Abstract
Bacillus anthracis, the etiological agent of anthrax, is a gram-positive, spore-forming bacterium. The inhalational form of anthrax is the most severe and is associated with rapid progression of the disease and the outcome is frequently fatal. Transfer from the respiratory epithelium to regional lymph nodes appears to be an essential early step in the establishment of infection. This transfer is believed to occur by means of carriage within alveolar macrophages following phagocytosis. Therefore, the ability of B. anthracis to transit through the host macrophage or dendritic cell appears to be an early and critical step in B. anthracis pathogenesis. In this work, we examined the cytokine responses to spore infection in mouse primary peritoneal macrophages, in primary human dendritic cells, and during a spore aerosol infection model utilizing the susceptible A/J mouse strain. We demonstrated that both mouse peritoneal macrophages and human dendritic cells exhibited significant intracellular bactericidal activity during the first hours following uptake, providing the necessary time to mount a cytokine response prior to cell lysis. Strong tumor necrosis factor (TNF-α) and interleukin-6 (IL-6) responses were seen in mouse peritoneal macrophages. In addition to TNF-α and IL-6, human dendritic cells produced the cytokines IL-1β, IL-8, and IL-12. A mixture of Th1 and Th2 cytokines were detected in sera obtained from infected animals. In this study, we provide further evidence of an acute cytokine response when cells in culture and mice are infected with B. anthracis spores.
Bacillus anthracis, the etiological agent of anthrax, is a gram-positive, aerobic, spore-forming, rod-shaped bacterium (20). Dormant spores are highly resistant to adverse environmental conditions and are able to reestablish vegetative growth in the presence of favorable environmental conditions (23). Fully virulent strains of B. anthracis carry two large plasmids, pXO1 and pXO2, that carry the genes encoding anthrax toxin production and capsule formation, respectively. The roles of these factors in pathogenesis have been extensively studied (for review, see references 8, 21, and 25). Infection can occur through the skin, by way of the gastrointestinal tract, or through the respiratory epithelium after inhalation of airborne spores, resulting in cutaneous, gastrointestinal, and inhalational anthrax, respectively (9, 19, 22, 33). The inhalation form of anthrax is the most severe, often associated with rapid progression of the disease and death (2, 10, 37).
Upon inhalation, anthrax spores reach the bronchioles and alveoli of the lung, where phagocytosis by alveolar macrophages occurs (5, 11, 13, 30, 32). It is believed that, following intracellular uptake, alveolar macrophages transport B. anthracis spores to the regional lymph nodes. Spores germinate and multiply within the macrophages, eventually resulting in lysis of the macrophage (5, 11-13, 16). Vegetative cells multiply within the mediastinal lymph node and gain entry into the bloodstream, resulting in the development of severe bacteremia (23, 30). This leads to vascular injury with edema, hemorrhage, and thrombosis, ultimately resulting in the death of the host (3).
Experimentally, germination of B. anthracis spores has been observed in the phagolysosome of alveolar macrophages. However, there have been contradictory reports regarding the intracellular survival and multiplication of B. anthracis and the role that the toxins play in the lysis of macrophages (5, 11, 36). From our own studies, it appears that the ability of B. anthracis to survive within macrophages does not require the pXO1 plasmid, while macrophage lysis following intracellular infection is dependent on a factor encoded on this virulence plasmid (27). Purified lethal toxin (LeTx) is known to lyse macrophages in vitro. However, Dixon and colleagues provided evidence that the transactivator, atxA, may be the only pXO1-encoded element necessary for this process to occur (5).
Hanna et al. demonstrated that the macrophage is essential for LeTx to cause toxicity in vivo (14). When mice were depleted of macrophages by silica treatment, they became insensitive to LeTx. At a cellular level, Hanna and colleagues showed that sublytic levels of LeTx triggered the production of tumor necrosis factor alpha (TNF-α) and interleukin-1β (IL-1β) by the macrophage cell line RAW 264.7 and that anti-IL-1 antibody or an IL-1 antagonist protected mice from toxin lethality. Subsequent publications have described studies that have contradicted this finding, reporting that purified LeTx inhibits cytokine responses to lipopolysaccharide (LPS) and postulating that this activity may play a role in the early stages of infection by dampening the immune response and permitting early replication (1, 4, 6, 18, 24, 26). We recently demonstrated that the mouse macrophage cell line J774A.1 produced IL-12 and TNF-α following intracellular infection with B. anthracis spores and that the LPS-induced cytokine response of these infected cells was not inhibited. In the study that we present here, we describe further evidence of the positive stimulation of the cytokine response by B. anthracis spore infection. We examined the cytokine responses to infection of mouse primary peritoneal macrophages and primary human dendritic cells with B. anthracis spores and evaluated the serum cytokine levels in the susceptible A/J mouse strain following inhalation of aerosolized spores of B. anthracis strain 7702.
MATERIALS AND METHODS
Generation and purification of B. anthracis spores.
Spores were prepared from B. anthracis strain 7702 (pXO1+ pXO2−) by the method described by Finlay et al. (7). Briefly, nutrient agar (NA) plates were inoculated with overnight cultures, and were incubated overnight at 30°C. Colonies from the NA plates were used to inoculate 2 ml of nutrient broth (NB) cultures, which were grown overnight at 30°C with shaking. An aliquot of the culture was spread onto NA plates containing 5-μg/ml MnSO4. These plates were incubated overnight at 30°C followed by incubation at room temperature (∼22°C) for 48 h in the dark. Colonies scraped from the surface of the agar were suspended in distilled water (dH2O) and were heat treated at 65°C for 30 min to kill any viable vegetative cells. The spores were washed once with distilled water and stored at 4°C. These preparations were stained with modified Ziehl-Neelsen stain and examined microscopically to evaluate the presence and purity of spores. Purification of spores was performed with 58% (vol/vol) Renografin (Renocal-76 diluted in dH2O; Bracco Diagnostics, Princeton, N.J.), prior to use. Spores were layered on the 58% Renografin and were spun at 4,000 × g for 30 min in a swinging bucket rotor. The spore pellet was washed twice with dH2O (6,000 × g for 30 min), and the spores were resuspended in dH2O. The final concentration of the stock spore solutions was adjusted to ∼5 × 109 spores/ml.
Isolation and infection of mouse primary peritoneal macrophages.
Peritoneal macrophages were harvested from BALB/c mice by lavage using ice-cold complete Dulbecco's modified Eagle medium (DMEM). Approximately 45 mice yielded enough cells for 60 wells at a density of 106 cells/ml following the attachment and washing steps described below. Following harvest, cells were spun down and resuspended in fresh complete DMEM. A 1-ml volume of resuspended cells was seeded into each well of a 24-well plate. The cells were incubated in the wells for 2 h to facilitate cell attachment prior to washing the cells once with complete DMEM. The cells were infected with 100 μl of 107 spores/ml to achieve a final concentration of 106 spores/ml (multiplicity of infection [MOI] = 1:1). Infection was allowed to proceed for 30 min at 37°C, at which point, gentamicin was added (to a final concentration of 10 μg/ml), and incubation was continued for an additional 30 min. A 10-min pulse with 10-μg/ml gentamicin resulted in 100% killing of B. anthracis in this tissue culture medium. After removal of the medium, cells were washed once with fresh medium and fresh medium without antibiotics was then added back. Counts of intracellular and extracellular CFU were made at 0, 2.5, 5, and 7.5 h following infection. For intracellular measurements, cells were washed once with phosphate-buffered saline (PBS) and then lysed by incubation in 0.05% deoxycholate solution for 10 min at 37°C.
Preparation and infection of human monocyte-derived dendritic cells.
Mononuclear cells were obtained by apheresis of normal volunteer donors as performed by the Blood Services Section in the Department of Transfusion Medicine at the National Institutes of Health Warren G. Magnuson Clinical Center (Bethesda, Md.). The mononuclear cells were further enriched for monocytes by centrifugal elutriation as performed by the Cell Processing Section in the Department of Transfusion Medicine. The elutriated monocytes were then cultured (106 cells/well) in six-well tissue-culture plates with 3-ml/well RPMI 1640 medium (Mediatech, Inc., Herndon, Va.) containing 10% fetal calf serum (FCS; Invitrogen, Inc., Grand Island, N.Y.), 800-U/ml granulocyte-macrophage colony-stimulating factor (GM-CSF) (Peprotech, Rocky Hill, N.J.), and 500-U/ml IL-4 (Peprotech). The nonadherent and loosely adherent cells were harvested after incubation of the plates for 5 days at 37°C in 5% CO2. The cells were centrifuged at 1,200 rpm in a Beckman GS-6KR centrifuge for 10 min and then plated (106/ml; 1 ml/well) in fresh RPMI containing 10% FCS and 800-U/ml GM-CSF in three replicate wells of each 24-well plate. This resulted in the generation of immature dendritic cells that were positive for CD11c but negative for CD14. The dendritic cells were infected with 100 μl of 107 spores/ml to achieve a final concentration of 106 spores per ml (MOI = 1:1). Infection was allowed to proceed for 30 min before addition of gentamicin (10 μg/ml). Following 30 min of incubation in the presence of gentamicin, the medium was removed, cells were washed once with fresh medium, and fresh medium without antibiotics was then added back. Counts of intracellular and extracellular CFU were made at 0, 2.5, 5, and 7.5 h following infection. For intracellular measurements, cells were washed once with PBS and lysed by incubation in 0.05% deoxycholate solution for 10 min at 37°C.
Spore aerosol challenge of A/J mice.
Female A/J mice (18 to 21 g) were exposed to aerosolized spores prepared from B. anthracis strain 7702 (5 × 109 spores/ml in dH2O) for 60 min. The spore aerosol was generated with a six-jet Collison nebulizer equipped with a precious fluids jar containing an inoculum of 10 ml (BGI, Inc., Waltham, Mass.). The mice were exposed using a nose-only exposure system (CH Technologies, Westwood, N.J.). Prior to exposure, mice were supplied with fresh air for 10 min to allow respiratory rates to normalize. One hour following exposure, four mice were euthanized via lethal injection of avertin and their lungs were homogenized and plated to determine the number of organisms that were retained (average retained dose). Ten mice were monitored for survival. At various time points following exposure, mice were sacrificed, and lungs, spleens, and sera were collected. Lungs and spleens were homogenized with a Stomacher (Seward, Inc., Thetford, Norfolk, United Kingdom) and were plated for CFU on brain heart infusion agar. The limit of detection of B. anthracis in the lung and spleen was 250 CFU for each organ. Blood samples were collected from the aorta following lethal injection with avertin. Blood was allowed to clot at room temperature for approximately 10 min before being placed at 4°C. Clotted blood was centrifuged at 5,000 rpm for 5 min, and the collected serum was stored at −70°C.
LPS treatment of anthrax-infected and control A/J mice.
Mice were injected with 200 μg of LPS from Escherichia coli serotype O111:B4 (Fluka, Buchs, Switzerland) dissolved in PBS. At 1, 3, and 5 h postinjection, mice were sacrificed by lethal intraperitoneal (i.p.) injection of avertin. Blood samples were collected by dissection and cutting of the aorta. The blood was allowed to clot at room temperature for approximately 10 min before being placed at 4°C. Clotted blood was centrifuged at 5,000 rpm for 5 min, and the serum was collected and stored at −70°C.
Measurement of cytokine concentrations in cell culture supernatants and mouse serum samples.
Cytokine concentrations in cell culture supernatants and mouse sera were measured with a mouse or human cytokine 10-plex antibody bead kit (Biosource International, Camarillo, Calif.) and a Luminex 100 analyzer (Luminex Corporation, Austin, Tex.) according to the manufacturer's instructions. For all measurements, supernatants and serum samples were frozen and stored at −70°C and were thawed immediately prior to assay. The limits of detection for each cytokine in this assay are as follows: IL-1β = 10 pg/ml, IL-2 = 20 pg/ml, IL-4 = 5 pg/ml, IL-5 = 10 pg/ml, IL-6 = 10 pg/ml, IL-10 = 15 pg/ml, IL-12 = 15 pg/ml, GM-CSF = 10 pg/ml, gamma interferon (IFN-γ) = 1 pg/ml, and TNF-α = 5 pg/ml.
RESULTS
Cytokine response of B. anthracis-infected primary mouse peritoneal macrophages.
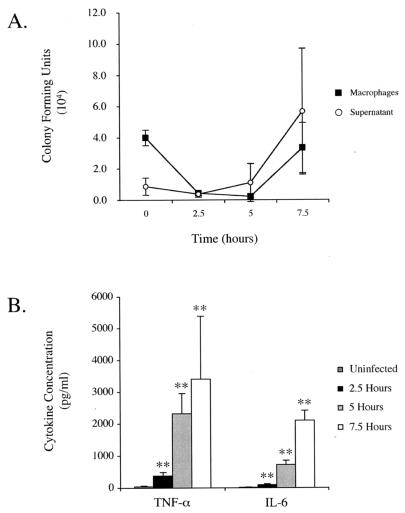
We reported previously that the mouse macrophage cell line J774A.1 produces IL-12 and TNF-α following intracellular infection with B. anthracis spores (27). We sought to determine if primary mouse macrophages behaved similarly. Primary peritoneal macrophages were harvested from BALB/c mice and infected with B. anthracis spores at an MOI of 1:1 as described in Materials and Methods. The numbers of CFU inside macrophages and in culture supernatants were determined at various time points postinfection (Fig. 1A). We observed significant bactericidal killing between the 0- and 2.5-h time points in all experiments. This typically resulted in an approximately 10-fold decrease in the number of CFU present inside the macrophages. The number of intracellular bacteria subsequently increased between the 5- and 7.5-h time points.
FIG. 1.
B. anthracis spore infection of mouse primary peritoneal macrophages. Macrophages were infected with B. anthracis spores prepared from B. anthracis strain 7702 as described in the text. (A) CFU inside the macrophages and in the supernatants were determined and are shown as a function of time postinfection. (B) The concentrations of 10 cytokines in the supernatants, collected from uninfected wells and infected wells at the indicated time points, were determined, and the results for TNF-α and IL-6 at 2.5, 5, and 7.5 h following infection are graphed. Three experiments were performed, and the results of a representative experiment are shown. Each value reported is the average of three samples. Error bars represent 1 standard deviation. Statistical significance was determined by Student's t test analysis. In all cases, means were compared to those of the uninfected control group. **, P < 0.01.
We examined the concentration of 10 cytokines in the supernatants from B. anthracis-infected primary peritoneal macrophages at 2.5, 5, and 7.5 h postinfection. The 10 cytokines assayed were IL-1β, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12 (p70), GM-CSF, IFN-γ, and TNF-α. High levels of IL-6 and TNF-α were observed at 5 and 7.5 h postinfection in all experiments (Fig. 1B). While we did observe small amounts of IL-12 release in some cultures following intracellular infection (results not shown), this was not a consistent observation in all experiments. No other cytokines were present at levels significantly higher than the limit of quantitation of the method (data not shown).
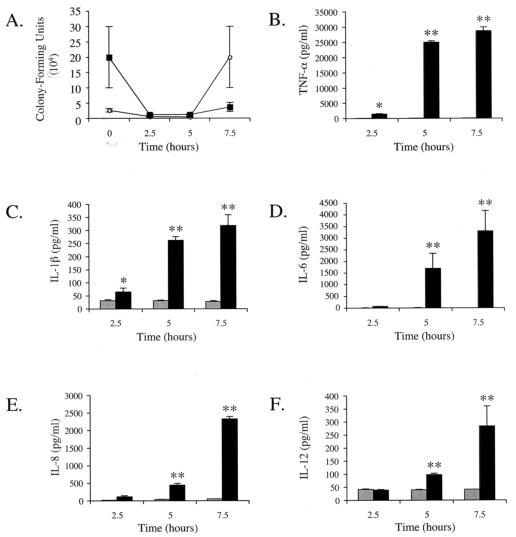
Cytokine response of B. anthracis-infected primary human dendritic cells.
Primary human dendritic cells were derived from human monocytes and infected with B. anthracis strain 7702 spores at an MOI of 1:1 as described in Materials and Methods. The number of intracellular and extracellular CFU was determined at 2.5, 5, and 7.5 h postinfection (Fig. 2A). As was seen with the mouse primary peritoneal macrophages, there was significant bactericidal activity observed between the 0- and 2.5-h time points in all experiments. Typically, there was a 10-fold decrease in the number of CFU present inside the dendritic cells. An increase in the number of CFU was seen in the 7.5-h samples. We examined the concentration of cytokines in the supernatants from B. anthracis-infected human dendritic cell cultures at 2.5, 5, and 7.5 h postinfection (Fig. 2B to F). High levels of TNF-α and IL-6 were evident in dendritic cell supernatants by 5 h following intracellular infection. Lower, but consistently detectable, responses for IL-1β and IL-12 were also observed. The level of IL-8, increased dramatically at the 7.5-h time point. The levels of IL-4, IL-5, IL-10, GM-CSF, and IFN-γ, were not significantly higher in supernatants from the B. anthracis-infected human dendritic cells relative to the uninfected cells at any time point (data not shown).
FIG. 2.
B. anthracis spore infection of primary human dendritic cells. Human dendritic cells were infected with B. anthracis spores prepared from B. anthracis strain 7702 as described in the text. (A) CFU inside the dendritic cells (closed squares) and in the supernatants (open circles) were determined and are shown as a function of time postinfection. (B to F) The concentrations of 10 cytokines in the supernatants collected from uninfected wells (gray bars) and infected wells (black bars) at the indicated time points are shown for TNF-α, IL-6, IL-1β, IL-8, and IL-12. Three experiments were performed, and the results of a representative experiment are shown. Each value reported is the average of three samples. Error bars represent 1 standard deviation. Statistical significance was determined by Student's t test analysis. For each cytokine, at each time point, means were compared to those of the uninfected control group. *, P < 0.05; **, P < 0.01.
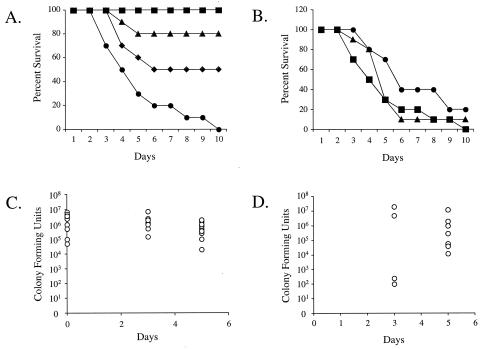
Spore aerosol challenge of A/J mice.
In order to examine the systemic host cytokine responses to aerosol exposure with B. anthracis spores, an inhalation model of anthrax using the susceptible A/J mouse strain was developed. In this model, A/J mice were exposed to aerosols containing high concentrations of spores derived from the pXO1+ pXO2− B. anthracis strain 7702. Retained spore doses of ∼103 resulted in no mortality in challenged mice, while retained doses of ∼105 caused 20 to 50% mortality, and retained doses of greater than 106 resulted in 80 to 100% killing (Fig. 3A and B). For animals that retained the highest dose, a majority of deaths observed occurred between days 3 and 6 (Fig. 3B). The mean time to death was 5 ± 2 days. No deaths were observed later than day 10. When mice were challenged with doses that resulted in a mean retained dose of approximately 2.9 × 106, high numbers of CFU were found in the lungs on days 0, 3, and 5 postinfection (Fig. 3C). A subset of these samples were examined for heat sensitivity and were found to be highly resistant, indicating that they were predominantly still in the dormant spore form (results not shown). CFU counts in the spleens of aerosol-infected mice were used as an indicator of systemic dissemination. For challenges that resulted in 80 to 100% mortality, none of the animals had detectable spleen colonization on day 0, 50% of the animals had detectable spleen colonization by the day 3, and this increased to 90% by day 5 following aerosol challenge (Fig. 3D). The CFU within spleens were tested for heat sensitivity in a small number of samples, and 100% of cells were found to be vegetative.
FIG. 3.
Mouse aerosol challenge model. Mice were exposed to aerosols of spores prepared from B. anthracis strain 7702 as described in the text. (A) The survival of groups of mice challenged with 2 × 103 (squares), 3 × 105 (triangles), 8 × 105 (diamonds), and 4 × 106 (circles) spores is shown as a function of time postchallenge. (B) The survival of groups of mice challenged with between 1 × 106 and 4 × 106 spores from three sequential experiments is shown: 1 × 106 (triangles), 3 × 106 (circles), and 4 × 106 (squares). Subsets of animals from the challenges presented in panel B were sacrificed on days 0, 3, and 5 postchallenge. The number of CFU present in the lungs (C) and in the spleens (D) is presented. The lower limit of detection of B. anthracis in spleen or lung was 250 CFU in each case. For panel D, values represent only positive spleen cultures as described in the Results section.
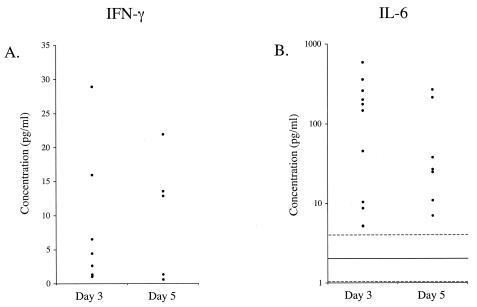
Serum cytokine response to spore aerosol infection in A/J mice.
We evaluated the systemic cytokine response in the A/J mice from the three challenges presented in Fig. 3B. The concentrations of the cytokines IL-1β, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12 (p70), GM-CSF, IFN-γ, and TNF-α in the serum of challenged mice were measured on days 3 and 5 postinfection. Serum samples from unchallenged A/J mice were also obtained as controls. Increased levels of IL-6 and IFN-γ were observed in several mice; however, the values for these three cytokines varied widely, ranging from no increase to greater than a 10-fold increase over the levels seen in serum from uninfected animals (Fig. 4). There was no correlation between the number of CFU in the spleens of challenged mice and the level of IL-6 or IFN-γ in the serum (data not shown). There appeared to be a correlation between the presence, but not the magnitude, of the IL-6 and IFN-γ responses. Eighteen of the 19 mice that had levels of IL-6 above that seen in uninfected mice also had IFN-γ levels above that seen in uninfected mice; however, no correlation was observed in the levels of the two cytokines observed (data not shown). No increase in cytokine concentration, relative to the levels seen in normal serum, was observed for IL-1β, IL-4, IL-5, IL-8, IL-10, GM-CSF, or TNF-α in the serum from any of the mice sacrificed on day 3 or day 5. Because the TNF-α response in animals is an early and transient event, we performed two additional challenges of A/J mice as described above and examined the serum cytokine response at 1, 3, 5, and 24 h postinfection. We did not detect a significant response for any of the 10 measured cytokines at those time points (data not shown).
FIG. 4.
Levels of serum cytokines in B. anthracis-infected mice. A subset of mice from the three challenges presented in Fig. 3B were examined for their serum cytokine response to the infection. On days 3 and 5 postchallenge, mice were sacrificed and sera were collected. The concentration of 10 cytokines in serum from each mouse was determined. (A) The results for IFN-γ are presented. Each data point represents a single mouse. The level of IFN-γ in the sera of uninfected mice (n = 6) was below the level of detection (1 pg/ml). (B) The results for IL-6 are presented. Each data point represents a single mouse. The solid line indicates the mean of the concentration of IL-6 in the sera of uninfected mice (n = 6). The dashed lines indicate 1 standard deviation above and below the mean.
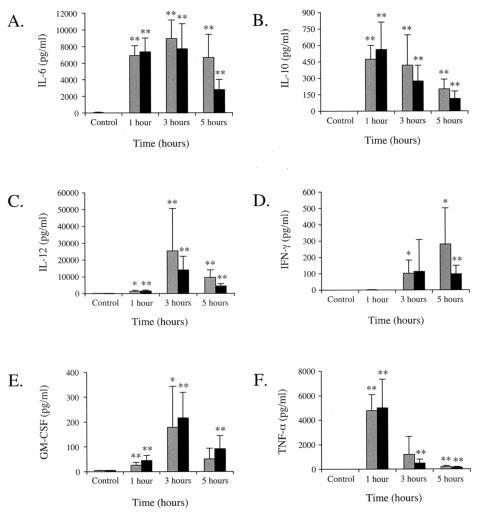
Effect of B. anthracis infection on systemic cytokine response to LPS.
In several recent publications, it has been reported that treatment of macrophages or dendritic cells with purified LeTx results in inhibition of LPS-induced cytokine responses (1, 6, 18, 24, 26). We have shown previously that infection of the mouse macrophage cell line J774A.1 with spores derived from B. anthracis strain 7702 does not result in an inhibition of the cytokine response to LPS (27). We sought to determine if B. anthracis infection results in an inhibition of the cytokine response in the mouse aerosol challenge model. Mice were challenged with a dose of 2 × 106 spores (retained dose in the lungs). Three days following the challenge, groups of challenged and unchallenged mice were injected with LPS as described in Materials and Methods. Serum samples were collected at 1, 3, and 5 h postinjection, and the concentrations of the cytokines IL-1β, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12 (p70), GM-CSF, IFN-γ, and TNF-α were determined (Fig. 5). LPS treatment alone resulted in high levels of expression of TNF-α, IL-6, and IL-12 and significant levels of expression of IL-10, IFN-γ, and GM-CSF. For those cytokines induced by LPS treatment, there was no statistically significant difference between B. anthracis-infected animals and uninfected animals at any time point, indicating that no inhibitory effect on the cytokine response was observed in B. anthracis-infected mice.
FIG. 5.
LPS-induced cytokines in uninfected and B. anthracis-infected mice. Mice were exposed by aerosol exposure to 2 × 106 spores prepared from B. anthracis strain 7702 as described in the text. Uninfected (gray bars) or B. anthracis-infected (black bars) mice were treated with LPS, and sera were collected at 1, 3, and 5 h post-LPS injection. In each panel, the control groups consisted of infected and uninfected mice that were not treated with LPS. The concentration of 10 cytokines in each serum sample was determined, and the concentrations of the 6 cytokines present at levels above the level of quantitation of the assay are shown. Three experiments were performed, and the results of a representative experiment are shown. Error bars represent 1 standard deviation. Statistical significance was determined by Student's t test analysis. For each cytokine, at each time point, the mean of the uninfected, LPS-treated group was compared to that of the uninfected, untreated control group and the mean of the infected, LPS-treated group was compared to that of the infected, untreated control group. *, P < 0.05; **, P < 0.01. For each cytokine, at each time point, no statistically relevant difference was observed between the mean infected and the uninfected groups.
DISCUSSION
Understanding the role of the primary phagocytic antigen-presenting cell, in particular, the role that macrophage cytokines play in propagating the B. anthracis infection, may be critical for understanding the mechanism by which this bacterium causes disease. There are at least two distinct interactions between B. anthracis and the host macrophage during the course of an infection. The first is the interaction between the spore and the macrophage that initiates the infection and the second is the interaction between the lethal and edema toxins and the macrophage, which occurs after infection is established. Results from several elegant experiments performed by Hanna and colleagues suggested that production of TNF-α and IL-1β by macrophages may play a critical role in LeTx-mediated killing of the host (14, 15). However, in a number of recent studies, various authors have reported that purified LeTx preparations are able to block cytokine responsiveness (1, 6, 18, 24, 26). The experiments in which purified toxin is administered most probably reflect the outcome of the second interaction described above. Importantly, none of the previous studies attempted to examine the cytokine response resulting from an intracellular infection initiated by B. anthracis spores. Herein, we report the results of studies performed in primary mouse peritoneal macrophages, human dendritic cells, and in an inhalational mouse model of anthrax in which the serum cytokine levels, resulting from B. anthracis spore infection, were investigated.
The two primary cell culture models of intracellular infection exhibited significant initial killing of B. anthracis following spore uptake. Typically, a 90% reduction in viable CFU was observed by 2.5 h postinfection. Despite this activity, the number of intracellular CFU recovered sufficiently to result in bacterial release by 7.5 h following infection. In a recent publication, Ruthel and colleagues suggested that the outcome of intracellular infection may be dependent on the initial number of spores phagocytosed by each cell (31). Our studies indicated that MOIs of greater than 1:1 resulted in an overwhelming infection with rapid lysis (results not shown). We also observed that the spore dose was a critical factor for determining the outcome of the infection in A/J mice. The relationship between spore dose and lethality is demonstrated by our findings that lung spore doses of 2 × 103, 3 × 105 to 8 × 105, and 1 × 106 to 4 × 106 resulted in 0, 50, and 80 to 100% mortality, respectively. Taken together, these results suggest that the host mounts a vigorous innate immune response to B. anthracis spore challenge. This interpretation is supported by the relatively high doses of fully virulent spores that are required to induce lethality in the rabbit (50% lethal dose [LD50] = 1.1 × 105) and nonhuman primates (LD50 = 5.5 × 104) (17, 28).
We reported recently that the J774A.1 mouse macrophage cell line releases TNF-α and IL-12 in response to intracellular infection with B. anthracis spores (27). As a follow-up to our original observations, we sought to examine whether a similar response would be seen in primary macrophages. The results presented herein demonstrate that primary mouse peritoneal macrophages responded to spore infection by releasing significant levels of TNF-α and IL-6. Similar results were also observed in studies with human dendritic cell cultures. In addition to increased levels of TNF-α and IL-6, we detected IL-12, IL-1β, and the chemokine IL-8 in human dendritic cells infected with B. anthracis spores. Together, these results indicate that phagocytic antigen-presenting cells respond to B. anthracis spore infection with a robust proinflammatory cytokine response.
We report herein the first study of an inhalational infection of A/J mice with spores from the pXO1+ pXO2− Sterne strain. According to published reports and our own observations, i.p. administration of spores results in a course of infection that is different from that observed when spores are administered via the inhalational route. When mice were infected via the i.p. route, mortality occurred rapidly between the 2nd and 4th days postinfection, with deaths occurring in a relatively synchronized manner (34, 35). In the inhalational model, however, mice succumbed to infection between the 3rd and the 9th days following aerosol challenge and a 10- to 100-fold greater dose was required to approach 100% mortality in mice. High spore numbers were retained within the lung throughout the duration of the experiment, with a small proportion escaping from the lung to cause systemic infection. We observed dissemination of B. anthracis infection to the spleen in ∼50% of animals by day 3, increasing to 90% by day 5. When we examined the nature of the colonization of the spleen, we found that 100% of cells were vegetative, as expected. This was in contrast to the retained numbers of spores within the lung, which were predominantly heat resistant (data not shown). The cytokine response in the mouse model may be highly localized to sites of infection, as we observed the systemic response to be low when compared to our in vitro studies. At days 3 and 5 postinfection, IFN-γ and IL-6 were detected in the serum of some of the mice. Recently, Popov and others presented a study in which they infected mice with B. anthracis spores via the i.p. route (29) and found that there was systemic release of IL-1β and IL-6 from A/J mice and increased expression of TNF-α-specific mRNA in the liver. These results provide valuable indicators of the cytokine response to B. anthracis spores. It should be noted, however, that under normal circumstances, the peritoneum is a sterile environment, whereas the respiratory tract is in a constant state of exposure and response to microbial challenge. Thus, i.p. infection of mice with anthrax is unlikely to result in an infection that involves the same cellular populations as those encountered by B. anthracis during inhalational infection. Further investigations are required to examine tissue-specific expression of the relevant cytokines following inhalational exposure of mice to B. anthracis spores.
In this study, we provide further evidence of the stimulation of cytokine responses from two key phagocytic cells infected with B. anthracis spores. While previous studies have presented evidence that purified LeTx causes disablement of the cytokine response (1, 6, 18, 24, 26), we saw no evidence of an inhibitory effect when cultured macrophages were infected with a live, replicating, toxin-positive strain of B. anthracis (27). When we injected B. anthracis-infected A/J mice with a bolus dose of LPS, no impairment of the LPS-induced cytokine response was observed. It has been proposed that the impairment of macrophage and dendritic cell cytokine responses by LeTx may be a mechanism by which B. anthracis inhibits the innate immune response, thereby enhancing its opportunity to establish infection. We would argue that experiments in which purified toxin is added to cultured cells are not reflective of the interaction between the spore and phagocytic antigen-presenting cells. By exerting a toxic effect on 100% of target monocyte/macrophages or dendritic cells within a cell culture system or animal model, these studies may reflect the terminal stages of anthrax pathogenesis, once bacteremia has reached critically high levels and sufficient toxin concentrations have been achieved in the circulation. We suggest that models in which purified spores are added to monocyte/macrophages or dendritic cells within a cell culture system more accurately model the early interactions between B. anthracis and the host. Furthermore, in animal models, in order to more accurately model the relevant early interactions between B. anthracis and the host in inhalational anthrax, it is necessary to deliver the bacterial spore by the aerosol route. In our studies using these models, we see no evidence of an inhibition of the innate immune response as a result of infection with B. anthracis spores. Our results indicate that the host responds to infection with B. anthracis spores with a robust cytokine response. Further studies using our inhalational model of anthrax will be directed towards enhancing our understanding of the mechanisms by which pathogenesis occurs and providing a clearer picture of the early immune response to infection with B. anthracis spores.
Acknowledgments
We would like to thank Gopa Raychaudhuri, Karen Elkins, and Karen Meysick for critical reading of the manuscript.
Editor: J. T. Barbieri
REFERENCES
- 1.Agrawal, A., J. Lingappa, S. H. Leppla, S. Agrawal, A. Jabbar, C. Quinn, and B. Pulendran. 2003. Impairment of dendritic cells and adaptive immunity by anthrax lethal toxin. Nature 424:329-334. [DOI] [PubMed] [Google Scholar]
- 2.Barnes, J. M. 1947. The development of anthrax following administration of spores by inhalation. Br. J. Exp. Pathol. 28:385-394. [Google Scholar]
- 3.Dalldorf, F. G., A. F. Kaufmann, and P. S. Brachman. 1971. Woolsorter's disease. Arch. Pathol. 92:418-426. [PubMed] [Google Scholar]
- 4.Dang, O., L. Navarro, K. Anderson, and M. David. 2004. Cutting edge: anthrax lethal toxin inhibits activation of IFN-regulatory factor 3 by lipopolysaccharide. J. Immunol. 172:747-751. [DOI] [PubMed] [Google Scholar]
- 5.Dixon, T. C., A. A. Fadl, T. M. Koehler, J. A. Swanson, and P. C. Hanna. 2000. Early Bacillus anthracis-macrophage interactions: intracellular survival and escape. Cell Microbiol. 2:453-463. [DOI] [PubMed] [Google Scholar]
- 6.Erwin, J. L., L. M. DaSilva, S. Bavari, S. F. Little, A. M. Friedlander, and T. C. Chanh. 2001. Macrophage-derived cell lines do not express proinflammatory cytokines after exposure to Bacillus anthracis lethal toxin. Infect. Immun. 69:1175-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finlay, W. J. J., N. A. Logan, and A. D. Sutherland. 2002. Bacillus cereus emetic toxin production in cooked rice. Food Microbiol. 19:431-439. [Google Scholar]
- 8.Fouet, A., and S. Mesnage. 2002. Bacillus anthracis cell envelope components. Curr. Top. Microbiol. Immunol. 271:87-113. [DOI] [PubMed] [Google Scholar]
- 9.Friedlander, A. M., S. L. Welkos, M. L. M. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, P. Mikesell, and W. B. Lawrence. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239-1243. [DOI] [PubMed] [Google Scholar]
- 10.Fritz, D. L., N. K. Jaax, W. B. Lawrence, K. J. Davis, M. L. M. Pitt, J. Ezzell, and A. Friedlander. 1995. Pathology of experimental inhalation anthrax in the Rhesus monkey. Lab. Investig. 73:691-702. [PubMed] [Google Scholar]
- 11.Guidi-Rontani, C., M. Levy, H. Ohayon, and M. Mock. 2002. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol. Microbiol. 42:931-938. [DOI] [PubMed] [Google Scholar]
- 12.Guidi-Rontani, C., Y. Pereira, S. Ruffie, J. C. Sirard, M. Weber-Levy, and M. Mock. 1999. Identification and characterization of a germination operon on the virulence plasmid pXO1 of Bacillus anthracis. Mol. Microbiol. 33:407-414. [DOI] [PubMed] [Google Scholar]
- 13.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 14.Hanna, P. C., D. Acosta, and R. J. Collier. 1993. On the role of macrophages in anthrax. Proc. Natl. Acad. Sci. USA 90:10198-10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanna, P. C., B. A. Kruskal, R. A. Ezekowitz, B. R. Bloom, and R. J. Collier. 1994. Role of macrophage oxidative burst in the action of anthrax lethal toxin. Mol. Med. 1:7-18. [PMC free article] [PubMed] [Google Scholar]
- 16.Ireland, J. A. W., and P. C. Hanna. 2002. Macrophage-enhanced germination of Bacillus anthracis endospores requires gerS. Infect. Immun. 70:5870-5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ivins, B. E., M. L. M. Pitt, P. F. Fellows, J. W. Farchaus, G. E. Benner, D. M. Waag, S. F. Little, G. W. Anderson, P. H. Gibbs, and A. M. Friedlander. 1998. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine 16:1141-1148. [DOI] [PubMed] [Google Scholar]
- 18.Kalns, J., J. Scruggs, N. Millenbaugh, J. Vivekananda, D. Shealy, J. Eggers, and J. Kiel. 2002. TNF receptor 1, IL-1 receptor, and iNOS genetic knockout mice are not protected from anthrax infection. Biochem. Biophys. Res. Commun. 292:41-44. [DOI] [PubMed] [Google Scholar]
- 19.Klein, F., J. S. Walker, D. F. Fitzpatrick, R. E. Lincoln, B. G. Mahlandt, W. I. J. Jones, J. P. Dobbs, and K. J. Hendrix. 1966. Pathophysiology of anthrax. J. Infect. Dis. 116:123-138. [DOI] [PubMed] [Google Scholar]
- 20.Koch, R. 1876. Die etiologie der milzbrand krankheit hegrundet auf die entwickelungsgeschichte des Bacillus anthracis. Beitr. Biol. Pflanz. 2:277-283. [Google Scholar]
- 21.Lacy, D. B., and R. J. Collier. 2002. Structure and function of anthrax toxin. Curr. Top. Microbiol. Immunol. 271:61-85. [DOI] [PubMed] [Google Scholar]
- 22.LaForce, F. M., F. H. Bumford, J. C. Feeley, S. L. Stokes, and D. B. Snow. 1969. Epidemiologic study of a fatal case of inhalation anthrax. Arch. Environ. Health 18:798-805. [DOI] [PubMed] [Google Scholar]
- 23.Lincoln, R. E., D. R. Hodges, F. Klein, B. G. Mahlandt, W. I. J. Jones, B. W. Haines, M. A. Rhian, and J. S. Walker. 1965. Role of lymphatics in the pathogenesis of anthrax. J. Infect. Dis. 115:481-494. [DOI] [PubMed] [Google Scholar]
- 24.Moayeri, M., D. Haines, H. A. Young, and S. H. Leppla. 2003. Bacillus anthracis lethal toxin induces TNF-alpha-independent hypoxia-mediated toxicity in mice. J. Clin. Investig. 112:670-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 26.Pellizzari, R., C. Guidi-Rontani, G. Vitale, M. Mock, and C. Montecucco. 1999. Anthrax lethal factor cleaves MKK3 in macrophages and inhibits the LPS/IFNgamma-induced release of NO and TNFalpha. FEBS Lett. 462:199-204. [DOI] [PubMed] [Google Scholar]
- 27.Pickering, A. K., and T. J. Merkel. 2004. Macrophages release tumor necrosis factor alpha and interleukin-12 in response to intracellular Bacillus anthracis spores. Infect. Immun. 72:3069-3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pitt, M. L. M., S. F. Little, B. E. Ivins, P. Fellows, J. Barth, J. Hewetson, P. Gibbs, M. Dertzbaugh, and A. M. Friedlander. 2001. In vitro correlate of immunity in a rabbit model of inhalational anthrax. Vaccine 19:4768-4773. [DOI] [PubMed] [Google Scholar]
- 29.Popov, S. G., T. G. Popova, E. Grene, F. Klotz, J. Cardwell, C. Bradburne, Y. Jama, M. Maland, J. Wells, A. Nalca, T. Voss, C. Bailey, and K. Alibek. 2004. Systemic cytokine response in murine anthrax. Cell Microbiol. 6:225-233. [DOI] [PubMed] [Google Scholar]
- 30.Ross, J. M. 1957. The pathogenesis of anthrax following the administration of spores by the respiratory route. J. Pathol. Bacteriol. 73:485-494. [Google Scholar]
- 31.Ruthel, G., W. J. Ribot, S. Bavari, and T. A. Hoover. 2004. Time-lapse confocal imaging of development of Bacillus anthracis in macrophages. J. Infect. Dis. 189:1313-1316. [DOI] [PubMed] [Google Scholar]
- 32.Shafa, F., B. J. Moberly, and P. Gerhardt. 1966. Cytological features of anthrax spores phagocytized in vitro by rabbit alveolar macrophages. J. Infect. Dis. 116:401-413. [DOI] [PubMed] [Google Scholar]
- 33.Turnbull, P. C. 2002. Introduction: anthrax history, disease and ecology. Curr. Top. Microbiol. Immunol. 271:1-19. [DOI] [PubMed] [Google Scholar]
- 34.Welkos, S. L., and A. M. Friedlander. 1988. Pathogenesis and genetic control of resistance to the Sterne strain of Bacillus anthracis. Microb. Pathog. 4:53-69. [DOI] [PubMed] [Google Scholar]
- 35.Welkos, S. L., T. J. Keener, and P. H. Gibbs. 1986. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 51:795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Welkos, S. L., R. W. Trotter, D. M. Becker, and G. O. Nelson. 1989. Resistance to the Sterne strain of Bacillus anthracis—phagocytic cell responses of resistant and susceptible mice. Microb. Pathog. 7:15-35. [DOI] [PubMed] [Google Scholar]
- 37.Zaucha, G. M., L. M. Pitt, J. Estep, B. E. Ivins, and A. Friedlander. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch. Pathol. Lab. Med. 122:982-992. [PubMed] [Google Scholar]