Abstract
Mucosal melanomas represent a rare entity with different risk factors and molecular features compared to cutaneous melanomas. They arise most commonly from mucosal surfaces in the head/neck region, the female genital tract (FGT) and the anorectal region. The aim of this study was to evaluate clinics, prognosis, and treatment options of patients with mucosal melanoma, in particular with regard to different primary sites.
We retrospectively analyzed 75 patients with mucosal melanomas diagnosed in the years 1993 to 2015 in our department. The primary melanomas were located in the head/neck region (n = 32), the FGT (n = 24), and the anorectal region (n = 19).
The median age of the patients was 66 years. At initial diagnosis the primary melanoma was not completely resectable in 11 (15%) patients, 18 (24%) patients had regional lymph node metastases, and 7 (9%) patients distant metastases. During follow-up, 22 (29%) patients suffered from a local recurrence, in particular patients with primary melanoma in the head/neck region without postoperative radiotherapy. By multivariate analysis location of the primary melanoma in the head/neck area or anorectal region and presence of metastases at time of diagnosis represented poor prognostic factors for recurrence-free survival. In 62 tested individuals 7 KIT mutations were found, 2 BRAF mutations in 57 tested patients. Four patients received targeted therapies, 14 checkpoint inhibitors, 4 (1/1 on vemurafenib, 1/7 on ipilimumab, and 2/7 on PD-1 inhibitors) patients showed responses of more than 100 days duration.
Mucosal melanomas are often locally advanced or metastatic at initial diagnosis, thus they require extensive staging procedures. The high rate of local recurrences in the head/neck region can be significantly reduced by postoperative radiotherapy. For the potential use of medical treatment a mutation analysis for KIT and BRAF genes should be performed. The use of new immunologic and targeted therapies has to be further evaluated.
Keywords: CTLA-4, immunotherapy, mucosal melanoma, PD-1 inhibitor, prognosis, radiotherapy, targeted therapy
1. Introduction
Mucosal melanomas are a rare clinical entity, in the literature the incidence is described with 1% to 2% of all melanomas and 2 to 2.6 per 1,000,000 persons/year.[1–3] Melanomas arising from mucosal surfaces have a different profile of risk factors (eg, no exposure to ultraviolet radiation) and other genetic mutations than cutaneous melanomas, especially KIT-mutations are more frequent in mucosal melanomas.[4] Mucosal melanomas have a poor prognosis which is much worse than that of cutaneous melanomas.[1] It remains uncertain whether the poorer prognosis is due to the usually more progressed disease at initial diagnosis or to the biologically more aggressive growth. Prognostic factors are not well established thus far.[5] Therefore, we have retrospectively analyzed 75 patients with mucosal melanomas at different locations of the primary tumor in regard to their prognostic factors. Furthermore, we summarized our experiences using new immunologic and targeted therapies.
2. Patients und methods
2.1. Patients
Patients of our Department including the years 1993 to 2015 with primary mucosal melanomas were recorded in a database, their history was regularly updated. The patients were divided in 3 groups in regard to the location of the primary tumor: head/neck, anorectal, and female genital tract (FGT). Since the American Joint Committee on Cancer-classification[6] for cutaneous melanoma is not established for mucosal melanoma, we implemented 3 groups for a clinical tumor grading according to the Mucosal Melanoma Staging System published by Iversen and Robins[7] in 1980 and proposed by Thoelke et al: I – local tumor, II – regional lymph node metastasis, and III – distant metastasis.[8,9]
The follow-up, adjuvant and palliative therapy, was done according to the recommendations for patients with cutaneous melanomas.[10] One patient with a KIT Exon 11 L576P Mutation was treated with imatinib, this case has already been published as a case report.[11] The median follow-up time was 32 months, with a minimum of 2 and a maximum of 231 months.
Mutation analysis was performed partly in the context of scientific research,[12] others within clinical trials and routine clinical treatment. Sixty-two patients were screened for KIT and 57 patients for BRAF-mutations by various methods: Sanger sequencing for the KIT-gene and on 5 patients for the BRAF-gene, further analysis of the BRAF-gene was performed via melting curve analysis for 29 and pyrosequencing for 23 patients.
The ethics committee of the Hannover Medical School provided IRB approval for the retrospective data collection of melanoma patients (vote no. 1612–2012).
2.2. Statistical analysis
The Programs Statistica 8 (Statsoft), GraphPad Prism version 5.01 for Windows, GraphPad Software, and EpiInfo 3.5.3 (Centers for Disease Control and Prevention) were used for the statistical analysis.
The evaluation included the usual descriptive statistics (mean, median, and percentages) and survival analysis with the Kaplan–Meier estimate. The Log-Rank-test was used for the calculation of significance for the overall and relapse-free survival between the groups. The influence of various prognostic factors was tested on the basis of the Cox proportional hazard model. The initial group comparison (Table 1) for nominal data was done with the Chi-square test or Fisher exact test, respectively, for the comparison of multiple groups with ordinal or metric data by use of the Kruskal–Wallis test. A P-value < 0.05 was considered significant.
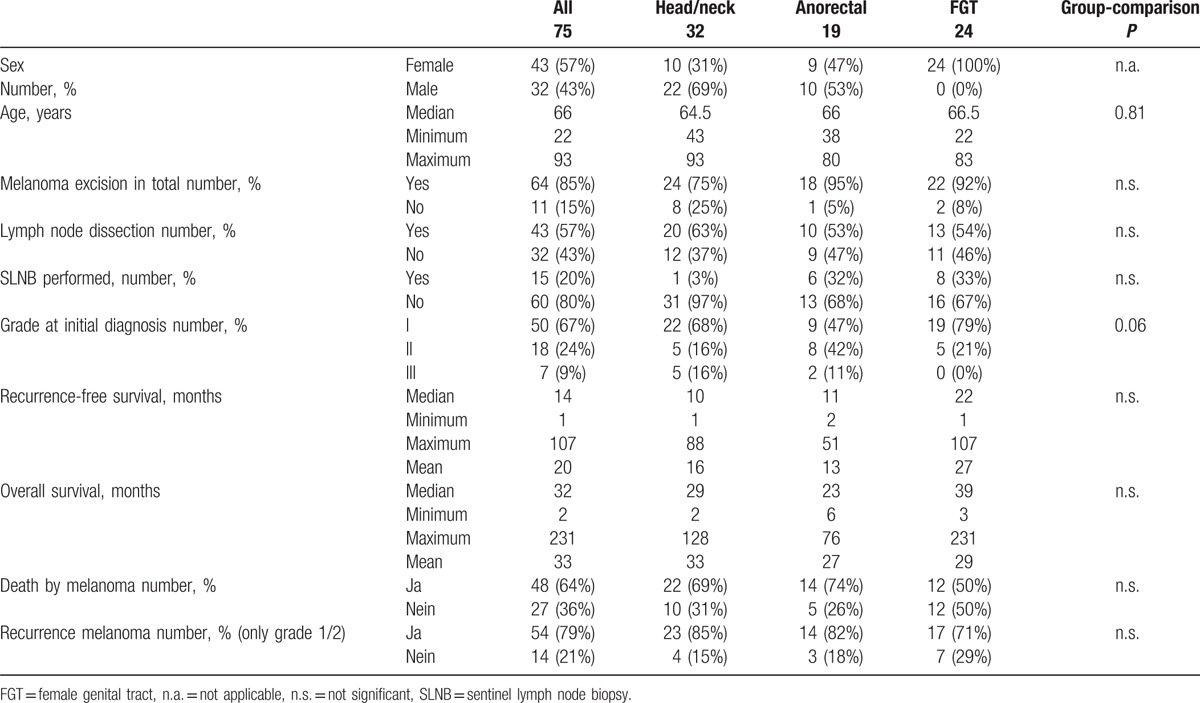
Table 1.
Characterization of the patients in regard to localization.
3. Results
3.1. Clinical parameters
We identified 75 patients with mucosal melanomas, 32 melanomas were localized in the head/neck area, 24 melanomas were situated in the FGT, and 19 melanomas were diagnosed in the anorectal region, respectively (Table 1).
The median age at the time of 1st diagnosis was 66 years, with 57% female and 43% male patients. The overall higher percentage of females is due to patients with a melanoma in the FGT, tumors in the head/neck region occurred more often in males, whereas anorectal melanomas were evenly distributed between females and males (Table 1). After initial diagnosis the total excision of the mucosal melanoma could be achieved in 64/75 patients (85%). Total lymphadenectomy of the regional lymph nodes was performed in 43/75 patients (57%), 20 of which had metastasis at time of initial diagnosis, 8 following a positive sentinel lymph node (SLN), and 15 as an elective procedure (Table 1).
A total of 34/75 patients received an adjuvant therapy. Adjuvant radiotherapy was applied in 20 patients, 17 of them with the primary tumor in the head/neck region, 2 with anorectal, and 1 with FGT tumors.
Adjuvant interferon alpha with a dosage of 3 × 3 million units per week for 24 month was administered to 21 patients, 5 of them also had succeeding adjuvant radiotherapy.
3.2. Prognosis
A recurrence of the disease was recorded in 48/61 (79%) of the patients where an initial complete excision had been realized. The median time until the 1st recurrence was 14 month (Table 1). An initial local recurrence or in transit metastasis was recorded in 18/48 patients, regional lymph node metastasis in 8/48 patients, and distant metastasis in 22/48 patients.
During follow-up 48/75 (64%) patients died of the melanoma, 1/75 (1.3%) patients of others causes. The median overall survival through all groups was 32 months (Table 1).
3.3. Prognostic factors in the univariate analysis for the overall and recurrence-free survival
The 5-year survival rate was 26.3%, 22.0% in the head/neck group, 10.6% anorectal, and 33.2% in the FGT group. Patients with the melanoma in the head/neck region and anorectal region displayed a significant worse overall survival than patients with melanomas in the FGT (P = 0.04, Table 2, Fig. 1B).
Table 2.
Univariate analysis of the prognostic factors (log rank test).
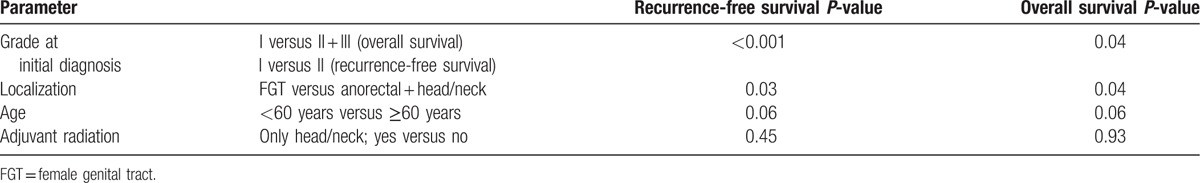
Figure 1.
Kaplan–Meier analysis of survival in regard to the location of the tumor (A and B), tumor grade at time of 1st diagnosis (C and D), age (E), and different time frames (F).
The probability for recurrence-free survival after 5 years was 13.8% overall 3 groups, 8.1% with mucosal melanoma in the head/neck region, and 23.8% in the FGT, a 5-year follow-up period was not reached for anorectal tumors (Fig. 1A). Again a significant advantage could be demonstrated for the group with melanomas in the FGT for the recurrence-free survival versus the patients with anorectal and head/neck tumors (P = 0.03, Table 2).
For patients under 60 years of age at the time of 1st diagnosis we saw a trend for an advantage in overall and recurrence-free survival (P = 0.06, Table 2, Fig. 1E).
Patients in disease stage I at the time of 1st diagnosis had significant advantage in terms of overall survival (P = 0.04, Fig. 1D, Table 2) and a highly significant for the recurrence-free survival (P < 0.001, Table 2) in comparison with patients with stages II and III at the time of the initial diagnosis.
In regard to gender no significance for overall and recurrence-free survival could be demonstrated.
Because of the long period of observation we divided the patients in 3 groups, 1993 to 2005, 2006 to 2009, and 2010 to 2015, the comparison showed no significant difference between the groups for recurrence-free survival and overall survival (Fig. 1F).
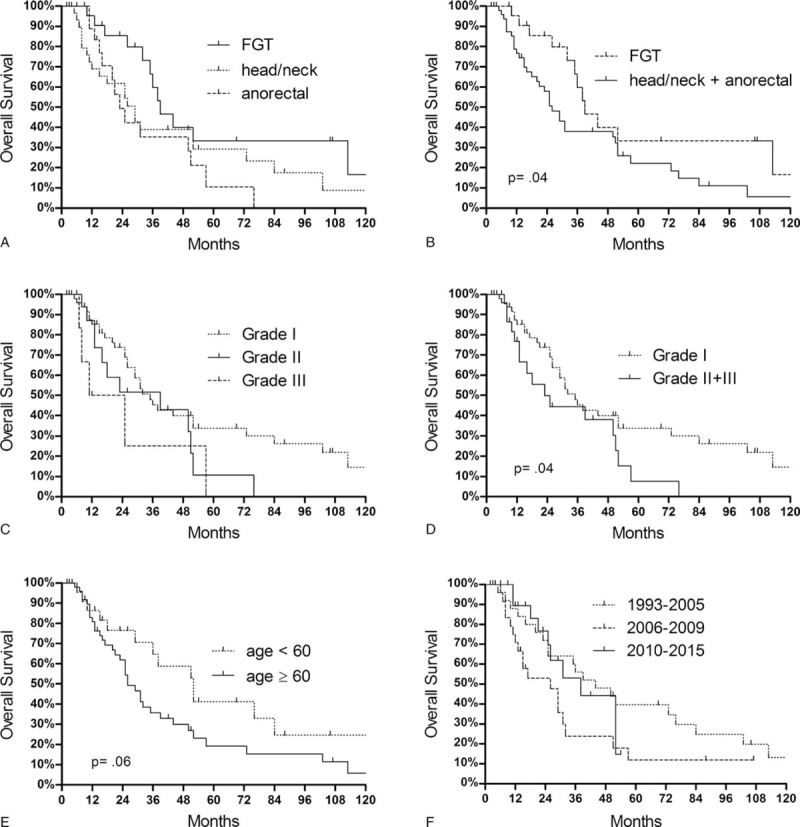
In the group of head/neck mucosal melanomas, in which the major part of the adjuvant radiation took place, a significant advantage (P = 0.02) toward the prevention of local recurrences was shown (Fig. 2).
Figure 2.
Impact of adjuvant radiation on the way of metastazation for 30 patients with mucosal melanoma in the head/neck region. (2 Patients with severe distant metastazation at the time of the initial diagnosis were not included).
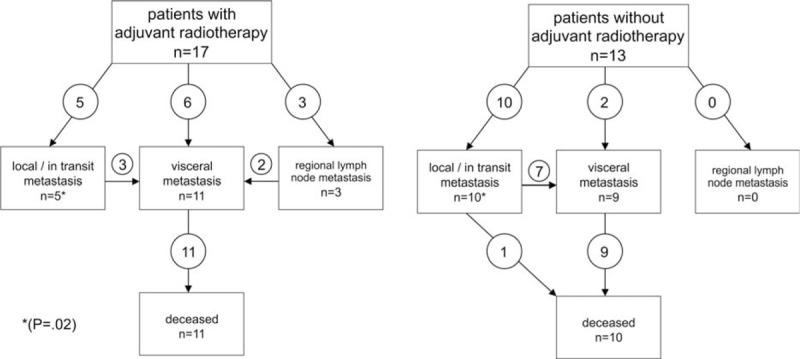
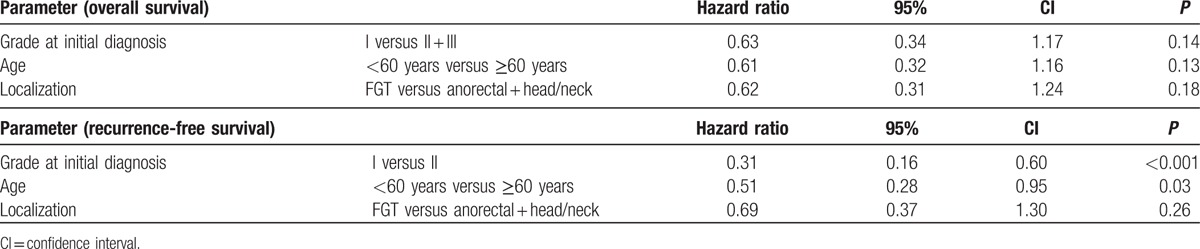
As expected the multivariate analysis (Table 3) showed a high statistical significance for the tumor-stage at time of the initial diagnosis in terms of recurrence-free survival (P < 0.001). Also age younger than 60 was correlated with a significant recurrence-free survival benefit (P = 0.03). In contrast the localization of the primary did not reach any independent prognostic significance.
Table 3.
Multivariate analysis of the prognostic factors (Cox proportional hazard).
3.4. KIT/BRAF mutations
A molecular analysis of the KIT-gene was performed in 62 of the patients studied. A total of 7/62 (11.3%) of the patients had a KIT mutation, 5 in exon 11 (once each 579del, K550N, W557R, twice L576P), 1 in exon 13 (K642E), and 1 in exon 18 of the KIT-gene (I841V). The analysis for 36 patients was done in our own laboratory (exons 9, 11, 13, 17, and 18), 6 of them showed a KIT-mutation. These results were already described in detail.[12] Within the TEAM-study (Tasigna Efficacy in Advanced Melanoma) the KIT-exons 9, 11, 13, and 17 were analyzed in 6 further patients, all 6 patients did not show a mutation. Another 20 analyses were done during routine diagnostics employing Sanger-Sequencing of the exons 9, 11, and 13, which revealed a K642E-mutation in 1 patient. In regard to localization of the primary tumor KIT-mutations were shown in 2/27 (7.4%) patients in the head/neck region, 2/16 (12.5%) anorectal, and 3/19 (15.8%) in the FGT.
A BRAF V600E Mutation was demonstrated in 2/57 (3.5%) of the patients, one each in the anorectal and head/neck-group.
3.5. Targeted therapy and therapy with checkpoint inhibitors
Four patients were treated with targeted therapies, patients 1 to 3 with imatinib due to a KIT-mutation in exon 11 or 13. Patient 1 achieved a short-term partial remission (PR), patient 2 a short-term stable disease (SD) (Table 4).
Table 4.
Therapy with targeted therapies and checkpoint inhibitors.
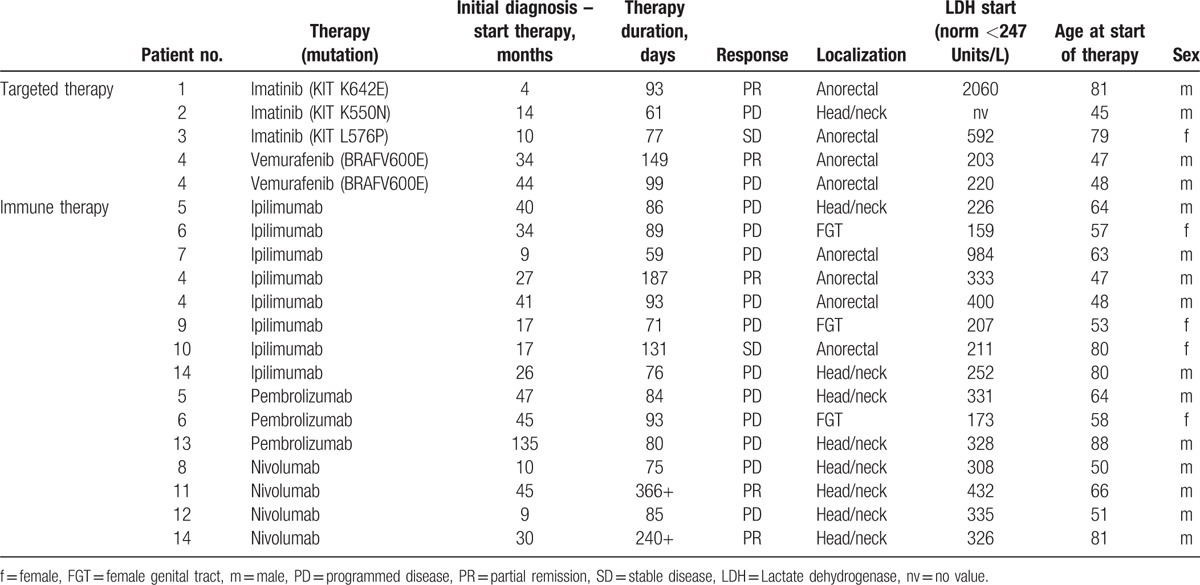
Patient 4 (Table 4) is a male patient with a metastasized anorectal melanoma harboring a BRAF mutation. Therapy with ipilimumab yielded in a PR for 6 month, subsequent vemurafenib-therapy resulted in a PR for another 5 month. Reexposition first with ipilimumab then with vemurafenib did not lead to any further tumor control.
Besides these patients 6 other patients were treated with ipilimumab (Table 4), one of those had an SD for 4.5 months. Seven patients received programmed disease-1 (PD-1)-checkpoint inhibitors (Table 4), in 2 patients a PR lasting 366+ and 240+ days was achieved.
4. Discussion
Mucosal melanoma is disease of advanced age, among our patients the median age over all 3 groups was 66 years corresponding well to the spectrum described in the literature ranging from 60 to 75 years.[8,13–17]
The gender distribution with 57% female patients was consistent with other observations and can be explained by the patients with melanoma in the FGT.[15,18] As described in the literature male patients suffered more often (69%) from mucosal melanomas in the head/neck region.[16] Anorectal melanomas showed a fairly balanced gender distribution with 53% male patients in our study in contrast to the literature where mostly a higher ratio of male patients is described.[16,19]
An SLN biopsy is particularly possible if lymph drainage into peripheral lymph stations is expected, for example, distal the linea dentata for anal melanomas[20] or vulvar melanomas in the FGT.[21] In individual cases SLN biopsy is described even for mucosal melanomas in the head/neck region.[19] Contrary to cutaneous melanomas the SLN is not established as a prognostic factor in mucosal melanoma. For having a poor prognosis in respect of distant metastasis a complete regional lymph node dissection following a positive SLN is discussed controversially.[20,21]
During follow-up 79% of the patients had a recurrence, especially mucosal melanomas in the head/neck region demonstrated a short recurrence-free survival time with a median of 10 months. In our study 64% of the patients died during follow-up, the 5-year survival rate was 26.3%, which is slightly lower than indicated in the literature with 5-year survival rates of 32.4%,[22] 34%,[15] and up to 55.8%.[23]
In line with expectations, the tumor-grade is an important prognostic factor as described in the literature.[17,22]
In our study, the age with a threshold value of 60 years was an additional important prognostic factor. In the literature age is described as a prognostic factor for either mucosal melanomas[14,22] and skin melanomas.[24]
A better prognosis for tumors in the FGT became apparent in our univariate analysis but could not be confirmed in the multivariate analysis. Mehra et al[23] could also show a better prognosis for vulvar melanomas in comparison to other localizations of the primary tumor.
Local recurrence occurred notably in patients with the primary tumor in the head/neck region, which had not undergone adjuvant radiotherapy, among the adjuvant group the local tumor control was significantly better.
Some studies already have shown that adjuvant radiation of mucosal melanomas in the head/neck region can reduce the risk of local recurrence from 33%–83% to 0%–56%.[19] Another study could demonstrate that at least 54 Gray should be applied to have a positive effect.[25]
For KIT-mutations we could show a higher rate in mucosal melanomas in the FGT (15.8%) in comparison to the other 2 groups, head/neck (7.4%) and anorectal (12.5%). This is consistent with a recent publication that outlined the highest rate of KIT-mutations for vulvovaginal melanomas (35%) followed by anorectal melanomas (25%) and mucosal melanomas in the head/neck region (10%).[26]
In our patient collection, the treatment with imatinib showed 1 short-term SD and 1 short-term PR in 2 of 3 patients with KIT-mutations in exon 11 and 13, respectively (Table 4).
In the literature, several case series describe an objective response in 16% to 30% of the patients treated imatinib, the median time for recurrence-free survival was about 3 months, with major benefit for patients with mutations in exon 11 and 13.[27–29]
In a case series with 7 patients with mucosal melanomas and KIT-mutations in exon 11 or 13 sunitinib showed a response in 3 cases.[30]
A reason for the relative poor response to KIT-inhibitors could be a concurrent NRAS-mutation, which are described in patients with KIT-mutations.[29] This results in activation of the pathway downstream of KIT, thus it is advisable to rule out NRAS-mutations before using a KIT-inhibitor.
BRAF-mutations are described in mucosal melanoma. In our cohort 3.5% of the patients examined displayed a BRAF-mutation, in the literature the values differ from 3.6%,[31] 6%[32] up to 11.1%,[33] and 16.5%.[34] Little is published on the response of targeted therapies in BRAF positive patients with mucosal melanomas, the response in our patient suggests that this is possible.
For the use of ipilimumab for the treatment of metastatic mucosal melanoma there are case studies mostly on pretreated patients. In a series of 30 patients (76% of which with the dosing of 3 mg/kg bodyweight, 24% with 10 mg per/kg) 1 patient responded with a complete remission, 1 patient with a PR, and 5 patients with an SD.[35] In a series of 71 patients in the Italian “early access program” a response rate of 12.5% and a 36% rate of SD was observed.[36]
On the use of PD-1 inhibitors in mucosal melanomas there are individual case reports.[37–39] A pooled analysis of mucosal melanomas in a variety of trials using nivolumab (n = 86), nivolumab plus ipilimumab (n = 35), or ipilimumab (n = 36) provided evidence for an effect of nivolumab in mucosal melanomas.[40] The median progression-free survival and response rates were 2.96 months and 23.2% for nivolumab, 5.85 months and 37.2% for nivolumab plus ipilimumab, and 2.69 months and 8.3% for ipilimumab, respectively. This corresponds well with our data showing a long-lasting response in 2/7 patients treated with PD-1 inhibitors.
5. Conclusions
In our study, mucosal melanomas displayed a poor prognosis with metastasis often being already present at the time of initial diagnosis.
We could confirm the recommendation for an adjuvant radiation of the primary tumor region on patients with head/neck mucosal melanomas in order to significantly lower the risk of local recurrence.
In case of metastazation considered inoperable targeted therapies and immunotherapies with checkpoint inhibitors can be considered. PD-1 inhibitors or their combination with ipilimumab appear to show the highest response rates and longest progression-free survival. In case of a KIT mutation, additional analysis of NRAS is recommended before treating with a KIT-inhibitor. In the rare event of a BRAF V600 mutation, targeted therapy analogous to cutaneous melanomas is recommended.
The limitations of this study are the small number of patients and the long period of patient acquisition, in particular the low number of patients with targeted and immunotherapy treatment. Therefore, no conclusions with regard to therapy standards can be achieved.
Footnotes
Abbreviations: FGT = female genital tract, PD-1 = programmed disease-1, PR = partial remission, SD = stable disease, SLN = sentinel lymph node, SLNB = sentinel lymph node biopsy.
The authors have no conflicts of interest to disclose.
References
- [1].Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma. Cancer 1998;83:1664–78. [DOI] [PubMed] [Google Scholar]
- [2].Marcoval J, Moreno A, Peyrí J. Cutaneous infiltration by cancer. J Am Acad Dermatol 2007;57:577–80. [DOI] [PubMed] [Google Scholar]
- [3].McLaughlin CC, Wu XC, Jemal A, et al. Incidence of noncutaneous melanomas in the US. Cancer 2005;103:1000–7. [DOI] [PubMed] [Google Scholar]
- [4].Curtin JA, Busam K, Pinkel D, et al. Somatic activation of KIT in distinct subtypes of melanoma. J Clin oncol 2006;24:4340–6. [DOI] [PubMed] [Google Scholar]
- [5].Mallone S, De Vries E, Guzzo M, et al. Descriptive epidemiology of malignant mucosal and uveal melanomas and adnexal skin carcinomas in Europe. Eur J Cancer 2012;48:1167–75. [DOI] [PubMed] [Google Scholar]
- [6].Balch CM, Gershenwald JE, Soong S-j, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol 2009;27:6199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Iversen K, Robins RE. Mucosal malignant melanomas. Am J Surg 1980;139:660–4. [DOI] [PubMed] [Google Scholar]
- [8].Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. J Am Acad Dermatol 2007;56:828–34. [DOI] [PubMed] [Google Scholar]
- [9].Thoelke A, Willrodt S, Hauschild A, et al. Primary extracutaneous malignant melanoma: a comprehensive review with emphasis on treatment. Onkologie 2004;27:492–9. [DOI] [PubMed] [Google Scholar]
- [10].Garbe C, Schadendorf D, Stolz W, et al. Short German guidelines: malignant melanoma. J Deutsch Dermatol Ges 2008;6(s1):S9–14. [DOI] [PubMed] [Google Scholar]
- [11].Satzger I, Kuttler U, Volker B, et al. Anal mucosal melanoma with KIT-activating mutation and response to imatinib therapy – case report and review of the literature. Dermatology 2010;220:77–81. [DOI] [PubMed] [Google Scholar]
- [12].Satzger I, Schaefer T, Kuettler U, et al. Analysis of c-KIT expression and KIT gene mutation in human mucosal melanomas. Br J Cancer 2008;99:2065–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Koomen ER, de Vries E, van Kempen LC, et al. Epidemiology of extracutaneous melanoma in The Netherlands. Cancer Epidemiol Biomarkers Prevent 2010;19:1453–9. [DOI] [PubMed] [Google Scholar]
- [14].Kim HS, Kim EK, Jun HJ, et al. Noncutaneous malignant melanoma: a prognostic model from a retrospective multicenter study. BMC Cancer 2010;10:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bishop KD, Olszewski AJ. Epidemiology and survival outcomes of ocular and mucosal melanomas: a population-based analysis. Int J Cancer 2014;134:2961–71. [DOI] [PubMed] [Google Scholar]
- [16].Gru AA, Becker N, Dehner LP, et al. Mucosal melanoma: correlation of clinicopathologic, prognostic, and molecular features. Melanoma Res 2014;24:360–70. [DOI] [PubMed] [Google Scholar]
- [17].Keller DS, Thomay AA, Gaughan J, et al. Outcomes in patients with mucosal melanomas. J Surg Oncol 2013;108:516–20. [DOI] [PubMed] [Google Scholar]
- [18].DeMatos P, Tyler DS, Seigler HF. Malignant melanoma of the mucous membranes: a review of 119 cases. Ann Surg Oncol 1998;5:733–42. [DOI] [PubMed] [Google Scholar]
- [19].Gavriel H, McArthur G, Sizeland A, et al. Review: mucosal melanoma of the head and neck. Melanoma Res 2011;21:257–66. [DOI] [PubMed] [Google Scholar]
- [20].Carcoforo P, Raiji M, Palini G, et al. Primary anorectal melanoma: an update. J Cancer 2012;3:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dhar K, Das N, Brinkman D, et al. Utility of sentinel node biopsy in vulvar and vaginal melanoma: report of two cases and review of the literature. Int J Gynecol Cancer 2007;17:720–3. [DOI] [PubMed] [Google Scholar]
- [22].Jethanamest D, Vila PM, Sikora AG, et al. Predictors of survival in mucosal melanoma of the head and neck. Ann Surg Oncol 2011;18:2748–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Mehra T, Grözinger G, Mann S, et al. Primary localization and tumor thickness as prognostic factors of survival in patients with mucosal melanoma. PLoS One 2014;9:e112535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kretschmer L, Starz H, Thoms KM, et al. Age as a key factor influencing metastasizing patterns and disease-specific survival after sentinel lymph node biopsy for cutaneous melanoma. Int J Cancer 2011;129:1435–42. [DOI] [PubMed] [Google Scholar]
- [25].Moreno MA, Roberts DB, Kupferman ME, et al. Mucosal melanoma of the nose and paranasal sinuses, a contemporary experience from the MD Anderson Cancer Center. Cancer 2010;116:2215–23. [DOI] [PubMed] [Google Scholar]
- [26].Schoenewolf NL, Bull C, Belloni B, et al. Sinonasal, genital and acrolentiginous melanomas show distinct characteristics of KIT expression and mutations. Eur J Cancer 2012;48:1842–52. [DOI] [PubMed] [Google Scholar]
- [27].Guo J, Si L, Kong Y, et al. Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol 2011;29:2904–9. [DOI] [PubMed] [Google Scholar]
- [28].Carvajal RD, Antonescu CR, Wolchok JD, et al. KIT as a therapeutic target in metastatic melanoma. JAMA 2011;305:2327–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Hodi FS, Corless CL, Giobbie-Hurder A, et al. Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol 2013;31:3182–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Minor DR, Kashani-Sabet M, Garrido M, et al. Sunitinib therapy for melanoma patients with KIT mutations. Clin Cancer Res 2012;18:1457–63. [DOI] [PubMed] [Google Scholar]
- [31].Zebary A, Jangard M, Omholt K, et al. KIT, NRAS and BRAF mutations in sinonasal mucosal melanoma: a study of 56 cases. Br J Cancer 2013;109:559–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Omholt K, Grafström E, Kanter-Lewensohn L, et al. KIT pathway alterations in mucosal melanomas of the vulva and other sites. Clin Cancer Res 2011;17:3933–42. [DOI] [PubMed] [Google Scholar]
- [33].Baiter M, Schuler G, Hartmann A, et al. Pathogenetic implications of BRAF mutation distribution in stage IV melanoma patients. Dermatology 2015;231:127–33. [DOI] [PubMed] [Google Scholar]
- [34].Lian B, Si L, Cui C, et al. Phase II randomized trial comparing high-dose IFN-(2b with temozolomide plus cisplatin as systemic adjuvant therapy for resected mucosal melanoma. Clin Cancer Res 2013;19:4488–98. [DOI] [PubMed] [Google Scholar]
- [35].Postow MA, Luke JJ, Bluth MJ, et al. Ipilimumab for patients with advanced mucosal melanoma. Oncologist 2013;18:726–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Del Vecchio M, Di Guardo L, Ascierto PA, et al. Efficacy and safety of ipilimumab 3 mg/kg in patients with pretreated, metastatic, mucosal melanoma. Eur J Cancer 2014;50:121–7. [DOI] [PubMed] [Google Scholar]
- [37].Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med 2013;369:134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Min L, Hodi FS. Anti-PD1 following ipilimumab for mucosal melanoma: durable tumor response associated with severe hypothyroidism and rhabdomyolysis. Cancer Immun Res 2014;2:15–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ohtsuka M, Miura T, Mori T, et al. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol 2015. [DOI] [PubMed] [Google Scholar]
- [40].Larkin J, D’Angelo S, Sosman JA, et al. Efficacy and safety of nivolumab monotherapy in the treatment of advanced mucosal melanoma, society for melanoma research 2015 congress, abstract. Pigment Cell Melanoma Res 2015;28:789. [Google Scholar]


