Introduction
Oropharyngeal candidiasis (OPC) occurs in a diverse group of patients. Risk factors for OPC include the use of dentures, corticosteroid inhalers, cigarettes, broad-spectrum antibiotics, and immunosuppressive and chemotherapeutic agents. Patients with HIV, diabetes, and iatrogenic or autoimmune-induced dry mouth are also at substantial risk for OPC. This infection is caused primarily by Candida albicans, a ubiquitous polymorphic fungus that is part of the normal microbiota of the gastrointestinal and reproductive tracts of healthy individuals. In order to persistently colonize the oropharynx, C. albicans must adhere to the epithelial cell lining of the oral mucosa while avoiding being killed by host antimicrobial factors. OPC develops when local host defenses are weakened, permitting the fungus to invade and damage oral epithelial cells. The epithelial cells respond to fungal infection by secreting antimicrobial peptides that directly kill the fungus and by releasing pro-inflammatory cytokines that recruit neutrophils to the focus of infection, where they can kill C. albicans and limit the extent of epithelial cell damage [1,2]. In this Pearl, we summarize recent advances in our knowledge of the pathogenesis of OPC, focusing on fungal-epithelial interactions.
C. albicans Invades, Damages, and Stimulates Oral Epithelial Cells
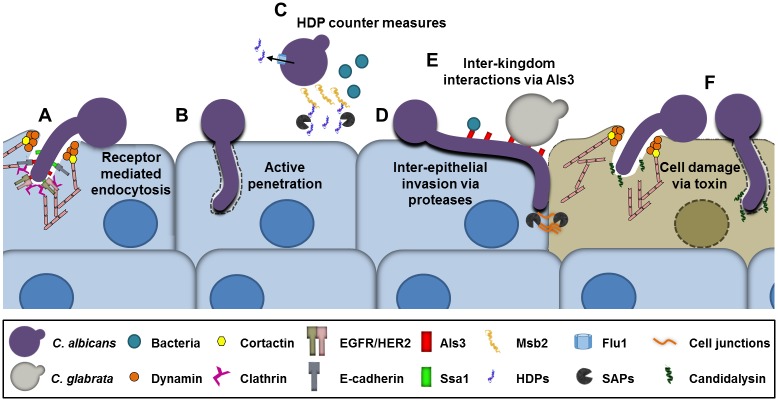
Although OPC is a superficial fungal infection, it is characterized by invasion of the epithelial cell lining of the oropharynx [3]. C. albicans can invade into oral epithelial cells by two distinct mechanisms, induced endocytosis and active penetration (Fig 1). During induced endocytosis, C. albicans hyphae express the Als3 [4] and Ssa1 [5] invasins, which bind to E-cadherin and a heterodimer composed of the epidermal growth factor receptor (EGFR) and HER2 on the epithelial cell surface [6] (Fig 1). These binding events trigger the clathrin-dependent endocytosis machinery and induce epithelial cells to produce pseudopods that engulf the fungus and pull it into the cell. Treatment of mice with a small molecule inhibitor of EGFR/HER2 reduces the severity of OPC, suggesting that induced endocytosis contributes to the pathogenesis of this infection [6]. Additional epithelial cell signaling pathways that are required for maximal endocytosis of C. albicans include the platelet-derived growth factor BB (PDGF BB) and neural precursor-cell-expressed developmentally down-regulated protein 9 (NEDD9) pathways. Activation of these signaling pathways requires C. albicans hyphal formation and expression of the Als3 invasin [7]. The relationship among these pathways and those activated by E-cadherin and EGFR/HER2 has not yet been determined.
Fig 1. Diagram of the interactions of Candida albicans with oral epithelial cells, host defense peptides (HDPs), and the oral microbiota.
(A) C. albicans invasion of epithelial cells by receptor-mediated endocytosis. The C. albicans Als3 and Ssa1 invasins interact with E-cadherin and a heterodimer composed of the epidermal growth factor receptor (EGFR) and HER2, which activate the clathrin endocytosis pathway, resulting in the endocytosis of the fungus. (B) C. albicans invasion by active penetration, in which a progressively elongating hyphus pushes its way into the epithelial cell. (C) Host defense peptides (HDPs) released by the infected epithelial cell can kill C. albicans. However, C. albicans can resist HDPs by up-regulating the Flu1 efflux pump, which reduces intracellular HDPs, by secreting aspartyl proteases (SAPs), which degrade HDPs, and by shedding of the Msb2 mucin, which binds to and inactivates HDPs. (D) C. albicans can invade between oral epithelial cells by proteolytic degradation of intercellular junctional proteins. (E) C. albicans hyphae bind Candida glabrata and bacteria such as Staphylococcus aureus and Streptococcus spp. C. albicans can enhance the capacity of some of these organisms to invade epithelial cells, while some of these organisms can increase the virulence of C. albicans. (F) C. albicans secretes candidalysin, a toxin that causes epithelial damage.
Active penetration occurs when elongating C. albicans hyphae physically push their way into the epithelial cell (Fig 1) [8]. While it is likely that both induced endocytosis and active penetration occur during OPC, it has been difficult to determine the role of active penetration in the pathogenesis of OPC because most invasins are hyphal specific. Thus, C. albicans mutants that do not form hyphae also fail to express invasins and, consequently, are defective in both active penetration and induced endocytosis.
C. albicans can also penetrate epithelial cell barriers via a paracellular route by secreting lytic enzymes such as members of the secreted aspartyl proteinase (SAP) family. These proteases degrade E-cadherin and other inter-epithelial cell junctional proteins, enabling the organism to penetrate between epithelial cells [9] (Fig 1). Recently, it has been found that C. albicans infection also stimulates the activity of epithelial cell calpain, a cysteine protease that degrades E-cadherin. Moreover, calpain activity is dramatically enhanced in epithelial cells that are co-infected with C. albicans and Streptococcus oralis [10].
When C. albicans invades epithelial cells, it damages them. Epithelial cells in turn respond to C. albicans by secreting proinflammatory cytokines and antimicrobial peptides. Recently, it was discovered that C. albicans-induced epithelial cell damage is mainly caused by candidalysin, a toxin released by the fungus (Fig 1). Candidalysin is encoded by the hyphal-specific gene ECE1. The protein is cleaved by the Kex2 protease into eight peptides, of which only one permeabilizes epithelial cell membranes, induces epithelial cell damage, and stimulates epithelial cell cytokine secretion. A C. albicans ece1Δ/Δ deletion mutant is defective in damaging and stimulating oral epithelial cells in vitro. Furthermore, it has a greatly attenuated virulence in the mouse model of OPC [11]. Thus, candidalysin and epithelial cell damage play a central role in the pathogenesis of OPC.
Although the presence of candidalysin is required to induce a maximal epithelial cell response to C. albicans, binding of yeast, yeast lysates, and Als3 to epithelial cells is sufficient to induce some epithelial cell responses even in the absence of this toxin. For example, contact with C. albicans yeast cells, which do not secrete candidalysin, stimulates phosphorylation of the Akt serine/threonine kinase within 5 minutes [12]. In addition, lysates of yeast cells induce secretion of IL-8, possibly by interacting with intercellular adhesion molecule-1 (ICAM-1) [13]. Finally, Saccharomyces cerevisiae cells expressing the Als3 invasin stimulate the phosphorylation of EGFR and HER2 within 20 minutes [6]. These data suggest that oral epithelial cells sense and respond to contact with C. albicans, and that this initial response is subsequently amplified by candidalysin. While EGFR/HER2 and E-cadherin interact with C. albicans hyphae, the epithelial cell receptor(s) that is activated by yeast-phase C. albicans is currently unknown.
Interplay between Epithelial Cell-Derived Antimicrobial Peptides and C. albicans
Host defense peptides (HDPs) represent one of the first lines of defense against invading microbes. Epithelial cells release multiple types of HDPs, including β-defensins and cathelicidins, that either kill or inhibit the growth of C. albicans. Different HDPs have different mechanisms of action, and their targets include the fungal cell membrane and mitochondria [14]. HDPs that are highly expressed during the early stage of OPC in mice include murine β-defensin 1 (mBD1), β-defensin 3 (the homolog of human β-defensin 2), and the alarmins S100A8 and S100A9 [15]. The importance of epithelial cell–derived HDPs in the host defense against OPC is demonstrated by finding that mBD1-deficient mice develop severe OPC, even in the absence of immunosuppression [16]. By contrast, immunocompetent wild-type mice are resistant to OPC, and when orally inoculated with C. albicans, clear the infection within 2–3 days. Mice that are deficient in either IL-17 receptor A (IL-17RA) or IL-17RC fail to up-regulate HDPs in the oral epithelium in response to C. albicans infection and are highly susceptible to OPC [1,15]. Recently, it was shown that mice with oral epithelial cell specific deletion of IL-17RA have reduced expression of Defb3 (encoding β-defensin 3) in the oral mucosa and increased susceptibility to OPC. This increased susceptibility is phenocopied by deletion of Defb3 [17]. Finally, people with mutations in signal transducer and activator of transcription 3 (STAT3) fail to mount a Th17 response, have significantly reduced salivary β-defensin 2 and histatins, and suffer from chronic mucocutaneous candidiasis [18]. Collectively, these data indicate that the response of oral epithelial cells to C. albicans, especially the production of HDPs, contributes to the host defense against OPC.
When C. albicans colonizes the oral mucosa of healthy individuals and causes OPC in patients, it must be able to withstand HDPs. The fungus has evolved multiple different mechanisms that enable it to evade the deleterious effects of HDPs and persist in the oral cavity [14]. These mechanisms include shedding of the Msb2 mucin, which binds to and inactivates HDPs, and secretion of aspartyl proteases, which break down HDPs [19,20,21] (Fig 1). C. albicans also expresses the Flu1 efflux pump that reduces intracellular HDP levels [22].
Exposure to HDPs induces a stress response in C. albicans, and susceptibility to HDPs is governed in part by the signaling pathways that are activated in response to these peptides. Activation of the high-osmolarity-glycerol (HOG) pathway enables C. albicans to resist histatin 5 and human β-defensins 2 and 3 [23,24]. The Ssd1 RNA-binding protein acts in part through the Bcr1 transcription factor to mediate resistance to human β-defensin 2 [25,26]. Conversely, activation of the Cek1 mitogen-activated protein kinase (MAPK) enhances surface exposure of β-1,3-glucans, elevating the uptake of histatin 5 and increasing sensitivity to this HDP [27].
Co-infection with C. albicans and Other Microorganisms Influences Virulence during OPC
C. albicans is frequently isolated from the oral cavity in conjunction with other microbial pathogens. In a study of AIDS patients with OPC [28], 107 out of 1,106 episodes of infection (9.7%) were caused by more than one species of Candida. Among the subjects with multispecies OPC, C. albicans plus C. glabrata (68.2%) was the most common co-infection, followed by C. albicans plus C. tropicalis (15.0%) and C. albicans plus C. glabrata plus C. tropicalis (8.4%). These epidemiological data suggest that C. glabrata has unique characteristics that facilitate co-infection with C. albicans.
Silva et al. [29] reported that C. glabrata is unable to invade reconstituted human oral epithelium in vitro and causes minimal epithelial cell damage. A potential explanation for this finding is that C. glabrata grows only as yeast in vivo and does not form hyphae at foci of infection. However, when oral epithelial cells are infected with a mixture of C. glabrata and C. albicans, the C. glabrata cells bind to C. albicans hyphae and are carried deeper into the epithelium, where they cause extensive epithelial cell damage (Fig 1). It was recently reported that C. glabrata alone is not able to cause disease in a mouse model of OPC. However, when mice are inoculated with a mixture of C. albicans and C. glabrata, they develop more severe disease than mice infected with C. albicans alone [30]. This synergistic infection requires the expression of the Als1 and Als3 adhesins/invasins by the C. albicans hyphae. Multiple C. glabrata adhesins, including Epa8, Epa19, Awp2, Awp7, and CAGL0F00181, mediate adherence to C. albicans hyphae; whether they interact specifically with C. albicans Als1 and/or Als3 remains to be determined [30]. Collectively, these results provide an explanation for the frequent co-isolation of C. glabrata and C. albicans in patients with OPC. Although C. tropicalis can occasionally cause OPC in conjunction with C. albicans, the mechanistic basis for this co-infection is currently unknown.
Co-infection with C. albicans can also augment infection with S. aureus. When mice are immunosuppressed with cortisone acetate and then orally inoculated with S. aureus, the bacteria persist in the oral cavity in relatively low numbers and do not cause detectable disease [31]. However, when mice with OPC due to C. albicans are orally inoculated with S. aureus, the bacteria adhere to the fungal hyphae, which transport the bacteria along with them as they invade into the superficial oral epithelium. Not only does the presence of C. albicans result in higher levels of S. aureus in the oral cavity but it also enables S. aureus to invade the oral mucosa and cause a fatal hematogenously disseminated infection. This pathologic interaction between S. aureus and C. albicans is dependent on Als3; even though an als3Δ/Δ null mutant is still able to cause OPC, S. aureus co-infection does not result in a disseminated staphylococcal infection [31]. Although OPC is not known to be associated with disseminated staphylococcal infection in patients, it is possible that the interaction of S. aureus with C. albicans at other anatomic sites, such as the gastrointestinal tract or peritoneal cavity [32], might facilitate the development of S. aureus bacteremia.
C. albicans is also known to interact with common oral commensal bacteria. In vitro studies demonstrate that Streptococcus gordonii and C. albicans co-adhere during mixed-species biofilm formation [33]. This interaction is mediated by the S. gordonii cell wall-anchored proteins SspA and SspB and the C. albicans surface proteins Als3, Eap1, and Hwp1. The presence of S. gordonii enhances C. albicans hyphal development and increases biofilm mass [33,34,35]; whether it also augments C. albicans virulence during OPC is currently unknown. Co-infection with Streptococcus mutans also increases C. albicans biofilm formation in vitro. However, Galleria mellonella larvae infected with both organisms have prolonged survival compared to larvae infected with C. albicans alone. This reduction in virulence is likely due to inhibition of fungal hyphal formation by the bacteria [36]. By contrast, Streptococcus oralis both augments C. albicans biofilm formation in vitro and increases virulence during experimental OPC in mice, as manifested by increased size of the oral lesions and greater fungal dissemination to distal organs [37,38]. These data demonstrate that the interaction of C. albicans with the oral microbiota has the potential to significantly influence the pathogenesis of OPC.
Conclusions and Perspective
The oral epithelium is a critical component of the host defense against OPC. However, C. albicans has evolved multiple strategies to breach the epithelial cell barrier, withstand HDPs, and cause a superficial infection. In mouse models of infection, other microbial pathogens can interact with C. albicans and alter virulence. This pathogenic interaction is undoubtedly relevant to human infection in the case of C. glabrata and streptococci because these organisms are commonly isolated in conjunction with C. albicans. Whether mucosal infection with C. albicans predisposes patients to develop invasive staphylococcal infections is currently unknown but is clearly worthy of investigation.
Acknowledgments
We would like to thank the students and faculty of the molecular mycology course “Current Approaches to Fungal Pathogenesis,” who stimulated us to write this Pearl.
Funding Statement
MS and SGF were supported in part by NIH grant R01AI124566. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Trautwein-Weidner K, Gladiator A, Nur S, Diethelm P, LeibundGut-Landmann S (2015) IL-17-mediated antifungal defense in the oral mucosa is independent of neutrophils. Mucosal Immunol 8: 221–231. 10.1038/mi.2014.57 [DOI] [PubMed] [Google Scholar]
- 2.Weindl G, Naglik JR, Kaesler S, Biedermann T, Hube B, et al. (2007) Human epithelial cells establish direct antifungal defense through TLR4-mediated signaling. J Clin Invest 117: 3664–3672. 10.1172/JCI28115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montes LF, Wilborn WH (1968) Ultrastructural features of host-parasite relationship in oral candidiasis. J Bacteriol 96: 1349–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phan QT, Myers CL, Fu Y, Sheppard DC, Yeaman MR, et al. (2007) Als3 is a Candida albicans invasin that binds to cadherins and induces endocytosis by host cells. PLoS Biol 5: e64 10.1371/journal.pbio.0050064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun JN, Solis NV, Phan QT, Bajwa JS, Kashleva H, et al. (2010) Host cell invasion and virulence mediated by Candida albicans Ssa1. PLoS Pathog 6: e1001181 10.1371/journal.ppat.1001181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu W, Phan QT, Boontheung P, Solis NV, Loo JA, et al. (2012) EGFR and HER2 receptor kinase signaling mediate epithelial cell invasion by Candida albicans during oropharyngeal infection. Proc Natl Acad Sci U S A 109: 14194–14199. 10.1073/pnas.1117676109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Shetty AC, Schwartz JA, Bradford LL, Xu W, et al. (2015) New signaling pathways govern the host response to C. albicans infection in various niches. Genome Res 25: 679–689. 10.1101/gr.187427.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wachtler B, Citiulo F, Jablonowski N, Forster S, Dalle F, et al. (2012) Candida albicans-epithelial interactions: dissecting the roles of active penetration, induced endocytosis and host factors on the infection process. PLoS ONE 7: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villar CC, Kashleva H, Nobile CJ, Mitchell AP, Dongari-Bagtzoglou A (2007) Mucosal tissue invasion by Candida albicans is associated with E-cadherin degradation, mediated by transcription factor Rim101p and protease Sap5p. Infect Immun 75: 2126–2135. 10.1128/IAI.00054-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu H, Sobue T, Bertolini M, Thompson A, Dongari-Bagtzoglou A (2016) Streptococcus oralis and Candida albicans synergistically activate m-calpain to degrade E-cadherin from oral epithelial junctions. J Infect Dis 214: 925–934. 10.1093/infdis/jiw201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moyes DL, Wilson D, Richardson JP, Mogavero S, Tang SX, et al. (2016) Candidalysin is a fungal peptide toxin critical for mucosal infection. Nature 532: 64–68. 10.1038/nature17625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moyes DL, Shen C, Murciano C, Runglall M, Richardson JP, et al. (2014) Protection against epithelial damage during Candida albicans infection is mediated by PI3K/Akt and mammalian target of rapamycin signaling. J Infect Dis 209: 1816–1826. 10.1093/infdis/jit824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egusa H, Nikawa H, Makihira S, Yatani H, Hamada T (2006) In vitro mechanisms of interleukin-8-mediated responses of human gingival epithelial cells to Candida albicans infection. Int J Med Microbiol 296: 301–311. 10.1016/j.ijmm.2005.12.017 [DOI] [PubMed] [Google Scholar]
- 14.Swidergall M, Ernst JF (2014) Interplay between Candida albicans and the antimicrobial peptide armory. Eukaryot cell 13: 950–957. 10.1128/EC.00093-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conti HR, Shen F, Nayyar N, Stocum E, Sun JN, et al. (2009) Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. J Exp Med 206: 299–311. 10.1084/jem.20081463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tomalka J, Azodi E, Narra HP, Patel K, O’Neill S, et al. (2015) β-Defensin 1 plays a role in acute mucosal defense against Candida albicans. J Immunol 194: 1788–1795. 10.4049/jimmunol.1203239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conti Heather R, Bruno Vincent M, Childs Erin E, Daugherty S, Hunter Joseph P, et al. (2016) IL-17 Receptor signaling in oral epithelial cells is critical for protection against oropharyngeal candidiasis. Cell Host Microbe 20: 606–617. 10.1016/j.chom.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conti HR, Baker O, Freeman AF, Jang WS, Holland SM, et al. (2011) New mechanism of oral immunity to mucosal candidiasis in hyper-IgE syndrome. Mucosal Immunol 4: 448–455. 10.1038/mi.2011.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Szafranski-Schneider E, Swidergall M, Cottier F, Tielker D, Roman E, et al. (2012) Msb2 shedding protects Candida albicans against antimicrobial peptides. PLoS Pathog 8: e1002501 10.1371/journal.ppat.1002501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swidergall M, Ernst AM, Ernst JF (2013) Candida albicans mucin Msb2 is a broad-range protectant against antimicrobial peptides. Antimicrob Agents Chemother 57: 3917–3922. 10.1128/AAC.00862-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rapala-Kozik M, Bochenska O, Zawrotniak M, Wolak N, Trebacz G, et al. (2015) Inactivation of the antifungal and immunomodulatory properties of human cathelicidin LL-37 by aspartic proteases produced by the pathogenic yeast Candida albicans. Infect Immun 83: 2518–2530. 10.1128/IAI.00023-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li R, Kumar R, Tati S, Puri S, Edgerton M (2013) Candida albicans flu1-mediated efflux of salivary histatin 5 reduces its cytosolic concentration and fungicidal activity. Antimicrob Agent Chemother 57: 1832–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Argimon S, Fanning S, Blankenship JR, Mitchell AP (2011) Interaction between the Candida albicans high-osmolarity glycerol (HOG) pathway and the response to human beta-defensins 2 and 3. Eukaryot Cell 10: 272–275. 10.1128/EC.00133-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vylkova S, Jang WS, Li W, Nayyar N, Edgerton M (2007) Histatin 5 initiates osmotic stress response in Candida albicans via activation of the Hog1 mitogen-activated protein kinase pathway. Eukaryot Cell 6: 1876–1888. 10.1128/EC.00039-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jung SI, Finkel JS, Solis NV, Chaili S, Mitchell AP, et al. (2013) Bcr1 functions downstream of Ssd1 to mediate antimicrobial peptide resistance in Candida albicans. Eukaryot Cell 12: 411–419. 10.1128/EC.00285-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gank KD, Yeaman MR, Kojima S, Yount NY, Park H, et al. (2008) SSD1 is integral to host defense peptide resistance in Candida albicans. Eukaryot Cell 7: 1318–1327. 10.1128/EC.00402-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li R, Puri S, Tati S, Cullen PJ, Edgerton M (2015) Candida albicans Cek1 mitogen-activated protein kinase signaling enhances fungicidal activity of salivary histatin 5. Antimicrob Agents Chemother 59: 3460–3468. 10.1128/AAC.00214-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldman M, Cloud GA, Wade KD, Reboli AC, Fichtenbaum CJ, et al. (2005) A randomized study of the use of fluconazole in continuous versus episodic therapy in patients with advanced HIV infection and a history of oropharyngeal candidiasis: AIDS Clinical Trials Group Study 323/Mycoses Study Group Study 40. Clin Infect Dis 41: 1473–1480. 10.1086/497373 [DOI] [PubMed] [Google Scholar]
- 29.Silva S, Henriques M, Hayes A, Oliveira R, Azeredo J, et al. (2011) Candida glabrata and Candida albicans co-infection of an in vitro oral epithelium. J Oral Pathol Med 40: 421–427. 10.1111/j.1600-0714.2010.00981.x [DOI] [PubMed] [Google Scholar]
- 30.Tati S, Davidow P, McCall A, Hwang-Wong E, Rojas IG, et al. (2016) Candida glabrata binding to Candida albicans hyphae enables Its development in oropharyngeal candidiasis. PLoS Pathog 12: e1005522 10.1371/journal.ppat.1005522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schlecht LM, Peters BM, Krom BP, Freiberg JA, Hansch GM, et al. (2015) Systemic Staphylococcus aureus infection mediated by Candida albicans hyphal invasion of mucosal tissue. Microbiology 161: 168–181. 10.1099/mic.0.083485-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nash EE, Peters BM, Palmer GE, Fidel PL, Noverr MC (2014) Morphogenesis is not required for Candida albicans-Staphylococcus aureus intra-abdominal infection-mediated dissemination and lethal sepsis. Infect Immun 82: 3426–3435. 10.1128/IAI.01746-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bamford CV, d'Mello A, Nobbs AH, Dutton LC, Vickerman MM, et al. (2009) Streptococcus gordonii modulates Candida albicans biofilm formation through intergeneric communication. Infect Immun 77: 3696–3704. 10.1128/IAI.00438-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bamford CV, Nobbs AH, Barbour ME, Lamont RJ, Jenkinson HF (2015) Functional regions of Candida albicans hyphal cell wall protein Als3 that determine interaction with the oral bacterium Streptococcus gordonii. Microbiology 161: 18–29. 10.1099/mic.0.083378-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nobbs AH, Vickerman MM, Jenkinson HF (2010) Heterologous expression of Candida albicans cell wall-associated adhesins in Saccharomyces cerevisiae reveals differential specificities in adherence and biofilm formation and in binding oral Streptococcus gordonii. Eukaryot Cell 9: 1622–1634. 10.1128/EC.00103-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barbosa JO, Rossoni RD, Vilela SF, de Alvarenga JA, Velloso Mdos S, et al. (2016) Streptococcus mutans can modulate biofilm formation and attenuate the virulence of Candida albicans. PLoS ONE 11: e0150457 10.1371/journal.pone.0150457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu H, Sobue T, Thompson A, Xie Z, Poon K, et al. (2014) Streptococcal co-infection augments Candida pathogenicity by amplifying the mucosal inflammatory response. Cell Microbiol 16: 214–231. 10.1111/cmi.12216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bertolini MM, Xu H, Sobue T, Nobile CJ, Del Bel Cury AA, et al. (2015) Candida-streptococcal mucosal biofilms display distinct structural and virulence characteristics depending on growth conditions and hyphal morphotypes. Mol Oral Microbiol 30: 307–322. 10.1111/omi.12095 [DOI] [PMC free article] [PubMed] [Google Scholar]