Abstract
Xanthohumol is a flavonoid compound that exhibits antioxidant and anticancer effects, and is used to treat atherosclerosis. The aim of the present study was to investigate the effect of xanthohumol on the cell proliferation of laryngeal squamous cell carcinoma and to understand the mechanism of its action. The effects of xanthohumol on the cell viability and apoptosis rate of laryngeal squamous cell carcinoma SCC4 cells were assessed by Annexin V-fluorescein isothiocyanate/propidium iodide staining. In addition, the expression levels of pro-apoptotic proteins, caspase-3, caspase-8, caspase-9, poly ADP ribose polymerase (PARP) p53 and apoptosis-inducing factor (AIF), as well as anti-apoptotic markers, B-cell lymphoma 2 (Bcl-2) and myeloid cell leukemia 1 (Mcl-1), were analyzed by western blotting. The results revealed that treatment with 40 µM xanthohumol significantly inhibited the proliferation of SCC4 cells. Furthermore, xanthohumol treatment (40 µM) induced SCC4 cell apoptosis, as indicated by the significant increase in activity and expression of caspase-3, caspase-8, caspase-9, PARP, p53 and AIF. By contrast, the protein expression of Bcl-2 and Mcl-1 was significantly decreased following treatment with 40 µM xanthohumol. Taken together, the results of the present study indicated that xanthohumol mediates growth suppression and apoptosis induction, which was mediated via the suppression of Bcl-2 and Mcl-1 and activation of PARP, p53 and AIF signaling pathways. Therefore, future studies that investigate xanthohumol as a potential therapeutic agent for laryngeal squamous cell carcinoma are required.
Keywords: xanthohumol, laryngeal squamous cell carcinoma, B-cell lymphoma 2, myeloid cell leukemia 1, poly ADP ribose polymerase, p53, apoptosis-inducing factor
Introduction
Laryngeal cancer is the most common malignancy of the throat in China. At present, the incidence rate of laryngeal cancer is increasing significantly, accounting for 5.7–7.6% of all malignant tumors in the northeast areas of China (1). A number of hypotheses regarding the pathogenesis of laryngeal carcinoma exist: Smoking, alcohol consumption, air pollution and viral infection are considered the main risk factors (2). Due to the anatomical site of the larynx, patients often mistake hoarseness and other clinical symptoms of the disease as an upper respiratory tract infection or symptom of voice overuse, which results in negligence of the illness (3). Supraglottic cancer and subglottic cancer exhibit no specific symptoms at the primary stages and thus, early diagnosis is difficult, which results in the majority of cases being diagnosed at late and terminal stages (4). Due to recent advances in minimally invasive surgery, radiotherapy, chemotherapy, concurrent radiochemotherapy, biological therapy and other comprehensive treatment modalities, patient survival times have increased and patient quality of life has improved (5). However, the high rates of relapse and metastasis of laryngeal cancer in addition to chemotherapy resistance lead to poor treatment outcomes (6,7). Thus, to investigate and develop novel targeted treatments for cancer, laryngeal cancer must be investigated from a novel perspective.
Effective cancer treatments aim to eradicate the majority of differentiated tumor cells, as well as tumor stem cells, which have potential to proliferate and differentiate (8). However, traditional therapies, including radiotherapy, chemotherapy and immunotherapy, kill differentiated tumor cells but not tumor stem cells, which results in the development of tumor cell resistance to treatment and subsequent relapse (9). Ideally, treatments should kill differentiated tumor cells without causing damage to other cell types, which requires the identification of specific cell markers, genes and signal transduction pathways associated with cancer that may be used as therapeutic targets to improve the efficacy of tumor treatment (10).
Xanthohumol is a flavonoid compound obtained from hops resin (11). It exhibits numerous biological properties, including anti-inflammation and anti-infection effects and has been demonstrated to inhibit the growth and proliferation of microorganisms (12). Recent studies investigating xanthohumol have predominantly focused on the prevention and treatment of cancer (13,14). Studies have demonstrated that xanthohumol inhibits tumor cell growth of colon cancer, prostate cancer, cervical cancer, liver cancer and leukemia cells (15–17). Therefore, the aim of the present study was to investigate the effect of xanthohumol on the proliferation of human laryngeal squamous cell carcinoma. The results of the present study may indicate whether xanthohumol presents a potential drug for the treatment of human laryngeal squamous cell carcinoma and may also provide information regarding potential molecular mechanisms of the disease.
Materials and methods
Cell and reagents
The human laryngeal squamous cell carcinoma SCC4 cell line was obtained from Shanghai Jiao Tong University Affiliated Sixth People's Hospital (Shanghai, China). Dulbecco's modified Eagle's medium (DMEM), penicillin and streptomycin were purchased from Gibco (Thermo Fisher Scientific, Inc., Waltham, MA, USA). Fetal bovine serum (FBS) was obtained from Gibco (Thermo Fisher Scientific, Inc.). Xanthohumol (Fig. 1) and 3-(4,5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) were purchased from Sigma-Aldrich (Merck Millipore, Darmstadt, Germany). Annexin V-fluorescein isothiocyanate (FITC)/propidium iodide (PI) staining kit was obtained from BestBio (Shanghai, China).
Figure 1.
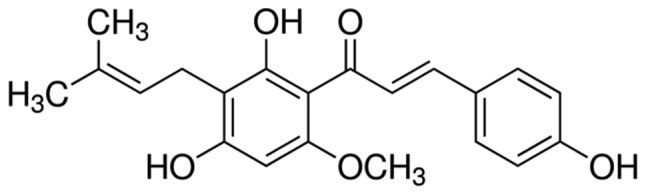
Chemical structure of xanthohumol.
Cell culture
The SCC4 cell line was cultured in DMEM supplemented with 10% FBS, 100 U/ml penicillin and 100 U/ml streptomycin in a humidified atmosphere with 5% CO2 at 37°C. The complete medium was changed every 2–3 days.
Proliferation assay
SCC4 cells (1×105/well) in the logarithmic growth phase were seeded in 96-well microplates. The medium was replaced with DMEM containing 0, 10, 20, 30, 40 or 50 µM xanthohumol and the cells were cultured for 72 h, after which 200 µl MTT (0.5 mg/ml; Sigma-Aldrich) was added to each well. Following incubation at 4°C, 150 µl DMSO was added and the absorbance was measured using a spectrophotometer (Infinite® 200 PRO; Tecan, San Jose, CA, USA) at a wavelength of 540 nm.
Annexin V-FITC/PI staining
SCC4 cells (2.4×106/well) in the logarithmic growth phase were seeded in 6-well microplates. The medium was replaced with DMEM containing 20, 30 or 40 µM xanthohumol and cells were cultured for 48 h at 4°C. SCC4 cells (1×106) were harvested, washed with PBS and resuspended in binding buffer (BestBio). Next, 5 µl Annexin V-FITC and 5 µl PI were added to each well and cultured for 20 min at 4°C. Apoptotic rate was determined using a flow cytometer (FACSCalibur™; BD Biosciences, San Jose, CA, USA).
Measurement of caspase-3, −8 and −9 activity
SCC4 cells (2.4×106/well) in the logarithmic growth phase were seeded in 6-well microplates. The medium was replaced with DMEM containing 20, 30 or 40 µM xanthohumol and cells were cultured for 48 h at 4°C. SCC4 cells (1×106) were harvested, washed with PBS and resuspended in binding buffer. A total of 1 µl fluorescent substrate [Ac-DEVD-pNA for caspase-3, Ac-IETD-pNA for caspase-8 and Ac-LEHD-pNA for caspase-9 (BestBio, Shanghai, China)] was added to each well and incubated for 1 h at 4°C. Cells were then centrifuged at 500 × g for 10 min at room temperature and the supernatant was removed. The cells were resuspended in 100 µl wash buffer (BestBio), and the fluorescence intensity was measured at 485 nm (excitation wavelength) and 535 nm (emission wavelength) using a spectrophotometer.
Western blot analysis
SCC4 cells (2.4×106/well) in the logarithmic growth phase were seeded in 6-well microplates. The medium was replaced with DMEM containing 20, 30 or 40 µM xanthohumol and cells were cultured for 48 h at 4°C. SCC4 cells (1×106) were harvested, washed with PBS, and lysed with cold RIPA buffer (BestBio) containing protease inhibitors. Protein concentrations were quantified using the bicinchonic acid assay method (BestBio). A total of 10 µg protein was boiled in water prior to separation by 12% SDS-PAGE for 10 min then transferred onto polyvinylidene difluoride membranes at 100 V for 1.5 h. Membranes were blocked with 5% skimmed milk in Tris-buffered saline with 0.1% Tween 20 for 2 h followed by incubation with anti-B-cell lymphoma 2 (Bcl-2; cat. no. sc-7382; 1:1,000), anti-myeloid cell leukemia 1 (Mcl-1; cat. no. sc-377487; 1:1,000), anti-poly ADP ribose polymerase (PARP; cat. no. sc-56197; 1:2,000), anti-p53 (sc-393031; 1:1,000), anti-apoptosis-inducing factor (AIF; cat. no. sc-390619; 1:1,000) and anti-β-actin (cat. no. sc-47778; 1:1,000) antibodies (Santa Cruz Biotechnology Inc., Dallas, TX, USA) overnight 4°C. The membranes were then incubated with mouse secondary antibodies (cat. no. sc-358914; 1:15,000; Santa Cruz Biotechnology, Inc.) for 2 h at 4°C. The proteins were visualized using BeyoECL Star (cat. no. P0018A; Beyotime Institute of Biotechnology, Jiangsu, China) and quantified using the Molecular Imager ChemiDoc XRS+ System with Image Lab™ software (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
All data are presented as the mean ± standard error of the mean. Data was analyzed by one-way analysis of variance followed by Dunnett's t-test using SPSS version 22 statistical software (SPPS, Inc., Chicago, IL, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
Xanthohumol inhibits proliferation of laryngeal squamous cell carcinoma cells
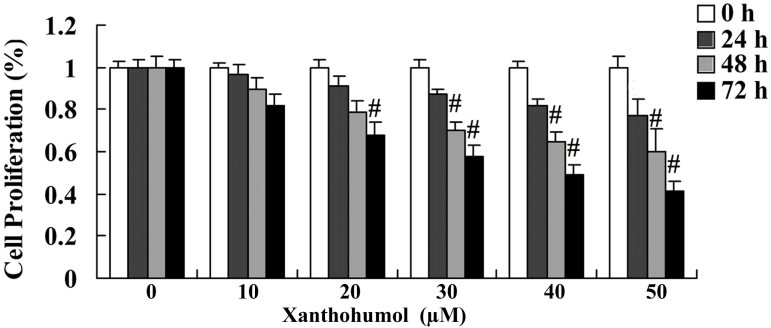
MTT assay was performed to determine the effect of xanthohumol on the proliferation of SCC4 cells following treatment with 30, 40 and 50 µM xanthohumol for 24, 48 and 72 h. The results revealed that xanthohumol inhibited the proliferation of SCC4 cells in a concentration- and time-dependent manner when compared with that of control group (Fig. 2). Following 24, 48 and 72 h treatment with 30, 40 and 50 µM xanthohumol significantly inhibited the proliferation of SCC4 cells (Fig. 2). In addition, following treatment with 20 µM xanthohumol for 72 h proliferation of SCC4 cells was significantly inhibited compared with the control group (Fig. 2).
Figure 2.
Treatment with 20 µM xanthohumol for 72 h, and 30, 40 and 50 µM for 24, 48 and 72 h significantly inhibits the proliferation of laryngeal squamous cell carcinoma cells. #P<0.01 vs. control.
Xanthohumol induces cell apoptosis of laryngeal squamous cell carcinoma cells
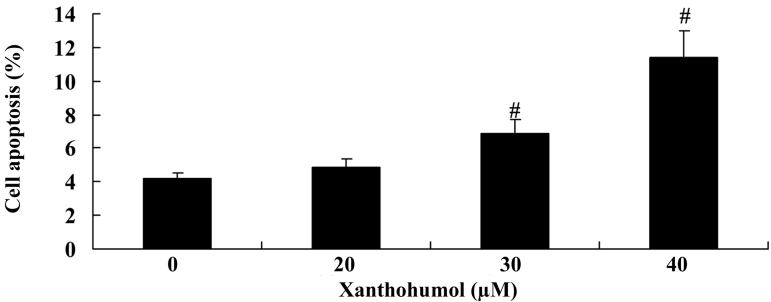
To evaluate the effect of xanthohumol on SCC4 cell apoptosis, flow cytometry analysis was performed. The results demonstrated that treatment with 30 and 40 µM xanthohumol for 48 h significantly induced apoptosis of SCC4 cells compared with the control group (Fig. 3).
Figure 3.
Xanthohumol induces cell apoptosis of laryngeal squamous cell carcinoma. #P<0.01 vs. control.
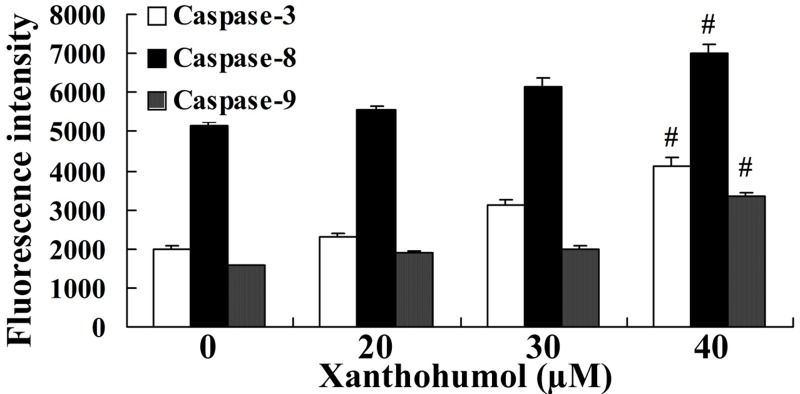
Xanthohumol increases caspase-3, −8 and −9 activity in laryngeal squamous cell carcinoma
To further investigate the effect of xanthohumol on caspase activity in laryngeal squamous cell carcinoma, the florescence intensities of caspase-3, −8 and −9 were measured in SCC4 cells following 48 h treatment with 20, 30 and 40 µM xanthohumol. The results revealed that caspase-3, −8 and −9 activity was significantly increased following treatment with 30 and 40 µM xanthohumol when compared with the control group (Fig. 4).
Figure 4.
Xanthohumol induces caspase-3, −8 and −9 activity in SSC4 cells. #P<0.01 vs. control.
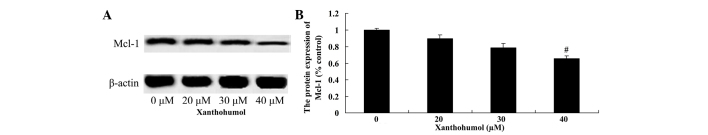
Xanthohumol decreases Bcl-2 and Mcl-1 protein expression in laryngeal squamous cell carcinoma cells
The effect of xanthohumol on the expression of Bcl-2 and Mcl-1 proteins in laryngeal squamous cell carcinoma SCC4 cells was examined by western blot analysis. Following treatment with 40 µM xanthohumol the expression of Bcl-2 (Fig. 5) and Mcl-1 (Fig. 6) proteins were significantly decreased compared with the control group.
Figure 5.
(A) Western blot revealing xanthohumol decreases Bcl-2 protein expression in laryngeal squamous cell carcinoma cells in a dose-dependent manner. (B) Quantification of Bcl-2 protein expression following xanthohumol treatment in laryngeal squamous cell carcinoma cells. #P<0.01 vs. control. Bcl-2, B-cell lymphoma 2.
Figure 6.
(A) Western blot revealing xanthohumol decreases Mcl-1 protein expression in laryngeal squamous cell carcinoma cells in a dose-dependent manner. (B) Quantification of Mcl-1 protein expression following xanthohumol treatment in laryngeal squamous cell carcinoma cells. #P<0.01 vs. control. Mcl-1, myeloid cell leukemia 1.
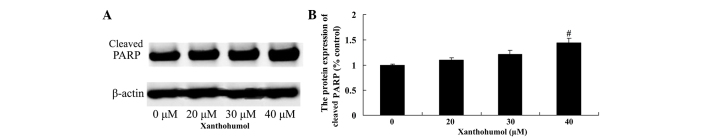
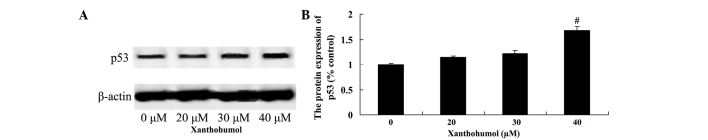
Xanthohumol increases PARP and p53 protein expression in laryngeal squamous cell carcinoma
The effect of xanthohumol on PARP and p53 protein expression in SSC4 cells was examined by western blot analysis. Following treatment with 40 µM xanthohumol for 48 h, the expression of PARP (Fig. 7) and p53 (Fig. 8) proteins were significantly increased compared with control group.
Figure 7.
(A) Western blot revealing xanthohumol increases PARP protein expression in laryngeal squamous cell carcinoma cells. (B) Quantification of PARP protein expression following xanthohumol treatment in laryngeal squamous cell carcinoma cells. #P<0.01 vs. control. PARP, poly ADP ribose polymerase.
Figure 8.
(A) Western blot revealing xanthohumol increases p53 protein expression in laryngeal squamous cell carcinoma cells. (B) Quantification of p53 protein expression following xanthohumol treatment in laryngeal squamous cell carcinoma cells. #P<0.01 vs. control.
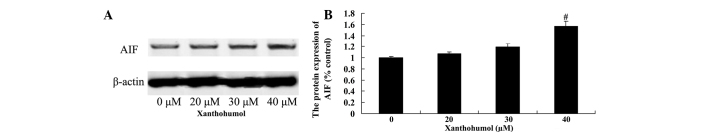
Xanthohumol increases AIF protein expression in laryngeal squamous cell carcinoma cells
To determine whether the AIF pathway mediates the anticancer effects of xanthohumol, AIF protein expression in SCC4 cells was measured using western blot analysis. Following treatment with 40 µM xanthohumol for 48 h, the expression of AIF protein was significantly increased compared with the control group (Fig. 9).
Figure 9.
Western blot revealing xanthohumol increases AIF protein expression in laryngeal squamous cell carcinoma cells. (B) Quantification of AIF protein expression following xanthohumol treatment in laryngeal squamous cell carcinoma cells. #P<0.01 vs. control. AIF, apoptosis-inducing factor.
Discussion
Laryngeal squamous cell carcinoma is a common malignant tumor derived from the laryngeal epithelium, which is the third most common cause of head and neck cancer morbidity, accounting for 1–5% of all malignant tumors (2). Notably, the incidence rate of laryngeal cancer is increasing significantly among young individuals and thus, better treatments are urgently required (18). Although the treatment of laryngeal cancer has markedly improved in recent years due to advances in surgical techniques and combined chemotherapy and radiotherapy regimens, certain cases of squamous cell carcinoma of the larynx do not respond to treatment (19). Furthermore, due to the rapid development of molecular biology technology, gene therapy is gaining increasing attention and is considered to present a promising option for cancer patients (20). Therefore, the identification of specific genes that are involved in the development of laryngeal squamous cell carcinoma may lead to further studies and the clinical application of gene therapy for laryngeal cancer. Previous studies have demonstrated that xanthohumol induces apoptosis in hepatocellular carcinoma (21), human cervical cancer cells (17) and breast cancer (22). To the best of our knowledge, the present study is the first to demonstrate that xanthohumol inhibits cell proliferation and induces cell apoptosis of laryngeal squamous cell carcinoma SCC4 cells.
Cancer is a disease caused by abnormal cell proliferation, differentiation and apoptosis. It has been reported that caspases are activated during tumor cell apoptosis (23). A series of novel caspase-related apoptosis-inducing pathways have been identified that may be targeted to control cancer, which have practical significance for the majority of tumors and thus, may result in breakthroughs with regard to the treatment of malignant tumors (24). The activation of caspase-9 and caspase-3 may underlie the apoptosis of fibroblasts in keloids (25). Furthermore, caspase-8 activates caspase-9 downstream of the apoptosis cascade to induce apoptosis (26). In the current study, xanthohumol promoted the activity of caspase-3, −8 and −9 and suppressed Bcl-2 and Mcl-1 protein expression in laryngeal squamous cell carcinoma SCC4 cells. These results are in accordance with those reported by Pan et al (27), which demonstrated that xanthohumol induces apoptosis of human colon cancer cells via caspase-3, −8 and −9. Furthermore, Zajc et al (15) reported that xanthohumol induces different cytotoxic and apoptotic pathways via Bax/Bcl-2 in malignant and normal astrocytes. Kunnimalaiyaan et al (28) demonstrated that xanthohumol inhibits induces apoptosis via the anti-apoptotic markers, survivin, cyclin D1 and Mcl-1, in hepatocellular carcinoma.
PARP-1 is a member of the PARP family, which initiates DNA damage repair via the modification of poly adenosine diphosphate glycosylation receptor protein. PARP-1 has been shown to trigger apoptosis signaling and activate caspase-3 to induce cell apoptosis and DNA damage (24,29). Thus, we hypothesize that treatment with xanthohumol promoted PARP protein expression in laryngeal squamous cell carcinoma SCC4 cells. Lust et al (11) demonstrated that xanthohumol activates the proapoptotic pathway via PARP activation in chronic lymphocytic leukemia.
The p53 gene is recognized as the most commonly mutated tumor suppressor gene (30). Recent studies have indicated that p53 gene mutations exhibit an important function in the development of laryngeal squamous cell carcinoma (31,32). The mutation rate of p53 is >90% in certain tumors (lung, liver, colon and gastric cancer) and ranges between 34 and 93% in head and neck tumor tissues and cell lines, which is associated with early relapse of cancer (33). Xanthohumol activates PARP protein expression in laryngeal squamous cell carcinoma cells. In the present study, p53 expression increased significantly following treatment with xanthohumol. Monteghirfo et al (12) reported that xanthohumol inhibits leukemia cell invasion via p53 modulation in Bcr/Abl-transformed cells.
AIF protein, which is located in the mitochondrial intermembrane space, exhibits apoptosis-inducing activity (34). In response to apoptotic stimuli, AIF molecules are released from the mitochondria into the cytoplasm followed by translocation to the nucleus and subsequent integration with chromosomal DNA, which leads to chromosome condensation and DNA breakage into large fragments (~50 kB) (35). AIF exhibits apoptosis-inducing activity and oxidoreductase activity, which result in interlinkage (36). Notably, AIF was the first molecule to be identified that mediates cell apoptosis directly, however, it has also been reported that caspases are involved in AIF apoptotic activity (37). The results of the present study also indicated that xanthohumol increased AIF protein expression in laryngeal squamous cell carcinoma cells. Yong and Abd Malek (17) reported that xanthohumol induces growth inhibition and apoptosis via AIF protein expression in Ca Ski human cervical cancer cells.
In conclusion, we postulate that xanthohumol mediates growth suppression and induces caspase-dependent cell death via the suppression of Bcl-2 and Mcl-1 and activation of PARP, p53 and AIF signaling pathways. Therefore, future studies that investigate xanthohumol as a potential therapeutic agent for laryngeal squamous cell carcinoma are required.
References
- 1.Guibert M, Lepage B, Woisard V, Rives M, Serrano E, Vergez S. Quality of life in patients treated for advanced hypopharyngeal or laryngeal cancer. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:218–223. doi: 10.1016/j.anorl.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Tuomi L, Andréll P, Finizia C. Effects of voice rehabilitation after radiation therapy for laryngeal cancer: A randomized controlled study. Int J Radiat Oncol Biol Phys. 2014;89:964–972. doi: 10.1016/j.ijrobp.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 3.Robertson SM, Yeo JC, Sabey L, Young D, MacKenzie K. Effects of tumor staging and treatment modality on functional outcome and quality of life after treatment for laryngeal cancer. Head Neck. 2013;35:1759–1763. doi: 10.1002/hed.23230. [DOI] [PubMed] [Google Scholar]
- 4.Möhner M, Lindtner M, Otten H. Ionizing radiation and risk of laryngeal cancer among German uranium miners. Health Phys. 2008;95:725–733. doi: 10.1097/01.HP.0000319906.41329.04. [DOI] [PubMed] [Google Scholar]
- 5.Giotakis AI, Kontos CK, Manolopoulos LD, Sismanis A, Konstadoulakis MM, Scorilas A. High BAX/BCL2 mRNA ratio predicts favorable prognosis in laryngeal squamous cell carcinoma, particularly in patients with negative lymph nodes at the time of diagnosis. Clin Biochem. 2016;49:890–896. doi: 10.1016/j.clinbiochem.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Tae K, Jin BJ, Ji YB, Jeong JH, Cho SH, Lee SH. The role of laryngopharyngeal reflux as a risk factor in laryngeal cancer: A preliminary report. Clin Exp Otorhinolaryngol. 2011;4:101–104. doi: 10.3342/ceo.2011.4.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narwani V, Nalamada K, Lee M, Kothari P, Lakhani R. Readability and quality assessment of internet-based patient education materials related to laryngeal cancer. Head Neck. 2016;38:601–605. doi: 10.1002/hed.23939. [DOI] [PubMed] [Google Scholar]
- 8.Xu CZ, Xie J, Jin B, Chen XW, Sun ZF, Wang BX, Dong P. Gene and microRNA expression reveals sensitivity to paclitaxel in laryngeal cancer cell line. Int J Clin Exp Pathol. 2013;6:1351–1361. [PMC free article] [PubMed] [Google Scholar]
- 9.Yu D, Jin C, Liu Y, Yang J, Zhao Y, Wang H, Zhao X, Cheng J, Liu X, Liu C. Clinical implications of cancer stem cell-like side population cells in human laryngeal cancer. Tumour Biol. 2013;34:3603–3610. doi: 10.1007/s13277-013-0941-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei X, Wang J, He J, Ma B, Chen J. Biological characteristics of CD133(+) cancer stem cells derived from human laryngeal carcinoma cell line. Int J Clin Exp Med. 2014;7:2453–2462. [PMC free article] [PubMed] [Google Scholar]
- 11.Lust S, Vanhoecke B, VAN Gele M, Boelens J, VAN Melckebeke H, Kaileh M, Berghe W Vanden, Haegeman G, Philippé J, Bracke M, Offner F. Xanthohumol activates the proapoptotic arm of the unfolded protein response in chronic lymphocytic leukemia. Anticancer Res. 2009;29:3797–3805. [PMC free article] [PubMed] [Google Scholar]
- 12.Monteghirfo S, Tosetti F, Ambrosini C, Stigliani S, Pozzi S, Frassoni F, Fassina G, Soverini S, Albini A, Ferrari N. Antileukemia effects of xanthohumol in Bcr/Abl-transformed cells involve nuclear factor-kappaB and p53 modulation. Mol Cancer Ther. 2008;7:2692–2702. doi: 10.1158/1535-7163.MCT-08-0132. [DOI] [PubMed] [Google Scholar]
- 13.Chen PH, Chang CK, Shih CM, Cheng CH, Lin CW, Lee CC, Liu AJ, Ho KH, Chen KC. The miR-204-3p-targeted IGFBP2 pathway is involved in xanthohumol-induced glioma cell apoptotic death. Neuropharmacology. 2016;110:362–375. doi: 10.1016/j.neuropharm.2016.07.038. [DOI] [PubMed] [Google Scholar]
- 14.Dokduang H, Yongvanit P, Namwat N, Pairojkul C, Sangkhamanon S, Yageta MS, Murakami Y, Loilome W. Xanthohumol inhibits STAT3 activation pathway leading to growth suppression and apoptosis induction in human cholangiocarcinoma cells. Oncol Rep. 2016;35:2065–2072. doi: 10.3892/or.2016.4584. [DOI] [PubMed] [Google Scholar]
- 15.Zajc I, Filipič M, Lah TT. Xanthohumol induces different cytotoxicity and apoptotic pathways in malignant and normal astrocytes. Phytother Res. 2012;26:1709–1713. doi: 10.1002/ptr.4636. [DOI] [PubMed] [Google Scholar]
- 16.Colgate EC, Miranda CL, Stevens JF, Bray TM, Ho E. Xanthohumol, a prenylflavonoid derived from hops induces apoptosis and inhibits NF-kappaB activation in prostate epithelial cells. Cancer Lett. 2007;246:201–209. doi: 10.1016/j.canlet.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 17.Yong WK, Abd Malek SN. Xanthohumol induces growth inhibition and apoptosis in ca ski human cervical cancer cells. Evid Based Complement Alternat Med. 2015;2015:921306. doi: 10.1155/2015/921306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wakisaka N, Kondo S, Endo K, Murono S, Yoshizaki T. Adjuvant chemotherapy with an oral fluoropyrimidine, S-1, following reduced RADPLAT in advanced laryngeal cancer. Ann Otol Rhinol Laryngol. 2012;121:555–562. doi: 10.1177/000348941212100810. [DOI] [PubMed] [Google Scholar]
- 19.Melinceanu L, Sarafoleanu C, Lerescu L, Tucureanu C, Caras I, Sălăgeanu A. Impact of smoking on the immunological profile of patients with laryngeal carcinoma. J Med Life. 2009;2:211–218. [PMC free article] [PubMed] [Google Scholar]
- 20.Wan G, Zhou L, Xie M, Chen H, Tian J. Characterization of side population cells from laryngeal cancer cell lines. Head Neck. 2010;32:1302–1309. doi: 10.1002/hed.21325. [DOI] [PubMed] [Google Scholar]
- 21.Qu X, Xu C, Wang H, Xu J, Liu W, Wang Y, Jia X, Xie Z, Xu Z, Ji C, et al. Hippocampal glutamate level and glutamate aspartate transporter (GLAST) are up-regulated in senior rat associated with isoflurane-induced spatial learning/memory impairment. Neurochem Res. 2013;38:59–73. doi: 10.1007/s11064-012-0889-8. [DOI] [PubMed] [Google Scholar]
- 22.Yoshimaru T, Komatsu M, Tashiro E, Imoto M, Osada H, Miyoshi Y, Honda J, Sasa M, Katagiri T. Xanthohumol suppresses oestrogen-signalling in breast cancer through the inhibition of BIG3-PHB2 interactions. Sci Rep. 2014;4:7355. doi: 10.1038/srep07355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang H, Li X, Zhang Y, Luan X. Luteolin induces apoptosis by activating Fas signaling pathway at the receptor level in laryngeal squamous cell line Hep-2 cells. Eur Arch Otorhinolaryngol. 2014;271:1653–1659. doi: 10.1007/s00405-014-2903-z. [DOI] [PubMed] [Google Scholar]
- 24.Corbiere C, Liagre B, Terro F, Beneytout JL. Induction of antiproliferative effect by diosgenin through activation of p53, release of apoptosis-inducing factor (AIF) and modulation of caspase-3 activity in different human cancer cells. Cell Res. 2004;14:188–196. doi: 10.1038/sj.cr.7290219. [DOI] [PubMed] [Google Scholar]
- 25.Chen X, Deng M, Ma L, Zhou J, Xiao Y, Zhou X, Zhang C, Wu M. Inhibitory effects of forkhead box L1 gene on osteosarcoma growth through the induction of cell cycle arrest and apoptosis. Oncol Rep. 2015;34:265–271. doi: 10.3892/or.2015.3969. [DOI] [PubMed] [Google Scholar]
- 26.Akagi T, Shimizu K, Takahama S, Iwasaki T, Sakamaki K, Endo Y, Sawasaki T. Caspase-8 cleavage of the interleukin-21 (IL-21) receptor is a negative feedback regulator of IL-21 signaling. FEBS Lett. 2011;585:1835–1840. doi: 10.1016/j.febslet.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 27.Pan L, Becker H, Gerhäuser C. Xanthohumol induces apoptosis in cultured 40–16 human colon cancer cells by activation of the death receptor- and mitochondrial pathway. Mol Nutr Food Res. 2005;49:837–843. doi: 10.1002/mnfr.200500065. [DOI] [PubMed] [Google Scholar]
- 28.Kunnimalaiyaan S, Sokolowski KM, Balamurugan M, Gamblin TC, Kunnimalaiyaan M. Xanthohumol inhibits Notch signaling and induces apoptosis in hepatocellular carcinoma. PLoS One. 2015;10:e0127464. doi: 10.1371/journal.pone.0127464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang N, Zhang JH, Qiu F, Tashiro S, Onodera S, Ikejima T. Inhibition of EGFR signaling augments oridonin-induced apoptosis in human laryngeal cancer cells via enhancing oxidative stress coincident with activation of both the intrinsic and extrinsic apoptotic pathways. Cancer Lett. 2010;294:147–158. doi: 10.1016/j.canlet.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 30.Kropveld A, Slootweg PJ, van Mansfeld AD, Blankenstein MA, Hordijk GJ. Radioresistance and p53 status of T2 laryngeal carcinoma. Analysis by immunohistochemistry and denaturing gradient gel electrophoresis. Cancer. 1996;78:991–997. doi: 10.1002/(SICI)1097-0142(19960901)78:5<991::AID-CNCR8>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 31.Pei SG, Wang JX, Wang XL, Zhang QJ, Zhang H. Correlation of survivin, p53 and Ki-67 in laryngeal cancer Hep-2 cell proliferation and invasion. Asian Pac J Trop Med. 2015;8:636–642. doi: 10.1016/j.apjtm.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 32.Simsek H, Han U, Onal B, Simisek G. The expression of EGFR, cerbB2, p16, and p53 and their relationship with conventional parameters in squamous cell carcinoma of the larynx. Turk J Med Sci. 2014;44:411–416. doi: 10.3906/sag-1305-9. [DOI] [PubMed] [Google Scholar]
- 33.Ogawa T, Shiga K, Tateda M, Saijo S, Suzuki T, Sasano H, Miyagi T, Kobayashi T. Protein expression of p53 and Bcl-2 has a strong correlation with radiation resistance of laryngeal squamous cell carcinoma but does not predict the radiation failure before treatment. Oncol Rep. 2003;10:1461–1466. [PubMed] [Google Scholar]
- 34.Mendivil-Perez M, Velez-Pardo C, Jimenez-Del-Rio M. TPEN induces apoptosis independently of zinc chelator activity in a model of acute lymphoblastic leukemia and ex vivo acute leukemia cells through oxidative stress and mitochondria caspase-3- and AIF-dependent pathways. Oxid Med Cell Longev. 2012;2012:313275. doi: 10.1155/2012/313275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cho SY, Lee JH, Ju MK, Jeong EM, Kim HJ, Lim J, Lee S, Cho NH, Park HH, Choi K, et al. Cystamine induces AIF-mediated apoptosis through glutathione depletion. Biochim Biophys Acta. 2015;1853:619–631. doi: 10.1016/j.bbamcr.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 36.Yang R, Cui HJ, Wang H, Wang Y, Liu JH, Li Y, Lu Y. N-stearoyltyrosine protects against glutamate-induced oxidative toxicity by an apoptosis-inducing factor (AIF)-mediated caspase-independent cell death pathway. J Pharmacol Sci. 2014;124:169–179. doi: 10.1254/jphs.13184FP. [DOI] [PubMed] [Google Scholar]
- 37.Hunter TB, Manimala NJ, Luddy KA, Catlin T, Antonia SJ. Paclitaxel and TRAIL synergize to kill paclitaxel-resistant small cell lung cancer cells through a caspase-independent mechanism mediated through AIF. Anticancer Res. 2011;31:3193–3204. [PMC free article] [PubMed] [Google Scholar]