Abstract
Genes expressed by Actinobacillus pleuropneumoniae in necrotic porcine lung tissue were identified by selective capture of transcribed sequences analysis. In total, 46 genes were identified, 20 of which have been previously reported to be associated with in vivo expression or virulence in A. pleuropneumoniae or in other organisms.
The porcine respiratory tract pathogen Actinobacillus pleuropneumoniae presents a major problem to the swine industry due to its ability to persist in the host, surviving in tonsils as well as in sequestered necrotic lung tissue, which leads to the occurrence of subclinically infected carrier animals (6, 11, 18). Genes expressed by A. pleuropneumoniae only in the host are likely to play an important role in virulence and persistence. This is demonstrated by the finding that natural infection with A. pleuropneumoniae results in protection from reinfection with homologous and heterologous serotypes (7); the latter cannot be achieved by vaccination with bacterin vaccines commercially available (26). Therefore, the identification of genes expressed in these tissues would contribute significantly to the understanding of A. pleuropneumoniae disease.
To identify genes expressed by A. pleuropneumoniae in vivo, a variety of approaches have been successfully employed, like in vivo expression technology (IVET) (14, 36), signature-tagged mutagenesis (STM) (13, 34), and representational difference analysis (RDA) of A. pleuropneumoniae grown with the addition of bronchoalveolar lavage fluid (BALF) (4, 19). The latter technique is an ex vivo approach mimicking in vivo conditions. IVET is based on complementation of an attenuating auxotrophic mutation by gene fusion. In STM, a tagged transposon is used that disrupts genes by randomly inserting in the genome. Both STM and IVET analyses involve the infection of animals with a pool of mutants followed by recovery, selection, and comparative analysis of mutants. IVET then allows the identification of promoters switched on in vivo (14), while STM results in the identification of genes that are essential for survival in vivo (34).
The technique used for this work, selective capture of transcribed sequences (SCOTS), involves the capture of transcribed sequences by using biotinylated chromosomal DNA coupled to streptavidin-coated paramagnetic beads and a PCR-based subtractive hybridization with transcripts from culture-grown bacteria. It was originally described by Graham and Clark-Curtiss in 1999 for the identification of genes expressed by Mycobacterium tuberculosis upon growth in macrophages (16). The technique was subsequently used for the isolation of macrophage-activated Mycobacterium avium (23) and Salmonella enterica serovar Typhi genes (8). Recently it was demonstrated that the technique is sensitive enough to isolate bacterial genes expressed in tissues of infected animals (10).
While the enrichment principle of SCOTS is very similar to that of RDA, RDA alone cannot differentiate between host and bacterial cDNA. Additionally, RDA using BALF to induce differential gene expression will allow the identification of some genes expressed from A. pleuropneumoniae in epithelial lining fluid, but transcriptional differences as they occur in necrotic lung tissue will not be detected. The STM technique, an in vivo approach, identifies genes whose function cannot be complemented by either the single organism or the coinfecting mutants and are, therefore, essential for survival in vivo. Hence, its scope differs from SCOTS, which aims to identify genes that are upregulated in vivo but are not necessarily essential. The second in vivo approach, IVET, aims at the identification of promoters only switched on in vivo, thereby targeting some of the same genes found via SCOTS; however, it requires animal experiments under biosafety level 2 conditions, using pools of transformants. Further, in both in vivo techniques the different growth rates of individual transformants within the pool require a termination of the experiment within hours after infection. In IVET, clones carrying promoters that are switched on in later stages of infection may be eliminated before that time, and in STM the outgrowth of single clones restricts the diversity of the recovered pool, resulting in a large number of false positives, i.e., genes being falsely identified as essential in vivo. As neither of these techniques is applicable to the identification of genes involved in the later stages of the disease, the SCOTS analysis is a valid complementation and might facilitate further elucidation of A. pleuropneumoniae virulence, particularly in the postacute stages of infection.
For the study presented here, we employed SCOTS to identify genes expressed by A. pleuropneumoniae in necrotic porcine lung tissue at the end of the acute stage of infection (7 days postinfection). Pigs were infected with A. pleuropneumoniae C1569 (Table 1) by using an aerosol infection model described previously (1, 3, 4). The dose used was 10.8 × 104 CFU for four pigs, a dose which has been shown to reliably induce acute but not fatal disease. Samples of necrotic lung tissue from five pigs were obtained after 7 days of infection, and the samples were confirmed to be culture positive, with surface smears yielding dense to confluent growth on Columbia blood agar plates. Such samples typically contain 106 to 108 CFU per gram of tissue. Samples intended for RNA isolation were immediately preserved in RNAlater solution (Ambion Inc., Houston, Tex.) at the time of collection, RNA was prepared with RNEasy columns (QIAGEN, Hilden, Germany), and RNA integrity was verified by visualization on an agarose gel. For use in this experiment, RNA from five animals was then pooled. RNA samples intended for reverse transcription were treated with TurboDNAse (Promega, Mannheim, Germany) according to the manufacturer's instructions, and absence of genomic DNA was confirmed by PCR using primers oRN5-1 and oRN5-2, which amplify a 180-bp fragment of the dimethyl sulfoxide reductase gene (2). For subtraction, A. pleuropneumoniae C1569 RNA was prepared from liquid cultures that had been grown aerobically with shaking to an optical density at 600 nm of 0.4. RNA samples prepared from porcine lung tissue as well as RNA prepared from A. pleuropneumoniae C1569 grown under standard culturing conditions were subjected to reverse transcription with primer oSCOTS-N9-1 or oSCOTS-N9-2, consisting of a defined terminal sequence at the 5′ end and a random 9mer 3′ end (Table 1), according to the descriptions of Daigle et al. (8). Each cDNA population was subjected to three rounds of normalization, consisting of hybridization to biotinylated genomic A. pleuropneumoniae C1569 DNA that had been blocked beforehand using DNA representing 16S and 23S A. pleuropneumoniae rRNA sequences with four PCR products representing ribosomal 16S and 23S RNA sequences (Table 1). For enrichment of sequences preferentially transcribed or upregulated during growth in porcine lung tissue, biotinylated genomic A. pleuropneumoniae C1569 DNA was preblocked with PCR products representing rRNA sequences as well as cDNA obtained from culture-grown bacteria after three rounds of normalization. Three rounds of capture hybridization with normalized cDNA from A. pleuropneumoniae C1569 grown in the porcine lung were then performed. Lung-specific cDNAs were then cloned with the TOPO TA Cloning kit (Invitrogen, Karlsruhe, Germany) according to the manufacturer's instructions. Cloned inserts were amplified by PCR, spotted on nylon membranes, and subjected to Southern dot blot analysis with [32P]dCTP-labeled lung- and culture-specific cDNA pools obtained after three rounds of normalization, respectively. Dot blots were washed with 3× SSC (1× SSC is 0.15 M NaCl plus 0.015 M sodium citrate), 0.1% sodium dodecyl sulfate at 60°C. In order to allow comparison of the signal intensities in both blots, 1 and 0.1 μg of genomic A. pleuropneumoniae C1569 DNA spotted on nylon membranes were used as positive controls exposed alongside their corresponding SCOTS clone dot blots (Fig. 1). Signals were weaker or absent for all cloned inserts on the blot hybridized to the normalized culture-specific cDNA compared to signals on the blot hybridized to normalized lung-specific cDNA (Fig. 1), indicating that these sequences are either absent or present in much less abundance in cDNA prepared from A. pleuropneumoniae grown under standard culturing conditions.
TABLE 1.
Characteristics of bacterial strains and primers used in this study
| Strain, plasmid or primer | Characteristics and/or sequences | Source and/or reference |
|---|---|---|
| Strains | ||
| A. pleuropneumoniae C1569 | A. pleuropneumoniae serotype 9, clinical isolate | Diagnostic unit of the Department of Infectious Diseases |
| Escherichia coli TOP10 F′ | F−mcrA Δ(mrr-hsdRMS-mcrBC) Φ80lacZΔM15 ΔlacX74 rec A1 deoR araD139 Δ(araleu)7697 galU galK rpsL (Strr) endA1 nupG | TOPO TA Cloning (Invitrogen) |
| Plasmid | ||
| pCR 2.1-TOPO | Topoisomerase I enhanced E. coli cloning vector | TOPO TA Cloning (Invitrogen) (35) |
| Primers | ||
| M13 forward | 5′ CAGGAAACAGCTATGAC 3′ | Amersham Biosciences |
| M13 reverse | 5′ GTAAAACGACGGCCAG 3′ | Amersham Biosciences |
| oSCOTS-N9-1 | 5′ GTGGTACCGCTCTCCGTCCGA-N9 3′ | 8 |
| oSCOTS-N9-2 | 5′ CGGGATCCAGCTTCTGACGCA-N9 3′ | 8 |
| oSCOTS1 | 5′ GTGGTACCGCTCTCCGTCCGA 3′ | 8 |
| oSCOTS2 | 5′ CGGGATCCAGCTTCTGACGCA 3′ | 8 |
| oRRN16-1 | 5′ TGGGTCGTAGGTTCAAATCC 3′ | This work |
| oRRN16-2 | 5′ GCGTCAGTACATTCCCAAGG 3′; amplifies 5′ end of 16s rRNA sequence; product size, 990 bp | |
| oRRN16-3 | 5′ TGTAGCGGTGAAATGCGTAG 3′ | This work |
| oRRN16-4 | 5′ ACTTGAACCACCGACCTCAC 3′; amplifies 3′ end of 16s rRNA sequence; product size, 1,000 bp | |
| oRRN23-1 | 5′ TTGGAAACAAGCTGAAAACTGA 3′ | This work |
| oRRN23-2 | 5′ GGACAGGAACCCTTGGTCTT 3′; amplifies 5′ end of 23s rRNA sequence; product size, 1,480 bp | |
| oRRN23-3 | 5′ TCAGAAGTGCGAATGCTGAC 3′ | This work |
| oRRN23-4 | 5′ CTGGCGAGACAACTGGTACA 3′; amplifies 3′ end of 23S rRNA sequence; product size, 1,466 bp | |
| oADH7 | 5′ ACACGTAATGACGGCGGTA 3′ | This work |
| oADH8 | 5′ CGAGTGGATTCACCCAATTT 3′; amplifies a 158-bp product from an A. pleuropneumoniae autotransporter adhesin; acc. no. ZP 00204542 | |
| oFLPD1 | 5′ TTTCTCTGTAGAGATGGTTTGTGC 3′ | This work |
| oFLPD2 | 5′ AACCCAATTAACCCAAATGGT 3′; amplifies a 154-bp product from an A. pleuropneumoniae fimbria-like protein; acc. no. NP 873737 |
FIG. 1.
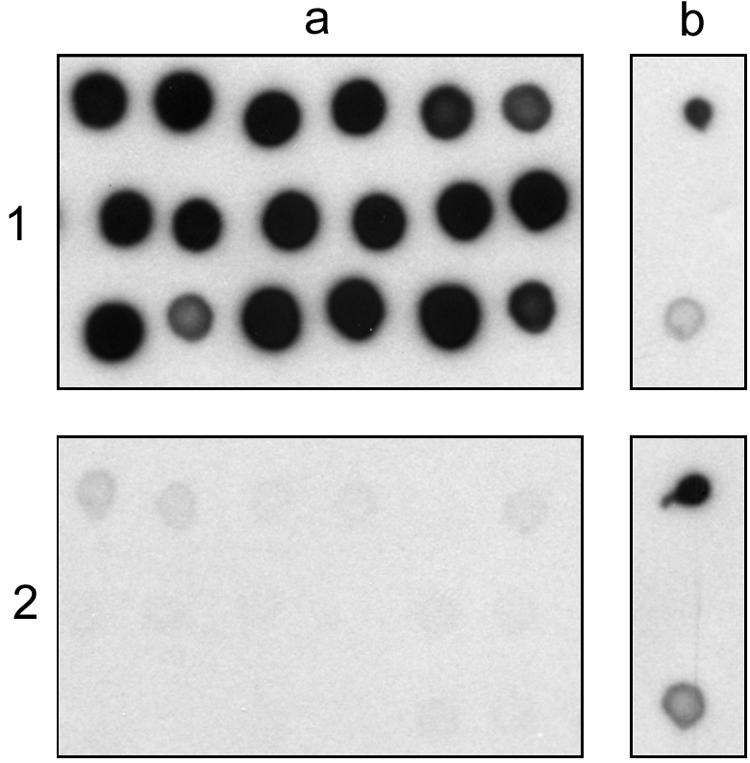
Southern dot blot showing (a) SCOTS clones and (b) 1 μg (top) or 0.1 μg (bottom) of genomic A. pleuropneumoniae DNA as positive controls, hybridized to a radiolabeled probe generated from lung-derived (1) or culture-derived cDNA (2) after three rounds of normalization.
Inserts were subjected to partial sequence analysis in a commercial laboratory (SeqLab, Goettingen, Germany). Sequence analyses were carried out using BLAST algorithms available in the HUSAR program package at the Deutsches Krebsforschungszentrum (dkfz) in Heidelberg, Germany. Sequence data were also compared to the database of the unfinished genomic sequence of A. pleuropneumoniae in a BLAST Search available at http://www.ncbi.nlm.nih.gov/sutils/genom_table.cgi. For reverse transcription-PCR, RNA was prepared and DNase treated as described above for SCOTS samples, and reverse transcription was carried out using 5 μg of RNA in the presence of 5 pmol of a gene-specific reverse primer.
We identified 46 genes differentially expressed by A. pleuropneumoniae in necrotic lung tissue (Table 2). Two of the sequences identified were confirmed to be part of A. pleuropneumoniae genes by database comparison but showed no homology to genes with known function. The remaining 44 genes identified by SCOTS analysis can be divided into six functional groups: secreted proteins, cell surface, metabolism, regulatory, stress, and transport (Table 2).
TABLE 2.
Genes identified via SCOTS
| Class | Clone(s) | Gene and/or possible functiona | % Identity/ % similarityb | Spanc | Reference(s)d | GenBank accession no. |
|---|---|---|---|---|---|---|
| Secreted | H7 | ApxIVA var3 RTX toxin (A. pleuropneumoniae) | 33 | AAD01905 | ||
| Cell surface | B5 | Autotransporter adhesin, similar to Hsf in H. influenzae (A. pleuropneumoniae) | 29, 39, 41 | ZP_00204542 | ||
| E4 | flpD, fimbria-like protein (H. ducreyi); flp genes are essential for microcolony formation in H. ducreyi | 65/66 | 188 | 12, 31, 37 | NP_873737 | |
| B9 | Outer membrane protein similar to immunogenic protein PomA of P. multocida (A. pleuropneumoniae) | 13, 42 | E47068 | |||
| F4 | Outer membrane protein of unknown function (A. pleuropneumoniae) | ZP_00135264 | ||||
| Metabolism | A7 | guaA GMP synthase (A. pleuropneumoniae), linked to virulence in various organisms, including P. multocida | 12, 27, 32, 34 | ZP_00134556 | ||
| A8 | Diadenosine tetraphosphatase similar to ApaH in S. enterica serovar Typhimurium (A. pleuropneumoniae); linked to virulence in H. parasuis and serovar Typhimurium | 21, 24 | ZP_00134055 | |||
| A9 | fuc1, l-fucose isomerase (H. influenzae); in Bacteroides thetaiotaomicron, the l-fucose metabolic pathway is coordinated with the production of fucosylated glycans in enterocytes | 76/78 | 222 | 22, 25 | P44779 | |
| C2 | ptsB, sucrose-specific phosphotransferase EII component (P. multocida); linked to virulence in serovar Typhimurium, S. aureus, and H. influenzae | 83/85 | 216 | 28 | NP_246785 | |
| H3 | Sugar phosphate permease (A. pleuropneumoniae) | ZP_00135166 | ||||
| C7 | Oxygen-sensitive ribonucleoside-triphosphate reductase (A. pleuropneumoniae) | ZP_00134686 | ||||
| D2 | Thiol:disulfide interchange protein, similar to DsbA in H. influenzae (A. pleuropneumoniae); essential for virulence factor expression in P. aeruginosa | 17, 34 | ZP_00134426 | |||
| D3 | 3-Polyprenyl-4-hydroxybenzoate decarboxylase (A. pleuropneumoniae) | ZP_00134932 | ||||
| G6 | Ribosomal protein RpS19 (H. influenzae) | 100/100 | 90 | P44385 | ||
| E12 | Biotin-(acetyl-coenzyme A carboxylase) ligase (A. pleuropneumoniae) | ZP_00134488 | ||||
| F12 | Dethiobiotin synthetase (A. pleuropneumoniae) | ZP_00135280 | ||||
| F11 | NADH ubiquinone oxidoreductase subunit 5 (A. pleuropneumoniae) | 34 | ZP_00135039 | |||
| G8 | SAM-dependent methyltransferase (A. pleuropneumoniae) | 34 | ZP_00134291 | |||
| A4 | Uncharacterized conserved protein involved in oxidation of intracellular sulfur (A. pleuropneumoniae) | ZP_00133817 | ||||
| A11 | Transposase (A. pleuropneumoniae) | ZP_00134532 | ||||
| D1 | 3-Oxoacyl-(acyl-carrier protein) reductase (H. influenzae) | 78/82 | 238 | P43713 | ||
| D4 | Predicted GTPase (A. pleuropneumoniae) | ZP_00134954 | ||||
| G11 | ATPase (A. pleuropneumoniae) | ZP_00134371 | ||||
| E9 | Restriction-modification system (ALXA and HSDM, M . haemolytica); M. haemolytica AlxA activates leukotoxin transcription in E. coli | 81/81 | 156 | 20 | P95510 | |
| F8 | Molybdopterin biosynthesis protein (H. ducreyi) | 84/86 | 174 | 34 | AAP95073 | |
| H6 | Leucyl-tRNA synthetase (A. pleuropneumoniae) | ZP_00133841 | ||||
| F9 | Predicted hydrolase of alkaline phosphatase superfamily (A. pleuropneumoniae) | ZP_00134565 | ||||
| Regulatory | A3 | rpoB, RNA polymerase subunit (H. ducreyi) | 91/94 | 207 | AAP96608 | |
| B2 | Cell shape-determining protein, similar to MreC (A. pleuropneumoniae) | ZP_00134717 | ||||
| A10 | Signal recognition particle protein (H. influenzae) | 88/93 | 243 | P44518 | ||
| H5 | Molecular chaperone (A. pleuropneumoniae) | ZP_00134922 | ||||
| H4 | Putative transcriptional regulator (A. pleuropneumoniae) | ZP_00134590 | ||||
| Stress | C9 | tufA, elongation factor (EF) Tu (H. ducreyi); EF-Tu acts as a fibronectin binding protein in M. pneumoniae, linked to virulence in K. pneumoniae | 100/100 | 135 | 9, 40 | NP_872680 |
| Transport | A5 | apaA, putative ABC transporter, immunogenic (A. pleuropneumoniae) | 30 | AF109148 | ||
| H1 | dmsA, dimethyl sulfoxide reductase, catalytic subunit (A. pleuropneumoniae); deletion mutants are attenuated | 2 | AY138463 | |||
| C4 | hgbA, hemoglobin-binding protein (A. pleuropneumoniae); enables iron uptake from hemoglobin | 5, 38 | AAO33396 | |||
| G1 | Na+/H+ antiporter (A. pleuropneumoniae); essential for in vivo survival in S. agalactiae | 27 | ZP_00134319 | |||
| E1 | Predicted metal-binding protein (A. pleuropneumoniae) | ZP_00135073 | ||||
| E7 | Membrane components of Kef-type potassium transport systems (A. pleuropneumoniae) | ZP_00134994 | ||||
| F1 | Anaerobic C4-dicarboxylate transporter (A. pleuropneumoniae) | 34 | ZP_00134386 | |||
| F2 | tbpA, transferrin receptor; small subunit (A. pleuropneumoniae); upregulated and essential in vivo | 1 | CAA90896 | |||
| F5 | ATPase; cation transport (A. pleuropneumoniae) | ZP_00135075 | ||||
| G10 | Di- and tricarboxylate transporters (A. pleuropneumoniae) | ZP_00135062 | ||||
| Unknown | B8 | Hypothetical protein PA2218 (P. aeruginosa) | 76/83 | 162 | Q01609 | |
| G7, F7e | A. pleuropneumoniae; no homology to known genes |
Genes with highest similarity to SCOTS sequences, obtained from public databases, source organism in parentheses, genes names given where available. SAM, S-adenosylmethionine.
Identity/similarity percentages apply to amino acids.
Span means the number of nucleotides over which similarity was detected.
Publications reporting the isolation of identical or similar sequences.
Sequences have not been submitted as these are partial open reading frames only.
Among the confirmed A. pleuropneumoniae sequences were four genes that are not expressed by A. pleuropneumoniae under standard culturing conditions but are present in vivo, such as the ApxIV toxin (33), the putative ABC transporter ApaA (30), the small subunit of the transferrin receptor, TbpB (15), and the catalytic subunit of dimethyl sulfoxide reductase (2) (Table 2). Further, some sequences identified in this study represent genes that have previously been identified in A. pleuropneumoniae via STM as being required for virulence (13, 34), such as GMP synthase, a thiol:disulfide interchange protein (DsbA), a molybdopterin cofactor synthesis protein, and an outer membrane protein similar to PomA of Pasteurella multocida (Table 2).
In addition, some of the identified genes have been reported to be expressed in vivo or to be involved in virulence in other organisms. Examples include a fimbria-like protein similar to FlpD of Haemophilus ducreyi which, in H. ducreyi, is necessary for microcolony formation and virulence in humans (31, 37); a diadenosine tetraphosphatase which plays a role in Salmonella spp. invasion (24); or hemoglobin binding protein HbgA, which is expressed in vivo in P. multocida (5) and under iron-deficient conditions in A. pleuropneumoniae (38). A homologue of the thiol:disulfide interchange protein identified in A. pleuropneumoniae via STM (34), DsbA, is required for the expression of the type III secretion system under low-calcium-inducing conditions, intracellular survival upon infection of HeLa cells, and twitching motility in P. aeruginosa (17).
Perhaps most importantly, a sequence similar to that of the high-molecular-weight autotransporter adhesin Hsf of Haemophilus influenzae, which is expressed by encapsulated H. influenzae strains and is homologous to the H. influenzae Hia adhesin (39), was identified. A Hia homologue is also expressed in vivo by Neisseria meningitidis (41). Autotransporter adhesins have not been characterized in A. pleuropneumoniae to date; however, a search of the unfinished genomic database for A. pleuropneumoniae revealed several putative autotransporter adhesin genes (GenBank accession numbers NZ_AACK01000066 and NZ_AACK01000041). In order to further confirm the results of the SCOTS analysis, transcription of the autotransporter adhesin and the flpD genes in porcine lung tissue was confirmed by reverse transcription-PCR using primers oADH1 and oADH2 as well as oFLPD1 and oFLPD2 (Fig. 2).
FIG. 2.

PCR following reverse transcription of 5 μg of RNA derived from A. pleuropneumoniae-infected lung (lanes 1 to 5). Also shown is serial dilution of the cDNA template, ranging from undiluted (lane 1) to 1:10,000 (lane 5). Lanes a and b show positive controls using primer pairs oADH1/oADH2 (a) and oFLPD1/oFLPD2 (b), with chromosomal A. pleuropneumoniae DNA as template. −, No template.
Our approach identified genes that may be upregulated in the host by a range of stimuli, including lack of iron, lack of oxygen, and host-specific factors. In order to confirm that we identified not only genes regulated by either iron deficiency or lack of oxygen, we repeated the enrichment procedure by using cDNA from bacteria grown under iron-deficient or anaerobic conditions, respectively, as previously described (2, 4). Thus, cDNA from bacteria grown under iron-deficient or anaerobic conditions after three rounds of normalization was used to preblock the biotinylated chromosomal A. pleuropneumoniae DNA before hybridization to lung-derived sequences. Subsequent analysis of differentially expressed sequences again identified the autotransporter adhesin and the ApxIV toxin, implying that their regulation is independent of iron deficiency and lack of oxygen.
For all other genes identified in this study and not mentioned explicitly above, putative functions as well as publications describing in vivo expression and/or involvement in virulence in A. pleuropneumoniae or other organisms are listed in Table 2. In total, 20 of the 46 identified genes have been linked to in vivo expression and/or virulence.
This finding strongly suggests that SCOTS analysis is a suitable tool for the study of gene expression in infected porcine lung tissue. Further experiments employing SCOTS analyses to identify transcriptional differences in bacteria at different localizations (i.e., tonsils and unaltered lung tissue) as well as in even later stages of infection might help to identify the molecular mechanisms for long-term colonization and give clues to its prevention.
Nucleotide sequence accession numbers.
The sequences identified in the course of this work have been deposited in GenBank, and their numbers are listed in Table 2.
Acknowledgments
This work was supported by grant GE522/3-2 and Sonderforschungsbereich 587 (Project A4) from the Deutsche Forschungsgemeinschaft, Bonn, Germany.
Editor: J. N. Weiser
REFERENCES
- 1.Baltes, N., I. Hennig-Pauka, and G. F. Gerlach. 2002. Both transferrin binding proteins are virulence factors in Actinobacillus pleuropneumoniae serotype 7 infection. FEMS Microbiol. Lett. 209:283-287. [DOI] [PubMed] [Google Scholar]
- 2.Baltes, N., I. Hennig-Pauka, I. Jacobsen, A. D. Gruber, and G. F. Gerlach. 2003. Identification of dimethyl sulfoxide reductase in Actinobacillus pleuropneumoniae and its role in infection. Infect. Immun. 71:6784-6792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baltes, N., W. Tonpitak, G. F. Gerlach, I. Hennig-Pauka, A. Hoffmann-Moujahid, M. Ganter, and H. J. Rothkotter. 2001. Actinobacillus pleuropneumoniae iron transport and urease activity: effects on bacterial virulence and host immune response. Infect. Immun. 69:472-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baltes, N., W. Tonpitak, I. Hennig-Pauka, A. D. Gruber, and G. F. Gerlach. 2003. Actinobacillus pleuropneumoniae serotype 7 siderophore receptor FhuA is not required for virulence. FEMS Microbiol. Lett. 220:41-48. [DOI] [PubMed] [Google Scholar]
- 5.Bosch, M., M. E. Garrido, M. Llagostera, A. M. Perez De Rozas, I. Badiola, and J. Barbe. 2002. Characterization of the Pasteurella multocida hgbA gene encoding a hemoglobin-binding protein. Infect. Immun. 70:5955-5964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chiers, K., I. van Overbeke, P. De Laender, R. Ducatelle, S. Carel, and F. Haesebrouck. 1998. Effects of endobronchial challenge with Actinobacillus pleuropneumoniae serotype 9 of pigs vaccinated with inactivated vaccines containing the Apx toxins. Vet. Q. 20:65-69. [DOI] [PubMed] [Google Scholar]
- 7.Cruijsen, T. L., L. A. van Leengoed, M. Ham-Hoffies, and J. H. Verheijden. 1995. Convalescent pigs are protected completely against infection with a homologous Actinobacillus pleuropneumoniae strain but incompletely against a heterologous-serotype strain. Infect. Immun. 63:2341-2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daigle, F., J. E. Graham, and R. Curtiss III. 2001. Identification of Salmonella typhi genes expressed within macrophages by selective capture of transcribed sequences (SCOTS). Mol. Microbiol. 41:1211-1222. [DOI] [PubMed] [Google Scholar]
- 9.Dallo, S. F., T. R. Kannan, M. W. Blaylock, and J. B. Baseman. 2002. Elongation factor Tu and E1 beta subunit of pyruvate dehydrogenase complex act as fibronectin binding proteins in Mycoplasma pneumoniae. Mol. Microbiol. 46:1041-1051. [DOI] [PubMed] [Google Scholar]
- 10.Dozois, C. M., F. Daigle, and R. Curtiss III. 2003. Identification of pathogen-specific and conserved genes expressed in vivo by an avian pathogenic Escherichia coli strain. Proc. Natl. Acad. Sci. USA 100:247-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fenwick, B., and S. Henry. 1994. Porcine pleuropneumonia. J. Am. Vet. Med. Assoc. 204:1334-1340. [PubMed] [Google Scholar]
- 12.Fuller, T. E., M. J. Kennedy, and D. E. Lowery. 2000. Identification of Pasteurella multocida virulence genes in a septicemic mouse model using signature-tagged mutagenesis. Microb. Pathog. 29:25-38. [DOI] [PubMed] [Google Scholar]
- 13.Fuller, T. E., S. Martin, J. F. Teel, G. R. Alaniz, M. J. Kennedy, and D. E. Lowery. 2000. Identification of Actinobacillus pleuropneumoniae virulence genes using signature-tagged mutagenesis in a swine infection model. Microb. Pathog. 29:39-51. [DOI] [PubMed] [Google Scholar]
- 14.Fuller, T. E., R. J. Shea, B. J. Thacker, and M. H. Mulks. 1999. Identification of in vivo induced genes in Actinobacillus pleuropneumoniae. Microb. Pathog. 27:311-327. [DOI] [PubMed] [Google Scholar]
- 15.Gerlach, G. F., C. Anderson, A. A. Potter, S. Klashinsky, and P. J. Willson. 1992. Cloning and expression of a transferrin-binding protein from Actinobacillus pleuropneumoniae. Infect. Immun. 60:892-898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham, J. E., and J. E. Clark-Curtiss. 1999. Identification of Mycobacterium tuberculosis RNAs synthesized in response to phagocytosis by human macrophages by selective capture of transcribed sequences (SCOTS). Proc. Natl. Acad. Sci. USA 96:11554-11559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ha, U. H., Y. Wang, and S. Jin. 2003. DsbA of Pseudomonas aeruginosa is essential for multiple virulence factors. Infect. Immun. 71:1590-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haesebrouck, F., K. Chiers, I. van Overbeke, and R. Ducatelle. 1997. Actinobacillus pleuropneumoniae infections in pigs: the role of virulence factors in pathogenesis and protection. Vet. Microbiol. 58:239-249. [DOI] [PubMed] [Google Scholar]
- 19.Hennig, I., B. Teutenberg-Riedel, and G. F. Gerlach. 1999. Downregulation of a protective Actinobacillus pleuropneumoniae antigen during the course of infection. Microb. Pathog. 26:53-63. [DOI] [PubMed] [Google Scholar]
- 20.Highlander, S. K., and V. T. Hang. 1997. A putative leucine zipper activator of Pasteurella haemolytica leukotoxin transcription and the potential for modulation of its synthesis by slipped-strand mispairing. Infect. Immun. 65:3970-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill, C. E., D. S. Metcalf, and J. I. MacInnes. 2003. A search for virulence genes of Haemophilus parasuis using differential display RT-PCR. Vet. Microbiol. 96:189-202. [DOI] [PubMed] [Google Scholar]
- 22.Hooper, L. V., J. Xu, P. G. Falk, T. Midtvedt, and J. I. Gordon. 1999. A molecular sensor that allows a gut commensal to control its nutrient foundation in a competitive ecosystem. Proc. Natl. Acad. Sci. USA 96:9833-9838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hou, J. Y., J. E. Graham, and J. E. Clark-Curtiss. 2002. Mycobacterium avium genes expressed during growth in human macrophages detected by selective capture of transcribed sequences (SCOTS). Infect. Immun. 70:3714-3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ismail, T. M., C. A. Hart, and A. G. McLennan. 2003. Regulation of dinucleoside polyphosphate pools by the YgdP and ApaH hydrolases is essential for the ability of Salmonella enterica serovar Typhimurium to invade cultured mammalian cells. J. Biol. Chem. 278:32602-32607. [DOI] [PubMed] [Google Scholar]
- 25.Jefcoat, A. M., J. A. Hotchkiss, V. Gerber, J. R. Harkema, C. B. Basbaum, and N. E. Robinson. 2001. Persistent mucin glycoprotein alterations in equine recurrent airway obstruction. Am. J. Physiol. Lung Cell Mol. Physiol. 281:L704-L712. [DOI] [PubMed] [Google Scholar]
- 26.Jolie, R. A., M. H. Mulks, and B. J. Thacker. 1995. Cross-protection experiments in pigs vaccinated with Actinobacillus pleuropneumoniae subtypes 1A and 1B. Vet. Microbiol. 45:383-391. [DOI] [PubMed] [Google Scholar]
- 27.Jones, A. L., K. M. Knoll, and C. E. Rubens. 2000. Identification of Streptococcus agalactiae virulence genes in the neonatal rat sepsis model using signature-tagged mutagenesis. Mol. Microbiol. 37:1444-1455. [DOI] [PubMed] [Google Scholar]
- 28.Kok, M., G. Bron, B. Erni, and S. Mukhija. 2003. Effect of enzyme I of the bacterial phosphoenolpyruvate: sugar phosphotransferase system (PTS) on virulence in a murine model. Microbiology 149:2645-2652. [DOI] [PubMed] [Google Scholar]
- 29.Lo, R. Y. 2001. Genetic analysis of virulence factors of Mannheimia (Pasteurella) haemolytica A1. Vet. Microbiol. 83:23-35. [DOI] [PubMed] [Google Scholar]
- 30.Martin, P. R., and M. H. Mulks. 1999. Cloning and characterization of a gene encoding an antigenic membrane protein from Actinobacillus pleuropneumoniae with homology to ABC transporters. FEMS Immunol. Med. Microbiol. 25:245-254. [DOI] [PubMed] [Google Scholar]
- 31.Nika, J. R., J. L. Latimer, C. K. Ward, R. J. Blick, N. J. Wagner, L. D. Cope, G. G. Mahairas, R. S. Munson, Jr., and E. J. Hansen. 2002. Haemophilus ducreyi requires the flp gene cluster for microcolony formation in vitro. Infect. Immun. 70:2965-2975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russo, T. A., S. T. Jodush, J. J. Brown, and J. R. Johnson. 1996. Identification of two previously unrecognized genes (guaA and argC) important for uropathogenesis. Mol. Microbiol. 22:217-229. [DOI] [PubMed] [Google Scholar]
- 33.Schaller, A., R. Kuhn, P. Kuhnert, J. Nicolet, T. J. Anderson, J. I. MacInnes, R. P. Segers, and J. Frey. 1999. Characterization of apxIVA, a new RTX determinant of Actinobacillus pleuropneumoniae. Microbiology 145:2105-2116. [DOI] [PubMed] [Google Scholar]
- 34.Sheehan, B. J., J. T. Bosse, A. J. Beddek, A. N. Rycroft, J. S. Kroll, and P. R. Langford. 2003. Identification of Actinobacillus pleuropneumoniae genes important for survival during infection in its natural host. Infect. Immun. 71:3960-3970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shuman, S. 1994. Novel approach to molecular cloning and polynucleotide synthesis using vaccinia DNA topoisomerase. J. Biol. Chem. 269:32678-32684. [PubMed] [Google Scholar]
- 36.Slauch, J. M., M. J. Mahan, and J. J. Mekalanos. 1994. In vivo expression technology for selection of bacterial genes specifically induced in host tissues. Methods Enzymol. 235:481-492. [DOI] [PubMed] [Google Scholar]
- 37.Spinola, S. M., K. R. Fortney, B. P. Katz, J. L. Latimer, J. R. Mock, M. Vakevainen, and E. J. Hansen. 2003. Haemophilus ducreyi requires an intact flp gene cluster for virulence in humans. Infect. Immun. 71:7178-7182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Srikumar, R., L. G. Mikael, P. D. Pawelek, A. Khamessan, B. F. Gibbs, M. Jacques, and J. W. Coulton. 2004. Molecular cloning of haemoglobin-binding protein HgbA in the outer membrane of Actinobacillus pleuropneumoniae. Microbiology 150:1723-1734. [DOI] [PubMed] [Google Scholar]
- 39.St. Geme, J. W. I., D. Cutter, and S. J. Barenkamp. 1996. Characterization of the genetic locus encoding Haemophilus influenzae type b surface fibrils. J. Bacteriol. 178:6281-6287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Struve, C., C. Forestier, and K. A. Krogfelt. 2003. Application of a novel multi-screening signature-tagged mutagenesis assay for identification of Klebsiella pneumoniae genes essential in colonization and infection. Microbiology 149:167-176. [DOI] [PubMed] [Google Scholar]
- 41.van Ulsen, P., L. van Alphen, C. T. Hopman, A. van der Ende, and J. Tommassen. 2001. In vivo expression of Neisseria meningitidis proteins homologous to the Haemophilus influenzae Hap and Hia autotransporters. FEMS Immunol. Med. Microbiol. 32:53-64. [DOI] [PubMed] [Google Scholar]
- 42.Zeng, H., K. Pandher, and G. L. Murphy. 1999. Molecular cloning of the Pasteurella haemolytica pomA gene and identification of bovine antibodies against PomA surface domains. Infect. Immun. 67:4968-4973. [DOI] [PMC free article] [PubMed] [Google Scholar]


