Introduction
Rheumatology laboratory tests are commonly ordered by pediatricians to screen for rheumatic diseases when children present with musculoskeletal (MSK) pain or non-specific symptoms such as fatigue. However, caution should be taken because in order for a screening laboratory test to be clinically useful, the positive predictive value (PPV) should be high. Childhood arthritis and other rheumatic diseases are rare with a prevalence of approximately 400 per 100,000 children in the United States.1 Conversely, the prevalence of MSK pain and other non-specific symptoms such as fatigue are quite common among children, with rates up to 40% for MSK pain and 30% for fatigue.2,3 Therefore the PPV of rheumatology laboratory tests among this group of pediatric patients is likely to be low. Particular caution should be taken with certain rheumatology tests such as the antinuclear antibody (ANA) and the human leukocyte antigen (HLA)-B27 genetic test which have been found to be positive in a relatively large percentage of healthy children.4–6
Moreover, the diagnostic criteria of most pediatric rheumatic diseases, including juvenile idiopathic arthritis (JIA), are based upon clinical findings rather than laboratory test results. Such tests may be helpful in categorizing the disease or prognosticating its course, but they are not used to establish the diagnosis. For example, although the rheumatoid factor (RF) and anti-cyclic-citrullinated peptide (CCP) antibody tests are used to screen for adult rheumatoid arthritis, these tests are only positive in approximately 3% of children with JIA because only a small subset of JIA patients have a disease equivalent to adult rheumatoid arthritis. 7–9 It is for these reasons that current guidelines do not support the use of ANA, anti-double-stranded DNA (dsDNA) antibody, RF, anti-CCP antibody, or HLA-B27 as diagnostic tests for undiagnosed MSK pain.6,10–15 Furthermore, MSK pain without other signs such as joint swelling or gait abnormality is rarely caused by an inflammatory condition.16 Nonetheless, many referrals come to the pediatric rheumatology (PR) clinic for positive rheumatology laboratory tests of uncertain significance and non-specific complaints such as MSK pain without evidence of arthritis or other physical examination abnormalities.
The primary goal of this study was to survey primary pediatricians to determine the frequency of use of common rheumatology tests and to understand the reasons behind ordering them. The secondary goals were to quantify the frequency of referral to the PR clinic for positive test results of uncertain significance and to investigate factors associated with appropriate utilization of these tests.
Methods
Physician study population
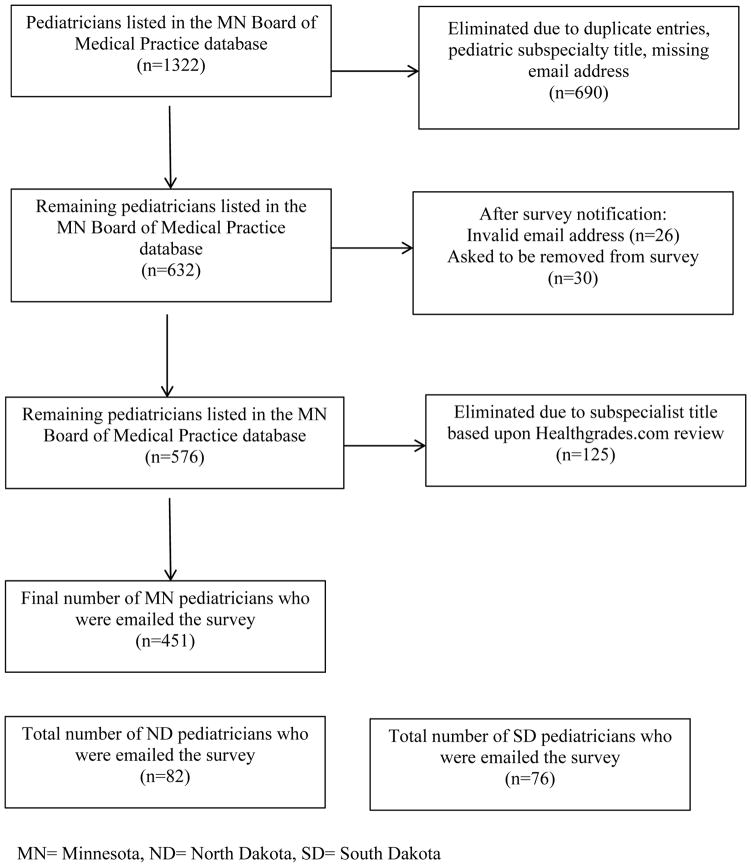
All general pediatricians practicing in Minnesota (MN), North Dakota (ND) and South Dakota (SD) with a valid email address were eligible for the survey. The MN and ND pediatricians’ email addresses were obtained from the MN Board of Medical Practice and the ND Board of Medical Examiners. The SD pediatricians’ email addresses were obtained from the SD chapter of the American Academy of Pediatrics. The MN Board of Medical Practice database contained contact information for 1322 pediatricians. Of these, 690 were eliminated due to duplicate entries, missing email address, or because the physician was not a general pediatrician. This left 632 MN pediatrician email addresses. When a notification about the survey was sent one week prior to the survey, 26 email addresses were found to be invalid and 30 physicians asked to be removed from the survey list. An additional 125 pediatricians were eliminated because they were determined to be pediatric subspecialists based upon a systematic review of each remaining physician in the database using Healthgrades.com. Thus, the survey was emailed to a total of 451 MN pediatricians (Figure 1). The survey was also emailed to a total of 76 pediatricians practicing in SD and 82 practicing in ND, however, the investigators did not have direct access to these databases; rather the link to the survey was forwarded to the pediatricians by the administrators of the databases. This survey was determined to be exempt from formal institutional review board (IRB) review at the University of Minnesota.
Figure 1.
Primary pediatrician study population
Instrument
The survey queried pediatricians to assess their experience in pediatric rheumatology, reasons for referring patients to PR and assessment of utilization of rheumatology laboratory tests. In order to evaluate the pediatricians’ experience in PR, survey questions included assessments such as years since completion of residency training, whether or not the training institution had a section of PR, number of weeks spent with a pediatric rheumatologist during training, and whether continuing medical education (CME) credits were focused on PR. In order to gauge utilization of rheumatology laboratory tests, pediatricians were queried regarding their reasons for ordering ANA, anti-dsDNA antibody, RF, anti-CCP antibody, and HLA-B27 tests. For each of the tests queried, respondents were able to select all of their reasons for ever ordering the test. In order to avoid possibly leading the survey participant toward a particular answer, each laboratory test queried had an identical list of possible answers. The survey consisted of multiple choice answers and “select all that apply” answers with options to add free text. The survey can be seen in Appendix A.
Survey administration
The survey was conducted between June and July, 2013 using the web-based program, Research Electronic Data Capture (REDCap™). One week prior to sending the survey, a notification email was sent. The survey was open for three weeks. A reminder email was sent one week prior to the closing of the survey. As an incentive to complete the survey, those who completed the survey were entered into a drawing to win a $400 gift card for an online retailer.
Analysis of responses
Responder and non-responder characteristics were compared using two-sample t-tests for continuous variables and Fisher’s exact test for categorical variables. General frequency distributions of responses were also performed. Subgroup analysis was performed to determine if increased experience in primary pediatrics and/or with PR increased the likelihood of correctly utilizing each of the ANA, anti-dsDNA antibody, RF, anti-CCP antibody, or HLA-B27 laboratory tests. Subgroups evaluated included years since completion of pediatrics residency (grouped as <5 y, 5–10 y, 11–20 y, and >20 y), whether or not the pediatrics residency had a division of PR (dichotomized as yes or no), amount of time spent in a PR clinic during medical school or pediatric residency (grouped as no time, 1 day to <4 weeks, 4–8 weeks, and >8 weeks), whether or not any continued medical education (CME) credits were focused on PR in the last three years (dichotomized as yes or no), and geographic location of the clinic (categorized as urban, suburban, rural).
We calculated how often each respondent correctly ordered each lab test. For each respondent, the utilization of each laboratory test was defined as “correct” as long as one correct answer was selected (regardless of whether “incorrect” or “possibly correct” choices were also selected). A response was defined as “possibly correct” as long as one “possibly correct” answer was selected and no “correct” answer was selected (regardless of whether “incorrect” choices were also selected). A response was defined as “incorrect” if only incorrect answers were selected. Definitions of “correct”, “possibly correct”, and “incorrect” responses were determined by the investigators based upon published recommendations and guidelines (Table 1). 6,10,11,13,14 If a respondent added a free-text reason for ordering a laboratory the response was not included in calculations. P-values were calculated using analysis of variance (ANOVA) and Fisher’s exact test for continuous and categorical variables, respectively.
Table 1.
Definition of “correct” response for ordering rheumatology lab tests.
| Lab Tests | |||||
|---|---|---|---|---|---|
| Responses | ANA | Anti-dsDNA antibody | RF | Anti-CCP antibody | HLA-B27 |
| MSK pain involving the small joints with an otherwise normal exam | I | I | I | I | I |
| MSK pain involving the large joints with an otherwise normal exam | I | I | I | I | I |
| MSK pain involving the small and large joints with an otherwise normal exam | I | I | I | I | I |
| Abnormal joint exam (such as swelling, warmth, pain with range of motion, and/or loss of range of motion) | P | I | P | P | I |
| Back pain | I | I | I | I | P |
| Fatigue | I | I | I | I | I |
| Persistent or recurrent fever | I | I | I | I | I |
| Rash | I | I | I | I | I |
| Hair loss | P | I | I | I | I |
| Raynaud phenomenon | P | I | I | I | I |
| GI complaints (such as chronic abdominal pain, diarrhea, nausea, and/or vomiting) | I | I | I | I | I |
| The patient clinically met criteria for SLE | C | C | I | I | I |
| The patient clinically met criteria for JIA | C | I | C | C | I |
C= correct reason to utilize lab test, P= possibly correct reason to utilize lab test, I= incorrect reason to utilize lab test
Results
The overall response rate was 15% (93/609); the response rates from each state were 16% (70/451) for MN, 13% (10/76) for ND, and 13% (11/82) for SD. Comparisons between responders and non-responders were performed only for the MN pediatricians because the investigators did not have access to the ND or SD databases. Respondents and non-respondents were compared by gender, age, years of practice and geographic setting of their clinic (urban, suburban, and rural). Respondents tended to be younger (mean age 48 yo versus 54 yo, p=0.0005), were more likely to be female (69% vs. 49%) and had been in practice for a shorter period of time (mean 22 y versus 27 y, p=0.0051) than non-respondents. However further analysis determined that among both respondent and non-respondent groups, women tended to be younger. Therefore the gender difference between the respondents and non-respondents is merely reflective of the age difference. There was no significant difference between respondents and non-respondents regarding geographical setting of the clinic. The demographics of the respondents are shown in Table 2.
Table 2.
Demographic comparison among respondents and non-respondents
| Respondent Demographics | Responders | Non-Responders | P-value |
|---|---|---|---|
|
| |||
| N (%) | 93 (15) | 516 (85) | |
| Mean age in years (range) | 48 (33–70) | 54 (31–84) | 0.0005 |
| Mean years in practice (range) | 22 (6–45) | 27 (2–58) | 0.0051 |
| Self-reported geographic location of clinic | 0.2390 | ||
| Urban: N (%) | 37 (40) | 254 (49) | |
| Suburban: N (%) | 37 (40) | 209 (41) | |
| Rural: N (%) | 18 (20) | 53 (10) | |
| Male | 29 (31) | 262 (51) | 0.0042 |
Data calculated using MN Data only
Frequency of laboratory utilization
ANA
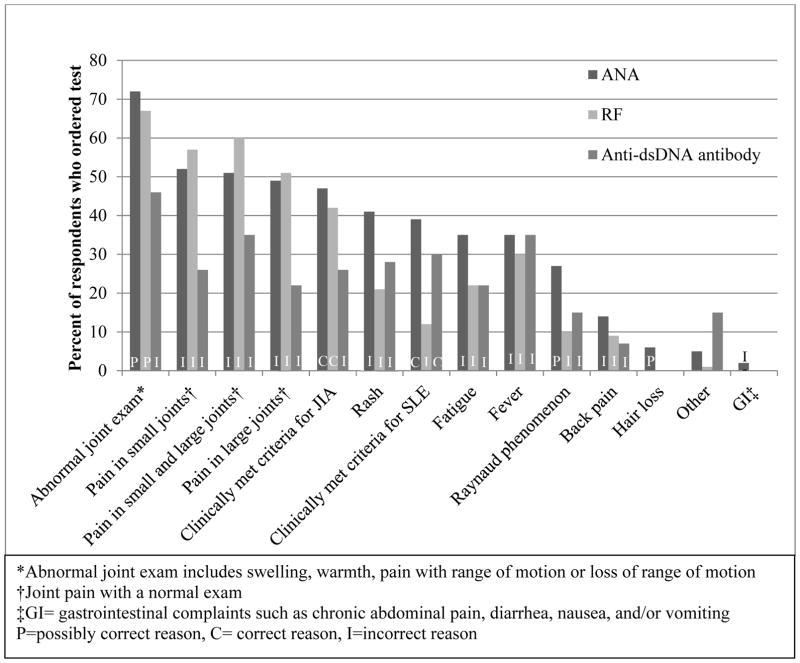
Ninety-one percent (83/91) of respondents had ordered an ANA. The most common reasons for doing so were for an abnormal joint exam described as swelling, warmth, pain with range of motion, and/or loss of range of motion (72%), pain in the small joints with a normal joint exam (52%), pain in the small and large joints with a normal joint exam (51%), pain in the large joints with a normal joint exam (49%), and because the patient met clinical criteria for JIA (48%). Forty percent of those who had ordered an ANA did so because the patient clinically met criteria for SLE (Figure 2).
Figure 2.
Self-reported reasons for ordering a rheumatology lab test
RF and anti-CCP antibody
Seventy-three percent (67/92) of respondents had ordered a RF, and the most common reason for doing so was an abnormal joint exam described as swelling, warmth, pain with range of motion and/or loss of range of motion (67%). The next three most common reasons were for pain with a normal exam involving the small and large joints (60%), small joints (57%), and large joints (51%). Forty-two percent of those who ordered a RF did so because the patient met criteria for JIA (Figure 2). Only 8% (7/92) of respondents had ordered an anti-CCP antibody.
Anti-dsDNA antibody
Fifty-nine percent of respondents (54/92) had ordered an anti-dsDNA antibody, and the most common reasons for doing so were abnormal joint exam described as swelling, warmth, pain with range of motion and/or loss of range of motion (46%), pain in the small and large joints with a normal exam (35%), and fever (35%). Thirty percent of those who ordered an anti-dsDNA did so because the patient met criteria for SLE (Figure 2).
HLA-B27
Forty-two percent (39/92) of respondents had ordered an HLA-B27 test, and the most common reason for doing so was back pain (59%), followed by abnormal joint exam (36%), and pain in the small and large joints with a normal joint exam (23%).
Association between experience level and correctly ordering rheumatology laboratory tests
Based upon the definitions of correct utilization as described above and as seen in Table 1, among those who had ordered an ANA, 86% (71/83) ordered it for correct or possibly correct reasons. Among those who ordered an anti-dsDNA antibody, 34% (16/47) did so for correct reasons. Eighty percent (53/66) of those who ordered a RF did so for correct or possibly correct reasons, 60% (3/5) of those who ordered an anti-CCP antibody did so for correct or possibly correct reasons and 59% (23/39) of those who ordered an HLA-B27 did so for possibly correct reasons.
Subgroup analysis demonstrated a statistically significant association between correct utilization of the ANA test and increased years since completion of residency training (<5 y since completion of residency: 17% correct, 5–10 y: 33%, 11–20 y: 46%, >20 y: 82%, p−= 0.0012). Those who spent no time in the PR clinic during residency were found to be more likely to correctly utilize the anti-dsDNA antibody test compared to those who had spent one day to eight weeks in the PR clinic (no time in the PR clinic: 58% correct, 1 d to <4 weeks: 15%, ≥4 weeks 17%). Only one respondent had spent more than eight weeks in the PR clinic and thus the groups 4–8 weeks and >8 weeks were merged (Table 3). No other significant associations between training experience and patterns of laboratory test ordering were observed.
Table 3.
Correct use of the ANA and anti-dsDNA antibody tests
| Years since completion of pediatrics residency | ||||||
|---|---|---|---|---|---|---|
| Total | <5 | 5–10 | 11–20 | >20 | p-value | |
| ANA | n=81 | n=6 | n=21 | n=26 | n=28 | |
| Incorrect (%) | 15 | 17 | 33 | 12 | 4 | |
| Possibly correct (%) | 32 | 67 | 33 | 42 | 14 | |
| Correct (%) | 53 | 17 | 33 | 46 | 82 | 0.0012 |
| Weeks spent in PR Clinic During Training | ||||||
| Total | None | 1d- <4 | ≥4 | p-value | ||
| Anti-dsDNA | n=47 | n=19 | n=20 | n=8 | ||
| Incorrect (%) | 66 | 42 | 85 | 83 | ||
| Correct (%) | 34 | 58 | 15 | 17 | 0.0070 | |
The remainder of subgroup analysis did not reveal statistically significant results and these results are not shown
Referral patterns to the PR clinic
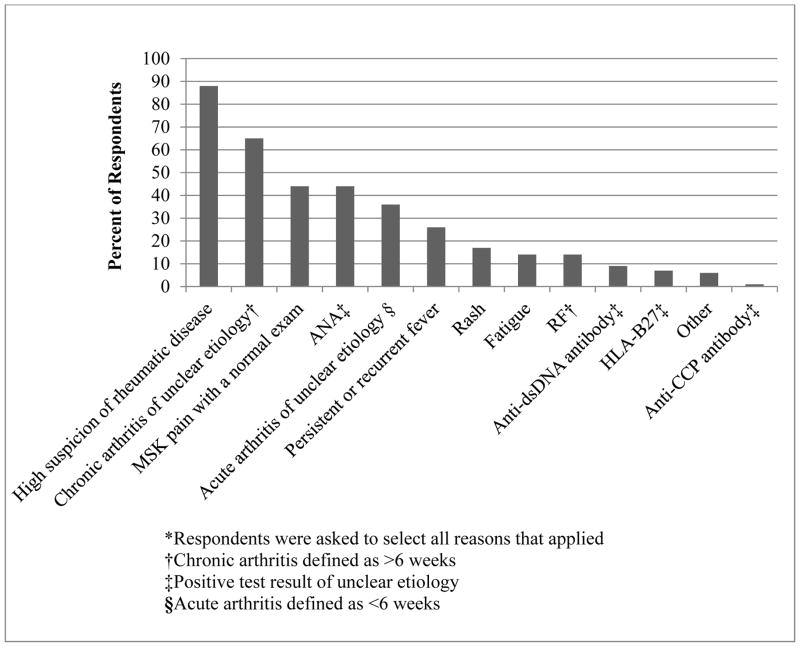
Ninety-two percent (85/92) of surveyed pediatricians had referred a patient to a PR clinic. The most commonly selected reasons for referral were for high suspicion for a rheumatic disease (88%), chronic arthritis of unclear etiology (65%), MSK pain with an otherwise normal exam (44%) and positive ANA of unclear significance (44%). Fourteen percent had referred a patient for fatigue, 14% for positive RF of unclear significance, 9% for positive anti-dsDNA of unclear significance, and 7% for positive HLA-B27 of unclear significance (Figure 3).
Figure 3.
Reasons indicated for referring to PR.*
Interest in continued medical education (CME) focusing on PR
Eighty-eight percent (81/92) of respondents were interested in CME focused on PR. Among these, 75% were interested in local presentations and 66% were interested in self-directed learning.
Discussion
Although there are published recommendations regarding proper use of rheumatologic laboratory tests in primary care, these tests are commonly ordered for incorrect reasons, as seen in this survey.10,11,13,14,17 This is an important issue because the laboratory tests are expensive (the price per test at the investigators’ institution ranged from $48.00 to $267.00).18 Furthermore, false positive laboratory results often result in unnecessary referrals to PR clinics and emotional stress to patients and their families. Referrals to subspecialty clinics may result in significant time and financial burden to patients and their families, especially when distance to care is great, and therefore unnecessary referrals should be minimized.
The single recommended reason to order an ANA in general pediatric practice is to address the question of whether a child has SLE.13 A positive ANA test in and of itself is not diagnostic of SLE but can contribute to the diagnosis of SLE in the context other signs and symptoms suggestive of SLE.19 Although the vast majority of respondents had ordered an ANA, less than half had ordered it because the patient had met significant criteria suggestive of SLE. A large percentage of respondents reported that they ordered the ANA because the patient met criteria for JIA or had arthritis on exam. However the ANA test has not been found to be diagnostic for JIA and thus it is not recommended to be used as a diagnostic test in this setting.13 Rather, the ANA test is used in patients with an established diagnosis of JIA in order to assess risk for uveitis and to guide frequency of ophthalmologic examinations.20 It is possible that in some circumstances the ANA had been ordered to prognosticate uveitis in a patient who had been determined to have JIA. This study did not assess for this specific reasoning. Most striking was that the ANA was very commonly ordered when a patient had joint pain without arthritis which is an incorrect reason for doing so.10,13
The majority of respondents had ordered the anti-dsDNA antibody, however it was ordered for the correct or possibly reasons by fewer than half of the respondents. The anti-dsDNA antibody test is one antibody test among the group of antinuclear antibodies that is highly specific for SLE and helpful for patients with signs and symptoms suggestive of SLE and a positive ANA screen.15
The RF test was commonly ordered for an abnormal joint exam and for MSK pain with a normal exam. Less than half of the respondents had ordered it because a patient met criteria for JIA. The RF test is not a diagnostic test for JIA; rather it is used to predict prognosis and guide treatment among children with an established diagnosis of JIA. There may have been some circumstances in which the use of the RF was ordered by pediatricians for prognostic reasons among children with JIA. However there is no indication to order a RF test for children with joint pain without arthritis, which, collectively, was the most common reason selected for ordering this test.10
While the ordering of the HLA-B27 test is justifiable in the setting of inflammatory back pain concerning for ankylosing spondylitis, it is not recommended as a diagnostic test in the setting of non-specific back pain.6 Therefore, its use in pediatric primary care is very limited, especially given the fact that true ankylosing spondylitis is extremely rare in children with an estimated prevalence rate between 0.01–0.09%.21 In this survey the HLA-B27 was ordered by 42% of respondents, most commonly for back pain. The survey did not differentiate between inflammatory and non-inflammatory back pain, so it remains possible that this test was used correctly if the child had inflammatory back pain.
The anti-CCP test was rarely ordered among the pediatricians surveyed. This is likely because this is a newer clinical test used to screen for adult rheumatoid arthritis and RF-positive polyarticular JIA and thus general pediatricians are less familiar with it.8,22 In regards to the above mentioned laboratory tests, it is also important to note that a negative result does not rule out JIA, SLE, or ankylosing spondylitis and should not be used in this capacity.
Although there was a positive relationship between increased years in practice and correct use of ANA, this positive relationship did not hold for other measures of experience and correct use of ANA or other rheumatology laboratory tests. Moreover, it was discouraging that respondents who spent no time in the PR clinic during residency were more likely to correctly order the anti-dsDNA test compared to those who spent any time in the PR clinic. This unexpected finding might be explainable by those pediatricians who spent some time in the PR clinic had become aware enough of the anti-dsDNA antibody test that they felt comfortable ordering the test, but not gaining a full understanding of the correct reasons to order it.
MSK pain in the setting of a normal exam was among the most common reasons for ordering any of the laboratory tests queried in this survey despite the fact that this is an incorrect reason to order any of these tests. It was also a common reason that respondents reported referring to a PR clinic. This is consistent with a previous study which reported that MSK pain was the primary reason for referral to a PR clinic, despite the fact that non-specific MSK pain is rarely due to inflammatory conditions.16 However, another study demonstrated that primary pediatricians report lack of confidence in their MSK exams.23 Therefore, it is possible that the respondents of this survey thought the patient most likely had a normal exam, but did not feel confident in their findings and thus referred to PR for further evaluation.
Two important limitations to this study are the low response rate and the inclusion of participants only from three states of the Upper Midwest. Due to the low response rate, the results of the survey may not be generalizable to all pediatricians and this makes interpretation of results difficult. The response rate was low despite attempts to improve responses by sending an introductory email, sending a reminder email, and providing a gift incentive. However, low response rates are common for physician surveys.24 The only statistically significant differences between respondents and non-respondents were age, years in practice, and gender. Age and years in practice would be expected to be linked. Further analysis determined that the gender difference was likely reflective of age, with women physicians tending to be younger in this survey. The higher response rate from younger individuals presumably reflects their tendency to attend more routinely to their email accounts compared to older individuals. Despite this difference in age, the characteristics of the respondents were representative of the primary pediatric workforce in MN.25
The survey was limited to MN, ND, and SD which are a part of the catchment area for the investigators’ PR clinic. It is possible that the majority of respondents trained in the same pediatric residency program, thus their responses may be more homogenous due to similar training than the responses from a more geographically extensive pediatrician population would be. Therefore the findings from this survey may not be representative of all primary pediatricians, particularly those practicing in other geographic areas in the United States.
Another limitation of the study was that it focused solely on general pediatricians and did not include family physicians. It would be important to capture responses from family physicians as they represent 50% of the primary care workforce in MN.25 Moreover national data show that approximately 20% of child health care is provided by family practitioners, and family physicians in rural areas are more likely to provide health care to children.26–28 An important future study would include family practitioners and compare their responses to general pediatricians’ responses.
Another limitation of this study is that there is not a gold standard to define the correct utilization of rheumatology laboratory tests in the pediatric primary care setting, and correct utilization of laboratory tests was defined by the investigators based upon published recommendations, guidelines and personal experience. Moreover, by survey design, pediatricians were asked to select all the reasons for which they had ever ordered each test. The investigators then determined that a pediatrician “correctly” or “possibly correctly” utilized the laboratory test if they ever ordered it correctly or possibly correctly, even if they also ordered the same test for incorrect reasons. Therefore the results overestimate correct use of these laboratory tests. For example, although it was determined that 86% of respondents correctly or possibly correctly ordered the ANA test, by this definition, the same respondents may have also incorrectly ordered the ANA. Therefore, 14% of all the respondents who ever ordered an ANA ordered it for incorrect reasons only. Likewise, 66% of those who ever ordered an anti-dsDNA antibody ordered it for incorrect reasons only, 20% who ever ordered a RF ordered it for incorrect reasons only, and 41% of those who ever ordered HLA-B27 ordered it for incorrect reasons only. Because it is not known how often each pediatrician ordered each test, a true correct usage rate could not be calculated.
Another commonly encountered issue is the use of so-called “rheumatology panels”, which are a single laboratory order that consists of a series of rheumatology laboratory tests which may or may not be related to one another. The tests included in the panels vary depending on the individual laboratories. Use of these panels may result in a pediatrician obtaining multiple unnecessary tests when he or she was only interested in obtaining one particular test. This survey did not assess for use of “rheumatology panels” among pediatricians.
According to this study, most parameters indicating increased exposure to PR during residency training did not equate to improved utilization of rheumatology laboratory tests. Therefore, alternative approaches may be needed to reduce unnecessary use of these tests. Systems-based approaches may be useful such as flagging rheumatology tests on the electronic medical record to provide guidance on correct use of these tests, or eliminating the “rheumatology panel” tests. Additionally, most of the respondents indicated interest in learning more about pediatric rheumatic disease, and most were interested in local presentations and self-directed learning. Therefore it would be important to increase resources into providing these learning opportunities for general pediatricians.
Conclusion
This study was the first to survey pediatricians in order to understand their reasons for ordering rheumatology laboratory tests. It demonstrates the fact that the majority of pediatricians have ordered several of the common rheumatology laboratory tests; however their reasons for ordering these tests are often incorrect despite published recommendations for their use. It is likely that pediatricians are unaware of these recommendations. Moreover, a substantial percentage of referrals from primary pediatricians to PR clinics are due to laboratory tests results of uncertain significance and for MSK pain without arthritis, and patients referred for these reasons rarely have a rheumatic disease. Having an understanding of why these tests are being utilized will provide strategies to increase their appropriate use and decrease unnecessary referrals.
Supplementary Material
Acknowledgments
Statistical support was provided by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1TR000114 to the University of Minnesota Clinical and Translational Sciences Institute.
Footnotes
Credits: CC developed, designed, and sent the survey. LS, BB, LZ, and RV edited the survey questions. CC collected the survey data. LZ analyzed the survey data and CC and LS interpreted the results. CC drafted the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest: The authors report no conflicts of interest regarding this research. The authors report no financial support or financial interest regarding this research.
References
- 1.Sacks JJ, Helmick CG, Luo YH, Ilowite NT, Bowyer S. Prevalence of and annual ambulatory health care visits for pediatric arthritis and other rheumatologic conditions in the united states in 2001–2004. Arthritis Rheum. 2007;57(8):1439–1445. doi: 10.1002/art.23087. [DOI] [PubMed] [Google Scholar]
- 2.Rimes KA, Goodman R, Hotopf M, Wessely S, Meltzer H, Chalder T. Incidence, prognosis, and risk factors for fatigue and chronic fatigue syndrome in adolescents: A prospective community study. Pediatrics. 2007;119(3):e603–9. doi: 10.1542/peds.2006-2231. 119/3/E603 [pii] [DOI] [PubMed] [Google Scholar]
- 3.King S, Chambers CT, Huguet A, MacNavin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain. 2011;152(12):2729–2738. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Allen RC, Dewez P, Stuart L, Gatenby PA, Sturgess A. Antinuclear antibodies using HEp-2 cells in normal children and in children with common infections. J Paediatr Child Health. 1991;27(1):39–42. doi: 10.1111/j.1440-1754.1991.tb00343.x. [DOI] [PubMed] [Google Scholar]
- 5.Hilario MO, Len CA, Roja SC, Terreri MT, Almeida G, Andrade LE. Frequency of antinuclear antibodies in healthy children and adolescents. Clin Pediatr (Phila) 2004;43(7):637–642. doi: 10.1177/000992280404300709. [DOI] [PubMed] [Google Scholar]
- 6.Gran JT, Husby G. HLA-B27 and spondyloarthropathy: Value for early diagnosis? J Med Genet. 1995;32(7):497–501. doi: 10.1136/jmg.32.7.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brunner J, Sitzmann FC. The diagnostic value of anti-cyclic citrullinated peptide (CCP) antibodies in children with juvenile idiopathic arthritis. Clin Exp Rheumatol. 2006;24(4):449–451. 1877 [pii] [PubMed] [Google Scholar]
- 8.van Rossum M, van Soesbergen R, de Kort S, et al. Anti-cyclic citrullinated peptide (anti-CCP) antibodies in children with juvenile idiopathic arthritis. J Rheumatol. 2003;30(4):825–828. 0315162X-30-825 [pii] [PubMed] [Google Scholar]
- 9.Eichenfield AH, Athreya BH, Doughty RA, Cebul RD. Utility of rheumatoid factor in the diagnosis of juvenile rheumatoid arthritis. Pediatrics. 1986;78(3):480–484. [PubMed] [Google Scholar]
- 10.John M Eisenberg Center for Clinical Decisions and Communications Science. Comparative effectiveness review summary guides for clinicians. Rockville (MD): 2007. Antinuclear antibody, rheumatoid factor, and cyclic-citrullinated peptide tests for evaluating musculoskeletal complaints in children. [PubMed] [Google Scholar]
- 11.Malleson PN, Mackinnon MJ, Sailer-Hoeck M, Spencer CH. Review for the generalist: The antinuclear antibody test in children - when to use it and what to do with a positive titer. Pediatr Rheumatol Online J. 2010;8:270096-8-27. doi: 10.1186/1546-0096-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deane PM, Liard G, Siegel DM, Baum J. The outcome of children referred to a pediatric rheumatology clinic with a positive antinuclear antibody test but without an autoimmune disease. Pediatrics. 1995;95(6):892–895. [PubMed] [Google Scholar]
- 13.McGhee JL, Kickingbird LM, Jarvis JN. Clinical utility of antinuclear antibody tests in children. BMC Pediatr. 2004;4:13. doi: 10.1186/1471-2431-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith JA. Testing for rheumatological diagnoses in children. Eur Paediatr Rev. 2009;3(1):30–34. [PMC free article] [PubMed] [Google Scholar]
- 15.Werle E, Blazek M, Fiehn W. The clinical significance of measuring different anti-dsDNA antibodies by using the farr assay, an enzyme immunoassay and a crithidia luciliae immunofluorescence test. Lupus. 1992;1(6):369–377. doi: 10.1177/096120339200100606. [DOI] [PubMed] [Google Scholar]
- 16.McGhee JL, Burks FN, Sheckels JL, Jarvis JN. Identifying children with chronic arthritis based on chief complaints: Absence of predictive value for musculoskeletal pain as an indicator of rheumatic disease in children. Pediatrics. 2002;110(2 Pt 1):354–359. doi: 10.1542/peds.110.2.354. [DOI] [PubMed] [Google Scholar]
- 17.Lane SK, Gravel JW., Jr Clinical utility of common serum rheumatologic tests. Am Fam Physician. 2002;65(6):1073–1080. [PubMed] [Google Scholar]
- 18.Fairview hospital. [Accessed May 29, 2014];Find a test Web site. http://applications.fairview.org/oldlab/default.asp. Updated 2014.
- 19.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25(11):1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 20.Cassidy J, Kivlin J, Lindsley C, Nocton J Section on Rheumatology, Section on Ophthalmology. Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 2006;117(5):1843–1845. doi: 10.1542/peds.2006-0421. 117/5/1843 [pii] [DOI] [PubMed] [Google Scholar]
- 21.Colbert RA. Classification of juvenile spondyloarthritis: Enthesitis-related arthritis and beyond. Nat Rev Rheumatol. 2010;6(8):477–485. doi: 10.1038/nrrheum.2010.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Boekel MA, Vossenaar ER, van den Hoogen FH, van Venrooij WJ. Autoantibody systems in rheumatoid arthritis: Specificity, sensitivity and diagnostic value. Arthritis Res. 2002;4(2):87–93. doi: 10.1186/ar395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woodward AL, Harris ZL. Employment of a needs assessment survey to shape a novel web-based pediatric rheumatology curriculum for primary care providers. Pediatr Rheumatol Online J. 2013;11(1):26-0096-11-26. doi: 10.1186/1546-0096-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1):61–67. doi: 10.1016/s0749-3797(00)00258-0. S0749-3797(00)00258-0 [pii] [DOI] [PubMed] [Google Scholar]
- 25.Minnesota department of health. [Accessed November 14, 2013];Minnesota’s primary care workforce. 2011–2012 www.health.state.mn.us/divs/orhpc/pubs/workforce/primary.pdf. Updated 2013.
- 26.About family medicine. [Accessed June 25, 2015];Minnesota Academy of Family Physicians Web site. http://www.mafp.org/about/about-family-medicine. Updated 2015.
- 27.Phillips RL, Dodoo MS, McCann JL, Bazemore A, Fryer GE, Klein LS, Weitzman M, Green LA. Report to the task force on the care of children by family physicians. Washington, DC: The Robert Graham center for policy studies in family medicine and primary care in collaboration with the American Academy of Pediatrics Center for Child Health Research; 2005. [Google Scholar]
- 28.Makaroff LA, Xierali IM, Petterson SM, Shipman SA, Puffer JC, Bazemore AW. Factors influencing family physicians’ contribution to the child health care workforce. Ann Fam Med. 2014;12(5):427–431. doi: 10.1370/afm.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.