Abstract
The widespread use of MRI in the assessment of low back pain has led to increased detection of degenerative cysts of the spine, which was essentially a surgical diagnosis earlier. The awareness of degenerative cysts, the significance of their role in the etiology of radicular and back pain and their effective management is evolving. We describe a case of bilateral, gas-filled lumbar facet synovial/ ganglion cysts causing focal arachnoid inflammation and lateral lumbar canal stenosis.
Keywords: degenerative cysts, synovial cysts, vacuum cysts, intraspinal gas
Introduction
Degenerative cysts of the spine include herniated disc cysts, facet joint cysts, ligamentum flavum cysts and cysts of the posterior longitudinal ligament1,2,3. Generally, these degenerative cysts are fluid-filled, so it is vital to differentiate them from more ominous conditions like neoplasms and infections1. Cysts associated with degenerative facet joints are categorised as either synovial cysts or ganglion cysts. Synovial cysts, as the name indicates, are lined by synovium, whereas ganglion cysts are lined by non-synovial tissue. It is generally not possible to make a distinction between the two by imaging, unless the cyst is far removed from the facet joint, which would then make it more likely to be a ganglion cyst1,2-4.
Vacuum phenomenon and gas collections are well-documented radiological findings in the spine. They commonly occur in discs, Schmorl's nodes and facet joints. They are also known to occur in the spinal canal (extra- or intra-dural) and in vertebral bodies (intravertebral cleft phenomenon). Rarely, they can be seen in synovial cysts and ganglion cysts2,5,6. Fick was the first to describe the vacuum phenomenon in 1910 while he was studying joints under traction7. In 1937, Magnusson reported the same phenomenon in intervertebral discs and postulated that the creation of spaces, subsequently filled by gas, required a reduction of barometric pressure within the joint8. In 1942, Knuttson correlated vacuum phenomenon with disc degeneration9. Ford, in 1977, analysed intradis-cal gas which was later confirmed by Yoshida et al. in 1997 to comprise predominantly of nitrogen (90-92%) combined with oxygen, carbon dioxide, and traces of other gases10,11.
Case Report
A 51-year-old woman with increasing low back pain, bilateral radicular pain and neurogenic claudication which had progressively worsened over the previous three months was referred to MRI of the lumbosacral (LS) spine. The patient's radicular pain extended into the posterior aspect of the thigh and leg, exacerbated by walking and attenuated by lying down. There was also numbness over the dorsum of the feet and big toe. Her clinical history was otherwise unremarkable. Clinical examination revealed limited straight leg raising test on 40?, bilaterally. There was some weakness of feet dorsiflexion and the extensor hollicus longus muscles, with diminished knee reflexes and hypoesthesia was detected over the right L4 and L5 dermatomes.
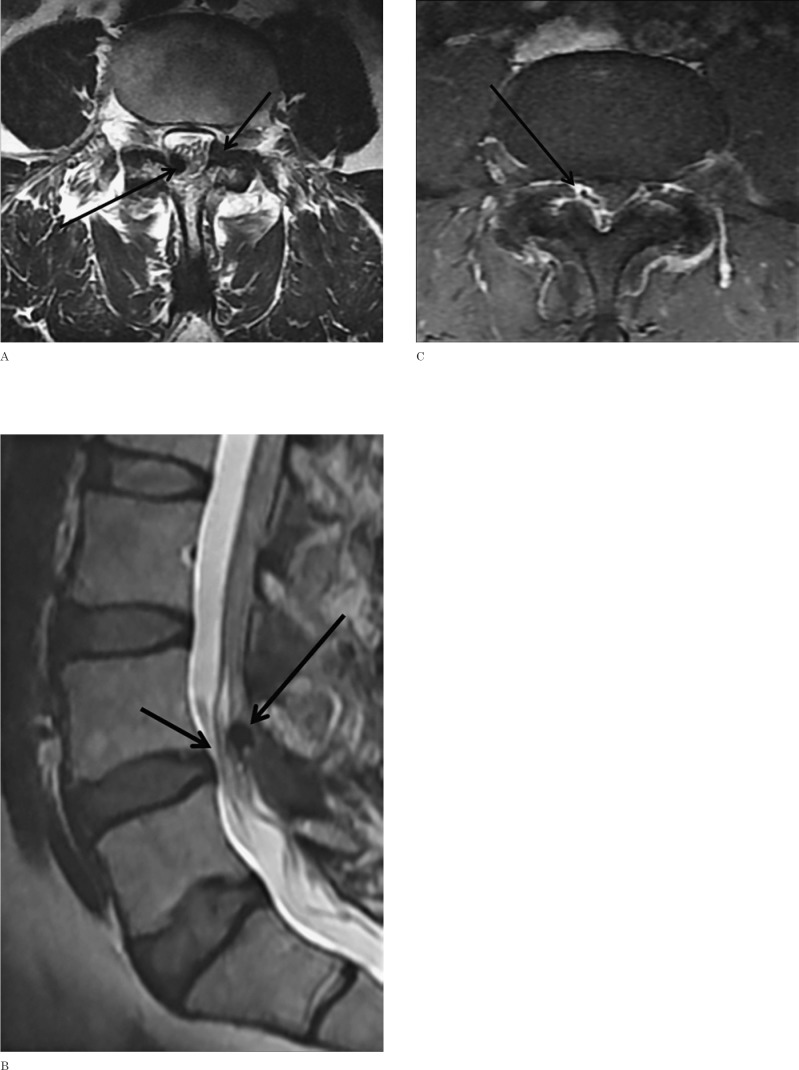
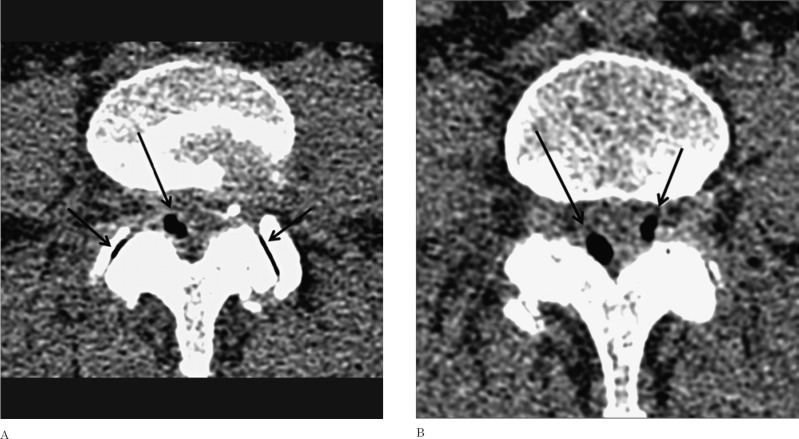
MRI of the LS spine showed a small, well defined, oval-shaped T1 and T2 signal void lesion in the right lateral epidural space at L4/5 level (Figure 1A) in close association with the adjacent facet joint and ligamentum flavum, it was compressing and displacing the thecal sac and causing clumping of the cauda equina (Figure 1B). There was marginal enhancement of the cyst wall and adjacent thecal sac (Figure 1C). Additionally, bilateral facet joint arthropathy at the same level with no significant disc bulge was also noted. To further characterize the intraspinal signal void, limited CT scan of the lumbar spine at L4-L5 level (Figures 2A, B) was done immediately after completing the MRI scan. It showed bilateral epidural gas-filled cysts. The larger one was in the right lateral space corresponding to the signal void noted in the MRI images. The other lesion in the left lateral epidural space was retrospectively located in the MRI scan (Figure 2A). Adjacent bilateral L4-L5 facet joints showed degenerative changes including intra-articular gas (vacuum) (Figure 2A).
Figure 1.
A) Axial T2-weighted MRI of the lumbosacral (LS) spine at L4-L5 level demonstrates a hypointense lesion in right lateral epidural space (long arrow) causing mass effect on the thecal sac and a smaller cyst (short arrow) in left epidural space. B) Sagittal T2-weighted image of the LS spine demonstrates crowding of the cauda equina spinal nerve roots (short arrow) by the epidural lesion. C) Axial post-contrast fat-saturated T1-weighted MRI showing enhancement of the wall of the right epidural gas cyst and adjacent thickened thecal sac (arrows).
Figure 2.
A, B) Axial CT scan at L4-L5 level (soft tissue window), showing a larger right epidural vacuum (gas) cyst (long arrows in A, B), a smaller left epidural vacuum (gas) cyst (short arrow in B) and bilateral facet joint arthropathy with joint vacuum phenomenon (short arrows in A).
Discussion
Degenerative cysts of the spine can be incidental or symptomatic, mimicking herniated discs or canal stenosis. These cystic lesions are being encountered more frequently as MRI has become the imaging modality of choice in evaluating low back pain. A vast majority of these lesions are epidural, but they can also be intradural, present within the neural foramen or located peri-spinally. These cysts contain serous or protein-rich fluid and are sometimes complicated by intracystic haemorrhage1.
The nomenclature of these cysts is variable and has not yet been standardized. The two commonly used systems to classify degenerative cysts are based on their pathology or the structures from which they originate. Based on the structure of origin, they are named disc herniation cysts, facet joint cysts, ligamen-tum flavum cysts and posterior longitudinal ligament cysts. Pathologically, these cysts are either synovial cysts or ganglion cysts. Alternatively, they can also be classified based on their location within the spinal canal as ventrolateral, lateral and posteromedian1,4,5.
Synovial cysts extend from adjacent apophyseal joints into the epidural space or neural foramen. Ganglion cysts develop in situ secondary to mucoid degeneration of the mesenchymal connective tissue or haemorrhage in the posterior longitudinal ligament or ligamen-tum flava. Disc cysts are often located in the ventrolateral space, and are believed to arise secondary to fluid production within a softened degenerated disc which leaks out and in time develops a pseudomembrane. Alternatively, the herniated disc can irritate the adjacent internal epidural venous plexus, causing it to rupture; the resulting haematoma evolves into a cyst. Posterior longitudinal ligament ganglion cyst, which is more common in young men, is also located in the ventrolateral space1,3.
Facet joint synovial cysts are by far the commonest degenerative cysts of the spine. Most of these are located in the lumbar spine at L4-L5 and L5-S1 levels adjacent to and communicating with the apophyseal joints. There is a definite predilection for females over the age of 50 years. They are believed to arise secondary to trauma or osteoarthrosis of the facet joints, more commonly in patients with hypermobile facet joints. Generally, cyst contents follow the signal intensity of CSF, but may contain protein-rich contents or haemorrhage. The cyst sac may have a hypointense rim due to calcification, fibrosis or haemosiderin deposition. Because these cysts communicate with the facet joints, the facet joint gas secondary to the vacuum phenomenon can potentially extend into these cysts, detected as signal void on all sequences as demonstrated in our case1,6.
It may not always be possible to differentiate a ganglion cyst from a synovial cyst by MRI. If communication with a facet joint is established, synovial facet joint cyst can be diagnosed. Cysts distant from the joints are more likely to be ganglion cysts. Cysts in the ventrolateral epidural space can be either a herniated disc cyst or posterior longitudinal ligament cyst. The lateral cysts can be synovial facet joint cysts or ligamentum flavum cysts. Cysts in the posterior median epidural space can arise secondary to intraspinal extension of interspinous bursae which occurs in Baastrup's disease8,9.
The term vacuum phenomenon used in radiological reporting describes any gas-like density in joints and spine. A real vacuum phenomenon is a dynamic process created by rapid expansion of a joint space resulting in negative pressure, whereas true gas collection occurs in degenerating discs and joints following sustained vacuum phenomenon. It has been hypothesized that the transition from true vacuum to gas and/or fluid and back to vacuum in joints and discs is a complex cyclical dynamic process, although experimental evidence is lacking. The vacuum phenomenon is triggered by distraction of the joint which occurs in the spine during extension and in the supine position. The gas is from dissolved nitrogen in tissues which escapes in a gaseous state when sufficient negative pressure is generated2,4. Gas collection depends on the permeability of surrounding tissues, vascularity, mobility and the attitude of the joints involved4,5.
Intraspinal gas collections are rare. In our patient, the facet joint synovial cysts were in a state of either being entirely gas-filled or collapsed with no fluid or gas content. The cyst in the right lateral epidural space showed rim and adjacent thecal sac enhancement, with aggregated nerve roots in the cauda equina. These findings may denote associated oedema and inflammatory changes with possible adherence of the cyst to the thecal sac, which has likely worsened our patient's symptoms. Kumar et al.2 reported a gas and fluid-containing herniated disc, which was found to be adherent to the nerve root and thecal sac intraoperatively. Demonstration of gas by CT was helpful in confirming the cause of the intraspinal epidural low signal on MRI as well as excluding calcified pseudoneoplasm of the neural axis (CAPNON)10.
Management of intraspinal epidural gas cyst ranges from conservative to minimally invasive to surgical resection. Different authors have published cases where surgical needle puncture of intraspinal lumbar cysts relieved radicular symptoms11. This highlights the importance of surgical management in symptomatic cysts. However, it has also been suggested they can spontaneously regress1,4. Our patient was reluctant to opt for the surgical management, she had temporary symptomatic relief by medical treatment and her subsequent course is unknown at present. It would have been ideal to reimage the patient after her symptoms subsided to further assess the dynamics of gas translocation (within the facet joints and adjacent synovial cysts), as well as the possible regression of adjacent dural enhancement. However, the patient was lost to follow-up.
In conclusion, the presence of intraspinal, extradural signal void associated with an adjacent degenerative facet joint in MRI suggests a vacuum synovial or ganglion cyst. CT imaging is recommended to differentiate calcification from air. The dynamic nature of these vacuum cysts, reflected by their change in size (as demonstrated in our patient in her CT images acquired immediately after MRI) can explain the intermittent exacerbation and relief of radicular symptoms related to posture. We suggest adjacent nerve root crowding and dural enhancement are indicators of associated oedema or acute inflammation which may indicate aspiration or surgical intervention for symptomatic relief rather than conservative management.
References
- 1.Khalatbaria K Ansari H. MRI of degenerative cysts of the lumbar spine. Clin Radiol. 2008; 63: 322–328. [DOI] [PubMed] [Google Scholar]
- 2.Kumar R West CG Gillespie JE. Gas in a spinal extradural cyst. Case report. J Neurosurg. 1989; 70 (3): 486–488. [DOI] [PubMed] [Google Scholar]
- 3.Fandino J Garcia J Garcia-Abeledo M. Radicular compression by gas ina spinal extradural cyst. Neurochirurgie. 1994; 40: 179–182. [PubMed] [Google Scholar]
- 4.Schulz EE West WL Hinshaw DB et al. Gas in a lumbar extradural juxtaarticular cyst: sign of synovial origin. Am J Roentgenol. 1984; 143 (4): 875–876. [DOI] [PubMed] [Google Scholar]
- 5.Coulier B. The spectrum of vacuum phenomenon and gas in spine. JBR-BTR. 2004; 87: 9–16. [PubMed] [Google Scholar]
- 6.Kawaguchi S Yamashita T Ida K et al. Gas-filled intradural cyst of the lumbar spine. Case report. J Neurosurg. 2001; 95 (Suppl. 2): 257–259. [DOI] [PubMed] [Google Scholar]
- 7.Yoshida H Shinomiya K Nakai O et al. Lumbar nerve root compression caused by lumbar intraspinal gas: report of three cases. Spine. 1997; 22: 348–351. [DOI] [PubMed] [Google Scholar]
- 8.Lin RM Wey KL Tzeng CC. Gas-containing “ganglion” cyst of lumbar posterior longitudinal ligament at L3. Case report. Spine. 1993; 18: 2528–2532. [DOI] [PubMed] [Google Scholar]
- 9.Gracia-Mata S Gozzi-Vallejo S Izco-Cabezón T et al. Intradural disc herniation and epidural gas: something more than a casual association? Spine. 2004; 29 (20): E463–467. [DOI] [PubMed] [Google Scholar]
- 10.Park P Schmidt LA Shah GV et al. Calcifying pseudoneoplasm of the spine. Clin Neurol Neurosurg. 2008; 110: 392–395. [DOI] [PubMed] [Google Scholar]
- 11.Impiombato FA Lunghi V Gambacorta D et al. Treatment of a symptomatic epidural gas cyst using an angiographic 5F Catheter in the epidural space of the spinal cord through the sacral hiatus. A Case Report. NRJ Digital. 2011; 24: 1105–1109. [DOI] [PubMed] [Google Scholar]
- 12.Fick R. Handbuch der Anatomie und Mechanik der Gelenke unter Verucksichtigung der bewegenden Muskeln. Vol. 2 Fischer JG, ed; 1910. [Google Scholar]
- 13.Magnusson W. Über die bedingungen des hervortretens der wirklichen genlenkspalte auf dem roe bedingunge. Acta Radiol. 1937; 18: 733–741. [Google Scholar]
- 14.Knutsson F. The vacuum phenomenon in the intervertebral discs. Acta Radiol. 1942; 23:173–179. [Google Scholar]
- 15.Ford LT Gilula LA Murphy WA et al. Analysis of gas in vacuum lumbar disc. Am J Roentgenol. 1977; 128: 1056–1057. [DOI] [PubMed] [Google Scholar]