Summary
Background
The prevalence of oral diseases including dental caries and periodontal conditions is remarkably higher in people with disabilities. The provision of accessible oral health services for people with learning disabilities may be challenging.
Objectives
The objectives of the review were to identify barriers in accessing oral health care that persists within society, enabling or disabling people with learning disabilities.
Methods
Using the Arksey O’Malley framework, a scoping review was conducted on PubMed/Medline, OVIDSP, and EMBASE. Studies were evaluated and short-listed based on the inclusion criteria, which consisted of: (1) study participants or population with learning disabilities, (2) aged 16 years or over, (3) reporting on access to oral health services, (4) published in the English language. Those that justified the inclusion criteria were carefully chosen after a blind peer-reviewed process when relevance and quality were debated.
Results
Nine studies were eventually included from searches. Tabulation of data was done under the heading of study type, outcomes, the year of publication and patient selection. The majority of studies provided a biomedical overview of access for adults with learning disabilities.
Conclusions
The concept of access for people with disability is still ill-defined and obscure. Access to oral health care and needs of people with learning disabilities are complex and multi-facet.
Keywords: learning disability, access, oral health, health service utilization, scoping review
Introduction
Access to affordable and acceptable health care, including access to oral health services is a basic and fundamental human right (1). Unfortunately, an inverse relationship exists in this context, and people who have greater health needs are the ones who receive the least amount of care (2). This is also evident when it comes to the oral health of marginalized groups, like those with mental, intellectual or behavioral challenges, and physical disabilities (3–5).
It is observed that similar to other marginalized groups, people with learning disabilities also have poorer oral hygiene status and a higher prevalence of dental caries and periodontal disease (6, 7). As a consequence, poor oral health not only affects the physical well-being of these groups but also has a marked impact on their quality of life, overall health and self-esteem (8). In a recent study, it was proposed that groups with special needs may present with complex needs that can be met through prevention and which require extensive focus towards further research (9).
Models of disability and access to care
The term “disability” has been defined and utilized in various forms in recent years. The medical model and the social model of disability present two contrasting concepts that define disability in completely different context and setting (10). While the medical model proposes that disability physical or behavioral should be seen as individualistic, the social model sees disability through a social lens and considers it as a challenge for the society as a whole. It focuses on systems structure that enables the society to access and utilize health care, thus preventing disability from becoming a handicap (11). Oliver and Zarb critique that health systems based on the biomedical model of health promotion influence the objectification, classification and categorization of people, thus promoting discrimination, labeling and victim blaming (12, 13).
Access to services for people with learning disabilities appears multi-dimensional and multi-faceted (14, 15). The poor oral health status of people with learning disabilities reflects the barriers to access faced by them and is evident as the marked variation seen in the utilization of these services (16). This eventually results in detrimental oral health outcomes (17). The most commonly identified barrier to health or oral health service utilization is physical access (18, 19). While physical access to roads, transportation, hospital buildings and clinical facilities is crucial, the ability to access a workforce which is conducive and trained to cater to the special needs of marginalized groups is of equal importance (20).
Various models of access including various criteria have been proposed by different Authors (17, 19, 21). However, there seems to be a variation in utilization of services. These variations in the uptake of services are due to attitudes, research, and policies based on the biomedical model of access rather than the social model (22).
Most of the work done on access for people with learning disabilities has taken place in the field of health, social care, and general medicine. Although evidence of good practice has been reported under these areas, yet more research is needed in this domain (23). Although Authors found a systematic review (24) of the oral health of people with intellectual disabilities and access to healthcare for disabled people (25), yet the Authors did not find any review analyzing disparity in access to oral health care for people with learning disabilities. Therefore, the aim of this scoping review was to review access to oral health care for people with learning disabilities, along with identifying barriers to accessing oral health care that persists within society.
Methods
The study followed the framework presented by Arksey O’Malley for scoping reviews (26). The review followed five stages: (1) Identifying the research question; (2) Literature search; (3) Study selection; (4) Data extraction; and (5) Summarizing and reporting the results. A broad research question was selected in order to scope the extent of research available on the subject and to avoid early exhaustion of literature during the search process.
An initial search of broader concepts using various search terms was conducted on PubMed and a log of relevant terms was maintained. Three major concepts were used: learning disability, oral health, and access to care. The pilot search developed the final research question and dictated the inclusion and exclusion criteria.
Research question: what are the barriers to the access of oral health care services for adults (16 years and over) with learning disabilities?
A detailed search strategy was then developed using relevant MeSH terms and keywords, with the assistance of an expert librarian (Tab. 1). The final search strategy, with database specific modifications, was executed on Medline via OvidSP, PubMed, and EM-BASE.
Table 1.
Search Strategy on Medline.
|
Studies meeting the following inclusion criteria were subsequently included in the scoping review: (1) study participants or population with learning disabilities, (2) aged 16 years or over, (3) reporting on access to oral health services, (4) published in English language. The exclusion criteria to filter out the studies were (1) any gray literature, (2) non-peer reviewed articles, (3) articles which were not focusing on oral health and focused on children disability (4) articles other than English were excluded. There were no date limitations applied for study designs or year of publication, and all studies published until February 2016 were considered for eligibility. An age limit was applied restricting the results to studies published on an adult study population “All adults-16 plus years” in Medline and “18 to 64 years” in EMBASE). Table 2 illustrates a list of databases, search engines and library resources used for the literature search. Screening and study selection: two reviewers (Author 1 and 2) conducted literature screening, and study selection independently, following duplicate removal after initial title and abstract screening, relevant studies meeting the research question theme were selected for full-text review. Following the full-text review, studies meeting the inclusion criteria were included in the scoping review. Data extraction for each study included in the final selection was carried out, using a data extraction form, recording information on the main characteristics and findings of each study.
Table 2.
List of data bases, search engines, libraries resources used for literature search.
| Resource Type | Resource name |
|---|---|
| Journals |
|
| Literature databases |
|
| Search engines | PubMed |
| Library | University of Sheffield Saudi Digital Library (www.sdl.edu.sa) |
Disagreements were resolved by discussion with a third reviewer (Author 3) and a consensus was achieved. The online search was further complemented by hand searching and sifting through the bibliography of studies shortlisted for inclusion.
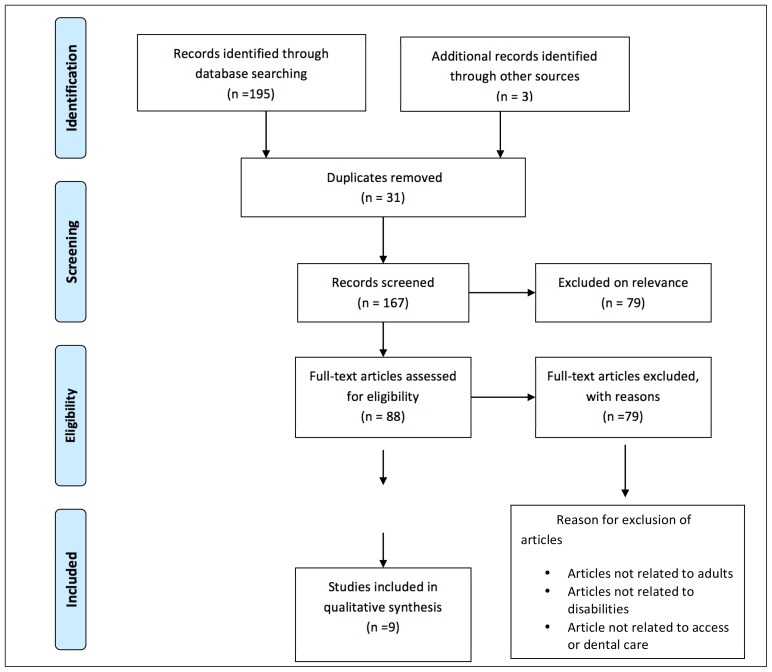
Endnote Citation Manager X7 was used to catalog the studies according to database, duplicates, initial screening and final inclusion. An of the scoping review process according to PRISMA guidelines is presented in Figure 1.
Figure 1.
Prisma flow diagram.
Results
Around 195 studies were retrieved from the search strategy and 3 studies were shortlisted through other resources. Following duplicate removal (n=31) 167 studies were screened for title and abstract and 88 studies were selected for full-text review. Following review and discussion, nine studies were included in the study (Fig. 1) Prisma Flow diagram.
Table 3 shows the general characteristics of studies considered in this scoping review. A total of nine articles were included in the final synthesis. These articles had been published between years 1991 to 2011. Among the nine reviewed articles, three studies were quantitative studies (27–29) with cross-sectional study design. Two were verifiable CPD papers (17, 30) based on the existing literature and two were qualitative studies based on interviews and opinions (5, 16). Two studies were review articles (19, 29). One-third of the studies used quantitative study designs to explore access to services with broader samples. The total number of responders (sample) ranged 485 to 1984 for quantitative researches. In the qualitative study the sample of the study participants ranged from 10 to 40.
Table 3.
List of studies and their general characteristics included in the review.
| First author (year) | Study design | Topic | Country | Sample size | Main findings |
|---|---|---|---|---|---|
| Gallagher (2007) | Review article- CPD paper | Current professional challenges for ensuring access to dental care. | United Kingdom | No sample | A skilled workforce is needed based on partnership between DWsI (Dentist with Special Interests) and primary dental care practitioners in improving oral health of people with disabilities. |
| Pradhan (2009) | Cross-sectional | Utilization of dental services-Residence factors. | Australia | n = 485 |
|
| Cumella (2000) | Qualitative | Experiences of people with learning disabilities in accessing dental care. | United Kingdom | n = 60 |
|
| Dougall (2008) | Review article | Impact of legislative and in-practice changes on access and utilization of dental care. | United Kingdom | No sample | Improving overall access to dental care for the population of interest needs:
|
| Wu (2007) | Cross sectional | Relationship between cognitive function and dental care utilization. | United States | n = 1984 |
|
| Owens (2010) | Review article | Strategies to improve access to oral care for people with learning disabilities. | United Kingdom | No sample |
|
| Owens (2011) | Qualitative | Experiences of people with learning disabilities and their caregivers in accessing dental care. | United Kingdom | n = 10 | From a perspective of the social model of disability:
|
| Koneru (2009) | Cross-sectional | Perceived barriers and challenges to accessing dental care for individuals with developmental disabilities in Ontario, Canada. | Ontario | n = 634 |
|
| Wilson (1992) | Review article | A review article of existing literature. | United Kingdom | No sample | The article reviews literature related to access problems for mentally and physically handicapped adults. Highlights recommendations to improve the situation. |
In general, CPD papers (17, 30) highlighted ways to address unmet needs and improve access to the most vulnerable sections of society i.e. disabled individuals. Similarly, in quantitative studies both internal and external barriers were identified, which compromised utilization of dental services among adults with disabilities. In all nine studies, access was poorly defined and the term remains ambiguous for people with learning disabilities.
Discussion
The present study was based on the hypothesis that access to oral health care for adults with learning disabilities is similar to the general population. To our understanding from indexed literature, this is the first scoping review that systematically reviewed access to Oral health care among adults with learning disabilities.
Interestingly, the majority of studies included in this review define access on the basis of the single concept of “utilization of services”. While both papers by Dougall and Fiske (17), Gallagher and Fiske (30) explain access to dental services for people with disabilities, they lean towards the biomedical model with minimal emphasis on the social aspect of care and access. Only those aspects of access are taken into account which may pose as physical barriers to oral care for adults with learning disabilities, while little attention is given to other multi-dimensional aspects of access.
Similarly, Koneru and Sigal (27) and Cumella et al. (5) also cite access as the “ability to obtain and use services”. The definition moves towards an indicator of access without describing what “access” really means for people with disabilities (31).
This was observed throughout the studies reviewed. Policy makers, professionals and Authors when attempting to suggest effective health care reforms, tend to assign different meanings to the term “access” based on the feasibility and suitability of the profession without justifying comprehension and complexity of issue (21, 32).
Recently, a renewed emphasis was given for access to oral care by Owens et al. (16) who presented a framework of access based on the social model of disability. The proposed model has been inspired by the works of Penchansky and Thomas (15, 21) and Donabedian (33). It negates the role of personal experience and professionally driven practice to access services. Instead, it deals with barriers by addressing societal discrimination against various forms of disability (12, 20). It divides access into six categories: physical access, acceptability, affordability, accommodation, appropriateness, and availability. Unfortunately, it appears that the social model of disability is not practiced in its true sense within dentistry. Evidence suggests that attitudes of the dentists and dental staff, lack of interdisciplinary collaboration among different health services and lack of acknowledgement of the rights of people with disabilities create barriers to service utilization (16).
A study by Koneru and Sigal (27) reported that while people with learning disabilities were able to access dental services, the greatest difficulty was experienced in accessing services when general anesthesia was required. They also cited the poor availability of services, affordability, and beliefs of caregivers as barriers to access and utilization. However, the weakness of the study was a weak sampling procedure resulting in recall bias. Similarly, in another study, it was observed that attention must be paid to creating an adequate dental workforce to respond to the demand that enables patients and dentists to participate in any programs that are aimed at improving access to care for underserved populations (34).
Cumella et al. (5) and Pradhan et al. (29) underlined the factors that create barriers to access for dental services, however, their recommendations lack a concrete definition of access. Both studies measured access in terms of service utilization. This uni-faceted approach is often simply not enough and may not do justice to the resources put to address the problem. Cumella et al. (5) highlight that the poor oral health status of individuals with learning disabilities is not adequately addressed and their oral health needs may continue to be unmet as compared to the general population.
The studies included here, highlight the barriers to access and service utilization, which include lack of knowledge or expertise on part of the dentist, hesitation or lack of confidence to treat patients with disabilities, attitudes of the dental workforce and issues with remuneration methods. From the other side, these barriers include limited awareness of carers and family about the services that may be available for their patients or loved ones. Cumella et al. (5) have classified these barriers into three broad categories:
Looking from a wider context these barriers can be appropriately addressed if discussed under the framework of access given by Owens et al. (16). Among the studies, the most common and widely reported barrier to access dental services was fear, lack of knowledge, and awareness of carers to visit dental services along with poor attitudes and skills of the dentist as pointed out by Owens et al. (16), Cumella et al. (5), Pradhan et al. (29), Koneru and Sigal (27).
The needs of people with disabilities are diverse, complex and go beyond the sole provision of oral healthcare (17). Gallagher and Fiske (30) suggested that the need for Special Care Dentistry (SCD) is the much-needed necessity of today’s time. SCD can address the oral health care needs of people with profound and severe disabilities, who require personalized one on one care (37, 39). Therefore, the Authors emphasized on the need for the commissioning of Dentists With Special Interests (DwSI), who may hold competencies between general and special dentists and may be able to, form a skilled workforce in order to address the unmet needs of people with learning disabilities (4, 30).
Conclusion
Within the limitations of this current scoping review, it can be concluded that access for people with disabilities is a multi-dimensional concept, which continues to be poorly demarcated and under-addressed. A better understanding of the problem at hand from a social perspective has the potential to effectively address the challenges present and fill the gaps in access to care.
Recommendations
It is vital that a more integrated model of access is defined, which takes into consideration both models of disability (i.e. social and medical) and seeks to understand the complexity of the lives of people with learning disabilities. It must also be taken into consideration that people with learning disabilities are special individuals and each will experience access in a different way. Additionally, in order to provide better access to care for people with learning disabilities, the role of ‘carers’ should be enhanced as they are considered as their gate keepers.
Furthermore, this scoping review follows the Arksey O’Malley framework (40) of scoping review. While the framework continues to be the widely used, recent improvements such as the JBI framework have the potential to provide a more robust methodology to the scoping review process. It is therefore recommended that in future, researchers may consider utilizing this improved framework.
References
- 1.Kuijken NM, Naaldenberg J, Nijhuis-van der Sanden MW, van Schrojenstein-Lantman de Valk HM. Healthy living according to adults with intellectual disabilities: towards tailoring health promotion initiatives. J Intellect Disabil Res. 2016;60(3):228–241. doi: 10.1111/jir.12243. [DOI] [PubMed] [Google Scholar]
- 2.Hart JT. The inverse care law. The Lancet. 1971;297(7696):405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 3.de Castilho LS, Abreu MH, de Oliveira RB, Souza ESME, Resende VL. Factors associated with mouth breathing in children with -developmental -disabilities. Spec Care Dentist. 2016 doi: 10.1111/scd.12157. [DOI] [PubMed] [Google Scholar]
- 4.Scott A, March L, Stokes ML. A survey of oral health in a population of adults with developmental disabilities: comparison with a national oral health survey of the general population. Aust Dent J. 1998;43(4):257–261. doi: 10.1111/j.1834-7819.1998.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 5.Cumella S, Ransford N, Lyons J, Burnham H. Needs for oral care among people with intellectual disability not in contact with Community Dental Services. J Intellect Disabil Res. 2000;44(Pt 1):45–52. doi: 10.1046/j.1365-2788.2000.00252.x. [DOI] [PubMed] [Google Scholar]
- 6.Merrick J, Kandel I, Lotan M, Aspler S, Fuchs BS, Morad M. National survey 2007 on medical services for persons with intellectual disability in residential care in Israel. Int J Adolesc Med Health. 2010;22(4):575–582. doi: 10.1515/ijamh.2010.22.4.575. [DOI] [PubMed] [Google Scholar]
- 7.Niazi F, Naseem M, Khurshid Z, Zafar MS, Almas K. Role of Salvadora persica chewing stick (miswak): A natural toothbrush for holistic oral health. European journal of dentistry. 2016;10(2):301. doi: 10.4103/1305-7456.178297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raftery J. NICE: Faster access to modern treatments? Analysis of guidance on health technologies. British Medical Journal. 2001;323(7324):1300. doi: 10.1136/bmj.323.7324.1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah A, Bindayel N, AlOlaywi F, Sheehan S, AlQahtani H, AlShalwi A. Oral health status of a group at a special needs centre in AlKharj, Saudi Arabia. Journal of Disability and Oral Health. 2015;16:3. [Google Scholar]
- 10.Scambler S, Low E, Zoitopoulos L, Gallagher J. Professional attitudes towards disability in special care dentistry. Journal of Disability and Oral Health. 2011;12(2):51. [Google Scholar]
- 11.Rapley M. The social construction of intellectual disability. Cambridge University Press; 2004. [Google Scholar]
- 12.Oliver M, Zarb G. The politics of disability: a new approach. Disability, Handicap & Society. 1989;4(3):221–239. [Google Scholar]
- 13.Khurshid Z, Naseem M, Sheikh Z, Najeeb S, Shahab S, Zafar MS. Oral antimicrobial peptides: Types and role in the oral cavity. Saudi Pharmaceutical Journal. 2015 doi: 10.1016/j.jsps.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shakespeare T. Disability rights and wrongs revisited. Routledge; 2013. [Google Scholar]
- 15.Thomas C. Sociologies of disability and illness: Contested ideas in disability studies and medical sociology. Palgrave Macmillan; 2007. [Google Scholar]
- 16.Owens J, Mistry K, Dyer T. Access to dental services for people with learning disabilities: Quality care? Journal of Disability and Oral Health. 2011;12(1):17. [Google Scholar]
- 17.Dougall A, Fiske J. Access to special care dentistry, part 1. Access. British dental journal. 2008;204(11):605–616. doi: 10.1038/sj.bdj.2008.457. [DOI] [PubMed] [Google Scholar]
- 18.Scully C, Dios PD, Kumar N. Special care in dentistry: handbook of oral healthcare. Elsevier Health Sciences; 2006. [Google Scholar]
- 19.Owens J, Dyer TA, Mistry K. People with learning disabilities and specialist services. Br Dent J. 2010;208(5):203–205. doi: 10.1038/sj.bdj.2010.204. [DOI] [PubMed] [Google Scholar]
- 20.Oliver M. Understanding disability: From theory to practice. St Martin’s Press; 1996. [Google Scholar]
- 21.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Medical care. 1981;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Power TJ, Eiraldi RB, Clarke AT, Mazzuca LB, Krain AL. Improving Mental Health Service Utilization for Children and Adolescents. School Psychology Quarterly. 2005;20(2):187. [Google Scholar]
- 23.Oliver M, Sapey B, Thomas P. Social work with disabled people. Palgrave Macmillan; 2012. [Google Scholar]
- 24.Anders PL, Davis EL. Oral health of patients with intellectual disabilities: a systematic review. Special Care in Dentistry. 2010;30(3):110–117. doi: 10.1111/j.1754-4505.2010.00136.x. [DOI] [PubMed] [Google Scholar]
- 25.Gibson J, O’Connor R. Access to health care for disabled people: a systematic review. Social care and Neurodisability. 2010;1(3):21–31. [Google Scholar]
- 26.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International journal of social research methodology. 2005;8(1):19–32. [Google Scholar]
- 27.Koneru A, Sigal MJ. Access to dental care for persons with developmental disabilities in Ontario. J Can Dent Assoc. 2009;75(2):121. [PubMed] [Google Scholar]
- 28.Wu B, Plassman BL, Liang J, Wei L. Cognitive function and dental care utilization among community-dwelling older adults. American Journal of Public Health. 2007;97(12):2216–2221. doi: 10.2105/AJPH.2007.109934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pradhan A, Slade G, Spencer A. Access to dental care among adults with physical and intellectual disabilities: residence factors. Australian dental journal. 2009;54(3):204–211. doi: 10.1111/j.1834-7819.2009.01120.x. [DOI] [PubMed] [Google Scholar]
- 30.Gallagher J, Fiske J. Special care dentistry: a professional challenge. British Dental Journal. 2007;202(10):619–629. doi: 10.1038/bdj.2007.426. [DOI] [PubMed] [Google Scholar]
- 31.Savedoff WD. A moving target: universal access to healthcare services in Latin America and the Caribbean. Working paper//Inter-American Development Bank, Research Department; 2009. [Google Scholar]
- 32.Khan AA-M. Evaluating the performance of a regional health care service system: a geographic methodology. University Microfilms; 1987. [Google Scholar]
- 33.Donabedian A. Models for organizing the delivery of personal health services and criteria for evaluating them. The Milbank Memorial Fund Quarterly. 1972;50(4):103–154. [Google Scholar]
- 34.Guay AH. Access to dental care: the triad of essential factors in access-to-care programs. The Journal of the American Dental Association. 2004;135(6):779–785. doi: 10.14219/jada.archive.2004.0307. [DOI] [PubMed] [Google Scholar]
- 35.Hallberg U, Klingberg G. Giving low priority to oral health care. Voices from people with disabilities in a grounded theory study. Acta Odontologica Scandinavica. 2007;65(5):265–270. doi: 10.1080/00016350701545734. [DOI] [PubMed] [Google Scholar]
- 36.Browne T. A small-scale exploratory study of the needs of learning disabled patients presenting for an x-ray examination. Radiography. 1999;5(2):89–97. [Google Scholar]
- 37.Dougall A, Fiske J. Access to special care dentistry, part 6. Special care dentistry services for young people. Br Dent J. 2008;205(5):235–249. doi: 10.1038/sj.bdj.2008.734. [DOI] [PubMed] [Google Scholar]
- 38.Lennox N, Diggens J, Ugoni A. The general practice care of people with intellectual disability: barriers and solutions. Journal of Intellectual Disability Research. 1997;41(5):380–390. doi: 10.1111/j.1365-2788.1997.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 39.Fiske J, Griffiths J, Jamieson R, Manger D. Guidelines for oral health care for long-stay patients and residents. doi: 10.1111/j.1741-2358.2000.00055.x. [DOI] [PubMed] [Google Scholar]
- 40.Perreira TA, Innis J, Berta W. Work motivation in health care: a scoping literature review. International Journal of Evidence-Based Healthcare. 2016 doi: 10.1097/XEB.0000000000000093. [DOI] [PubMed] [Google Scholar]