Abstract
Aims
To estimate cannabis use disorder (CUD) trajectory classes from ages 14 through 30 and compare classes on clinical characteristics, risk factors, and psychosocial outcomes.
Design
Four waves (T1-T4) of data from an epidemiological study of psychopathology among a regionally representative sample. Trajectory classes described risk for CUD as a function of age. The number of classes was determined by model fit.
Setting
Participants were randomly selected from nine high schools in western Oregon, U.S.A.
Participants
The sample included 816 participants (age at T1 M = 16.6, SD = 1.2; 56% female; 92% White).
Measurements
Participants completed diagnostic interviews, Child Trauma Questionnaire, Social Adjustment Scale, and items adapted from the Wisconsin Manual for Assessing Psychotic-Like Experiences.
Findings
There were three CUD trajectory classes (Lo-Mendell-Rubin likelihood ratio test < .001): (1) persistent increasing risk; (2) maturing out, with increasing risk then decreasing risk; and (3) stable low risk. The persistent increasing class had later initial CUD onsets (η2 = .16, p < .001) and greater cumulative CUD durations (η2 = .26, p < .001). Male sex (odds ratio [OR] = 2.57, p = .018), externalizing disorders between ages 24 and 30 (OR = 2.64, p < .001), and psychotic experiences during early adulthood (Cohen’s d = 0.44, p = .016) discriminated between the persistent increasing and the maturing out classes.
Conclusions
Evidence suggests three distinguishable types of trajectory for development of cannabis use disorder starting in early teens: (1) persistent increasing risk; (2) maturing out, with increasing risk then decreasing risk; and (3) stable low risk.
Keywords: Cannabis use disorder, marijuana, adolescence, adulthood, trajectories, risk factors, outcomes
Introduction
Recent national surveys conducted in the United States (U.S.) reported lifetime cannabis use prevalence rates of 16% by the 8th grade and 58% for young adults aged 19-28 years [1, 2]. Additionally, prospective research from Australasia, Europe, and the U.S. has indicated that 10% to 21% of adolescents are at risk for developing a cannabis abuse or dependence disorder (collectively, cannabis use disorder [CUD]) by early adulthood [3-6]. Despite high rates of cannabis use in the U.S. and high rates of CUD internationally, little is currently known about CUD trajectory patterns from adolescence through early adulthood or their correlates. These knowledge gaps are becoming increasingly important to fill given that twenty-five states and the District of Columbia (D.C.) have recently enacted laws that allow the use of cannabis for medicinal purposes, and four U.S. states and D.C. have legalized the use of cannabis for recreational purposes, thus potentially increasing the likelihood that problematic cannabis use in the U.S. will become more prevalent in the years ahead.
Rates of illicit substance use in the U.S. generally increase during adolescence and decline during early adulthood [7, 8]. Although the identification of population-average trajectories is important, evidence suggests that trajectories of problematic substance use are systematically heterogeneous within populations, whereby more homogeneous subgroups are defined by specific patterns in the timing, magnitude, and duration of risk. Commonly identified subgroups include a low incidence or non-using class, a chronically or persistently high incidence class, a class characterized by high use that declines over time, and a class characterized by low use that increases over time [9]. Relative to the extensive research on longitudinal trajectory patterns of alcohol use, abuse, and dependence, limited cannabis-specific research indicates that individuals who use cannabis also cannot be regarded as a single, homogeneous group [10-17].
One reason to study CUD trajectories is to gain knowledge of the profiles of individuals within specific trajectory classes with respect to risk factors and outcomes. Prior cannabis use trajectory research based on pattern mixture modeling techniques (e.g., latent class analysis, growth mixture modeling) has identified distinguishing adolescent risk factors such as stressful life events, conduct problems, and psychiatric disorders [12, 14, 16]. Variable outcomes associated with cannabis use trajectories include lower educational attainment, occupational impairment, marital problems, poor social adjustment, and psychiatric comorbidity [11, 12, 14]. Additional risk factors and outcomes associated with cannabis use and abuse include male sex [18], parental divorce [19-21], maltreatment during childhood [22], engagement in risky behavior [23], and psychotic-like experiences [24]. The extent to which these variables are associated with distinct CUD trajectory patterns, however, remains unclear.
The Current Study
The evaluation of CUD trajectory patterns and their correlates has not, to our knowledge, been previously published. Addressing these gaps will increase knowledge regarding the etiology, course, and outcomes of CUD. Data for this study were drawn from the Oregon Adolescent Depression Project (OADP) [25], a prospective investigation of the psychosocial functioning of a community-based sample between adolescence and early adulthood. We address current gaps in scientific knowledge by examining the following questions:
Is there significant heterogeneity in CUD trajectories from childhood through early adulthood and, if so, how many distinct trajectory classes emerge?
Do CUD clinical characteristics discriminate between trajectory classes (i.e., age of initial onset, number of episodes, cumulative duration across episodes, and cannabis dependence versus abuse)?
Do risk factors assessed during adolescence predict CUD trajectory classes?
Are CUD trajectory classes associated with differences in psychosocial functioning in early adulthood?
Methods
Sample
OADP was a four-panel epidemiological study (T1 to T4) of high school students randomly selected from nine high schools in western Oregon, U.S. An institutional review board granted approval prior to data collection and participants completed informed consent. The current study represents a secondary analysis project and, therefore, no a priori sample-size planning was conducted.
The T1 sample included 1,709 adolescents (mean age = 16.6, SD = 1.2) recruited between 1987 and 1989. Demographic characteristics of the T1 sample were representative of the geographical region [25]. One year following T1, 1,507 participants (88% of the T1 sample) participated in T2 (mean age = 17.7, SD = 1.2). Approximately seven years following T2, a stratified sampling procedure was implemented whereby eligible T3 participants included all ethnic and racial minorities, all persons with a positive history of a psychiatric diagnosis by T2 (n = 644), and a randomly selected subset of participants with no history of mental disorder by T2 (n = 457 of 863 persons). Of the 1,101 participants recruited for T3, 941 (85%) completed the assessment (mean age = 24.6, SD = 0.6). Approximately 6 years after T3 (mean age = 30.5, SD = 0.7), 816 of the 941 T3 participants (87%) participated in the T4 assessment. Participant attrition at different points in time was associated with male sex, childhood disruptive behavior disorders, and substance use disorders [3, 25, 26]. The T4 panel (n = 816) constitutes the analytic sample, of which 19% developed CUD by age 30 [3]. Table 1 presents sample demographic characteristics.
Table 1.
Sample Demographic Characteristics (n = 816)
| Variable | M (SD) or % (SE) |
|---|---|
| Age at T1, M (SD) | 16.6 (1.2) |
| Male, % (SE) | 43.9 (1.7) |
| Non White, % (SE) | 7.7 (1.0) |
| Raised in dual parent household, % (SE) | 57.3 (1.7) |
| At least one parent with bachelor’s degree, % (SE) | 45.0 (1.8) |
| Ever married by T4, % (SE) | 66.9 (1.7) |
| Years of education by T4, M (SD) | 14.6 (1.9) |
Note. M = mean; SD = standard deviation; SE = standard error.
Measures
Diagnostic assessments
From T1 to T3 psychiatric disorders were assessed with the Present Episode and Epidemiologic versions of the Schedule for Affective Disorders and Schizophrenia for School-Age Children [27, 28]. At T4, the Structured Clinical Interview for Axis I DSM-IV Disorders–Non-Patient Edition [29] was used. These interviews were supplemented with the Longitudinal Interval Follow-Up Evaluation [30] to assess disorders since the previous assessment. Symptom reports were evaluated in accordance with DSM-III-R at T1 and T2 and DSM-IV at T3 and T4. Interrater reliability was good to excellent across diagnostic categories and study waves [31-33].
Two-year period prevalence indicators for psychiatric disorders were calculated using age of onset and duration data for each episode. Trajectory analyses modeled the presence versus absence of CUD in two-year intervals from age 14 to 30 (e.g., 14 to 15.9, 16 to 17.9). For risk factor and outcome analyses, internalizing and externalizing disorders were coded as present or absent prior to age 14 and between ages 24 and 30, respectively. The internalizing disorder domain included the following disorders: major depressive, dysthymia, bipolar I, bipolar II, cyclothymia, separation anxiety, simple/specific phobia, generalized anxiety, obsessive-compulsive, panic, agoraphobia without panic, post-traumatic stress, and social phobia. The externalizing disorder domain included the following disorders: attention deficit/hyperactivity, oppositional defiant, conduct, alcohol abuse or dependence, and hard drug abuse or dependence (including cocaine, amphetamines, hallucinogens, inhalants, opioids, and sedatives).
Childhood maltreatment
Childhood maltreatment was assessed retrospectively at T3 with 12 items from the Assessing Environment II [34] (alpha = .71) and five items from the Childhood Trauma Questionnaire [35] (alpha = .96). A composite measure of childhood maltreatment was computed as the mean across z-score transformations of physical abuse and sexual abuse scale scores. Higher scores indicated greater levels of abuse.
Social adjustment
Fifty-four items from the Social Adjustment Scale [36] (alpha = .70) were used to assess social adjustment during the two weeks preceding the T4 interview. Higher scores indicated poorer adjustment.
Psychotic experiences
Thirteen items adapted from the Wisconsin Manual for Assessing Psychotic-Like Experiences [37] (alpha = .74) were used to assess whether participants experienced thought transmission, passivity experiences, thought withdrawal, auditory experiences, personally relevant aberrant beliefs, visual experiences, or deviant olfactory experiences during the year prior to the T4 assessment. Higher scores indicated more frequent psychotic experiences.
Risky sexual behavior
A composite measure of high-risk sexual behavior was computed as the mean across z-score transformations of the number of concurrent partners in the past year and total number of partners in the past year. A higher score indicates more risky sexual behavior.
Statistical Analyses
We identified CUD trajectory classes using a series of unconditional latent class growth models (LCGMs) with binary outcomes and linear and quadratic slopes. The optimal number of latent classes was guided by interpretability, the statistical significance of the Lo-Mendell-Rubin adjusted Likelihood Ratio Test [38], and Akaike’s information criterion (AIC) [39]. To estimate within class variability in trajectories of CUD we modeled risk for CUD over time within each latent class obtained in the final LCGM using multilevel longitudinal analyses [40], with age-based intervals nested within individuals.
Risk factors and outcomes were independently evaluated with multinomial logistic regression and Wald tests, respectively, using a three-step approach recommended by Asparouhov and Muthén [41]. Three-step approaches account for error in latent class membership when estimating associations between a covariate and the latent class variable and do not affect latent class formation as defined by the solution of the unconditional mixture model [42]. Cohen’s d effect sizes [43] and odds ratios (ORs) were computed to characterize magnitudes of associations.
Statistical estimation methods
LCGMs were conducted using Mplus version 7.11 [44] and model parameters were estimated using full information maximum likelihood with robust standard errors. Multiple random starting values were used and solutions were considered non-convergent if random starts did not result in consistent log likelihood values. Multilevel analyses were completed using HLM 7.0 [45] with the penalized quasi-likelihood estimator, logit link function for binary outcomes, and random intercept and slope parameters. Cases were weighted as a function of sampling procedure implemented at T3 and all reported findings are based on weighted data.
Multiple imputation (MI) was used to impute missing values on risk factors (0% to 12% missing). The MI procedure generated 10 complete data sets and pooled estimates are reported in the results. Single imputation was used to impute missing values on the psychosocial outcomes (5% to 8% missing) because MI procedures were not supported by the three-step procedure for distal outcomes when sampling weights are applied in Mplus. All self-report measures were included as auxiliary variables in the imputation processes.
Results
Cannabis Use Disorder Trajectory Classes
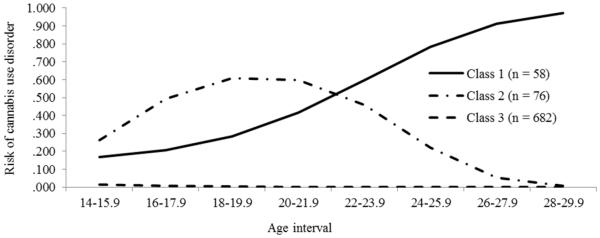
Table 2 summarizes the model selection criteria used to determine the optimal number of classes. The smallest AIC value was obtained with the four-class solution. However, the Lo-Mendell-Rubin adjusted Likelihood Ratio Test indicated that the increase in goodness-of-fit from the three-class to the four-class solution was not statistically significant, whereas the increase in goodness-of-fit from the two-class to the three-class solution was statistically significant. We chose the three-class solution as the final model based on interpretability and the results of the Lo-Mendell-Rubin adjusted Likelihood Ratio Tests. As illustrated in Figure 1, three trajectory classes were distinguished: a persistent increasing risk class (Class 1), a maturing out class (Class 2), and a stable low risk class (Class 3).
Table 2.
Criteria for Class Formation for the Unconditional Latent Class Growth Model
| Number of Classes | LR χ2 | df | p | AIC | LMR LRT | Entropy |
|---|---|---|---|---|---|---|
| 1 | 929.86 | 252 | <.001 | 3385.09 | -- | -- |
| 2 | 497.67 | 248 | <.001 | 2346.39 | <.001 | .952 |
| 3 | 304.82 | 244 | .005 | 2178.92 | <.001 | .960 |
| 4 | 226.65 | 240 | .691 | 2129.33 | .577 | .964 |
Note. LR = likelihood ratio; AIC = Akaike’s information criterion; LMR LRT = Lo-Mendell-Rubin likelihood ratio test; df = degrees of freedom. The five class solution did not converge.
Figure 1.
Risk probability of cannabis use disorder by age interval by latent class. Class 1 = persistent increasing risk over time, Class 2 = maturing out, and Class 3 = stable low risk over time.
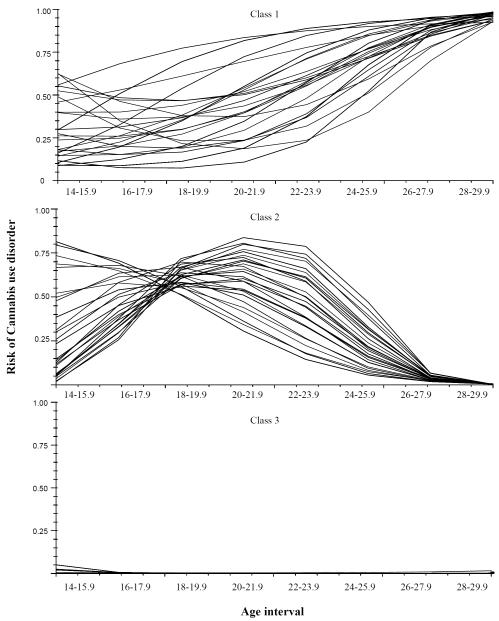
Figure 2 illustrates within class variability in CUD trajectories. The persistent increasing trajectory class demonstrated significant variability in the intercept (p = .049) but not in the linear or quadratic slopes (ps = .069 and .149, respectively). The maturing out trajectory class demonstrated significant variability in the intercept (p < .001), linear slope (p < .001), and quadratic slope (p = .034). None of the growth parameters demonstrated significant variability (ps > .500) in the stable low class.
Figure 2.
Estimated individual trajectories within cannabis use disorder trajectory classes. Class 1 = persistent increasing risk over time; Class 2 = maturing out; Class 3 = stable low risk over time.
Clinical Characteristics
A discriminant function analysis was conducted to test whether clinical characteristics of CUD discriminated between the persistent increasing and maturing out trajectory classes (Table 3). Predictors included age of initial CUD onset, total number of CUD episodes, cumulative duration across CUD episodes, and the presence versus absence of a cannabis dependence disorder. Class membership was significantly related to the weighted multivariate combination of the clinical characteristics of CUD (Λ = .29, χ2 [4] = 161.37, p < .001, η2 = .71). Compared to the maturing out class, the persistent increasing class had a greater average age of initial CUD onset (p < .001), more discrete CUD episodes (p = .030), and greater average cumulative duration across CUD episodes (p < .001).
Table 3.
Clinical Characteristics of the Persistent Increasing and Maturing Out Cannabis Use Disorder (CUD) Trajectory Classes
| Clinical Characteristic | Class 1 M (SD) |
Class 2 M (SD) |
F | η 2 |
|---|---|---|---|---|
| Initial age of CUD onset | 20.8 (4.1) | 17.6 (3.1) | 25.97*** | .16 |
| Number of CUD episodes | 1.5 (0.7) | 1.2 (0.5) | 4.84* | .03 |
| Cumulative duration of CUD in months | 90.6 (45.6) | 40.2 (39.9) | 46.29*** | .26 |
| Rate of cannabis dependence diagnosis | 0.56 (0.50) | 0.54 (0.50) | 0.05 | <.01 |
Note. Class 1 = persistent increasing risk over time; Class 2 = maturing out; M = mean; SD = standard deviation. F-tests obtained from the discriminant function analysis used 1 and 131 degrees of freedom.
p < .05.
p < .01.
p < .001.
Risk Factors
Table 4 summarizes results of multinomial logistic regression analyses that evaluated putative risk factors. Male sex was related to higher odds of persistent increasing class membership compared to the maturing out class (p = .018) and the stable low class (p = .001). Growing up in a dual parent household was related to lower odds of maturing out class membership compared to the stable low class (p = .001). The occurrence of externalizing psychiatric disorders prior to age 14 was associated with higher odds of persistent increasing class membership when compared to the stable low class (p = .009). Childhood maltreatment was related to higher odds of persistent increasing class membership (p < .001) and maturing out class membership (p < .001) compared to the stable low class.
Table 4.
Multinomial Logistic Regression Results Predicting Latent Cannabis Use Disorder Trajectory Class using Putative Risk Factors
| Latent Class Contrast, OR [CI95] |
|||
|---|---|---|---|
| Risk Factor | Class 1 vs. 2 | Class 1 vs. 3 | Class 2 vs. 3 |
| Participant and family characteristics | |||
| Male (versus female) participant | 2.57* [1.17, 5.61] |
2.78** [1.52, 5.06] |
1.08 [0.63, 1.87] |
| Dual (versus single) parent household | 1.92 [0.89, 4.13] |
0.75 [0.43, 1.32] |
0.39** [0.22, 0.69] |
| Psychiatric disorders before age 14 | |||
| Internalizing domain | 0.44 [0.16, 1.22] |
0.61 [0.26, 1.42] |
1.38 [0.74, 2.57] |
| Externalizing domain | 1.47 [0.52, 4.14] |
2.75** [1.29, 5.87] |
1.87 [0.82, 4.24] |
| Childhood maltreatment | 1.16 [0.79, 1.71] |
2.14*** [1.57, 2.91] |
1.84*** [1.34, 2.51] |
Note. OR = odds ratio; CI95 = 95% confidence interval. Separate models were conducted for each risk factor. Class 1 = persistent increasing risk over time; Class 2 = maturing out; Class 3 = stable low risk over time. The second class of each contrast is the reference category.
p < .05.
p < .01.
p < .001.
Psychosocial Outcomes
Table 5 summarizes descriptive statistics for adult psychosocial outcomes by trajectory class and the results of Wald tests of equality of trajectory class means or proportions. When compared to the maturing out class and the stable low class, participants in the increasing class had a higher likelihood of experiencing an externalizing disorder between ages 24 and 30 (Wald test = 7.29, p = .007, OR = 2.64 and Wald test = 60.56, p < .001, OR = 11.59; respectively) and greater levels of psychotic symptomology (Wald test = 5.79, p = .016, d = 0.44 and Wald test = 14.06, p < .001, d = 0.74; respectively). Participants in the increasing class had a lower likelihood of being married (Wald test = 6.46, p = .011, OR = 0.48), a higher likelihood of divorce or separation (Wald test = 5.52, p = .019, OR = 2.38), and poorer social adjustment (Wald test = 5.45, p = .020, d = 0.29) than did participants in the stable low class. Participants in the maturing out class had fewer years of education (Wald test = 10.50, p = .001, d = 0.42), more weeks unemployed in the past year (Wald test = 6.37, p = .012, d = 0.34), and a higher likelihood of experiencing internalizing (Wald test = 11.10, p = .001, OR = 2.47) and externalizing disorders (Wald test = 19.15, p < .001, OR = 4.38) than did participants in the stable low class.
Table 5.
Wald Tests of Equality of Cannabis Use Disorder Trajectory Class Means or Proportions on Adult Psychosocial Outcomes
| Psychosocial functioning measure | Trajectory class |
Wald pairwise class comparisons |
||
|---|---|---|---|---|
| Class 1 (n = 58) |
Class 2 (n = 76) |
Class 3 (n = 682) |
||
| Participant characteristics at T4 | ||||
| Years of education, M (SD) | 14.3 (2.1) | 13.8 (1.9) | 14.6 (1.9) | 2 < 3 |
| Weeks unemployed in past year, M (SD) | 1.8 (1.5) | 2.2 (1.6) | 1.7 (1.4) | 2 > 3 |
| Ever married, % (SE) | 50.9 (6.7) | 58.3 (6.1) | 68.5 (1.8) | 1 < 3 |
| History of divorce or separation, % (SE) | 30.2 (6.2) | 16.2 (4.6) | 15.4 (1.4) | 1 > 3 |
| Psychiatric disorders between 24 and 30, % (SE) | ||||
| Internalizing domain | 41.4 (6.6) | 53.9 (6.2) | 32.1 (1.8) | 2 > 3 |
| Externalizing domain | 64.4 (6.4) | 40.6 (6.0) | 13.5 (1.3) | 1 > 2, 3; 2 > 3 |
| Social adjustment at T4, M (SD) a | 1.8 (0.3) | 1.8 (0.4) | 1.7 (0.3) | 1 > 3 |
| Psychotic experiences in past year at T4, M (SD) a | 2.9 (2.9) | 1.8 (2.4) | 1.5 (1.8) | 1 > 2, 3 |
| High-risk sexual behavior in past year at T4, M (SD) a |
0.3 (1.5) | 0.2 (1.2) | −0.1 (0.6) | NS |
Note. M = mean; SD = standard deviation; SE = standard error; NS = no statistically significant pairwise class comparisons. Separate models were conducted for each outcome variable. Class 1 = persistent increasing risk over time; Class 2 = maturing out; Class 3 = stable low risk over time.
Lower scores indicated greater adjustment. Wald tests were based on one degree of freedom.
Discussion
The purpose of this study was to identify CUD trajectory classes through age 30 and compare classes on clinical characteristics of CUD, risk factors, and psychosocial outcomes. Three trajectory classes emerged: (1) a class with persistent increasing risk over time; (2) a maturing out class, marked by increasing risk through approximately age 20 and a declining risk thereafter; and (3) a generally non-abusing and non-dependent class marked by stable low risk over time. In her seminal review of longitudinal research on antisocial behavior, Moffitt [46] described similar subgroups of individuals characterized by life-course persistent and adolescent-limited antisocial behavior patterns, and the current findings are generally consistent with her observations.
Compared to individuals in the maturing out class, the persistent increasing class demonstrated later initial CUD onsets. This finding is consistent with those reported by Kandel and Chen [16] wherein persistent and heavy users were not necessarily the earliest to initiate cannabis use and the early initiation group was less likely to persist with cannabis use into adulthood. This finding is also consistent with others that suggest risk factors for substance use during adolescence may not be associated with continued use into adulthood [47]. Indeed, growing up in a single parent household was a risk factor for belonging to the maturing out class but not the persistent increasing risk class.
Maltreatment during childhood and childhood externalizing psychiatric disorders generally differentiated trajectory classes characterized by a history of CUD but were not distinguished between the persistent increasing class and the maturing out class. These findings are generally consistent with other epidemiological research on factors that predict cannabis initiation and CUD [18-22, 48]. Interestingly, the maturing out class completed the fewest years of education and reported the greatest amount of unemployment compared to the persistent increasing and stable low classes. These findings might be related to an additional study finding in which the average age of initial CUD onset coincided with high school years for the maturing out class, while the persistent increasing class typically did not meet criteria for CUD until well after high school. Future research on the temporal associations between CUD onset and educational and occupational attainment might further clarify these findings.
Self-reported psychotic experiences were greater in the persistent increasing class, while the maturing out and stable low risk classes reported similar levels of psychotic experiences. Studies often report positive associations between cannabis use and psychotic symptoms but the extent to which psychotic symptoms persist beyond transient cannabis intoxication is less clear [49]. The current results suggest that psychotic experiences may be a time-limited consequence of problematic cannabis use. A study limitation, however, was our inability to control for baseline psychotic experiences in the evaluation of these associations.
Implications
The current findings concerning CUD trajectories from mid-adolescence to early adulthood parallel those reported in the broader field of antisocial behavior [46], a domain of psychopathology highly associated with substance abuse. Although few risk factors evaluated in this study were different between the persistent increasing and maturing out trajectory classes, future research with additional time-independent and time-varying risk factors is warranted.
The identification of trajectory classes and their associated risk factors and outcomes can inform the development of comprehensive models of CUD etiology and course and, in turn, aid the development of trajectory-specific intervention approaches [50]. Findings from the current study suggest that altering the trajectories of CUD, especially persistent increasing trajectories, may be beneficial for reducing risk for psychotic-like symptoms and externalizing disorders during early adulthood. Still, the maturing out trajectory class was not exempt from disadvantages and psychosocial impairments during early adulthood despite the decreased risk for CUD. Optimal windows for prevention or intervention efforts may, therefore, be during late childhood or early adolescence.
Limitations
Study limitations included design features and restrictions in statistical modeling. The sampling procedure first involved recruiting all high schools within a 100-mile radius of project headquarters. Nine of ten recruited schools participated in the study. Students within schools were then randomly sampled. High school membership data were not available in the dataset and, therefore, potential clustering effects could not be modeled. Additional unmeasured or unavailable variables included age of cannabis initiation, frequency of cannabis use, and CUD symptomatology across episodes. This prevented the examination of heterogeneity in cannabis use profiles within trajectory classes and potentially confounded the associations between trajectory class membership and covariates. The stable low risk class, for example, is likely comprised of individuals who have never used cannabis as well as those who have used cannabis but did not meet DSM criteria for CUD. The extent to which differences in risk factors and outcomes between the stable low risk class and other classes are associated with cannabis use in general or with the trajectory of CUD specifically remains unclear. Study attrition was related to male sex, childhood disruptive behavior disorders, and substance use disorders [3, 25, 26]. It is unknown how attrition and resultant biases operated in the current analyses. Participants were relatively uniform with respect to race and geographic location. Consequently, the generalizability of the current findings to more diverse groups of individuals or locations is unclear. Data collection occurred prior to the passage of Oregon’s legislation to approve recreational cannabis use and overlapped with the passage of Oregon’s medical marijuana legislation by approximately two years. These initiatives, consequently, likely had little to no influence on the results. The timing of the assessments may have introduced retrospective recall biases into the measurement of CUD onsets and offsets for episodes that occurred further in time from the diagnostic interviews.1 Finally, the extent to which risk factors interact to predict trajectory membership was not evaluated and warrants investigation in future studies.
Conclusion
Three CUD trajectory classes emerged: a class with persistent increasing risk over time; a maturing out class, marked by increasing risk through age 20 and a declining risk thereafter; and a generally non-abusing and non-dependent class with stable low risk over time. Compared to individuals in the maturing out class, the persistent increasing class demonstrated later initial CUD onsets and similar rates of cannabis dependence versus abuse. Results partially supported distinctions between persistent increasing and maturing out CUD trajectories with several psychosocial functioning differences between classes evident in adulthood. Future research based on more diverse samples is warranted, as are well-controlled tests of associations between risk factors, trajectory class membership, and psychosocial outcomes.
Acknowledgements
National Institutes of Health grants MH40501, MH50522, and DA12951 to Peter M. Lewinsohn and R01DA032659 to Richard F. Farmer and John R. Seeley supported this research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This manuscript is based on data from the first author’s doctoral dissertation completed at the University of Oregon.
Footnotes
We compared CUD point-prevalence estimates at age 24 across participants who were assessed at T3 between ages 24.6-25.0 (n = 135) and those who were assessed at T3 after age 25.0 (n = 147). These parameters were chosen for comparison given that (a) the mean age of study participants at the time of the T3 interview was 24.6 and (b) the peak risk for CUD in this sample was between ages 18 and 25 [3]. Point prevalence rates for CUD at age 24 were not significantly different between participants interviewed between ages 24.6-25.0 and those interviewed after age 25.0 (5% vs. 8%; χ2 [1] = 1.01, p = .316). It is therefore unlikely that the timing of assessment waves influenced the trajectory classes.
Conflict of interest declaration: none.
References
- 1.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2014: Volume 2, College students and adults ages 19–55. Institute for Social Research, The University of Michigan; Ann Arbor: 2015. [Google Scholar]
- 2.Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2015: Overview, key findings on adolescent drug use. Insitute for Social Research, The University of Michigan; Ann Arbor: 2016. [Google Scholar]
- 3.Farmer RF, Kosty DB, Seeley JR, Duncan SC, Lynskey MT, Rohde P, et al. Natural course of cannabis use disorders. Psychological Medicine. 2015;45:63–72. doi: 10.1017/S003329171400107X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fergusson DM, Horwood LJ. Does cannabis use encourage other forms of illicit drug use? Addiction. 2000;95:505–520. doi: 10.1046/j.1360-0443.2000.9545053.x. [DOI] [PubMed] [Google Scholar]
- 5.Perkonigg A, Goodwin RD, Fiedler A, Behrendt S, Beesdo K, Lieb R, et al. The natural course of cannabis use, abuse and dependence during the first decades of life. Addiction. 2008;103:439–449. doi: 10.1111/j.1360-0443.2007.02064.x. [DOI] [PubMed] [Google Scholar]
- 6.Moffitt TE, Caspi A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40:899–999. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2012: Volume 1, Secondary school students. Vol. 1. The University of Michigan; Ann Arbor, Michigan: 2013. p. 645. [Google Scholar]
- 8.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2012: Volume 2, College students and adults ages 19-50. Vol. 2. The University of Michigan; Ann Arbor, MI: 2013. p. 427. [Google Scholar]
- 9.Sher KJ, Jackson KM, Steinley D. Alcohol use trajectories and the ubiquitous cat's cradle: cause for concern? Journal of Abnormal Psychology. 2011;120:322–35. doi: 10.1037/a0021813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baggio S, N'Goran AA, Deline S, Studer J, Dupuis M, Henchoz Y, et al. Patterns of cannabis use and prospective associations with health issues among young males. Addiction. 2014;109:937–945. doi: 10.1111/add.12490. [DOI] [PubMed] [Google Scholar]
- 11.Brook JS, Lee JY, Brown EN, Finch SJ, Brook DW. Developmental Trajectories of Marijuana Use from Adolescence to Adulthood: Personality and Social Role Outcomes. Psychological Reports. 2011;108:339–357. doi: 10.2466/10.18.PR0.108.2.339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: Predictors and outcomes. Development and Psychopathology. 2004;16:1007–1027. doi: 10.1017/s0954579404040118. [DOI] [PubMed] [Google Scholar]
- 13.Hix-Small H, Duncan TE, Duncan SC, Okut H. A multivariate associative finite growth mixture modeling approach examining adolescent alcohol and marijuana use. Journal of Psychopathology and Behavioral Assessment. 2004;26:255–270. [Google Scholar]
- 14.Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Development and Psychopathology. 2004;16:193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- 15.Babor TF, Webb C, Burleson JA, Kaminer Y. Subtypes for classifying adolescents with marijuana use disorders: construct validity and clinical implications. Addiction. 2002;97:58–69. doi: 10.1046/j.1360-0443.97.s1.1.x. [DOI] [PubMed] [Google Scholar]
- 16.Kandel DB, Chen K. Types of marijuana users by longitudinal course. Journal of Studies on Alcohol. 2000;61:367–378. doi: 10.15288/jsa.2000.61.367. [DOI] [PubMed] [Google Scholar]
- 17.Nelson SE, van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Development and Psychopathology. 2015;27:253–277. doi: 10.1017/S0954579414000650. [DOI] [PubMed] [Google Scholar]
- 18.Brook JS, Lee J, Finch S, Koppel J, Brook D. Psychosocial factors related to cannabis use disorders. Substance Abuse. 2011;32:242–251. doi: 10.1080/08897077.2011.605696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Butters JE. Family stressors and adolescent cannabis use: A pathway to problem use. Journal of Adolescence. 2002;25:645–654. doi: 10.1006/jado.2002.0514. [DOI] [PubMed] [Google Scholar]
- 20.Flewelling RL, Bauman KE. Family structure as a predictor of initial substance use and sexual intercourse in early adolescence. Journal of Marriage and the Family. 1990;52:171–181. [Google Scholar]
- 21.Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R. Do parents' marital circumstances predict young adults' DSM-IV cannabis use disorders? A prospective study. Addiction. 2006;101:1778–1786. doi: 10.1111/j.1360-0443.2006.01620.x. [DOI] [PubMed] [Google Scholar]
- 22.Oshri A, Rogosch FA, Burnette ML, Cicchetti D. Developmental pathways to adolescent cannabis abuse and dependence: Child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychology of Addictive Behaviors. 2011;25:634–644. doi: 10.1037/a0023151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall W, Babor TF. Cannabis use and public health: assessing the burden. Addiction. 2000;95:485–490. doi: 10.1046/j.1360-0443.2000.9544851.x. [DOI] [PubMed] [Google Scholar]
- 24.Mackie CJ, Castellanos-Ryan N, Conrod PJ. Developmental trajectories of psychotic-like experiences across adolescence: impact of victimization and substance use. Psychological Medicine. 2011;41:47–58. doi: 10.1017/S0033291710000449. [DOI] [PubMed] [Google Scholar]
- 25.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III—R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 26.Farmer RF, Kosty DB, Seeley JR, Olino TM, Lewinsohn PM. Aggregation of lifetime Axis I psychiatric disorders through age 30: incidence, predictors, and associated psychosocial outcomes. Journal of Abnormal Psychology. 2013;122:573–586. doi: 10.1037/a0031429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chambers WJ. The assessment of affective disorders in children and adolescents by semistructured interview: Test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode version. Archives of General Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- 28.Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. Journal of the American Academy of Child Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- 29.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM–IV Disorders—Non-Patient Edition. Biometrics Research Department; New York: 1994. [Google Scholar]
- 30.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott PA. The Longitudinal Interval Follow-up Evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 31.Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: Patterns of lifetime liability from mid-adolescence through early adulthood. Journal of Abnormal Psychology. 2009;118:699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seeley JR, Kosty DB, Farmer RF, Lewinsohn PM. The modeling of internalizing disorders on the basis of patterns of lifetime comorbidity: Associations with psychosocial functioning and pshychiatric disorders among first-degree relatives. Journal of Abnormal Psychology. 2011;120:308–321. doi: 10.1037/a0022621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kosty DB, Farmer RF, Seeley JR, Gau JM, Duncan SC, Lewinsohn PM. Parental transmission of risk for cannabis use disorders to offspring. Addiction. 2015;110:1110–1117. doi: 10.1111/add.12914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berger AM, Knutson JF, Mehm JG, Perkins KA. The self-report of punitive childhood experiences of young adults and adolescents. Child Abuse and Neglect. 1988;12:251–262. doi: 10.1016/0145-2134(88)90033-6. [DOI] [PubMed] [Google Scholar]
- 35.Bernstein DP, Fink L, Handelsman L, Foote J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 36.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 37.Kwapil TR, Chapman LJ, Chapman J. Validity and usefulness of the Wisconsin Manual for Rating Psychotic-Like Experiences. Schizophrenia Bulletin. 1999;25:363–375. doi: 10.1093/oxfordjournals.schbul.a033384. [DOI] [PubMed] [Google Scholar]
- 38.Yungtai LO, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- 39.Burnham KP, Anderson DR, Huyvaert KP. AIC model selection and multimodel inference in behavioral ecology: Some background, observations, and comparisons. Behavioral Ecology and Sociobiology. 2011;65:23–35. [Google Scholar]
- 40.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- 41.Asparouhov T, Muthén B. Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using Mplus. Structural Equation Modeling: A Multidisciplinary Journal. 2014:1–13. [Google Scholar]
- 42.McIntosh CN. Pitfalls in subgroup analysis based on growth mixture models: a commentary on van Leeuwen et al. (2012) Quality of Life Research. 2013;22:2625–2629. doi: 10.1007/s11136-013-0385-x. [DOI] [PubMed] [Google Scholar]
- 43.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 44.Muthén B, Muthén LK. Mplus User's Guide. Seventh Edition Muthen & Muthen; Los Angelas, CA: 1998-2012. [Google Scholar]
- 45.Raudenbush SW, Bryk AS, Cheong YF, Congdon RT, du Toit M. HLM 7: Hierarchical linear and nonlinear modeling. Scientific Software International; Lincolnwood, IL: 2011. [Google Scholar]
- 46.Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- 47.Bates ME, Labouvie EW. Adolescent risk factors and the prediction of persistent alcohol and drug use into adulthood. Alcoholism: Clinical and Experimental Research. 1997;21:944–950. [PubMed] [Google Scholar]
- 48.Farmer RF, Seeley JR, Kosty DB, Gau J, Duncan SC, Lynskey M, et al. Internalizing and externalizing psychopathology as predictors of cannabis use disorder onset during adolescence and early adulthood. Psychology of Addictive Behaviors. 2015;29:541–551. doi: 10.1037/adb0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moore THM, Zammit S, Lingford-Hughes A, Barnes TRE, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental heath outcomes: A systematic review. Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 50.Schulenberg JE, Maggs JL, Steinman KJ, Zucker RA. Developmental matters: Taking the long view on substance abuse etiology and intervention during adolescence. In: Monti PM, Colby SM, O'Leary TA, editors. Adolescents, alcohol, and substance abuse: Reaching teens through brief interventions. Guilford Press; New York, NY: 2001. pp. 19–57. [Google Scholar]