Abstract
Context:
Respiratory diseases are a common problem in our country and these are associated with significant morbidity and mortality.
Aims:
The aim of the paper was to analyze the pattern of diagnostic tests used and treatment prescribed for common respiratory diseases.
Settings and Design:
A total of 1028 pulmonologists, either member of Indian Chest Society or delegate attending the National Conference of Pulmonary Diseases (NAPCON) 2015, participated in the online survey.
Subjects and Methods:
The survey included questions pertinent to common respiratory diseases such as pulmonary tuberculosis (PTB), bronchial asthma, chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), and pneumonia.
Results:
Investigation used for severity assessment and diagnosis of PTB, was sputum for acid-fast bacilli (83.5%), for IPF was high-resolution computed tomography chest (85.6%), for severe pneumonia was arterial blood gas analysis (69.3%), for asthma was spirometery and peak flow (96.8%) and for COPDs was spirometry (87.2%). The most popular choice of treatment for PTB was directly observed treatment short course (55.7%), for bronchial asthma, it was long-acting beta agonist with inhaled corticosteroids (LABA + ICSs) (41.1%), for COPD, it was LABA, ICS, and long-acting muscarinic antagonist (LABA + ICS + long-acting muscarinic antagonist) (32.4%) and for IPF, it was pirfenidone and N acetyl cysteine (38.3%). About 67.5% of doctors preferred hospitalization for patients with severe pneumonia. About 84.5% pulmonologists ordered diagnostic tests and 55.5% prescribed treatment as per current guidelines.
Conclusions:
The majority of doctors (70.1%) in our survey followed recommended guidelines for respiratory disease diagnosis and treatment. However, there is a need for upgradation of treatment strategies currently used by doctors.
KEY WORDS: Asthma, chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, pneumonia, pulmonary tuberculosis, respiratory disease epidemiology, respiratory disease survey
INTRODUCTION
The common respiratory diseases afflicting Indian population are pulmonary tuberculosis (PTB), asthma, chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), and pneumonia. These diseases are associated with significant morbidity and mortality. Morbidity involves loss of school and work. It also implies significant financial costs for the patients in the form of hours of work lost, expenditure incurred for the diagnostic tests, and treatment prescribed. There are estimated 8.6 million cases of PTB that have been reported in 2012 among which India accounts for 26% of cases.[1] The data of global burden of diseases of death revealed that COPD, tuberculosis, and lower respiratory tract infection such as pneumonia are among the leading causes of death and disability in India.[2] Similarly, around 6% of school-going children are suffering from asthma and it has also been claimed that the prevalence of bronchial asthma is increasing.[3] COPD along with asthma account for 32 million cases in India.[4] Tobacco smoking, environmental tobacco smoke and biomass exposure account for the majority of cases of COPD. It has been suggested that treatment as per guidelines is more cost-effective. Murthy and Sastry[5] had calculated the estimated cost of treatment, as per guidelines for a patient with acute exacerbation of COPD, to be Rs. 11,660. However, the current trend in India of managing the respiratory disease as per recommended guidelines is largely unknown.
To assess this trend of diagnosis and treatment of common respiratory diseases this short questionnaire based online survey was planned during the National Conference of Pulmonary Disease (NAPCON-2015).
SUBJECTS AND METHODS
The pulmonologists who participated in the survey were members of Indian chest society and those who were registered for NAPCON-2015 held at Jaipur. The survey was conducted from September 5 to November 7, 2015, under the aegis of Asthma Bhawan, Jaipur. Members of Indian chest society and chest physicians registered for NAPCON from all throughout India were contacted through E-mail and text messages. The survey was also conducted during the conference at a display stall. The survey form was generated and displayed on Google on-line survey. The questionnaire [Appendix 1] link was sent to participants by E-mails and text messages. They were also sent two E-mails and four text message alerts as reminder. A total number of 1028 doctors responded and all were postgraduates with either an MD or diploma in chest medicine or MD in general medicine. They were asked questions about five respiratory diseases including PTB, asthma, COPD, IPF, and pneumonia. The study questionnaire was developed by a team of four pulmonologists to study the prescription behavior followed by medical officers and specialists in their regular clinical practices regarding investigation and treatment about the disease to the patient while managing cases of PTB, asthma, COPD, IPF, and pneumonia. The questionnaire was pretested and revised based on the pretest feedback. The correct answer for each question was decided by a panel of experts and was based on the recommended guidelines for management of asthma,[6] COPD,[7] PTB,[8] IPF,[9] and pneumonia.[10] The questionnaire along with the answer key is given in Appendix 1.
RESULTS
A total of 1028 doctors responded to the survey regarding the common respiratory diseases and the results are depicted in Table 1. The most common investigation and treatment for PTB were sputum acid-fast bacilli (AFB) by 857 (83.5%) pulmonologists and directly observed treatment short course (DOTS) by 573 (55.7%) pulmonologists, respectively. Similarly, for uncontrolled asthma, the common diagnostic investigations were spirometry – 806 (78.4%) and peak flow meter reading – 189 (18.4%). The most common prescription for uncontrolled asthma was long-acting beta-agonist (LABA) with inhaled corticosteroid (ICS) – 423 (41.1%). For COPD, the most common investigation for diagnosis was spirometry – 897 (87.2%). The most common prescription used was – LABA + LAMA + ICS – 333 (32.4%). For IPF, the most common investigation used was high-resolution computed tomography (HRCT) chest – 880 (85.6%). The common prescription given were pirfenidone + N acetyl cysteine (NAC) – 367 (38.3%), pirfenidone – 264 (27.5%), and prednisolone + NAC + azathioprine – 202 (21%).
Table 1.
Results of questions pertinent to the diagnosis and treatment of five respiratory diseases
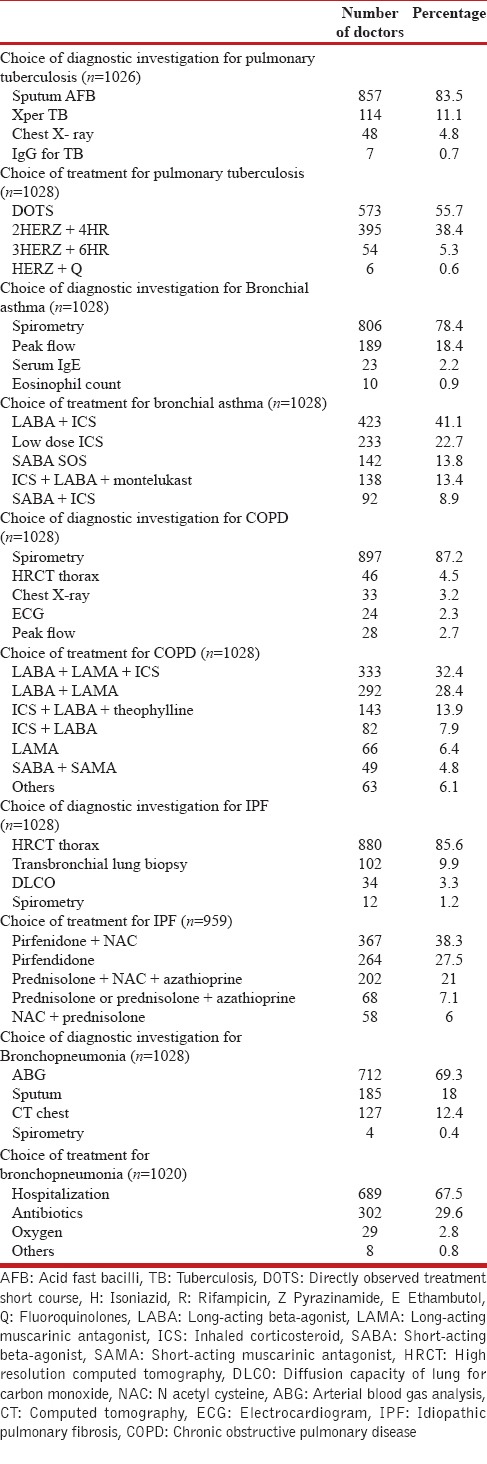
For severity assessment in a case of severe pneumonia, the most preferred diagnostic investigation included was arterial blood gas analysis (ABG) – 712 (69.3%). Most common prescription advised was hospitalization – 689 (67.5%), antibiotics – 302 (29.6%), and oxygen – 29 (2.8%).
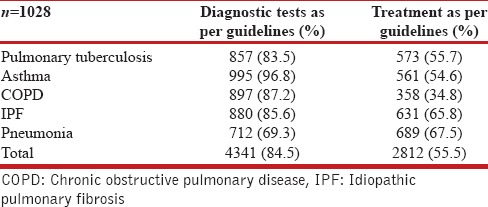
Table 2 reveals the adherence followed to current recommended guidelines while diagnosis and treatment. About 84.5% diagnostic tests and 55.5% treatment prescriptions by the pulmonologists followed current guidelines.
Table 2.
Pulmonologists practicing disease management as per recommended guidelines (n=1028)
DISCUSSION
Almost 84.5% of pulmonologist were using the basic diagnostic tools as per guidelines. It has been a common perception that spirometry has been an underused tool in the diagnosis of asthma and COPD. However, it is reassuring that 82.8% of pulmonologists were using it for the diagnosis of asthma and COPD. Strong recommendations by guidelines, easy availability, and low cost are some of the factors that are responsible for the widespread use of spirometry. Use of spirometry and peak flow in the diagnosis of asthma was noted in 995 (96.8%) doctors, which was in accordance with the guidelines recommended by Global Initiative of Asthma (GINA) committee.[6] GINA recommends the use of spirometry and peak flow for documenting reversible airflow obstruction in cases of asthma. A low reading on spirometry is a risk factor for asthma exacerbation also.
Similarly, for diagnosis of COPD also a global initiative of chronic obstructive lung disease (GOLD) recommends the use of spirometry which was used by 87.2% of doctors in our study.[7] A previous study conducted in Nigeria found out that only 33.3% of pulmonologists were using spirometry for diagnosis of COPD.[11] However, similar to our study, 86% of physicians were using spirometry for the diagnosis of COPD in a multinational study conducted in 12 countries.[12] GOLD presently recommends the use of spirometry, which is a reproducible test, for diagnosis and assessment of severity of COPD. The postbronchodilator spirometry values are being used to establish the GOLD stage of the disease and prescribe treatment accordingly.
Treatment of respiratory disease by pulmonologists as per recommendations was, however, practiced by 55.5% of pulmonologists only. In a patient with uncontrolled asthma, 54.6% of pulmonologists were using ICS and LABA combinations (with or without montelukast), but almost 45.4% of pulmonologists were not using inhaled steroids or used a sub-optimal dose, contrary to recommended guidelines.[6] Hesitation to use steroids may be a possible cause for this.
On the other hand, COPD patient of the survey (GOLD category B) was treated with ICS by almost 55% pulmonologists, contrary to guidelines with only 34.8% prescribing treatment as per guidelines.[7] The reason for the variance from guidelines could be a lack of knowledge of guidelines, availability of drugs and patient compliance.
Previous studies have revealed conflicting findings with regard to management of obstructive airway diseases. In 2007, a survey was conducted in the national pulmonology congress in Brazil to analyze the perception of asthma and COPD in pulmonologists.[13] Totally 227 pulmonologists participated in the survey and more than 50% of them were using LABA and ICS for the long-term treatment of asthma. The most commonly used treatment for COPD in the previous study was LAMA, LABA, and ICS. However, the limitation of the study was that the treatment as per the stage of both the diseases (asthma and COPD) was not specified. A multinational study conducted in 12 countries also revealed high awareness among treating physicians about COPD management.[12,14] The study also showed that for the treatment of COPD (GOLD Stage B), 38% general physicians and 67% of pulmonologists prescribed treatment as per guidelines.[14] In this study, we found that 34.8% of pulmonologists were prescribing treatment as per guidelines, and the patients of GOLD Stage B were being over-treated with ICSs.
There is another group of studies that have found deficiencies in the management of diseases in various countries.[15] General physicians were, particularly lacking in knowledge and offered sub-optimal management of COPD.[11] Similarly for asthma as well 92% physicians could not answer more than 50% of the questions in another survey.[16] Similarly, management of asthma was assessed in 976 physicians from Europe and the study revealed that the most common prescription for asthma was LABA and ICS.[17] However, depot steroids and LABA alone were still being by general physicians used contrary to recommendations.[17] A study conducted in primary care physicians in Kuwait found that only 32% were following guidelines for bronchial asthma.[18]
Sputum AFB was opted by more than 83.5% of pulmonologists, but 11.1% are using gene-Xpert as the first diagnostic test. In a resource limited setting diagnostic tests need to be used in a cost-effective manner. Although, diagnostic recommendations of sputum AFB by revised national tuberculosis control program (RNTCP)[8] were adopted by the majority of pulmonologists; treatment guidelines of RNTCP are not used whole heartedly. Almost 44% pulmonologist had reservations about DOTS therapy and they are using daily regimen. It emphasizes need to revise strategies of DOTS treatment plan.
IPF is a respiratory disease and its diagnosis and management remain a big challenge. Many of IPF patients are getting inadvertently treated for tuberculosis. In this study, we found that IPF was diagnosed with the help of HRCT in the majority of the cases. Almost 65.8% pulmonologists preferred pirfenidone as treatment option with 34.1% doctors still using prednisolone, for the treatment of IPF.[9] This demonstrates that Indian pulmonologists have quickly adopted the 2015 international guidelines. Frequent refresher courses and lectures during earlier NAPCONs might have played a role. Further, most of the doctors could correctly identify a case of severe pneumonia, 69.3% correctly recommended ABG and 67.5% recommended hospitalization for the same. The recent guidelines for management of pneumonia recommend the use of ABG in a patient with pneumonia with a pulse oxygen saturation of <90%.[10] ABG is, however, not available everywhere which explains that only 69.3% pulmonologists ordered the investigation to assess a patient with severe pneumonia. Similarly, the patient mentioned in the questionnaire had a CRB-65 score of more than 1, and thus had an indication for admission.[10] The use of this score will help reduce mortality related to severe pneumonia.
The results of the survey represent the opinion of the participating pulmonologists only, and the results require careful extrapolation with the pulmonologist group as a whole. However, around half of the pulmonologists attending the conference participated in the survey which could be completed by any doctor visiting the stall at the conference or online (to avoid selection bias). To the best of our knowledge, this has been the largest respiratory disease survey to be conducted in India. The survey helps us understand the current trend of respiratory disease management in India. It will help formulate future guidelines and to plan refresher courses for the practicing pulmonologists.
CONCLUSIONS
In summary, most of the pulmonologist are working according to the guidelines, but some strategies need amendments. The current treatment of respiratory diseases varies from the recommended guidelines, and thus, regular updates about new treatment guidelines are needed. Local issues that hinder the implementation of the guidelines should also be sorted out.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
APPENDIX
Appendix 1: NAPCON 2015 Survey
Purpose of the survey: To know the pattern of basic treatment and labeling of the respiratory diseases by physicians practicing Respiratory medicine in India, we are organizing this survey. The identity of the responder will be kept confidential. The results will be discussed in NAPCON 2015.
Participant benefit: Result of the survey will be useful in patient care. In addition, every participant will be given a Lung Smoker Model for patient education as an incentive at the time of NAPCON 2015. All fully evaluable answers will get a chance to win a lucky draw prize of Rs. 21,000/.
Method: An online questionnaire based survey will be conducted. The participant will be asked to select the most appropriate alternative to each of the questions.
*Required
Case I: A 60-year-old lady with probable pulmonary TB consults you (weight = 60 kg)*
-
One most relevant investigation to confirm the diagnosis.
- Sputum AFB
- Xray chest
- Mantoux test
- IgG for TB
- Xpert MTB.
Answer
a. Sputum AFB.
-
The investigation confirms pulmonary TB. Which is your most preferred prescription? The*
- DOTS
- HREZ 2 months HR 4 months
- HREZ 3 months HR 6 months
- HREZ + fluoroquinolone.
Answer
a. DOTS.
Case II: A 21-year-old and 63 kg asthmatic patient for last 12 years remains symptom free at rest but complains of some chest tightness on climbing a flight of stairs. He has good sleep except bouts of cough 2–3 times in a month. Asthma does not bother him much and he takes Salbutmol inhaler 2–3 times in a week*
-
One most relevant investigation to confirm the diagnosis
- Peak flow meter reading
- Spirometry
- Eosinophil count/CBC
- Serum IgE.
Answer
a. Peak flow meter reading or
b. Spirometry.
-
Which is your most preferred prescription?*
- Salbutamol SOS
- Low dose ICS
- LABA + ICS
- SABA + ICS
- ICS + LABA + montelukast.
Answer
c. LABA + ICS or
e. ICS + LABA + Montelukast.
Case III: A 62-year-old male, smoker with a label of COPD as diagnosis. He has almost stopped smoking, takes only 2 bidis/day. He gets breathless after walking 100 steps. He has had one exacerbation in the past one year*
-
One most relevant investigation to confirm the diagnosis.
- Xray chest
- Peak flow
- Spirometry
- ECG
- HRCT chest.
Answer
c. Spirometry.
-
Which is your most preferred prescription?*
- SABA + SAMA (need based)
- LAMA alone
- SABA + ICS
- LABA + LAMA
- SABA + LAMA
- LABA + LAMA + ICS
- ICS + LABA
- ICS + LABA + theophylline.
Answer
b. LAMA alone or
d. LABA + LAMA.
Case IV: 55 years, (weight = 60 kg) patient with bilateral reticular shadows in X-ray*
-
One most relevant investigation to confirm the diagnosis of IPF.
- Spirometry
- HRCT chest
- Diffusion test (DLCO)
- Transbronchial lung biopsy.
Answer
b. HRCT chest.
-
Investigations confirm diagnosis of IPF. Which is your most preferred prescription?*
- Prednisolone
- Prednisolone + azathioprine
- NAC + prednisolone
- Pirfenidone
- Pirfenidone + NAC
- Prednisolone + NAC + azathioprine.
Answer
d. Pirfenidone or
e. Pirfenidone + NAC.
Case V: 68-years, (weight = 70 kg) patient with bacterial pneumonia having respiratory rate 35/min, pulse rate 120/min. X-ray chest shows bilateral consolidation. Please write:*
-
One most relevant Prognostic Test.
- Sputum
- CT chest
- ABG
- Spirometry.
Answer
c. ABG.
-
Which is your most preferred prescription?*
- Antibiotics
- Oxygen
- Hospitalization
- Could not decide.
Answer
c. Hospitalization.
Name*
Address*
Mobile*
ICS Membership Number.
Place of Work*
Private Hospital
Government Hospital (teaching)
Government Hospital (nonteaching).
REFERENCES
- 1.WHO. Global Tuberculosis Report 2013. Geneva: WHO Press; 2013a. [Google Scholar]
- 2.GBD Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: A systematic analysis for the global burden of disease study 2013. Lancet. 2015;385:117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pal R, Dahal S, Pal S. Prevalence of bronchial asthma in Indian children. Indian J Community Med. 2009;34:310–6. doi: 10.4103/0970-0218.58389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, Kaur T, et al. Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH) Int J Tuberc Lung Dis. 2012;16:1270–7. doi: 10.5588/ijtld.12.0005. [DOI] [PubMed] [Google Scholar]
- 5.Murthy KJ, Sastry JG. Economic burden of chronic obstructive pulmonary disease. In: Rao KS, editor. Burden of Disease in India. New Delhi: National Commission on Macroeconomics and Health; 2005. pp. 264–74. [Google Scholar]
- 6.Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2015. [Last accessed on 2016 Jan 01]. Available from: http://www.ginasthma.org/
- 7.Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. [Last accessed on 2016 Jan 01]. Available from: http://www.goldcopd.org/
- 8.Agarwal SP. The revised national tuberculosis control programme: The gains and the future road map. Natl Med J India. 2005;18:225–9. [PubMed] [Google Scholar]
- 9.Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: Treatment of idiopathic pulmonary fibrosis. An update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192:e3–19. doi: 10.1164/rccm.201506-1063ST. [DOI] [PubMed] [Google Scholar]
- 10.Gupta D, Agarwal R, Aggarwal AN, Singh N, Mishra N, Khilnani GC, et al. Guidelines for diagnosis and management of community-and hospital-acquired pneumonia in adults: Joint ICS/NCCP(I) recommendations. Lung India. 2012;29(Suppl 2):S27–62. doi: 10.4103/0970-2113.99248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozoh OB, Awokola BI, Buist SA. A survey of the knowledge of general practitioners, family physicians and pulmonologists in Nigeria regarding the diagnosis and treatment of chronic obstructive pulmonary disease. West Afr J Med. 2014;33:100–6. [PubMed] [Google Scholar]
- 12.Menezes AM, Landis SH, Han MK, Muellerova H, Aisanov Z, van der Molen T, et al. Continuing to confront COPD international surveys: Comparison of patient and physician perceptions about COPD risk and management. Int J Chron Obstruct Pulmon Dis. 2015;10:159–72. doi: 10.2147/COPD.S74315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campos Hda S, Lemos AC. Asthma and COPD according to the pulmonologist. J Bras Pneumol. 2009;35:301–9. doi: 10.1590/s1806-37132009000400003. [DOI] [PubMed] [Google Scholar]
- 14.Davis KJ, Landis SH, Oh YM, Mannino DM, Han MK, van der Molen T, et al. Continuing to confront COPD international physician survey: Physician knowledge and application of COPD management guidelines in 12 countries. Int J Chron Obstruct Pulmon Dis. 2014;10:39–55. doi: 10.2147/COPD.S70162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Umoh VA, Ukpe IE. Knowledge of the asthma guidelines among doctors in a tertiary care hospital in Nigeria. Indian J Allergy Asthma Immunol. 2012;26:77–82. [Google Scholar]
- 16.Stukus DR, Green T, Montandon SV, Wada KJ. Deficits in allergy knowledge among physicians at academic medical centers. Ann Allergy Asthma Immunol. 2015;115:51–5.e1. doi: 10.1016/j.anai.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Caminati M, Magnoni MS, Rizzi A, Braido F, Foresi A, Bettoncelli G, et al. Asthma management among different specialists: Results from a national Italian survey. Eur Ann Allergy Clin Immunol. 2014;46:74–82. [PubMed] [Google Scholar]
- 18.Almutawa FN, Al-Mutairy G, Al-Arada N, Kamel MI. Perception of primary care physicians about guidelines of bronchial asthma. Alexandria J Med. 2014;50:17–24. [Google Scholar]


