Abstract
We report the case of a 17‐year‐old boy with cystic fibrosis (CF) who presented with persistent cough; after starting intravenous antibiotics for Pseudomonas aeruginosa he underwent a computed tomography (CT) scan of the chest. CT revealed extensive consolidation in the right lower lobe with relative bronchus obstruction; the cause of bronchial obstruction was detected in the mediastinal window, corresponding to a bronchial tree‐shaped, thick, tenacious mucous plug. This was extracted 48 h after unresponsive bronchial washing and endobronchial instillation of rhDNAse, using foreign‐body forceps, with subsequent resolution of cough. This case, which is the second report of plastic bronchitis in CF, was resolved by mechanical removal of the mucous plug, suggesting that a careful observation of CT imaging may guide intervention aimed at resolution of atelectasis.
Keywords: Atelectasis, cystic fibrosis, DNAse, imaging, plug
Introduction
Patients with cystic fibrosis (CF) are characterized by the production of abundant and purulent sputum, which can cause mucus impaction and lead to the development of bronchiectases.
The formation of mucus casts that obstruct the airway characterizes plastic bronchitis, a rare condition described only in one patient with CF 1. In this patient the cast consisted mainly of mucin which rendered the treatment of choice in CF patients with atelectasis, unsuccessful in this case.
Plastic bronchitis is a rare condition where bronchial casts are formed and are removed either by expectoration or bronchoscopy.
We describe a second case of plastic bronchitis in CF that required mechanical removal of the cast under guidance from CT images.
Case Report
A 17‐year‐old boy with CF was admitted to the CF Centre of our Hospital because of a worsening cough. He reported an uncomfortable, irritating cough with a very small amount of sputum. At the age of 5 months, the patient had been diagnosed with CF with homozygosity for the F508 mutation in the gene encoding CF transmembrane conductance regulator (CFTR), with pancreatic insufficiency. He had chronic colonization of Pseudomonas aeruginosa in bronchial secretions. At admission, forced expiratory volume in 1 s (FEV1) was 103% of the predicted value. As the cough persisted even after starting intravenous (IV) antibiotic therapy for Pseudomonas aeruginosa, a CT scan of the chest was performed (Fig. 1), revealing extensive consolidation in the right lower lobe with relative bronchus obstruction (panel A). In the mediastinal window, the cause of the bronchial obstruction was detected. It corresponded (panel B, arrowheads) to a bronchial tree‐shaped, thick, tenacious mucous plug (panel C), obstructing the right basal pyramid. This was extracted 48 h after unresponsive bronchial washing and endobronchial instillation of rhDNAse, using foreign‐body forceps, which resulted in subsequent resolution of cough as seen in the CT image (panel D). Histology showed an acellular bronchial cast.
Figure 1.
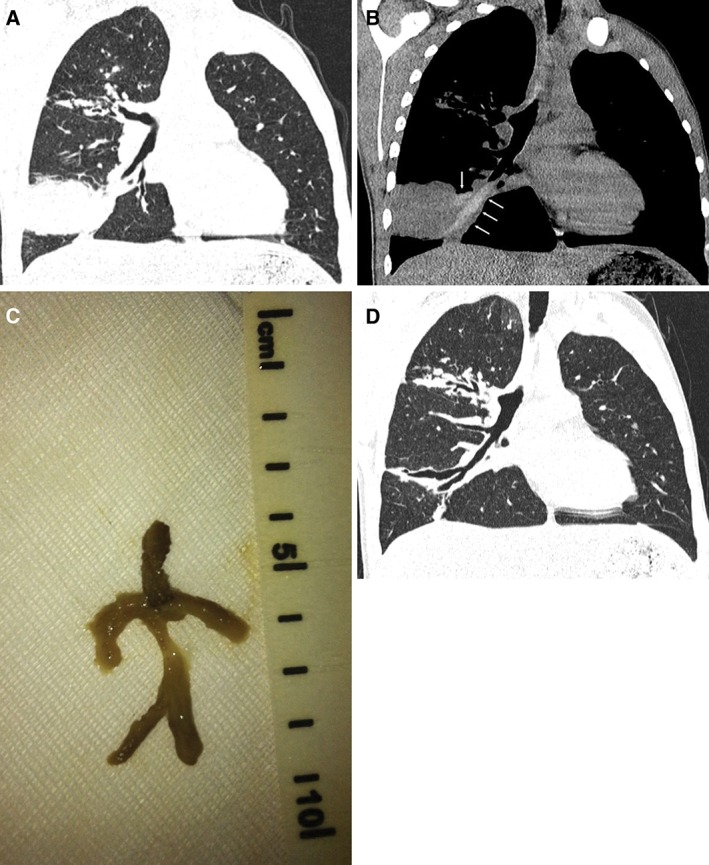
Extensive consolidation in the right lower lobe with relative bronchus obstruction (A). Bronchial tree‐shaped mucous plug (B arrowheads, and C). Resolution of CT image after extraction (D).
Discussion
Atelectasis occurs as a result of mucous plugs and severe parenchymal disease in CF. Patients typically respond to IV antibiotics and chest physiotherapy; however, it may persist predisposing to localized, severe bronchiectasis. Inhaled rhDNase has been used in CF 2 to reduce sputum viscosity by depolymerizing DNA derived from disintegrating neutrophils that are responsible for the high viscosity of patients’ secretions. Moreover, rhDNAse has successfully been used also by endobronchial instillation in a small series of patients resistant to conventional therapy with antibiotics, physiotherapy and inhaled rhDNAse 3. All these treatments were unsuccessfully applied in our case, including endobronchial instillation of rhDNAse. Resolution of symptoms resulted after extraction of a bronchial tree‐shaped, thick, tenacious mucous plug using foreign‐body forceps.
To the best of our knowledge, only one case of plastic bronchitis has previously been reported in CF by Mateos‐Corral et al. 1 where a 2½‐year‐old child expectorated a large mucus cast showing airway structure, after unresponsive suctioning, irrigation with saline and local administration of dornase alfa, used to mobilize the plug. The authors reported that, on histology, the casts were composed of laminated mucin with microscopic appearance and histochemical staining characteristics of an acellular bronchial cast, which explains why dornase alfa was unable to dissolve it. Similarly to the case reported by Mateos‐Corral et al., histology in our case showed an acellular bronchial cast.
The interest of our case report, apart from the rarity, lies in the exact definition that CT imaging provided, prompting a more invasive approach that led to removing of the mucus plug with foreign‐body forceps, whereas previous treatment, including the endobronchial instillation of rhDNAse, was unsuccessful in clearing the bronchial tree. Pulmonary improvement of CF in children treated with inhaled DNase has been demonstrated by high‐resolution CT (HRCT) imaging 4. Our case emphasizes the importance that CT scanning has in localizing and qualitatively describing focal areas of parenchymal abnormality of a mucous plug that may be responsive to mechanical removal after a previous medical and endoscopic treatment failure. The use of HRCT, as performed in our case, with low‐radiation‐dose protocols for whole lung imaging, provides radiation doses similar to those of chest X‐rays 5, so that the airways can be identified and followed longitudinally.
In conclusion, our case report, which is the second report of plastic bronchitis in CF, documented successful resolution with mechanical removal of the mucous plug, and suggests that careful observation of CT imaging may guide intervention aimed at resolution of atelectasis.
Disclosure Statement
No conflict of interest declared
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Acknowledgment
The authors thank the mother language speaker who revised the English of the article.
Salamone, I. , Mondello, B. , Lucanto, M.C. , Cristadoro, S. , Lombardo, M. and Barone, M. (2017) Bronchial tree‐shaped mucous plug in cystic fibrosis: imaging‐guided management. Respirology Case Reports, 5 (2), e00214. doi: 10.1002/rcr2.214.
Associate Editor: John Kolbe
References
- 1. Mateos‐Corral D, Cutz E, Solomon M, et al. 2009. Plastic bronchitis as an unusual cause of mucus plugging in cystic fibrosis. Pediatr. Pulmonol. 44:939–940. [DOI] [PubMed] [Google Scholar]
- 2. Fuchs HJ, Borowitz DS, Christiansen DH, et al. 1994. Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. The Pulmozyme Study Group. N. Engl. J. Med. 331:637–642. [DOI] [PubMed] [Google Scholar]
- 3. Slattery DM, Waltz DA, Denham B, et al. 2001. Bronchoscopically administered recombinant human DNase for lobar atelectasis in cystic fibrosis. Pediatr. Pulmonol. 31:383–388. [DOI] [PubMed] [Google Scholar]
- 4. Nasr SZ, Kuhns LR, Brown RW, et al. 2001. Use of computerized tomography and chest X‐rays in evaluating efficacy of aerosolized recombinant human DNase in cystic fibrosis patients younger than age 5 years: a preliminary study. Pediatr. Pulmonol. 31:383–388. [DOI] [PubMed] [Google Scholar]
- 5. Santamaria F, Grillo G, Guidi G, et al. 1998. Cystic fibrosis: when should high‐resolution computed tomography of the chest be obtained? Pediatrics 101:908–913. [DOI] [PubMed] [Google Scholar]


