Supplemental Digital Content is available in the text
Keywords: apolipoprotein A1, apolipoprotein B, type 2 diabetes
Abstract
The ratio of ApoB/apolipoprotein A1 (ApoA1) has been found to be associated with type 2 diabetes, and it was proposed as a new biomarker for type 2 diabetes predictions. Previous studies have assumed that the association between apoB/apoA1 and type 2 diabetes was linear. However, the linearity assumption has rarely been examined. In the present study, we aimed to examine whether this association showed a linear trend in a nationally representative population.
Participants aged 18 years and over (n = 8220) were selected from the China Health Nutrition Survey (CHNS). We used restricted cubic spline to model the association between ApoB/ApoA1 ratio and type 2 diabetes using logistic regression models. Additionally, we categorized the ApoB/ApoA1 ratio according to quartiles to compare with previous results. Age, gender, education, smoking status, high sensitivity C-reactive protein (hsCRP), lipid, body mass index (BMI), and hypertension were controlled as potential confounders.
We found that the association between apoB/apoA1 ratio and type 2 diabetes may be nonlinear after adjusting for multiple potential confounders. Compared with the lowest quartile of apoB/apoA1 ratio, participants in the fourth quartile had a higher odds of type 2 diabetes [odds ratio (OR) = 1.35, 95% confidence interval (CI) = 1.01–1.81].
Our results suggest that, higher apoB/apoA1 ratio was associated with higher prevalence of type 2 diabetes. However, the association may be nonlinear.
1. Introduction
Recent studies reported the prevalence of type 2 diabetes has been rapidly increasing for the last decades.[1,2] Given the high prevalence of type 2 diabetes and its complications, investigating its etiology, exploring the most modifiable risk factors, and searching for the predictive clinical parameters are of extreme importance for type 2 diabetes prevention and treatment.[3–5] Apolipoproteins are the primary structural proteins for lipoprotein particles. Apolipoprotein B (ApoB) is the basic apolipoprotein for low density lipoprotein cholesterol (LDL) and apolipoprotein A1 (ApoA1) is the major apolipoprotein for high density lipoprotein cholesterol (HDL). Thus, the ratio of ApoB/ApoA1 could reflect the cholesterol balance of these atherogenic and antiatherogenic lipid particles. Several previous studies suggested that the elevated ApoB to ApoA1 ratio was a more powerful parameter than other lipid fractions for metabolic disorders including type 2 diabetes.[5–9] However, these studies also assumed that the relationship between ApoB to ApoA1 ratio and type 2 diabetes risk was linear, which was seldom examined in published literatures.
In the present study, we aimed to investigate the association between ApoB to ApoA1 ratio and type 2 diabetes and to examine whether the association was linear in a national representative sample with more than 8000 participants from the China Health and Nutrition Survey (CHNS).[10]
2. Methods
2.1. Study participants
The CHNS started in 1989 and aimed to understand the changes of health status with the follow-up intervals of 2 or 3 years.[10] The CHNS selected individuals from 228 communities and was designed to represent 56% of China's population from 9 provinces. All participants provided written informed consent. Details about the study design were reported elsewhere.[10] In the 2009 wave of CHNS, blood samples were collected and assessed for the first time. Institutional review board of the University of North Carolina at Chapel Hill and the Chinese Center for Disease Control and Prevention approved this study. In our study, we excluded those with missing information on ApoB, ApoA, type 2 diabetes, or other interested variables. Altogether, 8220 adults aged 18 years and over were included in the analysis.
2.2. Data collection
All participants were interviewed by trained physicians and nutritionists using a validated questionnaire to collect demographic, anthropometric, and lifestyle data, which included date of birth, gender, education, height, weight, and smoking. Height and weight were measured by physicians following a standard protocol similar to that developed by the National Center for Health Statistics for the National Health and Nutrition Examination Survey in the United States of America. Height was measured without shoes and rounded to the nearest 0.1 cm. Weight was recorded in light clothing to the nearest 0.1 kg.
2.3. Measurements of glucose, lipid, and HbA1c
Blood samples were collected by venipuncture after an overnight fast. Plasma and serum samples were then frozen, and stored at −86°C for laboratory analysis. The samples were analyzed in a national central lab in Beijing (medical laboratory accreditation certificate ISO 15189:2007) with strict quality control. Type 2 diabetes was defined as fasting glucose ≥7.0 mmol/L or current usage of antidiabetes medications, or HbA1c ≥6.5%.
2.4. Covariates
Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters. Education level was classified into 0 to 9 years, 10 to 12 years, and ≥13 years. Smoking status was categorized as never smoker, former smoker, and current smoker. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or current antihypertensive drug use.
2.5. Statistical analysis
In the descriptive analysis, we presented the basic characteristics of the study participants as mean (standard deviation) for continuous variables and number (percentage) for category variables by quartiles of ApoB/ApoA1 ratio. Chi-square test was applied to compare the differences of category variables among the quartiles, while ANOVA was used for continuous variables. Then we used multivariable logistic regression models to examine the association between ApoB/ApoA1 ratio and type 2 diabetes by restricted cubic spline method for the continuous ApoB/ApoA1 ratio after adjusting the multiple covariates, and plotted the odds ratio (OR) and 95% confidence interval (CI) against this ratio. We constructed 3 models to examine the association between ApoB/ApoA1 ratio and type 2 diabetes. The first model included ApoB/ApoA1 ratio to estimate the crude association, while the second model was further adjusted for age and gender. The third model was additionally adjusted for education, smoking status, hsCRP, hypertension, BMI, and lipid. These variables were considered as potential confounders which may bias the observed estimates. Because of the close relationship between HDL and ApoA1, additional analyses were performed to examine the association between the non-HDL/HDL ratio and type 2 diabetes and to calculate the area under the receiver operating characteristic (ROC) curve for the performance of these lipid ratios. P values were 2-tailed and P < 0.05 was considered as statistical significance. All analysis was conducted using R 3.2.
3. Results
3.1. Demographic characteristics of participants by ApoB/ApoA1 ratio
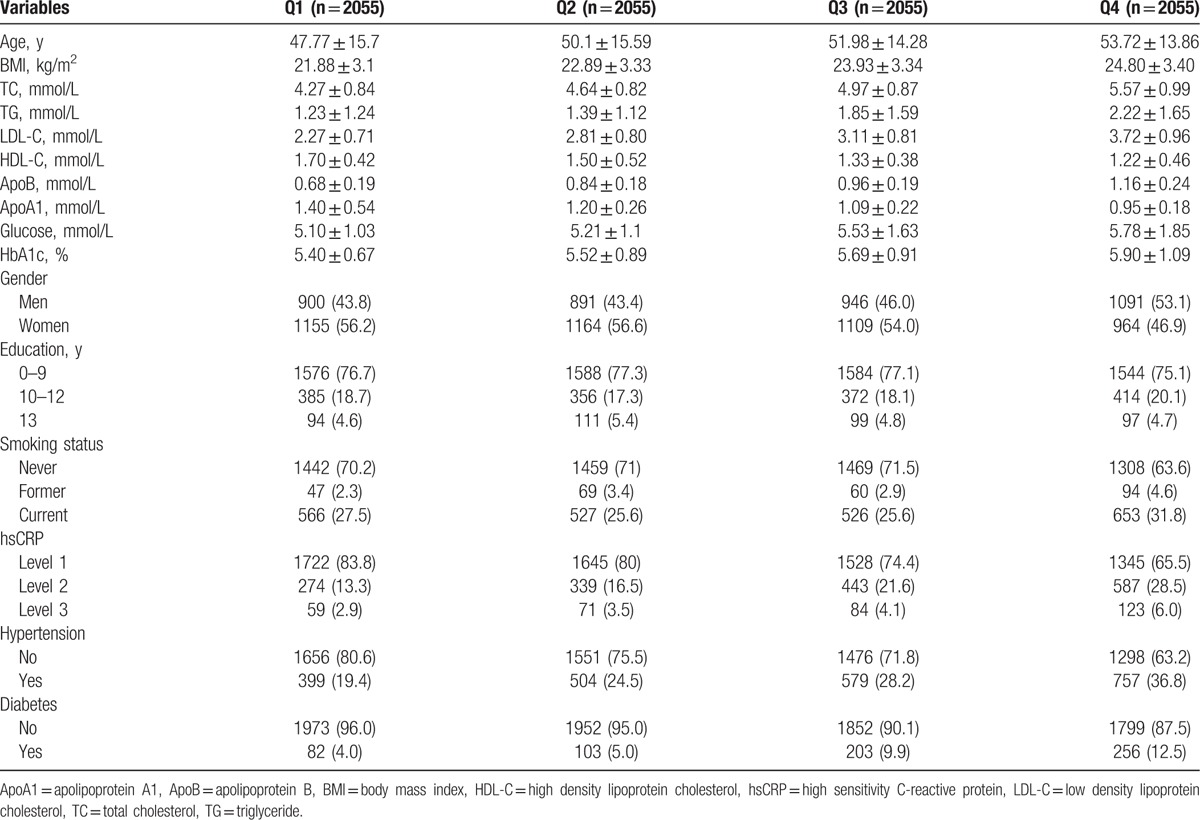
Table 1 shows the basic characteristics by quartiles of ApoB/ApoA1 ratio in 8220 participants (3828 men and 4392 women). The distribution of ApoB/ApoA1 ratio is approximately normal (Supplementary Fig. 1) and its correlation with other variables is shown in Supplementary Table 1. Both the fasting glucose (5.10 ± 1.03, 5.21 ± 1.10, 5.53 ± 1.63, and 5.78 ± 1.85 mmol/L) and the prevalence of type 2 diabetes (4.0%, 5.0%, 9.9%, and 12.5%) increase with increasing quartiles of ApoB/ApoA1 ratio (P < 0.01).
Table 1.
Basic characteristics of study participants.
3.2. Association between ApoB/ApoA1 ratio and type 2 diabetes
As shown in Table 2, compared with the first quartile, people in the fourth quartile of ApoB/ApoA1 ratio had a higher prevalence of type 2 diabetes (OR: 1.35, 95% CI: 1.10–1.81) after multivariable adjustment. One unit increase of ApoB/ApoA1 ratio was significantly associated with type 2 diabetes prevalence (OR: 1.48, 95% CI: 1.35–1.62) assuming the relationship was linear. When treating ApoB/ApoA1 ratio as a continuous variable using restricted cubic spline method, the relationship between ApoB/ApoA1 ratio and type 2 diabetes were not linear, as depicted in Fig. 1. The association with type 2 diabetes levels off when ApoB/ApoA1 ratio is less than 0.6 and increases almost linearly for ApoB/ApoA1 ratio > 0.6. We carried out additional analyses to examine the association between the non-HDL/HDL ratio and type 2 diabetes. A nonlinear relationship between non-HDL/HDL ratio and type 2 diabetes was obtained (Supplementary Table 2 and Fig. 2). The area under ROC curve was also calculated to compare the performance of ApoB/ApoA1 ratio with non-HDL/HDL ratio for type 2 diabetes, however, the result did not show any significant difference (0.77 vs 0.76, P = 0.58).
Table 2.
Association between ApoB/ApoA1 ratio and type 2 diabetes, OR (95% CI).
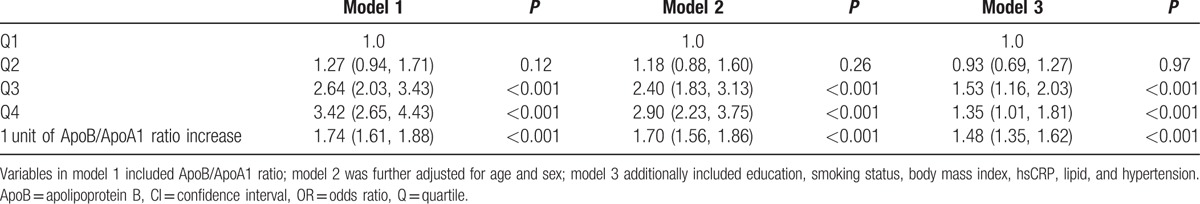
Figure 1.
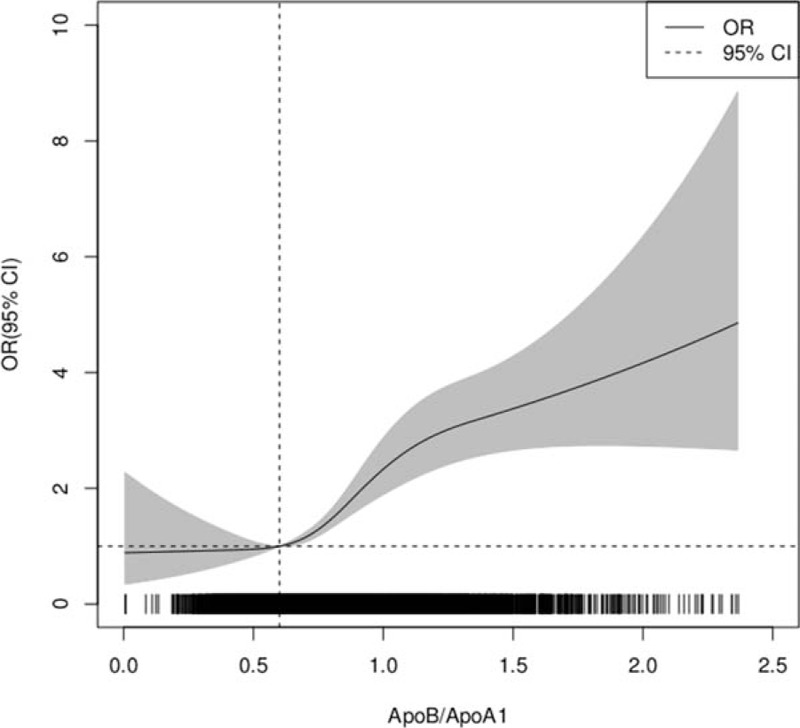
The association between ApoB/ApoA1 with type 2 diabetes. The solid line indicates the odds ratio with gray shaded area meaning 95% confidence interval. The bottom black bar shows the cluster of participants in the range of ApoB/ApoA1 ratio (most participants are in the range of 0.2–2.0 for ApoB/ApoA ratio).
4. Discussion
In the present study, we examined the association between ApoB/ApoA1 ratio and type 2 diabetes prevalence in a national large sample, and observed a significant association between ApoB/ApoA1 ratio and type 2 diabetes. Higher ApoB/ApoA1 ratio was associated with higher prevalence of type 2 diabetes. However, this association seems to be nonlinear, which is a new finding and was not evaluated in previous studies. These findings imply that ApoB/ApoA1 ratio posed a nonlinear dose relationship for type 2 diabetes prevalence.
Our finding that ApoB/ApoA1 ratio was significantly associated with type 2 diabetes was consistent with previous results.[11–14] One study in United States found the association between ApoB/ApoA1 ratio and insulin resistance might be nonlinear when categorizing ApoB/ApoA1 ratio to quartiles.[11] However, that study did not offer a complete picture of the association between ApoB/ApoA1 ratio and insulin resistance using restricted cubic spline method or similar smoothing approach, which gave us more statistical perspective to describe the potential relationship. Another study conducted in a Taiwanese population also found a significant association with diabetes when categorizing ApoB/ApoA1 ratio to 3 groups,[15] while this study did not thoroughly examine if this relationship was linear. Interestingly, a previous Korean study found the optimal cut-off values for ApoB/ApoA1 ratio might be around 0.65 in men and 0.62 in women to identify people with metabolic syndrome.[16] Our result showing a nonlinear turn point being around 0.6 is very similar to this report, except that our study aiming to identify diabetes that is a major component of metabolic syndrome.
In this study, we also compared the performance of ApoB/ApoA1 ratio with non-HDL/HDL ratio for predicting type 2 diabetes. We found there was no strong evidence to support that one ratio was superior to the other. However, the relationship of both 2 lipid ratios with diabetes was similar and the nonlinear association was observed for both. As noted previously, there are a number of problems caused by categorizing a continuous variable, such as lipid ratio for our study, in multiple regression modeling.[17] These include loss of power and loss of precision of estimated effect size. Most importantly, the choice of cutoff values may lack clinical meaning.[17,18] Our results suggest that ApoB/ApoA1 ratio should be modeled in a nonlinear fashion with diabetes in the future.
The strength of our population-based study is a large size and homogeneous population, which enabled us to draw a relatively confident conclusion. Despite of this, we still cannot examine the causal relationship between ApoB/ApoA1 ratio and type 2 diabetes due to the weakness of the cross-sectional study design. Additionally, although a number of potential confounders have been adjusted for, residual confounding by unmeasured variables may still bias the observed results. Future studies with more measured variables controlled for are needed to validate this finding. The study population is only comprised of Chinese population, extrapolating these findings to other racial or ethnic population should be interpreted with caution.
In conclusion, our study describes the nonlinear relationship between ApoB/ApoA1 ratio and type 2 diabetes prevalence in a large national population. Thus, the nonlinear relationship warrants further investigation and the cut-off value of 0.6 should be examined in another independent study.
Supplementary Material
Footnotes
Abbreviations: ApoA1 = apolipoprotein A1, ApoB = apolipoprotein B, BMI = body mass index, CHNS = China Health and Nutrition Survey, CI = confidence interval, HDL = high density lipoprotein, LDL = low density lipoprotein, OR = odds ratio, TC = total cholesterol, TG = triglyceride.
Funding: This research uses data from China Health and Nutrition Survey (CHNS). We thank the National Institute of Nutrition and Food Safety, China Center for Disease Control and Prevention, Carolina Population Center, the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, and R01-HD38700) and the Fogarty International Center, NIH for financial support for the CHNS data collection and analysis files from 1989 to 2006 and both parties plus the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009 and future surveys.
YM and YX contributed equally to this work.
Statement of human and animal rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of informed consent: Informed consent was obtained from all patients for being included in the study.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med 2010;362:1090–101. [DOI] [PubMed] [Google Scholar]
- [2].Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948–59. [DOI] [PubMed] [Google Scholar]
- [3].Zhan Y, Tang Z, Yu J. Serum ferritin, diabetes, diabetes control, and insulin resistance. Acta Diabetol 2014;51:991–8. [DOI] [PubMed] [Google Scholar]
- [4].Ardisson Korat AV, Willett WC, Hu FB. Diet, lifestyle, and genetic risk factors for type 2 diabetes: a review from the Nurses’ Health Study, Nurses’ Health Study 2, and Health Professionals’ Follow-up Study. Curr Nutr Rep 2014;3:345–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Janghorbani M, Amini M. Utility of serum lipid ratios for predicting incident type 2 diabetes: the Isfahan Diabetes Prevention Study. Diabetes Metab Res Rev 2016;32:572–80. [DOI] [PubMed] [Google Scholar]
- [6].Thompson A, Danesh J. Associations between apolipoprotein B, apolipoprotein AI, the apolipoprotein B/AI ratio and coronary heart disease: a literature-based meta-analysis of prospective studies. J Intern Med 2006;259:481–92. [DOI] [PubMed] [Google Scholar]
- [7].Hwang YC, Ahn HY, Park SW, et al. Apolipoprotein B and non-HDL cholesterol are more powerful predictors for incident type 2 diabetes than fasting glucose or glycated hemoglobin in subjects with normal glucose tolerance: a 3.3-year retrospective longitudinal study. Acta Diabetol 2014;51:941–6. [DOI] [PubMed] [Google Scholar]
- [8].TODAY Study Group Lipid and inflammatory cardiovascular risk worsens over 3 years in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 2013;36:1758–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jing F, Mao Y, Guo J, et al. The value of Apolipoprotein B/Apolipoprotein A1 ratio for metabolic syndrome diagnosis in a Chinese population: a cross-sectional study. Lipids Health Dis 2014;13:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Popkin BM, Du S, Zhai F, et al. Cohort profile: The China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol 2010;39:1435–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sierra-Johnson J, Romero-Corral A, Somers VK, et al. ApoB/apoA-I ratio: an independent predictor of insulin resistance in US non-diabetic subjects. Eur Heart J 2007;28:2637–43. [DOI] [PubMed] [Google Scholar]
- [12].Du T, Yuan G, Zhang M, et al. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol 2014;13:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hwang YC, Ahn Y, Kim WJ, et al. Increased apoB/A-I ratio independently associated with Type 2 diabetes mellitus: cross-sectional study in a Korean population. Diabet Med 2012;29:1165–70. [DOI] [PubMed] [Google Scholar]
- [14].Taskinen MR, Barter BJ, Ehnholm C, et al. Ability of traditional lipid ratios and apolipoprotein ratios to predict cardiovascular risk in people with type 2 diabetes. Diabetologia 2010;53:1846–55. [DOI] [PubMed] [Google Scholar]
- [15].Jian Z-H, Lung C-C, Ko P-C, et al. The association between the apolipoprotein A1/high density lipoprotein-cholesterol and diabetes in Taiwan—a cross-sectional study. BMC Endocr Disord 2013;13:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Jung CH, Hwang JY, Yu JH, et al. The value of apolipoprotein B/A1 ratio in the diagnosis of metabolic syndrome in a Korean population. Clin Endocrinol 2012;77:699–706. [DOI] [PubMed] [Google Scholar]
- [17].Frank E, Harrell J. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2015;New York:Springer International Publishing, 13–44. [Google Scholar]
- [18].Frank E., Harrell J. Problems Caused by Categorizing Continuous Variables. Available from: http://biostat.mc.vanderbilt.edu/wiki/Main/CatContinuous Accessed Nov 30, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


