Abstract
Background:
Smoking is a learned habit that has an impact on the psychological and biochemical health of individuals. It is the leading preventable cause of chronic illness worldwide. The purpose of this study was to examine the effects of a group-focused cognitive behavioral health education program (GCBHEP) on cigarette smoking in a sample of Nigerian prisoners.
Methods:
The study used a pretest–posttest randomized control group design. Twenty inmates were identified through self-reporting, 1-to-1 counseling, and observation. The treatment group took part in a GCBHEP for 10 weeks, while the control group received 10 weeks’ conventional counseling. After the intervention program, both the treatment and control groups were evaluated. The repeated measures analysis of variance was used for data analysis and partial η2 was also used as a measure of effect size.
Results:
The findings showed that the GCBHEP had a strong effect on cigarette-smoking habits among the inmates in the treatment group compared with those in the control group. The effect of the GCBHEP by age was moderate, and modest by educational qualification.
Conclusion:
Group-focused cognitive behavioral health education is effective in breaking the habit of cigarette smoking among Nigerian prisoners. Therefore, future researchers are encouraged to adopt this approach in helping individuals with a smoking problem and other drug-abuse behaviors in Nigerian prisons.
Keywords: cigarette smoking, cognitive behavioral health education program, habit, inmates, Nigerian prisons, prisoners
1. Introduction
In recent years, one of the main goals of health promotion programs in Nigeria and most parts of the world has been to reduce the prevalence of cigarette smoking. Worldwide, cigarette smoking has damaged the lives of many individuals.[1] Smoking causes cancer, breathing problems, heart attacks, and stroke; second-hand smoke causes asthma and breathing problems.[2] Cigarette smoke contains a mix of thousands of chemicals (from 4000 to 7300) with hundreds of them being very harmful, and about 70 can lead to cancer.[2]
Smoking is a learned habit that affects both the psychological and the biochemical health of individuals. It is the leading preventable cause of chronic illness. More than 420,000 deaths occur each year from cancer and heart and lung disease, and smoking is often a contributory factor.[3] Smokers often become addicted to nicotine, a drug that is found naturally in tobacco.[1] The addictive nature of nicotine is highlighted by the difficulty that smokers exhibit in attempting abstinence. In fact, <7% of smokers who try to stop smoking on their own achieve >1 year of abstinence, and most relapse within a few days of attempting to quit. These smokers experience heightened stress, and smoking briefly restores their stress levels to normal.[4] As a result, breaking a smoking habit can be very difficult and may take a series of repeated attempts and effective strategies to help a smoker reduce and cope with the urge to smoke. An effective evidence-based treatment program that enables individuals to break the habit successfully is therefore needed.[5]
Support groups, nicotine replacement therapy, and other medications can help individuals to quit smoking.[6] People who do manage to stop greatly reduce their risk for disease and early death, and the health benefits are greater for people who stop at a younger age, although there are benefits at any age.[7–9] The most successful approaches in tobacco-use control, however, can be broadly conceptualized as cognitive behavioral therapies.[10] According to Beck, cognitive behavior therapy (CBT) is an effective approach for solving current problems and changing unhelpful thinking and behavior.[11] The CBT approach could be described as being problem-focused, action-oriented, or directive in its therapeutic approach. The CBT approach is a promising psychological intervention for individuals who want to quit smoking, since changing and restructuring thought processes, combined with new learning behaviors, is essential for those who want to effectively quit smoking and maintain cessation.[12]
Previous studies have shown that cognitive behavioral therapies and techniques are effective in breaking the smoking habit. For instance, Sykes and Marks found that self-help CBT intervention had the potential to reduce the prevalence of smoking among lower socioeconomic status smokers.[13] Alireza et al investigated the effectiveness of emotional regulation training group therapy on the emotional and addiction problems of substance abusers. It was found to be effective in reducing the emotional and addiction problems of substance abusers.[14] Raja et al found that CBT was more effective compared with basic health education in helping participants to quit tobacco smoking.[15] Yunusa et al found that a cognitive restructuring intervention program significantly led to tobacco-use cessation in senior secondary school adolescents in Zaria, in the Kaduna State of Nigeria.[16]
In light of this, the group-focused cognitive behavioral health education program (GCBHEP) is an extension of CBT with the capacity to re-educate and reconstruct the problematic mindsets of individual smokers to more rational and adaptive ones with respect to quitting smoking and sustaining the learned behavior. The GCBHEP for breaking the smoking habit (called “the program” hereafter) is a psychoeducation that could become an evidence-based treatment in the prison population. The program focuses on changing a smoker's reactions to the urge to smoke by changing the thought patterns and behaviors of the smoker. In this program, changing the thoughts of participants occurs by examining unhelpful thought patterns that lead to smoking. This happens alongside learning more effective patterns and alternative behaviors that involve identifying the functions that smoking serves, and replacing the smoking with other behaviors that serve the same function. In particular, the behavioral training in mindfulness and emotional regulation techniques of the program can be helpful in coping with particularly strong urges to smoke.[17]
The program comprises 5 techniques designed in modules. It offers holistic behavioral treatment that enables participants to gradually quit cigarette smoking through a series of well-structured module lessons. Generally, a GCBHEP is a group counseling therapy that deals with the concerns of smokers through the use of interpersonal interactions and cognitive behavioral techniques. The group counseling encounter provides the opportunity for participants to build relationships and help one another overcome life issues related to smoking, and find effective ways to explore and support the changes individuals wish to make in their lives.[18] Some group counseling techniques and approaches—such as cognitive restructuring, mindfulness training, stimulus control, emotional regulation training, and self-modification—were incorporated into the group-focused counseling sessions, and this led to what is termed a “GCBHEP,” designed to break prisoners’ cigarette-smoking habit.
The program was deemed appropriate in that the guidance and counseling experience of some of the researchers in the Nigerian Prison Service in Nsukka, in the Enugu State of Nigeria, revealed cigarette smoking to be one of the most challenging habits for prisoners to break. On arrival at the prison, the researchers carried out a Prisoners’ Problem Inventory to identify the problems that the inmates were facing. Cigarette smoking was the top-ranked problem, with 92% of the inmates identified as smokers. Inmates seemed to be experiencing both the ill-health and the psychological effects of this habit, and the habit seemed to be increasing on a daily basis. Personal interactions with the inmates revealed that most had been trying to break this habit using individual approaches but without success. The researchers saw the need to use a group counseling approach to see whether the inmates could be helped to break their cigarette-smoking habit. A treatment program adopting a group counseling approach was necessary to help toward this goal, and also to educate them on the health and psychological implications of their habit.
The study question was, therefore, the following: what effect would a GCBHEP have on the breaking of the cigarette-smoking habit among Nigerian prisoners? The following hypotheses were made: there will be a statistically significant effect of a group-focused program on breaking the cigarette-smoking habit among inmates in the treatment group compared with those in the control group; there will be a statistically significant effect of a group-focused program on breaking the cigarette-smoking habit among prisoners in the treatment group, by age; and there will be a statistically significant effect of a group-focused program on breaking the cigarette-smoking habit among prisoners in the treatment group, by educational qualification.
2. Methods
2.1. Ethical approval
The approval for conducting this study was granted by the Faculty of Education Research Grants Committee, University of Nigeria, Nsukka, and the Nsukka Prison Administration as part of practical work in guidance and counseling. The participants’ informed consent was also obtained.
2.2. Design
The design of this study was a pretest–posttest randomized control group.
2.3. Population and sample
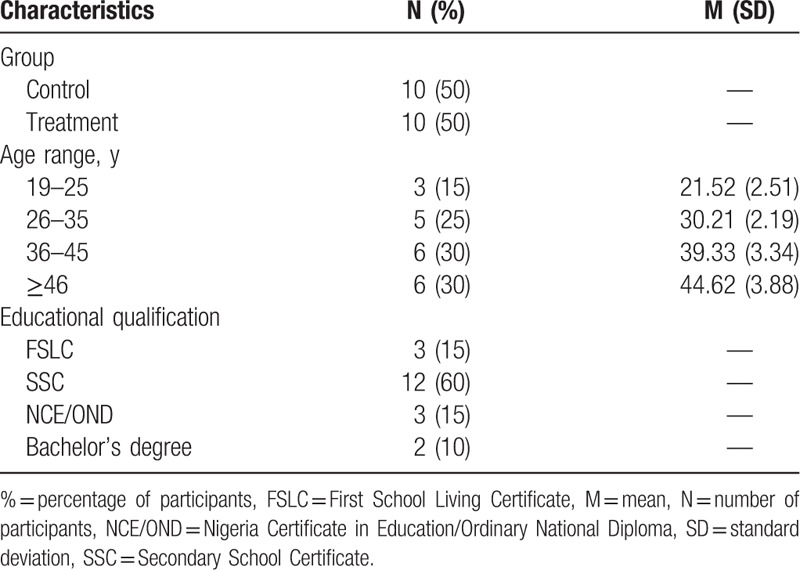
The population was made up of the 301 prisoners held at Nsukka at the time of the study. The sample comprised 20 prison inmates identified through 1-to-1 counseling and observation as having a cigarette-smoking habit. This number is considered ideal for an effective group counseling program.[19]Table 1 shows the demographic characteristics of the participants.
Table 1.
Demographic characteristics of participants.
2.4. Measure
2.4.1. Cigarette Dependence Scale
Cigarette Dependence Scale (CDS-12) is a 12-item scale developed and titled by Etter et al.[20] The CDS-12 covers the key components of Diagnostic and Statistical Manual of Mental Disorders, 4th ed, and International Statistical Classification of Diseases and Related Health Problems, 10th revision, definitions of dependence: compulsion, withdrawal symptoms, loss of control, time allocation, neglect of other activities, and persistence despite harm. The CDS-12 has a high test–retest reliability (r ≥ 0.83) and high internal consistency (Cronbach's α ≥ 0.84). After piloting the instrument twice on 70 prison inmates, the CDS-12 used in the current study yielded a good test–retest reliability (r ≥ 0.90) and internal consistency (Cronbach's α ≥0.86). The English language version of the CDS-12 used in this study also sought participants’ personal information such as age, and educational qualification. The response options in the CDS-12 vary considerably with regard to how each question is structured.
2.5. Procedure
The 301 prison inmates completed the CDS-12 at baseline. Eligible participants were selected and assigned numbers from 1 to 20 using the lottery method. The participants were randomly assigned to either the cognitive behavioral health education program group (treatment group) or the conventional counseling group (control group).
A behavioral chart was used to show the number of times per day each participant smoked before, during, and after the intervention program. The treatment process took up to 20 sessions and was scheduled for twice a week, making a total of 10 weeks plus 4 weekly follow-up sessions held after 6 months. Each session lasted for 40 minutes. The inmates in the control group were given 10 weeks of conventional counseling, and so were included in the evaluation process but not in the treatment program.
Participants with higher scores on the CDS-12 were chosen, although participants were more eligible if they reported smoking cigarette regularly in the past 30 days. Participants also needed to be able to attend the counseling sessions held in the prison hall. Both the treatment and control groups took part in the final evaluation at the end of the program. Figure 1 shows the eligibility criteria of the participants by treatment and control groups.
Figure 1.
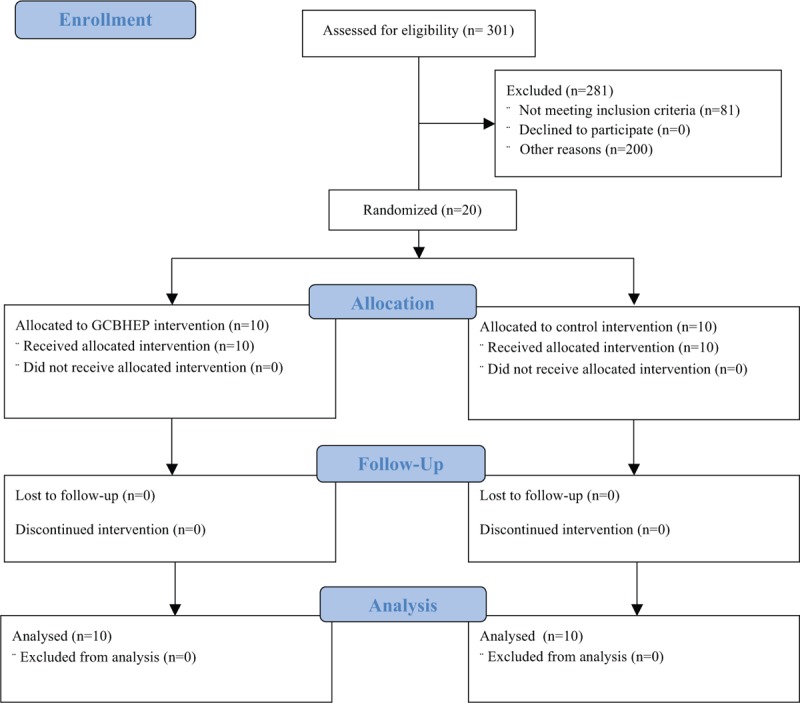
Participants’ eligibility criteria. GCBHEP = group-focused cognitive behavioral health education program.
2.6. Data analysis
The repeated measures analysis of variance (ANOVA) was used to test the hypotheses at a 0.05 probability level. A repeated measures ANOVA (2 repeated assessments—time as a within-subjects factor; group, age, and educational qualification as between-subjects factors) was conducted on the outcome variable. Mean, standard deviation, and partial eta squared
 |
were also reported. The effect size of the treatment was determined using Muijs’ criteria[21] as follows: 0 to 0.1, weak effect; 0.1 to 0.3, modest effect; 0.3 to 0.5, moderate effect; >0.5, strong effect.
2.7. Intervention package
The treatment process was guided by a group-focused cognitive behavioral health education training manual developed by the researchers. The manual had 5 modules. Every treatment module lasted for 2 weeks with sessions of 40 minutes each.
2.7.1. Module 1: cognitive restructuring
The cognitive restructuring session played a central role in the group-focused program. This module session lasted for 2 weeks. The cognitive restructuring technique was used to help clients correct their problematic thought processes about cigarette smoking and change them to adaptive ones. The session adopted the 3 phases of Meichenbaum's cognitive restructuring approach[22] to facilitate changes in the clients’ behavior as follows:
Phase 1: The first step in the change process consists of clients learning to observe their own behavior. When clients begin therapy, their internal dialogue is characterized by negative self-statements and imagery. A critical factor is their willingness and ability to listen to themselves. This process involves an increased sensitivity to their thoughts, feelings, actions, physiological reactions, and ways of reacting to others. As the group counseling progresses, clients are expected to acquire new cognitive structures that will enable them to view their problems in a new way. This reconceptualization process comes about through the collaborative effort of the clients and the counselor.
Phase 2: When the client–counselor contact is initiated at the early stage of the program, clients learn to perceive smoking as a maladaptive behavior, and begin to see opportunities for breaking the habit. Clients hope to achieve change by initiating a new behavioral chain. At this stage, clients learn to change their internal dialogue through counseling, and the new internal dialogue serves as a guide to new behavior. In turn, this process influences clients’ cognitive structures.
Phase 3: The third phase of the counseling process consists of teaching clients more effective coping skills that are practiced in real-life situations. At the same time, clients continue to focus on learning new adaptive skills while observing and recording the outcomes. The stability of what they learn is greatly influenced by what they say to themselves about their newly acquired or intended behavior and its consequences.
2.7.2. Module 2: mindfulness training
Mindfulness has to do with developing attention control, nonjudgmental awareness, and a sense of “true self.” Participants learn to simply observe and then describe events, thoughts, emotions, and body sensations, and fully participate in their actions and experiences in a nonevaluative manner, focusing on one thing at a time and reorienting attention when distracted.[23] Mindfulness helps clients become aware of their mind from one moment to the next, with gentle acceptance.[24] In mindfulness practice, clients train themselves to focus on their present experience. Mindfulness training is, therefore, a good avenue for the integration of spirituality into the counseling process. In this study, the skill taught in the mindfulness session was meditation. The study's participants were provided with life-transforming scripture verses to meditate upon because they were all Christians. One portion of the scripture was used per day for 1 week. They were also given a script on the effects of smoking to meditate upon in order to realize what was happening to them and how it would be if they continued to smoke. The participants were given meditation time of 15 minutes every day. This module session lasted for 2 weeks.
2.7.3. Module 3: self-modification training
This module session also lasted for 2 weeks. This training was used to help clients have a direct role in their own treatment. Because this technique aims at self-change, it increases clients’ involvement and commitment to their treatment.[19] Self-modification strategies used include self-monitoring, self-reward, self-contracting, stimulus control, and self-as-model. The basic idea of this training is that behavioral change can be brought about by teaching individuals to use coping skills in problematic situations. In this module, generalization and maintenance of the outcomes are enhanced by encouraging participants to accept the responsibility for implementing the self-modification strategies in their daily life.
2.7.4. Module 4: impulse tolerance and emotional regulation training
The objective of this module session was to help participants develop positive emotions that reflected on their intention to quit smoking. In this session, participants were taught how to control impulses and manage their emotions in the knowledge that smoking could be due to emotional imbalance. Emotion regulation involves learning skills to decrease labile affect. It includes learning to identify, label, and describe emotions, using mindfulness around the emotional experience, reducing vulnerability to negative emotions, increasing the occurrence of positive emotions, and acting in opposition to the motivational tendency associated with negative emotion.[23] The participants are expected to acquire abilities to control their impulses and become more aware of themselves and others. The participants are also expected to become more effective at describing and regulating their emotions.
2.7.5. Module 5: psychodrama
This last module focused on a psychodrama with the theme “cigarette smokers are liable to die young.” This was used to enable the participants in the study to perceive the health and psychological consequences of smoking, how they could give up smoking habits, and what benefits they could gain by not relapsing. Every group member had a role to play in acting out the psychodrama through role reversal. Individual participants shared with the researchers and group members the lessons they learned at the end of each psychodrama session. This module session lasted for 2 weeks.
3. Results
The result of the data analysis in Table 2 shows that the treatment group had a pretest mean score of 84.60 ± 2.95, while the control group had a pretest mean score of 82.60 ± 2.95. With an exact probability value of 0.06, which is greater than the a priori probability value of 0.05, the result confirmed that both groups did not significantly differ at pre-intervention in their cigarette-smoking habit: F(1,18) = 4.157, P = 0.06,
 |
.
Table 2.
Summary statistics for repeated measures analysis of variance showing effect of group-focused cognitive behavioral health education program on cigarette-smoking habit-breaking among prison inmates by treatment condition and time.
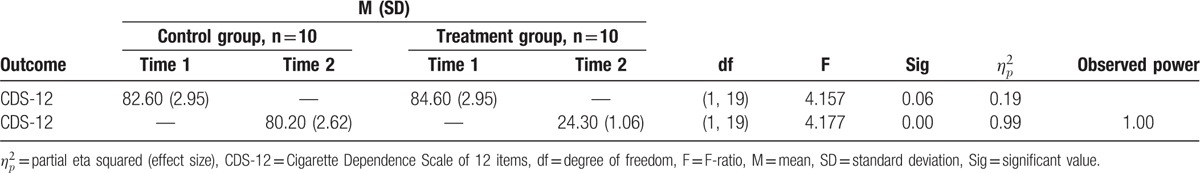
After the intervention, however, the treatment group had a posttest mean score of 24.30 ± 1.06, while the control group had a posttest mean score of 80.20 ± 2.62. Thus, Table 2 also shows the exact probability value of 0.00, which is less than the a priori probability value of 0.05 at post-intervention. Therefore, there is statistically significant effect of the program on breaking the cigarette-smoking habit among prisoners in the treatment group compared with the control group: F(1,18) = 4.177, P = 0.00. The value of
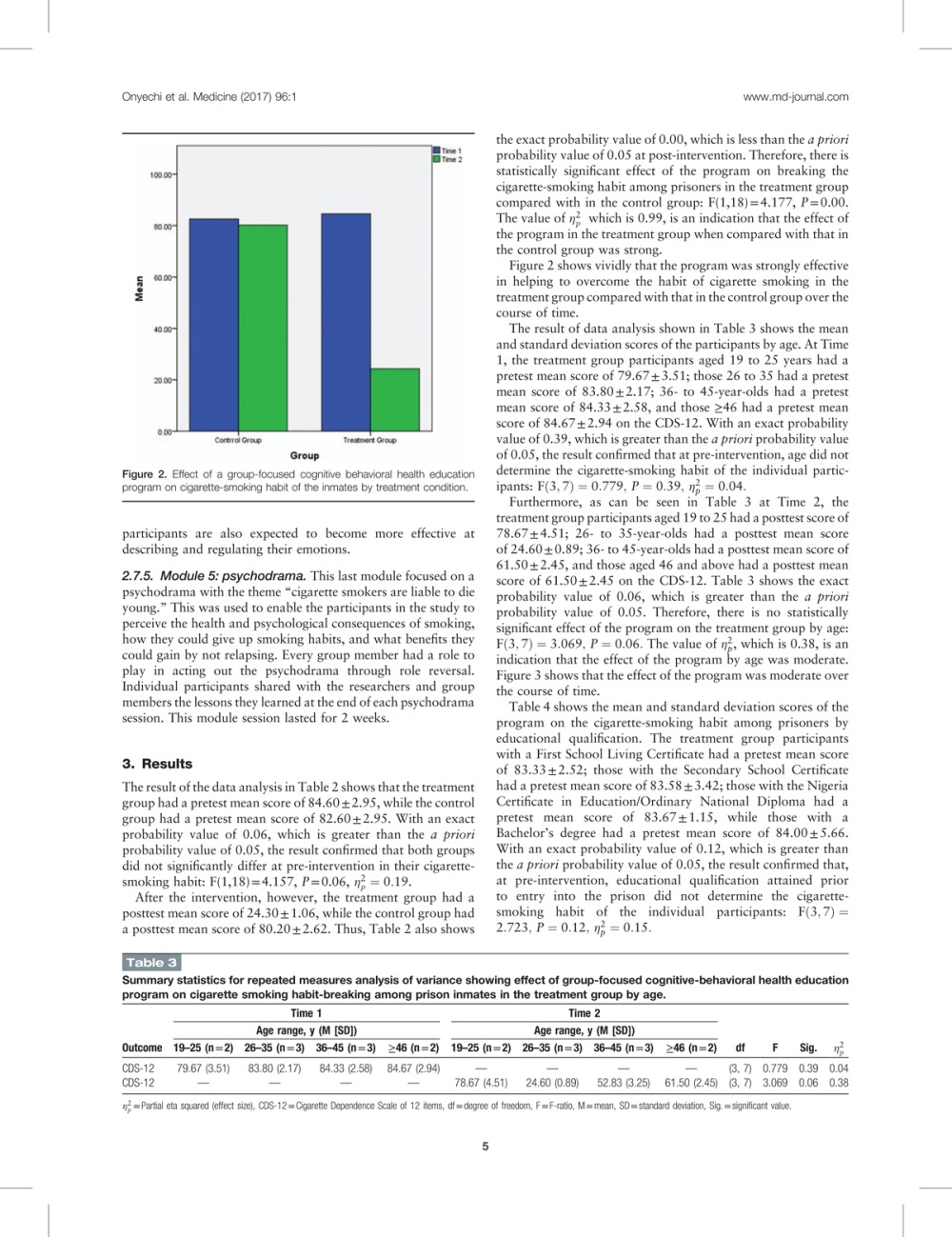 |
, which is 0.99, is an indication that the effect of the program in the treatment group when compared with those in control group was strong.
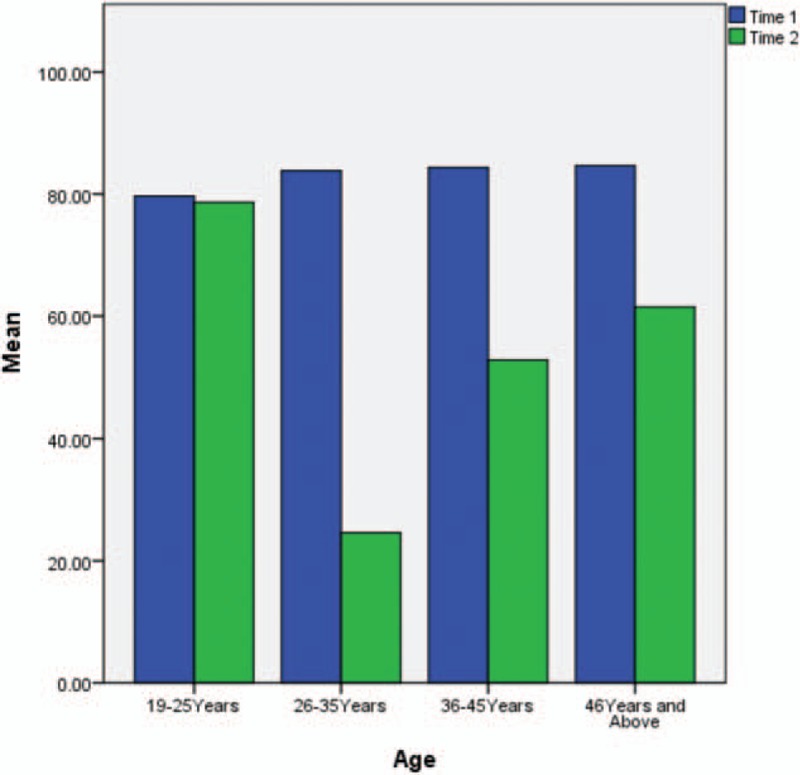
Figure 2 shows vividly that the program was strongly effective in helping to overcome the habit of cigarette smoking in the treatment group compared with that in the control group over the course of time.
Figure 2.
Effect of a group-focused cognitive behavioral health education program on cigarette-smoking habit of the inmates by treatment condition.
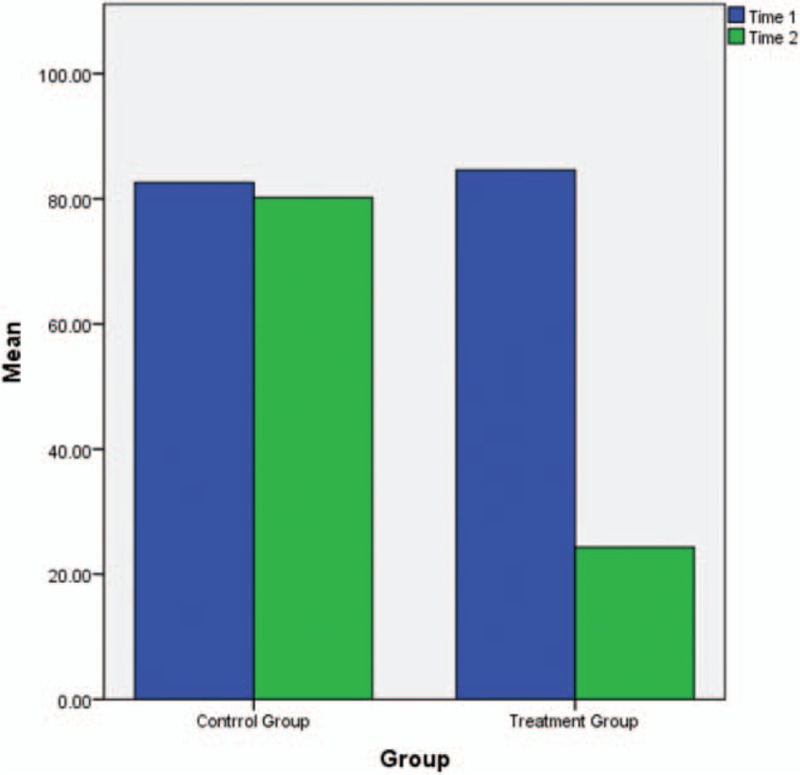
The result of data analysis shown in Table 3 shows the mean and standard deviation scores of the participants by age. At Time 1, the treatment group participants aged 19 to 25 years had a pretest mean score of 79.67 ± 3.51; those 26 to 35 had a pretest mean score of 83.80 ± 2.17; 36- to 45-year-olds had a pretest mean score of 84.33 ± 2.58, and those ≥46 had a pretest mean score of 84.67 ± 2.94 on the CDS-12. With an exact probability value of 0.39, which is greater than the a priori probability value of 0.05, the result confirmed that at pre-intervention, age did not determine the cigarette-smoking habit of the individual participants:
 |
Table 3.
Summary statistics for repeated measures analysis of variance showing effect of group-focused cognitive-behavioral health education program on cigarette smoking habit-breaking among prison inmates in the treatment group by age.
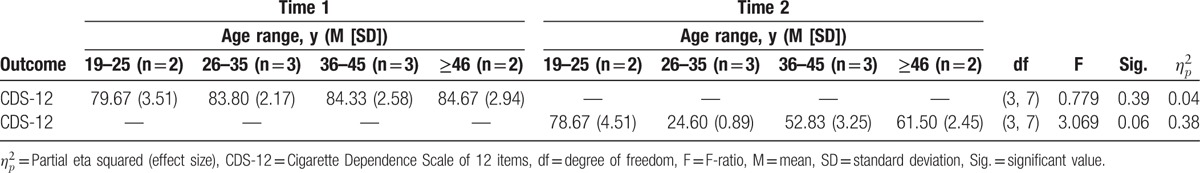
Furthermore, as can be seen in Table 3 at Time 2, the treatment group participants aged 19 to 25 had a posttest score of 78.67 ± 4.51; 26- to 35-year-olds had a posttest mean score of 24.60 ± 0.89; 36- to 45-year-olds had a posttest mean score of 61.50 ± 2.45, and those aged 46 and above had a posttest mean score of 61.50 ± 2.45 on the CDS-12. Table 3 shows the exact probability value of 0.06, which is greater than the a priori probability value of 0.05. Therefore, there is no statistically significant effect of the program on the treatment group by age: F(3,7) = 3.069, P = 0.06. The value of
 |
, which is 0.38, is an indication that the effect of the program by age was moderate. Figure 3 shows that the effect of the program was moderate over the course of time.
Figure 3.
Effect of a group-focused cognitive behavioral health education program on cigarette-smoking habit of the inmates by age.
Table 4 shows the mean and standard deviation scores of the program on the cigarette-smoking habit among prisoners by educational qualification. The treatment group participants with a First School Living Certificate had a pretest mean score of 83.33 ± 2.52; those with the Secondary School Certificate had a pretest mean score of 83.58 ± 3.42; those with the Nigeria Certificate in Education/Ordinary National Diploma had a pretest mean score of 83.67 ± 1.15, while those with a Bachelor's degree had a pretest mean score of 84.00 ± 5.66. With an exact probability value of 0.12, which is greater than the a priori probability value of 0.05, the result confirmed that, at pre-intervention, educational qualification attained prior to entry into the prison did not determine the cigarette-smoking habit of the individual participants:
 |
Table 4.
Summary statistics for repeated measures analysis of variance showing effect of group-focused cognitive-behavioral health education program in the treatment group by educational qualification.
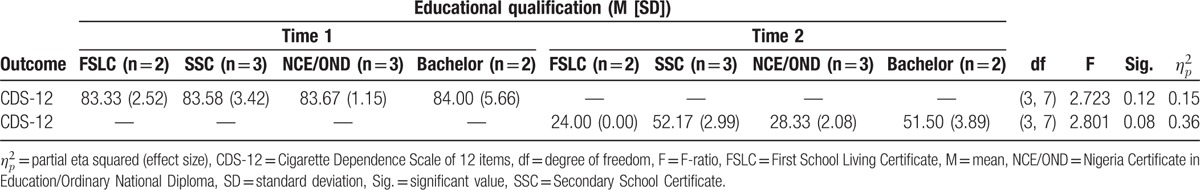
Treatment group participants with the FSLC had a posttest mean score of 24.00 ± 0.00; those with an SSC had a posttest mean score of 52.17 ± 2.99; those with an NCE/OND had a posttest mean score of 28.33 ± 2.08, and those with a degree had a posttest mean score of 51.50 ± 3.89. Table 4 shows the exact probability value of 0.08, which is greater than the a priori probability value of 0.05. Therefore, there is no statistically significant effect of the program on breaking the cigarette smoking in the treatment group by educational qualification: F = (3,7) = 2.801, P = 0.08. The value of
 |
, which is 0.36, is an indication that the effect of the program by educational qualification was modest. Figure 4 shows that the effect of the program by educational qualification was modest over the course of time.
Figure 4.
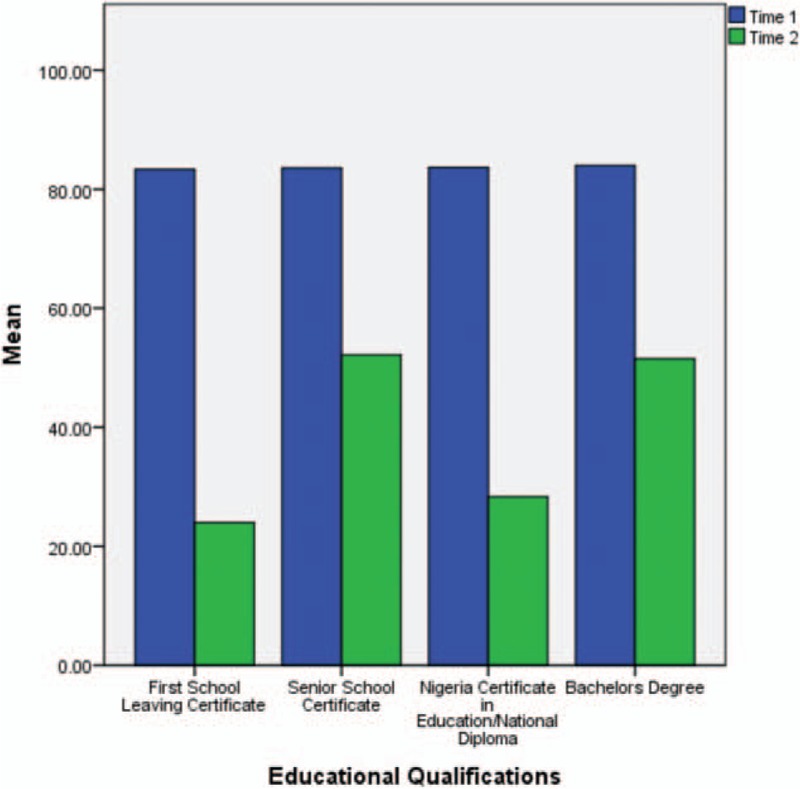
Effect of a group-focused cognitive behavioral health education program on cigarette-smoking habit of the inmates by educational qualification.
4. Discussion
This study examined the effects of a GCBHEP on breaking the cigarette-smoking habit among a sample of Nigerian prisoners. The baseline results show that the participants in both treatment and control groups were active cigarette smokers. At the end of the intervention program, there were noticeable changes in the smoking habits of the prison inmates in the treatment group compared with in those in the control group. Overall, the researchers found that the GCBHEP was strongly effective in breaking the habit for those in the treatment group compared with for those in the control group. The researchers also found that the effect of the program was moderate by age, and its effect by educational qualification was modest. Besides age and educational qualifications as mediating variables, the study's results support previous studies[11,15,16] that effectively used CBT to achieve smoking cessation. The current result also supports those of Sykes and Marks,[13] who found that a CBT intervention has the potential to help smokers stop smoking.
In the current study, the GCBHEP techniques were effective in restructuring the thought patterns of participants, helping them realize that smoking would not help them live a comfortable life, but could ruin their lives. Individual participants’ problematic thinking and beliefs about cigarette smoking were modified, and the inmates conditioned their minds toward maintaining a nonsmoking habit. The modules enabled the inmates to think about the realities surrounding their smoking habit. The cognitive behavioral techniques helped the participants adjust to a new life without smoking and they were expected to continue to sustain this lifestyle even outside the prison environment. The implication is, therefore, that new behaviors and coping skills for managing the smoking habit were acquired, and that these would enable participants to live a cigarette-free life. The present findings are strengthened by the fact that the positive effects of CBT treatments and techniques on various problem behaviors among inmates have been documented by several researchers.[25–33] With group-focused cognitive behavior health education to target irrational and faulty thoughts that increase the likelihood of cigarette smoking, the individual is able to gain increased adaptive and functional behaviors against this habit.
4.1. Limitations
The first noticeable limitation is the difficulty involved in ascertaining whether the sample is representative of the general prison population. This clinical trial included a very low number of participants; however, trials using a CBT approach are not usually affected by small sample sizes.[34]
The second limitation is that only male inmates took part in the current study. It may be that different outcomes would result with female prisoners or mixed groups. The findings may not be fully generalizable. The researchers suggest, therefore, that future research should use larger samples and carry out cross-sectional and more in-depth longitudinal follow-up studies to ascertain the validity of the present findings.
The study's design faces the drawbacks of repeated measures ANOVA within-subject designs in that there is no 1 specific design without a limitation. However, the researchers hope that more rigorous methodologies will be applied by future researchers to test empirically the efficacy of a GCBHEP in correctional institutions. Other recommendations would be to conduct comparative investigations with other approaches in terms of cost-effectiveness and efficacy and to carry out follow-up assessments at around 6 to 12 months.
4.2. Practical implications
Despite the observed limitations, the study has important implications for research and practice. The main aim of behavioral change programs in Nigerian prisons is to transform the lives of the inmates. Nigerian cognitive behavioral therapists are expected to help inmates quit smoking through effective interventions. Because smoking is a learned habit and is difficult to give up, mere discouragement is not effective. Psychoeducational treatment programs that can help inmates break the habit without any observable syndrome would be more appropriate. Nigerian prison counselors need to familiarize themselves with GCBHEPs to help inmates break smoking habits successfully. These programs are beneficial in that they combine CBT and basic health education to yield effective results. Nigerian prison counselors also need to ensure that all categories of inmates with smoking habit are helped, whatever their age and educational level. Because the effectiveness of the GCBHEP is in the techniques and the treatment procedure, researchers should follow the same steps and techniques to generate positive outcomes.
The implication of this study for policy making is that counseling programs should be fully used in Nigerian prisons to transform the lives of inmates before release. The lack of counselors in the Nigerian prison system undermines the objectives of the national rehabilitation framework.
5. Conclusion
The researchers conclude that group-focused cognitive behavioral health education is effective in breaking the cigarette-smoking habit of inmates in Nigerian prisons. The age and education level of the prison inmates are important factors to consider in implementing such a program. The researchers therefore encourage future researchers to adopt this approach in helping Nigerian prison inmates with cigarette-smoking habits and other drug-related behavior.
Acknowledgement
We deeply appreciate the Editor-in-Chief, the Anonymous Reviewers, the Academic Editor, and the Production Manager for their assistance in improving the quality of this report. We also thank the Staff and Inmates in the Nigeria Prisons Service at Nsukka, Enugu State for giving us the opportunity to conduct this research as part of our clinical experience.
Footnotes
Abbreviations: ANOVA = analysis of variance, CBT = cognitive behavior therapy, CDS-12 = Cigarette Dependence Scale, GCBHEP = group-focused cognitive behavioral health education program.
The authors have no conflicts of interest to disclose.
References
- [1].National Institute on Drug Abuse. Tobacco/Nicotine. Research Report Series 3. July 2012. NIH publication no. 16-4342. Available at: https://www.drugabuse.gov/publications/research-reports/tobacco/nicotine-addictive [accessed February 28, 2016]. [Google Scholar]
- [2].Centers for Disease Control and Prevention. Chemicals in Tobacco Smoke. 2011. Available at: http://www.cdc.gov/tobacco/data_statistics/sgr/2010/consumer_booklet/chemicals_smoke/ [accessed November 27, 2015]. [Google Scholar]
- [3].Carey B. In clue to addictive behavior, a brain injury halts smoking. New York Times. Vol 1 January 26, 2007:18. [Google Scholar]
- [4].Parrott AC. Does cigarette smoking cause stress? Am Psychol 1999;54:817–20. [DOI] [PubMed] [Google Scholar]
- [5].Prochaska JO, Velicer WF, DiClemente C, et al. Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol 2008;56:520–8. [DOI] [PubMed] [Google Scholar]
- [6].WebMD Smoking Cessation Health Center. Smoking Cessation Overview. 2015. Available at: http://www.webmd.com/smoking-cessation/ [accessed October 28, 2015]. [Google Scholar]
- [7].Stead LF, Perera R, Bullen C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2012;11:CD000146. [DOI] [PubMed] [Google Scholar]
- [8].U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis For Smoking-Attributable Disease. A report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [Google Scholar]
- [9].U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- [10].The Cancer Council. Cessation: Theories-About-Smoking-and-Quitting. Chapter 7. 2015. Available at: http://www.tobaccoinaustralia.org.au/7–13-methods-services-and-products-for-quitting-co [accessed October 13, 2015]. [Google Scholar]
- [11].Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd ed2011;New York, NY:The Guilford Press, 19–20. [Google Scholar]
- [12].Virtual Medical Center. Cognitive-Behavioral Therapy (CBT) for Quitting Smoking. 2015. Available at: http://www.myvmc.com/treatments/cognitive-behavioural-therapy-cbt-for-quitting-smoking/ [accessed October 20, 2015]. [Google Scholar]
- [13].Sykes CM, Marks DF. Effectiveness of a cognitive behaviour therapy self-help programme for smokers in London, UK. Health Promot Int 2001;16:255–60. [DOI] [PubMed] [Google Scholar]
- [14].Alireza MA, Ahmad B, Mahmoud G. The effectiveness of emotion regulation training and cognitive therapy on the emotional and addictional problems of substance abusers. Iran J Psychiatry 2010;5:60–5. [PMC free article] [PubMed] [Google Scholar]
- [15].Raja M, Saha S, Mohd S, et al. Cognitive behavioral therapy versus basic health education for tobacco cessation among tobacco users: a randomized clinical trial. J Clin Diagn Res 2014;8:ZC47–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yunusa U, Abdullahi MI, Oliagba O, et al. The effect of cognitive restructuring intervention on tobacco smoking among adolescents in senior secondary school in Zaria Kaduna State, Nigeria. Eur Sci J 2014;10:327–36. [Google Scholar]
- [17].Abadinsky H. Drug Use and Abuse: A Comprehensive Introduction. Belmont, CA:Wadsworth Publishing; 2007. [Google Scholar]
- [18].Wimmer CL. Group Counseling. Ames, IA:Iowa State University; 2015. [Google Scholar]
- [19].Corey G. Theory and Practice of Counseling and Psychotherapy. Australia:Thompson Brooks/Cole; 2009. [Google Scholar]
- [20].Etter J, Houezec JL, Perneger TV. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 2003;28:359–70. [DOI] [PubMed] [Google Scholar]
- [21].Muijs D. Doing Quantitative Research in Education With SPSS. London:Sage; 2004. [Google Scholar]
- [22].Meichenbaum D. Cognitive Behavior Modification: An Integrative Approach. New York:Plenum Press; 1977. [Google Scholar]
- [23].Soler J, Pascual JC, Tiana T, et al. Dialectical behavior therapy skills training compared to standard group therapy in borderline personality disorder: a 3-month randomised controlled clinical trial. Behav Res Ther 2009;47:353–8. [DOI] [PubMed] [Google Scholar]
- [24].Germer CK. Germer CK, Siegel RD, Fulton PR. Teaching mindfulness in therapy. Mindfulness and Psychotherapy. New York:Guilford Press; 2005. 113–29. [Google Scholar]
- [25].Asonaba KA, Antwi T, Avonokadzi IK. Impact of cognitive restructuring on students with low self esteem and academic performance in Dambai College of Education in the Volta region of Ghana. Pro J Humanit Soc Sci 2014;2:1–6. [Google Scholar]
- [26].Adeusi SO. Efficacy of Cognitive Restructuring and Behavioral Rehearsal on Conduct Disorder in Adolescents in Special Correctional Centres in Lagos State. PhD thesis. Ota, Ogun State, Nigeria: Department of Psychology, Covenant University; 2013. [Google Scholar]
- [27].Osarenren N, Ajaero I. Effects of cognitive restructuring and assertiveness training on the self-esteem and family relationship of victims of sibling maltreatment among junior students in Lagos State. Res J Organ Psychol Educ Stud 2013;2:93–100. [Google Scholar]
- [28].Shih A. The Impact of Punitive vs. Rehabilitative Justice Systems on Juvenile Criminal Recidivism. Lexington, VA:Washington and Lee University; 2008. [Google Scholar]
- [29].Gatotoh AM, Omulema BEE, Nassimu D. Correctional attitudes: an impetus for a paradigm shift in inmate rehabilitation. Int J Humanit Soc Sci 2011;1:263–70. [Google Scholar]
- [30].Cullen FT, Gendreau P. Horney J. Assessing correctional rehabilitation: policy, practice, and prospects. Criminal Justice: Policies, Processes, and Decisions of the Criminal Justice System. Washington, DC:U.S. Department of Justice, Office of Justice Programs, National Institute of Justice (NCJ); 2000. 109–75. [Google Scholar]
- [31].Rogers P. What Works: Effective Recidivism Reduction and Risk-Factor Prevention Programs. A compendium of evidence-based options for preventing new and persistent criminal behavior prepared for the Colorado division of criminal justice United Kingdom; 2008. [Google Scholar]
- [32].Lipsey MW, Cullen FT. The effectiveness of correctional rehabilitation: a review of systematic reviews. Annu Rev Law Soc Sci 2007;3:297–320. [Google Scholar]
- [33].Obikwelu CL. Effect of Need-Focused Cognitive Restructuring Intervention Program on Self-Esteem and Self-Efficacy of Recidivist Inmates in the Prisons in Nigeria. PhD thesis. Nsukka, Enugu State, Nigeria: Department of Educational Foundations, University of Nigeria; 2015. [Google Scholar]
- [34].Eseadi C, Anyanwu JI, Ogbuabor SE, et al. Effects of cognitive restructuring intervention program of rational-emotive behavior therapy on adverse childhood stress in Nigeria. J Ration Emot Cogn Behav Ther 2016;34:51–72. [Google Scholar]


