Abstract
Our study was designed to contribute to an understanding of the timing and conditions under which transmission of Andes hantavirus in Oligoryzomys longicaudatus reservoir populations takes place. Mice were caged in test habitats consisting of steel drums containing holding cages, where seronegative rodents were exposed to wild seropositive individuals by freely sharing the same cage or being separated by a wire mesh. Tests were also performed for potential viral transmission to mice from excrement-tainted bedding in the cages. Andes virus transmitted efficiently; from 130 attempts with direct contact, 12.3% resulted in virus transmission. However, if we consider only those rodents that proved to be infectious, from 93 attempts we obtained 16 infected animals (17.2%). Twelve of them resulted from intraspecies O. longicaudatus encounters where male mice were differentially affected and 4 resulted from O. longicaudatus to Abrothrix olivaceus. Experiments using Abrothrix longipilis as receptors were not successful. Transmission was not observed between wire mesh-separated animals, and mice were not infected from excrement-tainted bedding. Bites seemed not to be a requisite for oral transmission. Genomic viral RNA was amplified in two out of three saliva samples from seropositive rodents, but it was not detected in urine samples obtained by vesicle puncture from two other infected rodents. Immunohistochemistry, using antibodies against Andes (AND) hantavirus proteins, revealed strong reactions in the lung and salivary glands, supporting the possibility of oral transmission. Our study suggests that AND hantavirus may be principally transmitted via saliva or saliva aerosols rather than via feces and urine.
Hantavirus comprises a genus in the family Bunyaviridae, and the enveloped virus genome consists of three segments of single-stranded, negative sense RNA (34). Hantaviruses are known to cause two serious and often fatal human diseases: hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome (HPS) (27, 33). Hantaviruses are most frequently transmitted to humans via inhalation of aerosolized virus apparently contained in rodent excreta. Epidemiological studies have shown that peridomestic environments, especially indoor situations with active infested rodents, may represent the greatest risk for human infection (1, 6).
Hantaviruses cause persistent infections in rodents that are marked by a short acute stage, during which the levels of infectious viruses are high. Subsequently, there is a prolonged chronic stage when the infection is productive but the virus is usually present at much lower levels, which can vary cyclically. The factors contributing to hantavirus persistence in rodents are not yet clearly defined (19). A single rodent species was found to host a genetically distinct hantavirus, while transient or spillover infections occur from the primary rodent host into other species (5).
In South America, Andes (AND) hantavirus has been responsible for the large majority of more than 900 HPS cases recorded in Argentina and Chile since 1995 (18, 28). Person-to-person transmission has been described only for the viral lineage AND Sout circulating in southern Argentina and Chile (8, 29, 36, 38). Moreover, this strain and Maporal virus were the only hantaviruses to produce respiratory disease and to be lethal in hamsters (11, 20).
The Oligoryzomys longicaudatus is the reservoir of the AND virus Sout lineage (4, 17, 36). Previous studies have revealed a high prevalence of AND virus-reactive antibody in O. longicaudatus populations in southern Chile and southern Argentina (4, 25). Other species of rodents in Chile which have tested seropositive include the akodontines Abrothrix olivaceus, Abrothrix longipilis, and Akodon sanborni and two filotenes, Loxodontomys micropus and Phyllotis darwini (23, 31). There have been no reports of these species involved in human or rodent transmission, and they may represent an overflow of the virus from its typical reservoir host. In Chile's X Region (39 to 44° south), the most abundant species include O. longicaudatus, A. olivaceus and A. longipilis, which are sympatric and utilize the same general habitat, with differences in microhabitat and segregation based on seasonal activity (24). Spatial and temporal superposition of the ranges of these species have been observed at collecting stations (3).
Field studies with Sin Nombre virus (SNV) (7) indicate that viral transmission occurs primarily via a horizontal mechanism by wounds among rodents (21). However, a relationship between wounds and horizontal transmission of the AND virus in rodents was not reported. For Seoul virus animal models, infected mice shed virus in urine, feces, and saliva, and intracage transmission was efficient during the acute phase of infection (13).
The mechanism(s) by which AND virus is maintained in the rodent population is unclear. Using outdoor experimental test enclosures as a quarantine laboratory, we investigated the primary means of infection in nature of AND hantavirus. The mechanism of transmission of AND virus from seropositive to seronegative mice was studied at intra- and interspecies levels by using holding cages that allowed both direct transmission between an infected host and a healthy recipient and indirect transmission through a wire mesh or an environment contaminated with the feces and urine of an infected individual.
MATERIALS AND METHODS
Habitat design.
The outdoor experimental facility study area was located within a temperate rain forest at the San Martin Experimental Reserve (39°38′S, 73°W), Valdivia, Chile. This forest is 13 m above sea level and is characterized by volcanic soils and precipitation which exceeds 2,000 mm annually, 80% of which normally occurs in the fall and winter. The experimental area was delimited by an outer fence of heavy galvanized wire mesh and an inner fence 1 m high to prevent the entrance of potential predators and to provide adequate warning to unauthorized persons. The inner barrier was sunk 20 cm into a trench filled with gravel (26). Fine metal screening was attached to the sheet metal to raise the height of the enclosure to 1.8 m, as suggested in the literature for this type of study (2). The area was maintained clear of low-growing vegetation to facilitate the movement of researchers and the recapture of any possible escaped mice.
Each experimental habitat unit was installed by using a 200 l steel drum buried in the ground, with the top 20 cm above ground level; the drum contained a holding cage (300 × 300 × 140 mm). A total of 20 habitat units were prepared. Food, consisting primarily of safflower seeds and wheat germ, was given ad libitum. For experiments in which test mice were allowed to have only indirect contact, the cage was divided into two compartments by a wire mesh. Each of these compartments included water and food devices. Shavings were changed every 1 or 2 weeks, depending on the degree of dirtiness and humidity. Experimental cages were provided with wood shavings. Between experiments the cages were disinfected with 10% NaHClO3 or Lysol and sun dried.
Collection and serological screening of wild rodent samples.
During 2001 and 2002, rodents were trapped in different localities of the X Chilean Region by using Sherman traps. Blood and tissue samples were collected as previously described (22). Wild donors were bled only on the capture day. The immunoglobulin G (IgG) response of the rodents was detected in blood samples by using an AND virus-specific enzyme-linked immunosorbent assay (ELISA) as previously described (30). Briefly, the blood samples (including samples from the controls) were diluted 1:100 and fourfold up to 1:6,400. Recombinant AND virus nucleoprotein (N-AND) was used as a specific antigen. IgG in rodents was detected by using peroxidase-labeled affinity-purified antibody to Peromyscus leucopus IgG (heavy plus light chains) as the conjugate. All commercial reagents were from Kirkegaard and Perry. ABTS (2.2′-azino-di[3-ethyl-benzthiazoline sulfonate]) was used as the substrate for peroxidase, and absorbance was measured at 405 nm. The optical density (OD) of each test sample was subtracted from the OD of the corresponding dilution of the unspecific antigen run on the same microtiter plate. Samples with titers of less than 0.2 IgG units were considered negative. Seronegative individuals were kept in the experimental cages for a sufficient period for them to develop detectable antibodies (around 45 days), after which they were again tested to confirm seronegativity and thus qualify to be used in experimentation.
Experimental design.
All the transmission attempts were done with wild infected rodents except when experimentally infected animals were used as indicated in Results. The following tests were performed. (i) One seropositive and one seronegative rodent were placed together in the cage located within the drum for 24 h. Evidence of bites or wounds resulting from aggressive behavior was recorded. (ii) One seropositive and one seronegative individual were placed for up to 7 days on each side of a wire mesh-partitioned cage to determine transmission by the aerosol route. (iii) One seropositive animal was placed in a simple cage for 7 days and then removed and, without the cage being cleaned, was replaced by a seronegative animal for a further 7-day period in order to determine viral transmission via feces and urine. Most of the time infected and infectious rodents were passed from a naïve cage to another one or kept waiting in a separate steel drum because the number of infectious rodents was very limited.
Rodent and rodent sample handling in the experimental facility.
We adhered strictly to the biosafety recommendations of the Centers for Disease Control and Prevention of the United States in all aspects of this work (22). Animal handling was carried out in an open atmosphere. Workers were equipped with Tyvek suits fitted with respirators having high efficiency air filters. Recipient mice were recovered from the cages by using Sherman traps and removed to a handling chamber to prevent escape (26). The mice were tested for seropositivity several times by obtaining 70- to 150-μl blood samples in heparinized tubes by retro-orbital puncture under ether anesthesia (Fig. 1). Experimentally infected rodents were not bled after the seroconversion day. Urine and saliva samples were obtained from some rodents. Saliva was obtained only in rodents Ol24m, Ol25m, and Ol56m by carefully wiping the cheek and tongue areas to prevent breakage of blood vessels and was placed in tubes with Eagle's minimal essential medium with Earle's salts containing 2% heat-inactivated fetal bovine serum medium. Urine samples were collected only from rodents Ol37m and Ao43m by vesicle puncture in order to prevent blood contamination.
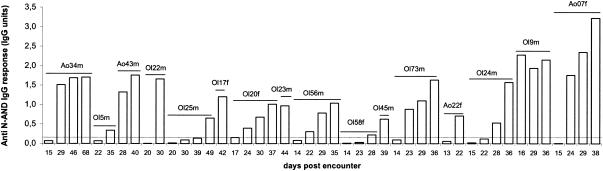
FIG. 1.
Anti-N-AND IgG responses in sera from rodents infected experimentally. Blood samples were collected at the indicated days postencounter and were examined for reactivity to the N-AND antigen by ELISA. Data are presented in IgG units, in which the OD of each test sample was divided by the OD of the positive control sample run on the same microtiter plate. Samples with titers less than 0.2 IgG units (indicated with dashed line) were considered negative.
Preparation of antisera.
Rabbits averaging 2 kg were inoculated subcutaneously with multiple injections (three times at 15-day intervals) with 200 μg of N-AND or cell-cultured AND viral fluids. Serum was obtained 20 days after the last immunization. The reactivity of the sera was checked by IgG ELISA.
RNA preparation, RT-PCR amplification, and sequencing.
Total RNA from urine and saliva samples and from lung, salivary gland, and kidney tissues of infected rodents was extracted by using Trizol and RNAid kits (Bio 101, Inc.) for RNA purification. One-step reverse transcription (RT)-PCR was performed, followed by a second round of nested or heminested PCR. Specific oligonucleotide primers for amplification and sequencing of the G1- and G2-encoding M-segment fragments (positions 27 to 445 and 2729 to 2946, respectively) were used as previously described. The amplified fragments were AND virus-numbered in the antigenome sense (7, 29). PCR products were separated on agarose gels, gel purified (QIAquick Gel Extraction Kit; QIAGEN), and sequenced by using ABI PRISM Big Dye Terminator Sequencing kits (Perkin-Elmer Applied Biosystems Division PE/ABI, Foster City, Calif.). Reactions were performed on a Perkin-Elmer GeneAmp PCR System 2400. Comparison of nucleic acid sequences was performed by using N ALIGN, a program of the PCGENE version 6.8 software (IntelliGenetics, Inc., Mountain View, Calif.).
IHC assay.
One seropositive mouse infected in nature and one seronegative mouse were caged together in the drum for 24 h. After 35 days and once the experimentally infected mouse displayed hantavirus IgG antibodies, both mice were sacrificed, and tissue samples from the lung and salivary glands were fixed in Bouin fixative for 2 to 3 days. After being dehydrated, the tissue samples were embedded in Paraplast. Sections 4-μm thick were hydrated and sequentially treated with Proteinase K (Dako, Copenhagen, Denmark) (41) and 10% H2O2 in methanol. The sections were then processed for IHC by using as the primary antibody an antiserum against recombinant N-AND and cell-cultured AND virus that was raised in rabbits (see above), and they were then diluted at 1:8,000. Incubation was in a moist chamber for 18 h at room temperature. The biotin-streptavidin-peroxidase method was used (DAKO kit K0679). 3-Amino-9-ethilcarbazol was used as the electron donor. Sections that were processed for the whole procedure but were not incubated with the primary antibody were used as controls for the immunoreaction.
Nucleotide sequence accession number.
Accession numbers of the new sequences obtained are available from GenBank.
RESULTS
Rodent population and AND virus antibody prevalence in captured animals.
During 22 months of trapping at eight grids, we captured 514 different animals, yielding 460 serum samples. The selected trapping area was in accordance with those of previous HPS case reports. The overall success rate for trapping with the Sherman traps was 10.2%.
Out of the 514 rodents captured, 209 were O. longicaudatus, 163 were A. longipilis, 98 were A. olivaceus, 24 were Rattus rattus, 8 were Loxodontomys micropus, 7 were Rattus norvegicus, 2 were Irenomys tarsalis, 1 was Pearsonnomys annectens, 1 was Mus musculus, and 1was Dromiciops gliroides. All sigmodontine rodents were tested for N-AND IgG antibodies by ELISA. A total of 23 specimens, 20 O. longicaudatus and 3 A. longipilis, were found to be positive. Total seroprevalence was 5.0%.
Few reproductive rodents were positive (4/23). The ratio of positive males to positive females was significantly greater (7:1) than the negative male to negative female ratio (1:1).
Direct intracage viral transmission.
We investigated the ability of infected mice to transmit infection to cage mates by direct transmission between an infected host and a healthy recipient.
The population was divided into susceptible and donor rodents. Seropositive donor rodents were considered infected, and within this group rodents that were able to infect at least one other animal were considered infectious donors. For the intracage experiments, animals were placed together for 24 h, and then both rodents were placed in a new cage. An infected or infectious rodent was used for a new experiment, and the recipient was quarantined for around 45 days. Out of 130 attempts to transmit infection by coinhabiting infectious donor rodents with seronegative cage mates (experimental design i), 16 cases of viral transmission were recorded, taking in account those animals that seroconverted (Table 1 and Fig. 2). Counting only infectious rodents, we obtained 17.2% (16/93) infected animals (Table 1). Differences in antibody titers by sex or species were not observed (Fig. 1).
TABLE 1.
Occurrence of transmission by gender and species from direct and indirect contact between infected or infectious donors and susceptible rodents
| Rodent encountera | No. (%) of rodents infected by direct contact between:
|
No. (%) of rodents infected by indirect contact between infected donor and susceptible rodent | |
|---|---|---|---|
| Infected donor and susceptible rodent | Infectious donor and susceptible rodent | ||
| Olm x Olm | 8/22 (9) | 8/15 (53.3) | 0/23 (0) |
| Olm x Olf | 1/24 (4.17) | 1/18 (5.6) | 0/10 (0) |
| Olf x Olm | 1/13 (7.69) | 1/13 (7.7) | 0/2 (0) |
| Olf x Olf | 2/11 (20) | 2/11 (18.2) | 0/0 (0) |
| Subtotal | 12/70 (17.4) | 12/57 (21.5) | 0/35 (0) |
| Olm x Aom | 2/25 (8) | 2/13 (15.4) | 0/16 (0) |
| Olm x Aof | 2/15 (13.33) | 2/9 (22.2) | 0/4 (0) |
| Olf x Aom | |||
| Olf x Aof | 0/1 (0) | ||
| Subtotal | 4/40 (10) | 4/22 (18.2) | 0/21 (0) |
| Olm x Alm | 0/9 (0) | 0/6 (0) | 0/2 (0) |
| Olm x Alf | 0/11 (0) | 0/8 (0) | 0/3 (0) |
| Olf x Alm | 0/1 (0) | ||
| Olf x Alf | |||
| Subtotal | 0/20 (0) | 0/14 (0) | 0/6 (0) |
| Total | 16/130 (12.3) | 16/93 (17.2) | 0/62 (0) |
Olm, O. longicaudatus male; Olf, O. longicaudatus female; Aom, A. olivaceus male; Aof, A. olivaceus female; Alm, A. longipilis male; Alf A. longipilis female; x, encounter with.
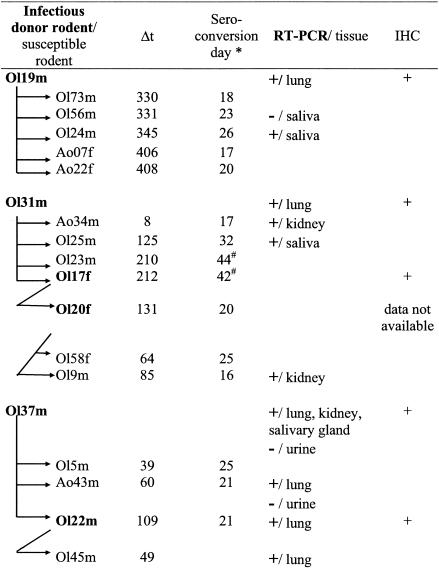
FIG. 2.
Intracage experiments indicating positive transmission chains related to the date of 24-h encounter. Distribution of AND viral antigen and detection of viral RNA in tissues are shown. IHC was performed on tissues from the salivary glands of infectious rodents. Δt, interval between date of first positive serology of donor rodent and date of viral transmission from donor to susceptible rodent; Olm, O. longicaudatus male; Olf, O. longicaudatus female; Aom, A. olivaceus male; Aof, A. olivaceus female; *, estimate by linear regression of IgG OD values for each rodent; #, unique serum sample; +, positive transmission.
When rodent wounds from 91 experimental encounters were analyzed, we found two seropositive individuals who had been wounded and six seropositive individuals who had not been wounded. In this way, we found around 9% infected animals in both groups. (Table 2).
TABLE 2.
Comparison of number of positive viral transmissions between infectious and susceptible rodents by gender and species
| Rodent encountera | No. of wounded rodents/no. of encounters | No. of infected rodents/no. of wounded rodents | No. of infected rodents/no. of rodents not wounded |
|---|---|---|---|
| Olm x Olm | 5/11 | 1/5 | 2/6 |
| Olm x Olf | 6/10 | 0/6 | 0/4 |
| Olf x Olm | 3/13 | 0/3 | 1/10 |
| Olf x Olf | 2/11 | 0/2 | 2/9 |
| Subtotal | 16/45 | 1/16 | 5/29 |
| Olm x Aom | 0/11 | 0/0 | 0/11 |
| Olm x Aof | 2/15 | 1/2 | 1/13 |
| Subtotal | 2/26 | 1/2 | 1/24 |
| Olm x Alm | 1/9 | 0/1 | 0/8 |
| Olm x Alf | 3/11 | 0/3 | 0/8 |
| Subtotal | 4/20 | 0/4 | 0/16 |
| Total | 22/91 | 2/22 (9.1%) | 6/69 (8.7%) |
Olm, O. longicaudatus male; Olf, O. longicaudatus female; Aom, A. olivaceus male; Aof, A. olivaceus female; Alm, A. longipilis male; Alf, A. longipilis female; x, encounter with.
Indirect viral transmission.
Another aim of this study was to examine indirect transmission through an environment contaminated by an infected host. None of the 27 experiments in which infected male O. longicaudatus were exposed for 7 days to healthy O. longicaudatus, A. olivaceus, or A. longipilis through a wire mesh cage (experimental design ii) resulted in transmission of the virus infection. Similarly, 20 experiments (8 of 20 using infectious donors) done in order to determine viral transmission via feces and urine were negative (experimental design iii). Four O. longicaudatus and three A. olivaceus were used as susceptible rodents in the dirty cages (Table 1).
Efficiency of AND virus infection by species and gender.
To examine whether gender influences AND virus infection, the same 2 infectious female O. longicaudatus rodents were placed in contact with 13 male and 11 female susceptible O. longicaudatus; we obtained one male and two female seropositive rodents (Table 1). The numbers of males and females that became infected differed when transmission between Oligoryzomys species was considered. Female rodents were less susceptible than males (5 versus 57%) when we considered only encounters with proven infectious male donor rodents. Encounters between animals of the same gender transmitted the infection more efficiently than those between animals of different genders (Table 1). Four out of 22 direct-contact encounters between O. longicaudatus and A. olivaceus resulted in viral transmission with approximately the same efficiency, regardless of the susceptible rodent's gender. Although male O. longicaudatus (females were not tested) were able to infect A. olivaceus, A. longipilis could not be infected in our experimental conditions (Fig. 3). A distribution of encounters over time is shown in Fig. 3. We could not obtain a cyclic time pattern of infection related to the day of encounter, suggesting that more than one variable influences transmission.
FIG. 3.
Timeline (in weeks) of intracage experiments with intra- and interspecies direct contacts between susceptible and infectious donor rodents. Ol, O. longicaudatus; Ao, A. olivaceus; Al, A. longipilis; *, rodent infected in experimental encounter. Filled blocks indicate rodents who tested positive; underlining indicates male rodents.
Duration of persistent infection.
To examine whether the reservoir host for AND virus is persistently infected in nature and to determine how efficiently it transmits virus over time, rodent Ol31m was placed in contact with noninfected animals at different days until day 428 (Fig. 3). Viral transmission was efficient on days 8, 125, 210, and 212. On day 512 the animal was sacrificed, and lung tissue was examined for the viral genome by RT-PCR, which was positive (Fig. 2). Rodent Ol19m was able to infect others until day 408, although before day 330 it did not transmit virus to any of the three (two male and one female) susceptible A. olivaceus or four susceptible female O. longicaudatus rodents (Fig. 3). Lung tissue from rodent Ol19m was positive by RT-PCR (Fig. 2).
Viral RNA was identified in saliva samples from two out of three rodents, rodents Ol24m and Ol25m, collected as much as 299 and 519 days, respectively, after the rodents had been infected by a 24-h encounter with an infectious donor rodent, rodent Ol19m or Ol31m. Unfortunately, we did not monitor saliva samples during the experiments because the prevalence of transmission through saliva and not through excreta appeared as a result of the experiments. No nucleotide differences were found between samples from rodents Ol24m and Ol19m or between those from rodents Ol25m and Ol31m when the G1- and G2-encoding M fragments (635 nucleotides) were analyzed.
Although 4 serologically positive male wild-caught O. longicaudatus rodents were unable to infect either 9 susceptible O. longicaudatus rodents (3 males and 6 females) or 19 A. olivaceus rodents (13 males and 6 females), viral RNA from their lungs was amplified. RT-PCR amplification of samples from the four O. longicaudatus-infected rodents was positive for three animals 274 days after capture and after 295 days for the other. Viral antigen was also in these tissues by IHC.
Viral RNA was not amplified in urine obtained by vesicle puncture either in infectious rodent Ol37m 463 days after capture or in infectious rodent Ao43m after 235 days of infection. However, in both animals viral RNA was amplified from lung tissue. Kidney and salivary glands from infectious rodent Ol37m were also positive by RT-PCR (Fig. 2).
IHC.
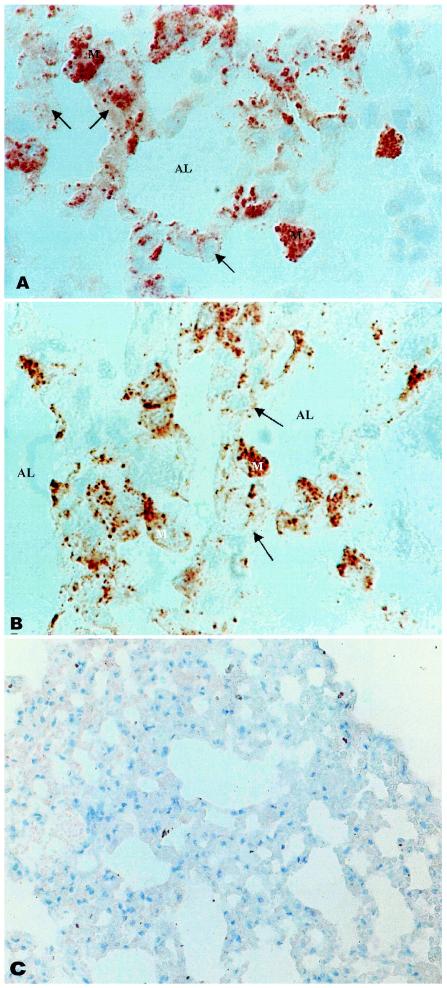
The results of IHC of lung tissue from naturally and experimentally infected mice are shown in Fig. 4. By using cell-cultured AND virus antiserum, immunoreactive hantavirus proteins were detected in most of the epithelial cells lining the alveoli and in some endothelial cells of the septal capillaries. In some epithelial cells, the immunoreaction appeared as scarce granules distributed throughout the cytoplasm; other cells were loaded with immunoreactive particles (Fig. 4A). No reaction was detected in control tissue samples from noninfected rodents (Fig. 4C). IHC of the salivary glands also revealed a strong reaction, while control sections showed no reaction (data not shown).
FIG. 4.
Hantavirus immunoreactivity is localized in epithelial cells (arrows) lining the alveolar lumen (AL) and in macrophages (M). Paraffin sections of the lung of an infectious (A) and an experimentally infected (B) rodent are shown. For the infectious rodent used as the control, a section (C) was processed for IHC but was not incubated with antibodies against AND virus proteins.
The cell distribution and amount of immunoreactive AND virus proteins in the lung of the experimentally infected mouse (Fig. 4B) completely resembled that of the naturally infected mouse. When N-AND immunosera was used, a similar staining pattern was obtained (data not shown).
DISCUSSION
Our study was designed to contribute to an understanding of the timing and conditions under which transmission of AND virus in reservoir populations takes place.
The simulated habitat system used in this work complied with biosafety level 4 conditions similar to those previously described (2). This study represents the first experimental manipulation with AND hantavirus in rodents, showing horizontal transmission of the virus between wild mice by a direct contact route.
Several important differences are found when our results are compared with a previous work on SNV, where a single case of transmission between Peromyscus maniculatus occurred in a total of 54 attempts at 14-day intervals at exposure to experimentally infected animals in the same cage (2). At variance, AND virus transmitted virus more efficiently among cage mates; of 130 attempts at transmission by direct contact, 12.3% were successful. The efficiency rate is even higher (16 of 93) when only rodents that proved to be infectious are considered. From these 93 attempts, 57 encounters were done with O. longicaudatus as susceptible rodents, 22 were done with A. olivaceus as susceptible rodents, and only 14 were done with A. longipilis as susceptible rodents. This last species has not been infected. However, because of the low number of animals used in the experiments, we cannot completely exclude the possibility that they could become infected. The lack of virus transmission between infected and healthy animals coinhabiting the same cage and separated by a wire mesh for 7 days could be attributed to the lack of physical contact or to the experimental design properties, which did not include air turbulence, which might mimic the conditions in nature.
In most infected animals, the anti-N-AND antibodies were evident 16 to 26 days after experimental transmission (Fig. 1). This period is similar to the incubation period of 12 to 27 days estimated for AND virus in humans (28). For SNV, this period is thought to be 9 to 33 days (40). Our results also reaffirm the need for maintaining test animals in quarantine long enough to produce detectable circulating antibodies before declaring them seronegative (2).
A laboratory study of another etiologic agent of HPS, Black Creek Canal virus, in its natural reservoir, Sigmodon hispidus, resulted in persistent infections and virus shedding for at least 150 days (12). For AND virus, infectious virus was determined to be present at least as long as 408 days from the last positive transmission. The delay in transmission from rodent Ol19m is surprising, but it could be due to the use of rodents of less-susceptible gender and species, as was observed with rodent Ol37m, which did not transmit the virus during a 7-month period when it had no encounters with male O. longicaudatus rodents.
Intermittent shedding may have occurred during persistent infection, as transmission was effective in 57% of the attempts where the donor was infectious and the gender and species of the receptor rodent were the most appropriated. From these experiments it is not clear why nearly one out of two encounters rendered productive transmission. Bleeding infectious donors could have been useful in finding out if intermittent shedding occurred, but as this study was designed to learn the capability of Andes virus-infected rodents to transmit infection to other animals, we tried to keep conditions as natural as possible, avoiding stressing rodents by manipulation or introducing other variables that could modify the mimic the donor rodent system and viral transmission. The types of interactions we have attempted to study in the present investigation do not reflect all aspects of behavior thought to be important in determining patterns of infection. Also important is the fact that at the time the experiments were designed we had not planned to evaluate seasonal variations in transmission efficiency. However, we observed that there were twice as many positive transmissions from intra-O. longicaudatus encounters in spring and summer than in fall or winter. A study of wild-caught Apodemus species in eastern Russia suggested increased viral replication in the spring and summer months when rodents are most active, probably influenced by seasonal physiological changes (35).
Negative results obtained in attempts to infect mice by the fecal and/or urine route are not definitive, due to the small number of tests performed. We obtained negative PCR results from urine from an infectious rodent, although a kidney sample was positive. This finding could be due to the virus being located only in blood or tissue cells. Nevertheless, in three urine samples we could not detect viral genomic RNA although the virus was present intermittently in urine. Whether urine represents an important source of infection needs more investigation, since human infection has been postulated as occurring by contact with rodent excretory residues in low-income dwellings (16). Seoul virus-infected rats excrete virus in urine but virus shedding was not consistently observed (15).
Horizontal transmission between rodents through biting and direct contact between mucosae during aggressive encounters between larger, heavier males has been described for P. maniculatus (21). Also, a positive relationship has been established between seropositivity and wounded animals, both with hantavirus reservoirs of hemorrhagic fever with renal syndrome (37) and reservoirs of SNV (21). We have found that infected individuals showed as much evidence of wounds as noninfected animals. Interestingly, nonaggressive contact patterns have been described for the rodent species studied in this work: they may mount each other or engage in sniffing, touching, and mutual exploration, during which physical contact occurs (10). Collections carried out in 1998 and 1999 in different sectors of Chile's X Region produced different percentages of wounded animals among the three most abundant rodent species (3); it was suggested that these species showed a hierarchical pattern of aggression, with A. olivaceus being the most aggressive, followed by O. longicaudatus, and finally by A. longipilis, which had the lowest level of aggressive behavior either in intraspecies encounters or in interspecies encounters with O. longicaudatus (10). The presence of scars on the head, ears, body, or tail may be considered indicators of intraspecies or interspecies encounters. The results obtained either in the field or in this AND virus transmission experiment should be taken as evidence that viral transmission following bites does not account for the greater prevalence of infection in O. longicaudatus. Our data underscore the significance of bite wounds or scars in AND virus infection. Moreover, infection in the susceptible rodents resulted in persistent infection and viral shedding into the environment, as was demonstrated by the chains of infection. Based upon our transmission data, it seems unlikely that wounds play a major role in the maintenance of AND virus. It is likely that other factors, such as grooming or aerosol transmission, are required for efficient AND virus transmission. Thus, horizontal transmission in this species is probably mediated by the presence of the virus in salivary secretions that, in turn, contaminate other elements (like hair or food); aerosols containing the virus could then be formed after saliva is dried out. The infection might be transmitted by inhaling aerosols from contaminated materials or by directly inhaling saliva aerosols, as happens in person to person transmission in close and prolonged contact situations described in Argentina. The primary mode of transmission appears to be direct mucous membrane (eyes, nose, and mouth) contact with saliva or respiratory droplets (29, 32). Whether intermittent secretion of the virus into rodent saliva could account for the low incidence of transmission remains to be examined.
Horizontal transmission to cage mates was also demonstrated, with the highest transmission occurring when male O. longicaudatus rodents were used as recipients. It has already been suggested that virus maintenance in endemic foci might be related to the grooming behavior of voles (39). Field surveys of several rodent species, including brush mice, deer mice, harvest mice, bank voles, and cotton rats, indicate that males are more commonly infected than females (14). Our experimental data confirm these results only for O. longicaudatus to O. longicaudatus transmission. In North America, the prevalence of antibody to SNV among male deer mice, brush mice, and western harvest mice is at least twice that among females (21), and scarring appears associated with antibody in some of these species. In our experiments, males and females are not equally susceptible to infection with AND virus. On the other hand, male and female rats are equally susceptible to infection with Seoul virus, and it was shown that males shed virus in saliva and feces longer than females (9), which could be also inferred for rodents with AND virus. Differences in behavior due to gender could be an alternative explanation.
Although we have demonstrated that A. olivaceus can be infected, the epidemiological relevance of A. olivaceus in South America could be clarified only by genetic studies matching the viruses from this host species with viruses obtained from human patients.
The question of how, if at all, the virulence of any particular pathogen is linked to its transmissibility is important, because transmission determines the evolutionary success of pathogenic organisms. AND hantavirus is harbored in several tissues of the infected rodent reservoir, but the salivary glands and the lung seem to be most important in the transmission mechanism. It is generally believed that hantavirus infection in rodents is lifelong and has no deleterious effects (19). Both SNV and Hantaan primarily infect endothelial cells without causing apparent cytopathic effects (41). In our study, epithelial cells were as immunoreactive as endothelial cells. Studies focusing on localization of the virus in epithelial cells by using specific cell markers are under way in our laboratories.
There are two significant implications of our results. A significant observation of this investigation is that experimental transmission of AND virus is possible between rodents of the O. longicaudatus species and between those of O. longicaudatus and A. olivaceus. The other contribution is insight into the probable mechanisms of transmission of AND virus within reservoir populations, which indicates that saliva is the principal mode of transmission but does not discard the fecal and/or urine route.
There is clearly a need to obtain direct estimates of the contact behavior important in transmission of aerosol- or saliva-borne close-contact infections in both rodents and humans.
Reservoir studies are an essential component of any integrated public health response to emerging zoonotic diseases. Although the results derived from this study are not generalizable to the wild population, the study did identify some interesting patterns of contact which may have epidemiological implications.
Acknowledgments
This work was supported by FONDEF-Conicyt grant D99I 1105.
Footnotes
This paper is a tribute to our late colleague, Luz A. González, coapplicant of the grant, who died in January 2002.
REFERENCES
- 1.Armstrong, L. R., S. R. Zaki, M. J. Goldoft, R. L. Todd, A. S. Khan, R. F. Khabbaz, T. G. Ksiazek, and C. J. Peters. 1995. Hantavirus pulmonary syndrome associated with entering or cleaning rarely used, rodent-infested structures. J. Infect. Dis. 172:1166. [DOI] [PubMed] [Google Scholar]
- 2.Botten, J., K. Mirowsky, D. Kusewitt, M. Bharadwaj, J. Yee, R. Ricci, R. M. Feddersen, and B. Hjelle. 2000. Experimental infection model for Sin Nombre hantavirus in the deer mouse (Peromyscus maniculatus). Proc. Natl. Acad. Sci. USA 97:10578-10583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cadiz, R. 2000. Estudio de la seroprevalencia de hantavirus en reservorios silvestres en distintos habitat de la décima región y análisis de su comportamiento temporal en poblaciones de roedores del fundo experimental San Martín. Tesis de grado, medico veterinario. Universidad Austral de Chile, Valdivia.
- 4.Cantoni, G., P. Padula, G. Calderon, J. Mills, E. Herrero, P. Sandoval, V. Martinez, N. Pini, and E. Larrieu. 2001. Seasonal variation in prevalence of antibody to hantaviruses in rodents from southern Argentina. Trop. Med. Int. Health 6:811-816. [DOI] [PubMed] [Google Scholar]
- 5.Childs, J. E., T. G. Ksiazek, C. F. Spiropoulou, J. W. Krebs, S. Morzunov, G. O. Maupin, K. L. Gage, P. E. Rollin, J. Sarisky, R. E. Enscore, et al. 1994. Serologic and genetic identification of Peromyscus maniculatus as the primary rodent reservoir for a new hantavirus in the southwestern United States. J. Infect. Dis. 169:1271-1280. [DOI] [PubMed] [Google Scholar]
- 6.Douglass, R. J., A. J. Kuenzi, C. Y. Williams, S. J. Douglass, and J. N. Mills. 2003. Removing deer mice from buildings and the risk for human exposure to Sin Nombre virus. Emerg. Infect. Dis. 9:390-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elliott, L. H., T. G. Ksiazek, P. E. Rollin, C. F. Spiropoulou, S. Morzunov, M. Monroe, C. S. Goldsmith, C. D. Humphrey, S. R. Zaki, J. W. Krebs, et al. 1994. Isolation of the causative agent of hantavirus pulmonary syndrome. Am. J. Trop. Med. Hyg. 51:102-108. [DOI] [PubMed] [Google Scholar]
- 8.Enria, D., P. Padula, E. L. Segura, N. Pini, A. Edelstein, C. R. Posse, and M. C. Weissenbacher. 1996. Hantavirus pulmonary syndrome in Argentina. Possibility of person to person transmission. Medicina (B. Aires). 56:709-711. [PubMed] [Google Scholar]
- 9.Glass, G. E., J. E. Childs, G. W. Korch, and J. W. LeDuc. 1988. Association of intraspecific wounding with hantaviral infection in wild rats (Rattus norvegicus). Epidemiol. Infect. 101:459-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez, L. A., H. Gaete, C. Jofre. 1990. Variación estacional de los patrones conductuales en Oryzomys longicaudatus y Akodon longipilis en encuentros intraespecíficos e interespecíficos. Bol. Soc. Biol. Concepción 61:63-70. [Google Scholar]
- 11.Hooper, J. W., T. Larsen, D. M. Custer, and C. S. Schmaljohn. 2001. A lethal disease model for hantavirus pulmonary syndrome. Virology 289:6-14. [DOI] [PubMed] [Google Scholar]
- 12.Hutchinson, K. L., P. E. Rollin, and C. J. Peters. 1998. Pathogenesis of a North American hantavirus, Black Creek Canal virus, in experimentally infected Sigmodon hispidus. Am. J. Trop. Med. Hyg. 59:58-65. [DOI] [PubMed] [Google Scholar]
- 13.Klein, S. L., B. H. Bird, and G. E. Glass. 2001. Sex differences in immune responses and viral shedding following Seoul virus infection in Norway rats. Am. J. Trop. Med. Hyg. 65:57-63. [DOI] [PubMed] [Google Scholar]
- 14.Klein, S. L., B. H. Bird, and G. E. Glass. 2000. Sex differences in Seoul virus infection are not related to adult sex steroid concentrations in Norway rats. J. Virol. 74:8213-8217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee, H. W., L. J. Baek, and K. M. Johnson. 1982. Isolation of Hantaan virus, the etiologic agent of Korean hemorrhagic fever, from wild urban rats. J. Infect. Dis. 146:638-644. [DOI] [PubMed] [Google Scholar]
- 16.Lee, H. W., and G. van der Groen. 1989. Hemorrhagic fever with renal syndrome. Prog. Med. Virol. 36:62-102. [PubMed] [Google Scholar]
- 17.Levis, S. 1998. Reservoirs and genetic viral diversity. Medicina (B. Aires) 58(Suppl. 1):37. (In Spanish.) [PubMed] [Google Scholar]
- 18.Lopez, N., P. Padula, C. Rossi, M. E. Lazaro, and M. T. Franze-Fernandez. 1996. Genetic identification of a new hantavirus causing severe pulmonary syndrome in Argentina. Virology 220:223-226. [DOI] [PubMed] [Google Scholar]
- 19.Meyer, B. J., and C. S. Schmaljohn. 2000. Persistent hantavirus infections: characteristics and mechanisms. Trends Microbiol. 8:61-67. [DOI] [PubMed] [Google Scholar]
- 20.Milazzo, M. L., E. J. Eyzaguirre, C. P. Molina, and C. F. Fulhorst. 2002. Maporal viral infection in the Syrian golden hamster: a model of hantavirus pulmonary syndrome. J. Infect. Dis. 186:1390-1395. [DOI] [PubMed] [Google Scholar]
- 21.Mills, J. N., T. G. Ksiazek, B. A. Ellis, P. E. Rollin, S. T. Nichol, T. L. Yates, W. L. Gannon, C. E. Levy, D. M. Engelthaler, T. Davis, D. T. Tanda, J. W. Frampton, C. R. Nichols, C. J. Peters, and J. E. Childs. 1997. Patterns of association with host and habitat: antibody reactive with Sin Nombre virus in small mammals in the major biotic communities of the southwestern United States. Am. J. Trop. Med. Hyg. 56:273-284. [DOI] [PubMed] [Google Scholar]
- 22.Mills, J. N., T. L. Yates, J. E. Childs, R.R. Parmenter, T. G. Ksiazek, P. E. Rollin, and C. J. Peters. 1995. Guidelines for working with rodents potentially infected with hantavirus. J. Mammal. 76:716-722. [Google Scholar]
- 23.Murua, R. 1999. Hantavirus en Chile: los mastozoologos como un grupo ocupacional de riesgo epidemiólogico. Rev. Chil. Hist. Nat. 72:7-12. [Google Scholar]
- 24.Murua, R., L. A. Gonzalez, and P. L. Meserve. 1986. Population ecology of Oryzomys longicaudatus philippii (Rodentia: Cricetidae) in southern Chile. J. Anim. Ecol. 55:281-293. [Google Scholar]
- 25.Murua, R., M. Navarrete, R. Cadiz, R. Figueroa, P. Padula, L. Zaror, R. Mansilla, L. Gonzalez, and A. Muñoz-Pedreros. 2003. Hantavirus pulmonary syndrome: current situation among rodent reservoirs and human population in the 10th region, Chile. Rev. Med. Chil. 131:169-176. (In Spanish.) [PubMed] [Google Scholar]
- 26.Murúa, R. J., C. Jofre, R. Figueroa, R. Cadiz, M. Navarrete, E. Pizarro, E. Rodríguez, P. Padula, and L. Zaror. 2002. Transmisión intra e interespecífica de hantavirus (Cepa Andes) en dos roedores sigmodontinos. Biol. Res. 35.R149.
- 27.Nichol, S. 2001. Bunyaviruses, p. 1603-1633. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus, Fields virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 28.Padula, P. J., S. B. Colavecchia, V. P. Martinez, M. O. Gonzalez Della Valle, A. Edelstein, S. D. Miguel, J. Russi, J. M. Riquelme, N. Colucci, M. Almiron, and R. D. Rabinovich. 2000. Genetic diversity, distribution, and serological features of hantavirus infection in five countries in South America. J. Clin. Microbiol. 38:3029-3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Padula, P. J., A. Edelstein, S. D. Miguel, N. M. Lopez, C. M. Rossi, and R. D. Rabinovich. 1998. Hantavirus pulmonary syndrome outbreak in Argentina: molecular evidence for person-to-person transmission of Andes virus. Virology 241:323-330. [DOI] [PubMed] [Google Scholar]
- 30.Padula, P. J., C. M. Rossi, M. O. Della Valle, P. V. Martinez, S. B. Colavecchia, A. Edelstein, S. D. Miguel, R. D. Rabinovich, and E. L. Segura. 2000. Development and evaluation of a solid-phase enzyme immunoassay based on Andes hantavirus recombinant nucleoprotein. J. Med. Microbiol. 49:149-155. [DOI] [PubMed] [Google Scholar]
- 31.Pavletic, B. C. 2000. Hantavirus: su distribución geográfica entre los roedores silvestres de Chile. Rev. Chil. Infect. 17:186-196. [Google Scholar]
- 32.Pinna, D. 2004. Nueva evidencia epidemiológica y molecular a favor de la transmisión interhumana para el linaje Sout del Hantavirus Andes. Medicina (B. Aires) 64:43-46. [PubMed] [Google Scholar]
- 33.Schmaljohn, C., and B. Hjelle. 1997. Hantaviruses: a global disease problem. Emerg. Infect. Dis. 3:95-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmaljohn, C. S. 1996. Molecular biology of hantaviruses, p. 63-90. In R. M. Elliott (ed.), The Bunyaviridae. Plenum Press, New York, N.Y.
- 35.Slonova, R. A., E. A. Tkachenko, T. I. Astakhova, and T. K. Dzagurova. 1990. Hantaan virus serotypes circulating in foci of the Far Eastern region of the USSR. Vopr. Virusol. 35:391-393. (In Russian.) [PubMed] [Google Scholar]
- 36.Toro, J., J. D. Vega, A. S. Khan, J. N. Mills, P. Padula, W. Terry, Z. Yadon, R. Valderrama, B. A. Ellis, C. Pavletic, R. Cerda, S. Zaki, W. J. Shieh, R. Meyer, M. Tapia, C. Mansilla, M. Baro, J. A. Vergara, M. Concha, G. Calderon, D. Enria, C. J. Peters, and T. G. Ksiazek. 1998. An outbreak of hantavirus pulmonary syndrome, Chile, 1997. Emerg. Infect. Dis. 4:687-694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsai, T. F. 1987. Hemorrhagic fever with renal syndrome: mode of transmission to humans. Lab. Anim. Sci. 37:428-430. [PubMed] [Google Scholar]
- 38.Wells, R. M., S. Sosa Estani, Z. E. Yadon, D. Enria, P. Padula, N. Pini, J. N. Mills, C. J. Peters, and E. L. Segura. 1997. An unusual hantavirus outbreak in southern Argentina: person-to-person transmission? Hantavirus Pulmonary Syndrome Study Group for Patagonia. Emerg. Infect. Dis. 3:171-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yanagihara, R., H. L. Amyx, and D. C. Gajdusek. 1985. Experimental infection with Puumala virus, the etiologic agent of nephropathia epidemica, in bank voles (Clethrionomys glareolus). J. Virol. 55:34-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Young, J. C., G. R. Hansen, T. K. Graves, M. P. Deasy, J. G. Humphreys, C. L. Fritz, K. L. Gorham, A. S. Khan, T. G. Ksiazek, K. B. Metzger, and C. J. Peters. 2000. The incubation period of hantavirus pulmonary syndrome. Am. J. Trop. Med. Hyg. 62:714-717. [DOI] [PubMed] [Google Scholar]
- 41.Zaki, S. R., P. W. Greer, L. M. Coffield, C. S. Goldsmith, K. B. Nolte, K. Foucar, R. M. Feddersen, R. E. Zumwalt, G. L. Miller, A. S. Khan, et al. 1995. Hantavirus pulmonary syndrome. Pathogenesis of an emerging infectious disease. Am. J. Pathol. 146:552-579. [PMC free article] [PubMed] [Google Scholar]