Abstract
This study was designed to examine the contribution of multiple risk factors to early internalizing problems and to investigate whether family and ecological context moderated the association between child temperament and internalizing outcomes. A sample of 1,202 mothers of 2- and 3-year-old children completed a survey of child social-emotional functioning, family environment, and violence exposure. Child temperament, maternal affective symptoms, and family expressiveness were associated with child anxiety and depression problems. Violence exposure was related only to child anxiety. When maternal affective symptoms were elevated, inhibited girls but not boys were rated as more anxious and youngsters with heightened negative emotionality were rated as more depressed. Family expressiveness moderated the association between inhibited temperament and anxiety symptoms.
For 2- and 3-year-olds, fear of monsters under the bed or sadness when a beloved toy is lost are most often normative, transient feelings ameliorated through self-regulation or guidance from parents. However, not all experiences of fear, worry, sadness, and irritability are normative in early childhood. Even young children can have clinically concerning symptoms along the internalizing dimension (Carter, Briggs-Gowan, & Davis, 2004; Egger & Angold, 2006). Yet less attention has been paid to the early manifestations of internalizing than externalizing problems, and children suffering from internalizing problems are often underidentified because their symptoms tend to be subtler and less disruptive (Warren, 2004).
Advances in early childhood assessment, although still largely dependent on parental reports, make it feasible to study internalizing symptoms in young children using developmentally-sensitive, psychometrically-sound behavior rating measures (Achenbach, 1992; Carter, Briggs-Gowan, Jones, & Little, 2003). Maternal-reported internalizing problems show moderate stability (r =.38) from ages 3 to 7 (van der Valk, van den Oord, Verhulst, & Boomsma, 2003) and from childhood through adolescence (Bosquet & Egeland, 2006). Mesman and Koot (2001) also found that 2- to 3-year-olds exhibiting elevated internalizing symptoms were 3 times more likely than other youngsters to have internalizing disorders at age 10 to 11.
The internalizing domain encompasses anxiety and depression. Anxiety disorders are among the most frequently occurring child psychiatric problems with prevalence estimates approaching 10% among preschool children. Depression is less often diagnosed in early childhood but prevalence estimates up to 2% for pre-schoolers using criteria modified to be age-appropriate have been reported (Egger & Angold, 2006; Luby et al., 2002). There is also evidence of elevated anxiety and depressive symptoms in 1- to 2-year-olds (Carter et al., 2003). Although sometimes thought of as transient, elevated anxiety and depressive symptoms persist in young children (Briggs-Gowan, Carter, Bosson-Heenan, Guyer, & Horwitz, 2006). In older children, anxiety symptoms predict anxiety disorders, depression, and externalizing disorders in adolescence (Bittner et al., 2007). Anxiety and depression are often comorbid (Moffit et al., 2007), suggesting unclear boundaries between these dimensions. However, differentiation into distinct anxiety syndromes as well as between anxiety and depressive problems has been supported (Carter et al., 2003; Sterba, Egger, & Angold, 2007).
RISK FACTORS FOR EARLY CHILDHOOD ANXIETY AND DEPRESSION
Research on early emerging internalizing problems has often employed a broadband approach (e.g., Bongers, Koot, van der Ende, & Verhulst, 2003; Sterba, Prinstein, & Cox, 2007) that may limit our understanding of pathways and associated risk factors for anxiety and depression. Consistent with an ecological-transactional perspective (Cicchetti & Toth, 1997), the etiology of anxiety and depressive symptoms is likely to be multi-determined with involvement of child factors such as temperament and contextual factors such as family environment.
Child Factors
Temperament and psychopathology, although difficult to disentangle at early ages, can be conceptualized as overlapping but distinct. Even extreme temperamental styles arise in specific contexts (e.g., novelty) and are associated with less pervasive dysregulation and impairment than manifestations of psychopathology (Goldsmith & Lemery, 2000; Lahey, 2004). Furthermore, some but not all individuals classified as temperamentally vulnerable go on to develop disorders (Biederman et al., 2001; Schwartz, Snidman, & Kagan, 1999), suggesting that temperamental risk is not necessarily synonymous with disorder.
Behavioral inhibition has been defined as a consistent tendency to display fear or withdrawal in novel or unfamiliar situations (Kagan, 1984). Findings from prospective longitudinal studies indicate that behavioral inhibition in preschool increases the likelihood that a child will develop an anxiety disorder (Biederman et al., 2001; Schwartz et al., 1999) but also suggest that behavioral inhibition is related to later depression (Rosenbaum et al., 2000). Negative emotionality is another commonly identified temperament dimension that can be distinguished from fear/behavioral inhibition (Rothbart & Posner, 2006) and has been documented as a risk factor for internalizing and externalizing problems (Prior, Smart, Sanson, Pedlow, & Oberklaid, 1992; Shaw, Keenan, Vondra, Delliquadri, & Giovannelli, 1997). Behavioral inhibition and negative emotionality may play important roles in the development of internalizing problems. In a recent prospective study, child shyness akin to behavioral inhibition demonstrated higher stability than contextual risk factors (family adversity, maternal distress, social support) from ages to 9. Emotionality, which also showed stability, was the strongest predictor of internalizing problems in adolescence (Karevold, Roysamb, Ystrom, & Mathiesen, 2009).
The consistent sex differences in internalizing problems found among older children and adolescents generally have not been evident in younger children (Bongers et al., 2003; Bosquet & Egeland, 2006). Yet a few studies have identified subtle or complex patterns of sex differences. For example, in a large, community sample, 1- and 2-year-old girls exhibited greater anxiety but not depressive problems than boys (Carter et al., 2003). In an investigation of internalizing problems from ages 2 to 11 using latent growth mixture modeling, almost twice as many girls as boys were classified as elevated-stable and almost twice as many boys as girls were classified as decreasing or increasing (Sterba, Prinstein, et al., 2007). Also, self-reported postpartum maternal depression symptoms for girls and maternal anxiety for boys were associated with elevated internalizing problems at age 2. These mixed results highlight that key questions remain as to whether or not early vulnerabilities and developmental processes underlie later sex differences in internalizing psychopathology.
Family Environment and Ecological Factors
Several recent studies indicate that in early childhood maternal anxiety/depression is a risk factor for elevated internalizing problems and increasing trajectories (Bayer, Hiscock, Ukoumunne, Price, & Wake, 2008; Feng, Shaw, & Silk, 2008; Sterba, Prinstein, et al., 2007). The transmission of anxious and depressive symptoms from parent to child may reflect both shared genetic vulnerability and problematic parenting. Anxiety disorders aggregate in families, and children of anxious parents have a sevenfold risk for anxiety disorders (Turner, Beidel, & Costello, 1987). Similar trends are evident for depressive disorders, with a three-fold risk for children of depressed parents (Weissman, Gammon, John, & Merikangas, 1987). Twin studies provide evidence of moderate heritability for anxiety and depression as well as environmental contributions (Eley et al., 2003; Saudino, Carter, Purper-Ouakil, & Gorwood, 2008). It is unclear if anxiety and depressive symptoms in parents show specificity in transmission. Twin research points to a common genetic vulnerability for anxiety and depression (Eley & Stevenson, 1999), suggesting that conferred risk may be nonspecific.
Affective disorders can interfere with parenting. Anxious and depressed parents may expose children to more frequent, intense displays of negative emotions; model anxious and depressive reactions; and respond to child emotional displays in a manner that maintains or amplifies rather than diminishes emotional arousal (Goodman & Gotlib, 1999; Wood, McLeod, Sigman, Hwang, & Chu, 2003). Observational evidence suggests that parents with anxiety disorders tend to be more controlling and convey less warmth than parents without anxiety disorders (Dumas, LaFreniere, & Serketich, 1995) and to model reactions such as catastrophizing (Moore, Whaley, & Sigman, 2004). Depressed mothers have been rated as less engaged, more authoritarian, and more rejecting (e.g., McLeod, Weisz, & Wood, 2007; Pelaez, Field, Pickens, & Hart, 2008) and less responsive to preschoolers’ expressions of distress (Shaw et al., 2006).
Other aspects of the family environment and broader ecology may also contribute to child anxiety and depression. Children in families that restrict emotional expressiveness may have less elaborated emotional understanding and learn to suppress both positive and negative emotions (Eisenberg, Cumberland, & Spinrad, 1998). Overcontrol of negative emotions and dampening of positive emotions could heighten negativity and lead to less adaptive regulation behaviors such as avoidance, thereby increasing risk for internalizing problems. Empirical work linking family expressiveness and internalizing problems is still limited. However, in one study, anxiety-disordered children and their mothers, in comparison to their nondisordered counterparts, rated the family environment as less expressive (Suveg, Zeman, Flannery-Schroeder, & Cassano, 2005). Similarly, in an emotion discussion task, mothers of children with anxiety disorders spoke less frequently than their children, used fewer positive emotion words, and generally discouraged discussion of emotions more than mothers of children without anxiety disorders.
Exposure to family conflict, and marital conflict in particular, has been shown to predict internalizing problems (Cummings & Davies, 2002). Most research has been done with older children, but toddlers also respond to marital conflict (Easterbrooks, Cummings, & Emde, 1994) and mother–child conflict (Laible, Panfile, & Makariev, 2008) with reactions that impact adjustment negatively. Although exposure to violence is studied only rarely in young children, evidence suggests that, like family conflict, this exposure increases the risk of adjustment and internalizing problems (McDonald, Jouriles, Briggs-Gowan, Rosenfeld, & Carter, 2007; Shahinfar, Fox, & Leavitt, 2000). In a recent study, elevated risk for anxiety, particularly separation anxiety, but not depression was identified among violence exposed toddlers and preschoolers (Briggs-Gowan et al., 2009). Family conflict and exposure to violence could contribute to the early manifestations of both anxiety and depression because these experiences represent stressful life events linked to a negative emotional climate (Luby, Belden, & Spitznagel, 2006; Vasey & Dadds, 2001). Alternatively, violence exposure may more specifically relate to early anxiety because it heightens susceptibility to an attentional bias for threat (Waters, Mogg, Bradley, & Pine, 2008) and decreases a sense of control (Chorpita & Barlow, 1988).
CHILD TEMPERAMENT AND INTERNALIZING OUTCOMES: ASSOCIATIONS MODERATED BY FAMILY AND ECOLOGICAL FACTORS?
It is possible that the same risk factor poses differential effects depending on specific child attributes. In fact, behavioral inhibition and negative emotionality have been linked to internalizing problems for some but not all children, raising the question of whether interactions between temperament and environment contribute to internalizing outcomes. Research has most often focused on child temperament as a moderator of the associations between maternal psychopathology and/or parenting practices and child problems (Rothbart & Posner, 2006). However, developmental models of internalizing problems posit that parenting practices may shape temperamental risk (Rapee, 2002). A small body of work has demonstrated that children with temperamental vulnerabilities such as high reactivity in infancy (i.e., considered an antecedent of behavioral inhibition) whose mothers are high on anxious/depressed symptomatology (Degnan, Henderson, Fox, & Rubin, 2008) or whose mothers are less sensitive and engaged (Crockenberg & Leerkes, 2006) show elevated anxiety problems. The potential moderating role of other environmental factors such as family expressiveness, conflict, and violence exposure is understudied despite theoretical relevance deriving from the role of emotion regulation and chronic stress in the development of internalizing problems.
THE PRESENT STUDY
The current study was designed to examine the contribution of child, family, and ecological risk factors to child anxiety and depression symptoms and to empirically test whether associations between child temperamental risk and child anxiety and depression symptoms would be moderated by family and ecological risk factors. Specific risk factors included in our models are child temperament (i.e., inhibition to novelty and negative emotionality), child sex, maternal affective symptoms, family conflict and family expressiveness, and violence exposure. It was hypothesized that child temperament, family, and ecological risk factors would be directly related to both child anxiety and depressive symptoms. It was also expected that maternal affective symptoms and family expressiveness would moderate the association between inhibition to novelty and child anxiety. Examination of whether the associations between temperamental risk and child anxiety would be moderated by family conflict and violence exposure and whether the associations between temperamental risk and child depression would be moderated by family and ecological factors were exploratory. Patterns of association and moderation were expected to differ minimally for boys and girls.
METHOD
Participants
Participants were from the second annual survey of a longitudinal epidemiologic healthy birth cohort sample. An age- and sex-stratified sample was randomly selected from birth records provided by the State of Connecticut Department of Public Health for children living in the New Haven–Meriden Standard Metropolitan Statistical Area (see Briggs-Gowan, Carter, Moye Skuban, & McCue Horwitz, 2001). Children were ineligible if they were premature, were low birth weight, or had serious birth complications (n =675); had a sibling who was sampled (n =277); were deceased (n =4); or were adopted. A random sample of 1,788 was drawn from 7,433 eligible children. In addition, the parent had to participate in English, have custody, and reside in the state. These criteria were not met by 183 children, 112 could not be located to determine eligibility, and 2 were excluded due to severe parental illness. Compared with eligible families, ineligible families (n =297) were significantly lower in child birth weight (Cohen’s d =.18), paternal age (Cohen’s d =.27) and maternal age (Cohen’s d =.41), maternal education (Cohen’s d =.31), years at the birth address (Cohen’s d =.34), and more likely to be of minority ethnicity (t =2.84–6.26, p <.01). The effect sizes for these differences were within the range generally considered to be very small (Cohen’s d <.20) or small (Cohen’s d =.20–.41) although the effect size for maternal age reached the upper limit of this range (Cohen, 1988). There were no differences in gestational age, paternal education, or child sex.
In the 2nd year of the larger study, 1,223 parents of 2- and 3-year-olds participated (83% response). The majority also participated in the 1st year of data collection (n =1,174) with 49 eligible families joining the study in the 2nd year. Seventeen children were deemed ineligible after participation due to the identification of serious developmental disabilities. In addition, data on 4 children were considered invalid and, therefore, excluded. Participants and eligible nonparticipants (n =162) were comparable on all birth record variables (p >.05). The final sample size was 1,202, which is the sample used in all analyses.
The mean age of children was 36.8 months (SD =7.2 months) with relatively equal numbers of girls (51.8%) and boys (48.2%). Further, 63.8% of the toddlers were White/Caucasian, 18.0% were Black/African American, 5.7% Hispanic/Latino, 8.6% Black/Hispanic, 2.4% Asian/Asian American, and 1.5% identified as “Other.” Approximately 15% of families reported income below the poverty line (14.9%) and 20% lived in single-parent homes. This sample was comparable to families with young children in the region according to the 1990 Census (i.e., 77% Caucasian, 19% single-parent homes, 14% living in poverty).
Procedure
In the first 2 years of the study, parents were mailed a letter describing the study, followed 1 week later by a survey booklet and book as a gift for the child. Staff members subsequently telephoned parents and visited homes to address questions and/or concerns and encourage participation. Parents received $25 for completing each early childhood survey. All procedures were approved by the Institutional Review Boards at two universities. Informed consent was obtained from all participants.
Measures
Child temperament and internalizing symptoms
The Infant-Toddler Social and Emotional Assessment (ITSEA) is a 166-item parent-report measure of social-emotional/behavioral problems and competencies in 1- to 3-year-olds (Carter & Briggs-Gowan, 2006; Carter et al., 2003). In this study, the Inhibition to Novelty and Negative Emotionality subscales were employed as separate measures of child temperament. There was a significant but low correlation (r =.23, p <.001) between these two subscales. The General Anxiety and Depression/Withdrawal subscales were used to characterize early anxiety and depression problems, respectively. There was a moderate correlation between these two subscales (r =.44, p <.001). Item examples from these subscales include (a) Inhibition to Novelty: “Is quiet or less active in new situations” and “Is shy with new children,” (b) Negative Emotionality: “Is impatient or easily frustrated” and “Is hard to soothe when upset,” (c) General Anxiety: “Seems nervous, tense or fearful” and “Worries a lot or is very serious,” and (d) Depression/Withdrawal: “Seems very unhappy or sad without any reason” and “Has less fun than other children.” All ITSEA items are rated on a 3-point scale from not true/rarely to very true/often. Internal consistency of these scales for the study sample was adequate. Cronbach’s alpha was .77 for Inhibition to Novelty, .84 for Negative Emotionality, .69 for General Anxiety, and .77 for Depression/Withdrawal. All scales have demonstrated acceptable test–retest reliability (Intraclass Correlation Coefficients =0.64–0.80) and interrater reliability (0.43–0.73; Carter et al., 2003).
Maternal affective symptoms
A Maternal Affective Symptoms composite was created by taking the mean of the standardized Center for Epidemiologic Studies Depression Inventory (CES-D) and Beck Anxiety Inventory (BAI) scores. The CES-D (Radloff, 1977) is a 20-item self-report checklist that assesses adult depressive symptoms. It has demonstrated adequate internal consistency (α~=.84–.90) and test–retest reliability (r~=.51–.67). The BAI (Beck, Epstein, Brown, & Steer, 1988) is a self-report measure that assesses how much respondents have been bothered by symptoms of anxiety. It has 21 items with answers given on a 4-point scale of 0 (not at all) to 3 (severely). Internal consistency (alpha) is .92 and 1-week test–retest correlation is .75. These measures also showed adequate internal consistency for the present study sample (BAI, α~=.88 and CES-D, α~=.90) and were significantly correlated (r =.64, p <.001).
Family environment
The Family Environment Scale (FES) Expressiveness and Conflict subscales were used (Moos & Moos, 1986). These subscales measure disruptions in family function with acceptable reliability and validity. The nine-item Expressiveness subscale taps the degree to which family members directly express their emotions to one another and has adequate internal consistency (α~=.69). The nine-item Conflict subscale measures the degree to which the family is characterized by anger and conflict and has adequate internal consistency (α~=.75). In the current sample, internal consistency for the FES Expressiveness (α~=.50) and FES Conflict scales (α~=.75) was lower than originally reported (Moos & Moos, 1986).
Violence exposure
Respondents rated their child’s exposure to 14 stressful events (Carter & Briggs-Gowan, unpublished scale, 1998). Three of these were summed to create an index of Violence Exposure: (a) seen violence in your neighborhood; (b) seen someone use a weapon to threaten or hurt a family member; and (c) seen someone hit, push, or kick a family member.
Data Analyses
We used multiple-group structural equation models to estimate the effects of child temperament (i.e., ITSEA Inhibition to Novelty and Negative Emotionality), family risk factors (i.e., Maternal Affective Symptoms, FES Family Expressiveness and Family Conflict), and Violence Exposure on child anxiety and depressive symptoms (ITSEA Generalized Anxiety and Depression/Withdrawal). An important advantage of this method is that it is possible to test the relationship between risk factors and multiple symptom outcomes rather than testing the relationships between risk factors and a single outcome (as in regression). Multiple-group analysis allowed for invariance testing across groups for models as well as for individual parameters. Child anxiety and depression random errors were estimated with a mean of zero, and independent and normally distributed, and had constant variances across levels of the independent variables. These errors were allowed to be correlated.
The multiple-group model enabled us to estimate parameters independently for boys and girls and to use chi-square difference tests to compare the patterns of association for boys and girls. This test assesses whether a model in which the paths for boys and girls were constrained to be identical (constrained model) fit the data worse than the model in which these paths are allowed to vary (the unconstrained model). If the chi-square difference statistic is significant, it can be inferred that the pathways for boys and girls are significantly different, and the unconstrained results are interpreted. In the constrained models, the estimated error variances and the correlation between these errors were allowed to vary by sex.
We estimated several different models to evaluate our hypotheses about direct and interactive effects of risk factors. First, we estimated a baseline model that included all child, family, and ecological risk factors. We then estimated a series of models that assessed whether the effects of temperamental risk factors on children’s anxiety and depressive symptoms were moderated by family and ecological risk factors. All independent variables were mean centered to reduce multicollinearity (Aiken & West, 1991). Due to the number of comparisons tested, only relationships with a p value of .01 or smaller were reported as statistically significant. To adjust for differences in sampling probability, nonresponse, and loss to follow-up during the longitudinal study, statistical weights were applied in all analyses. Weights were calculated with sociodemographic background information from birth records (e.g., parental age, education and race) and infant birth status (e.g., birth weight and gestational age).
RESULTS
Baseline Model With Direct Effects
Table 1 displays estimated coefficients for the model that includes only the direct effects of the child, family, and ecological risk factors. Both the constrained and unconstrained models are displayed. The chi-square difference test for the model with direct effects, Δχ2(12) =11.14, p =.517, indicated that associations between risk factors and depression and anxiety symptoms in early childhood are similar for boys and girls. Consequently, we discuss only estimates from the constrained model. Both Inhibition to Novelty and Negative Emotionality were positively associated with both child anxiety and depression symptoms. Maternal Affective Symptoms were also positively associated with both child anxiety and depression. In contrast to these nonspecific effects, Violence Exposure was associated positively with anxiety but not depression, whereas Family Expressiveness was associated negatively with depression but not anxiety. Family Conflict was not significantly associated with child anxiety or depression symptoms.
TABLE 1.
Standardized Parameter Estimates from Unconstrained and Constrained Multiple-Group Structural Equation Models Predicting to Anxiety and Depression Symptoms
| Variable | Unconstrained
|
Constrained
|
||||
|---|---|---|---|---|---|---|
| Girls
|
Boys
|
|
||||
| Depression (SE) | Anxiety (SE) | Depression (SE) | Anxiety (SE) | Depression (SE) | Anxiety (SE) | |
| Inhibition to Novelty | 0.037 (0.016) | 0.093** (0.023) | 0.032 (0.015) | 0.081** (0.022) | 0.033** (0.011) | 0.086** (0.016) |
| Negative Emotionality | 0.219** (0.024) | 0.269** (0.034) | 0.172** (0.023) | 0.192** (0.035) | 0.195** (0.017) | 0.231** (0.024) |
| Family Expressiveness | −0.008 (0.005) | 0.000 (0.007) | −0.018** (0.004) | −0.012 (0.006) | −0.014** (0.003) | −0.007 (0.004) |
| Family Conflict | −0.003 (0.005) | −0.011 (0.007) | 0.004 (0.004) | −0.004 (0.007) | 0.001 (0.003) | −0.007 (0.005) |
| Maternal Affect | 0.033** (0.010) | 0.049** (0.014) | 0.028** (0.008) | 0.044** (0.012) | 0.029** (0.006) | 0.045** (0.009) |
| Violence Exposure | 0.055** (0.020) | 0.077* (0.028) | −0.005 (0.022) | 0.047 (0.032) | 0.027 (0.015) | 0.060* (0.021) |
|
| ||||||
| Girls | Boys | |||||
|
| ||||||
| Correlations | ||||||
| Anxiety and Depression | 0.016** (0.002) | 0.009 ** (0.002) | 0.016** (0.002) | 0.010** (0.002) | ||
| Residual Variances | ||||||
| Depression | 0.032** (0.002) | 0.025 ** (0.002) | 0.032 ** (0.002) | 0.026** (0.002) | ||
| Anxiety | 0.065** (0.004) | 0.056 ** (0.003) | 0.065 ** (0.004) | 0.056** (0.003) | ||
| Δχ2 | — | 11.14 | ||||
| df | — | 12 | ||||
| p | — | .517 | ||||
| N | 579 | 539 | 579 | 539 | ||
Note: SE =standard error.
p <.01.
p <.001.
Moderator Models
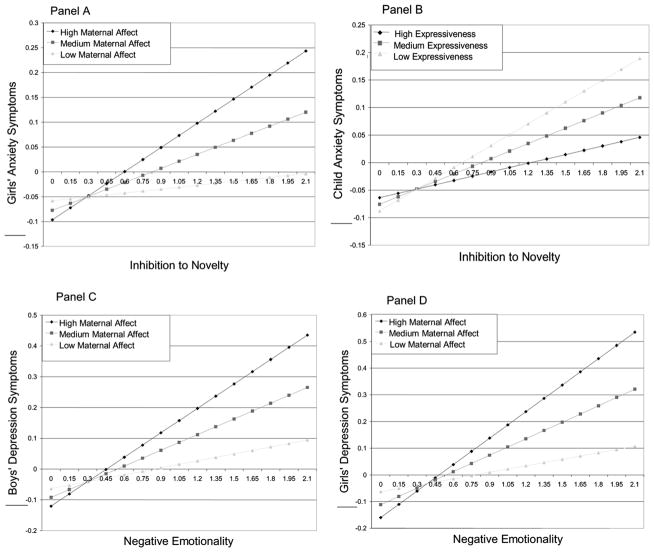
To test the hypothesis that child temperamental risk factors on child anxiety and depression symptoms are moderated by family and ecological risk factors, a series of models (see Table 2 and Figure 1) examining potential interactions were run. To decompose significant interactions, the moderating variable was examined at the mean and at one standard deviation above and below the mean. Chi-square difference tests indicated that there were sex differences in patterns of association between Maternal Affective Symptoms and early childhood anxiety and depression, Δχ2(10) =18.55, p =.046, but not for Family Conflict, Family Expressiveness, or Violence Exposure. Therefore, we report findings (see Table 2) from the model that allowed estimated coefficients for boys and girls to differ for Maternal Affective Symptoms and report results from constrained models for all other risk factors.
TABLE 2.
Standardized Parameter Estimates from Multiple Group Structural Equation Models of Child Temperament with Maternal Affect, Family Environment, and Violence Exposure Predicting to Child Anxiety and Depression Symptoms
| Variable | Maternal Affect
|
Family Environment
|
Violence Exposure
|
|||||
|---|---|---|---|---|---|---|---|---|
| Anxiety
|
Depression
|
Anxiety (SE) | Depression (SE) | Anxiety (SE) | Depression (SE) | |||
| Girls (SE) | Boys (SE) | Girls (SE) | Boys (SE) | |||||
| Inhibition to Novelty (IN) | .09** (.02) | .08** (.02) | .04* (.02) | .03 (.01) | .09** (.02) | .04** (.01) | .10** (.02) | .04** (.01) |
| Negative Emotionality (NE) | .26** (.03) | .20** (.03) | .21** (.02) | .17** (.02) | .27** (.02) | .20** (.02) | .27** (.02) | .23** (.02) |
| Maternal affect | .04* (.01) | .05** (.01) | .02 (.01) | .03* (.01) | ||||
| Maternal Affect × IN | .07* (.02) | −.04 (.02) | .01 (.02) | −.01 (.02) | ||||
| Maternal Affect ×NE | .04 (.03) | .04 (.03) | .14** (.02) | .10** (.02) | ||||
| Family Expressiveness | −.01* (.00) | −.02** (.00) | ||||||
| Family Expressiveness × IN | −.02* (.01) | −.01 (.01) | ||||||
| Family Expressiveness × NE | .01 (.01) | .00 (.01) | ||||||
| Family Conflict | .00 (.00) | .00 (.00) | ||||||
| Family Conflict × IN | −.01 (.01) | −.02 (.01) | ||||||
| Family Conflict × NE | −.01 (.01) | .04** (.01) | ||||||
| Violence exposure | .08** (.02) | .05* (.02) | ||||||
| Violence Exposure × IN | .03 (.04) | .02 (.03) | ||||||
| Violence Exposure × NE | −.02 (.01) | −.03** (.01) | ||||||
|
| ||||||||
| Girls | Boys | Girls | Boys | Girls | Boys | |||
|
| ||||||||
| Correlations | ||||||||
| Depression and Anxiety | .02** (.00) | .01** (.00) | .02** (.00) | .01** (.00) | .02** (.00) | .01** (.00) | ||
| Residual Variances | ||||||||
| Depression | .03** (.00) | .03**(.00) | .03** (.00) | .03** (.00) | .03** (.00) | .03** (.00) | ||
| Anxiety | .07** (.00) | .06** (.00) | .07** (.00) | .06** (.00) | .07** (.00) | .06** (.00) | ||
| N | 603 | 565 | 593 | 546 | 588 | 542 | ||
| Δχ2 (p) | 18.55 (.046) | 11.78 (.759) | 7.34 (.693) | |||||
| df | 10 | 16 | 10 | |||||
Note: SE =standard error.
p <.01.
p <.001.
FIGURE 1.
Representative graphs of risk factors predicting to child anxiety and depressive symptoms at high, medium, and low levels of moderator variables.
Maternal Affective Symptoms was a significant moderator of the association between Inhibition to Novelty and anxiety for girls but not for boys. In contrast, this moderated relationship did not significantly relate to depression for either boys or girls. For girls, increases in inhibition have much more modest effects on child anxiety at low levels of Maternal Affective Symptoms than they do at medium and high levels (see Figure 1, Panel A). For both boys and girls, maternal affect moderated the association between Negative Emotionality and depression but not anxiety (see Panel C and D). This significant interaction effect suggests there is a weak association between Negative Emotionality and child depression at low levels of Maternal Affective Symptoms, but as maternal symptoms increase the association is strengthened.
Family environment was generally a weak moderator of the effect of child temperament on child anxiety and depression symptoms. However, the association between Inhibition to Novelty and child anxiety tended to be somewhat stronger in families with lower levels of expressiveness (see Panel B). Although the coefficient for the interaction between Family Conflict and Negative Emotionality in the equation predicting depression was significant at conventional levels (p < .001), graphing children high and low on Negative Emotionality revealed that it was not substantively significant.
Violence Exposure did not significantly moderate either the effect of Negative Emotionality or Inhibition to Novelty on child anxiety or depression outcomes. Although the coefficient for the interaction between Violence Exposure and Negative Emotionality in the equation predicting depression was significant at conventional levels, the effect size was of small magnitude.
DISCUSSION
This study examined the contributions of multiple risk factors to differentiated anxiety and depressive symptoms in young children. Due to the nature of the sample and the focus on very young children, we adopted a symptom-oriented rather than a diagnostic approach for investigating anxiety and depression. In this large, healthy birth cohort of 2- and 3-year-olds, child temperament, family, and broader ecological factors were each independently associated with the early manifestations of anxious and depressive symptoms. For the internalizing outcomes, there was some, albeit limited, differentiation that was predominantly revealed in moderator models addressing the differential impact of family factors on temperamental vulnerabilities.
Child temperament characteristics and maternal internalizing affect were nonspecific, contributing to both child anxiety and depressive symptoms. Our findings for parent-reported inhibition to novelty are consistent with research supporting an association between shyness/behavioral inhibition and anxiety (Biederman et al., 2001), as well as some evidence relating it to depression (Rosenbaum et al., 2000). Young children with higher negative emotionality also exhibited elevated internalizing symptoms, consistent with empirical work on older children and adults (Phillips, Lonigan, Driscoll, & Hooe, 2002) and young children (Cote et al., 2009; Shaw et al., 1997). That maternal depressive and anxious symptoms were associated with both child internalizing outcomes is consistent with mothers and children sharing an underlying genetic diathesis (Eley & Stevenson, 1999). Because maternal anxiety and depression often co-occur, mothers may model a mixture of anxious or depressive behaviors and emotional displays and/or use parenting strategies that curb adaptive emotional regulation skills in their children (Goodman & Gotlib, 1999; Wood et al., 2003). Children’s reliance on maternal expressions of fear, sadness, distress, and concerns about threat to interpret their environments may also contribute to or strengthen attentional biases that place them at risk (Waters et al., 2008). Our use of a unitary maternal affective measure created because of the high correlation between maternal anxiety and depression scales may also account for the lack of specificity in associations with child outcomes.
Despite the hypothesized relevance of family conflict and violence exposure to child internalizing problems, only violence exposure emerged as meaningful. Children who witnessed violence were rated as showing elevated anxiety symptoms. Exposure to violence in the home and community has a high probability of being viewed as threatening; violating a sense of the environment as safe and predictable; and eliciting feelings of arousal, fear, helplessness, and reduced control, all of which are factors linked to anxiety vulnerability (Chorpita & Barlow, 1998). The lack of association between family conflict and child internalizing symptoms in this study may have arisen because the “family conflict” measure tapped both constructive (e.g., conflicts are resolved or nonresolution is framed optimistically) and destructive (e.g., interparental hostility and aggression, marital withdrawal, and child-centered themes) elements (Cummings & Davies, 2002) thereby obscuring the association with child maladjustment. Overall, our findings contribute to the small body of research showing the negative effect of violence exposure on the social-emotional adjustment of toddlers and preschoolers (Briggs-Gowan et al., 2009; Shahinfar et al., 2000) and indicate the need for more refined measurement of family risk factors like conflict.
When factors or interactions were specific, it was predominantly in relation to elevated levels of anxiety. Because there is moderate stability of anxiety symptoms from early childhood through adolescence (Bosquet & Egeland, 2006), early manifestations of anxiety may pose a significant developmental risk. It is interesting that maternal affective symptoms only moderated the association between inhibition to novelty and anxiety for girls, which is consistent with findings that young girls may be more sensitive to others’ emotional displays/facial expressions (McClure, 2000) and less likely to approach novel situations in response to maternal cues (Rosen, Adamson, & Bakeman, 1992). Specificity for the anxiety outcome may reflect stronger differentiation of sex expectations for fear and anxiety.
Lower levels of family expressiveness were generally related to both internalizing outcomes. During this formative period of emotional development, young children in families that restrict expression of positive and negative emotions may have fewer avenues for making sense of their emotional experiences and may use maladaptive display rules and regulation strategies learned through modeling (Eisenberg et al., 1998). For example, emotional control may heighten the arousal related to anxiety and negative reactions such as sadness and anger related to depression; it may also result in dampened positive affect and less effective up-regulation (Silk, Shaw, Forbes, Lane, & Kovacs, 2006). Of interest, children who exhibited higher levels of inhibition to novelty and were nested in less expressive families were rated as displaying higher levels of anxiety but not depressive symptoms. For these young, inhibited children, underdeveloped emotion understanding and competence may leave them vulnerable to interpreting ambiguous situations as threatening and to employing regulatory strategies such as avoidance and/or withdrawal that are less adaptive but potentially reinforcing and, therefore, maintained.
Although there have been recent efforts to characterize and diagnose depression in young children (Luby et al., 2002), we took a symptom-oriented approach thought to be more appropriate for a normative toddler sample. Few specific patterns of risk for child depressive problems emerged, which may be due to the low base rate in young children (Egger & Angold, 2006). Nevertheless, boys and girls temperamentally predisposed to negative emotionality and whose mothers reported higher levels of internalizing symptoms were rated as exhibiting higher levels of depressive but not anxiety symptoms. Because negative emotionality has been linked to both anxiety and depression (Phillips et al., 2002), this result was somewhat surprising. However, the negative emotionality measure used in this study tapped irritability, frustration, and proneness to anger—emotions that may align more closely with depressive symptoms when mothers are experiencing elevations in similar symptoms and struggling to provide scaffolding for adaptive emotion regulation.
Findings from this study should be considered along with several limitations. The results are constrained by reliance on a single informant and on parent report as the only method of measurement, raising the possibility that biased reporting contributed to the significant associations between risk factors and child internalizing problems. Yet primary caregivers of young children have extensive and detailed knowledge of their child’s development and are likely the most important informant (Loeber, Green, & Lahey, 1990). In fact, Carter, Little, Briggs-Gowan, and Kogan (1999) found congruence between maternal ratings on the ITSEA and observer ratings in the laboratory. For example, observer ratings of infant negativity were significantly correlated with ITSEA Negative Emotionality (r =.22, p <.05) and observer ratings of positive regulation strategies were negatively associated with ITSEA Inhibition/Separation (r =−.38, p <.01). Thus, there is support for the utility of maternal report but also recognition that future research will be strengthened by employing multi-informant, multimethod designs. Also, we were specifically interested in understanding the associations between risk factors and child anxiety and depression symptoms as well as factors that might moderate at-risk temperament in the toddler years. However, due to the cross-sectional nature of this investigation, it is not clear whether our findings reflect variations in normative development for toddlers or early, meaningful manifestations of and risk for internalizing problems.
Implications for Research, Policy, and Practice
From the developmental psychopathology perspective, single factors are rarely sufficient to explain negative outcomes (Cicchetti & Toth, 1997). Our results indicate that early emerging internalizing problems are associated not only with temperamental risks but also with facets of family functioning linked to emotion regulation such as family expressiveness and stressful life circumstances such as violence exposure. By investigating these processes in a large, community sample of toddlers using a multiple group (i.e., sex) and a differentiated (i.e., anxiety and depression) approach for child outcomes, we were also able to identify non-specific and specific patterns of association that might have been missed with a more typical (undifferentiated) approach.
In aggregate, our findings as well as study design suggest a number of avenues for further investigation. To understand the implications of the associations in toddlerhood between risk factors and internalizing outcomes, moderation of at-risk temperament and limited sex differences; longitudinal studies using large, community-based samples; more than one informant; and multiple methods of assessment are needed. We expected and found that the associations between maternal internalizing problems and child internalizing outcomes were non-specific. Maternal internalizing symptoms also emerged as an important moderator of at-risk temperament with more specificity. However, controversy remains regarding the distinctness of anxiety and depression in children and adults (Moffit et al., 2007). Similarly, some factor analytic research in young children has identified these constructs as related but distinct syndromes (Carter et al., 2003). Other research has shown less differentiation with an emphasis on the blurred boundaries between them (Achenbach, 1992; Sterba, Egger, et al., 2007). Research examining not only the role of combined maternal internalizing symptoms but also maternal anxiety and depression separately on both combined and differentiated child anxiety and depression symptoms could further elucidate the developmental processes that underlie internalizing trajectories.
This study provides additional empirical grounding for early detection, intervention, and prevention efforts. In particular, intervention programs for young, behaviorally inhibited children and their families (e.g., Kennedy, Rapee, & Edwards, 2009) might incorporate additional psychoeducational components focused on emotional regulation and the family climate. Similar programs could also target young children at risk due to high levels of negative emotionality and maternal depression problems. It may be more difficult to identify and enlist families of young children with multiple risk factors including chronic adversities. Thus, alternative approaches to intervention that are linked to service settings for at-risk families and address the real-world barriers to parent engagement are also needed (Shaw, Connell, Dishion, Wilson, & Gardner, 2009).
Contributor Information
Susan E. Marakovitz, Psychiatric and Neurodevelopmental Genetics Unit, Center for Human Genetic Research, Massachusetts General Hospital
Robert L. Wagmiller, Department of Sociology, University at Buffalo
Nicholas D. Mian, Department of Psychology, University of Massachusetts Boston
Margaret J. Briggs-Gowan, Department of Psychiatry, University of Connecticut Health Center
Alice S. Carter, Department of Psychology, University of Massachusetts Boston
References
- Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 profile. Burlington: University of Vermont, Department of Psychiatry; 1992. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Bayer JK, Hiscock H, Ukoumunne OC, Price A, Wake M. Early childhood aetiology of mental health problems: A longitudinal population-based study. Journal of Child Psychology and Psychiatry. 2008;49:1166–1174. doi: 10.1111/j.1469-7610.2008.01943.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Biederman J, Hirshfeld-Becker DR, Rosenbaum JF, Hérot C, Friedman D, Snidman N, et al. Further evidence of association between behavioral inhibition and social anxiety in children. American Journal of Psychiatry. 2001;158:1673–1679. doi: 10.1176/appi.ajp.158.10.1673. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Bongers IL, Koot HM, van der Ende J, Verhulst FC. The normative development of child and adolescent problem behavior. Journal of Abnormal Psychology. 2003;112:179–192. doi: 10.1037/0021-843x.112.2.179. [DOI] [PubMed] [Google Scholar]
- Bosquet M, Egeland B. The development and maintenance of anxiety symptoms from infancy through adolescence in a longitudinal sample. Development and Psychopathology. 2006;18:517–550. doi: 10.1017/S0954579406060275. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM. Are infant-toddler social-emotional and behavioral problems transient? Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:849–858. doi: 10.1097/01.chi.0000220849.48650.59. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Clark R, Augustyn M, McCarthy KJ, Ford J. Trauma exposure and preschool psychopathology: Are different clinical patterns associated with non-interpersonal trauma and violence? 2009. Manuscript submitted for publication. [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Moye Skuban E, McCue Horwitz S. Prevalence of social-emotional and behavioral problems in a community sample of 1- and 2-year-old children. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:811–819. doi: 10.1097/00004583-200107000-00016. [DOI] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan M. ITSEA Infant-Toddler Social and Emotional Assessment. San Antonio, TX: Psychological Corporation Harcourt Press; 2006. [Google Scholar]
- Carter AS, Briggs-Gowan M. Child Life Events Scale. 1998. Unpublished scale. [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Davis NO. Assessment of young children’s social-emotional development and psychopathology: Recent advances and recommendations for practice. Journal of Child Psychology and Psychiatry. 2004;45:109–134. doi: 10.1046/j.0021-9630.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Jones SM, Little TD. The Infant-Toddler Social and Emotional Assessment (ITSEA): Factor structure, reliability, and validity. Journal of Abnormal Child Psychology. 2003;31:495–514. doi: 10.1023/a:1025449031360. [DOI] [PubMed] [Google Scholar]
- Carter AS, Little C, Briggs-Gowan MJ, Kogan N. The infant-toddler social and emotional assessment (ITSEA): Comparing parent ratings to laboratory observations of task mastery, emotion regulation, coping behaviors and attachment status. Infant Mental Health Journal. 1999;20:375–392. [Google Scholar]
- Chorpita BF, Barlow DH. The development of anxiety: The role of control in the early environment. Psychological Bulletin. 1998;124(1):3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Transactional ecological systems in developmental psychopathology. In: Luthar SS, Burack JA, Cicchetti D, Weisz JR, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. pp. 317–349. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cote SM, Boivin M, Liu X, Nagin DS, Zoccolillo M, Tremblay R. Depression and anxiety symptoms: Onset, developmental course, and risk factors during early childhood. Journal of Child Psychology and Psychiatry. 2009;50:1201–1208. doi: 10.1111/j.1469-7610.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- Crockenberg SC, Leerkes EM. Infant and maternal behavior moderate reactivity to novelty to predict anxious behaviors at 2.5 years. Developmental and Psychopathology. 2006;18:17–84. doi: 10.1017/S0954579406060020. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Effects of marital conflict on children: Recent advances and emerging themes in process-oriented research. Journal of Child Psychology and Psychiatry. 2002;43(1):31–63. doi: 10.1111/1469-7610.00003. [DOI] [PubMed] [Google Scholar]
- Degnan KA, Henderson HA, Fox NA, Rubin KH. Predicting social wariness in middle childhood: The moderating roles of childcare history, maternal personality and maternal behavior. Social Development. 2008;17:471–487. doi: 10.1111/j.1467-9507.2007.00437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas JE, LaFreniere PJ, Serketich WJ. ‘Balance of power’: A transactional analysis of control in mother–child dyads involving socially competent, aggressive, and anxious children. Journal of Abnormal Psychology. 1995;104(1):104–113. doi: 10.1037//0021-843x.104.1.104. [DOI] [PubMed] [Google Scholar]
- Easterbrooks MA, Cummings EM, Emde RN. Young children’s responses to constructive marital disputes. Journal of Family Psychology. 1994;8:160–169. [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9:241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eley TC, Bolton D, O’Connor TG, Perrin S, Smith P, Plomin R. A twin study of anxiety-related behaviours in pre-school children. Journal of Child Psychology and Psychiatry. 2003;44:945–960. doi: 10.1111/1469-7610.00179. [DOI] [PubMed] [Google Scholar]
- Eley TC, Stevenson J. Using genetic analyses to clarify the distinction between depressive and anxious symptoms in children. Journal of Abnormal Child Psychology. 1999;27:105–114. doi: 10.1023/a:1021947113860. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. Journal of Abnormal Psychology. 2008;117(1):32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith HH, Lemery KS. Linking temperamental fearfulness and anxiety symptoms: A behavior–genetic perspective. Biological Psychiatry. 2000;48:1199–1209. doi: 10.1016/s0006-3223(00)01003-9. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Kagan J. Behavioral inhibition to the unfamiliar. Child Development. 1984;55:2212–2225. [Google Scholar]
- Karevold E, Roysamb E, Ystrom E, Mathiesen KS. Predictors and pathways from infancy to symptoms of anxiety and depression in early adolescence. Developmental Psychology. 2009;45:1051–1060. doi: 10.1037/a0016123. [DOI] [PubMed] [Google Scholar]
- Kennedy SJ, Rapee RM, Edwards S. A selective intervention program for inhibited preschool-aged children of parents with an anxiety disorder: Effects on current anxiety disorders and temperament. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:602–609. doi: 10.1097/CHI.0b013e31819f6fa9. [DOI] [PubMed] [Google Scholar]
- Lahey BB. Commentary: Role of temperament in developmental models of psychopathology. Journal of Clinical Child and Adolescent Psychology. 2004;33:88–93. doi: 10.1207/S15374424JCCP3301_9. [DOI] [PubMed] [Google Scholar]
- Laible D, Panfile T, Makariev D. The quality and frequency of mother–toddler conflict: Links with attachment and temperament. Child Development. 2008;79:426–443. doi: 10.1111/j.1467-8624.2007.01134.x. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB. Mental health professionals’ perception of the utility of children, mothers, and teachers as informants on childhood psychopathology. Journal of Clinical Child Psychology. 1990;19:136–143. [Google Scholar]
- Luby JL, Belden AC, Spitznagel E. Risk factors for preschool depression: The mediating role of early stressful life events. Journal of Child Psychology and Psychiatry. 2006;47:1292–1298. doi: 10.1111/j.1469-7610.2006.01672.x. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger AK, Mrakotsky C, Hessler MJ, Brown KM, Hildebrand T. Preschool major depressive disorder: Preliminary validation for developmentally modified DSM–V criteria. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:928–937. doi: 10.1097/00004583-200208000-00011. [DOI] [PubMed] [Google Scholar]
- McClure EB. A meta-analytic review of sex differences in facial expression processing and their development in infants, children, and adolescents. Psychological Bulletin. 2000;126:424–453. doi: 10.1037/0033-2909.126.3.424. [DOI] [PubMed] [Google Scholar]
- McDonald R, Jouriles EN, Briggs-Gowan MJ, Rosenfield D, Carter AS. Violence toward a family member, angry adult conflict, and child adjustment difficulties: Relations in families with 1- to 3-year-old children. Journal of Family Psychology. 2007;21:176–184. doi: 10.1037/0893-3200.21.2.176. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Weisz J, Wood JJ. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007;27:986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Mesman J, Koot HM. Early preschool predictors of preadolescent internalizing and externalizing DSM–IV diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:1029–1036. doi: 10.1097/00004583-200109000-00011. [DOI] [PubMed] [Google Scholar]
- Moffit TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, et al. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Moore PS, Whaley SE, Sigman M. Interactions between mother and children: Impacts of maternal and child anxiety. Journal of Abnormal Psychology. 2004;113:471–476. doi: 10.1037/0021-843X.113.3.471. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale Manual. 2. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Pelaez M, Field T, Pickens JN, Hart S. Disengaged and authoritarian parenting behavior of depressed mothers with their toddlers. Infant Behavior & Development. 2008;31:145–148. doi: 10.1016/j.infbeh.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Phillips BM, Lonigan CJ, Driscoll K, Hooe ES. Positive and negative affectivity in children: A multitrait–multimethod investigation. Journal of Clinical Child and Adolescent Psychology. 2002;31:465–479. doi: 10.1207/S15374424JCCP3104_6. [DOI] [PubMed] [Google Scholar]
- Prior M, Smart D, Sanson A, Pedlow R, Oberklaid F. Transient versus stable behavior problems in a normative sample: Infancy to school age. Journal of Pediatric Psychology. 1992;17:423–443. doi: 10.1093/jpepsy/17.4.423. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES–D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rapee RM. The development and modification of temperamental risk for anxiety disorders: Prevention of a lifetime of anxiety? Biological Psychiatry. 2002;52:947–957. doi: 10.1016/s0006-3223(02)01572-x. [DOI] [PubMed] [Google Scholar]
- Rosen WD, Adamson LB, Bakeman R. An experimental investigation of infant social referencing: Mothers’ messages and gender differences. Developmental Psychology. 1992;28:1172–1178. [Google Scholar]
- Rosenbaum J, Biederman J, Hirshfeld-Becker DR, Kagan J, Snidman N, Friedman D, et al. A controlled study of behavioral inhibition in children of parents with panic disorder and depression. American Journal of Psychiatry. 2000;157:2002–2010. doi: 10.1176/appi.ajp.157.12.2002. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Posner MI. Temperament, attention and developmental psychopathology. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Volume 2: Developmental neuroscience. 2. Hoboken, NJ: Wiley; 2006. pp. 465–501. [Google Scholar]
- Saudino KJ, Carter AS, Purper-Ouakil D, Gorwood P. The etiology of behavioral problems and competencies in very young twins. Journal of Abnormal Psychology. 2008;117(1):48–62. doi: 10.1037/0021-843X.117.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz CE, Snidman N, Kagan J. Adolescent social anxiety as an outcome of inhibited temperament in childhood. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1008–1014. doi: 10.1097/00004583-199908000-00017. [DOI] [PubMed] [Google Scholar]
- Shahinfar A, Fox NA, Leavitt LA. Preschool children’s exposure to violence: Relation of behavior problems to parent and child reports. American Journal of Orthopsychiatry. 2000;70(1):115–125. doi: 10.1037/h0087690. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI, Delliquadri E, Giovannelli J. Antecedents of preschool children’s internalizing problems: A longitudinal study of low-income families. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1760–1767. [PubMed] [Google Scholar]
- Shaw DS, Schonberg M, Sherrill J, Huffman D, Lukon J, Obrosky D, et al. Responsivity to offspring’s expression of emotion among childhood-onset depressed mothers. Journal of Clinical Child and Adolescent Psychology. 2006;35:490–503. doi: 10.1207/s15374424jccp3504_1. [DOI] [PubMed] [Google Scholar]
- Silk JS, Shaw DS, Forbes EE, Lane TL, Kovacs M. Maternal depression and child internalizing: The moderating role of child emotion regulation. Journal of Clinical and Adolescent Psychology. 2006;35:116–126. doi: 10.1207/s15374424jccp3501_10. [DOI] [PubMed] [Google Scholar]
- Sterba SK, Egger HL, Angold A. Diagnostic specificity and nonspecificity in the dimensions of preschool psychopathology. Journal of Child Psychology and Psychiatry. 2007;48:1005–1013. doi: 10.1111/j.1469-7610.2007.01770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterba SK, Prinstein MJ, Cox MJ. Trajectories of internalizing problems across childhood: Heterogeneity, external validity, and gender differences. Development and Psychopathology. 2007;19:345–366. doi: 10.1017/S0954579407070174. [DOI] [PubMed] [Google Scholar]
- Suveg C, Zeman J, Flannery-Schroeder E, Cassano M. Emotional socialization in families of children with an anxiety disorder. Journal of Abnormal Child Psychology. 2005;33:145–155. doi: 10.1007/s10802-005-1823-1. [DOI] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Costello A. Psychopathology in the offspring of anxiety disorders patients. Journal of Consulting and Clinical Psychology. 1987;55:229–235. doi: 10.1037//0022-006x.55.2.229. [DOI] [PubMed] [Google Scholar]
- van der Valk JC, van den Oord EJ, Verhulst FC, Boomsma DI. Genetic and environmental contributions to stability and change in children’s internalizing and externalizing problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1212–1220. doi: 10.1097/00004583-200310000-00012. [DOI] [PubMed] [Google Scholar]
- Vasey MW, Dadds MR. The developmental psychopathology of anxiety. New York: Oxford University Press; 2001. [Google Scholar]
- Warren SL. Anxiety disorders. In: DelCarmen-Wiggins R, Carter A, editors. Handbook of infant, toddler, and preschool mental health assessment. New York: Oxford University Press; 2004. pp. 355–375. [Google Scholar]
- Waters AM, Mogg K, Bradley BP, Pine DS. Attentional bias for emotional faces in children with generalized anxiety disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:435–442. doi: 10.1097/CHI.0b013e3181642992. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Gammon GD, John K, Merikangas KR. Children of depressed parents: Increased psychopathology and early onset of major depression. Archives of General Psychiatry. 1987;44:847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Sigman M, Hwang WC, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry. 2003;44(1):134–151. doi: 10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]