Abstract
The role of yogurt consumption in the risk of developing overweight, obesity, or metabolic syndrome has been the subject of epidemiologic studies over the last 10 y. A comprehensive literature search on MEDLINE and ISI Web of Knowledge from 1966 through June 2016 was conducted to examine the relation between yogurt consumption and weight gain, as well as the risk of overweight, obesity, or metabolic syndrome, in prospective cohort studies. Ten articles met all the inclusion criteria and were included in our systematic review. Of the 10 cohort studies, 3 analyzed the relation between yogurt consumption and the risk of overweight or obesity, 8 analyzed changes in waist circumference or weight changes, 3 studied the association with the risk of developing metabolic syndrome, and 1 studied the probability of abdominal obesity reversion. Although an inverse association between yogurt consumption and the risk of developing overweight or obesity was not fully consistent or always statistically significant, all studies but one showed in their point estimates inverse associations between yogurt consumption and changes in waist circumference, changes in weight, risk of overweight or obesity, and risk of metabolic syndrome during follow-up, although not all estimates were statistically significant (2 studies). Prospective cohort studies consistently suggested that yogurt consumption may contribute to a reduction in adiposity indexes and the risk of metabolic syndrome. Therefore, there is a need for more prospective studies and high-quality randomized clinical trials to confirm this apparent inverse association.
Keywords: functional foods, metabolic syndrome, obesity, probiotics, waist circumference
Introduction
According to the WHO, overweight and obesity is defined as an excessive or abnormal fat accumulation that may affect human health. The WHO estimates that being overweight or obese is the cause of ≥2.8 million deaths in adults every year (1). The term metabolic syndrome (MetS)10 has been used to describe a combination of metabolic disorders that, all together, increase the risk of cardiovascular diseases and type 2 diabetes (2). MetS includes the following metabolic disorders: hypertriglyceridemia (TGs ≥150 mg/dL or specific medication), low concentrations of HDL cholesterol (<40 mg/dL for men and <50 mg/dL for women, or specific medication), elevated blood pressure (systolic ≥130 mm Hg and/or diastolic ≥85 mm Hg or antihypertensive drug treatment in a patient with a history of hypertension), impaired glucose metabolism (fasting plasma glucose ≥100 mg/dL, specific medication, or previous diagnosis of type 2 diabetes), and central obesity (3). The prevalence of MetS is growing; this mainly is due to sedentary lifestyles, as well as the increasing prevalence of obesity. Therefore, the increasing prevalence of obesity and MetS are major, growing concerns that should be a priority for public health (4).
Yogurt is the result of milk fermentation by lactic acid with the use of thermophilic strains of bacteria. The nutrient content (macronutrients and micronutrients) of yogurt is very similar to milk, although the concentration of proteins (3.2 g/100 compared with 3.5 g/100 g), vitamins [riboflavin (vitamin B-2) and cyanocobalamin (vitamin B-12)], and minerals (calcium, magnesium, potassium, and zinc), are higher in yogurt than in milk (5). Recently, in a cross-sectional study, Wang et al. (6) reported that individuals who consumed yogurt had a better quality diet than those who did not consume yogurt; likewise, potassium intake was higher, and yogurt consumers were less likely to have an inadequate intake of vitamins (vitamins B-2 and B-12), and minerals (calcium, magnesium, and zinc).
Primarily in the last decade, the possible association between dairy (not only yogurt) consumption and body weight has been studied with inconclusive results. For example, a review that included 9 prospective cohort studies in adults conducted in 2010 concluded that more evidence was needed to support the claim that a high consumption of dairy products was associated with body weight (7). In addition, a recent systematic review that included randomized controlled trials (RCTs) and observational studies assessed the impact of all dairy products and yogurt consumption specifically on the risk factors for cardiovascular disease (8). This review concluded that some dairy products and yogurt consumption were associated with reduced risks of weight gain and obesity, as well as of cardiovascular disease. A systematic review of the role of dairy product consumption as a protective factor against the development of MetS was published recently (9). This review concluded that higher dairy consumption significantly reduced the risk of MetS, and that each additional increment of 1 dairy product serving/d conferred a 6% reduction (RR: 0.94; 95% CI: 0.89, 0.99) in the risk of developing MetS. Furthermore, 2 meta-analyses of RCTs that studied the effect of dairy consumption on weight and body composition found that, in short-term RCTs, dairy products, although not specifically yogurt consumption, may have shown some benefits for weight loss (10, 11). These 2 meta-analyses included 2 RCTs that assessed the association between yogurt consumption and weight loss. More recently, a meta-analysis assessed the association between dairy consumption and changes in anthropometric variables, and concluded that a higher intake of dairy products was not associated with increased body weight gain; moreover, yogurt was the only dairy food that showed some evidence of beneficial effects on weight, waist circumference, and risk of obesity (12). In this context, to our knowledge, there are only a few epidemiologic studies that have specifically assessed the role of yogurt consumption on changes in adiposity or the risk of developing overweight and obesity or MetS. The relation between the role of yogurt consumption, adiposity changes, and the risk of developing overweight and obesity or MetS needs more comprehensive examination.
In order to clarify these associations, we conducted a systematic review to summarize the existing evidence of the available prospective studies. This review analyzed the relation between yogurt consumption and changes in weight or waist circumference and the risk of becoming overweight or obese or developing MetS in published reports of prospective cohort studies.
Methods
The present systematic review was conducted with the standard methods proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (13). We initially screened published studies that assessed the relation between yogurt consumption and weight or waist gain, as well as the risk of overweight or obesity or the risk of MetS. A systematic search was conducted in 2 databases: PubMed (http://www.ncbi.nlm.nih.gov/pubmed); and Web of Science (http://webofknowledge.com). All the studies that were published between 1966 and June 2016 were included initially. The search terms that were used as search strategy included the following: “yogurt” or “yoghurt” or “dairy” or “yogurt consumption” or “yoghurt consumption” or “dairy consumption” hedged with “weight gain,” “weight change,” “waist circumference,” “waist change,” “waist gain,” “overweight,” “obesity,” or “metabolic syndrome.” For details on the search strategy, see Online Supporting Material. The inclusion criteria included the following: 1) publication language in English or Spanish; 2) only human studies; 3) only prospective studies; 4) yogurt consumption was the exposure of interest; 4) the outcome was weight or waist gain, weight or waist change, risk of overweight, obesity, or MetS; and 5) the authors reported results from an original peer-reviewed study (i.e., not reviews, editorial comments, letters, or meeting abstracts). Additional articles were identified from the reference list of included studies or relevant reviews.
Two investigators (CS-O and MB-R) screened the titles and abstracts of the potentially eligible articles. The full text of the selected articles were read to verify whether they fulfilled all the inclusion and exclusion criteria.The following information was extracted from each study that was included in the systematic review: name of the first author; year of publication; name of the study and the country; sample size and characteristics of the included participants, such as age, sex, and baseline BMI; length of follow-up; dietary intake assessment method; number of FFQ items and validation of the FFQ (yes or no); exposure (type of yogurt: whole-fat, low-fat, or total yogurt consumption); and categorization and serving size (for every study, a serving size was considered to be 125 g or 1 cup). We also extracted a number of events when applicable, including the covariates included in the fully adjusted models, the main outcome (weight or waist change, overweight, obesity, and MetS), β-regression coefficients, and ORs or HRs with corresponding 95% CIs. This information was extracted by 2 reviewers (CS-O and MB-R), and discrepancies were resolved.
The Newcastle–Ottawa Scale was used to assess the methodologic quality of the studies (14). Better methodologic quality was indicated with a higher score in this scale. Studies with a total score of ≥7 are usually considered to be high quality. This scale evaluates 3 aspects: selection of the participants, measurement of exposure and outcome, and comparability.
Results
Literature search.
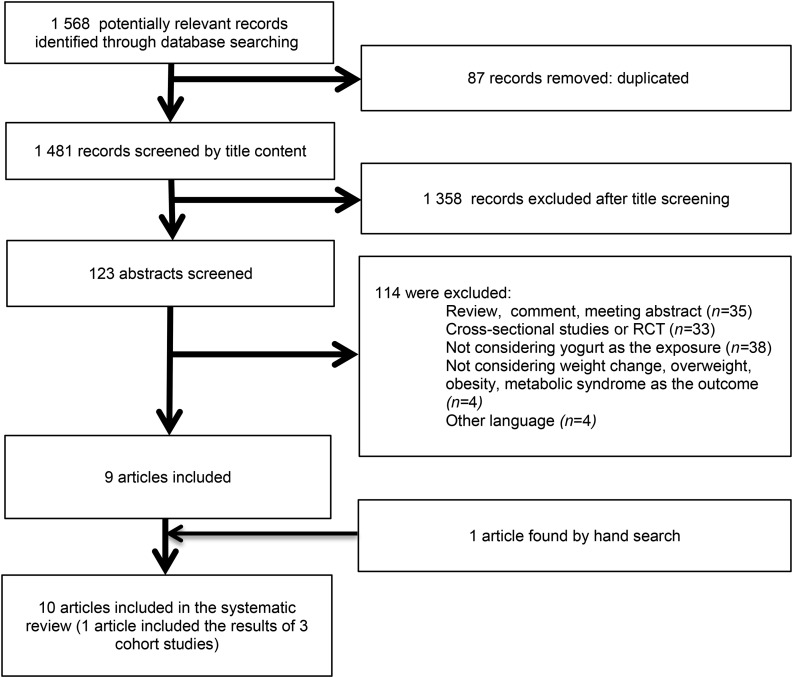
The results of the literature search are shown in Figure 1. In total, 1568 records were identified in PubMed and Web of Science until June 2016; after exclusion of duplicate records (n = 87), 1481 records were screened. In the first instance, records were screened only by title content, and 1358 records were excluded. Then the full texts of the remaining 123 records were read, and the articles that did not meet the inclusion criteria were excluded. These included reviews, comments, and meeting abstracts (n = 35); cross-sectional studies or RCTs (n = 33); those not considering yogurt as exposure (n = 38); those not considering weight or waist circumference change, overweight, obesity, or MetS as the outcome (n = 4); and those in other languages (n = 4). We added 1 more article that was found by hand search. Of the remaining 10 articles, 1 presented the results of 3 different cohort studies that we analyzed separately, and 4 presented the results of the same cohorts, but with different outcomes [the Seguimiento Universidad de Navarra (SUN) study (2 articles): risk of overweight or obesity and risk of MetS; and the Prevención con Dieta Mediterránea study (2 articles): risk of MetS and change in waist circumference]. Therefore, this systematic review finally included 10 cohort studies in total.
FIGURE 1.
Flow diagram depicting the identification and selection processes of relevant studies that investigated the association between yogurt consumption and the risk of overweight and obesity or weight gain and metabolic syndrome. RCT, randomized controlled trial.
Study characteristics.
The studies included in the review had a Newcastle–Ottawa Scale score between a minimum of 6 and a maximum of 8 points (Table 1).
TABLE 1.
Quality assessment scores according to the Newcastle–Ottawa Scale1
| Study (reference) | Year | Country | Selection (maximum = 4) | Comparability (maximum = 2) | Outcome (maximum = 3) | Total score (maximum = 9) |
| CARDIA (15) | 2002 | United States | 3 | 2 | 3 | 8 |
| SU.VI.MAX. (16) | 2008 | France | 3 | 2 | 2 | 7 |
| NHS I (17) | 2011 | United States | 2 | 2 | 2 | 6 |
| NHS II (17) | 2011 | United States | 2 | 2 | 2 | 6 |
| HPFUS (17) | 2011 | United States | 2 | 2 | 2 | 6 |
| EPIC (18) | 2011 | Italy, United Kingdom, Netherlands, Germany, and Denmark | 2 | 2 | 2 | 6 |
| Framingham Heart Study (19) | 2014 | United States | 2 | 2 | 3 | 7 |
| SUN (20) | 2014 | Spain | 2 | 2 | 2 | 6 |
| SUN (21) | 2015 | Spain | 2 | 2 | 2 | 6 |
| PREDIMED (22) | 2015 | Spain | 3 | 2 | 3 | 8 |
| Women’s Health Study (23) | 2016 | United States | 2 | 2 | 2 | 6 |
| PREDIMED (24) | 2016 | Spain | 3 | 2 | 3 | 8 |
CARDIA, Coronary Artery Risk Development in Young Adults; EPIC, European Prospective Investigation in Cancer and Nutrition; HPFUS, Health Professionals Follow-Up Study; NHS, Nurses’ Health Study; PREDIMED, Prevención con Dieta Mediterránea; SUN, Seguimiento Universidad de Navarra; SU.VI.MAX., Supplémentation en Vitamines et Minéraux Antioxydants.
The information extracted from the 9 cohort studies included in the present systematic review are summarized in Tables 2 and 3. Studies that investigated weight gain, change in waist circumference, or the risk of overweight or obesity as outcomes were conducted in the United States (15, 17, 19, 23); France (16); Italy, the United Kingdom, Netherlands, Germany, and Denmark (18); and Spain (20, 24). Studies that assessed the incidence of MetS were conducted in the United States (15) and Spain (21, 22) (Table 2). Yogurt consumption was measured with the use of FFQs in all studies except one that used a 24-h dietary recall (16). Dietary information was updated in 7 studies (16, 17, 19, 22, 24) by using repeated measurements of dietary intake from repeated FFQs during the follow-up period (data not shown).
TABLE 2.
Study design and characteristics of the prospective epidemiologic studies investigating weight change, incident overweight and obesity, or metabolic syndrome in relation to yogurt consumption1
| Author, year (reference) | Study | Country | Participants, n | Age, y | Men, % | Baseline BMI, kg/m2 | Mean duration of follow-up, y | Dietary assessment method | FFQ items, n | Validation of FFQ | Type of yogurt and categorization (serving size) |
| Pereira et al., 2002 (15) | CARDIA | United States | 3157 (923 overweight) | 18–30 | NR | NR | 10 | Quantitative FFQ | ∼700 | Yes | Not specified: 1 daily eating occasion of yogurt |
| Vergnaud et al., 2008 (16) | SU.VI.MAX. | France | 2267 | Men: 51.5 ± 4.4 | 55 | Men: 25.2 ± 3.0 | 6 | 24-h dietary recall | NA | NR | Total yogurt: quartiles of yogurt consumption (125 g) |
| Mozaffarian et al., 2011 (17) | NHS I | United States | 50,422 | 52.2 ± 7.2 | 0 | 23.7 ± 1.4 | 20 | FFQ | NR | Yes | Yogurt: increase in the number of servings per day (220 g) |
| Mozaffarian et al., 2011 (17) | NHS II | United States | 47,898 | 37.5 ± 4.1 | 0 | 23.0 ± 2.7 | 12 | FFQ | NR | Yes | Yogurt: increase in the number of servings per day (220 g) |
| Mozaffarian et al., 2011 (17) | HPFUS | United States | 22,557 | 50.8 ± 7.5 | 100 | 24.7 ± 1.1 | 20 | FFQ | NR | Yes | Yogurt: increase in the number of servings per day (220 g) |
| Romaguera et al., 2011 (18) | EPIC | Italy, United Kingdom, Netherlands, Germany, and Denmark | 48,631 | <60 at baseline | 40.4 | NR | 5.5 | FFQ | NR | Yes | Yogurt: 100-kcal increase in intake |
| Wang et al., 2014 (19) | Framingham Heart Study | United States | 3440 | 54.5 ± 9.6 | 45 | 27.4 ± 4.9 | 13 | FFQ | 126 | Yes | Yogurt: <1, 1 to <3, and ≥3 servings/wk (220 g) |
| Martínez-González et al., 2014 (20) | SUN | Spain | 8516 | 37.1 ± 10.8 | 34.1 | 21.9 ± 1.9 | 6.6 | FFQ | 136 | Yes | Total yogurt: whole-fat yogurt; low-fat yogurt; 0–2, >2 to <5, 5 to <7, 7, and ≥7 servings/wk (125 g) |
| Sayon-Orea et al., 2015 (21) | SUN | Spain | 8063 | 36.4 ± 11.6 | 34.2 | 22.7 ± 2.7 | 6 | FFQ | 136 | Yes | Total yogurt: whole-fat yogurt; low-fat yogurt; 0–2, >2 to <7, and ≥7 servings/wk (125 g) |
| Babio et al., 2015 (22) | PREDIMED | Spain | 1868 | 55–80 | 46.2 | T1:28.2 ± 3.4 T2:28.3 ± 3.4 T3:28.6 ± 3.7 | 3.2 | FFQ | 137 | Yes | Total yogurt: whole-fat yogurt; low-fat yogurt; tertiles (125 g) |
| Rautiainen et al., 2016 (23) | Women’s Health Study | United States | 18,438 | ≥45 | 0 | ∼22.4 ± 1.6 | 11.2 | FFQ | 131 | Yes | Yogurt: 0, >0 to <0.5, 0.5 to <1, and ≥1 servings/d (220 g) |
| Santiago et al., 2016 (24) | PREDIMED | Spain | 4545 | 55–80 | 32.7 | 31.1 ± 3.5 | 4.9 | FFQ | 137 | Yes | Total yogurt: whole-fat yogurt; low-fat yogurt; quintiles (125 g) |
Values are means ± SDs or ranges, unless otherwise indicated. CARDIA, Coronary Artery Risk Development in Young Adults; EPIC, European Prospective Investigation in Cancer and Nutrition; HPFUS, Health Professionals Follow-Up Study; NA, not applicable; NHS, Nurses’ Health Study; NR, not reported; PREDIMED, Prevención con Dieta Mediterránea; SUN, Seguimiento Universidad de Navarra; SU.VI.MAX., Supplémentation en Vitamines et Minéraux Antioxydants; T, tertile.
TABLE 3.
Values for the association between yogurt consumption and weight change, incident overweight/obesity, or metabolic syndrome in prospective epidemiologic studies1
| Author, year (reference) | Study | Events, n | Covariates in the adjusted model | Outcome2 |
| Pereira et al., 2002 (15) | CARDIA | Obesity: 331 | Age; sex; calorie intake per day; study center; baseline BMI; educational level; alcohol intake; smoking status; physical activity; vitamin supplements; PUFA, caffeine, and fiber intake; whole and refined grain, meat, fruit, vegetable, and soda consumption; and magnesium, calcium, and vitamin D intake | OR for obesity: 0.47 (0.16, 1.43) |
| IRS: 293 | OR for IRS: 0.58 (0.20, 1.66) | |||
| Vergnaud et al., 2008 (16) | SU.VI.MAX. | NA | Age, intervention group, baseline value of the outcome, educational level, smoking status, physical activity level, energy intake, mean adequacy ratio, alcohol intake, menopausal status (in women), and milk and cheese consumption | Normal weight: quartile 1 weight change, 1.00 ± 0.25 kg; quartile 4 weight change, 2.05 ± 0.27 kg; quartile 1 WC, 2.06 ± 0.43 cm; quartile 4 WC, 2.42 ± 0.46 cm; Overweight: quartile 1 weight change: 1.70 ± 0.82 kg; quartile 4 weight change: 1.59 ± 0.712 kg; quartile 1 WC: 1.62 ± 1.03 cm; quartile 4 WC: 0.33 ± 0.432 cm |
| Mozaffarian et al., 2011 (17) | NHS I | NA | Age, baseline BMI, sleep duration, changes in physical activity, alcohol use, television watching, smoking, and dietary factors | Weight change within each 4-y period: −0.34 kg (−0.41, −0.27 kg)3 |
| Mozaffarian et al., 2011 (17) | NHS II | NA | Age, baseline BMI, sleep duration, changes in physical activity, alcohol use, television watching, smoking, and dietary factors | Weight change within each 4-y period: −0.45 kg (−0.54, −0.36 kg)3 |
| Mozaffarian et al., 2011 (17) | HPFUS | NA | Age, baseline BMI, sleep duration, changes in physical activity, alcohol use, television watching, smoking, and dietary factors | Weight change within each 4-y period: −0.31 kg (−0.43, −0.20 kg)3 |
| Romaguera et al., 2011 (18) | EPIC | NA | Total energy intake; age; baseline weight, height, and WC; smoking; alcohol intake; physical activity; education; follow-up duration; and menopausal status and hormone replacement therapy (in women) | Change in WC: all, −0.02 (−0.03, −0.01)3; men, −0.03 (−0.05, −0.01)3; women, −0.02 (−0.04, −0.01)3 |
| Wang et al., 2014 (19) | Framingham Heart Study | NA | Sex, age, smoking status, physical activity, and weight or WC at the beginning of each exam interval; and mean total energy intake and DAGI score during each exam interval | Annual change in weight: <1 serving, 0.16 ± 0.02 kg/y; ≥3 servings, 0.07 ± 0.042 kg/y Annual change in WC: <1 serving, 0.71 ± 0.02 cm/y; ≥3 servings, 0.57 ± 0.042 cm/y |
| Martínez-González et al., 2014 (20) | SUN | Obesity: 1860 | Sex, age, baseline weight, physical activity, hours of television watching, hours spent sitting down, smoking status, snacking between meals, following a special diet, total energy intake, adherence to Mediterranean diet, marital status, and years of education | Annual change in weight, >7 vs. <2 servings/wk: total yogurt, −0.029 kg (−0.088, 0.030 kg); whole-fat yogurt, −0.052 kg (−0.150, 0.045 kg); low-fat yogurt, −0.032 kg (−0.134, 0.069 kg) Overweight or obesity, HR: total yogurt, 0.80 (0.68, 0.94)3; whole-fat yogurt, 0.62 (0.47, 0.82)3; low-fat yogurt, 0.84 (0.61, 1.15) |
| Sayon-Orea et al., 2015 (21) | SUN | MetS: 306 | Age, sex, baseline weight, total energy intake, alcohol intake, soft drinks, red meat, french fries, fast food, Mediterranean diet, physical activity, sedentary behavior, hours sitting, smoking status, snacking between meals, following a special diet | Incident MetS, OR: total yogurt, 0.84 (0.60, 1.18); whole-fat yogurt, 0.98 (0.68, 1.41); low-fat yogurt, 0.63 (0.39, 1.02) |
| Babio et al., 2015 (22) | PREDIMED | MetS: 930 | Sex; age; leisure time physical activity; BMI; smoking status; use of hypoglycemic, hypolipidemic, antihypertensive, or insulin treatment at baseline; mean consumption of vegetables, fruit, legumes, cereals, fish, red meat, cookies, olive oil, nuts, and alcohol; and MetS components at baseline | Incident MetS, HR: total yogurt, 0.77 (0.65, 0.91)3; whole-fat yogurt, 0.78 (0.66, 0.92)3; low-fat yogurt, 0.73 (0.62, 0.86)3 |
| Rautiainen et al., 2016 (23) | Women’s Health Study, United States | Overweight orobesity: 8102 | Age, randomization treatment, smoking status, physical activity, postmenopausal status, postmenopausal hormone use, history of hypercholesterolemia, history of hypertension, multivitamin use, alcohol intake, energy intake, and fruit and vegetable intake | Overweight or obesity, HR: yogurt, 1.16 (1.02, 1.31)3 |
| Santiago et al., 2016 (24) | PREDIMED | Reversion of abdominal obesity: 867 | Age, sex, physical activity, Mediterranean diet adherence, total energy intake, smoking status, baseline BMI, intervention group, and center | Annual change in WC, quintile 5 vs. quintile 1: total yogurt, −0.21 cm (−0.46, 0.05 cm); whole-fat yogurt, −0.23 cm (−0.46, −0.00 cm)3; low-fat yogurt, −0.15 cm (−0.47, 0.17 cm) |
| Reversion of abdominal obesity, OR: total yogurt, 1.29 (0.96, 1.73); whole-fat yogurt, 1.43 (1.06, 1.93)3; low-fat yogurt, 1.02 (0.73, 1.44) |
CARDIA, Coronary Artery Risk Development in Young Adults; DAGI, Dietary Guidelines Adherence Index; EPIC, European Prospective Investigation in Cancer and Nutrition; HPFUS, Health Professionals Follow-Up Study; IRS, insulin resistance syndrome; MetS, metabolic syndrome; NA, not applicable; NHS, Nurses’ Health Study; PREDIMED, Prevención con Dieta Mediterránea; SUN, Seguimiento Universidad de Navarra; SU.VI.MAX., Supplémentation en Vitamines et Minéraux Antioxydants; WC, waist circumference.
Values are means (95% CIs) or means ± SEs.
Statistically significant results.
Association between yogurt consumption and weight or waist circumference change.
A total of 8 cohort studies (16–20, 24) evaluated the association between yogurt consumption and weight or waist circumference changes during follow-up. Vergnaud et al. (16) found that yogurt consumption was inversely associated with changes in weight and waist circumference, especially in men who were initially overweight. In this context, the results by Mozaffarian et al. (17), which used data from 3 separate large US cohorts, investigated the relation between yogurt consumption (among other dietary components) and long-term weight gain. These 3 cohorts were the Nurses’ Health Study (NHS); the NHS II, a prospective study of younger female registered nurses; and the Health Professionals Follow-Up Study. Participants included in these cohorts were followed-up through mailed questionnaires that were sent every 2 y. The sample sizes of these 3 cohorts were very large; however, they were substantially reduced after exclusions. In the final sample, a total of 120,877 participants [98,320 women (50,422 from the NHS and 47,898 from the NHS II) and 22,557 men from the Health Professionals Follow-Up Study] were included in the analyses. All included participants were free of obesity and chronic disease at baseline and all also had complete data on weight and lifestyle habits. This study concluded that an increase in the number of servings per day of yogurt was inversely associated with weight changes. The pooled results from the 3 studies were −0.37 kg (95% CI: −0.45, −0.30 kg); P value < 0.001 (the results for each cohort are shown in Table 3). Along these lines, Romaguera et al. (18) analyzed data from 48,631 men and women from 5 countries who participated in the European Prospective Investigation in to Cancer and Nutrition study. After a median follow-up time of 5.5 y, the estimated inverse association between yogurt consumption and annual change in waist circumference for a given BMI was −0.02 cm/y (95% CI: −0.03, −0.01 cm/y) per each 100-kcal increase in yogurt consumption (P < 0.001). Consistent with these results, in the Framingham Study, Wang et al. (19) also found an inverse association. Consumption of ≥3 servings/wk compared with the lowest category of yogurt consumption (<1 serving/wk) was associated with a mean ± SE annual decrease in weight and WC of −0.10 ± 0.04 kg (P-trend = 0.03) and −0.13 ± 0.05 cm (P-trend = 0.008), respectively. Martínez-González et al. (20) did not find a significant association between yogurt consumption and weight change (P-trend = 0.182, 0.153, and 0.566 for total, whole-fat, and low-fat yogurt consumption, respectively. Finally, Santiago et al. (24) found that the highest quintile of whole-fat yogurt consumption in comparison with the lowest quintile of consumption was associated with the greatest reduction in waist circumference. The mean yearly waist circumference change difference between the fifth and the first quintiles was −0.23 cm/y (95% CI: −0.46, −0.00 cm/y; P-trend = 0.05).
Association between yogurt consumption and the risk of overweight and obesity.
Three cohort studies assessed the association between yogurt consumption and the risk of overweight and obesity. Pereira et al. (15) found an inverse but not statistically significant association between yogurt consumption and the risk of obesity in initially overweight participants (OR: 0.47; 95% CI: 0.19, 1.43). The other study that assessed the association between yogurt consumption and the risk of overweight or obesity was the SUN cohort in Spain (20). The SUN cohort assessed the association between total, whole-fat, and low-fat yogurt consumption and the risk of becoming overweight or obese in 8516 university graduates initially free of overweight who were followed up for a median period of 6.6 y. During the follow-up period, a total of 1860 incident cases were identified. Total yogurt and whole-fat yogurt consumption were found to be inversely and significantly associated with the risk of becoming overweight or obese (HR: 0.80; 95% CI: 0.68, 0.94; P-trend = 0.001; and HR: 0.62; 95% CI: 0.47, 0.82; P-trend < 0.001 for total and whole-fat yogurt consumption, respectively) when comparing high consumption (>7 servings/wk) with low consumption (0–2 servings/wk).
Interestingly, in the SUN study, stratified analyses by low or high fruit consumption found that in those participants whose fruit consumption was above the median, yogurt consumption exhibited a stronger inverse association with the risk of becoming overweight or obese (HR: 0.68; 95% CI: 0.54, 0.86; P-trend = 0.001 for total yogurt; HR: 0.61; 95% CI: 0.41, 0.91; P-trend = 0.004 for whole-fat yogurt; and HR: 0.67; 95% CI: 0.44, 1.02; P-trend = 0.103 for low-fat yogurt consumption), with a statistically significant interaction (P = 0.03). The inverse association of yogurt consumption with the risk of becoming overweight or obese was not apparent when fruit consumption was below the median (16).
The third study that assessed the association between yogurt consumption and the risk of overweight and obesity was conducted in the United States as a part of the Women’s Health Study (23). This study included 18,438 middle-aged women with a baseline BMI (in kg/m2) >18.5 and <25. These women were followed up for a mean of 11.2 y. During the follow-up period, 8238 incident cases of overweight or obesity were found. Contrary to previous studies, the Women’s Health Study found a higher risk of overweight and obesity associated with yogurt consumption. The HR of becoming overweight or obese for the highest category of consumption compared with nonconsumers of yogurt was 1.16 (95% CI: 1.02, 1.31; P-trend = 0.002).
Only one study assessed the association between yogurt consumption and the probability of abdominal obesity reversion. In this study, Santiago et al. (24) included 4545 participants at high cardiovascular disease risk, all of whom had abdominal obesity at baseline. After a median follow-up of 4.9 y, they found that participants in the highest quintile of whole-fat yogurt consumption had a 43% higher probability of reverting their abdominal obesity than did participants in the lowest quintile of whole-fat yogurt consumption (OR: 1.43; 95% CI: 1.06, 1.93; P-trend = 0.26).
Association between yogurt consumption and the risk of MetS.
Three prospective cohort studies assessed the association between yogurt consumption and the risk of MetS. The first study was conducted by Pereira et al. (15) in 2002. That study evaluated this association in the Coronary Artery Risk Development in Young Adults study, a US cohort of black and white adults aged between 18 and 30 y. The study was a multicenter population-based study of cardiovascular disease risk factor evolution. The study found an inverse but not statistically significant association between yogurt consumption and lower risk of MetS (OR: 0.58; 95% CI: 0.20, 1.66) in overweight individuals at baseline. The second cohort study that assessed this relation was conducted in Spain. In the SUN study, Sayon-Orea et al. (21) analyzed the association between total, whole-fat, and low-fat yogurt consumption and the risk of MetS and each of its components. During the first 6 y of follow-up, 306 incident cases of MetS were identified in 8063 participants who were included in the study and free of any of these 5 components of MetS at baseline. Participants who were in the highest category of consumption (≥7 servings/wk) compared with those in the lowest category (≤2 servings/wk) of total, whole-fat, and low-fat yogurt consumption showed nonsignificant inverse associations with MetS (OR: 0.84; 95% CI: 0.60, 1.18; P-trend = 0.32; OR: 0.98; 95% CI: 0.68, 1.41; P-trend = 0.89; and OR: 0.63; 95% CI: 0.39, 1.02; P-trend = 0.17, respectively]. When each component of MetS was analyzed, only central adiposity was found to be inversely associated with total and whole-fat yogurt consumption (OR: 0.85; 95% CI: 0.74, 0.98 and OR: 0.85; 95% CI: 0.73, 0.99, respectively). As in the previous study of this same cohort, when the joint exposures were assessed while combining total yogurt consumption and fruit consumption, those in the highest category of total yogurt consumption who were high consumers of fruit [(≥264.5 g/d (the median)] exhibited a significantly lower risk of developing MetS (OR: 0.61; 95% CI: 0.38, 0.99) than did those in the lowest category of total yogurt consumption and who were low consumers of fruit (below the study median). The last cohort that studied this association was conducted as a part of the Prevención con Dieta Mediterránea study. Babio et al. (22) evaluated the association between yogurt consumption and the incidence of MetS in a Mediterranean population at high risk of cardiovascular disease. This study prospectively analyzed 1868 men and women >55 y old who did not have MetS at baseline, with a median follow-up of 3.2 y. They observed 930 incident cases of MetS during follow-up. The adjusted HRs for the highest compared with the lowest tertile of yogurt consumption were 0.77; 95% CI: 0.65, 0.91; P-trend = 0.14; 0.73; 95% CI: 0.62, 0.86; P-trend = 0.004; and 0.78; 95% CI: 0.66, 0.92; P-trend = 0.003 for total, low-fat, and whole-fat yogurt consumption, respectively.
Discussion
To the best of our knowledge, this is the first systematic review to include only longitudinal cohort studies to assess the association between total yogurt consumption and change in waist circumference or body weight or the risk of being overweight or obese or developing MetS or reversion of abdominal obesity. To our knowledge, there is only one previous review that summarized the evidence until 2014 on yogurt consumption and management or maintenance of body weight. In that review, Jacques and Wang (25) concluded that knowledge of the specific role that yogurt might play in weight management was still limited. However, one of the recommendations they gave was to include yogurt as part of a healthy diet to meet dairy recommendations, because yogurt is a nutrient-dense, lower-calorie food. Therefore, with the present systematic review, we tried to expand on and update the available evidence on the association between yogurt consumption and body weight–related outcomes.
Of the 10 cohort studies included in this systematic review, 3 analyzed the association between yogurt consumption and the risk of being overweight or obese (15, 20, 23), 8 analyzed changes in waist circumference and/or weight changes (16–20, 24), 3 studied the association with the risk of developing MetS (15, 21, 22), and 1 studied the association with the probability of abdominal obesity reversion (24). Cohorts that studied changes in waist circumference or body weight during follow-up showed inverse associations in their point estimates for both changes in waist circumference and body weight. This association was not statistically significant in only one study (20). None of the included studies showed a detrimental effect of yogurt consumption on weight status or on the risk of developing MetS.
There was also one systematic review of dairy consumption and overweight and obesity (7). In that review, Louie et al. (7) suggested that there might be a protective effect of dairy consumption (not exclusively yogurt consumption) on the risk of overweight and obesity. However, the evidence was not consistent. That review and the results of another cohort study (20) concluded that low-fat dairy products or low-fat yogurts, respectively, did not have more beneficial effects on weight status or overweight and obesity risk than did regular whole-fat products. This might be explained by some benefit inherent in the fat contained in whole-fat dairy products (26), or alternatively by residual confounding derived from the fact that participants who consume low-fat yogurts have special lifestyle characteristics (27), or by the higher sugar content of low-fat yogurts.
Of the three cohort studies that assessed the association between yogurt consumption and the risk of becoming overweight or obese, 2 found an inverse association (19, 20), and 1 found a positive association (23). The study that found a positive association was conducted in middle-aged women (>45 y of age) at prepostmenopausal stage. There is no clear explanation for these conflicting results. Although the menopause transition may play a role in adipose tissue expansion (28) and may partly account for the heterogeneity in the association with yogurt, further studies are needed to better assess this hypothesis.
Two of the studies included in the present review found that when yogurt was consumed together with a fruit-rich overall dietary pattern, the beneficial observed associations were even more apparent (20, 21). This suggestion of a potential synergistic effect is consistent with the current view that it is more likely that the interactions between many components of the diet or the overall quality of a dietary pattern may offer greater protection against obesity or MetS than each of the isolated food components (29).
Of the mechanisms that have been proposed to support the observed associations, the most accepted theory is the one proposed by Zemel et al. (30–32) in relation to the metabolism of calcium. It has been suggested that calcium intake may be able to reduce lipogenesis and increase lipolysis by the suppression of the formation of 1,25-dihydroxyvitamin D, and also by the secretion of parathyroid hormone. In this context, it is known that increased intake of the calcium contained in dairy products, and especially in yogurts, might lead to an increase in fat oxidation (33). A second mechanism could be explained by the formation of calcium soaps in the intestine, which is promoted after yogurt consumption because of the content of calcium in yogurt. These calcium soaps help to produce increased fat excretion and reduced fat absorption (33).
Another possible mechanism that could be implicated in these beneficial effects might be the role that microbiota may play in the development of obesity and cardiometabolic diseases (34). Some bacteria that are used as probiotics in yogurt, such as Lactobacillus acidophilus and Bifidobacterium bifidus, are suggested as helping to prevent or treat some diseases (35, 36). Recently, it has been proposed by Butel (35) that in some diseases, such as infectious diarrhea, inflammatory bowel disease, irritable bowel syndrome, some allergies, and diseases due to Helicobacter pylori (such as gastric ulcers and some gastric cancers), and of course in obesity and diabetes, probiotics might be beneficial. This beneficial effect can be explained by the probiotic content of yogurt, which may improve gut health and reduce chronic inflammation by enhancing innate and adaptive immune responses, intestinal barrier function, and lipid profiles, and by regulating appetite (37).
The available evidence from epidemiologic longitudinal studies is consistent with the existence of inverse associations between yogurt consumption and adiposity or MetS. However, given the scarcity of cohort studies specifically assessing these associations, a pending issue is the need to better assess the possibility of publication bias. This bias could occur if authors of studies finding inverse associations were more likely to submit these studies very early to publication, whereas authors of cohort studies with null or positive associations were more likely to delay their submissions. Nevertheless, it is interesting to note that some of the published studies did not show statistically significant results. This fact does not suggest a publication bias. Another limitation of this review is that we were only able to search 2 different data bases; therefore, we might have missed some articles. In addition, because of the heterogeneity of the included articles, a quantitative meta-analysis of the results was not possible.
Conclusions
From the results of the investigations presented in this review, we can conclude the following: 1) the inverse association between yogurt consumption and the risk of developing overweight or obesity is neither clear nor consistent; therefore, there is a need for further prospective studies and high-quality randomized clinical trials to confirm this suggestion of an inverse association; 2) anthropometric variables such as weight and waist change might be reduced within an overall dietary pattern that includes frequent consumption of yogurt, especially when yogurt is consumed as part of a healthy diet together with high fruit consumption; 3) high consumption of yogurt in tandem with high consumption of fruit seems to be inversely associated with the development of MetS; and 4) there is a need to increase the number of cohort studies that specifically assess the association of yogurt consumption with adiposity or MetS and to better ascertain the possibility of publication bias.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: MetS, metabolic syndrome; NHS, Nurses’ Health Study; RCT, randomized controlled trial; SUN, Seguimiento Universidad de Navarra.
References
- 1.World Health Organization. Obesity and overweight. Fact sheet no. 311. Updated January2015 [cited 2015 Aug 19]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.
- 2.Wilson PWF, D’Agostino R, Parise H, Sullivan L, Meigs J. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005;112:3066–72. [DOI] [PubMed] [Google Scholar]
- 3.Grundy SM, Brewer HB, Cleeman J, Smith S, Lenfant C. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004;109:433–8. [DOI] [PubMed] [Google Scholar]
- 4.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr., et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation task force on epidemiology and prevention, National Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity. Circulation 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
- 5. The Dairy Council. The nutritional composition of dairy products. London:The Dairy Council; 2007–2016. [Google Scholar]
- 6.Wang H, Livingston KA, Fox CS, Meigs JB, Jacques PF. Yogurt consumption is associated with better diet quality and metabolic profile in American men and women. Nutr Res 2013;33:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Louie JCY, Flood VM, Hector DJ, Rangan AM, Gill TP. Dairy consumption and overweight and obesity: a systematic review of prospective cohort studies. Obes Rev 2011;12:e582–92. [DOI] [PubMed] [Google Scholar]
- 8.Astrup A. Yogurt and dairy product consumption to prevent cardiometabolic diseases: epidemiologic and experimental studies. Am J Clin Nutr 2014;99:1235S–42S. [DOI] [PubMed] [Google Scholar]
- 9.Chen GC, Szeto IM, Chen LH, Han SF, Li YJ, van Hekezen R, Qin LQ. Dairy products consumption and metabolic syndrome in adults: systematic review and meta-analysis of observational studies. Sci Rep 2015;5:14606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abargouei AS, Janghorbani M, Salehi-Marzijarani M, Esmaillzadeh A. Effect of dairy consumption on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Int J Obes (Lond) 2012;36:1485–93. [DOI] [PubMed] [Google Scholar]
- 11.Chen M, Pan A, Malik VS, Hu FB. Effects of dairy intake on body weight and fat: A meta-analysis of randomized controlled trials. Am J Clin Nutr 2012;96:735–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwingshackl L, Hoffmann G, Schwedhelm C, Kalle-Uhlmann T, Missbach B, Knuppel S, Boeing H. Consumption of dairy products in relation to changes in anthropometric variables in adult populations: a systematic review and meta-analysis of cohort studies. PLoS One 2016;11:e0157461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. [DOI] [PubMed] [Google Scholar]
- 14.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Updated 2010 [cited 2015 Aug 20]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf.
- 15.Pereira MA, Jacobs DR, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA study. JAMA 2002;287:2081–9. [DOI] [PubMed] [Google Scholar]
- 16.Vergnaud AC, Péneau S, Chat-Yung S, Kesse E, Czernichow S, Galan P, Hercberg S, Bertrais S. Dairy consumption and 6-y changes in body weight and waist circumference in middle-aged French adults. Am J Clin Nutr 2008;88:1248–55. [DOI] [PubMed] [Google Scholar]
- 17.Mozaffarian D, Hao T, Rimm E, Willett W, Hu F. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011;364:2392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romaguera D, Ängquist L, Du H, Jakobsen MU, Forouhi NG, Halkjær J, Feskens EJ, van der A DL, Masala G, Steffen A, et al. Food composition of the diet in relation to changes in waist circumference adjusted for body mass index. PLoS One 2011;6:e23384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Troy LM, Rogers GT, Fox CS, McKeown NM, Meigs JB, Jacques PF. Longitudinal association between dairy consumption and changes of body weight and waist circumference: the Framingham Heart Study. Int J Obes (Lond) 2014;38:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martínez-González MA, Sayon-Orea C, Ruiz-Canela M, de la Fuente C, Gea A, Bes-Rastrollo M. Yogurt consumption, weight change and risk of overweight/obesity: The SUN cohort study. Nutr Metab Cardiovasc Dis 2014;24:1189–96. [DOI] [PubMed] [Google Scholar]
- 21.Sayón-Orea C, Bes-Rastrollo M, Marti A, Pimenta AM, Martin-Calvo N, Martínez-González MA. Association between yogurt consumption and the risk of metabolic syndrome over 6 years in the SUN study. BMC Public Health 2015;15:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Babio N, Becerra-Tomás N, Martínez-González MÁ, Corella D, Estruch R, Ros E, Sayón-Orea C, Fitó M, Serra-Majem L, Arós F, et al. Consumption of yogurt, low-fat milk, and other low-fat dairy products is associated with lower risk of metabolic syndrome incidence in an elderly Mediterranean population. J Nutr 2015;145:2308–16. [DOI] [PubMed] [Google Scholar]
- 23.Rautiainen S, Wang L, Lee IM, Manson JE, Buring JE, Sesso HD. Dairy consumption in association with weight change and risk of becoming overweight or obese in middle-aged and older women: a prospective cohort study. Am J Clin Nutr 2016;103:979–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santiago S, Sayon-Orea C, Babio N, Ruiz-Canela M, Marti A, Corella D, Estruch R, Fito M, Aros F, Ros E, et al. Yogurt consumption and abdominal obesity reversion in the PREDIMED study. Nutr Metab Cardiovasc Dis 2016;26:468–75. [DOI] [PubMed] [Google Scholar]
- 25.Jacques PF, Wang H. Yogurt and weight management. Am J Clin Nutr 2014;99:1229S–34S. [DOI] [PubMed] [Google Scholar]
- 26.Krishnan S, Cooper JA. Effect of dietary fatty acid composition on substrate utilization and body weight maintenance in humans. Eur J Nutr 2014;53:691–710. [DOI] [PubMed] [Google Scholar]
- 27.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed Philadelphia: Lippincott Williams and Wilkins; 2008. [Google Scholar]
- 28.Davis SR, Castelo-Branco C, Chedraui P, Lumsden MA, Nappi RE, Shah D, Villaseca P. Understanding weight gain at menopause. Climacteric 2012;15:419–29. [DOI] [PubMed] [Google Scholar]
- 29.Baxter AJ, Coyne T, McClintock C. Dietary patterns and metabolic syndrome–a review of epidemiologic evidence. Asia Pac J Clin Nutr 2006;15:134–42. [PubMed] [Google Scholar]
- 30.Zemel MB, Richards J, Mathis S, Milstead A, Gebhardt L, Silva E. Dairy augmentation of total and central fat loss in obese subjects. Int J Obes (Lond) 2005;29:391–7. [DOI] [PubMed] [Google Scholar]
- 31.Zemel MB. Proposed role of calcium and dairy food components in weight management and metabolic health. Phys Sportsmed 2009;37:29–39. [DOI] [PubMed] [Google Scholar]
- 32.Zemel MB. Role of dietary calcium and dairy products in modulating adiposity. Lipids 2003;38:139–46. [DOI] [PubMed] [Google Scholar]
- 33.Melanson EL, Sharp TA, Schneider J, Donahoo WT, Grunwald GK, Hill JO. Relation between calcium intake and fat oxidation in adult humans. Int J Obes Relat Metab Disord 2003;27:196–203. [DOI] [PubMed] [Google Scholar]
- 34.Ebel B, Lemetais G, Beney L, Cachon R, Sokol H, Langella P, Gervais P. Impact of probiotics on risk factors for cardiovascular diseases. A review. Crit Rev Food Sci Nutr 2014;54:175–89. [DOI] [PubMed] [Google Scholar]
- 35.Butel MJ. Probiotics, gut microbiota and health. Med Mal Infect 2014;44:1–8. [DOI] [PubMed] [Google Scholar]
- 36.DiBaise JK, Frank DN, Mathur R. Impact of the gut microbiota on the development of obesity: current concepts. Am J Gastroenterol 2012;1:22–7. [Google Scholar]
- 37.Pei R, Martin DA, DiMarco DM, Bolling BW. Evidence for the effects of yogurt on gut health and obesity. Crit Rev Food Sci Nutr 2015. (Epub ahead of print; DOI: 10.1080/10408398.2014.883356). [DOI] [PubMed] [Google Scholar]