Abstract
Introduction
Although the use of an endoprosthesis for distal femoral fractures remains a valid treatment option the widespread use is in its infancy.
Methodology
In this retrospective case series, we review cases of distal femoral fracture treated with endoprosthetic replacement (EPR). The outcomes we assessed were the time to start mobilising, the time to discharge, morbidity and mortality as well as an Oxford knee score to assess pain and function and also the early survivorship. 6 of the 11 from the cohort had existing Total Knee Replacements (TKRs) in situ.
Results
There were 11 knees in our cohort with a mean age of 81.5 years (range 52–102 years). The median time to follow up was 3.5 years (range 1.6 to 5.5 years). The median times to theatre was 3 days and to discharge was 16 days.
Oxford functional and pain scores were 32/48.
Discussion
In the appropriate patient and fracture pattern, Endoprosthetic knee replacement is an excellent option in the treatment of distal femoral fractures whether associated with an existing TKR or not. The implant is more costly than traditional open reduction and internal fixation, but the earlier return to full mobility post-operatively may save on hospital/care home stay and free up hospital space and minimise complications.
Keywords: Fracture femur, Endoprosthesis, Trauma, Knee replacement, Distal femoral fracture treatment
1. Introduction
The incidence of distal femoral fractures has been estimated to be 37/100,000 population.1 In the elderly population, the mechanism of injury is usually low energy trauma following a fall. However, the injury may be complicated by a poor soft tissue envelope and poor bone stock. Moreover, significant degenerative changes in the adjacent joint could be present.
Treatment options for these injuries include non-operative management but carries a higher risk of non-union (over 30%) and the risks of immobilisation,2, 3 and reconstruction with such implants as the intercondylar blade or screw plate,4, 5, 6, 7, 8 locking plates,9, 10, 11, 12 and retrograde intramedullary nails.13, 14, 15 It is of interest that cadaveric studies have consistently showed that regardless of fracture pattern, retrograde intramedullary fixation with distal locking screws has demonstrated the highest resistance to fatigue, failure and resistance to both axial and torsional forces when compared to fixed angle devices.16, 17, 18, 19 In the line with the above, Pekmezci et al.15 confirmed that the new locking retrograde femoral nail (with more distal screw fixation) displayed better stiffness and fatigue life than locking plates and the mode of failure for the plate was invariably plate fatigue. Another surgical option that could be considered in these distal femoral fractures with fragmentation is acute endoprosthetic replacement. This approach can be applied for not only in comminuted fractures but also in cases of periprosthetic fractures with either very distal fracture patterns not allowing adequate fixation or associated with loosening of the underlying implants. The literature reporting on this option remains poor.
We have therefore undertaken a retrospective review of patients that were managed with this philosophy in our institution.
2. Patients and methods
The following manuscript reports the follow up of 11 patients, 12 knees treated directly with an Endo-Model Endoprosthesis.
Between 2007 and 2012 elderly patients that presented to our institution with either distal femoral fractures or periprosthetic distal femoral fractures were eligible to participate in this study. Inclusion criteria were the presence of a distal femoral fracture not amenable to fixation. Exclusion criteria were young patients (under 50 yrs) and elderly patients that were initially managed with fixation. Such details were documented as patient demographics, mechanism of injury, type of fracture, comorbidities, time to theatre, perioperative and postoperative complications, time to start fully weight bearing, radiological time to union and signs of radiological loosening at the time of last follow up. Function was assessed using the Oxford knee score.20
Classification of fractures was carried out using the AO system for distal femoral metaphyseal fractures as described by Muller.10 Radiological loosening was assessed using the Miller technique.21
2.1. Description of surgical technique and patient management
The Endo-Model arthroplasty technique is well described and has been long used for treatment of complex primary osteoarthritis as well as in revision knee surgery.16, 22, 23, 24, 25, 26, 27, 28, 29 Its use in the trauma setting has yet to be published. The prosthesis has antitorsional, antitilt and antimigration properties. The ability to rotate gives secure bonding at the interfaces. The central flexion-rotation system can be converted to an anti-subluxation system and controls movement and stability (Fig. 1). It also avoids sliding and shares load with the tibial polyethylene spacer. The femoral and tibial components are connected through a tibial guide pin and a femoral bushing. The patella can be replaced or left according to surgeon preference.
Fig. 1.

Endo-Model® – M.
The technique in distal femoral fracture treatment requires detachment of all soft tissues from the fragment(s) to be excised, including the collateral ligaments, posterior capsule, popliteus and if necessary gastrocnemius (Fig. 2). The principle of safe dissection is to “stick to bone” to avoid injury to the underlying neurovascular structures. An approximation of the level of the joint line is made using patella position, distance from fibular head, or from meniscal remnants if available. Ultimately the extensor mechanism has to maintain appropriate tension to facilitate balanced knee flexion and extension. Lack of tension potentially allows pistoning of the implants in the medullary canals and an extensor lag. Conversely, excessive tension potentially risks limiting flexion and raises patellofemoral contact pressures. Modular blocks and collars are available in various sizes to fill in the defect left by the excised bony fragments.
Fig. 2.
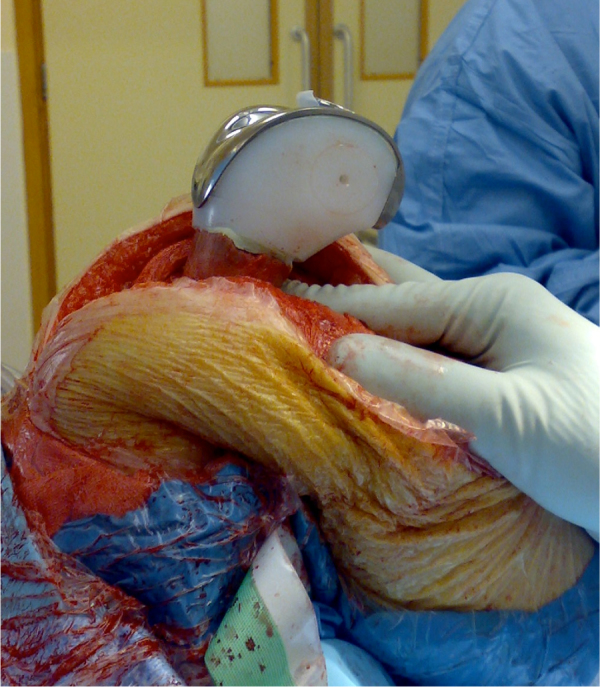
Femoral component with 55 mm polyethylene block in-situ.
The original prosthesis was non-modular in design and came in small, medium and large sizes with 180 mm stems. However the option to replace the distal femur was only available for the medium prosthesis, for which longer stem lengths of 240 mm were available. A polyethylene block, in the shape of the distal femoral condyles was available to fit over the stem within the distal part of the prosthesis. This block was 65 mm in height but could have one or two 10 mm sections removed giving the option to replace 45, 55, or 65 mm of distal femoral bone. The updated design is a modular prosthesis with stem length options ranging from 95 to 280 mm. A minimum stem length of 160 mm is recommended when a distal femoral replacement block is used. Small, Medium and Large size options are now available for both cemented or uncemented fixation. In all our cases the stems were cemented in place due to the poor quality of the surrounding bone. The distal femoral block is now titanium and is available in either 50 or 80 mm sizes. A series of collars (10–25 mm) are then available to fill bigger defects in fractures that extend more proximally. All cases were performed by the lead surgeon (JW) using a tourniquet (Fig. 3).
Fig. 3.
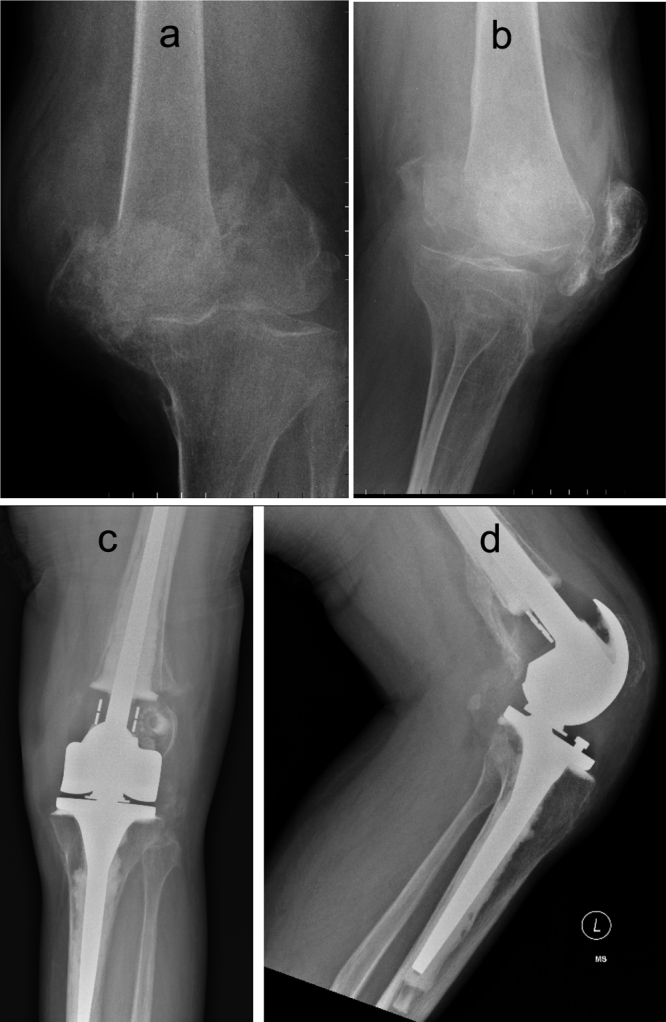
a & b: AP and Lateral views of the comminuted distal femoral fracture in 52yr old man (AO 33-C). c & d: AP and Lateral views of EPR post-operatively.
Patients were given a standard antibiotic regimen of flucloxacillin and gentamicin followed by 3 further post-operative doses of flucloxacillin (teicoplanin was administered as an alternative in penicillin-allergic patients). The antithrombotic regimen was a Low Molecular Weight Heparin (LMWH) for 4 weeks.
The minimum follow up was 36 months.
3. Results
During the pre-specified study period 12 displaced distal femoral metaphyseal fractures in 11 patients who were treated with an endoprosthesis (Endo-Model® – M, Link Orthopaedics, Hamburg) met the inclusion criteria.
-
i
Patient Demographics and mechanism of injury 6 patients had an existing knee arthroplasty in situ. In the remaining patients, 3 patients had severe degenerative changes of the knee at the time of surgery.
All the patients were pre-operatively able to walk outside and were medically fit for anaesthesia. Some were socially independent and lived in the community and some were living in nursing or social care (Table 1).
There were 3 men and 8 women with a mean age of 79 years (50 to 102 years). Table 2, Table 3: Table 1 of pre-operative mobility
Demographic information on all patients was prospectively coded onto a trauma database. The early and late post-operative complications, including prosthetic revision, were also recorded in the patient’s trauma records.
-
ii
Fracture classification
Of the 6 patients with existing knee implants, 2 had fractures with a 33-C1, 3 with 33-C2 and the remaining one with 33-C3. Although not applicable to periprosthetic fractures, the 6 cases with implants in situ had 2 cases with a 33-A2 “type” fracture pattern, 1 with a 33-A3 and the remaining 3 had a 33-C2 “type” fracture pattern.
-
iii
Length of hospital stay and complications
The average length of time to surgery was 5.75 days (in the calculation of this Fig. 2 entries [150 days and 280 days] were excluded as these were delayed referrals following failure of previous conservative management). The time to discharge was an average 18.8 days. The average time after operation the patient began to FWB was 3.6 days. This allowed for an early discharge with more patients able to go directly to their own homes.
In contrast to other studies, there were no mortalities, infections, wound complications or thromboembolic events in this patient group. The only significant complication was of lymphoedema in an 84 year old which persisted despite lymphoedema/compression stockings (see Table 4).
-
iv
Time to union
Time to union was not a factor as the fractured bone was excised. Implants were secured with intramedullary fixation and augmented with cement. The patients were able to fully weight bear from day one post-op.
-
v
Radiological loosening
At final review, none of the implants showed any signs of radiological loosening at either the AP or Lateral views.
-
vi
Oxford knee score
Mean Post-operative Oxford knee scores was 32/48 with a median of 35 (average follow up 3.6yrs; range 2.5–6.5yrs)
Table 1.
Table of patients demographics, results and complications.
| Name | Age | Date Injury | Days Until op | Days until FWB | Days until Discharge | Discharged to | Oxford Knee Score | Date of OKS | TKR | Co morbidity | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| JW | 88 | 01/06/2008 | 1 | 2 | 16 | Nursing Home | ? Dementia | 2004 | |||
| EO | 85 | 28/10/2007 | 150 (failed conservative Rx) | 2 | 36 | Nursing Home | 29 | 02/01/2013 | |||
| RC | 52 | 16/10/2008 | 3 | 2 | 16 | Home | 40 | 02/01/2013 | Osteogenesis-Imperfecta | ||
| AB | 82 | 11/01/2011 | 280(failed conservative Rx) | 7 | 28 | Rehab Ward | 26 | 16/04/2013 | 2001 | ||
| MS | 82 | 10/04/2011 | 1 | 2 | 14 | Home | 36 | 14/09/2011 | 2006 | ||
| EM − (bilat #) | 102 | 07/09/2011 | 28 | 13 | 28 | Rehab hosp | 25 & 25 | 16/04/2013 | Other femur Nailed | ||
| MR | 84 | 16/11/2011 | 2 | 1 | 14 | Home | 40 | 02/01/2013 | 1997 | Lymphoedema | |
| DC | 74 | 07/03/2012 | 2 | 1 | 15 | Home | 42 | 02/01/2013 | 1995 | Alkaptonuria | |
| BR − Left | 89 | 02/05/2012 | 2 | 5 | 13 | Res Home | 24 | 16/04/2013 | 2002 | ||
| BR − right | 29 | ||||||||||
| PE | 52 | 09/06/2011 | 7 | 3 | 8 | Home | 35 | 18/04/2013 | MS | ||
| Average | 79 | 5.75 | 3.6 | 18.8 | 32 | ||||||
Table 2.
Table of pre-operative mobility.
| EPR Group | |
|---|---|
| Able to Walk unaided | 6 |
| Frame or walking aids | 4 |
| Significant help needed | 1 |
Table 3.
Pre-operative living state.
| EPR Group | |
|---|---|
| Home | 7 |
| Residential Home | 3 |
| Nursing/psychiatric Home | 1 |
Table 4.
Data from EPR and ORIF groups for those with distal femoral fractures.
| Average age (mean) | Average no of days until theatre | No of post-op days until discharge | Oxford Knee scores | |
|---|---|---|---|---|
| EPR Group | 74.1 | 5.75 | 18.3 | 32 |
4. Discussion
Shape about 6–8 paragraphs and each paragraph must focus on one parameter of importance. Do not repeat your results again.
Treatment of this fracture pattern (with or without existing knee implant in situ) includes non-operative or operative management. Operative options include intercondylar blade or screw plate,30, 31, 32, 33, 34 locking plates35, 36, 37, 38 and retrograde intramedullary nails retrograde intramedullary nailing, fixed plate. In this study we introduce the Endoprosthetic replacement option.
4.1. Plate fixation
One rehabilitative issue with any plate fixation is that the patient is usually required to be non- or touch-weight-bearing until such time as the fracture has sufficiently healed and is structurally strong enough to support weight.4, 6, 7, 8 Osseous healing is often described as radiographs showing union in 3 out of four cortices.6 This usually takes at least 6 weeks following fixation but may be much longer in this age group. Studies report up to 14 weeks for allowing full weight bearing and 16 weeks for bony union after plate fixation.39 During this time the patient may develop other severe co-morbidities such as pneumonia, pressure sores and muscular atrophy.40 While one paper reported non-union rates as high as 43% and pre-morbid return to function in just over 50%41 others using the LISS technique have had no non-unions and a full recovery of flexion.9 None-the-less, in the elderly, a high one year mortality rate13 (21%) persists and early mobilisation and return to function is advocated.
4.2. Retrograde IM fixation
As previously stated in the introduction, other studies have shown that the retrograde IM fixation allows patients to weight-bear immediately with good clinical and radiological healing – as long as there is adequate distal fixation.42, 43 However, the distal location of the fracture (and often articular involvement) meant that the majority of the fractures in our series were not appropriate for retrograde nailing, meaning ORIF and non-weight bearing were the only options.
The treatment modality of a fracture around an existing knee arthroplasty (as defined by Rorabeck et al.44) is also difficult. The incidence of Periprosthetic fractures is increasing with time and the patient cohort will be older and more osteoporotic.45 While plate fixation is usually an option, the design and size of the intercondylar notch of the femoral implant may preclude the passing of a retrograde nail in many designs.46 Retrograde femoral nailing in this patient group also has good outcome with union usually occurring within 3 months.47 With either fixation method, concerns include the site of the original scar/vascularity of flaps, the position of screws and the need for graft and whether to consider minimal access surgery.48
The treatment for periprosthetic injuries with stemmed and stabilised arthroplasty has some good reported outcomes,49 but an article from Thomas Jefferson’s Hospital; Philadelphia also noted a 45% complication and 25% reoperation rate.50 The same study group in a different paper performed delayed knee arthroplasty for non-union in native knees.51 Although radiological outcome was satisfactory, 14% developed infections, 20% required manipulation for stiffness and 10% had aseptic loosening. Similarly, a study examining the treatment of failed internal fixation by knee arthroplasty is technically demanding. Although pain and functional outcomes were better, there was a 20% infection rate and had 33% failed due to loosening.52 Better functional results were obtained using the distal femoral replacement for distal fractures of the elderly.53 However, this group from Leipzig, Germany also had a 50% complication rate requiring surgical intervention (22% periprosthetic fracture, 10% infection rate, 5% patellar tendon rupture). Malvia et al.,53, 54 reported a better functional outcome score with fewer complications regarding fractures at both the tibia and femur, but with little homogeneity in their implant choice.
Appleton et al.,55 followed a similar patient cohort to ours, treated with three different hinged knee prostheses (2 with Kotz [Stryker-Howmedica, Newbury, UK], 38 with Guepar [Stryker-Howmedica] and 14 using the Stanmore [Biomet, Bridgend, UK]). A similar surgical technique was used, but cement was used to “fill up” any bony deficit, rather than endoprosthetic replacement. This study also had a high mortality rate − 3 patients within the first 10 days and 22 (42%) at one year. Mean survival after fracture was 1.7 years. Complications in the surviving group were 4 periprosthetic fractures and one patient suffering each vascular damage requiring amputation, quadriceps rupture, deep wound infection, haematoma and implant loosening.
Pearce et al.,56 also published their results of distal femoral replacement treated with either ORIF (4 patients) and another cohort again treated with a cemented Stanmore TKR (6 patients). While the results were again similar to or study with early mobilisation and few complications, the sample sizes was smaller in this group and the follow up only 6 months.
Although 23 years ago, Bell et al.,57 published their results following a similar cohort of patients treated with three types of hinged knee replacements in Type A and C fractures with three different cemented hinged implants. At 15 months, 11 had returned to pre-injury function and there was only one complication of a ruptured patellar tendon which was repaired.
Endoprosthesic Knee replacement is a viable treatment option for distal femoral fractures in the elderly or patients with similarly poor quality bone. It represents a good alternative to the more commonly used option of distal femoral ORIF/retrograde femoral nail, especially in those patients with radiological evidence of existing osteoarthritis and in the very distal fractures (within 50 mm) where reconstruction is difficult. It is also appropriate for the treatment of periprosthetic fractures.
This treatment option has tended to be ignored on the basis of implant cost and unfamiliarity with the technique and implants. The cost of implant is higher than that of ORIF but the time to start fully weight-bearing and therefore to discharge from hospital is less and therefore off-sets the cost. A large proportion of the extra cost relating to the prosthesis could potentially be justified. The technique, as explained above, is relatively simple to replicate. The desire to avoid resecting bone also seems to play a part in deciding on definitive treatment, particularly when there is no pre-existing prosthesis. However the bone is usually of very poor quality, meaning fracture healing is often slow, delaying mobility and restoration of knee function. This elderly group of patients find non- or partial weight-bearing often impossible and are then limited to bed-to-chair transfers or a wheelchair existence. The ability to weight-bear immediately postoperatively after EPR seems to help reduce complications when compared with ORIF (except retrograde intramedullary nailing). This would seem to be analogous with the principle of hip fracture surgery treatment, where the aim is to allow patients to begin full mobilisation as soon as possible, thereby reducing the risk of complications relating to immobility. We feel the benefits of early mobilisation and restoration of knee function are also reflected in the high post-operative Oxford Knee Scores (OKS).
The decision to proceed straight to EPR tends to be more difficult if there is no pre-existing prosthesis, and it is therefore not a Revision TKR procedure. The first patient in our EPR cohort who presented with a fracture in a native knee had Osteogenesis Imperfecta. He had a simple fall causing a catastrophic multi-fragmentary fracture that was deemed to be unreconstructable. Despite his young age (52yrs at the time of surgery), an EPR was felt to be his only appropriate treatment option and he is functioning extremely well with an OKS of 40 at 4 years.
One patient had previously been treated by ORIF which had failed (due to the screws in the femoral metaphysis cutting through the poor quality bone to become intra-articular). Revision to EPR took place at 150 days after the initial injury. She had lower than average post-operative knee scores compared with the rest of the EPR group (29). Following revision to EPR her time to discharge was also longer than average at 36, suggesting that the long period of relative immobility relating to their failed previous surgery compromised their definitive outcome. Similarly, patient AB had a failed period of conservative management (280 days). She subsequently took 28 days until discharge and her OKS was lower than the average.
Two patients in our group had bilateral fractures. One was 102yrs old with severe degenerative change in both knees. The right sided fracture was an entirely diaphyseal fracture (AO 33C) and was treated by the admitting surgeon with a retrograde femoral nail. The left-sided fracture was a low metaphyseal fracture that could not be maintained in good position in a plaster. Fixation would have been difficult as there was very little distal bone to accommodate screws. This would also have rendered the patient confined to bed/chair for an extended period, unable to weight-bear on either leg. An EPR was undertaken allowing full mobilisation on the left leg, expediting discharge at 28days. She remains alive at 18months post-surgery at 104yrs old. Her poor functional score (OKS 28) represents her age and limitation due to her delayed healing in the right knee with ongoing underlying osteoarthritis.
A second patient with bilateral fractures was treated by sequential EPRs in a single procedure. This 89 yr old female who was fully independent prior to the fall was therefore able to return to full mobilisation immediately post-surgery and was discharged back to her Residential home at 13 days. She suffered no complications and retains reasonable function with an OKS of 24 and 29.
The prosthesis used in our EPR group was the Endolink hinged TKR prosthesis. There are many different designs of hinged TKR available, often with multiple options for replacing bone following fracture or after resection of tumour. However, almost all of these designs require a minimum resection of 80 mm of distal femoral bone for implantation. Distal femoral fracture following a fall in the elderly usually occurs at the diaphyseal/metaphyseal junction as this seems to be the weakest area. This area is approximately 50 mm proximal to the joint line in most patients. Use of a prosthesis requiring a minimum bone resection of 80 mm is therefore undesirable, and makes the Endolink prosthesis, with its minimum resection of 50 mm (originally 45 mm) appealing. In our cohort only one patient required an 80 mm replacement block.
The longer time to theatre for this group (5.2 days) reflects the fact that a specialist knee surgeon is usually required to perform endoprosthetic replacement, whereas many surgeons are happy to undertake distal femoral ORIF. This minimal pre-operative delay does not seem to adversely affect outcome.
The limitations of this study are the small number of cases, but this reflects the relative rarity of this type of injury. The fact a specialist knee surgeon undertook the cases means it does not reflect the capabilities of the general orthopaedic community.
5. Conclusion
Distal Femoral Endoprosthetic Replacement offers a good alternative to traditional fixation techniques in elderly patients with low diaphyseal or metaphyseal fractures. It allows immediate full mobilisation and restoration of knee function, potentially reducing complications associated with post-operative immobility. Functional outcomes are good and although prosthetic costs are significantly higher than ORIF, we predict recovery and discharge are quicker and overall costs are comparable. The Endolink hinged TKR offers the option of smaller bone resection heights when compared to most other designs of EPR which corresponds favourably with the resection level required in this type of distal femoral fracture in the elderly.
Contributor Information
A. Atrey, Email: aatrey@me.com.
N. Hussain, Email: hussa1n@cmich.edu.
O. Gosling, Email: oliver.gosling@doctors.net.uk.
P. Giannoudis, Email: pgiannoudi@aol.com.
A. Shepherd, Email: shepherd.andrew@me.com.
S. Young, Email: steveyoung5@me.com.
J. Waite, Email: jonwaite@me.com.
References
- 1.Arneson T.J., Melton L.J., Lewallen D.G. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965–1984. ClinOrthop. 1988;234:188–194. [PubMed] [Google Scholar]
- 2.Kolmert L., Wulff K. Epidemiology and Treatment of Distal Femoral Fractures in Adults. Acta Orthop. 1982;53(6):957–962. doi: 10.3109/17453678208992855. [DOI] [PubMed] [Google Scholar]
- 3.Mahorner H.R., Bradburnr M. Surg Gynec Obst. 1933;56:1066. [Google Scholar]
- 4.Giles J.B., DeLee J.C., Heckman J.D. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am. 1982;64-A:864–870. [PubMed] [Google Scholar]
- 5.Pritchett J.W. Supracondylar fractures of the femur. Clin Orthop. 1984;184:173–177. [PubMed] [Google Scholar]
- 6.Sanders R., Regazzoni P., Ruedi T.P. Treatment of supracondylar-intracondylar fractures of the femur using the dynamic condylar screw. J Orthop Trauma. 1989;3:214–222. doi: 10.1097/00005131-198909000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Siliski J.M., Mahring M., Hofer H.P. Supracondylar-intercondylar fractures of the femur: treatment by internal fixation. J Bone Joint Surg Am. 1989;71-A:95–104. [PubMed] [Google Scholar]
- 8.Zehntner M.K., Marchesi D.G., Burch H., Ganz R. Alignment of supracondylar/intercondylar fractures of the femur after internal fixation by AO/ASIF technique. J Orthop Trauma. 1992;6:318–326. doi: 10.1097/00005131-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Kregor P.J., Stannard J.A., Zlowodski M., Cole P.A. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18:509–520. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Krettek C., Muller M., Miclau T. Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury. 2001;32(Suppl. 3):14–23. doi: 10.1016/s0020-1383(01)00180-2. [DOI] [PubMed] [Google Scholar]
- 11.Ricci A.R., Yue J.J., Taffet R. Less invasive stabilization system for treatment of distal femur fractures. Am J Orthop. 2004;33:250–255. [PubMed] [Google Scholar]
- 12.Danziger M.B., Caucci D., Zecher S.B., Segal D., Covall D.J. Treatment of inter-condylar and supracondylar distal femur fractures using the GSH supracondylar nail. Am J Orthop. 1995;24:684–690. [PubMed] [Google Scholar]
- 13.Helfet D.L., Lorich D.G. Retrograde intramedullary nailing of supracondylar femoral fractures. ClinOrthop. 1998;350:80–84. [PubMed] [Google Scholar]
- 14.Dunlop D.G., Brenkel I.J. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury. 1999;30:475–484. doi: 10.1016/s0020-1383(99)00136-9. [DOI] [PubMed] [Google Scholar]
- 15.Karpman R.R., Del Mar N.B. Supracondylar femoral fractures in the frail elderly: fractures in need of treatment. ClinOrthop. 1995;316:21–24. [PubMed] [Google Scholar]
- 16.Wähnert D., Hoffmeier K.L., von Oldenburg G. Internal fixation of type-C distal femoral fractures in osteoporotic bone. J Bone Joint Surg Am. 2010;92(June (6)):1442–1452. doi: 10.2106/JBJS.H.01722. [DOI] [PubMed] [Google Scholar]
- 17.Pekmezci M., McDonald E., Buckley J. Retrograde intramedullary nails with distal screws locked to the nail have higher fatigue strength than locking plates in the treatment of supracondylar femoral fractures: a cadaver-based laboratory investigation. Bone Joint J. 2014;96-B(January (1)):114–121. doi: 10.1302/0301-620X.96B1.31135. [DOI] [PubMed] [Google Scholar]
- 18.Heiney J.P., Barnett M.D., Vrabec G.A. Distal femoral fixation: a biomechanical comparison of trigen retrograde intramedullary (i.m.) nail, dynamic condylar screw (DCS), and locking compression plate (LCP) condylar plate. J Trauma. 2009;66(February (2)):443–449. doi: 10.1097/TA.0b013e31815edeb8. [DOI] [PubMed] [Google Scholar]
- 19.Wähnert D., Hoffmeier K., Fröber R. Distal femur fractures of the elderly?different treatment options in a biomechanical comparison. Injury. 2011;42(July (7)):655–659. doi: 10.1016/j.injury.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Murray D.W., Fitzpatrick R., Rogers K., Pandit H., Beard D.J., Carr A.J. The use of the Oxford hip and knee scores. J Bone Joint Surg [Br] 2007;89-B:1010–1014. doi: 10.1302/0301-620X.89B8.19424. [Dawson] [DOI] [PubMed] [Google Scholar]
- 21.Miller T.T. Imaging of knee arthroplasty. Europ. J Radiology MayVolume. 2005;54(Issue 2):164–177. doi: 10.1016/j.ejrad.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 22.Petrou G., Petrou G., Tilkeridis C. Medium-term results with a primary cemented rotating-hinge total knee replacement; a 7- to 15-year follow up. J Bone Joint Surg [Br] 2004;86-B:813–817. doi: 10.1302/0301-620x.86b6.14708. [DOI] [PubMed] [Google Scholar]
- 23.Joshi N., Navarro-Quilis A. Is there a place for rotating-Hinge arthroplasty in knee revision surgery for aseptic loosening? The Journal of Arthroplasty. 2008;23(No. 8) doi: 10.1016/j.arth.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 24.Pradhan N.R., Bale L., Kay P., Porter M.L. Salvage revision total knee replacement using the Endo-Model® rotating hinge prosthesis. The Knee. 2004;11(December 6):469–473. doi: 10.1016/j.knee.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Sanguineti F., Mangano T., Formica M., Franchin F. Total knee arthroplasty with rotating-hinge Endo-Model prosthesis: clinical results in complex primary and revision surgery. Arch Orthop Trauma Surg. 2014;134(November (11)):1601–1607. doi: 10.1007/s00402-014-2061-1. [DOI] [PubMed] [Google Scholar]
- 26.Hilgen V., Citak M., Vettorazzi E. 10-year results following impaction bone grafting of major bone defects in 29 rotational and hinged knee revision arthroplasties: a follow-up of a previous report. Acta Orthop. 2013;84(August (4)):387–391. doi: 10.3109/17453674.2013.814012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gudnason A., Milbrink J., Hailer N.P. Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg. 2011;131(November (11)):1601–1607. doi: 10.1007/s00402-011-1330-5. [DOI] [PubMed] [Google Scholar]
- 28.Petrou G.1, Petrou H., Tilkeridis C. Medium-term results with a primary cemented rotating-hinge total knee replacement. A 7- to 15-year follow-up. J Bone Joint Surg Br. 2004;86(August (6)):813–817. doi: 10.1302/0301-620x.86b6.14708. [DOI] [PubMed] [Google Scholar]
- 29.Plutat J., Friesecke C., Klüber D. [Endo-Model hinged prosthesis–a model with a future? Experiences and outcome after 20 years use] Orthopade. 2000;29(Suppl. 1):S56–S58. doi: 10.1007/pl00003688. [June (article in German −translated by AA)] [DOI] [PubMed] [Google Scholar]
- 30.Giles J.B., DeLee J.C., Heckman J.D., Keever J.E. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am. 1982;64-A:864–870. [PubMed] [Google Scholar]
- 31.Pritchett J.W. Supracondylar fractures of the femur. Clin Orthop. 1984;184:173–177. [PubMed] [Google Scholar]
- 32.Sanders R., Regazzoni P., Ruedi T.P. Treatment of supracondylar-intracondylar fractures of the femur using the dynamic condylar screw. J Orthop Trauma. 1989;3:214–222. doi: 10.1097/00005131-198909000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Siliski J.M., Mahring M., Hofer H.P. Supracondylar-intercondylar fractures of the femur: treatment by internal fixation. J Bone Joint Surg Am. 1989;71-A:95–104. [PubMed] [Google Scholar]
- 34.Zehntner M.K., Marchesi D.G., Burch H., Ganz R. Alignment of supracondylar/intercondylar fractures of the femur after internal fixation by AO/ASIF technique. J Orthop Trauma. 1992;6:318–326. doi: 10.1097/00005131-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Kregor P.J., Stannard J.A., Zlowodski M., Cole P.A. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18:509–520. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Krettek C., Muller M., Miclau T. Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury. 2001;32(Suppl. 3):14–23. doi: 10.1016/s0020-1383(01)00180-2. [DOI] [PubMed] [Google Scholar]
- 37.Ricci A.R., Yue J.J., Taffet R. Less invasive stabilization system for treatment of distal femur fractures. Am J Orthop. 2004;33:250–255. [PubMed] [Google Scholar]
- 38.Danziger M.B., Caucci D., Zecher S.B., Segal D., Covall D.J. Treatment of inter-condylar and supracondylar distal femur fractures using the GSH supracondylar nail. Am J Orthop. 1995;24:684–690. [PubMed] [Google Scholar]
- 39.Khursheed O., Wani M.M., Rashid S. Results of treatment of distal extra: articular femur fractures with locking plates using minimally invasive approach-experience with 25 consecutive geriatric patients. Musculoskelet Surg. 2014;(December 14) doi: 10.1007/s12306-014-0343-y. [DOI] [PubMed] [Google Scholar]
- 40.Hou Z., Bowen T.R., Irgit K. Locked plating of periprosthetic femur fractures above total knee arthroplasty. J Orthop Trauma. 2012;26(July (7)):427–432. doi: 10.1097/BOT.0b013e31822c050b. [DOI] [PubMed] [Google Scholar]
- 41.Marsh J.L., Slongo T.F., Agel J. Fracture and dislocation classification compendium: 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Ortho Trauma. 2007;21:S1–133. doi: 10.1097/00005131-200711101-00001. [Suppl.] [DOI] [PubMed] [Google Scholar]
- 42.Brumback R.J., Toal T.R., Jr., Murphy-Zane M.S. Immediate weight-bearing after treatment of a comminuted fracture of the femoral shaft with a statically locked intramedullary nail. J Bone Joint Surg Am. 1999;81(November (11)):1538–1544. doi: 10.2106/00004623-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Arazi M., Ogun T.C., Oktar M.N. early weight-bearing after statically locked reamed intramedullary nailing of comminuteed distal femoral fractures: is it a safe procedure? J Trauma. 2001;50(April (4)):711–716. doi: 10.1097/00005373-200104000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Rorabeck C.H., Taylor J.W. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am. 1999;30(April (2)):209–214. doi: 10.1016/s0030-5898(05)70075-4. [DOI] [PubMed] [Google Scholar]
- 45.Della Rocca G.J., Leung K.S. Pape HC Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011;25(Suppl. 2):S66–S70. doi: 10.1097/BOT.0b013e31821b8c28. June. [DOI] [PubMed] [Google Scholar]
- 46.Thompson S.M., Lindisfarne E.A., Bradley N., Solan M. Periprosthetic supracondylar femoral fractures above a total knee replacement: compatibility guide for fixation with a retrograde intramedullary nail. J Arthroplasty. 2014;29(August (8)):1639–1641. doi: 10.1016/j.arth.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 47.Gliatis J., Megas P., Panagiotopoulos E., Lambiris E. Midterm results of treatment with a retrograde nail for supracondylar periprosthetic fractures of the femur following total knee arthroplasty. J Orthop Trauma. 2005;19(March (3)):164–170. doi: 10.1097/00005131-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Hernigou P., Poignard A., Manicom O., Chabane-Sari M.A. Treatment of fractures of the distal femur on total knee arthroplasty. Rev Chir Orthop Reparatrice Appar Mot. 2016 doi: 10.1016/s0035-1040(06)75700-2. [DOI] [PubMed] [Google Scholar]
- 49.Deshmukh A.J., Thakur R.R., Rasquinha V.J., Rodriguez J.A. Femoral revision arthroplasty for su type 3 supracondylar periprosthetic knee fractures. J Knee Surg Sep. 2014;24 doi: 10.1055/s-0034-1390029. [DOI] [PubMed] [Google Scholar]
- 50.Mortazavi S.M., Kurd M.F., Bender B. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty. 2010;25(August (5)):775–780. doi: 10.1016/j.arth.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 51.Papadopoulos E.C., Parvizi J., Lai C.H., Lewallen D.G. Total knee arthroplasty following prior distal femoral fracture. Knee. 2002;9(December (4)):267–274. doi: 10.1016/s0968-0160(02)00046-7. [DOI] [PubMed] [Google Scholar]
- 52.Saleh K.J., Sherman P., Katkin P. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. J Bone Joint Surg Am. 2001;83-A(August (8)):1144–1148. doi: 10.2106/00004623-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 53.Rosen A.L., Strauss E. Primary total knee arthroplasty for complex distal femur fractures in elderly patients. Clin Orthop Relat Res. 2004;425:101–105. doi: 10.1097/01.blo.0000132466.65220.62. [DOI] [PubMed] [Google Scholar]
- 54.Malviya A., Reed M.R., Partington P.F. Acute primary total knee arthroplasty for peri-articular knee fractures in patients over 65 years of age. Injury. 2011;42(November (1)):1368–1371. doi: 10.1016/j.injury.2011.06.198. [DOI] [PubMed] [Google Scholar]
- 55.Appleton P., Moran M., Houshian S., Robinson C.M. Distal Femoral treated by hinged total knee replacement in elderly patients. JBJS (Br) 2006;88:1065. doi: 10.1302/0301-620X.88B8.17878. [DOI] [PubMed] [Google Scholar]
- 56.Pearse E.O., Klass B., Bendall S., Railton G.T. Stanmore total knee replacement versus internal fixation for supracondylar fractures of the distal femur in elderly patients. Injury. 2005;36(January (1)):163–168. doi: 10.1016/j.injury.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 57.Bell K.M., Johnstone A.L., Court-Brown C.M., Hughes S.P. Primary knee arthroplasty for distal femoral fractures in elderly patients. JBJS (Br) 1992;74(May (3)):400–402. doi: 10.1302/0301-620X.74B3.1587887. [DOI] [PubMed] [Google Scholar]


