One can scarcely pick up a newspaper or popular magazine these days without finding an article describing how our health, well‐being and even our happiness are influenced by the microbial communities that co‐exist with us. A Google search for the term ‘microbiota’ returned almost 4M results. In fact, there has been an explosion of information in recent years regarding the characteristics and possible functions of the trillions of microbial cells that live on and within the human body. Perhaps because of its sheer biomass, complexity, and response to diet (including the consumption of probiotics), the gut microbiota has received the most attention. This is particularly in regard to its ability to shape the mucosal immune system and produce small molecule metabolites with diverse biological effects, leading to the notion that it may play a critical role in the pathogenesis of many digestive disease states. However, it is becoming increasingly apparent that the gut microbiota can influence physiological functions outside of the gastrointestinal system, and also that microbial communities in other body sites are relevant for human health and disease via their impact on physiological processes. This special issue of The Journal of Physiology was therefore planned to pull together short Topical Reviews that illustrate the breadth of this emerging field, solicited from individuals whose labs have made pivotal contributions to our understanding. The goal of this accompanying editorial is to introduce the constituent reviews and underscore common themes. We also seek to illuminate areas in which more research is needed to fully realize the potential of microbial manipulation in improving human health.
The five reviews that follow fall into two groups. Three address the nature and physiological effects of microbiota outside the alimentary tract – the skin, vaginal canal and the oral cavity (authored by Barnard & Li (2017), Smith & Ravel (2017) and Kumar (2017), respectively). The remaining articles focus on the gut microbiota, but rather than asking how this extensive microbial community influences digestive health and disease, they summarize evidence to support a role for the gut microbiota in regulating either systemic metabolism (Janssen & Kersten, 2017) or brain function (Dinan & Cryan, 2017). One immediate impression that arises from this collection is that while different sites in the body normally harbour distinct assemblages of microbes (and not just bacteria, but also viruses, fungi, archaea and protists), the functional effects that these fellow travellers exert are often overlapping (Fig. 1). Thus, commensal microbes may shape immune responses, protect us from colonization with pathogenic microorganisms, and supply metabolites that may be important to the health of the site where they are produced and/or which may enter the circulation to affect the function of distant sites. In this way, distinct niches that favour the growth of specific microorganisms based on conditions of humidity, pH, nutrient availability, etc., may nevertheless provide the opportunity for comparable beneficial effects on the host.
Figure 1. Physiological effects of diverse microbiota.
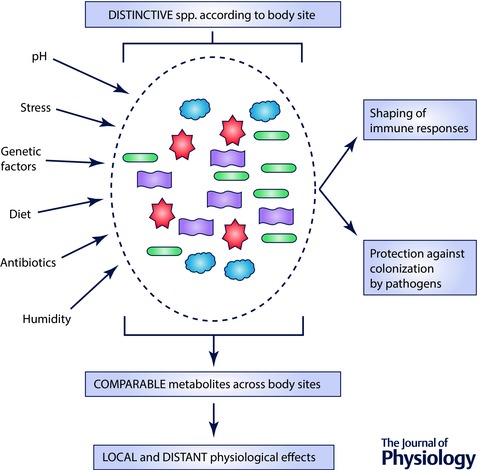
The microbiota that inhabits a given body site is a diverse collection of microbes (central oval) whose composition is established by the influences of a variety of factors, including those shown on the left‐hand side of the figure. (Note that the microbiota may also, in turn, further influence at least some of those conditions, such as pH (not shown).) Although the precise make‐up of the microbiota in a given body site may be distinctive, the collective microbiota tends to encode a comparable set of metabolic capabilities, leading to the production of common small molecules that can influence physiological functions both locally and, via the bloodstream or effects on nerve endings, more distantly. Various tissue microbiota also share the ability to shape local immune responses and to protect the niche that they inhabit from colonization by pathogens.
In considering the ways in which commensals may benefit cutaneous function, Barnard and Li address the vast surface area of the skin and the many different environments that it comprises, such as dry, moist and lipid‐rich areas (Barnard & Li, 2017). Interestingly, microbial communities are most diverse in the first of these, but the physiological properties of a given skin site are critical drivers of microbial colonization. When microbes were transferred from the forehead to the forearm, they quickly took on the characteristics of the recipient site – and vice versa. These authors also stressed the fact that strain‐level information is often needed to predict the impact of specific constituents of the cutaneous microbiota. Using the example of Proprionibacterium acnes, some strains are indeed associated with acne but others are found in health. These bacteria may supply protective functions, such as metabolism of triglycerides in sebum to short chain fatty acids (SCFAs) that are antimicrobial and lower skin pH, further restricting colonization. The beneficial roles of fungi and viruses are also stressed. Nevertheless, the authors also caution that skin commensals may become opportunistic pathogens in the setting of wounds. In fact, the actual effect (beneficial vs. injurious) of a given commensal may depend significantly upon its neighbouring microbes. Thus, the combination of two or more otherwise innocuous bacteria may represent a complementary ‘pathogroup’ contributing to poor healing in diabetic foot ulcers. Conversely, the possibility of phage therapy for infectious skin conditions is attracting growing attention.
Turning to the vaginal microbiota, Smith and Ravel cover five ‘community state types’ (CSTs) that have been described in women (Smith & Ravel, 2017). Four of these are dominated by Lactobacillus spp., which supply lactic acid that reduces vaginal pH and protects against infection. Lactic acid also stimulates antiviral responses and inhibits inflammation. Lactobacilli have also been shown to strengthen vaginal barrier functions, and especially the protective properties of cervicovaginal mucus. On the other hand, CST IV is characterized by other microbes and has been associated with an amplified inflammatory response. In some studies, the presence of CST IV has been associated with pre‐term birth but this is controversial. It is possible that the effect, if any, may reflect an interplay with host factors, such as polymorphisms that reduce mechanisms that control the inflammatory response. In this scenario, the acquisition of CST IV could represent a ‘second hit’ in a susceptible individual. Smith and Ravel also make clear that the vaginal microbiota changes dynamically as women move through various reproductive stages. For example, the loss of oestrogen after menopause has significant effects on the microbiota via a reduction in available glycogen. In that this effect can be reversed by topical oestrogen, a case might be made for more widespread application to restore a healthy microbial population.
Kumar covers the oral microbiota, which she characterizes as being in dynamic equilibrium with the host immune system (Kumar, 2017). In fact, she takes an interesting historical perspective as to whether bacteria in the mouth are the cause of disease at distant sites, a concept that was previously labelled as the ‘focal infection theory’. In the early 20th century, some proponents of this theory went as far as to recommend removal of all of the teeth to prevent or even treat a huge range of conditions. Thankfully, this unfounded approach fell from favour, but the improved analytical approaches of recent years have revealed that periodontal bacteria can be detected in a surprising range of extra oral sites, and may exert adverse effects in susceptible individuals. While there remains much work to be done, the possibility that improved oral hygiene may reduce the risk of negative pregnancy outcomes, pneumonia and cardiovascular disease has significant public health implications.
Janssen and Kersten tackle the question of whether the gut microbiota has a role to play in regulating metabolism (Janssen & Kersten, 2017). They develop the hypothesis that genetic and lifestyle factors may interact to cause obesity and metabolic disease, at least in part, via their ability to alter the microbiota. Nevertheless, they recognize that, at present, the data that support this hypothesis derive almost exclusively from cross‐sectional and correlative studies. They also discuss the evidence for putative bacterial and host/diet‐derived mediators of the crosstalk between the microbiota and metabolic regulation, including lipopolysaccharide, angiopoietin‐like protein 4 (Angptl4), bile acids and short chain fatty acids. Angptl4 is particularly intriguing. It acts as an inhibitor of lipoprotein lipase, and has been shown to be required for the protective effect of germ‐free status against the metabolic impact of a high fat diet. Similarly, the ability of bariatric surgery to improve metabolic dysfunction has highlighted possible roles for various bile acids and short chain fatty acids in protecting against obesity and improving glucose homeostasis. Since bile acids and short chain fatty acid levels are markedly influenced by the gut microbiota, and vice versa, delineation of their roles may identify new druggable targets. However, the authors also caution that most studies to date have been conducted in mice, which have very different profiles of these mediators than do humans.
Finally, Dinan and Cryan describe the multiple ways in which the microbiota and its products can signal to the brain, and the relevance of this microbiota–gut–brain axis for brain development, neurocognitive disorders, and changes in cognitive function that occur with ageing (Dinan & Cryan, 2017). They emphasize that the mode of delivery, lack of breastfeeding, infections, stress and environmental influences may all alter brain development via their impact on the microbiota, coupled with the genetic background of the host. At the other end of life, a reduction in the diversity of the microbiota, perhaps driven by dietary changes, may also impact mood and cognition. They also review the emerging evidence for links to diseases such as autism and Parkinson's disease, but sound a cautionary note about whether microbiota changes are core to the development of brain disease or are simply epiphenomena. Clearly, additional research is needed, not least because germ‐free mice exhibit both gastrointestinal and immune abnormalities that might influence results, and because neurocognitive disorders may impact dietary practices.
In summary, this set of Topical Reviews illustrates that, despite rapid advances, this overall field is still in its infancy and we need to move beyond cross‐sectional and correlative studies to fully understand effects and mechanisms. The field will also need to take on the challenging prospect of performing more work in human subjects, including longitudinal and interventional studies to prove cause‐and‐effect relationships, given that nearly all work to date showing a functional effect of the microbiota has been performed in animal model systems such as germ‐free mice with their own limitations. Improved analytical and computational approaches would accelerate such work. Critical questions to be addressed include: Which physiological effects of the microbiota in animal models are relevant to human biology? Amongst those that are relevant, what is the effect size in humans? Is it large or very small? And will these insights lead to new approaches to prevent, treat and/or diagnose illnesses that are more efficacious than currently available modalities? Overall, it is hoped that the articles included in this special issue will trigger further research into the many ways in which the microbiota may affect the physiological functioning of a variety of body systems. Indeed, there is substantial optimism that research in the microbiome field will lead to the development of additional therapeutic modalities to improve human health, which will move beyond the use of faecal microbiota transplantation for the treatment of refractory Clostridium difficile infection as well as currently available pre‐, pro‐, and synbiotics.
Additional information
Competing interests
Neither of the authors has any conflicts of interest with regard to this manuscript.
Funding
No direct funding was received in support of this manuscript.
Acknowledgements
Work from the authors’ laboratories on related topics has been supported by grants from the National Institutes of Health, the Crohn's and Colitis Foundation of America, Seres Therapeutics, Nestle, Takeda, and Intercept Pharmaceuticals, and unrestricted grants from the Shape Up and Estratest settlement funds.
This is an Editor's Choice article from the 15 January 2017 issue.
References
- Barnard E & Li H (2017). Shaping of cutaneous function by encounters with commensals. J Physiol 595, 437–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinan TG & Cryan JF (2017). Gut instincts: microbiota as a key regulator of brain development, ageing and neurodegeneration J Physiol 595, 489–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen AW & Kersten S (2017). Potential mediators linking gut bacteria to metabolic health: a critical view. J Physiol 595, 477–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar PS (2017). From focal sepsis to periodontal medicine: a century of exploring the role of the oral microbiome in systemic disease. J Physiol 595, 465–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SB & Ravel J (2017). The vaginal microbiota, host defence and reproductive physiology. J Physiol 595, 451–463. [DOI] [PMC free article] [PubMed] [Google Scholar]


