Short abstract
A new international classification system for kidney problems is currently being developed. How can it meet the challenges of avoiding labelling all patients with low function as having kidney disease and being usable in countries with limited resources?
Patients with low kidney function may eventually need dialysis or transplantation and can die if these treatments are declined or not available. Early intervention is required to prevent these severe outcomes. Interventions that reduce the rate of loss of kidney function have been shown to be effective in selected patient groups. However, mild to moderate low kidney function is prevalent and often unrecognised in the general population, particularly in elderly people. An internationally accepted classification scheme for kidney problems is needed to facilitate research, clinical management, and the development of health policy.
Importance of kidney disease
End stage renal disease, defined as kidney function so low that dialysis or transplantation is needed, currently affects 404-1022 people per million population in Europe.1 The burden is large for both patients, whose quality of life and life expectancy are impaired,2 and society because of the high cost of renal replacement therapy.3
Low kidney function refers to abnormalities in clearance of uraemic toxins, often assessed as creatinine clearance or glomerular filtration rate. Low clearance, or low glomerular filtration rate, is commonly known as chronic renal failure. The term chronic renal insufficiency is also widely used; it may have been coined to reduce the apparent severity of this diagnosis. A standard definition does not exist for either term.4
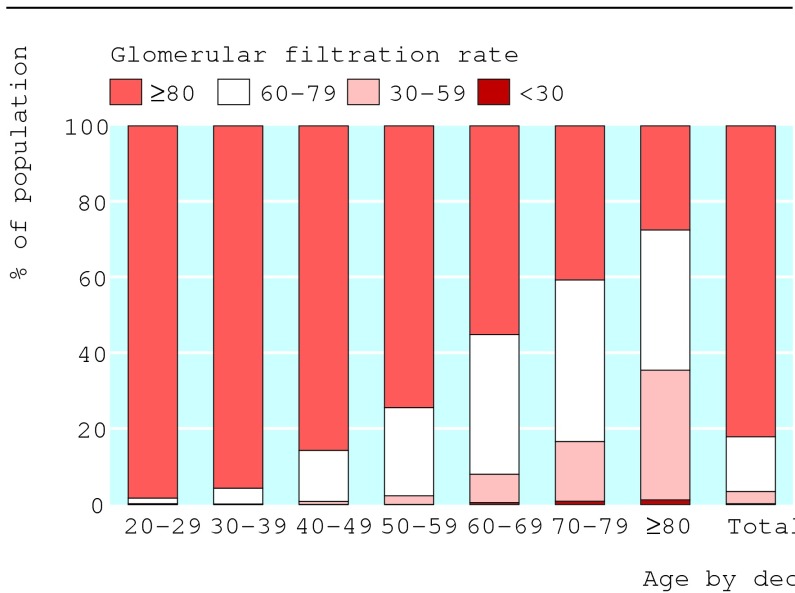
Our understanding of the progression of low glomerular filtration rate derives from observational studies and randomised trials conducted in patients referred for specialist care; these have shown falls in glomerular filtration rate of about 7 to 8 ml/min.5 Until recently it was assumed that all patients with low glomerular filtration would continue to lose function and develop end stage renal disease within about 10 to 20 years. A creatinine clearance of 150 ml/min (standard deviation 20 ml/min) is generally considered normal for men aged 20-30, and longitudinal studies of ageing show that clearance falls by 0.75 ml/min a year.6 On this basis, average clearances of 90-100 ml/min are expected in healthy elderly people. However, recent analyses of data from the third national health and nutrition survey (NHANES III)—a population based survey conducted in the United States—have shown that raised creatinine concentration7 w1 w2 and low glomerular filtration rate7-10 w2 are prevalent, especially in elderly people (figure).
Figure 1.
Weighted distribution of predicted glomerular filtration rate by the modification of diet in renal diseases equation, by age (in decades), for non-diabetic adults in third national health and nutrition examination survey. (Estimates are calculated after subtraction of 20.3 μmol/l from serum creatinine concentration to account for differences between White Sands and Cleveland clinic laboratories). Values are given in ml/min/1.73 m2. Modified from Clase et al9
This unexpected finding generated controversy in the nephrology community. Some argued that since the incidence of end stage renal failure is increasing rapidly in most developed counties, the high prevalence of low glomerular filtration rate represents an epidemic of chronic kidney disease. This led to recommendations that people with low glomerular filtration rate should be aggressively identified and treated.7 However, a large disparity exists between the prevalence of low kidney function and that of end stage renal failure and large differences are also seen in the prevalence of proteinuria in studies of referred patients and community studies. We therefore believe it is unlikely that low glomerular filtration rate always carries the same prognosis.9 Recent data on the rate of progression in unreferred patients with low glomerular filtration rate has confirmed this hypothesis.11 Thus current evidence suggests low glomerular filtration rate should not always be considered a disease. In addition, because the evidence for differential management of low glomerular filtration rate is limited to highly selected patient groups,12,13 further data are needed before recommendations for health policy can be made.8 w3
Classification of kidney disease
In February 2002, the US National Kidney Foundation's Kidney Disease Quality Initiative published a series of recommendations for the identification and management of people with low glomerular filtration rate. A classification system for chronic kidney disease based on glomerular filtration rate, urinary and anatomic abnormities is an integral part of this document (table 1).7
Table 1.
US National Kidney Foundation Kidney Disease Quality Outcomes Initiative classification of stages of chronic kidney disease7
| Stage | Description | Glomerular filtration rate in ml/min/1.73 m2 |
|---|---|---|
| 1 |
Kidney damage with normal or high GFR |
≥90 |
| 2 |
Kidney damage with slightly low GFR |
60-89 |
| 3 |
Moderately low GFR |
30-59 |
| 4 |
Severe low GFR |
15-29 |
| 5 | Kidney failure | <15 or dialysis |
GFR=glomerular filtration rate.
Chronic kidney disease is defined as either kidney damage or glomerular filtration rate <60 ml/min/1.73m2 for ≥3 months. Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.
Since then, the classification scheme has been adopted by some US researchersw4 and criticised by others.w5 In 2004, the Kidney Disease: Improving Global Outcomes Initiative was formed, with equal representation from Europe, North and South America, Africa, and Asia. The initiative includes a working group on evaluation and classification of chronic kidney disease, the goal of which is: “To adopt a common evaluation and classification of chronic kidney disease. To facilitate the adoption of a common nomenclature worldwide.” Below we suggest some changes to the existing classification system that would help meet this goal.
Terminology
The current US classification is one of “chronic kidney disease.” However, chronicity, a function of time, could better be considered an optional separate dimension. This would allow the classification to be used in non-chronic situations and in cross sectional studies in which chronicity cannot be established. Individual observational data sets and specific clinical questions will require different definitions of chronicity. The classification could suggest a definition of chronicity for use in prospective studies (for example, based on two measurements at least three months apart), but it need not be prescriptive.
The word “kidney,” however, is an excellent choice and likely to convey more information than alternatives such as renal. In other languages, the word chosen should similarly be based on common usage.
Figure 2.

Recent evidence suggests not all patients with low kidney function require treatment to prevent end stage disease
Credit: SIMON FRASER/RVI, NEWCASTLE
The word “disease” presents more problems. It is defined in the Oxford English Dictionary as “A condition of the body, or of some part or organ of the body, in which its functions are disturbed or deranged; a morbid physical condition; a departure from the state of health, especially when caused by structural change.” The word carries connotations that we believe are out of keeping with our current knowledge about many kinds of kidney problems. For example, cut-off points distinguishing abnormal from normal glomerular filtration rate at the upper end of the scale are highly debatable, even kidney function that is indubitably abnormal often does not cause ill health, and proteinuria is only a disease when it leads to symptomatic nephrotic syndrome. Low glomerular filtration rate is a risk factor for severe complicated kidney failure and end stage renal disease14 and may be a causal risk factor for cardiovascular events15; however, it remains a risk factor, and not a disease. A clinically useful classification scheme must consider and minimise the possibility of labelling effects that might influence psychosocial wellbeing and insurability16 and must avoid the promotion of disease to people who do not have symptoms (disease mongering).17
Measurement of kidney health
The principle dimensions of kidney health are glomerular filtration rate and proteinuria: their consequences are different and independent.18,19 Proteinuria should be included in the classification, but separately from glomerular filtration rate so that the two scales can be used alone or in combination. A lay term is needed for the glomerular filtration rate; we suggest using kidney function. The whole system could be described as a classification of kidney problems or perhaps (somewhat euphemistically) a classification of kidney health.
Because several methods of assessment are available, we suggest that the new classification scheme be inclusive, allowing kidney function to be defined by any valid method—for example, the Cockcroft-Gault formula,w7 the modification of diet in renal diseases equation,7 w8 w9 the cut-off points defined by Couchoud,w11 or 24 hour urine creatinine clearance. It is not necessary to specify whether these values should be normalised for body surface area. It is the researcher's responsibility to determine the best method for a particular study, which depends on the scientific question being addressed.
End stage renal disease
End stage renal disease (requirement for dialysis or transplantation) does not fit happily within the lowest category of glomerular filtration rate in the US classification.7 We suggest that haemodialysis, peritoneal dialysis, and transplantation be regarded as additional separate categories, although patients with functioning transplants could be further categorised using the kidney function and proteinuria dimensions of the scale. We would add further categories for patients who would benefit from renal replacement therapy but are not receiving it because of a doctor's recommendation or for personal or economic reasons. This would allow researchers to distinguish patients with very low glomerular filtration rate who do not yet require dialysis from those who are pursuing a palliative or conservative care.
Proteinuria
Proteinuria is a strong predictor of end stage renal disease14 and cardiovascular events.20 As with the assessment of kidney function, no single method of assessing proteinuria will satisfy all needs. However, the creation of a five or six point scale for proteinuria (from no proteinuria to full nephrotic syndrome) and suggested cut-off points for results of random or morning urine dipstick tests, albumin:creatinine ratio, and timed urine measurements (such as 24 hour total albumin or protein), together with a summary of available evidence for the equivalence of the chosen cut-off points,w12 would be useful. Inclusion of dipstick test for proteinuria as an option would be particularly helpful for mass screening and in resource constrained environments. Cut-off points will not be exactly equivalent from measure to measure.
What other dimensions are important?
Blood pressure, diabetic status, age, race, aetiology of kidney disease, and structural abnormalities are all important in predicting progression. However, classification systems for these variables already exist and can be combined with one or both dimensions of the kidney classification proposed here as needed.
Stages or groups?
We believe the word “stage” (Oxford English Dictionary: “A period of development, a degree of progress, a step in a process”) implies more about the inevitability of progression than we currently know. We would prefer a less value laden word such as group to describe the ordinal categories in each dimension. A numbering or lettering system would be helpful because it permits brief reference to a category. We suggest using numbers for glomerular filtration rate groups and letters for degree of proteinuria (table 2). We have used a cut-off point of 80 ml/min rather than 90 ml/min as the division between the referent category and other categories for glomerular filtration rate. This is because our bias is towards conservatism and avoidance of labelling. If 80 ml/min is used, the sex specific cut-off points defined by Couchoudw11 are an option for classifying patients when only the serum creatinine is known. Researchers who need a finer classification system than that defined by the cut-off points we propose should use bands of 5-10 ml/min for glomerular filtration rate to subdivide their participants further.
Table 2.
Skeleton for a suggested classification of kidney health classification using Cockcroft-Gault calculation of creatinine clearance and dipstick evaluation of proteinuria. The same framework could be used with any other validated measures of clearance and albuminuria or proteinuria
|
Proteinuria |
|||||||
|---|---|---|---|---|---|---|---|
| Group | Kidney function (ml/min/1.73 m2) | a (negative) | b (trace) | c (1+) | d (2+) | e*(3+) | f*(nephrotic syndrome) |
| 1 |
≥80 |
||||||
| 2 |
60-79 |
||||||
| 3 |
30-59 |
||||||
| 4 |
15-29 |
||||||
| 5* |
<15, not requiring renal replacement therapy |
||||||
| 6* |
<15, renal replacement therapy offered but declined |
||||||
| 7* |
<15, might benefit from renal replacement therapy but pursuing conservative treatment on medical advice |
||||||
| 8* |
<15, requiring, but not receiving, renal replacement therapy because of resource constraints or lack of availability |
||||||
| HD |
Haemodialysis |
||||||
| PD |
Peritoneal dialysis |
||||||
| T | Transplantation† | ||||||
When data are not available, categories can be collapsed. For example, if information about clinical nephrotic syndrome is not available, proteinuria groups e and f would be reported together as group e-f.
Patients with functioning renal transplants can be further classified into the clearance and protein categories described above (eg, T3c would represent transplanted patients with clearance of 30-59 ml/min/1.73 m2 and 1+ proteinuria).
Importance of progression
The classification scheme we propose provides a snapshot of kidney health at an instant or over a few months. Previous progression is likely to be a strong predictor of future progression, though direct data to support this hypothesis are not, to our knowledge, available. Because we do not know the relation between past and future progression or whether threshold effects are present (that is, whether there is a rate of loss of glomerular filtration rate above which further clinically important loss is very likely), we do not have sufficient data to suggest categories for this dimension at present.
Separating classification from healthcare recommendations
The creation of classification schemes and choice of cut-off points has both political and philosophical implications. The close association of the US classification system with prescriptions for health policy, laboratory reporting, and individual patient care7 has been confusing, and has sadly politicised what should have been scientific debate about a classification scheme. Publication of the new international classification scheme should be divorced from research, practice, or policy recommendations in order to separate debate about the validity and usefulness of the classification from debate about the appropriateness of any subsequent recommendations. The scheme we propose would be of value in facilitating recommendations that are sensitive to variations in different parts of the world in terms of healthcare priorities, current state of knowledge, and availability of resources.
Summary points
Most patients who require dialysis or a kidney transplant do so because of gradual worsening of severe low kidney function
Mild and moderate low kidney function are prevalent in the general population
The prognosis and optimal management of modest abnormalities in kidney function and proteinuria are unknown
An international classification for kidney health is being developed to facilitate research, patient care, and policy development
An inclusive classification system that avoids labelling is proposed that could be used in disparate international settings
Contributors and sources: CMC, AXG and BAK have reported on the population epidemiology of low renal function and have continuing research interests in the area of prevention of end stage renal disease through screening and early intervention. The article is based on data from large trials and meta-analyses. Our thinking about the development of a classification system and about healthcare recommendations has been greatly influenced by D L Sackett.w13 CMC wrote the orignal draft and revisions. AMX conducted the original analyses on which the work depends and contributed to the discussion of the issues and revision of the manuscript. BAK contributed to data interpretation and writing and revising the article. P Roderick reviewed the article for the BMJ and suggested the inclusion of an additional category into the classification system. CMC is guarantor.
Funding: AXG was supported by a phase 1 Canadian Institutes of Health Research clinician scientist training award.
Competing interests: All authors have been asked for and provided input into the Kidney Disease Improving Global Outcomes Initiative. CMC will participate later this year in a conference organised by this initiative: Definition, Diagnosis and Classification of Chronic Kidney Disease in Adults.
References
- 1.ERA-EDTA Registry: Annual report, 2003. Amsterdam: Academic Medical Center, 2003.
- 2.Khan IH, Garratt AM, Kumar A, Cody DJ, Catto GR, Edward N, et al. Patients' perception of health on renal replacement therapy: evaluation using a new instrument. Nephrol Dial Transplant 1995;10: 684-9. [PubMed] [Google Scholar]
- 3.Lamping DL, Constantinovici N, Roderick P, Normand C, Henderson L, Harris S, et al. Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. Lancet 2000;356: 1543-50. [DOI] [PubMed] [Google Scholar]
- 4.Hsu CY, Chertow GM. Chronic renal confusion: insufficiency, failure, dysfunction, or disease. Am J Kidney Dis 2000;36: 415-8. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi H, Pang M, Campbell A, Saab P. Slowing the progression of chronic renal failure: economic benefits and patients' perspectives. Am J Kidney Dis 2002;39: 721-9. [DOI] [PubMed] [Google Scholar]
- 6.Lindeman RD, Tobin J, Shock NW. Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc 1985;33: 278-85. [DOI] [PubMed] [Google Scholar]
- 7.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis 2002;39(suppl 1):S1-266. (Also available at www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm, accessed 3 Sep 2004). [PubMed]
- 8.Clase CM, Garg AX, Kiberd BA. Prevalence of low glomerular filtration rate in non-diabetic Americans: Third National Health and Nutrition Examination Survey (NHANES III). J Am Soc Nephrol 2002;13: 1338-49. [DOI] [PubMed] [Google Scholar]
- 9.Clase CM, Garg AX, Kiberd B. Estimating the prevalence of low glomerular filtration rate requires attention to the creatinine assay calibration. J Am Soc Nephrol 2002;13: 2812-6. [DOI] [PubMed] [Google Scholar]
- 10.Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis 2003;41: 1-12. [DOI] [PubMed] [Google Scholar]
- 11.John R, Webb M, Young ASPE. Unreferred chronic kidney disease: a longitudinal study. Am J Kidney Dis 2004;43: 825-35. [DOI] [PubMed] [Google Scholar]
- 12.Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med 1993;329: 1456-62. [DOI] [PubMed] [Google Scholar]
- 13.Ruggenenti P, Perna A, Gherardi G, Garini G, Zoccali C, Salvadori M, et al. Renoprotective properties of ACE-inhibition in non-diabetic nephropathies with non-nephrotic proteinuria. Lancet 1999;354: 359-64. [DOI] [PubMed] [Google Scholar]
- 14.Iseki K, Iseki C, Ikemiya Y, Fukiyama K. Risk of developing end-stage renal disease in a cohort of mass screening. Kidney Int 1996;49: 800-5. [DOI] [PubMed] [Google Scholar]
- 15.Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med 2001;134: 629-36. [DOI] [PubMed] [Google Scholar]
- 16.Haynes RB, Sackett DL, Taylor DW, Gibson ES, Johnson AL. Increased absenteeism from work after detection and labeling of hypertensive patients. N Engl J Med 1978;299: 741-4. [DOI] [PubMed] [Google Scholar]
- 17.Moynihan R, Heath I, Henry D. Selling sickness: the pharmaceutical industry and disease mongering. BMJ. 2002;324: 886-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iseki K, Ikemiya Y, Fukiyama K. Risk factors of end-stage renal disease and serum creatinine in a community-based mass screening. Kidney Int 1997;51: 850-4. [DOI] [PubMed] [Google Scholar]
- 19.Iseki K, Ikemiya Y, Iseki C, Takishita S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int 2003;63: 1468-74. [DOI] [PubMed] [Google Scholar]
- 20.Kannel WB, Stampfer MJ, Castelli WP, Verter J. The prognostic significance of proteinuria: the Framingham study. Am Heart J 1984;108: 1347-52. [DOI] [PubMed] [Google Scholar]