The increase in antibiotic resistance is one of the most worrying trends facing 21st century medicine. Much antibiotic prescribing is of little therapeutic value, and lower prescribing rates may lead to lower rates of resistance.w1 Consequently, doctors are being encouraged to use antibiotics less frequently. However, lower levels of antibiotic prescribing may lead to an increase in complications from infectious diseases.w2 We analysed NHS primary care prescribing data in England to examine the number of antibiotic prescriptions per 1000 population (STAR-PU weighted) between 1996 and 2002, as well as the standardised hospital admission rate for respiratory tract infections during the same period.
The bottom line
• A sustained decrease in community antibiotic prescribing rates in recent years has been associated with a smaller corresponding increase in admission rates for respiratory tract infections
We examined NHS primary care prescribing data and hospital admissions data for respiratory tract infections in England for the period 1996-2002.w3 To account for differences in demography between primary care trusts, we weighted populations by specific therapeutic group age-sex weightings related prescribing units (STAR-PUs).w4 Information on admissions came from hospital episode statistics. To avoid double counting of diagnoses, we used admissions rather than consultant episodes as the numerator in the calculation of annual standardised admission ratios.
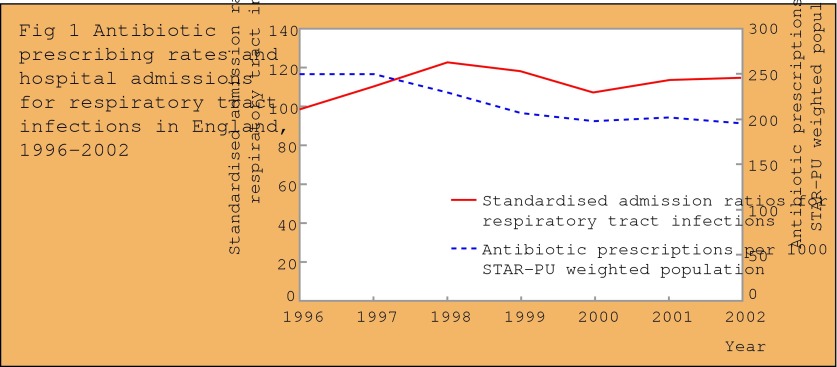
We found that prescriptions of antibiotics decreased from 254 to 196 per 1000 STAR-PU weighted population between 1996 and 2002. The standardised admission ratio for respiratory tract infections increased from a baseline of 100 in 1996 to 123 in 1998 before declining to 115 in 2002 (fig 1).
Figure 1.
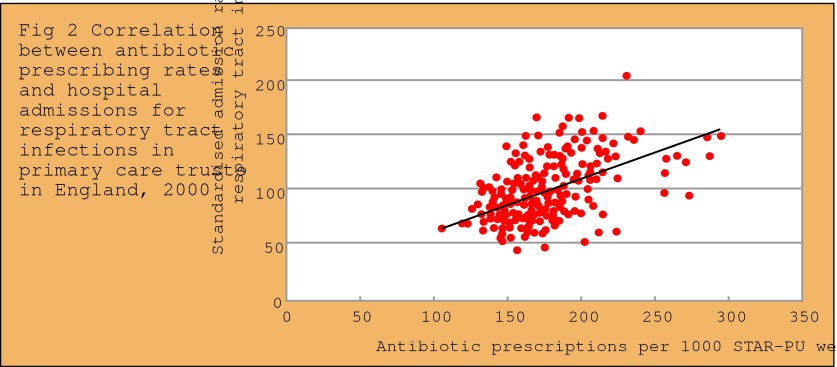
Primary care trusts in England showed a nearly threefold variation in antibiotic prescribing rates in 2000, from 105.3 to 295.8 prescriptions per 1000 STAR-PU weighted population. Standardised admission ratios for respiratory tract infections varied more than fourfold, from 45 to 204 in the same year. Prescription rates showed a significant correlation with standardised admission ratios (Spearman's correlation coefficient 0.51, P < 0.001) (fig 2). Hence, at primary care trust level, lower prescribing rates were not associated with higher admission rates.
Figure 2.
The positive association between prescribing and admissions may reflect variations in underlying socioeconomic, environmental and medical factors that influence the likelihood of developing a respiratory tract infection severe enough to lead to hospital admission. Some of the variation may also be due to general practitioners' propensity to refer patients to hospitals and differences in hospital admission policies. Finally, not all the antibiotic prescribing will have been for respiratory tract infections; some will have been for other indications such as urinary tract infections.
The large local variation in antibiotic prescribing rates may reflect the difficulties faced by general practitioners in treating patients with infectious diseases in the community without the benefit of immediately available investigations that could help identify the more serious cases.w5 This problem is particularly apparent with lower respiratory tract infections, when even careful clinical examination is not sufficient to detect many patients with radiological evidence of pneumonia.w6 Finally, the national findings are equivocal on the question of whether lower antibiotic prescribing rates lead to an increase in adverse population outcomes such as admission rates for respiratory tract infections. There was an initial increase in admission rates between 1996 and 1998, followed by a slight decline. Hence, this subject would benefit from further investigation.
Supplementary Material
 Dr Foster's case notes was compiled by Azeem Majeed, Susan Williams, Brian Jarman, and Paul Aylin at the Dr Foster Unit at Imperial College. Dr Foster is an independent research and publishing organisation created to examine measures of clinical performance.
Dr Foster's case notes was compiled by Azeem Majeed, Susan Williams, Brian Jarman, and Paul Aylin at the Dr Foster Unit at Imperial College. Dr Foster is an independent research and publishing organisation created to examine measures of clinical performance.
 References and full methodological details are on bmj.com and drfoster.com
References and full methodological details are on bmj.com and drfoster.com
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.