Abstract
OBJECTIVES
The aim of this study was to assess the prevalence and associations between anal intercourse and fecal incontinence.
METHODS
Analyses were based on data from 6,150 adults (≥20 years) from the 2009–2010 cycle of the National Health and Nutrition Examination Surveys. Fecal incontinence was defined as the loss of liquid, solid, or mucus stool occurring at least monthly on a validated questionnaire. A gender-specific sexual behavior questionnaire assessed any anal intercourse via an audio computer-assisted personal interview. Co-variables included: age, race, education, poverty income ratio, body mass index, chronic illnesses, depression, loose stool consistency (Bristol Stool Scale types 6 or 7), and reproductive variables in women. Prevalence estimates and prevalence odds ratios (PORs) were analyzed in adjusted multivariable models using appropriate sampling weights.
RESULTS
Overall, 4,170 adults aged 20–69 years (2,070 women and 2,100 men) completed sexual behavior questionnaires and responded to fecal incontinence questions. Anal intercourse was higher among women (37.3%) than men (4.5%), P<0.001. Fecal incontinence rates were higher among women (9.9 vs. 7.4%, P=0.05) and men (11.6 vs. 5.3%, P=0.03) reporting anal intercourse compared with those not reporting anal intercourse. After multivariable adjustment for other factors associated with fecal incontinence, anal intercourse remained a predictor of fecal incontinence among women (POR: 1.5; 95% confidence interval (CI): 1.0–2.0) and men (POR: 2.8; 95% CI: 1.6–5.0).
CONCLUSIONS
The findings support the assessment of anal intercourse as a factor contributing to fecal incontinence in adults, especially among men.
INTRODUCTION
Anal intercourse is a common practice among both heterosexual and homosexual couples where at least one of the partners is male. Approximately 20% of women engage in anal intercourse and among homosexual male populations, anal intercourse is common, yet little is known about the impact of anal intercourse on fecal continence (1–4). Men engaged in anal intercourse may have lower manometry pressures than men not engaged in anal intercourse; however, few studies have examined fecal incontinence (FI) symptoms and anal intercourse (5,6).
Although specific sexual practices of women with FI are undescribed, women with FI are as likely to be sexually active as women without FI but their sexual function scores are lower (7,8). Studies evaluating the impact of FI treatment on sexual function are limited to descriptions in small populations following sphincteroplasty, with most studies reporting improved function and less embarrassment with sexual activity following treatment for FI (9–11).
The primary aim of this study was to determine if anal intercourse is associated with reports of FI, defined as the accidental loss of liquid, solid, or mucus stool occurring at least monthly. Secondary aims were (i) to characterize the prevalence of anal intercourse in a nationally representative sample of non-institutionalized US adults aged 20–69 years and (ii) to assess the relationship of anal intercourse with other known factors associated with FI, such as age, comorbid diseases, depression, and stool consistency. We hypothesized that both women and men who engaged in anal intercourse would have higher rates of FI.
METHODS
Study population
The National Health and Nutrition Examination Surveys (NHANES) are cross-sectional surveys of a nationally representative sample of a non-institutionalized population sampled using a complex, stratified, multi-stage, probability cluster design. The National Center for Health Statistics (NCHS) ethics review board approved the survey protocols, and all participants provided written informed consent.
The NHANES cycle for 2009–2010 included 6,150 adults aged ≥20 years of age. Questions specific to anal intercourse were administered to men and women aged 18–69 years. Women who were pregnant were excluded from the analysis. Questions about bowel symptoms were ascertained in the mobile examination center interview room using a computer-assisted personal interview system. Questions about sexual behaviors were ascertained in a private mobile examination center interview room using an audio computer-assisted personal interview system. Our final analytic sample included 4,170 adults aged 20–69 years who answered questions about anal intercourse and FI (Figure 1).
Figure 1.
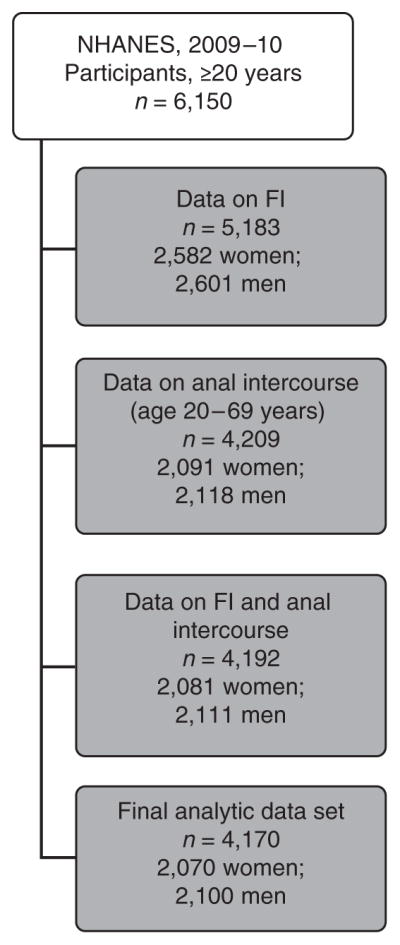
NHANES 2009–2010 participants responding to questions on fecal incontinence (FI) and anal intercourse.
FI definition
For purposes of this analysis, FI was defined as leakage of mucus, liquid, and/or solid stool occurring at least monthly as reported on the Fecal Incontinence Severity Index (FISI). The FISI has subjects ranked according to the frequency of incontinence into four separate categories of gas, mucus, liquid, and solid stool, ranging from 1 to 20, with higher scores indicating greater severity (12). Stool consistency was assessed using the Bristol Stool Form Scale (color picture card with pictures and written descriptors of the seven stool types) and the following written question: “Please look at this card and tell me the number that corresponds with your usual or most common stool type” (13). Hard stool was defined as a Type 1 (separate hard lumps, like nuts) or Type 2 rating (sausage like, but lumpy). Normal stool consistency was defined as Bristol Stool Scale Type 3, Type 4, and Type 5, and, as in other NHANES publications (14), Type 6 and Type 7 Bristol Stool Scale Types defined loose stool consistency.
Sexual behavior measures
The NHANES sexual behavior questionnaire uses different questions to assess anal intercourse according to gender. For women, a positive response to the question, “Have you ever had anal sex? (the contact of a man’s penis with your anus or butt)” defined anal intercourse. For men, a positive response to the question, “Have you ever had any kind of sex with a man, including oral or anal?” defined having anal intercourse. To validate the use of this question to define anal intercourse in men, we analyzed the concordance for the men responding affirmatively to the question for anal intercourse who also answered the following question, “In your lifetime, with how many men have you had anal sex?” Women were not asked about the number of anal intercourse encounters. No questions queried the frequency of anal intercourse.
Other measurements
Sociodemographic measures included age categories (20–29, 30–39, 40–49, 50–59, and 60–69 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic-Mexican American, Hispanic—other, Other—including multi-racial), education (less than high school, high school, or more than high school), and poverty income ratio categorized as <1 (below the poverty threshold), 1 to 2 (1–2×the poverty threshold), and ≥2 (2×the poverty threshold). Participants’ weight and height were measured and body mass index was calculated as normal weight, over-weight, or obese (<25.0, 25.0–29.9, ≥30 kg/m2, respectively).
Other medical conditions were ascertained through the question “Has a doctor or other health professional told you that you had [disease]?” Disease types were examined and categorized as positive by self-report: hypertension, arthritis, cerebrovascular accident, chronic lower respiratory tract disease, coronary heart disease, congestive heart failure, liver disease, thyroid disease, cancer (other than skin), and diabetes mellitus (15). Chronic lower respiratory tract disease included self-reported emphysema, chronic bronchitis, or asthma; coronary heart disease included coronary artery disease, angina, or a myocardial infarction. Diabetes included participants who also were taking insulin and/or diabetic pills. The cumulative number of positive responses to the disease types was divided into four categories: 0, 1, 2, and ≥3. Depression was assessed using the validated Patient Health Questionnaire–9 (PHQ-9). The PHQ-9 yields scores from 0 to 27 and scores≥10 are used to define major depression (16).
Statistical methods
All estimates, standard errors, and association measures were derived using the sampling weights provided by the NCHS. These weights take into account unequal probabilities of selection resulting from the sample design, non-response, and planned over-sampling of specific racial and ethnic groups in the US population.
Appropriately weighted χ2 analysis and Pearson correlation coefficients according to gender were used to compare differences in those who reported anal intercourse and those who did not. Comparisons for those with and without FI have been published elsewhere (14). We used appropriate sample weighting for two-sample t-tests for testing differences in means. Survey-weighted multivariable logistic regression analysis with step-wise backward elimination was used to calculate odds ratio (OR) estimates and corresponding 95% confidence intervals (CIs) adjusting for variables associated with FI from a prior NHANES publication (14). The following variables associated with FI were included in the multivariable models: age, race/ethnicity, education, family income, body mass index, stool consistency, comorbidity count, and depression. P-values<0.05 were considered statistically significant (no adjustment for multiple testing). Statistical analyses were performed using STATA statistical soft ware version 12.0 (College Station, TX).
RESULTS
Of the 6,150 men and non-pregnant women aged 20 years or older from the NHANES 2009–2010 cycle (Figure 1), 5,183 had data on FI. From the sexual behavior questionnaires, 4,209 participants aged 20–69 years had data regarding anal intercourse. After exclusions for those who did not answer FI or sexual behavior questions, 2,100 men and 2,070 women had complete data and comprised the final analytic sample in the multivariable models.
Anal intercourse was higher among women (37.3%) than men (4.5%), P<0.001. Up to 42% of women and 6% of men affirmed a history of anal intercourse depending on the age group assessed (Table 1). Anal intercourse was reported more frequently among younger women (aged 20–49 years) with at least a high school education as well as women reporting symptoms of moderate-to-severe depression. Men reporting anal intercourse were more likely to have at least a high school education. Overall, FI prevalence was 8.3% (6.9–10.0%) for women and 5.6% (4.3–7.2%) for men. FI rates were higher among women (9.9 vs. 7.4%; P=0.05) and men (11.6 vs. 5.3%; P=0.03) reporting anal intercourse compared with those not reporting anal intercourse. For both genders, FISI scores were low and did not differ among those with or without a history of anal intercourse. As expected, FISI scores were higher among men and women with FI than without FI (men: 15.3 vs. 3.3, P<0.001; women: 15.4 vs. 3.4, P<0.001). FISI scores were not higher in men or women (14.8 vs. 14.7, P=0.9) with FI who also reported anal intercourse.
Table 1.
Baseline characteristics of men and women reporting anal intercourse, NHANES 2009–2010
| Characteristica | Men (anal and oral intercourse) N=2,118
|
P value | Women (anal intercourse) N=2,091
|
P value | ||
|---|---|---|---|---|---|---|
| No (n=2,017) | Yes (n=101) | No (n=1,348) | Yes (n=743) | |||
| Age decade (years) | 0.22 | 0.009 | ||||
|
| ||||||
| 20–29 | 97.0 (95.1–98.2) | 3.0 (1.8–5.0) | 57.7 (50.5–64.6) | 42.3 (35.4–49.7) | ||
|
| ||||||
| 30–39 | 93.7 (90.4–95.9) | 6.3 (4.1–9.6) | 60.0 (54.6–64.5) | 40.3 (35.5–45.4) | ||
|
| ||||||
| 40–49 | 96.5 (93.1–95.9) | 3.5 (1.8–6.9) | 59.4 (54.3–64.3) | 40.6 (35.7–45.8) | ||
|
| ||||||
| 50–59 | 94.0 (88.3–97.0) | 6.0 (3.0–11.7) | 66.2 (60.0–71.9) | 33.8 (28.1–40.0) | ||
|
| ||||||
| 66–69 | 96.3 (92.5–98.1) | 3.7 (1.8–7.5) | 72.5 (67.2–77.3) | 27.5 (39.1–47.0) | ||
|
| ||||||
| Race/Ethnicity | 0.50 | 0.06 | ||||
|
| ||||||
| Hispanic-Mexican American | 96.1 (91.2–98.3) | 3.9 (1.7–8.8) | 67.9 (61.6–73.5) | 32.2 (26.5–38.4) | ||
|
| ||||||
| Hispanic—other | 94.6 (88.9–97.5) | 5.4 (2.5–11.1) | 60.7 (49.0–71.2) | 39.4 (28.8–51.0) | ||
|
| ||||||
| Non-Hispanic white | 95.1 (92.9–96.7) | 4.9 (3.3–7.1) | 60.0 (56.0–63.9) | 40.0 (36.1–44.0) | ||
|
| ||||||
| Non-Hispanic black | 95.7 (93.2–97.3) | 4.3 (2.7–6.8) | 71.8 (65.2–77.5) | 28.2 (22.5–34.8) | ||
|
| ||||||
| Other—including multi-racial | 98.5 (91.9–99.7) | 1.5 (0.3–8.1) | 69.9 (54.1–80.6) | 31.1 (19.4–45.9) | ||
|
| ||||||
| Education | 0.02 | 0.02 | ||||
|
| ||||||
| <High school | 98.6 (97.6–99.2) | 1.4 (0.8–2.4) | 70.3 (64.3–75.8) | 29.7 (24.2–35.8) | ||
|
| ||||||
| High school | 95.8 (93.1–97.5) | 4.2 (2.5–6.9) | 57.6 (51.9–63.1) | 42.4 (36.9–48.1) | ||
|
| ||||||
| >High school | 94.4 (91.8–96.2) | 5.6 (3.8–8.2) | 62.4 (59.1–65.6) | 37.6 (34.4–40.9) | ||
|
| ||||||
| Poverty status | 0.13 | 0.70 | ||||
|
| ||||||
| At or below level | 92.5 (86.7–95.9) | 7.5 (4.1–13.3) | 61.7 (55.9–67.2) | 38.3 (32.8–44.1) | ||
|
| ||||||
| 1× above level | 96.1 (92.1–98.1) | 3.9 (1.9–7.8) | 64.5 (58.6–70.0) | 35.5 (30.0–41.4) | ||
|
| ||||||
| 2× above level | 95.8 (94.4–96.9) | 4.2 (3.1–5.6) | 62.4 (59.5–65.3) | 37.6 (34.7–40.6) | ||
|
| ||||||
| BMI | 0.45 | 0.76 | ||||
|
| ||||||
| <25.0 | 94.9 (92.0–96.8) | 5.1 (3.2–8.0) | 63.8 (58.1–69.1) | 36.2 (30.9–41.9) | ||
|
| ||||||
| 25.0–29.9 | 95.0 (92.7–96.7) | 5.0 (3.3–7.3) | 61.2 (54.7–67.1) | 38.9 (33.0–45.3) | ||
|
| ||||||
| >30.0 | 96.4 (93.8–97.9) | 3.6 (2.1–6.2) | 62.8 (59.3–66.2) | 37.2 (33.8–40.7) | ||
|
| ||||||
| Number of comorbid conditions | 0.72 | 0.67 | ||||
|
| ||||||
| None | 95.5 (94.1–96.6) | 4.5 (3.4–5.9) | 62.4 (58.4–66.3) | 37.6 (33.8–41.6) | ||
|
| ||||||
| 1 | 96.2 (93.5–97.8) | 3.9 (2.3–6.5) | 63.4 (60.9–65.9) | 36.6 (34.1–39.1) | ||
|
| ||||||
| 2 | 93.6 (81.0–98.1) | 6.4 (1.9–19.0) | 65.2 (56.2–73.2) | 34.9 (26.8–43.8) | ||
|
| ||||||
| 3 or more | 93.0 (69.7–98.7) | 7.0 (1.3–30.3) | 57.2 (42.4–70.9) | 42.8 (29.1–57.6) | ||
|
| ||||||
| Depression (moderate–severe)b | 0.37 | 0.01 | ||||
|
| ||||||
| No | 95.5 (94.0–96.7) | 4.5 (3.3–6.0) | 63.2 (60.5–65.7) | 36.9 (34.3–39.5) | ||
|
| ||||||
| Yes | 93.8 (86.8–97.2) | 6.2 (2.8–13.2) | 50.4 (41.0–59.8) | 49.6 (40.2–59.0) | ||
|
| ||||||
| Fecal incontinence (monthly or more) | 0.03 | 0.05 | ||||
|
| ||||||
| No | 95.8 (94.1–97.0) | 4.3 (3.0–5.9) | 63.4 (61.0–65.6) | 36.7 (34.4–39.0) | ||
|
| ||||||
| Yes | 90.6 (83.7–94.7) | 9.4 (5.3–16.3) | 55.6 (46.9–63.9) | 44.4 (36.1–53.1) | ||
|
| ||||||
| Fecal Incontinence Severity Index (FISI) scores (mean, 95% CI) | 0.28 | 0.20 | ||||
|
| ||||||
| 4.0 (3.5–4.4) | 4.6 (3.5–5.6) | 4.3 (3.9–4.7) | 4.6 (4.3–4.9) | |||
|
| ||||||
| Stool consistency, Bristol Stool Form Scale | 0.99 | 0.12 | ||||
|
| ||||||
| Hard, type 1–2 | 94.2 (82.6–98.2) | 4.6 (1.3–15.2) | 60.6 (54.7–66.2) | 39.4 (33.8–45.3) | ||
|
| ||||||
| Normal, type 3–5 | 95.5 (94.0–96.6) | 4.6 (3.3–6.3) | 63.3 (60.7–65.9) | 36.7 (34.2–39.3) | ||
|
| ||||||
| Loose, type 6–7 | 95.9 (89.6–98.4) | 4.2 (1.3–12.9) | 56.7 (49.1–63.9) | 43.3 (36.1–50.9) | ||
|
| ||||||
| Vaginal delivery | 0.13 | |||||
|
| ||||||
| None | NA | NA | 57.2 (50.3–63.9) | 42.8 (36.1–40.6) | ||
|
| ||||||
| 1 or more | NA | NA | 63.3 (59.5–66.9) | 36.8 (33.1–40.6) | ||
|
| ||||||
| Hysterectomy | 0.60 | |||||
|
| ||||||
| No | NA | NA | 62.5 (59.9–65.0) | 37.5 (35.0–40.1) | ||
|
| ||||||
| Yes | NA | NA | 63.5 (59.5–67.3) | 36.5 (32.7–40.5) | ||
BMI, body mass index; CI, confidence interval; NA, not applicable; NHANES, National Health and Nutrition Examination Survey.
Proportion (95% CI) unless noted.
Based upon a PHQ-9 score of ≥10.
After multivariable adjustment including other known FI clinical risk factors (Table 2), anal intercourse remained significantly associated with prevalent FI among both men and women. The adjusted odds of FI were higher in men reporting anal intercourse (OR: 2.8 (95% CI: 1.6–5.0); P<0.001) than women (OR: 1.5 (95% CI: 1.0–2.0)). A sensitivity analysis was performed to assess if the association changed among the group of men (n=69, 68%) who reported anal intercourse at least once in their lifetime (validation question only available for men). Men who confirmed anal intercourse at least once in their lifetime reported a higher prevalence of FI (12.0 vs. 5.4%; P=0.07) than men with no lifetime anal intercourse and the adjusted OR for anal intercourse and FI remained significant (OR: 2.2 (95% CI: 1.02–4.6); P=0.04).
Table 2.
Anal intercourse associations with at least monthly fecal incontinence in multivariable models for men and women, NHANES 2009–10
| Men, n=2,100a odds ratio (95% CI) |
Women, n=2,070a,b odds ratio (95% CI) |
|
|---|---|---|
| Anal intercourse | 2.8 (1.6–5.0) | 1.5 (1.0–2.0) |
| Age (per decade) | 1.2 (1.1–1.4) | 1.5 (1.4–1.8) |
| Depression | 3.2 (1.6–6.4) | 3.5 (2.2–5.7) |
| Loose stool consistency | 2.4 (1.4–4.0) | 2.2 (1.5–3.4) |
CI, confidence interval; NHANES, National Health and Nutrition Examination Survey.
Multivariable logistic regression models with step-wise backward elimination models controlling for age (decade categories as per Table 1), race/ethnicity, education, family income, BMI, loose stool consistency (Bristol Stool Form Scale Type 6 and 7), comorbidity count, and depression (PHQ-9 scores ≥10).
Hysterectomy and number of live births included in model for women.
DISCUSSION
From a US population-based survey that involved private interviews with an audio-enabled computer-assisted questionnaire, women reported higher prevalence than men for anal intercourse (37 vs. 5%). Despite higher overall prevalence of anal intercourse in women, men reporting anal intercourse had a higher prevalence of FI than women (11.6 vs. 9.9%, P<0.001). After controlling for other known factors for FI in adults, anal intercourse was associated with an increased odds of having FI in both men and women. Better recognition of factors that may contribute to FI may open dialogue and improve discussion of two taboo topics in the healthcare setting: individual sexual practices and accidental bowel leakage (17).
In the lay press there is a common belief that anal intercourse is related to FI and other bowel symptoms, such as constipation; online forums on sexual practices and health often contain content regarding these associations (Websites accessed using the search terms, “anal intercourse” and “fecal incontinence” (http://www.salon.com/2011/12/30/does_gay_sex_cause_incontinence/) and (http://www.netdoctor.co.uk/ate/sexandrelationships/sex/200700.html)). Despite public concern, little work has examined anal intercourse as a possible risk factor for FI in the scientific community. Studies have mainly focused on the relationship between anorectal structure and function and anal intercourse among men with mixed results. Lower anal resting pressure has been noted among men who engaged in anal intercourse (5,6). However, studies have had inconsistent results regarding lower maximum squeeze pressures and the complaint of FI in men who practice anal intercourse (5,6). These studies had small numbers of men who had anal intercourse, 40 and 14—respectively. Data on the effects of anal intercourse on anorectal structure and function among women are lacking.
Biologic plausibility exists for anal intercourse as a risk factor for FI. The internal anal sphincter contributes to the majority of the anal resting pressure. Anal intercourse could dilate and eventually stretch the internal and external anal sphincters leading to damage of these structures, as demonstrated by the lower resting pressure. This lower pressure and possible damage to the internal and external anal sphincters could lead to FI via muscle atrophy and sensory deficits. Smaller clinical cohort studies have found than women with and without FI have lower anal pressures than men (18,19).
We did not see differences in the FISI scores among those with and without the self-report of anal intercourse. FI severity, as measured by the FISI scores, only measures the frequency of stool loss and the type of leakage (including flatus, mucus, liquid, or solid stool). FISI scores do not take into account fecal urgency or the conditions when FI occurs, such as passive leakage or urgency leakage. Anal intercourse may affect urgency or passive FI more than the type of leakage that occurs. In addition, anal intercourse may only have a small impact on fecal continence so that it lowers the threshold for occurrence without worsening severity. In addition, we were unable to quantify the frequency of anal intercourse in this population and it is possible that the majority of individuals rarely practice anal intercourse, which would have decreased the impact on FI severity. More data are needed to further test this hypothesis.
The strengths of this study include the population-based study design as well as a large sample size. Prior studies have been limited by gender and we were able to include both genders in this study. Finally, validated questions were used for both FI and stool consistency, which have been shown to be valid and reliable in the assessment of bowel symptoms. There are several limitations in this work. There are no validated questions for anal intercourse and we were unable to assess the frequency of anal intercourse among women. In addition, the definition utilized in this study for male anal intercourse is imperfect and limited to the questions asked in this NHANES cycle. We did, however, find concurrence between the two questions related to anal intercourse in 68% of our male population. A sensitivity analysis including only the 69 men who responded positively to both questions, revealed similar results. Although the definition of anal intercourse for men in this study may overestimate the number of men engaged in anal intercourse, studies have shown that men who report sex with men frequently report at least some experience with anal intercourse (20). In addition, other sexual practices that involve the rectum, such as “fisting” were not measured, and could impact the results of this current analysis. We could not distinguish between consensual anal intercourse and non-consensual anal intercourse in this cohort. Both men and women may be reluctant to divulge anal intercourse practices. We have previously found that women are more likely to respond positively to a written questionnaire than oral history taking with regard to FI; although the questions were administered in private, we do not know the concordance between oral and written history taking for anal intercourse (21).
When using cross-sectional data sets, such as NHANES, we are not able to prove causality between the outcome of interest (FI) and the exposure variables. We also did not adjust our analyses for multiple testing and all the potential confounding variables of the association between anal incontinence and FI may not have been queried in a broad study of health factors such as NHANES. Lastly, stool consistency assessment was only asked for the usual or most common type and may not represent the more episodic changes in stool consistency that may occur with FI episodes.
These results provide initial epidemiologic evidence supporting a link between anal intercourse and FI among both men and women. These results provide evidence to inform discussions between patients and providers with regard to the association between FI and anal intercourse. Future studies evaluating multicomponent interventions to improve FI could consider counseling regarding the association of anal intercourse and FI as part of standard practice.
Study Highlights.
WHAT IS CURRENT KNOWLEDGE
Fecal incontinence has a prevalence of 8% among adults; with equal prevalence rates among older men and women.
Risk factors for fecal incontinence that are similar among women and men include comorbidity and loose stool consistency.
Decreased anal sphincter pressures may be related to anal intercourse in small clinical series data.
WHAT IS NEW HERE
Women and men who practice anal intercourse have higher rates of fecal incontinence.
Men who practiced anal intercourse had higher odds of having fecal incontinence than women.
Assessment of sexual behaviors may be important consideration among adults with fecal incontinence.
Acknowledgments
Financial support: This study was supported in part from a Veterans Health Administration Career Development Award (CDA-2) to Alayne D. Markland and Camille P. Vaughan (1 IK2 RX000747-01).
Footnotes
CONFLICT OF INTEREST
Guarantor of the article: Alayne D. Markland, DO, MSc.
Specific author contributions: Conception, initiation, and writing: Alayne D. Markland; conception, writing and editing of manuscript: Gena C. Dunivan, Camille P. Vaughan and Rebecca G. Rogers. Rebecca G. Rogers receives royalties from UptoDate and McGraw Hill for educational writings; she is the DSMB chair for the TRANSFORM trial sponsored by American Medical Systems. Gena C. Dunivan receives research support from Pelvalon.
Potential competing interests: None.
References
- 1.Baggaley RF, Dimitrov D, Owen BN, et al. Heterosexual anal intercourse: a neglected risk factor for HIV? Am J Reproduct Immunol. 2013;69:95–105. doi: 10.1111/aji.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owen BN, Brock PM, Butler AR, et al. Prevalence and frequency of heterosexual anal intercourse among young people: a systematic review and meta-analysis. AIDS Behav. 2015;19:1338–60. doi: 10.1007/s10461-015-0997-y. [DOI] [PubMed] [Google Scholar]
- 3.Stulhofer A, Ajdukovic D. A mixed-methods exploration of women’s experiences of anal intercourse: meanings related to pain and pleasure. Arch Sex Behav. 2013;42:1053–62. doi: 10.1007/s10508-012-0068-7. [DOI] [PubMed] [Google Scholar]
- 4.Prestage G, Mao L, Fogarty A, et al. How has the sexual behaviour of gay men changed since the onset of AIDS: 1986–2003. Aust N Z J Public Health. 2005;29:530–5. doi: 10.1111/j.1467-842x.2005.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 5.Chun AB, Rose S, Mitrani C, et al. Anal sphincter structure and function in homosexual males engaging in anoreceptive intercourse. Am J Gastroenterol. 1997;92:465–8. [PubMed] [Google Scholar]
- 6.Miles AJ, Allen-Mersh TG, Wastell C. Effect of anoreceptive intercourse on anorectal function. J Royal Soc Med. 1993;86:144–7. doi: 10.1177/014107689308600309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cichowski SB, Komesu YM, Dunivan GC, et al. The association between fecal incontinence and sexual activity and function in women attending a tertiary referral center. Int Urogynecol J. 2013;24:1489–94. doi: 10.1007/s00192-013-2044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imhoff LR, Brown JS, Creasman JM, et al. Fecal incontinence decreases sexual quality of life, but does not prevent sexual activity in women. Dis Colon Rectum. 2012;55:1059–65. doi: 10.1097/DCR.0b013e318265795d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trowbridge ER, Morgan D, Trowbridge MJ, et al. Sexual function, quality of life, and severity of anal incontinence after anal sphincteroplasty. Am J Obstet Gynecol. 2006;195:1753–7. doi: 10.1016/j.ajog.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 10.Pauls RN, Silva WA, Rooney CM, et al. Sexual function following anal sphincteroplasty for fecal incontinence. Am J Obstet Gynecol. 2007;197:618. doi: 10.1016/j.ajog.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 11.Riss S, Stift A, Teleky B, et al. Long-term anorectal and sexual function after overlapping anterior anal sphincter repair: a case-match study. Dis Colon Rectum. 2009;52:1095–100. doi: 10.1007/DCR.0b013e31819f60f6. [DOI] [PubMed] [Google Scholar]
- 12.Rockwood TH, Church JM, Fleshman JW, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum. 1999;42:1525–32. doi: 10.1007/BF02236199. [DOI] [PubMed] [Google Scholar]
- 13.Heaton KW, Radvan J, Cripps H, et al. Defecation frequency and timing, and stool form in the general population: a prospective study. Gut. 1992;33:818–24. doi: 10.1136/gut.33.6.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whitehead WE, Borrud L, Goode PS, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009;137:517. doi: 10.1053/j.gastro.2009.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiss CO, Boyd CM, Yu Q, et al. Patterns of prevalent major chronic disease among older adults in the United States. JAMA. 2007;298:1160–2. doi: 10.1001/jama.298.10.1160-b. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satcher D, Hook EW, III , et al. Sexual health in america: Improving patient care and public health. JAMA. 2015;314:765–6. doi: 10.1001/jama.2015.6831. [DOI] [PubMed] [Google Scholar]
- 18.Mitrani C, Chun A, Desautels S, et al. Anorectal manometric characteristics in men and women with idiopathic fecal incontinence. J Clin Gastroenterol. 1998;26:175–8. doi: 10.1097/00004836-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Williams AB, Cheetham MJ, Bartram CI, et al. Gender differences in the longitudinal pressure profile of the anal canal related to anatomical structure as demonstrated on three-dimensional anal endosonography. Br J Surg. 2000;87:1674–9. doi: 10.1046/j.1365-2168.2000.01581.x. [DOI] [PubMed] [Google Scholar]
- 20.Mayer KH, Bekker LG, Stall R, et al. Comprehensive clinical care for men who have sex with men: an integrated approach. Lancet. 2012;380:378–87. doi: 10.1016/S0140-6736(12)60835-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cichowski SB, Dunivan GC, Rogers RG, et al. Standard compared with mnemonic counseling for fecal incontinence: a randomized controlled trial. Obstet Gynecol. 2015;125:1063–70. doi: 10.1097/AOG.0000000000000755. [DOI] [PMC free article] [PubMed] [Google Scholar]


