Abstract
Background:
Multiple fractures of the atlas and axis are rare. The management of multiple fragment axis fractures and unstable atlas fractures is still challenging for the spinal surgeon. There are no published reports of similar fractures with 3-part fracture of axis associated with an unstable atlas fracture.
Case summary:
We present a patient with concurrent axis and atlas fractures, which have not been reported. The patient suffered hyperextension injury with neck pain and numbness of the bilateral upper extremity associated with weakness after a 2-m fall. The axis fractures included an odontoid type IIA fracture and traumatic spondylolisthesis of C2-C3. The atlas fracture was unstable. The neurological examination manifested as central canal syndrome, which was due to the hyperextension injury of cervical spine and spondylolisthesis of C2-C3. The patient was diagnosed as multiple unstable upper cervical fractures with spinal cord compromise. We performed posterior arthrodesis of C1-C3. Postoperatively, the patient showed neurological improvement, and C1-C3 had fused at the 3-month follow-up.
Conclusion:
Posterior arthrodesis of C1-C3 could provide a stable fixation for the 3 parts of axis (an odontoid type IIA fracture and traumatic spondylolisthesis of C2-C3) combined an unstable atlas fracture. Both the patient and the doctor were satisfied with the results of the treatment. So posterior arthrodesis of C1-C3 is a suitable treatment option for the treatment of a concurrent unstable atlas fracture and multiple fractures of the axis.
Keywords: multifragmentary axis fractures, posterior fusion, unstable atlas fractures
1. Introduction
Upper cervical spine injuries are relatively common and generally occur as a result of significant forces applied to the head during trauma. Isolated atlas or axis fractures account for more than 20% of all cervical spine fractures, while multiple fractures of the atlas and axis are rare, accounting for less than 1%.[1] Successful management of isolated atlas or axis fractures has been well documented.[2,3] However, the managements of multiple fragment axis fractures and unstable atlas fractures are still challenging for the spinal surgeon. There are no strong consensus therapeutic strategies on how to treat such fractures.
The treatment of upper cervical fractures depends mainly on the remaining segmental stability. Traditionally, conservative treatment with external immobilization has been used. However, surgeons increasingly hope to achieve high primary stability and early patient mobilization.[4] Consequently, surgical treatments have been suggested for unstable upper cervical fractures. The surgical treatment of the upper cervical includes reducing and stabilizing the injured spinal segment, preventing further neurological injury, and providing long-term stability.[5] The surgical managements of unstable upper cervical fractures depending on the types of fracture and the experiences of surgeons, including anterior odontoid screw fixation,[6] posterior C1-C2 pedicle screw fixation,[7] posterior atlantoaxial transarticular screw fixation,[8] and posterior occipitocervical fusion.[9]
Here, we present a patient with fracture of the axis into 3 parts (an odontoid type IIA fracture and traumatic spondylolisthesis of C2-C3) and an unstable atlas fracture. This patent was treated with posterior arthrodesis of C1 to C3, which offered stability and a good functional outcome. There was only limited case report about anterior and posterior approaches for the treatment of 3-part fracture of axis.[10] But there was no report about case with 3-part fracture of axis associated with an unstable atlas fracture. This is the first report describing the use of posterior screw fixation of C1-C3 for treating this type of fracture.
2. Case report
Informed consents of surgery and participate in our research were obtained from the patient. A 26-year-old woman arrived at the emergency department in an ambulance suffering from neck pain and bilateral upper extremity numbness and weakness after a 2-m fall. The neurological examination revealed weakness of the upper extremities and reduced sensation bilaterally in the C3 to C7 dermatomes. The sensory level was at bilateral shoulder and the patient felt hyperalgesia and numbness of bilateral upper extremity. The motor strength of the left biceps and triceps was grade 4/5 and that of the wrist flexors and extensors, left finger flexors, and intrinsic hand muscles was 1/5. The flexors and extension of the right triceps, biceps, and wrist were 4/5; the hand flexors and intrinsic muscles were 3/5. Sensation of both lower extremities was normal. The motor strength of both lower extremities was graded 5/5. The deep tendon reflexes of the upper and lower extremities were normal. Rectal tone and bulbocavernosus reflex were also normal. The patient was graded C according to the American Spinal Injury Association (ASIA). The initial diagnosis of the patient was head contusion with related soft tissue damage and a hyperextension injury of the neck. This patient had spinal cord injury and manifested as central canal syndrome. According to the neurological examination, the spinal cord injury level may be located upper than C4. The JOA score was 9 points. The only comorbidity of this patient was head and soft tissue contusions without intracranial hemorrhage. The patient had no history of cervical spondylosis, tumors or neurological disorders, long-term use of any medication, hypertension, heart disease, diabetes, mental illness, or family history of cervical spondylosis.
Cervical computed tomography (CT) and magnetic resonance imaging (MRI) showed a complex fracture of C2 and a burst fracture of C1, including the rare association of an odontoid type IIA fracture, traumatic spondylolisthesis of C2-C3 type IIA in the modified Levine–Effendi classification, rupture of the C2-C3 disc, and a C1 burst fracture with transverse atlantal ligament rupture (type IIA[11]) (Fig. 1A–H). The level of spinal cord injury level was mainly located at C2 to C4 level, which was consistent with physical examination. Surgical treatment was chosen because of the spinal instability caused by this traumatic lesion. The principle of our surgery was stabilizing the ring of C1, C1-C2, and C2-C3. Because the posterior fixation and infusion of C1 to C3 could achieve above surgical goal, we chose posterior fixation and infusion of C1 to C3.
Figure 1.
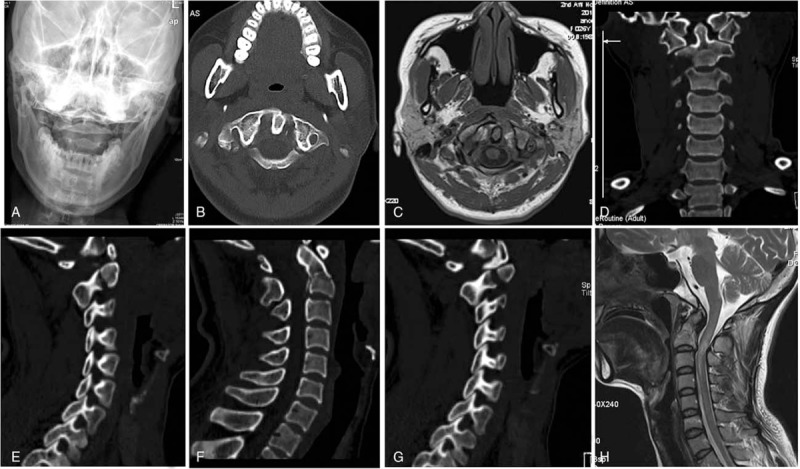
Open mouth view X-ray showed lateral displacement of C1 lateral mass which indicting C1 unstable fracture; CT showed multiple fragments of the axis (an unstable odontoid fracture type IIA, traumatic spondylolisthesis of C2-C3, and a C1 burst fracture); MRI showed type IIA transverse atlantal ligament rupture of C1 and an unstable C2-C3.
After inducing general endotracheal anesthesia, the patient was positioned prone in a Mayfield head holder. A midline skin incision (8–10 cm long) was made starting at the external occipital protuberance. The posterior arch and lateral mass of C1, C2, and C3 were subsequently exposed by subperiosteal dissection. The posterior arch was broken. C1 lateral mass screws were inserted following the report of Tan et al.[12] The walls of the lateral mass were carefully probed to confirm the correct trajectory. After tapping, a 3.5 mm × 24 mm C1 Vertex polyaxial screw (Medtronic Spine, Memphis, TN) was placed unicortically. The entry point to C2 was targeted in the vertebral arch-plant junction of the axis, and a 3.5 mm × 24 mm C2 Vertex polyaxial screw was implanted from this point through the pedicle of the axis. A 3.5 mm × 16 mm Vertex polyaxial screw was placed into the C3 lateral mass bicortically, using the Magerl technique.[13] An iliac crest graft was harvested and implanted posterior to C1-C3.
Drainage was used and a Philadelphia cervical collar was put on the patient at the end of the procedure and used for postoperative neck immobilization for 6 to 8 weeks. The postoperative CT showed sufficient reduction and good positioning of the implants (Fig. 2). Two days after surgery, we reassessed the neurological status of the patient by physical examination. There was no significant difference in neurological status between the patients before and after operation. So we did not aggravate the spinal cord injury during surgery. The patient started rehabilitation 5 days postoperatively.
Figure 2.
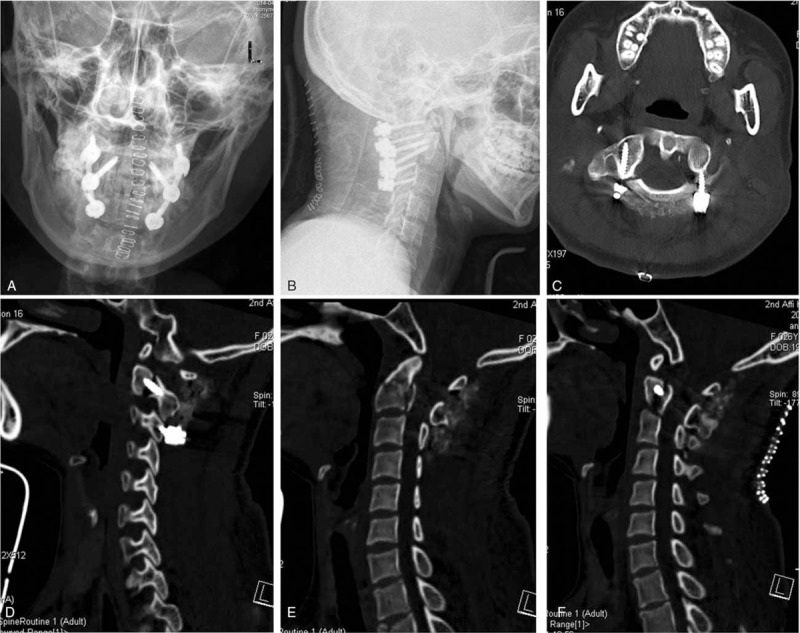
Postoperative X-ray and CT showing solid fixation of the unstable fractures.
The adherence of the patient was very well. The patient was evaluated 1 and 3 months postoperatively at outpatient department. Physical examination and image examination were taken during follow-up. At the 3-month follow-up, CT showed fracture healing and C1-C3 fusion (Fig. 3). The neurological examination revealed only numbness of both hands. The motor strength had recovered completely. The JOA score was 16 points. There were no adverse events.
Figure 3.
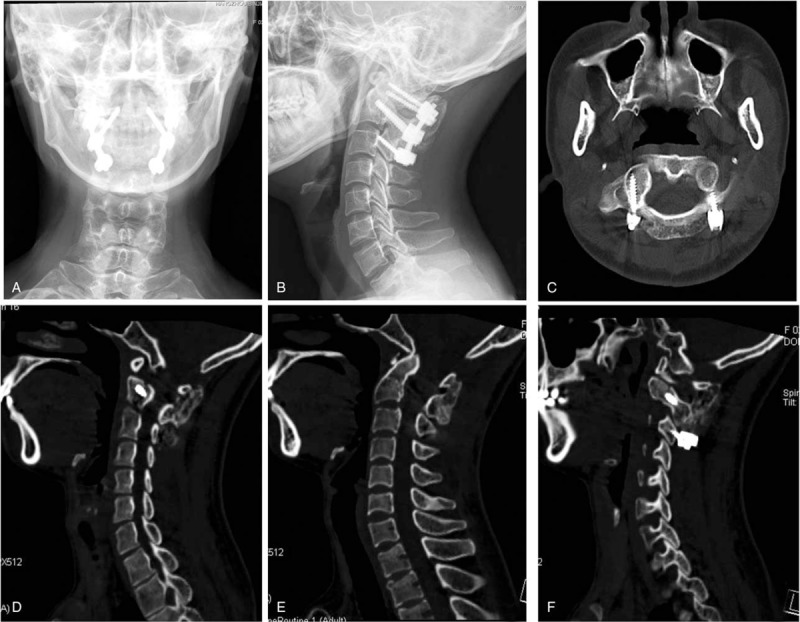
Three months postoperative CT showing fracture healing and C1-C3 fusion.
3. Discussion
In our case, the multiple upper cervical fractures consisted of 2 parts: multiple axis fractures and unstable atlas fracture. Several surgeons have reported the treatment of multiple fractures of the axis.[10,14] Koller et al[15] reported a patient with combined traumatic spondylolisthesis of C2-C3, fracture of the lateral mass of C2, and a type IIA odontoid fracture, who was managed with anterior odontoid screw fixation and C2-C3 arthrodesis. Shinbo et al[10] presented 2 patients with 3-part fractures of the axis consisting of a type II odontoid fracture and a type IA Levine–Edwards fracture. Both patients were treated with concurrent insertion of an anterior odontoid screw and bilateral posterior pedicle screws. The first patient had rupture of the C2-C3 disc and an unstable C2 fracture, and was treated with C2-C3 arthrodesis. The second case did not have rupture of the C2-C3 disc and was treated only with C2 fixation. Both patients had preserved ranges of motion of the cervical spine at C1-C2, and good osteosynthesis was acquired. In our case, the axis fracture was similar to previous 2 cases reports. However, the unstable atlas fracture complicated the case; we cannot simply fix the odontoid fracture through anterior approach or posterior stable C2-C3.
The atlas fracture of our case is an unstable fracture. An unstable atlas burst fracture is a fracture of the anterior and posterior atlantal arch with rupture of the transverse atlantal ligament. According to Dickman and Sonntag report,[11] the injuries of transverse atlantal ligament were classified into 2 types: disruptions of the substance of the ligament (type I) and fractures or avulsions involving the tubercle for insertion of the transverse ligament on the C1 lateral mass (type II). Most type I injuries chose nonsurgical treatment and the treatment result was satisfied; type II injuries should be treated with rigid fixation and usually were fixed with internal fixation by surgical treatments.[16] The rupture of transverse atlantal ligament in our case was type II. The management of unstable Jefferson fractures remains controversial. Conservative treatment usually involves a long period of immobilization in a halo vest; however, the bony fusion is often unsatisfactory. Surgical intervention usually includes fusion, eliminating motion of the upper cervical spine.[17,18] Li et al[19] treated unstable atlas fractures with direct posterior C1 lateral mass screws to achieve compression reduction and osteosynthesis. This method avoids traditional fusion and preserves the function of C0-C1-C2. However, our patient with atlas burst fractures have associated axis fractures, this method may be not suitable.
According to previous analysis, the situation of our case was more complex, the patient with fracture of the axis into 3 parts (an odontoid type IIA fracture and traumatic spondylolisthesis of C2-C3) and an unstable atlas fracture. We chose C1-C2 fusion for treating the unstable atlas fracture. However, the patient had an unstable C2-C3, due to a hangman fracture and rupture of the C2-C3 disc. Consequently, C2-C3 fusion was also needed. If we had chosen anterior C2-C3 fusion, posterior C1-C2 fusion would also have been required. Therefore, we ultimately decided to treat these complex upper cervical fractures by performing a single posterior C1-C3 fusion. Our patient had a favorable outcome, with sufficient stability of the fracture sites to allow early mobilization, and good osteosynthesis was achieved.
There are several strengths and limitations in our management. First, we achieved solid fixation for early mobilization through posterior approach. It avoids the potential risks and complication of anterior approach. Second, there was only 1 case in our report which may limit the significance of our treatment results. Third, we did not take flexion and extension views of cervical spine which was important for function assessment. And we only documented the function outcomes by physical examination. We may perform this in future case study.
In conclusion, posterior arthrodesis of C1-C3 could provide a stable fixation for the 3 parts of axis (an odontoid type IIA fracture and traumatic spondylolisthesis of C2-C3) combined an unstable atlas fracture. Both the patient and the doctor were satisfied with the results of the treatment. So posterior arthrodesis of C1-C3 is a suitable treatment option for the treatment of a concurrent unstable atlas fracture and multiple fractures of the axis.
Footnotes
Abbreviations: ASIA = American Spinal Injury Association, CT = computed tomography, MRI = magnetic resonance imaging.
Funding: This work was supported by the National Natural Science Foundation of China (no. 81271973, no. 81201397, and no. 81672147), the Zhejiang Provincial Natural Science Foundation of China (no. LY16H060003, no. LY15H060001, and no. LY15H060002), and Zhejiang medical and health science and technology plan project (no. 2015KYB182 and no. 2017KY382).
The authors have no conflicts of interest to disclose.
References
- [1].Korres DS, Papagelopoulos PJ, Mavrogenis AF, et al. Multiple fractures of the axis. Orthopedics 2004;27:1096–9. [DOI] [PubMed] [Google Scholar]
- [2].Kumar Singh P, Garg K, Sawarkar D, et al. CT-guided C2 pedicle screw placement for treatment of unstable Hangman's fractures. Spine (Phila Pa 1976) 2014;39:1058–65. [DOI] [PubMed] [Google Scholar]
- [3].Ma W, Xu N, Hu Y, et al. Unstable atlas fracture treatment by anterior plate C1-ring osteosynthesis using a transoral approach. Eur Spine J 2013;22:2232–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Syre P, Petrov D, Malhotra NR. Management of upper cervical spine injuries: a review. J Neurosurg Sci 2013;57:219–40. [PubMed] [Google Scholar]
- [5].Jackson RS, Banit DM, Rhyne AL, III, et al. Upper cervical spine injuries. J Am Acad Orthop Surg 2002;10:271–80. [DOI] [PubMed] [Google Scholar]
- [6].Marwan Y, Kombar OR, Al-Saeed O, et al. The feasibility of two screws anterior fixation for Type II odontoid fracture among Arabs. Spine (Phila Pa 1976) 2016;41:E643–6. [DOI] [PubMed] [Google Scholar]
- [7].Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the C1-C2 complex for pedicle screw fixation. Spine (Phila Pa 1976) 2002;27:1494–8. [DOI] [PubMed] [Google Scholar]
- [8].Melcher RP, Puttlitz CM, Kleinstueck FS, et al. Biomechanical testing of posterior atlantoaxial fixation techniques. Spine (Phila Pa 1976) 2002;27:2435–40. [DOI] [PubMed] [Google Scholar]
- [9].Lee SC, Chen JF, Lee ST. Clinical experience with rigid occipitocervical fusion in the management of traumatic upper cervical spinal instability. J Clin Neurosci 2006;13:193–8. [DOI] [PubMed] [Google Scholar]
- [10].Shinbo J, Sameda H, Ikenoue S, et al. Simultaneous anterior and posterior screw fixations confined to the axis for stabilization of a 3-part fracture of the axis (odontoid, dens, and hangman fractures): report of 2 cases. J Neurosurg Spine 2014;20:265–9. [DOI] [PubMed] [Google Scholar]
- [11].Dickman CA, Sonntag VK. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery 1997;40:886–7. [DOI] [PubMed] [Google Scholar]
- [12].Tan M, Wang H, Wang Y, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976) 2003;28:888–95. [DOI] [PubMed] [Google Scholar]
- [13].Jeanneret B, Magerl F, Ward EH, et al. Posterior stabilization of the cervical spine with hook plates. Spine (Phila Pa 1976) 1991;16:S56–63. [DOI] [PubMed] [Google Scholar]
- [14].Blondel B, Metellus P, Fuentes S, et al. Single anterior procedure for stabilization of a three-part fracture of the axis (odontoid dens and hangman fracture): case report. Spine (Phila Pa 1976) 2009;34:E255–7. [DOI] [PubMed] [Google Scholar]
- [15].Koller H, Assuncao A, Kammermeier V, et al. Simultaneous anterior arthrodesis C2-C3 and anterior odontoid screw fixation for stabilization of a 4-part fracture of the axis—a technical description. J Spinal Disord Tech 2006;19:362–7. [DOI] [PubMed] [Google Scholar]
- [16].Koller H, Resch H, Tauber M, et al. A biomechanical rationale for C1-ring osteosynthesis as treatment for displaced Jefferson burst fractures with incompetency of the transverse atlantal ligament. Eur Spine J 2010;19:1288–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Tan J, Li L, Sun G, et al. C1 lateral mass-C2 pedicle screws and crosslink compression fixation for unstable atlas fracture. Spine (Phila Pa 1976) 2009;34:2505–9. [DOI] [PubMed] [Google Scholar]
- [18].Hein C, Richter HP, Rath SA. Atlantoaxial screw fixation for the treatment of isolated and combined unstable jefferson fractures—experiences with 8 patients. Acta Neurochir (Wien) 2002;144:1187–92. [DOI] [PubMed] [Google Scholar]
- [19].Li L, Teng H, Pan J, et al. Direct posterior c1 lateral mass screws compression reduction and osteosynthesis in the treatment of unstable jefferson fractures. Spine (Phila Pa 1976) 2011;36:E1046–51. [DOI] [PubMed] [Google Scholar]


