-ICC group), including five with prolonged air leakage and one with postoperative lymph node dissection area oozing.
Figure 5.
Patients with ICC had less pain, less postoperative analgesia drug demand, better triflow performance, shorter drainage duration and hospitalization compared with patients without ICC. (A) Pain score for patients who received continuous intercostal nerve block (ICC) or single shot intercostal nerve analgesia (No ICC) on postoperative day 0, 1, 2, 3, discharge day (P=0.023, 0.001, 0.481, 0.594, 0.531); (B) triflow rehabilitation performance for patients who received continuous intercostal block or single shot intercostal nerve analgesia (no ICC) on pre op, day 1, 2, 3, discharge day (P=0.175, 0.015, 0.032, 0.815, 0.864); (C) postoperative IV form morphine demand, chest tube drainage duration, hospital stay on ICC and no ICC group (P=0.017, 0.001, 0.005). ICC, intercostal catheter.
Discussion
Continuous regional nerve block has proven useful in total knee arthroplasty (13), hernia repair (14), living liver donors (15), multiport VATS (16), uniport VATS non anatomatic resection (17), and so on. In this retrospective study, we try to evaluate the benefit of continuous intercostal nerve block in single port VATS anatomic resection patients. We found patients with ICC had less pain sensation on postoperative day 0 and 1, better postoperative day 1 and 2 triflow rehabilitation, lower IV form morphine usage frequency and dose, shorter chest drainage duration and postoperative hospital stay. Better triflow performance, shorter chest drainage duration and hospitalization might result from less postoperative pain sensation in patients with ICC. Consequently, patients with ICC had more willing and no fear to do triflow rehabilitation and had better mobility. Under such circumstances, patients with ICC were easier to meet the criteria of removal drainage and discharged from hospital early. These preliminary results inspire us to pursue more delicate and individualized postoperative pain management for each patient. Various kinds of postoperative analgesia have been tried by surgeons and anesthesiologists; each with its pros and cons. When a new procedure is adopted, safety cannot be overemphasized. In our experience, no analgesia related complications, such as vomiting, dizziness, seizure, or chest wall hematoma occurred in our patients
In 2004, Rocco G first published their experience of single port VATS wedge resection (7). Since then, a series of articles have discussed its safety and feasibility in relatively simple procedures. Subsequently, Gonzalez-Rivas et al. expanded the applications of single port VATS to lobectomy (18), segmentectomy (19), pneumonectomy (20), and sleeve lobectomy (21). Recently, single port VATS has become more widely accepted with surgical indications similar to conventional VATS. However, regardless of its growing acceptance and applications, the benefit of single port VATS has remained controversial with regard to postoperative pain outcome (10) and long term oncological result. However, it does seem that single port VATS is a good candidate for continuous intercostal nerve block having been found to cause less intercostal nerve injury in our study. Since over 90% of patients have needed a hospital stay of more than one day, single shot intercostal nerve analgesia levobupivacaine (0.5%) has been insufficient for postoperative pain control. Epidural analgesia carries the risk of rare but undesirable complications, while liposomal bupivacaine is not easily accessible everywhere (22). Intraoperatively placing an ICC through the sub-pleural space is a feasible and easily practiced procedure for postoperative pain control. But, how long to continue giving intercostal analgesia is an interesting issue worth studying in depth. Our study might just provide a hint. It seems that the benefit of the continual intercostal nerve block dissipated after postoperative day 2. To remove the ICC or to stop levobupivacaine (0.5%) administration on postoperative day 3 might be a reasonable choice. Due to the limitation of this study, we dare not to jump to conclusion. A further prospective study is warranted
Initially, five cases were excluded from this study due to learning curve effects since every procedure needs a certain number of cases to reach relatively stable performance (23,24). In our surgical team, the operator and two assistants are all experienced surgeons who have done more than one hundred cases of conventional VATS anatomic resection. Given the dedication of this surgical team, only one case was converted to thoracotomy due to left truncus anterior artery bleeding. With accumulated single port VATS experience, we were able to handle accidental pulmonary artery injury without conversion (Figure 6). Even we could complete the minimal invasive thoracic surgery safely, however, still a few patients were suffering from postoperative pain so that they dared not to do rehabilitation or ambulation after single port VATS in our clinical observation. This clinical observation also evoked the idea that we want to improve the improve patients’ pain experience after surgery. From the viewpoint of preliminary result, management of acute postoperative pain with continuous intercostal nerve block after single port VATS is a feasible and effective method
Figure 6.

Bleeding control of segmental artery (A6) by single port surgery (25). Available online: http://www.asvide.com/articles/1304
The retrospective design and relatively small case numbers are the main limitations of this study. However, the use of a single operator with standardized operation method, the single data collector, and the postoperative oral and IV form analgesia regimen could all strengthen the validity of this study. Additionally, we also averaged physician’s records and nursing records to express the reality of pain perception in each patient. Although our assessments of analgesia on NRS were not collected on prospective protocol, we used the same collecting method between both groups. It was unlikely to have statistical bias in favor of one group over another. In addition, all involved nursing staff was trained in a standardized way to inquire about patients’ pain with the timing of pain assessment standardized for all patients. The NRS were not measured dynamically or statically. For pain evaluation, a prospective protocol was more convincing and objective. Nevertheless, we still attempt to present a rigorous, quantitative evaluation of postoperative pain and rehabilitation in an observational cohort, which could serve as the basis for further prospective, randomized study.
Conclusions
Continuous intercostal nerve block in single port VATS anatomic resection patients is both safe and feasible. By placing an ICC through the sub-pleural space in single port VATS patients we were able to lower postoperative pain, improve postoperative rehabilitation, shorten chest tube drainage duration and hospital stay in our preliminary report. This might serve as a suitable alternative choice in postoperative pain management.
Acknowledgements
None.
Ethical Statement: The study was approved by Chang Gung Memorial Hospital (IRB No. 104-1204 B) and written informed consent was obtained from all patients.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.de Leon-Casasola OA, Parker B, Lema MJ, et al. Postoperative epidural bupivacaine-morphine therapy. Experience with 4,227 surgical cancer patients. Anesthesiology 1994;81:368-75. 10.1097/00000542-199408000-00015 [DOI] [PubMed] [Google Scholar]
- 2.Liu S, Carpenter RL, Neal JM. Epidural anesthesia and analgesia. Their role in postoperative outcome. Anesthesiology 1995;82:1474-506. 10.1097/00000542-199506000-00019 [DOI] [PubMed] [Google Scholar]
- 3.American Society of Anesthesiologists Task Force on Acute Pain Management . Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248-73. 10.1097/ALN.0b013e31823c1030 [DOI] [PubMed] [Google Scholar]
- 4.Leslie K, Myles P, Devereaux P, et al. Neuraxial block, death and serious cardiovascular morbidity in the POISE trial. Br J Anaesth 2013;111:382-90. 10.1093/bja/aet120 [DOI] [PubMed] [Google Scholar]
- 5.Ghaly G, Kamel M, Nasar A, et al. Video-Assisted Thoracoscopic Surgery Is a Safe and Effective Alternative to Thoracotomy for Anatomical Segmentectomy in Patients With Clinical Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg 2016;101:465-72; discussion 472. 10.1016/j.athoracsur.2015.06.112 [DOI] [PubMed] [Google Scholar]
- 6.Kuritzky AM, Aswad BI, Jones RN, et al. Lobectomy by Video-Assisted Thoracic Surgery vs Muscle-Sparing Thoracotomy for Stage I Lung Cancer: A Critical Evaluation of Short- and Long-Term Outcomes. J Am Coll Surg 2015;220:1044-53. 10.1016/j.jamcollsurg.2014.12.049 [DOI] [PubMed] [Google Scholar]
- 7.Son BS, Kim DH, Lee SK, et al. Small Single-Incision Thoracoscopic Surgery Using an Anchoring Suture in Patients With Primary Spontaneous Pneumothorax: A Safe and Feasible Procedure. Ann Thorac Surg 2015;100:1224-9. 10.1016/j.athoracsur.2015.04.095 [DOI] [PubMed] [Google Scholar]
- 8.Wu CF, Gonzalez-Rivas D, Wen CT, et al. Comparative Short-Term Clinical Outcomes of Mediastinum Tumor Excision Performed by Conventional VATS and Single-Port VATS: Is It Worthwhile? Medicine (Baltimore) 2015;94:e1975. 10.1097/MD.0000000000001975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. 10.1016/S0003-4975(03)01219-0 [DOI] [PubMed] [Google Scholar]
- 10.Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. 10.1093/icvts/ivu391 [DOI] [PubMed] [Google Scholar]
- 11.Detterbeck FC. Efficacy of methods of intercostal nerve blockade for pain relief after thoracotomy. Ann Thorac Surg 2005;80:1550-9. 10.1016/j.athoracsur.2004.11.051 [DOI] [PubMed] [Google Scholar]
- 12.Wildgaard K, Petersen RH, Hansen HJ, et al. Multimodal analgesic treatment in video-assisted thoracic surgery lobectomy using an intraoperative intercostal catheter. Eur J Cardiothorac Surg 2012;41:1072-7. 10.1093/ejcts/ezr151 [DOI] [PubMed] [Google Scholar]
- 13.Chelly JE, Greger J, Gebhard R, et al. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty 2001;16:436-45. 10.1054/arth.2001.23622 [DOI] [PubMed] [Google Scholar]
- 14.Heil JW, Nakanote KA, Madison SJ, et al. Continuous transversus abdominis plane (TAP) blocks for postoperative pain control after hernia surgery: a randomized, triple-masked, placebo-controlled study. Pain Med 2014;15:1957-64. 10.1111/pme.12530 [DOI] [PubMed] [Google Scholar]
- 15.Maeda A, Shibata SC, Wada H, et al. The efficacy of continuous subcostal transversus abdominis plane block for analgesia after living liver donation: a retrospective study. J Anesth 2016;30:39-46. 10.1007/s00540-015-2085-x [DOI] [PubMed] [Google Scholar]
- 16.Milone L, Edmondson D, Lebenthal A, et al. Multiple nerve blocks after video-assisted thoracic surgery (VATS). Surg Endosc 2011;25:2731-2. 10.1007/s00464-011-1613-5 [DOI] [PubMed] [Google Scholar]
- 17.Wu CF, Hsieh MJ, Liu HP, et al. Management of post-operative pain by placement of an intraoperative intercostal catheter after single port video-assisted thoracoscopic surgery: a propensity-score matched study. J Thorac Dis 2016;8:1087-93. 10.21037/jtd.2016.04.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. 10.1510/icvts.2011.274746 [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. 10.1093/ejcts/ezs482 [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. 10.1007/s00464-011-2127-x [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [DOI] [PubMed] [Google Scholar]
- 22.Rice DC, Cata JP, Mena GE, et al. Posterior Intercostal Nerve Block With Liposomal Bupivacaine: An Alternative to Thoracic Epidural Analgesia. Ann Thorac Surg 2015;99:1953-60. 10.1016/j.athoracsur.2015.02.074 [DOI] [PubMed] [Google Scholar]
- 23.Huang CL, Liu CC, Cheng CY, et al. Learning thoracoscopic lobectomy in resident training. Thorac Cardiovasc Surg 2014;62:690-5. 10.1055/s-0033-1364203 [DOI] [PubMed] [Google Scholar]
- 24.Okyere S, Attia R, Toufektzian L, et al. Is the learning curve for video-assisted thoracoscopic lobectomy affected by prior experience in open lobectomy? Interact Cardiovasc Thorac Surg 2015;21:108-12. 10.1093/icvts/ivv090 [DOI] [PubMed] [Google Scholar]
- 25.Hsieh MJ, Wang KC, Wu CF, et al. Bleeding control of segmental artery (A6) by single port surgery. Asvide 2016;3:529. Available online: http://www.asvide.com/articles/1304