Abstract
Protective antigen (PA) is central to the action of the lethal and edema toxins produced by Bacillus anthracis. It is the common cell-binding component, mediating the translocation of the enzymatic moieties (lethal factor [LF] and edema factor) into the cytoplasm of the host cell. Monoclonal antibodies (MAbs) against PA, able to neutralize the activities of the toxins in vitro and in vivo, were screened. Two such MAbs, named 7.5 and 48.3, were purified and further characterized. MAb 7.5 binds to domain 4 of PA and prevents the binding of PA to its cell receptor. MAb 48.3 binds to domain 2 and blocks the cleavage of PA into PA63, a step necessary for the subsequent interaction with the enzymatic moieties. The epitope recognized by this antibody is in a region involved in the oligomerization of PA63; thus, MAb 48.3 does not recognize the oligomer form. MAbs 7.5 and 48.3 neutralize the activities of anthrax toxins produced by B. anthracis in mice. Also, there is an additive effect between the two MAbs against PA and a MAb against LF, in protecting mice against a lethal challenge by the Sterne strain. This work contributes to the functional analysis of PA and offers immunotherapeutic perspectives for the treatment of anthrax disease.
Bacillus anthracis, a spore-forming bacterium, is the causative agent of anthrax. Virulent strains are encapsulated and secrete two toxins composed of three proteins: the protective antigen 83 (PA83; 83 kDa), the lethal factor (LF; 85 kDa), and the edema factor (EF; 89 kDa) (18). Intravenous injection of the lethal toxin (Letx; PA83 plus LF) into animals causes sudden death (2). The Fisher 344 rat is commonly used to test the activity of Letx in vivo. In macrophage cell lines, such as RAW264.7, the lethal toxin induces lysis (10). The edema toxin (PA83 plus EF) causes edema at the inoculation site (34). The three-dimensional structure of PA83 has been solved (29) and consists of four folding domains. PA83 binds via domain 4 to an ubiquitous proteinaceous cell receptor which has been identified as the anthrax toxin receptor) (3, 4, 33, 35). PA83 is then cleaved at a site in domain 1 by furin-like proteases into PA63 and PA20 (a 20-kDa amino-terminal fragment) (14). This processing leads to the heptamerization of PA63 (24) and the subsequent binding of EF or LF. The heptamerization involves domains 1, 2, and 3 (26, 29). The clustering of anthrax toxin receptor into lipid rafts via PA63 heptamerization is necessary and sufficient to trigger efficient internalization of the toxic complexes into the cytoplasm, where EF and LF exert their catalytic effects (1). EF is a calmodulin-dependent adenylate cyclase (17). LF is a zinc metalloprotease, which cleaves mitogen-activated protein kinase kinases (8, 13, 28, 36). PA83 is therefore a key protein, promoting both the binding of the toxins to the cell surface and the translocation of their enzymatic moieties into the cytoplasm of the host cell (25, 30). Previous work with strains of B. anthracis harboring mutant PA83, LF, and EF proteins has determined the role of the functional domains of the toxin components, produced by the bacteria within the host (4, 5). Monoclonal antibodies (MAbs) against PA83 have been used to analyze the structure-function relationships of the protein (20, 22). Some of these MAbs or other antibodies, including single-chain variable fragments or single-chain variable fragments fused to a human constant κ domain that binds to PA83 (23), prevent the Letx-induced lysis of macrophages and protect Fisher 344 rats from death after intravenous injection of Letx. They do so either by blocking the interaction of PA83 with its cell receptor or by preventing the binding of LF to PA63 (20, 22). Here, we describe MAbs that we raised against PA83 and LF and screened for their ability to neutralize the activities of the toxins. Characterization of the epitopes of PA83 recognized by the MAbs improves our knowledge of the protein. Passive administration of polyclonal antisera against PA83 prevents spore infection in guinea pigs (15, 19): we show that the neutralizing activities of MAbs against PA83 and LF protect mice against a lethal spore challenge with the toxinogenic Sterne strain.
MATERIALS AND METHODS
Hybridoma production.
BP2 mice were immunized subcutaneously (s.c.) with 20 μg of PA83 or LF in 100 μl of NaCl (150 mM) emulsified with 100 μl of complete Freund's adjuvant. Four s.c. booster injections in incomplete Freund's adjuvant were given 1, 3, 5, and 7 weeks later. Fifteen days later, mice received the last intraperitoneal booster of antigen (10 μg). Splenocytes were collected 3 days later and immortalized by fusion with mouse myeloma cells (x63Ag8-653) (16). Cells were grown on 24-well plates, and the culture medium was screened by enzyme-linked immunosorbent assay (ELISA) for PA antibodies. Hybridomas from positive wells were cloned by limiting dilution and plated on microtiter plates. Positive clones identified by ELISA were expanded and used to inject mice for ascites production. Antibodies were purified by precipitation with ammonium sulfate.
ELISA.
We used a modified version of a standard ELISA to test for the presence of antibodies in culture supernatants (7). Microtiter plates (Nunc, Roskilde, Denmark) were incubated overnight at 4°C with 1 μg of antigen/ml of phosphate-buffered saline (PBS). Plates were washed four times with buffer A (0.1% Tween 20 in PBS), and supernatants were diluted in buffer B (0.5% gelatin in buffer A). The plates were incubated for 2 h at 37°C and washed again, and horseradish peroxidase-labeled rabbit anti-mouse antibodies (Bio-Rad Pasteur, Marnes-la-Coquette, France) were added for 1 h at 37°C. Then, the plates were washed with buffer A, and freshly prepared 0.2% orthophenylenediamine (Dakopatts A/S, Glostrup, Denmark) and 0.03% H2O2 in 0.1 M citrate buffer (pH 5.2) were added to each well. The peroxidase reaction was stopped by adding 3 M HCl, and the optical density was measured at 490 nm. The dissociation constants were determined as previously described by Friguet et al. (11).
Phage display techniques.
The PhD-7 phage display kit (New England Biolabs, Beverly, Mass.) was used for the biopanning experiments essentially as recommended by the manufacturer. Briefly, MAb 48.3 at a concentration of 100 μg/ml in carbonate buffer (0.1 M NaHCO3 [pH 8.6]) was immobilized in 96-well plates with gentle agitation for 15 h at 4°C. The coating solution was removed, and each well was filled with blocking buffer (0.1 M NaHCO3 [pH 8.6], 5 mg of bovine serum albumin/ml, 0.02% NaN3) for 1 h at 4°C. Then, the blocking solution was discarded, and the wells were washed six times with Tris-buffered saline (TBS) (50 mM Tris-HCl [pH 7.5], 150 mM NaCl) containing 0.1% vol/vol Tween 20. We added 4 × 1010 phages from the original library in TBS-0.1% Tween 20 and left them to absorb for 30 min at room temperature. Unbound phage was removed by washing with TBS containing 0.1% Tween 20. The bound phages were eluted by the addition of 0.2 M glycine-HCl (pH 2.2) and 1 mg of bovine serum albumin/ml for 10 min with subsequent neutralization with a 1:10 volume of 1 M Tris-HCl (pH 9.1). An aliquot of the eluted phage was kept for titration, and the remainder was added to exponentially growing Escherichia coli ER2537 cells and amplified by incubation for 4 h at 37°C. To precipitate the phages, a one-sixth volume of PEG 8000-NaCl (20% [wt/vol] polyethylene glycol 8000, 2.5 M NaCl) was added to the cultures. Phages were finally resuspended in 100 μl of TBS, and titers were obtained by standard microbiological techniques. This biopanning procedure was repeated twice, using 2 × 1011 of the amplified phage as an input for each biopanning experiment. The binding stringency was increased in three successive steps by increasing the concentration of Tween 20 used from 0.1 to 0.3% and finally to 0.5%.
Characterization of phage inserts.
A total of 30 phages from a single lysis plaque were amplified as described above and resuspended in 200 μl of iodide buffer (10 mM Tris-HCl [pH 8.0], 1 mM EDTA, 4 M NaI). DNA was precipitated by the addition of 500 μl of ethanol and centrifugation for 30 min at 12,000 × g at room temperature. After being washed in 70% ethanol, the DNA was resuspended in 30 μl of TE (10 mM Tris-HCl [pH 8.0], 1 mM EDTA). Five microliters of the resuspended template was used for automatic sequencing with primer PhD-28 (5′-GTA TGG GAT TTT GCT AAA CAA C-3′) or PhD-96 (5′-CCC TCA TAG TTA GCG TAA CG-3′) and a T7 sequencing kit (Amersham Pharmacia Biotech, Saclay, France). The sequences were aligned with ClustalW software (EMBL, Heidelberg, Germany) to find a consensus.
Cytotoxic assay of macrophages.
Supernatants from hybridomas producing antibodies against PA83 or purified MAbs 7.5 and 48.3 (10 to 0.01 μg/ml) were preincubated with PA83 (500 ng/ml, corresponding to 10 times the 50% effective concentration) for 1 h at 37°C. The complexes were incubated in the presence of LF (1 μg/ml) with RAW264.7 macrophages for 4 h. The viability of the macrophages was assessed by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay (12).
Characterization of MAbs in vitro.
Purified PA83 was cleaved by chymotrypsin (1:1; Sigma) for 30 min at 30°C. Digested fragments were resolved on a sodium dodecyl sulfate-10% polyacrylamide gel electrophoresis gel for Western blotting with purified MAb 7.5 or 48.3 (1:5,000) as first antibodies (32). For dot blot experiments, PA83 mutant proteins (1,000 ng), PA83 (from 8 to 1,000 ng), or heptamers of PA63 (from 8 to 1,000 ng) obtained by trypsin cleavage as previously described (4) were adsorbed on a nitrocellulose membrane. MAbs 7.5 or 48.3 (1:1,000) were used as first antibodies.
Cellular experiments.
PA83 was labeled with 125I-Na with Iodo-Beads (Pierce, Rockford, Ill.). Radiolabeled PA83 (1 μg/ml) was preincubated with various dilutions of the antibodies (from 0.01 to 10 μg/ml) for 1 h at 37°C. The complexes were then incubated with the cells at 4°C to prevent endocytosis for 1 h. Cells were washed four times with PBS (pH 7.2). Cell associated proteins were solubilized with β,-d-glucopyranoside (200 μg/ml) (Sigma, Saint Louis, Mo.), and samples were loaded into a 10% polyacrylamide gel. The presence of PA83 in these samples from the cell surface was revealed by autoradiography.
In vivo characterization of MAbs.
Adoptive transfers were performed with outbred OF1 mice (IffaCredo, Labresles, France). Groups of four mice each were injected intravenously with one or more of the following: MAbs 48.3, 7.5, and 50.8 (1, 10, or 100 μg/mouse). Animals were challenged s.c. with 10 times the 50% lethal dose of the toxinogenic, nonencapsulated Sterne strain 16 h after the adoptive transfer, and survival was followed for 10 days.
RESULTS AND DISCUSSION
In vitro characterization of MAbs.
Supernatants from hybridomas producing antibodies against PA83 were screened for their capacity to neutralize the activity of Letx in a cytotoxic assay on macrophages RAW264.7. Of the 96 supernatants tested, 9 had this property. All nine were cloned, and two MAbs, named 7.5 and 48.3, were purified and studied because of their higher affinities. MAbs 7.5 and 48.3 had the same isotype [immunoglobulin G1(κ)] and their affinities for PA83 were similar (Kd = 1.6 × 10−10 M). A cytotoxicity assay of macrophages was performed with the purified antibodies. The minimal concentration of MAbs 48.3 and 7.5 required to neutralize 100% of Letx activity on macrophages was 1 and 10 μg/ml, respectively (Fig. 1).
FIG. 1.

Lethal toxin-neutralizing activity of anti-PA MAbs 7.5 and 48.3 on RAW264.7 macrophages. MAbs 7.5 (•) and 48.3 (▪) were preincubated with PA83, and the complexes were further incubated in the presence of LF with RAW264.7 cells. The viability of the cells was then assessed by a colorimetric assay. Results are expressed as the percentages of cells still viable. The experiment was carried out at least three times for each MAb with less than 10% of variability.
The domains of PA83 recognized by MAbs 7.5 and 48.3 were determined by Western blotting with chymotrypsin digestion fragments of PA83 (Fig. 2). Chymotrypsin cleaves PA83 at a consensus site after residue F313 within domain 2, leading to an amino-terminal fragment of 37 kDa (PA37) and a carboxy-terminal fragment of 47 kDa (PA47) (Fig. 2A) (26, 27, 31). Both of the MAbs recognized PA47, indicating that the epitopes mapped between positions 313 and 735, corresponding to the region from domain 2 to the end of domain 4 (Fig. 2B). We then tested the antibodies against mutant PA83 proteins carrying deletions in domain 4: PA608, PA711, and PA705 (Fig. 2C) (4). PA608 does not have a domain 4, and PA711 and PA705 contain deletions of 9 and 16 amino acids, respectively, in the exposed loop of 19 amino acids beginning at position 705 (4). Both antibodies recognized PA705 and PA711. MAb 48.3 recognized PA608, but MAb 7.5 did not. Thus, MAb 7.5 recognizes an epitope located between residues 608 and 735 (domain 4), and MAb 48.3 recognizes an epitope between residues 314 and 608 (part of domain 2 through domain 3).
FIG. 2.
PA83 domains recognized by the MAbs. (A) Schematic representation of fragments generated by cleavage of PA83 by chymotrypsin. Domain 1 (residues 1 to 258), domain 2 (residues 259 to 487), domain 3 (residues 488 to 595), and domain 4 (residues 596 to 735) are shown. (B) Chymotrypsin digestion fragments of PA83 (each, 1 μg) were subjected to electrophoresis and were transferred to a nitrocellulose membrane for Western blotting with MAbs 7.5 and 48.3 as first antibodies. (C) PA83 and PA83 proteins with mutations in domain 4 (PA608, PA705, and PA711) were absorbed onto a nitrocellulose membrane for a dot blot experiment with MAbs 7.5 and 48.3 as first antibodies.
Steps of cellular trafficking of PA83 blocked by MAbs.
We used CHO-K1 cells to determine which steps of the action of anthrax toxins are affected by MAbs. PA83 was incubated at 4°C with cells in the absence of MAbs or in the presence of concentrations of MAbs that do not affect Letx activity (10 ng/ml) (Fig. 1). PA83 was partially cleaved by furin, thus explaining the presence of PA63 at a concentration of 10 ng of both MAbs/ml (Fig. 3 and data not shown). As the concentration of MAb 7.5 increased, the signal intensity observed by autoradiography (the amount of PA83 bound to the cells) decreased. Thus, binding of MAb 7.5 to domain 4 of PA83 prevented its interaction with its cell receptor. This result agrees with previous findings and is consistent with the essential role of domain 4 of PA83 in the interaction of the molecule with the cell receptor. In contrast, addition of MAb 48.3 did not affect binding of PA83 to the cell surface: the amount of cell-bound PA83 was the same at all MAb 48.3 concentrations. However, the abundance of the PA63 form decreased as the concentration of MAb 48.3 increased and as the amount bound to PA83 increased. Therefore, MAb 48.3 blocks the cleavage of PA83 at the RKKR site. Consequently, in the absence of PA83 cleavage, LF cannot interact with PA63, which presumably explains the neutralizing effect of MAb 48.3 on Letx activity. PA83 was also protected from the proteolytic cleavage of trypsin and protease in serum in vitro (5, 9) by the presence of MAb 48.3 (data not shown). This indicates that the effect of MAb 48.3 is not dependent on the interaction between PA83 and the cell surface.
FIG. 3.
Inhibition of the initial steps of the intoxication process. MAbs 7.5 and 48.3 were separately incubated with radiolabeled PA83 and then added to CHO-K1 cells at 4°C. Membrane proteins were solubilized and subjected to electrophoresis. The presence of PA83 at the surface of the cells was revealed by autoradiography. The experiment was carried out at least three times for each MAb.
Mapping of the epitope recognized by MAb 48.3.
We mapped the epitope recognized by MAb 48.3 by the phage display method (see Materials and Methods). Phages displaying at their surface random peptides of seven amino acids were tested for their capacity to bind to the antibody. After three rounds of selection, the affinity of the peptides for MAb 48.3 was quantified by ELISA. Thirty peptides with the best affinities were sequenced and analyzed with ClustalW software. Two consensus groups corresponding to 27 independent clones have been deduced, while three other sequences were determined and were unrelated. The first group, consisting of 16 clones, is characterized by Ser or Thr in first position, His in second position, Arg or Lys in third position, and a hydrophobic amino acid (Leu, Phe, or Ile) in fourth position. In 10 clones, the sixth position is occupied by Pro. The fifth and seventh positions are occupied by various amino acids. The sequences fit with the sequence 412SKNLAPI419, corresponding to a loop within domain 2, between β sheets 2β9 and 2β10 of PA (29). Comparison of the crystal structures of PA83 with that of the heptamer of PA63 (29) predicted that this loop may be involved in the interaction between two monomers of PA63 and thus may be hidden when PA63 is in the heptamer form. We therefore tested the ability of MAb 48.3 to recognize the heptamer (Fig. 4). It recognized PA83 but not the heptamer, in contrast to MAb 7.5, which recognized both PA83 and the heptamer. Therefore, the exposed loop between 2β9 and 2β10 in the heptamer is not accessible, suggesting that it is involved in the interaction between monomers of PA63.
FIG. 4.
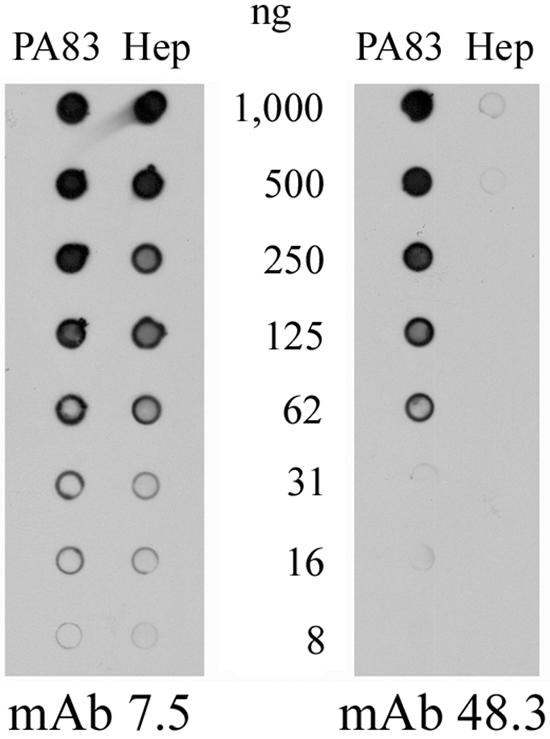
Purified PA83 or heptamer (Hep) of PA63 were diluted (from 1,000 to 8 ng) and adsorbed onto a nitrocellulose membrane for dot blotting with MAbs 7.5 and 48.3 as first antibodies. The experiment was carried out at least three times for each MAb.
The second group, consisting of 11 clones, is characterized by the sequence WDSPWWY/F, the seventh position being occupied by Tyr in two clones and by Phe in nine clones. These sequences are quite different from those of the first group. Sequence comparison with PA showed that none of these clones shares a significant similarity with the antigen. Nevertheless, they react with MAb 48-3 and thus represent PA mimotopes. Obtention of two types of consensus sequences, one corresponding to the epitope and the other corresponding to a mimotope, has previously been documented by phage display (6).
In vivo neutralizing activity of the antibodies.
We investigated the capacity of the MAbs to protect mice against a challenge with the toxinogenic Sterne strain (Fig. 5). The Sterne strain has a residual virulence, due exclusively to the activities of the toxins. These toxins act synergistically to produce an edema at the inoculation site and, at sufficiently high spore doses, cause death (5).
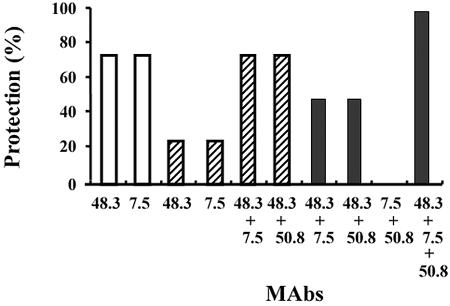
FIG. 5.
Protection of mice conferred by MAbs against challenge with Sterne strain spores. MAbs, alone or in combination as indicated, were administered intravenously to mice at doses per animal of 100 μg (white bars), 10 μg (hatched bars), and 1 μg (black bars). Results are expressed as the percentage of animals surviving challenge with the Sterne strain. Each point is the mean of at least two duplicate experiments.
Mice were injected intravenously with MAbs 48.3 and 7.5, alone or in combination. Sixteen hours later, they were challenged with 10 times the 50% lethal dose of the toxinogenic Sterne strain. None of the mice developed an edema at the inoculation site, suggesting that both MAbs neutralized the activity of the edema toxin. Doses of 1 μg per animal of either antibody failed to protect the mice (data not shown). Doses of 100 or 10 μg of each antibody separately protected 75 and 25% of animals, respectively. Interestingly, the simultaneous injection of the two MAbs at 10 or 1 μg per animal protected 75 and 50% of mice, respectively. Thus, there was additivity between the protective effects of the two MAbs. We then investigated the effects of inclusion of a neutralizing MAb directed against LF (MAb 50.8). MAb 50.8 [immunoglobulin G1(κ); Kd = 3 × 10−10 M] is directed against the amino-terminal part of LF involved in binding to PA63, similar to MAbs against LF described in previous studies (21, 22). MAb 50.8 may thus prevent the interaction of LF with PA63. The injection of 1 μg of MAb 50.8 failed to protect mice against a challenge with the Sterne strain (data not shown). Likewise, the combination of 1 μg of MAb 7.5 and 1 μg of MAb 50.8 did not protect animals (Fig. 5). In contrast, the combination of either 1 μg of MAb 7.5 and 1 μg of MAb 48.3 or 1 μg 48.3 and 1 μg of MAb 50.8 protected 50% of mice, thus providing evidence of cooperative effect between MAbs. The combination of MAbs 7.5, 48.3, and 50.8 at doses of 1 μg each fully protected mice. This is the first demonstration of protection induced by MAbs directed against PA83 and LF, neutralizing the anthrax toxin activities in an experimental mouse model of infection.
Here, we describe two MAbs against PA83, which neutralize the anthrax toxin activities in vitro and in vivo. These antibodies block the first steps in the mechanism of action of the toxin, i.e., the binding of PA83 to the cell surface (MAb 7.5) and the cleavage of PA83 by cellular furin-like proteases (MAb 48.3). PA83 is cleaved in domain 1, but interestingly MAb 48.3 (which blocks this cleavage) recognizes an epitope in domain 2 from residues 412 to 419. Possibly the antibody prevents cleavage of PA83 at the RKKR site, either due to steric hindrance or to an antibody-induced conformational change preventing protease recognition of the RKKR site in PA83.
Anthrax causes both septicemia and toxemia: septicemia due to the presence of a poly-γ-d-glutamic acid capsule covering the bacilli and toxemia due to the production of toxins. We show here that MAbs 7.5 and 48.3 prevent edema formation and the death of mice after infection by spores of the toxinogenic Sterne strain. This protective effect is enhanced by the addition of a neutralizing MAb directed against LF. Our findings show that MAbs against toxin components can prevent toxemia associated with Sterne strain infection.
The bioterrorist events in the United States in 2001 revealed that treatment with antibiotics is not always sufficient to prevent patient deaths, due to the effects of toxin production. Humanized neutralizing MAbs may therefore be of great therapeutic value, complementing antibiotic treatment to prevent the toxin-dependent symptoms of anthrax.
Acknowledgments
We are grateful to Odile Jeannequin and Sylvie Rouyre for the production of the MAbs and for their help with epitope mapping. We thank Patricia Sylvestre for her help in the mapping and sequencing of the epitope of MAb 48.3.
This work was supported by the Délégation Générale à l'Armement (DGA), grant 99-34030. F.B. was supported by DGA.
Editor: J. T. Barbieri
Footnotes
This work is dedicated to the memory of Martine Lévy.
REFERENCES
- 1.Abrami, L., S. H. Liu, P. Cosson, S. H. Leppla, and F. G. van der Goot. 2003. Anthrax toxin triggers endocytosis of its receptor via a lipid raft-mediated clathrin-dependent process. J. Cell Biol. 160:321-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beall, F. A., M. J. Taylor, and C. B. Thorne. 1962. Rapid lethal effects in rats of a third component found upon fractionating the toxin of Bacillus anthracis. J. Bacteriol. 83:1274-1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley, K. A., J. Mogridge, M. Mourez, R. J. Collier, and J. A. Young. 2001. Identification of the cellular receptor for anthrax toxin. Nature 414:225-229. [DOI] [PubMed] [Google Scholar]
- 4.Brossier, F., J. C. Sirard, C. Guidi-Rontani, E. Duflot, and M. Mock. 1999. Functional analysis of the carboxy-terminal domain of Bacillus anthracis protective antigen. Infect. Immun. 67:964-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brossier, F., M. Weber-Levy, M. Mock, and J. C. Sirard. 2000. Role of toxin functional domains in anthrax pathogenesis. Infect. Immun. 68:1781-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demangel, C., P. Lafaye, and J. C. Mazié. 1996. Reproducing the immune response against the Plasmodium vivax merozoite surface protein 1 with mimotopes selected from a phage-displayed peptide library. Mol. Immunol. 33:909-916. [DOI] [PubMed] [Google Scholar]
- 7.Doyen, N., C. Lapresle, P. Lafaye, and J. C. Mazié. 1985. Study of the antigenic structure of human serum albumin with monoclonal antibodies. Mol. Immunol. 22:1-10. [DOI] [PubMed] [Google Scholar]
- 8.Duesbery, N. S., C. P. Webb, S. H. Leppla, V. M. Gordon, K. R. Klimpel, T. D. Copeland, N. G. Ahn, M. K. Oskarsson, K. Fukasawa, K. D. Paull, and G. F. Vandewoude. 1998. Proteolytic inactivation of map-kinase-kinase by anthrax lethal factor. Science 280:734-737. [DOI] [PubMed] [Google Scholar]
- 9.Ezzell, J. W., Jr., and T. G. Abshire. 1992. Serum protease cleavage of Bacillus anthracis protective antigen. J. Gen. Microbiol. 138:543-549. [DOI] [PubMed] [Google Scholar]
- 10.Friedlander, A. M. 1986. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J. Biol. Chem. 261:7123-7126. [PubMed] [Google Scholar]
- 11.Friguet, B., A. F. Chaffotte, L. Djavadi-Ohaniance, and M. E. Goldberg. 1985. Measurements of the true affinity constant in solution of antigen-antibody complexes by enzyme-linked immunosorbent assay. J. Immunol. Methods 18:305-319. [DOI] [PubMed] [Google Scholar]
- 12.Hansen, M. B., S. E. Nielsen, and K. Berg. 1989. Re-examination and further development of a precise and rapid dye method for measuring cell growth/cell kill. J. Immunol. Methods 119:203-210. [DOI] [PubMed] [Google Scholar]
- 13.Klimpel, K. R., N. Arora, and S. H. Leppla. 1994. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol. Microbiol. 13:1093-1100. [DOI] [PubMed] [Google Scholar]
- 14.Klimpel, K. R., S. S. Molloy, G. Thomas, and S. H. Leppla. 1992. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc. Natl. Acad. Sci. USA 89:10277-10281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kobiler, D., Y. Gozes, H. Rosenberg, D. Marcus, S. Reuveny, and Z. Altboum. 2002. Efficiency of protection of guinea pigs against infection with Bacillus anthracis spores by passive immunization. Infect. Immun. 70:544-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohler, G., and C. Milstein. 1975. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256:495-497. [DOI] [PubMed] [Google Scholar]
- 17.Leppla, S. H. 1982. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations in eukaryotic cells. Proc. Natl. Acad. Sci. USA 79:3162-3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leppla, S. H. 1995. Anthrax toxins, p. 543-563. In J. Moss, B. Iglewski, M. Vaughan, and A. T. Tu (ed.), Bacterial toxins and virulence factors in disease, vol. 8. Handbook of natural toxins. Marcel Dekker, New York, N.Y.
- 19.Little, S. F., B. E. Ivins, M. F. Fellows, and A. M. Friedlander. 1997. Passive protection by polyclonal antibodies against Bacillus anthracis infection in guinea pigs. Infect. Immun. 65:5171-5175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Little, S. F., S. H. Leppla, and E. Cora. 1988. Production and characterization of monoclonal antibodies to the protective antigen component of Bacillus anthracis toxin. Infect. Immun. 56:1807-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Little, S. F., S. H. Leppla, and A. M. Friedlander. 1990. Production and characterization of monoclonal antibodies against the lethal factor component of Bacillus anthracis lethal toxin. Infect. Immun. 58:1606-1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Little, S. F., J. M. Novak, J. R. Lowe, S. H. Leppla, Y. Singh, K. R. Klimpel, B. C. Lidgerding, and A. M. Friedlander. 1996. Characterization of lethal factor binding and cell receptor binding domains of protective antigen of Bacillus anthracis using monoclonal antibodies. Microbiology 142:707-715. [DOI] [PubMed] [Google Scholar]
- 23.Maynard, J. A., C. B. M. Maassen, S. H. Leppla, K. Brasky, J. L. Patterson, B. L. Iverson, and G. Georgiou. 2002. Protection against anthrax toxin by recombinant antibody fragments correlates with antigen affinity. Nat. Biotechnol. 20:597-601. [DOI] [PubMed] [Google Scholar]
- 24.Milne, J. C., D. Furlong, P. C. Hanna, J. S. Wall, and R. J. Collier. 1994. Anthrax protective antigen forms oligomers during intoxication of mammalian cells. J. Biol. Chem. 269:20607-20612. [PubMed] [Google Scholar]
- 25.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 26.Mogridge, J., M. Mourez, and R. J. Collier. 2001. Involvement of domain 3 in oligomerization by the protective antigen moiety of anthrax toxin. J. Bacteriol. 183:2111-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Novak, J. M., P. Stein, S. F. Little, S. H. Leppla, and A. M. Friedlander. 1992. Functional characterization of protease-treated Bacillus anthracis protective antigen. J. Biol. Chem. 267:17186-17193. [PubMed] [Google Scholar]
- 28.Pellizzari, R., C. Guidi-Rontani, G. Vitale, M. Mock, and C. Montecucco. 2000. lethal factor of Bacillus anthracis cleaves the N-terminus of MAPKKs: analysis of the intracellular consequences in macrophages. Int. J. Med. Microbiol. 290:421-427. [DOI] [PubMed] [Google Scholar]
- 29.Petosa, C., R. J. Collier, K. R. Klimple, S. H. Leppla, and R. Lidindgton. 1997. Crystal structure of the anthrax toxin protective antigen. Nature 385:933-938. [DOI] [PubMed] [Google Scholar]
- 30.Sellman, B. R., S. Nassi, and J. R. Collier. 2001. Point mutations in anthrax protective antigen that block translocation. J. Biol. Chem. 16:8371-8376. [DOI] [PubMed] [Google Scholar]
- 31.Singh, Y., V. K. Chaudhary, and S. H. Leppla. 1989. A deleted variant of Bacillus anthracis protective antigen is non-toxic and blocks anthrax toxin in vivo. J. Biol. Chem. 264:19103-19107. [PubMed] [Google Scholar]
- 32.Singh, Y., K. R. Klimpel, N. Arora, M. Sharma, and S. H. Leppla. 1994. The chymotrypsin-sensitive site, FFD315, in anthrax toxin protective antigen is required for translocation of lethal factor. J. Biol. Chem. 269:29039-29046. [PubMed] [Google Scholar]
- 33.Singh, Y., K. R. Klimpel, C. P. Quinn, V. K. Chaudhary, and S. H. Leppla. 1991. The carboxyl-terminal end of protective antigen is required for receptor binding and anthrax toxin activity. J. Biol. Chem. 266:15493-15497. [PubMed] [Google Scholar]
- 34.Stanley, J. L., and H. Smith. 1961. Purification of factor I and recognition of a third factor of anthrax toxin. J. Gen. Microbiol. 26:49-66. [DOI] [PubMed] [Google Scholar]
- 35.Varughese, M., A. V., Teixeira, S. Liu, and S. H. Leppla. 1999. Identification of a receptor-binding region within domain 4 of the protective antigen component of anthrax toxin. Infect. Immun. 67:1860-1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vitale, G., R. Pellizzarri, C. Recchi, G. Napolitani, M. Mock, and C. Montecucco. 1998. Anthrax lethal factor cleaves the N-terminus of MAPKKs and induces tyrosine/threonine phosphorylation of MAPKs in cultured macrophages. Biochem. Biophys. Res. Commun. 248:706-711. [DOI] [PubMed] [Google Scholar]