Abstract
Infection of macrophages with Mycobacterium tuberculosis or exposure to M. tuberculosis 19-kDa lipoprotein for >16 h inhibits gamma interferon (IFN-γ)-induced major histocompatibility complex class II (MHC-II) expression by a mechanism involving Toll-like receptors (TLRs). M. tuberculosis was found to inhibit murine macrophage MHC-II antigen (Ag) processing activity induced by IFN-γ but not by interleukin-4 (IL-4), suggesting inhibition of IFN-γ-induced gene regulation. We designed an approach to test the ability of M. tuberculosis-infected cells to respond to IFN-γ. To model chronic infection with M. tuberculosis with accompanying prolonged TLR signaling, macrophages were infected with M. tuberculosis or incubated with M. tuberculosis 19-kDa lipoprotein for 24 h prior to the addition of IFN-γ. Microarray gene expression studies were then used to determine whether prolonged TLR signaling by M. tuberculosis broadly inhibits IFN-γ regulation of macrophage gene expression. Of 347 IFN-γ-induced genes, M. tuberculosis and 19-kDa lipoprotein inhibited induction of 42 and 36%, respectively. Key genes or gene products were also examined by quantitative reverse transcription-PCR and flow cytometry, confirming and extending the results obtained by microarray studies. M. tuberculosis inhibited IFN-γ induction of genes involved in MHC-II Ag processing, Ag presentation, and recruitment of T cells. These effects were largely dependent on myeloid differentiation factor 88, implying a role for TLRs. Thus, prolonged TLR signaling by M. tuberculosis inhibits certain macrophage responses to IFN-γ, particularly those related to MHC-II Ag presentation. This inhibition may promote M. tuberculosis evasion of T-cell responses and persistence of infection in tuberculosis.
Gamma interferon (IFN-γ) plays a critical role in host responses to a wide variety of viral and microbial pathogens (15, 31), including Mycobacterium tuberculosis. IFN-γ−/− mice are extremely susceptible to M. tuberculosis infection, and infection of these mice with M. tuberculosis leads to rapid death (6, 10). Genetic defects in IFN-γ signaling in humans also severely compromise host immune responses to mycobacterial infections (7, 16). In tuberculosis, one action of IFN-γ is to activate macrophages to control intracellular M. tuberculosis. Among genes induced by IFN-γ are inducible nitric oxide synthase (NOS2) (42) and phagocyte oxidase (23), leading to the production of reactive nitrogen and oxygen intermediates. IFN-γ also enhances the ability of macrophages to process and present antigens (Ags) to CD4+ T cells through upregulation of class II major histocompatibility complex (MHC-II), H-2M, invariant chain, and accessory molecules.
Our studies address the ability of M. tuberculosis to inhibit IFN-γ-induced macrophage responses. Due to the importance of IFN-γ-induced responses to host defense in tuberculosis, it is important to consider that M. tuberculosis may have mechanisms to inhibit or evade certain IFN-γ-induced responses, and published data support this hypothesis. Human macrophages infected with M. tuberculosis are defective in their ability to upregulate CD64 (Fcγ RI), CIITA, and MHC-II upon stimulation with IFN-γ (11, 12, 19, 26, 28, 38). We have previously shown that chronic (>16 h) infection with M. tuberculosis or treatment with M. tuberculosis 19-kDa lipoprotein inhibits IFN-γ-induced expression of CIITA and MHC-II, resulting in decreased MHC-II Ag processing and/or presentation by macrophages (25, 26, 28, 39). On the other hand, M. tuberculosis does not appear to inhibit the expression of other IFN-γ-responsive genes (19). The present study was designed to test the extent to which IFN-γ-regulated genes are similarly or differentially affected by exposure of macrophages to M. tuberculosis or M. tuberculosis 19-kDa lipoprotein.
The ability of M. tuberculosis 19-kDa lipoprotein to inhibit MHC-II expression is critically dependent on signaling through Toll-like receptors (TLRs), in particular TLR2 (26). TLR recognition of microbial molecules or pathogen-associated molecular patterns (PAMPs) is acutely associated with induction of host-beneficial innate immune responses. It is likely, however, that counterregulatory mechanisms are induced after prolonged TLR stimulation to limit potentially excessive proinflammatory reactions. One example of this is provided by the phenomenon of endotoxin tolerance. We propose that prolonged stimulation of TLRs by bacteria may downregulate certain immune mechanisms. For many acute bacterial infections, this may provide host-beneficial limitation of acute proinflammatory responses. For certain intracellular pathogens that have mechanisms to survive the acute phase, e.g., M. tuberculosis, these downregulatory mechanisms may provide a means to evade certain host immune functions.
We used microarray gene expression studies and other approaches to study macrophage gene expression and investigate the hypothesis that prolonged stimulation of TLRs by M. tuberculosis or a major M. tuberculosis PAMP, 19-kDa lipoprotein, inhibits IFN-γ-induced gene regulation. To model the impact of prolonged TLR signaling in chronic infection with M. tuberculosis, macrophages were infected with M. tuberculosis or incubated with M. tuberculosis 19-kDa lipoprotein for 24 h prior to addition of IFN-γ. This approach was designed to investigate the ability of a macrophage that is chronically infected with M. tuberculosis to respond to IFN-γ. We report that M. tuberculosis and 19-kDa lipoprotein inhibit induction of a significant proportion of IFN-γ-induced genes, including genes associated with Ag-presenting cell function. Our in vitro studies with M. tuberculosis were performed mostly with the avirulent H37Ra strain of M. tuberculosis, but we confirmed that similar inhibition of IFN-γ-induced gene expression was produced by virulent M. tuberculosis H37Rv. We conclude that inhibition of IFN-γ-induced responses may allow intracellular M. tuberculosis to evade immune surveillance by T cells, contributing to maintenance of chronic infection.
MATERIALS AND METHODS
Cells and reagents.
Standard medium was Dulbecco modified Eagle medium (Gibco, Rockville, Md.) supplemented with 10% heat-inactivated fetal calf serum (HyClone, Logan, Utah), 50 μM 2-mercaptoethanol, 1 mM sodium pyruvate, and 10 mM HEPES buffer. C57BL/6 mice (Jackson Laboratory, Bar Harbor, Maine) and myeloid differentiation factor 88 (MyD88)−/− mice (generously provided by Osamu Takeuchi and Shizua Akira, Osaka University, Osaka, Japan [1, 34] and bred onto the C57BL/6 background) were housed under specific-pathogen-free conditions. Macrophages were derived from femur marrow precursors differentiated in bacterial-grade dishes for at least 10 days in standard medium with 20% LADMAC conditioned medium (32). Resulting macrophages were used between days 10 to 12. Recombinant murine IFN-γ was from R&D Systems (Minneapolis, Minn.).
M. tuberculosis culture and purification of 19-kDa lipoprotein.
Unless otherwise stated, M. tuberculosis H37Ra was used; some experiments used M. tuberculosis H37Rv. M. tuberculosis (American Type Culture Collection) was grown to log phase in Middlebrook 7H9 medium (Difco, Detroit, Mich.) with albumin, dextrose, and catalase enrichments (Difco) and then harvested and frozen at −80°C (13). Bacterial titer was determined by counting CFU on 7H10 medium (Difco). M. tuberculosis 19-kDa lipoprotein was purified as described previously (28). Sodium dodecyl sulfate-polyacrylamide gel electrophoresis with silver staining or Western analysis by using a polyclonal rabbit anti-BCG serum (that detects many mycobacterial Ags) revealed a single major band of appropriate size that stained with monoclonal Ab to 19-kDa lipoprotein.
MHC-II Ag processing and presentation assays.
Macrophages were removed from dishes with trypsin-EDTA (Gibco) and plated in 96-well flat bottom plates (105 cells/well). Cells were incubated with or without M. tuberculosis 19-kDa lipoprotein for 24 h and then with 2 ng of recombinant IFN-γ or 10 ng of recombinant interleukin-4 (IL-4)/ml for 24 h in the continued presence or absence of M. tuberculosis 19-kDa lipoprotein. Cells were incubated with OVA for 2 h, fixed in 0.5% paraformaldehyde, washed and incubated with DOBW T hybridoma cells (105/well) for 24 h to detect OVA:I-Ab complexes. Supernatants were assessed for IL-2 by CTLL-2 bioassay with colorimetric determination by using Alamar Blue (Alamar Biosciences, Sacramento, Calif.) and a Bio-Rad 550 microplate reader.
Sample preparation for microarray analysis.
Macrophages were washed in standard medium and incubated with or without 30 nM 19-kDa lipoprotein for 24 h or infected with M. tuberculosis for 24 h (by incubation with M. tuberculosis at a multiplicity of infection [MOI] of 30:1 for 3 h, followed by washing and incubation for 21 h). Macrophages then were incubated for an additional 15 h with or without IFN-γ (2 ng/ml) in the continued presence or absence of the lipoprotein or M. tuberculosis. Total RNA was purified by using an RNeasy kit (Qiagen, Valencia, Calif.). Residual genomic DNA was removed by using RNase-free DNase (Qiagen). RNA was stored in RNase-free water at −80°C. RNA (5 to 8 μg) was reverse transcribed by using Superscript II reverse transcriptase (Invitrogen, Carlsbad, Calif.) with a T7-poly(dT) primer (Operon, Alameda, Calif.). After synthesis of the second strand, double-stranded cDNA was used to transcribe cRNA by using T7 RNA polymerase and biotinylated dUTP and dCTP ribonucleotides (Enzo, Farmingdale, N.Y.). Hybridization of cRNA to the mouse MG-U74Av2 GeneChip (Affymetrix, Santa Clara, Calif.) was carried out according to Affymetrix protocols, and chips were scanned with a gene array scanner. Test arrays (Affymetrix) were used to check cRNA samples for equal hybridization to 5′ and 3′ oligonucleotide probes of certain housekeeping genes.
Microarray data analysis.
For each condition, arrays from at least three independent experiments were processed and analyzed by using Microarray Suite version 5.0 (Affymetrix). To account for variations in staining of arrays, Affymetrix chip intensities were globally scaled to 1,500. Each gene on the chip was evaluated with a set of perfect match and mismatch probe pairs. A signal comprising a Tukey biweighted mean of the difference of perfect match minus mismatch probe values was generated. In addition, a Qualifier (“present,” “marginally present,” or “absent”) was assigned based upon the consistency of performance of the probe pairs in the probe sets by using the one-sided Wilcoxon's signed rank test. Two analyses were used to determine the genes induced or suppressed in treatment relative to baseline samples. First, the batch analysis tool was used to perform binary comparisons to filter out genes with inconsistent or minimal changes relative to baseline. For each gene, batch analysis provided a signal log ratio (SLR; a measure of the change in expression) and a degree of change (no change, increased, marginally increased, decreased, or marginally decreased). To determine the degree of change, each probe set in the treatment chip was compared to the same probe set in the baseline chip by using the Wilcoxon's signed rank statistical test. A gene was considered to be increased or decreased if the P value was <0.0025. A gene was considered to be marginally increased or marginally decreased if the P value was between 0.0025 and 0.003. Nine sample comparisons were performed (each of three treatment samples with each of three baseline samples). The mean fold change was calculated by averaging the nine SLRs and by using the following calculations. If the mean SLR was >0, then the mean fold change was 2avg SLR; if the mean SLR was <0, then the mean fold change was −2−avg SLR. In the initial stage of statistical analysis, genes were screened for induction by a single primary stimulus (e.g., IFN-γ) and included for subsequent analysis if the qualifier was “present” in all three treatment samples, the degree of change was “increased” in nine of nine comparisons, and the mean fold change was ≥1.6. Suppressed genes were filtered by using similar criteria, requiring an absolute call of “present” in all three baseline samples, a difference call of “decreased” in nine of nine comparisons, and a mean fold change of ≤−1.6. These criteria set a stringent statistical basis for exclusively identifying only genes that were induced or suppressed (P < 0.0025) in nine of nine comparisons. Furthermore, a second set of statistical criteria were imposed by using GeneSpring 5.0 (GeneSpring, Redwood City, Calif.). The baseline and treatment expression values of genes passing the initial screen were compared by using a Welch's t test (assuming that the variances between the groups were not equal) with a P value cutoff of 0.05 for a change to be considered statistically significant.
To study the impact of a secondary stimulus (e.g., M. tuberculosis) on the response to the primary stimulus (IFN-γ), we performed analyses to assign genes regulated by the primary stimulus into a response category. IFN-γ-induced genes were termed “inhibited” by M. tuberculosis or 19-kDa lipoprotein (i.e., the expression in IFN-γ plus M. tuberculosis or IFN-γ plus 19-kDa lipoprotein was less than the expression in IFN-γ) if at least five of nine difference calls were “decreased” or “marginally decreased” with a mean fold change for all nine samples less than or equal to −1.2 and if the differences in expression between the two treatment groups were determined to be significant by using Welch's t test with a P value of <0.05. These criteria allowed us to categorize IFN-γ-induced genes into groups that were or were not inhibited by M. tuberculosis or 19-kDa lipoprotein. Similarly, IFN-γ-suppressed genes were termed rescued (i.e., the expression in IFN-γ plus M. tuberculosis or IFN-γ plus 19-kDa lipoprotein is greater than the expression in IFN-γ) if at least five of nine difference calls were “increased” or “marginally increased” with a mean fold change for all nine samples greater than or equal to 1.2 and if the differences in expression between the two treatment groups were determined to be significant by using Welch's t test with a P value of <0.05.
Flow cytometry.
Macrophages were collected by scraping; incubated in V-bottom 96-well plates (2 × 105/well) with 10% normal mouse serum (Jackson), 1% fetal calf serum, and 1:100 FcBlock (BD Pharmingen) in phosphate-buffered saline for 30 min; and stained with phycoerythrin-conjugated anti-CD80, anti-CD86, or rat IgG2a isotype control antibody. Cells were washed, resuspended in 2% paraformaldehyde, and analyzed with a FACScan flow cytometer (Becton Dickinson Immunocytometry Systems, San Jose, Calif.).
RNA purification, cDNA synthesis, and real-time quantitative PCR.
RNA (4 μg) was converted to cDNA by using SuperScript preamplification system (Life Technologies) for first-strand cDNA synthesis. The cDNA mixture was diluted 1:20 with PCR-grade water, and 2.5% (10 μl) of the cDNA product was used per reaction for real-time quantitative PCR by using a high-speed thermal cycler (I-Cycler; Bio-Rad). Product was detected by using iQ SYBR Green Supermix (Bio-Rad, Hercules, Calif.). The amplification cycle was 95°C for 10 s, 52°C for 15 s, and 72°C for 20 s. Primers were designed by using OLIGO v6.4 (Molecular Biology Insights, Cascade, Colo.). The primer sequences were as follows (5′ to 3′): CIITA mRNA, sense (ACGCTTTCTGGCTGGATTAGT) and antisense (TCAACGCCAGTCTGACGAAGG) (predicted size, 342 bp); I-Ab beta chain, sense (GCTCCTCAAGCGACTGTG) and antisense (AAGCTGGTCTCATAAACACCG) (predicted size, 155 bp); H-2M, sense (CAACAAGGAGAAGACGGCTCA) and antisense (CGCTGTGCTGAACCACG) (predicted size, 113 bp); invariant chain, sense (CTGAGATAAAGGCCCGCAGAC) and antisense (GCAGGATGTGAGGAGGGGTTA) (predicted size, 131 bp); VCAM-1, sense (TGACTTTCAGGTACTACTTTC) and antisense (CGCATTTAAATCAGGTTA) (predicted size, 129 bp); MIG, sense (GAATTTGGGGTGCTGTATCC) and antisense (AAGGTGTGGTTTGGGCTACTC) (predicted size, 169 bp); and GAPDH, sense (AACGACCCCTTCATTGAC) and antisense (TCCACGACATACTCAGCAC) (predicted size, 191 bp). Specific cDNA was quantified by standard curves. Standards were generated from amplified cDNA purified on agarose gels by QiaQuick gel extraction (Qiagen). Melting curve analysis confirmed that only one product was amplified. Specificity was confirmed by electrophoresis of PCR products through 1.5% agarose gels (stained with ethidium bromide). Only one product was observed with each primer set, and the product size matched that predicted from published cDNA sequences. Expression was normalized to GAPDH (shown not to be significantly affected by any treatment condition by microarray analysis).
RESULTS
M. tuberculosis and M. tuberculosis 19-kDa lipoprotein inhibit the ability of IFN-γ but not IL-4 to induce MHC-II Ag processing in macrophages.
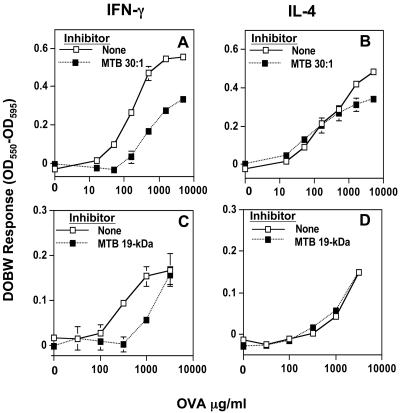
We explored the impact of M. tuberculosis and M. tuberculosis 19-kDa lipoprotein on IFN-γ induction of macrophage MHC-II Ag processing function (unless otherwise stated, M. tuberculosis refers to the H37Ra strain; certain results were confirmed with the H37Rv strain). IFN-γ-dependent induction of MHC-II Ag processing function was inhibited by prolonged incubation of macrophages with M. tuberculosis (Fig. 1A) or 19-kDa lipoprotein (Fig. 1C and reference (28). In addition, M. tuberculosis and 19-kDa lipoprotein have been shown to inhibit IFN-γ-dependent expression of MHC-II (26, 28) and class II transactivator (CIITA, a transcription factor that controls MHC-II expression) (28). MHC-II Ag processing and/or presentation function was also induced by IL-4 (Fig. 1 and data not shown), although to a lesser degree than with IFN-γ. In contrast to the results with IFN-γ, induction of MHC-II Ag processing by IL-4 was not inhibited by M. tuberculosis (Fig. 1B) or 19-kDa lipoprotein (Fig. 1D and reference 28). This observation suggested a selective inhibition of IFN-γ-dependent regulation of genes involved in MHC-II Ag processing, leading to the hypothesis that prolonged exposure of macrophages to M. tuberculosis or 19-kDa lipoprotein inhibits many genes regulated by IFN-γ. Therefore, we tested the extent to which IFN-γ regulation of gene expression was inhibited by prior exposure to M. tuberculosis and 19-kDa lipoprotein by using microarray gene expression analysis.
FIG. 1.
M. tuberculosis and its 19-kDa lipoprotein inhibit IFN-γ but not IL-4 induced MHC-II Ag processing. (A and B) C57BL/6 macrophages were treated for 24 h with or without M. tuberculosis 19-kDa lipoprotein (30 nM) or M. tuberculosis (MOI = 30:1). Macrophages then were incubated with IFN-γ (A) or IL-4 (B) for 24 h in the continued presence or absence of the lipoprotein or whole bacteria, incubated with OVA for 2 h, fixed, and incubated with DOBW T hybridoma cells for 24 h. The results of a colorimetric bioassay for IL-2 are expressed as the mean for triplicate wells ± the standard deviation. When error bars are not visible, they are smaller than the symbol width.
Gene regulation by M. tuberculosis, 19-kDa lipoprotein and IFN-γ.
To study regulation of gene expression, macrophages were incubated with or without 19-kDa lipoprotein or infected with M. tuberculosis for 24 h. Macrophages were then incubated for 15 h with or without IFN-γ in the continued presence or absence of the lipoprotein or M. tuberculosis infection. This protocol has been used for other studies of inhibition of Ag processing by 19-kDa lipoprotein and M. tuberculosis (28; data not shown). It is important to note that this protocol does not decrease viability of macrophages as assessed by trypan blue exclusion or cell yields from culture, does not induce detectable signs of apoptosis by TUNEL (terminal deoxynucleotidyltransferase-mediated dUTP-biotin nick end labeling) assays, does not inhibit certain active physiological functions of macrophages (e.g., phagocytosis), does not decrease expression of MHC-I (as opposed to MHC-II) or the ability of macrophages to present exogenous MHC-I-restricted peptides to CD8 T hybridoma cells, and does not decrease RNA yield (data not shown). Furthermore, the expression of many genes is unaltered by this protocol (below). We conclude that changes in gene expression observed with this protocol are not due to generalized toxicity or loss of viability.
To assess changes in expression of individual genes, cRNA was prepared and hybridized to the Affymetrix MG-U74Av2 microarray. Replicate samples from multiple experiments were analyzed, and two successive sets of statistical criteria were used to define genes affected by various treatments. First, analysis with Microarray Suite v5.0 was used to analyze results with each sample to exclude genes with low and/or statistically inconsistent expression values and to require a statistically significant increase or decrease by the experimental stimulus (see Materials and Methods). Genes passing the initial screen were subjected to a Welch's t test analysis of the results with multiple samples, and only genes with statistically significant (P < 0.05) increase or decrease in expression were identified (see Materials and Methods).
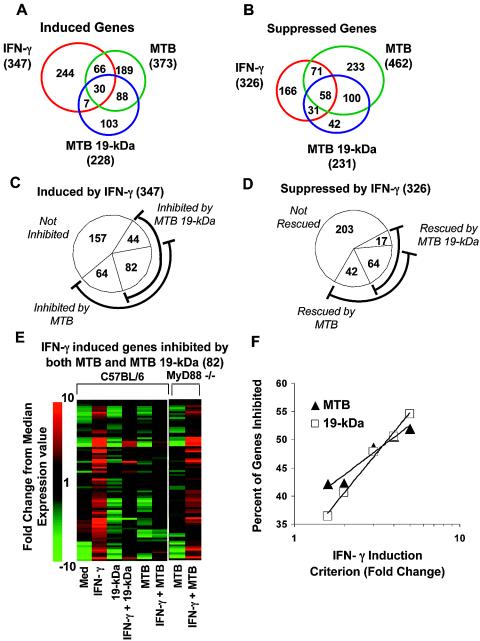
Infection of macrophages with M. tuberculosis resulted in induction of 373 genes and suppression of 462 genes (Fig. 2A and B). M. tuberculosis 19-kDa lipoprotein induced 228 genes and suppressed 231 genes. There was significant overlap in the sets of genes modulated by M. tuberculosis and 19-kDa lipoprotein. Of genes induced by M. tuberculosis, 32% were also induced by 19-kDa lipoprotein, and 34% of genes suppressed by M. tuberculosis were also suppressed by 19-kDa lipoprotein. Thus, a single component of M. tuberculosis may account for a significant proportion of observed changes in the macrophage transcriptome (similar to observations in other systems [3, 14]). After incubation of macrophages with standard medium for 24 h, the addition of IFN-γ for 15 h induced expression of 347 genes and suppressed expression of 326 genes (Fig. 2A and B). Although there was some overlap between genes induced by IFN-γ and those induced by M. tuberculosis and 19-kDa lipoprotein, the majority (70%) of genes induced by IFN-γ were not induced by mycobacterial stimuli (Fig. 2A). Thus, although both IFN-γ and mycobacterial products have long been known to activate macrophages, they induce distinct patterns of activation.
FIG. 2.
Effects of M. tuberculosis and 19-kDa lipoprotein on IFN-γ-induced regulation of macrophage gene expression. Macrophages were incubated for 24 h with or without 30 nM 19-kDa lipoprotein or infected with M. tuberculosis (MOI = 30:1) for 24 h. Cells were then incubated for 15 h with or without 2 ng of IFN-γ/ml in the continued presence or absence of the lipoprotein or M. tuberculosis infection. The baseline sample was macrophages incubated in standard medium. RNA was isolated for microarray analysis. (A and B) Venn diagrams of genes induced (A) or suppressed (B) by IFN-γ, M. tuberculosis, and M. tuberculosis 19-kDa lipoprotein. Numbers below the treatment condition represent the total number of genes induced or suppressed. Numbers within the diagram represent the shared or unique genes induced by these stimuli. A gene was considered induced or suppressed by the stimulus if all nine comparisons were marked increased or decreased with absolute value of a mean fold change of ≥1.6, and the difference in expression values between the two groups was statistically significant based on Welch's t test. (C) Impact of M. tuberculosis and 19-kDa lipoprotein on expression of genes induced by IFN-γ. Inhibited genes were defined as those with decreased or marginally decreased expression in IFN-γ plus M. tuberculosis (or IFN-γ plus 19-kDa lipoprotein) compared to IFN-γ alone in at least five of nine comparisons with a mean fold change less than or equal to −1.2 and a statistically significant difference in expression by using the Welch's t test. (D) Impact of M. tuberculosis and 19-kDa lipoprotein on IFN-γ-mediated gene suppression. A gene was considered rescued if it was marked increased or marginally increased in at least five of nine comparisons with mean fold change greater than or equal to 1.2 and a statistically significant difference in expression as determined by using Welch's t test. (E) Expression patterns of the genes inhibited by both M. tuberculosis and M. tuberculosis 19-kDa lipoprotein. The 82 genes inhibited by both M. tuberculosis and M. tuberculosis 19-kDa lipoprotein were organized by using hierarchical clustering. The relative expression values of the inhibited genes are shown. (F) Genes strongly induced by IFN-γ are more likely to be inhibited by M. tuberculosis and 19-kDa lipoprotein. The x axis shows the fold change criterion used to determine the subset of genes that were induced by IFN-γ (as in Fig. 2A). The y axis shows the percentage of genes determined to be inhibited by either M. tuberculosis or M. tuberculosis 19-kDa lipoprotein (as in Fig. 2C).
Table 1 lists the 10 most highly regulated genes (with highest fold change values) and some selected genes regulated by IFN-γ, 19-kDa lipoprotein, and M. tuberculosis (a full list of genes is also available from the authors). Not surprisingly, the genes induced by IFN-γ include genes that are critical in presentation of Ag to CD4+ T cells, including CIITA, MHC-II, H-2M, and CD86. IFN-γ also induced T-cell attractants, e.g., monokine induced by IFN-γ (MIG) and IP-10, as well as chemokines involved in the recruitment of monocytes, e.g., MCP-2 and MCP-5. IFN-γ-induced genes also included many GTP-binding proteins, e.g., GBP-1, IIGP, IGTP, TGTP/Mg21, Mx1, IRG-47, and LRG-47, many of which have been shown to have antiviral or antibacterial activity. Of these proteins, LRG-47 has been implicated in the control of M. tuberculosis infection (21), and it is interesting to consider that the others may also have antimycobacterial activity. IFN-γ also induced important transcription factors such as Stat1, IRF-1, and IRF-7.
TABLE 1.
List of genes induced or suppressed by IFN-γ, 19-kDa lipoprotein, and M. tuberculosis
| Conditiona | Induced
|
Suppressed
|
||
|---|---|---|---|---|
| Gene/GenBank accession no. | Fold change | Gene/GenBank accession no. | Fold change | |
| IFN-γ | ||||
| Ten most regulated genes | Monokine induced by IFN-γ/M34815 | 496 | Gab1/AI046826 | −42 |
| Guanylate binding protein-1/M55544 | 489 | Matrix metalloproteinase 9/X72795 | −25 | |
| Calponin 3/AW125626 | 164 | Hydroxyprostaglandin dehydrogenase 15/U44389 | −15 | |
| IIGP protein/AJ007971 | 62 | Epithelial membrane protein 1/X98471 | −14 | |
| T-cell-specific protein/L38444 | 58 | Basic helix-loop-helix domain, class 2/Y07836 | −14 | |
| Uridine phosphorylase/D44464 | 54 | Cyclin-dependent kinase inhibitor 2B/AF059567 | −12 | |
| Prostaglandin synthase 2/M88242 | 51 | CD28/M34563 | −11 | |
| Serine proteinase inhibitor 2/M64085 | 40 | Growth arrest specific protein 6/X59846 | −11 | |
| IL-12 receptor beta chain precursor/U23922 | 39 | Ras homolog/AW121127 | −10 | |
| Ly6E.1/X04653 | 36 | CXCR-4/Z80112 | −10 | |
| IFN-γ | ||||
| Selected genes | MCP-2 precursor/AB023418 | 36 | C-type lectin (MCL)/AF061272 | −10 |
| IP-10/M33266 | 27 | IL-1 receptor-like protein 1 (IL1RL1)/D13695 | −8 | |
| CD86/L25606 | 12 | MIP-1α/J04491 | −7 | |
| IRF-7/U73037 | 10 | CD14/X13333 | −7 | |
| MCP-5/U50712 | 9 | IGF-1/X04480 | −6 | |
| IRF-1/M21065 | 7 | IL-7 receptor/M29697 | −6 | |
| H-2M α-chain/U35323 | 6 | CD24a/M58661 | −6 | |
| VCAM-1/M84487 | 5 | Mannose receptor/Z11974 | −5 | |
| MHC-II/X52643 | 3 | C5a receptor/S46665 | −5 | |
| CIITA/AF042158 | 3 | TGF-β1/X62940 | −4 | |
| M. tuberculosis 19-kDa protein | ||||
| Ten most regulated genes | MARCO/U18424 | 415 | Lymphocyte-specific protein/D49691 | −21 |
| Lipocalin 2/X81627 | 180 | High-mobility-group protein 1, isoform C/X99915 | −18 | |
| Formyl peptide receptor 1/L22181 | 150 | Rabkinesin-6/Y09632 | −11 | |
| SOCS-3/U88328 | 64 | Mast cell growth factor/M57647 | −10 | |
| Serum amyloid A/X03505 | 56 | Epithelial membrane protein 1/X9871 | −9 | |
| IL-1β/M15131 | 42 | Hydroxyprostaglandin dehydrogenase 15/U44389 | −8 | |
| DAF-1/D63679 | 37 | Cyclin D1/AI849928 | −8 | |
| N-Formylpeptide receptor like 2/AF071180 | 36 | Cysteine-rich intestinal protein/M13018 | −8 | |
| Lysyl oxidase/D10837 | 36 | Carboxypeptidase H/X61232 | −8 | |
| DAF-2/L41365 | 32 | Pcdh7/AB006758 | −8 | |
| Selected genes | CD38/L11332 | 25 | TGF-β1/X62940 | −7 |
| SLPI/AF002719 | 16 | IL-1 receptor-like protein 1 (IL1RL1)/D13695 | −7 | |
| PAI-II/X16490 | 11 | CCR2/U56819 | −7 | |
| CD11a/M60778 | 10 | Topoismerase II α/U01915 | −7 | |
| Fas/M83649 | 5 | Regulator of G-protein signaling-2/U67187 | −6 | |
| IL-4R, secreted form/M279604 | 4 | MHC-II/X52643 | −5 | |
| Superoxide dismutase/L35528 | 4 | CD24a/M58661 | −5 | |
| IL-10/M37897 | 4 | CCR5/AF022990 | −4 | |
| FcγRII/M31312 | 3 | CD9/L08115 | −4 | |
| Dendritic cell immunoreceptor/AJ133533 | 3 | CD36/L23108 | −3 | |
| M. tuberculosis | ||||
| Ten most regulated genes | IL-1α/M14639 | 439 | Hydroxyprostaglandin dehydrogenase 15/U44389 | −55 |
| Lipocalin 2/X81627 | 432 | PPARγ/U10374 | −49 | |
| IL-6/X54542 | 379 | Topoisomerase II α/U01915 | −28 | |
| PAI-II/X16490 | 281 | CCR2/U56819 | −25 | |
| Formyl peptide receptor 1/L22181 | 241 | Mannose receptor/Z11974 | −21 | |
| MARCO/U18424 | 209 | Transforming, acidic coiled-coil protein 3/AW209238 | −19 | |
| SOCS-3/U88328 | 185 | Microsomal expoxide hydrolase/U89491 | −18 | |
| IL-1b/M15131 | 182 | Cyclin D1/AI849928 | −17 | |
| KC (Gro-1)/J04596 | 127 | Apoptosis inhibitor 6/AF0114028 | −17 | |
| SLPI/AF002719 | 119 | Lymphocyte-specific protein/ D49691 | −15 | |
| Selected genes | Prostaglandin synthase 2/M88242 | 105 | CD39 (ATDPase)/ AF037366 | −15 |
| TRAF1/L35302 | 83 | Regulator of G-protein signaling-2/ U67187 | −14 | |
| IL-12 p35/ M86672 | 33 | Mast cell growth factor/M57647 | −12 | |
| MIP2/X53798 | 23 | IL-1 receptor-like protein 1 (IL1RL1)/D13695 | −6 | |
| DEC205/U19271 | 23 | IGF-1/X04480 | −6 | |
| CD1d1/M63695 | 18 | TGF-β1/X62940 | −5 | |
| Fas/M83649 | 11 | CCR5/ AF022990 | −5 | |
| G-CSF/ M13926 | 10 | CD36/L23108 | −5 | |
| NOS2/ U43428 | 10 | MHC-II/ X52643 | −4 | |
| TNF-α/D84196 | 6 | CD83/ AF001036 | −4 | |
See Fig. 2A and B.
Many of the genes that were induced by M. tuberculosis and 19-kDa lipoprotein are involved in acute inflammatory responses, including IL-1β, RANTES, griPGHS, and serum amyloid A. Cell surface receptors that were induced by M. tuberculosis and 19-kDa lipoprotein included the chemotactic bacterial peptide receptors for fMLP, FPR-1, and FPR-like-2 and the scavenger receptor MARCO. Genes that were induced by M. tuberculosis but not by 19-kDa lipoprotein included NOS2, CD1d1, DEC 205, and IL-12 p35 (IL-12 p40 was not induced by either stimulus at the time point that was analyzed).
The 326 genes that were suppressed by IFN-γ include many cell surface receptors, e.g., CXCR4, MCL, CD14, mannose receptor, C5a receptor, and IL-7 receptor. In addition, IFN-γ suppressed expression of the proinflammatory chemokines MIP-1α and MIP-1β. Like IFN-γ, M. tuberculosis 19-kDa lipoprotein suppressed expression of the mannose receptor. Both M. tuberculosis and 19-kDa lipoprotein suppressed many other genes, including CCR2, CCR5, CD36 (a scavenger receptor), and MHC-II.
M. tuberculosis and 19-kDa lipoprotein inhibit IFN-γ-dependent induction of many genes.
To determine the effect of M. tuberculosis on induction of IFN-γ responsive genes, we compared expression of the 347 IFN-γ-induced genes in macrophages with or without incubation with 19-kDa lipoprotein or infection with M. tuberculosis for 24 h prior to treatment with IFN-γ for 15 h. Statistical analysis was used to exclude genes with minimal or inconsistent changes and include only genes with statistically significant (P < 0.05) changes in expression (see Materials and Methods). Many genes induced by IFN-γ were inhibited by 19-kDa lipoprotein (36% or 126 of 347 genes were inhibited) or infection with M. tuberculosis (42% or 146 of 347 were inhibited) (Fig. 2C). A large proportion (56%) of genes that were inhibited by M. tuberculosis were also inhibited by 19-kDa lipoprotein (Fig. 2C and E), again suggesting the importance of this molecule in determining macrophage responses to M. tuberculosis. Figure 2E shows expression profiles of the 82 IFN-γ-induced genes that were inhibited by both M. tuberculosis 19-kDa lipoprotein and M. tuberculosis; this analysis clearly shows that IFN-γ-induced gene expression was inhibited for many, though not all, genes. In contrast, IFN-γ-induction of gene expression was increased by 19-kDa lipoprotein for only 12 genes (3.5%) and by M. tuberculosis infection for only 25 genes (7.2%). Table 2 lists some of the genes that were induced by IFN-γ but inhibited in macrophages infected with M. tuberculosis or treated with 19-kDa lipoprotein (a full list of genes is available). Although most experiments were done with M. tuberculosis H37Ra, parallel experiments confirmed that M. tuberculosis H37Rv inhibited a similar set of IFN-γ-induced genes that included genes related to Ag presentation (Table 2). The greater degree of inhibition seen in Table 2 with H37Ra may not be biologically significant and probably reflects minor differences between bacterial stocks or minor technical differences that were required to adapt the protocol for greater biological safety measures in samples with H37Rv. These results demonstrate that M. tuberculosis and 19-kDa lipoprotein both substantially inhibit IFN-γ-induced expression of a large number of genes.
TABLE 2.
Selected genes induced by IFN-γ but inhibited by M. tuberculosis or 19-kDa lipoprotein
| Gene/GenBank accession no. | Fold inductiona
|
|||
|---|---|---|---|---|
| IFN-γ | IFN-γ + 19-kDa lipoprotein | IFN-γ + H37Ra | IFN-γ + H37Rv | |
| I-A β chain/M21932 | 4.7 | −1.6* | −1.0* | 1.7* |
| I-A α chain/X52643 | 3.4 | −2.5* | −2.6* | 1.4* |
| CD86/L25606 | 11.6 | 1.9* | 3.0* | 4.3* |
| VCAM-1/M84487 | 5.5 | −7.8* | −1.2* | 1.5* |
| MIG/M34815 | 496.5 | 195.5* | 78.8* | 186.7* |
| IL-12 receptor, β2/U64199 | 4.1 | −1.3* | −1.6* | 1.1* |
| TRAIL/U37522 | 13.2 | 4.3* | 4.8* | 8.1* |
| NKG2D/AF054819 | 16.7 | 2.3* | 2.3* | 7.8* |
| Inositol triphosphate receptor/X15373 | 4.2 | 1.3* | −1.0* | 2.2* |
| Thromboxane A synthase/L18868 | 1.9 | −1.3* | −1.9* | −1.3* |
| ALK1: TGF-b receptor type II/L48015 | 2.5 | 1.3* | 1.4* | 1.3* |
| Caspase 3/U54803 | 3.4 | 1.8* | 1.2* | 2.0* |
| Serine protease inhibitor 2/M64085 | 40.0 | 20.5* | 5.6* | 14.0* |
| Cyclin D2/M83749 | 23.9 | 1.7* | 1.3* | 5.2* |
| Ly6E.1/X04653 | 35.6 | 9.1* | 25.0* | 18.2* |
| GBP-1/M55544 | 489.0 | 48.9* | 1.5* | 32.2 |
| CIITA/AF042158 | 3.2 | 1.1* | −1.0* | 1.7 |
| Chromaffin ATPase/U75321 | 2.4 | 1.7 | −2.2* | −2.2* |
| MD-1/AB007599 | 2.6 | 1.3 | −1.8* | 1.5* |
| H-2M α-chain/U35323 | 6.3 | 1.8 | 1.1* | 2.3* |
| H-2M β-chain/U35330 | 6.7 | 1.4 | 1.2* | 2.5* |
| TNF receptor 1a/X57796 | 2.1 | 1.6 | 1.1* | 1.3* |
| Cyclin 3/M86183 | 1.8 | 1.4 | 1.1* | 1.2* |
| IL-10Rα/L12120 | 3.5 | 1.3 | −1.5* | 1.3* |
| Invariant chain/X00496b | 1.59 | −2.2 | −2.8* | 1.2* |
Asterisks indicate changes relative to IFN-γ alone that reached statistical significance in microarray studies (see Materials and Methods). RT-PCR studies indicated statistically significant inhibition by both 19-kDa lipoprotein and M. tuberculosis H37Ra of invariant chain induction by IFN-γ.
Invariant chain is included in this table, although it narrowly missed fulfilling the 1.6-fold criterion for induction by IFN-γ in microarray studies. Inhibition of invariant chain expression reached statistical significance with M. tuberculosis H37Ra and H37Rv but not 19-kDa lipoprotein. RT-PCR studies indicated statistically significant inhibition by both 19-kDa lipoprotein and M. tuberculosis (P < 0.001).
We also tested whether genes that were more strongly induced by IFN-γ were more likely to be inhibited by mycobacterial products. The fold change criterion used to define the set of IFN-γ-induced genes was varied, and the ability of M. tuberculosis and 19-kDa lipoprotein to block IFN-γ induction of these genes was then determined. As the fold change criterion for IFN-γ induction increased, an increasing proportion of genes was inhibited by M. tuberculosis and 19-kDa lipoprotein (Fig. 2F). Of 77 genes with a fold change of ≥5 in response to IFN-γ, 54% had decreased expression in the presence of 19-kDa lipoprotein, and 52% were inhibited upon infection with M. tuberculosis. Thus, genes with expression that was more dependent on IFN-γ were more likely to be identified as inhibited by 19-kDa lipoprotein or M. tuberculosis. This effect may be based on a statistical or technical phenomenon rather than a biological mechanism, since a statistically significant impact of M. tuberculosis on IFN-γ-regulated gene expression may be easier to detect for genes with high fold induction by IFN-γ. Nonetheless, this observation underscores the inhibition of gene expression for a set of IFN-γ-induced genes.
M. tuberculosis and 19-kDa lipoprotein rescue many genes from IFN-γ-mediated suppression.
IFN-γ was also shown to suppress 326 genes, and many were rescued from suppression by the presence of M. tuberculosis (32% rescued) or 19-kDa lipoprotein (25% rescued) (Fig. 2D [a full list of genes is available from the authors]). Once again, there was overlap in the genes affected by M. tuberculosis and 19-kDa lipoprotein, since 60% of genes rescued from suppression by M. tuberculosis were also rescued by 19-kDa lipoprotein. A much smaller proportion of genes suppressed by IFN-γ were further suppressed by M. tuberculosis (11%) or 19-kDa lipoprotein (4%). M. tuberculosis and 19-kDa lipoprotein rescued IFN-γ-suppressed expression of CD14, macrophage scavenger receptor 1, p75 TNF receptor, and C5a receptor. In summary, M. tuberculosis and 19-kDa lipoprotein affect the ability of IFN-γ to modulate the expression of many genes involved in the regulation of the immune response.
Flow cytometry and real-time quantitative RT-PCR studies confirm that M. tuberculosis and 19-kDa lipoprotein inhibit IFN-γ-induced genes involved in MHC-II Ag processing, Ag presentation, and T-cell recruitment.
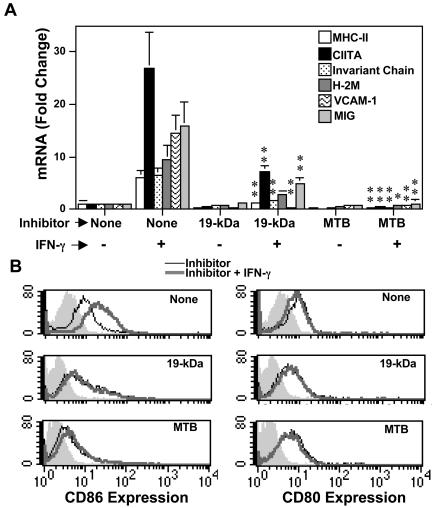
Quantitative real-time reverse transcription-PCR (RT-PCR) and flow cytometry were used to independently confirm conclusions based on microarray studies, particularly the conclusion that M. tuberculosis and 19-kDa lipoprotein inhibited IFN-γ induction of genes involved in MHC-II Ag presentation (Table 2). Quantitative RT-PCR showed that IFN-γ induction of genes related to MHC-II Ag processing (e.g., CIITA, MHC-II, H-2M, and invariant chain) was substantially inhibited by 19-kDa lipoprotein and to an even greater degree by M. tuberculosis (Fig. 3A). For example, IFN-γ-induced expression of CIITA was inhibited to 27 and 2% of control levels by 19-kDa lipoprotein and M. tuberculosis, respectively. Figure 3A also shows that invariant chain was inhibited by M. tuberculosis and 19-kDa lipoprotein (expression of invariant chain, MHC-II and H-2M is at least partially controlled by CIITA). Invariant chain narrowly missed the ≥1.6-fold IFN-γ induction criterion (the fold induction by IFN-γ was 1.59 for invariant chain), but it is discussed here due to its involvement in MHC-II Ag processing. In microarray studies, significant inhibition of invariant chain was produced by M. tuberculosis (both H37Ra and H37Rv); 19-kDa lipoprotein produced a decrease that did not reach statistical significance (Table 2). Quantitative RT-PCR studies showed that induction of invariant chain by IFN-γ was also significantly decreased (P < 0.01) by both M. tuberculosis and 19-kDa lipoprotein. Thus, additional studies confirmed that IFN-γ induction of MHC-II Ag processing genes (MHC-II, CIITA, H-2M, and invariant chain) was blocked by M. tuberculosis and 19-kDa lipoprotein. It is important to note that the RT-PCR studies revealed a greater degree of inhibition than the microarray studies, supporting the biological significance of these observations.
FIG. 3.
M. tuberculosis and 19-kDa lipoprotein inhibit IFN-γ-induced expression of molecules involved in MHC-II Ag processing and presentation. Macrophages were infected with M. tuberculosis (MOI = 30:1) or incubated with 30 nM 19-kDa lipoprotein for 24 h. IFN-γ (2 ng/ml) was added for 24 h. (A) RNA was isolated, and quantitative real-time RT-PCR was used to analyze expression of MHC-II, CIITA, invariant chain, H-2M, VCAM-1, and MIG. The results are expressed as mean ± the standard deviation for triplicate samples. Welch's t test was used to determine the significance of the difference in expression of the indicated mRNA species in the presence of IFN-γ alone versus expression with IFN-γ plus M. tuberculosis or 19-kDa lipoprotein. A single asterisk indicates a P value of <0.05, and two asterisks indicate a P value of <0.01. (B) Macrophages were analyzed for expression of CD86 (left panels) and CD80 (right panels) by flow cytometry. Shaded histograms denote isotype-matched negative control antibody labeling, thin lines indicate expression in the presence of the inhibitor indicated in the panel (none, 19-kDa lipoprotein, or M. tuberculosis), and thick lines indicate expression with both inhibitor and IFN-γ. The percent control expression (expression with IFN-γ alone) was calculated based on specific mean fluorescence values (MFVs), i.e., specific MFV = MFVspecific antibody − MFVisotype-matched control antibody) by using the following equation: (specific MFVInhibitor + IFN-γ/specific MFVIFN-γ) × 100. IFN-γ-induced expression of CD86 was reduced to 50 and 28% of control by M. tuberculosis and 19-kDa lipoprotein, respectively.
We studied protein expression by flow cytometry or mRNA expression by quantitative RT-PCR to extend the microarray analysis and further assess regulation of genes associated with Ag presentation, recruitment of T cells or other IFN-γ-induced functions. IFN-γ induction of the costimulatory molecule CD86 was inhibited by 19-kDa lipoprotein or infection with M. tuberculosis (microarray studies shown in Table 2). Flow cytometry (Fig. 3B) indicated that IFN-γ-dependent CD86 expression was inhibited to 50 and 28% of control levels by 19-kDa lipoprotein and M. tuberculosis, respectively. In contrast, expression of CD80 was not influenced by IFN-γ, M. tuberculosis or 19-kDa lipoprotein (by microarray analysis or flow cytometry). Expression of VCAM-1 was also inhibited by M. tuberculosis and 19-kDa lipoprotein (Table 2, Fig. 3A). VCAM-1 is a ligand for α4/β1, and α4/β7 integrins that are believed to function in homing of M. tuberculosis-specific CD4+ T cells to the lung in tuberculosis (9) and may facilitate Ag presentation. Expression of MIG was also decreased by M. tuberculosis and 19-kDa lipoprotein (Table 2, Fig. 3A). MIG recruits activated T cells by binding to the chemokine receptor, CXCR3. Quantitative RT-PCR also confirmed microarray expression results for GBP-1, TRAIL, and NKG2D (i.e., 19-kDa lipoprotein and M. tuberculosis decreased gene induction by IFN-γ; P < 0.05 [data not shown]). In summary, M. tuberculosis and 19-kDa lipoprotein decreased IFN-γ-induced expression of many genes. Decreased expression of genes involved in MHC-II Ag processing, Ag presentation, and T-cell recruitment may reduce the ability of infected macrophages to activate M. tuberculosis-specific CD4+ T cells.
Some IFN-γ-induced genes are not inhibited by M. tuberculosis and 19-kDa lipoprotein.
Although many IFN-γ-induced genes were inhibited by M. tuberculosis and 19-kDa lipoprotein, many genes potentially involved in controlling M. tuberculosis infection, e.g., NOS2, TGTP, LRG-47, GBP-2, and NRAMP-1, were expressed in the presence of both M. tuberculosis and IFN-γ. Relative to the baseline, expression of NOS2 was induced 10-fold by M. tuberculosis, was not induced by IFN-γ alone, and was induced 72-fold by the synergistic combination of M. tuberculosis and IFN-γ. M. tuberculosis 19-kDa lipoprotein was also synergistic with IFN-γ in the induction of NOS2. The expression of LRG-47, which has been implicated in control of M. tuberculosis infection (21), was not significantly altered by M. tuberculosis or 19-kDa lipoprotein. LRG-47 expression was induced 6.5-fold in response to IFN-γ compared to 5.3- or 5.0-fold in response to IFN-γ plus M. tuberculosis or 19-kDa lipoprotein, respectively. We conclude that M. tuberculosis and 19-kDa lipoprotein inhibit IFN-γ induction of many genes, including those involved in Ag-presenting-cell function, but do not decrease IFN-γ induction of other genes, including some that are involved in innate immunity and control of intracellular M. tuberculosis. Thus, M. tuberculosis and 19-kDa lipoprotein do not produce a global inhibition of IFN-γ-mediated regulation of gene expression; rather, they produce differential effects on different sets of IFN-γ-regulated genes.
Role of MyD88 in M. tuberculosis-mediated effects on macrophage gene transcription.
Inhibition of IFN-γ-induced MHC-II expression by 19-kDa lipoprotein was dependent on TLR2 (26) and MyD88 (28). MyD88 is an adaptor molecule involved in signaling by all known TLRs, although components of TLR4 and TLR3 signaling are MyD88 independent (17, 18). To determine the role of MyD88 in M. tuberculosis regulation of macrophage gene expression, MyD88−/− macrophages were infected with M. tuberculosis for 24 h and then incubated with or without IFN-γ for 15 h. Fully 87% of 373 M. tuberculosis-induced genes were dependent on MyD88 (i.e., had significantly less expression in MyD88−/− macrophages compared to wild-type macrophages; Table 3), and 77% of M. tuberculosis-induced genes were absolutely dependent on MyD88 (i.e., were not detectably induced in MyD88−/− macrophages). Similarly, of 462 genes suppressed by M. tuberculosis in wild-type macrophages, 82% were dependent on MyD88, and 70% were absolutely dependent on MyD88. Thus, regulation of macrophage gene expression by M. tuberculosis is largely dependent on MyD88, implying a major role for TLRs in the modulation of gene expression by M. tuberculosis. Our data are consistent with many observations that TLRs and MyD88 are involved in recognition of M. tuberculosis (2, 36, 37, 40, 41). A recent report by Shi et al. (30) provides a different perspective and indicates MyD88-independent regulation of many genes by M. tuberculosis. Nonetheless, there is agreement for some genes whose induction was determined by both our study and that of Shi et al. to be MyD88 dependent (e.g., MCP-5, MARCO, IL-1β, IL-6, FPR, and SAA-3) or MyD88 independent (e.g., RANTES, IP-10, MIG, Stat1, and LRG-47). Other genes showed regulation that was MyD88 dependent in our study but not that of Shi et al. (e.g., NOS2, KC, and IRG-1). The differences between the studies may reflect differences in culture conditions that are further explored in the Discussion.
TABLE 3.
Gene regulation by M. tuberculosis role of MyD88a
| Gene list | No. of genes regulated in wild-type cells | % of genes absolutely requiring MyD88b | % of genes dependent on MyD88c |
|---|---|---|---|
| Induced by M. tuberculosisd | 373 | 77 | 87 |
| Suppressed by M. tuberculosisd | 462 | 70 | 82 |
| IFN-γ-induced genes inhibited by M. tuberculosise | 146 | 64 | 80 |
| IFN-γ-suppressed genes rescued by M. tuberculosise | 106 | 61 | 75 |
MyD88−/− and wild-type macrophages were infected with M. tuberculosis or incubated in standard medium for 24 h and then incubated with IFN-γ for 15 h as described in Fig. 2.
Genes that were not detectably induced in MyD88−/− macrophages.
Genes for which induction was greater in wild-type macrophages than in MyD88−/− macrophages in at least five of nine comparisons with an absolute value of the mean fold change in all nine comparisons of >1.2 and a P value of < 0.05 by Welch's t test.
Next, we determined the role of MyD88 in the inhibition of IFN-γ-induced gene expression by M. tuberculosis. Of 146 IFN-γ-induced genes that were inhibited by M. tuberculosis in wild-type macrophages, fully 82% were dependent on MyD88 for the inhibitory regulation (i.e., were inhibited to a lesser degree in MyD88−/− macrophages, Table 2), and 64% had M. tuberculosis-mediated inhibition that was absolutely dependent on MyD88 (i.e., were not inhibited in MyD88−/− macrophages). In addition, the expression profiles of the 82 IFN-γ-induced genes that were inhibited by both M. tuberculosis and M. tuberculosis 19-kDa lipoprotein show that the ability of M. tuberculosis to inhibit many of these genes is clearly reversed in MyD88−/− macrophages (Fig. 2E). Genes for which M. tuberculosis-mediated inhibition was absolutely dependent on MyD88 included CIITA, MHC-II, CD86, MIG, VCAM-1, IIGP, and IGTP. Conversely, of 106 genes that were suppressed by IFN-γ but rescued by M. tuberculosis in control macrophages, 75% were rescued to a lesser degree in MyD88−/− macrophages, and rescue was absolutely dependent on MyD88 for 61%. In summary, the ability of M. tuberculosis to block IFN-γ-mediated regulation of gene expression was largely dependent on MyD88 and, by implication, signaling through TLRs.
DISCUSSION
IFN-γ is critically important in controlling M. tuberculosis infection, since defects in the IFN-γ signaling pathway in both mice and humans lead to severe mycobacterial infections (6, 7, 10, 15, 16). We propose that M. tuberculosis can inhibit IFN-γ-induced regulation of certain genes in chronically infected cells. To model the impact of prolonged TLR signaling in chronic infection with M. tuberculosis, macrophages were infected with M. tuberculosis or incubated with M. tuberculosis 19-kDa lipoprotein for 24 h prior to addition of IFN-γ. Our results demonstrate that M. tuberculosis and 19-kDa lipoprotein inhibit the ability of IFN-γ to regulate expression of many genes in macrophages, particularly those involved in MHC-II Ag processing, Ag presentation, and T-cell recruitment.
M. tuberculosis 19-kDa lipoprotein does not decrease expression of IFN-γ receptor or prevent IFN-γ-induced phosphorylation of Stat1 or translocation of Stat1 to the nucleus (28), suggesting that inhibition occurs at a distal site in the pathway for regulation of gene expression by IFN-γ, possibly involving chromatin remodeling. Induction of CIITA is dependent on changes in chromatin structure; remodeling of the CIITA locus occurs after stimulation with IFN-γ and is dependent on BRG-1, a member of the SWI/SNF chromatin-remodeling complex (29). Our finding that IFN-γ induction of a subset of genes is not inhibited by M. tuberculosis or 19-kDa lipoprotein is also consistent with unperturbed proximal IFN-γ signaling and distal control of sets of IFN-γ-responsive genes. In other words, blockade in IFN-γ regulation of gene expression occurs by a distal control mechanism that allows differential effects on different subsets of IFN-γ-regulated genes.
Microarray analysis of M. tuberculosis-infected MyD88−/− macrophages revealed that MyD88 is critical to the ability of M. tuberculosis and 19-kDa lipoprotein to regulate gene expression. A total of 87% of M. tuberculosis-induced genes had decreased induction in MyD88−/− macrophages, and 82% of M. tuberculosis-suppressed genes had decreased suppression in the absence of MyD88. Regulation of some genes, however, was only partially dependent on MyD88, whereas others were regulated independent of MyD88, suggesting the coexistence of MyD88-dependent and MyD88-independent signaling in response to M. tuberculosis. In contrast, Shi et al. reported that MyD88 was not required for the induction of many genes by M. tuberculosis, although they did find several MyD88-dependent genes, e.g., MCP-5, MARCO, IL-1b, IL-6, FPR, and SAA-3 (each of these was similarly found to be MyD88 dependent in our study). RANTES, IP-10, MIG, Stat1, and LRG-47 were found to be MyD88 independent in both studies, whereas regulation of some other genes was MyD88 dependent in our study but not that of Shi et al. (e.g., NOS2, KC, and IRG-1). Overall, there are differences as well as some overlap in the data from the two studies, and the differences likely reflect different cell culture conditions (discussed below). In summary, signaling in response to M. tuberculosis appears to include both MyD88-dependent and MyD88-independent mechanisms.
Shi et al. reported that MyD88 was required for full activation of macrophages by IFN-γ and proposed a mechanism involving macrophage preactivation via MyD88-dependent production of TNF-α that could prime macrophages to respond to IFN-γ (30). In contrast, we found that TLR/MyD88 signaling in macrophages decreased induction of many genes by IFN-γ. The difference may reflect dependence of macrophage preactivation on different culture conditions used for the experiments. For example, Shi et al. incubated macrophages for 48 h with IFN-γ in the continued presence of conditioned medium from L929 cells, whereas in our study macrophages were washed and removed from conditioned medium 24 h prior to addition of IFN-γ for 15 h. In our studies, MyD88−/− and wild-type macrophages exhibited no statistically significant difference in TNF-α expression in response to M. tuberculosis, suggesting that TNF-α-induced macrophage preactivation may not have been a factor in our system. In another study, Ehrt et al. reported that “M. tuberculosis mimicked and synergized with IFN-γ more than antagonized its actions” (8). For example, M. tuberculosis was reported to synergize with IFN-γ to induce MIG and MCP-5, whereas we observed that M. tuberculosis suppressed IFN-γ induction of these genes. Again, these variations may reflect differences in experimental design (similar to the study by Shi et al., macrophages were incubated first with IFN-γ and then with M. tuberculosis in the continued presence of L929 cell conditioned medium). On the other hand, results with some genes (e.g., KC, SLPI, and NOS2) were concordant between the studies. Moreover, the data of Ehrt et al. show that 33% of 615 IFN-γ-induced genes were not expressed in macrophages that were treated with IFN-γ and infected with M. tuberculosis (8); these data fit with our conclusion that M. tuberculosis inhibits IFN-γ-induced expression of certain genes in macrophages.
After exposure to 19-kDa lipoprotein or M. tuberculosis, some gene regulation may be dependent on cytokines (e.g., IL-6, IL-10, or transforming growth factor β [TGF-β]) or other signaling molecules that are produced upon microbial stimulation, but it is not clear how such indirect regulation contributes to the system we have studied. IL-6 has been proposed to inhibit IFN-γ-mediated induction of some genes (22), but other studies suggest that it may not be a physiological regulator of IFN-γ-mediated gene expression after exposure to M. tuberculosis or 19-kDa lipoprotein (11). IL-10 may be produced after microbial stimulation and is known to inhibit MHC-II but does so by posttranscriptional regulation (20), different from the mechanism observed in our studies. We showed that IL-10 and TGF-β were induced by M. tuberculosis or 19-kDa lipoprotein and that IL-6 expression was increased by both treatments. These studies do not, however, further dissect these mechanisms, and the contribution of cytokines to M. tuberculosis inhibition of IFN-γ-induced gene regulation requires further study.
M. tuberculosis 19-kDa lipoprotein is one of several PAMPs that inhibit MHC-II expression and Ag processing by macrophages after prolonged exposure (others include CpG DNA and lipopolysaccharide) (5, 26). Although the signaling pathways and mechanisms whereby M. tuberculosis inhibits IFN-γ-induced gene expression may be induced by PAMPs from other bacteria, M. tuberculosis and a subset of intracellular pathogens may be particularly successful in inducing and exploiting these responses. First, M. tuberculosis resides mainly inside macrophages, a cell type that expresses TLRs and exhibits IFN-γ-dependent modulation of many genes involved in host defense (including those involved in MHC-II Ag processing and presentation). Second, M. tuberculosis has mechanisms to resist acute innate microbicidal mechanisms, allowing it to persist inside macrophages for a sufficient period to provide chronic exposure to PAMPs. Third, the 19-kDa lipoprotein is shed from live, intracellular mycobacteria (24), making it available to stimulate TLR2 (4, 26, 33) in association with TLR1 (35), which are both recruited to phagosomal compartments (27). Intracellular persistence of M. tuberculosis and shedding of M. tuberculosis 19-kDa lipoprotein provide effective means for chronic stimulation of TLR2 and consequent inhibition of IFN-γ-induced gene modulation.
Inhibition of IFN-γ-induced responses through prolonged TLR signaling may seem discordant with the roles of TLRs in acute immune activation, but this inhibition may represent a counterregulatory mechanism to promote immune homeostasis. PAMP-induced TLR signaling acutely produces proinflammatory innate immune responses that contribute to host defense, but some aspects of these responses may be downregulated after the acute phase to limit damage to vital tissues. For many acute bacterial infections (e.g., with extracellular pathogens), necessary innate immune functions may be provided within the acute phase. M. tuberculosis, however, is able to survive the acute phase of innate immunity and persist inside macrophages. Prolonged TLR signaling may then reduce Ag-presenting function of infected macrophages, which would then serve as niches in which M. tuberculosis could persist without detection by CD4+ T cells. If even a small proportion of macrophages provided such niches, this would create an effective immune evasion mechanism to promote chronic infection even with continued Ag presentation by other cells. Since dendritic cells are not subject to this mechanism (TLR signaling promotes dendritic cell maturation and priming of T-cell responses), this model predicts the induction of CD4 T-cell responses but the persistence of M. tuberculosis within the protected niches provided by chronically infected macrophages, as observed in tuberculosis.
Acknowledgments
Advice and support for microarray analysis were provided by Patrick Leahy and the Microarray Core Facility of the Comprehensive Cancer Center of Case Western Reserve University and University Hospitals of Cleveland (P30 CA43703).
This work was supported by NIH grants AI35726, AI34343, and AI44794 to C.V.H., HL55967 and AI27243 to W.H.B., AI01581 to D.H.C., AI36219 to the Case Western Reserve University Center for AIDS Research, and contract AI95383 to the Tuberculosis Research Unit. D.H.C. was supported in part by a grant from the American Lung Association. R.K.P. and A.A.R.T. were supported in part by NIH training grants CA73515 and GM07250.
Editor: F. C. Fang
REFERENCES
- 1.Adachi, O., T. Kawai, K. Takeda, M. Matsumoto, H. Tsutsui, M. Sakagami, K. Nakanishi, and S. Akira. 1998. Targeted disruption of the MyD88 gene results in loss of IL-1- and IL-18-mediated function. Immunity 9:143-150. [DOI] [PubMed] [Google Scholar]
- 2.Bochud, P. Y., T. R. Hawn, and A. Aderem. 2003. Cutting edge: a Toll-like receptor 2 polymorphism that is associated with lepromatous leprosy is unable to mediate mycobacterial signaling. J. Immunol. 170:3451-3454. [DOI] [PubMed] [Google Scholar]
- 3.Boldrick, J. C., A. A. Alizadeh, M. Diehn, S. Dudoit, C. L. Liu, C. E. Belcher, D. Botstein, L. M. Staudt, P. O. Brown, and D. A. Relman. 2002. Stereotyped and specific gene expression programs in human innate immune responses to bacteria. Proc. Natl. Acad. Sci. USA 99:972-977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brightbill, H. D., D. H. Libraty, S. R. Krutzik, R. B. Yang, J. T. Belisle, J. R. Bleharski, M. Maitland, M. V. Norgard, S. E. Plevy, S. T. Smale, P. J. Brennan, B. R. Bloom, P. J. Godowski, and R. L. Modlin. 1999. Host defense mechanisms triggered by microbial lipoproteins through toll-like receptors. Science 285:732-736. [DOI] [PubMed] [Google Scholar]
- 5.Chu, R. S., D. Askew, E. H. Noss, A. Tobian, A. M. Krieg, and C. V. Harding. 1999. CpG oligodeoxynucleotides down-regulate macrophage class II MHC antigen processing. J. Immunol. 163:1188-1194. [PubMed] [Google Scholar]
- 6.Cooper, A. M., D. K. Dalton, T. A. Stewart, J. P. Griffin, D. G. Russell, and I. M. Orme. 1993. Disseminated tuberculosis in interferon gamma gene-disrupted mice. J. Exp. Med. 178:2243-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dupuis, S., C. Dargemont, C. Fieschi, N. Thomassin, S. Rosenzweig, J. Harris, S. M. Holland, R. D. Schreiber, and J. L. Casanova. 2001. Impairment of mycobacterial but not viral immunity by a germline human STAT1 mutation. Science 293:300-303. [DOI] [PubMed] [Google Scholar]
- 8.Ehrt, S. S. D., S. Bekiranov, J. Drenkow, S. Shi, T. R. Gingeras, T. Gaasterland, G. Schoolnik, and C. Nathan. 2001. Reprogramming of the macrophage transcriptome in response to interferon-gamma and Mycobacterium tuberculosis: signaling roles of nitric oxide synthase-2 and phagocyte oxidase. J. Exp. Med. 194:1123-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng, C. G., W. J. Britton, U. Palendira, N. L. Groat, H. Briscoe, and A. G. Bean. 2000. Up-regulation of VCAM-1 and differential expansion of beta integrin-expressing T lymphocytes are associated with immunity to pulmonary Mycobacterium tuberculosis infection. J. Immunol. 164:4853-4860. [DOI] [PubMed] [Google Scholar]
- 10.Flynn, J. L., J. Chan, K. J. Triebold, D. K. Dalton, T. A. Stewart, and B. R. Bloom. 1993. An essential role for interferon gamma in resistance to Mycobacterium tuberculosis infection. J. Exp. Med. 178:2249-2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortune, S. M., A. Solache, A. Jaeger, P. J. Hill, J. T. Belisle, B. R. Bloom, E. J. Rubin, and J. D. Ernst. 2004. Mycobacterium tuberculosis inhibits macrophage responses to IFN-gamma through myeloid differentiation factor 88-dependent and -independent mechanisms. J. Immunol. 172:6272-6280. [DOI] [PubMed] [Google Scholar]
- 12.Gehring, A. J., R. E. Rojas, D. H. Canaday, D. L. Lakey, C. V. Harding, and W. H. Boom. 2003. The Mycobacterium tuberculosis 19-kilodalton lipoprotein inhibits gamma interferon-regulated HLA-DR and Fc gamma R1 on human macrophages through Toll-like receptor 2. Infect. Immun. 71:4487-4497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Havlir, D. V., R. S. Wallis, W. H. Boom, T. M. Daniel, K. Chervenak, and J. J. Ellner. 1991. Human immune responses to Mycobacterium tuberculosis antigens. Infect. Immun. 59:665-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang, Q., D. Liu, P. Majewski, A. C. Schultele, J. M. Korn, R. A. Young, E. S. Lander, and N. Hacohen. 2001. The plasticity of dendritic cell responses to pathogens and their components. Science 294:870-875. [DOI] [PubMed] [Google Scholar]
- 15.Huang, S., W. Hendriks, A. Althage, S. Hemmi, H. Bluethmann, R. Kamijo, J. Vilcek, R. M. Zinkernagel, and M. Aguet. 1993. Immune response in mice that lack the interferon-gamma receptor. Science 259:1742-1745. [DOI] [PubMed] [Google Scholar]
- 16.Jouanguy, E., S. Lamhamedi-Cherradi, D. Lammas, S. E. Dorman, M. C. Fondaneche, S. Dupuis, R. Doffinger, F. Altare, J. Girdlestone, J. F. Emile, H. Ducoulombier, D. Edgar, J. Clarke, V. A. Oxelius, M. Brai, V. Novelli, K. Heyne, A. Fischer, S. M. Holland, D. S. Kumararatne, R. D. Schreiber, and J. L. Casanova. 1999. A human IFNGR1 small deletion hotspot associated with dominant susceptibility to mycobacterial infection. Nat. Genet. 21:370-378. [DOI] [PubMed] [Google Scholar]
- 17.Kaisho, T., and S. Akira. 2001. Dendritic-cell function in Toll-like receptor- and MyD88-knockout mice. Trends Immunol. 22:78-83. [DOI] [PubMed] [Google Scholar]
- 18.Kawai, T., O. Adachi, T. Ogawa, K. Takeda, and S. Akira. 1999. Unresponsiveness of MyD88-deficient mice to endotoxin. Immunity 11:115-122. [DOI] [PubMed] [Google Scholar]
- 19.Kincaid, E. Z., and J. D. Ernst. 2003. Mycobacterium tuberculosis exerts gene-selective inhibition of transcriptional responses to IFN-gamma without inhibiting STAT1 function. J. Immunol. 171:2042-2049. [DOI] [PubMed] [Google Scholar]
- 20.Koppelman, B., J. J. Neefjes, J. E. de Vries, and R. de Waal Malefyt. 1997. Interleukin-10 down-regulates MHC class II alphabeta peptide complexes at the plasma membrane of monocytes by affecting arrival and recycling. Immunity 7:861-871. [DOI] [PubMed] [Google Scholar]
- 21.MacMicking, J. D., G. A. Taylor, and J. D. McKinney. 2003. Immune control of tuberculosis by IFN-gamma-inducible LRG-47. Science 302:654-659. [DOI] [PubMed] [Google Scholar]
- 22.Nagabhushanam, V., A. Solache, L. M. Ting, C. J. Escaron, J. Y. Zhang, and J. D. Ernst. 2003. Innate inhibition of adaptive immunity: Mycobacterium tuberculosis-induced IL-6 inhibits macrophage responses to IFN-gamma. J. Immunol. 171:4750-4757. [DOI] [PubMed] [Google Scholar]
- 23.Nathan, C. F., H. W. Murray, M. E. Wiebe, and B. Y. Rubin. 1983. Identification of interferon-gamma as the lymphokine that activates human macrophage oxidative metabolism and antimicrobial activity. J. Exp. Med. 158:670-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neyrolles, O., K. Gould, M. P. Gares, S. Brett, R. Janssen, P. O'Gaora, J. L. Herrmann, M. C. Prevost, E. Perret, J. E. Thole, and D. Young. 2001. Lipoprotein access to MHC class I presentation during infection of murine macrophages with live mycobacteria. J. Immunol. 166:447-457. [DOI] [PubMed] [Google Scholar]
- 25.Noss, E. H., C. V. Harding, and W. H. Boom. 2000. Mycobacterium tuberculosis inhibits MHC class II antigen processing in murine bone marrow macrophages. Cell. Immunol. 201:63-74. [DOI] [PubMed] [Google Scholar]
- 26.Noss, E. H., R. K. Pai, T. J. Sellati, J. D. Radolf, J. Belisle, D. T. Golenbock, W. H. Boom, and C. V. Harding. 2001. Toll-like receptor 2-dependent inhibition of macrophage class II MHC expression and antigen processing by 19 kD lipoprotein of Mycobacterium tuberculosis. J. Immunol. 167:910-918. [DOI] [PubMed] [Google Scholar]
- 27.Ozinsky, A., D. M. Underhill, J. D. Fontenot, A. M. Hajjar, K. D. Smith, C. B. Wilson, L. Schroeder, and A. Aderem. 2000. The repertoire for pattern recognition of pathogens by the innate immune system is defined by cooperation between toll-like receptors. Proc. Natl. Acad. Sci. USA 97:13766-13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pai, R. K., M. Convery, T. A. Hamilton, W. H. Boom, and C. V. Harding. 2003. Inhibition of IFN-gamma-induced class II transactivator expression by a 19-kDa lipoprotein from Mycobacterium tuberculosis: a potential mechanism for immune evasion. J. Immunol. 171:175-184. [DOI] [PubMed] [Google Scholar]
- 29.Pattenden, S. G., R. Klose, E. Karaskov, and R. Bremner. 2002. Interferon-gamma-induced chromatin remodeling at the CIITA locus is BRG1 dependent. EMBO J. 21:1978-1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi, S., C. Nathan, D. Schnappinger, J. Drenkow, M. Fuortes, E. Block, A. Ding, T. R. Gingeras, G. Schoolnik, S. Akira, K. Takeda, and S. Ehrt. 2003. MyD88 primes macrophages for full-scale activation by interferon-γ yet mediates few responses to Mycobacterium tuberculosis. J. Exp. Med. 198:987-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shtrichman, R., and C. E. Samuel. 2001. The role of gamma interferon in antimicrobial immunity. Curr. Opin. Microbiol. 4:251-259. [DOI] [PubMed] [Google Scholar]
- 32.Sklar, M. D., A. Tereba, B. D. Chen, and W. S. Walker. 1985. Transformation of mouse bone marrow cells by transfection with a human oncogene related to c-myc is associated with the endogenous production of macrophage colony stimulating factor 1. J. Cell Physiol. 125:403-412. [DOI] [PubMed] [Google Scholar]
- 33.Stenger, S., and R. L. Modlin. 2002. Control of Mycobacterium tuberculosis through mammalian Toll-like receptors. Curr. Opin. Immunol. 14:452-457. [DOI] [PubMed] [Google Scholar]
- 34.Takeuchi, O., K. Hoshino, T. Kawai, H. Sanjo, H. Takada, T. Ogawa, K. Takeda, and S. Akira. 1999. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity 11:443-451. [DOI] [PubMed] [Google Scholar]
- 35.Takeuchi, O., S. Sato, T. Horiuchi, K. Hoshino, K. Takeda, Z. Dong, R. L. Modlin, and S. Akira. 2002. Cutting edge: role of toll-like receptor 1 in mediating immune response to microbial lipoproteins. J. Immunol. 169:10-14. [DOI] [PubMed] [Google Scholar]
- 36.Takeuchi, O., K. Takeda, K. Hoshino, O. Adachi, T. Ogawa, and S. Akira. 2000. Cellular responses to bacterial cell wall components are mediated through MyD88-dependent signaling cascades. Int. Immunol. 12:113-117. [DOI] [PubMed] [Google Scholar]
- 37.Thoma-Uszynski, S., S. Stenger, O. Takeuchi, M. T. Ochoa, M. Engele, P. A. Sieling, P. F. Barnes, M. Rollinghoff, P. L. Bolcskei, M. Wagner, S. Akira, M. V. Norgard, J. T. Belisle, P. J. Godowski, B. R. Bloom, and R. L. Modlin. 2001. Induction of direct antimicrobial activity through mammalian toll-like receptors. Science 291:1544-1547. [DOI] [PubMed] [Google Scholar]
- 38.Ting, L. M., A. C. Kim, A. Cattamanchi, and J. D. Ernst. 1999. Mycobacterium tuberculosis inhibits IFN-gamma transcriptional responses without inhibiting activation of STAT1. J. Immunol. 163:3898-3906. [PubMed] [Google Scholar]
- 39.Tobian, A. A., N. S. Potter, L. Ramachandra, R. K. Pai, M. Convery, W. H. Boom, and C. V. Harding. 2003. Alternate class I MHC antigen processing is inhibited by Toll-like receptor signaling pathogen-associated molecular patterns: Mycobacterium tuberculosis 19-kDa lipoprotein, CpG DNA, and lipopolysaccharide. J. Immunol. 171:1413-1422. [DOI] [PubMed] [Google Scholar]
- 40.Uehori, J., M. Matsumoto, S. Tsuji, T. Akazawa, O. Takeuchi, S. Akira, T. Kawata, I. Azuma, K. Toyoshima, and T. Seya. 2003. Simultaneous blocking of human Toll-like receptors 2 and 4 suppresses myeloid dendritic cell activation induced by Mycobacterium bovis bacillus Calmette-Guerin peptidoglycan. Infect. Immun. 71:4238-4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Underhill, D. M., A. Ozinsky, K. D. Smith, and A. Aderem. 1999. Toll-like receptor-2 mediates mycobacteria-induced proinflammatory signaling in macrophages. Proc. Natl. Acad. Sci. USA 96:14459-14463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xie, Q. W., H. J. Cho, J. Calaycay, R. A. Mumford, K. M. Swiderek, T. D. Lee, A. Ding, T. Troso, and C. Nathan. 1992. Cloning and characterization of inducible nitric oxide synthase from mouse macrophages. Science 256:225-228. [DOI] [PubMed] [Google Scholar]