Abstract
HIV testing promotion is a critical HIV prevention strategy, especially among at-risk groups such as young men who have sex with men (YMSM). Based on a web survey of 194 YMSM (18–24), we examine the association of social network characteristics and functions, and of individual-level characteristics, with three HIV testing behaviors (ever, repeat, and recent testing). Network homophily was associated with recent testing in multivariable models. The network function of information acquisition was associated with ever testing and repeat testing. Perceived stigma regarding HIV-related help-seeking was negatively related to recent testing. Individual characteristics were associated with testing outcomes in all models; age, perceived behavioral control, and positive attitudes had the greatest influence. Individual characteristics had a stronger association with ever testing and repeat testing than network characteristics and functions; however, this relationship was reversed for recent testing. Findings support the value of multi-level and network-focused interventions for promoting HIV testing among YMSM.
Keywords: Homophily, Network range, Stigma, Information acquisition, Core discussion networks
Resumen
La promoción de la prueba del VIH es una estrategia fundamental de prevención en grupos de riesgo, incluyendo los hombres jóvenes que tienen sexo con otros hombres (YMSM). Utilizando una encuesta realizada por el internet (N = 194 YMSM entre las edades de 18–24 anos), analizamos la asociación entre tres comportamientos de pruebas del VIH (nunca testeado, prueba repetida, y prueba reciente), las características y funciones de las redes sociales, y las características a nivel individual de los YMSM. La homofilia de red estuvo asociada con pruebas recientes en modelos multivariables. La función de la red para adquirir información de VIH estuvo asociada con haber testeado y haber repetido la prueba. El estigma de VIH asociado con búsqueda de ayuda estuvo negativa-mente asociado con con pruebas recientes. Características individuales se asociaron con los resultados de pruebas en todos los modelos; la edad, la percepción de control del comportamiento, y actitudes positivas tuvieron la mayor influencia. Las características individuales tuvieron una asociación más fuerte que las características y funciones de la red; sin embargo, esta relacion se invirtió para la prueba reciente. Los resultados apoyan el valor de intervenciones multiniveles con un enfoque de redes sociales para pro-mover la prueba del VIH entre los YMSM.
Introduction
Young men who have sex with men (YMSM) represent a disproportionate number of new HIV cases. Indeed, MSM aged 13–24 are the highest-risk group for new HIV infections in the United States (US) [1]. Moreover, rates of new HIV infections in this group have been increasing: between 2006 and 2009, there was a 34 % increase in HIV infection rates among YMSM [2]. These trends in HIV incidence among YMSM stand in contrast to trends in the US population as a whole, for whom HIV incidence rates have remained stable over the same time period [1].
A key HIV prevention strategy is to promote testing so as to increase the number of people who are aware of their HIV status. This is an important focus because most HIV transmission occurs among undiagnosed persons [2]. National goals have been set to increase testing amongst MSM [3], and annual testing guidelines have been established for sexually active members of this group. Additionally, more frequent HIV testing is recommended for MSM who have multiple or anonymous partners, who use drugs while having sex, or whose sex partners participate in these activities [4]. Despite these efforts, national surveillance data show that many MSM don’t adhere to these HIV testing guidelines, and that many HIV-positive MSM remain unaware of their infection [1, 5]. Therefore, there is a need for concerted effort to promote regular testing among sexually active MSM.
To inform prevention efforts, increasing research has focused on understanding the correlates of HIV testing among MSM [6, 7]. Although social networks are recognized as important drivers of both HIV risk behavior and prevention efforts among MSM [8], the published literature has been disjointed with respect to the many network effects which may simultaneously influence HIV testing behavior. Therefore, we seek to theoretically advance the field by investigating the concurrent contribution of several theoretically-derived network-related variables to HIV testing behavior. Specifically, we examine correlates of the history of ever testing, repeat testing, and recent testing (i.e., in the past 12 months).
Individual-Level Correlates of HIV Testing
Most of the literature has focused on individual-level correlates of HIV testing. The following demographic factors have been associated with HIV testing behavior among MSM: older age, [6, 9–18]; education level [16, 19, 20]; and socio-economic status (SES) [11, 16, 21]. MSM’s high-risk sexual behavior has also been found to be either negatively associated with timely HIV testing [11, 15, 20, 22], or to be unassociated with it [10, 12, 23]. Seeking sexual partners on the Internet has been negatively associated with HIV testing among MSM [19, 20]. As for psychosocial factors, perceptions of risk have been positively associated with HIV testing [6, 15, 18, 23, 24], as has self-efficacy to engage in protective behaviors [21]. More use of information regarding HIV/AIDS has also been associated with greater HIV testing intentions among YMSM [25]. Concern about potentially transmitting HIV to others is an attitude that has also been positively associated with HIV testing [26].
Social Networks and HIV Testing
Social networks can be defined as sets of actors and their relationships [27]. Two general types of social network characteristics may affect health: (1) characteristics of relationships between individual people in a network, or ties; and (2) characteristics of the overall network structure, or patterns of relationships between all of the members of a network [28].
Longitudinal research in varied health domains has shown that social similarity between people, or the tie characteristic of “ homophily” [29], promotes the spread of health behaviors between them [30–33]. Homophily can refer to similarity in demographics such as race, gender or age; attitudes; or behavior (e.g., substance use). Similarly, research in the context of HIV testing in several countries has shown that MSM who have more social interaction with other MSM are more likely to have had an HIV test [22, 23, 34].
People are also more influenced by those for whom they have positive feelings. Social influence theory contends that individuals are more likely to be influenced by people they “like” [35]—particularly in ambiguous situations in which they rely upon others for cues as to how to behave [36]. Closer relationships or “stronger ties” (37) constitute a tie characteristic usually characterized by “liking”, and there is typically stronger interpersonal influence in relationships that are emotionally closer [31]. Stronger relationships may be characterized by greater contact frequency and more time spent together [37–40]. While we are unaware of any research regarding strong ties and HIV testing among MSM, one study showed that HIV risk behavior among MSM is related to the influence of strong ties [41].
Although structural characteristics of networks have been associated with the transmission of health behaviors in general [42–45], there has not yet been a research focus on potential relationships between structural characteristics of MSMs’ social networks and their HIV testing behavior. “Cohesion”, or connectedness between network members [46], is an especially important structural characteristic due to the potential for social influence within cohesive networks [47, 48]. Such influence may be driven by exposure to common messages [49], message reinforcement [45], informal social control [50] and similarity in attitudes and opinions [51].
Network cohesion is often measured by network density [47], which is the number of links present in a network divided by the total possible links between network members [31]. In essence, this refers to the number of people in a person’s network who have any connection to one another. Greater network density is associated with the transmission of health behaviors within a network [42–45]. Similarly, the overall network proportion of ties in a network based on close interpersonal relationships, which we call “strong tie proportion”, can be an indicator of cohesion [47]; that is, the number of people in a person’s networks who are close to one another (as opposed to just having some connection, as with network density). While not previously investigated, both measures hold potential for influencing HIV testing among YMSM.
Network “range”, or the extent to which one’s ties cross the social boundaries of different cohesive subgroups in a network [52], is another structural network characteristic that network theory suggests may exert an influence on HIV testing behavior. Network range is an indicator of network diversity since people occupying different roles in relation to an individual (e.g., family members, best friends, acquaintances or health care providers) are likely drawn from different network subgroups, and thus have access to different network-mediated resources. This network characteristic has been associated with acquisition of resources that can affect health behavior [28]. The potential relationship between network range and HIV testing behavior has yet to be investigated.
In addition to network characteristics, networks can influence health via the functions they perform, including (1) social support; (2) social influence; and (3) access to resources [28]. Social support has indeed been associated with HIV testing in the US [11, 17, 21, 53, 54] and internationally [16, 55]. Additionally, HIV-related stigma is characterized by social distancing [56] from people who are HIV-positive (or perceived to be HIV-positive); indeed, several studies have found a significant, negative association between social support and both perceived and enacted stigma among people with HIV/AIDS [57–59]. HIV-related stigma from one’s network members has been negatively associated with testing, or positively associated with delayed testing [18, 60, 61].
Additionally, the network function of social influence has been repeatedly shown to influence health behavior. Perceived social norms are a key form of network-mediated influence [31, 49]. Norms are “prevailing codes of conduct that either prescribe or proscribe behaviors that members of a group can enact” [62]. Behavioral norms emerge when our shared attitudes, or positive or negative evaluations of a behavior, receive social validation [63]. Health-related research has primarily investigated perceived norms, of which two main types are most important: (1) descriptive norms: what we believe that other people do; and (2) injunctive norms: the perception that others want us to perform a behavior. For example, in prior research regarding safer sex among MSM, the injunctive norm of “assumed approval of condom use by others” was a significant predictor of self-reported condom use [64]. Descriptive norms are powerful correlates of motivation to engage in a behavior among youth [65].
Social systems theory suggests that networks provide resources such as information in ways that can affect HIV testing behavior [66]. Theory suggests that new information can facilitate action in a number of ways that could affect HIV testing behavior, including assisting with decision making [67, 68], problem solving [69–72], and pursuit or coordination of new lines of action [73–75]. Notably, prior research has shown a strong relationship between YMSMs’ HIV-related information acquisition and their involvement in the gay community [76]. However, the potential role of social information acquisition in HIV testing behavior has not yet been examined.
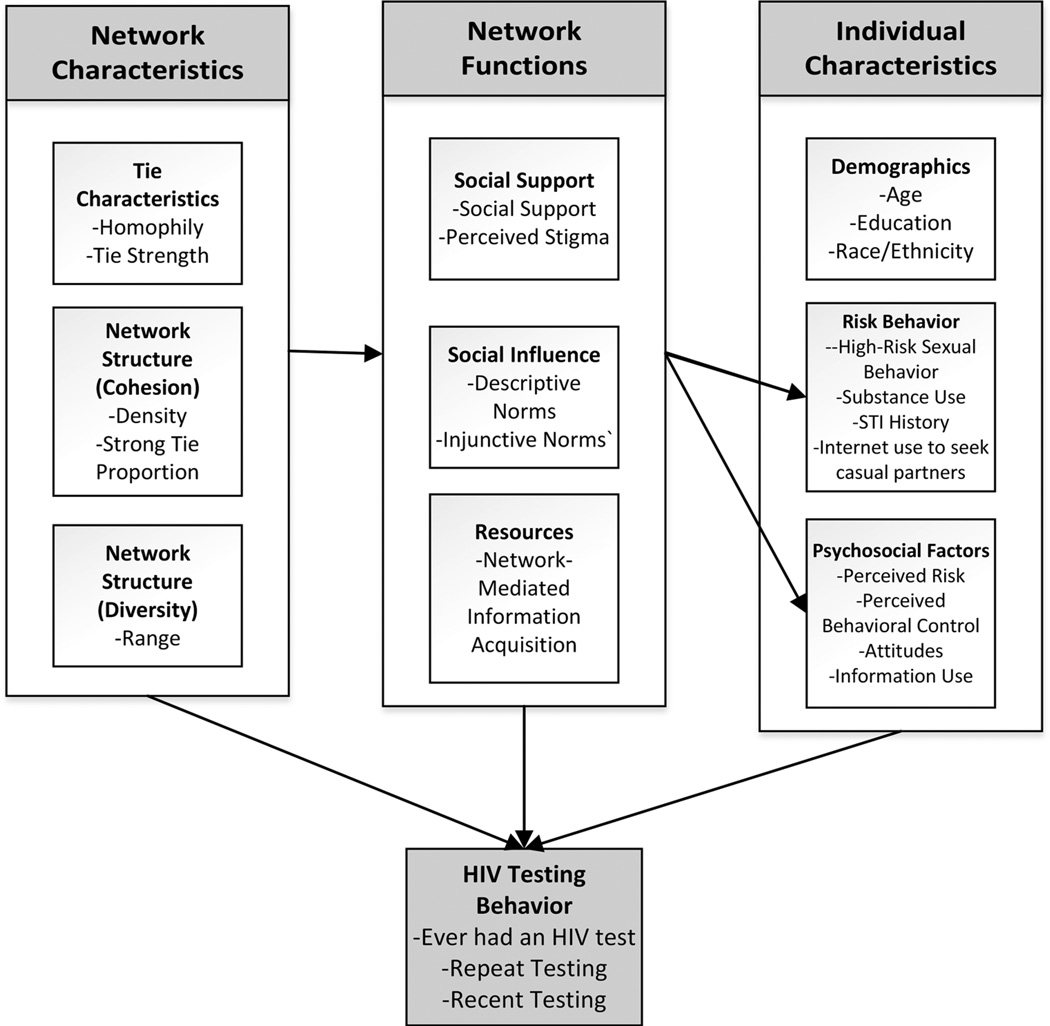
We examine the simultaneous contribution of each of the above network characteristics and functions in HIV testing behaviors among YMSM. Building on the literature reviewed above, Fig. 1 depicts a model outlining the variables included in the analyses, and their relationships. In doing so, we focus on core discussion networks. The concept of “core discussion networks” refers to the subset of one’s personal network with whom one discusses “important personal matters”; this measure has been used since 1985 in the General Social Survey of the US population [77, 78]. The core discussion network typically includes people with whom we share moderately strong ties; these are people who are important in our lives and are often the people who provide us with various types of support [78]. For most Americans, core discussion networks include a mix of both kin and non-kin [78]. In this study, the primary theoretical justification for focusing on core discussion networks derives from previous research that showed that HIV-related issues tend to be discussed only with a subset of network members, typically including strong ties, such as partners, close friends or family, or health care or service providers [66–68].
Fig. 1.
Model of the role of network characteristics, network functions and individual characteristics in HIV testing behavior
To examine the relative importance of network- and individual-level factors, we assess network effects independent of the aforementioned individual-level traits, and compare the relative explanatory power (R2) of network-versus individual-level features on testing behaviors.
Methods
Sample
Participants included 194 YMSM who completed a web survey in 2011. Eligible participants were men between the ages of 18 and 24 who resided in Metropolitan Detroit and reported sexual activity with a male partner in the previous 6 months. We did not exclude HIV-positive participants from the study since the factors contributing to their decisions to seek HIV testing could contribute to our overall understanding of testing behavior among YMSM. Therefore, HIV status was not mentioned in any of the recruitment materials. To recruit a diverse sample, we recruited participants through a range of venues: university health clinics, dating websites, lesbian, gay, bisexual and transgendered (LGBT) organizations in the area, local bars/clubs, social media sites, public postings, AIDS service organizations (ASOs), and health departments. All participants were screened using an online tool that verified their eligibility, and they had to confirm comprehension of informed consent material and agree to participate in the study in order to complete the self-administered survey. Each participant received a $25 e-gift card from either Amazon or iTunes for participating, based on their preference.
Procedures
The survey asked questions about demographics, social network relationships and interactions, HIV testing behavior and experiences, sexual and risk behavior, HIV-related knowledge and perceptions, and HIV information acquisition and use. The survey was designed according to published best practices [79], pilot-tested and hosted on a Sawtooth web survey software-enabled dedicated website; this allowed participants to complete surveys online and have their responses recorded in a database. To address potential duplicate or false entries [80], we verified unique cases by cross checking participant IP and email addresses with various web applications (e.g. IP lookup, Facebook), without maintaining any record of this information or tying it to the data. All unverified cases and flagged entries were removed from analysis. After the final cases were identified, data were de-identified and transmitted to SPSS software. The National Institutes of Health granted the study a Certificate of Confidentiality, which ensured respondents’ privacy, even in the case of a legal subpoena. The study was approved by the Health Sciences and Behavioral Sciences Institutional Review Board of the University of Michigan. The survey was completed between March 29, 2011 and May 26, 2011.
Measures
Dependent Variables
Ever Had an HIV Test
This binary variable was created based on participants’ responses to the question with a free-text response: “How many times in total have you been tested for HIV?” and “Of the X times you have been tested for HIV, how many times have you been notified of the test results?” Due to the heavily skewed nature of these variables, a binary outcome variable (Yes = 1) was created to indicate whether participants had ever received an HIV test and if they had received the test results at least once.
Repeat Testing
Those who had been tested more than once, who and had received their test results every time they had been tested, were identified as “repeat testers” (Yes = 1).
Last Test in Past 12 Months
Participants who reported having been tested were then asked to “enter the date of your last HIV testing and counseling session”. The difference between the last test date and the date of the survey was then calculated in months. A binary variable (1 = Yes) was then created to identify whether participants had received their last HIV test within the past 12 months.
Independent Variables—Individual-Level Variables
Demographics
Participants provided their date of birth, which was used to calculate “Age”. The highest “Level of education” that they had completed was transformed, due to variable skewness, into a binary variable with two values: (1) “High school education or less” and (2) “Education beyond high school”. They also indicated their race (White/European American, Black/African American, Asian, Native American/Alaska Native, Hawaiian/Pacific Islander and Other), and ethnicity (Hispanic/Latino or not). To investigate potential testing disparities suggested by available literature [81], a binary “Black/African American or Hispanic/Latino” variable indicated that the participant identified as being part of one or both of these groups.
Risk Behavior High-risk Sexual Behavior
A binary variable (High risk = 1) was created for participants who reported having engaged in anal (either receptive or insertive) or vaginal sex (insertive only) without a condom in the previous 2 months with one or more partners whom they knew to be HIV-positive, or whose HIV status was unknown to them.
Substance Use
Participants were asked to answer “yes” or “no” to whether they used any of twelve controlled substances (not including alcohol) within the past 2 months. Responses were totaled and made into a binary variable (Yes = 1).
Sexually Transmitted Infection (STI) History
This was assessed by the question, “have ever been told by a doctor, nurse, or other health professional that you had any of the following sexually transmitted diseases?” Participants indicated “yes” or “no” to eight options, including “none of the above”. The total number of STIs that the participant had was then calculated as an “STI history” variable.
Internet Use to Seek Casual Partners
Based on an existing measure of partner-seeking among young MSM on the Internet [82], participants were asked how many times they had used the Internet in the past 2 months “to hook up”. Responses were on a 7-point scale ranging from “Never” to “More than once a day”. Because this survey was conducted prior to the widespread adoption of mobile applications to facilitate partner seeking among MSM (e.g., Grindr, Scruff), respondents’ answers most likely refer to use of web-based applications.
Psychosocial Factors Perceived Risk of HIV
Similar to Golub and Gamarel [18], this construct was assessed using a single question that asked participants to evaluate the likelihood that they will become “HIV-positive in the future”. Responses were on a 6-point scale ranging from “Extremely unlikely” to “Extremely likely”.
Perceived Behavioral Control Regarding HIV Testing
Drawing from the Theory of Planned Behavior (TPB) [83] and our previous published work on HIV testing intentions of YMSM [25], we administered a 5-point Likert-like scale asking respondents how easy or hard it would be for them to find a location nearby to get an HIV test. Higher values on this variable meant it was easier.
Attitudes Toward HIV Testing
Also drawing from the TPB and our previous research, we operationalized attitudes as the level of agreement with the statement, “Getting an HIV test is the responsible thing to do”. Response options were on a 5-point Likert-like scale, with “Strongly disagree” as the lowest value and “Strongly agree” the highest.
Information Use Regarding HIV Testing
Drawing from other research [84, 85], we developed an original 15-item scale that assessed use of HIV/AIDS information to make decisions related to HIV testing. We asked respondents, “In which of the following ways did you use the HIV/ AIDS information that you got in the past 12 months?” Among those participants who had indicated that they had received HIV/AIDS information from their social networks, we then measured frequency of using information as a summed score of five items focused on HIV testing, including “Decide whether to get tested for HIV,” “Find a place to get tested for HIV,” and “Decide whether to ask a casual sexual partner to get tested for HIV.” The five answer options ranged from “Never” to “A great deal.” When subjected to a principal axis factor analysis with varimax rotation, one factor was produced with an Eigenvalue of 3.848 and explained 76.96 % of the variance explained. Reliability was excellent (α = 0.925).
Network Characteristics
Participants’ social networks were elicited using a name generator for core discussion networks adapted from the General Social Survey [86]. Participants were asked, “From time to time, most people discuss important personal matters with other people. Think about all of the people in your life with whom you have discussed, or would feel comfortable discussing, HIV/ AIDS prevention or testing. This might include friends, members of your family, sexual partners, coworkers, health care providers or acquaintances…please select up to 7 people that come to mind.” We believed it was important to specify that the core discussion network members named should be people with whom one could talk about HIV/ AIDS since such people would be those who would be most likely to affect one’s HIV/AIDS-related testing behavior, or provide support if someone were to test positive. The maximum network size of seven was chosen in light of national survey data showing that the average network size of Americans is 2.08, with the modal network size being zero and a mere 4.9 % of the population having six or more core discussion network members [78]. Due to the limitations of human memory, core discussion network data tend to be more accurate than alternatives that incorporate less close relationships, or “weak ties” [78]. After naming each network member, participants were asked to answer questions about the demographic characteristics of each member, their relationship with each them, the nature of interactions between them, and how well each of these network members knew one another (if at all).
Network Homophily
Gender and age homophily were first calculated using the validated E-I index measure, which assesses the number of ties external to the group minus the number of ties internal to the group, divided by the total number of ties [87]. In this case, the E–I measure considered the number of people in the same age group (an age within 5 years of that of the participant vs. not in that age range) and the gender group (males vs. not males). Each score was then standardized. Next, we included responses to the question, “How many of your friends are men who also have sex with other men?” Responses were on a 5-point scale ranging from “None” to “Some” to “All”. Responses to this question were also standardized. Standardized scores for all three types of homophily were summed; in the resulting composite score, higher scores indicated more tie homophily.
Ego-Alter Tie Strength
In line with the extant literature, we used frequency of contact as an indicator of time spent with a person and therefore of tie strength [37–40, 88]. Our novel measure was constructed as follows. In free-text fields, participants indicated how often they communicated with each network member per week via several media “on average”. Media included the Internet, telephone, and face-to-face. Additionally, participants indicated how many text messages they send to each person “on an average day”; these were then transformed into weekly values. Responses for all media were then totaled for each network member, and then divided by network size to create an indicator of mean tie strength between the participant and their network members.
Network Density
We used the standard measure of density [27]: the total number of ties present in a network divided by the number of possible ties in that network.
Strong Tie Proportion
Following the published literature [47], we assessed the overall network proportion of ties based on close interpersonal relationships. This was measured by the number of pairs of network members that participants indicated “know each other well”, divided by the total number of ties in the network.
Network Range
Based on the literature regarding network range as a measure of relationship type diversity [89], we calculated range using participants’ responses to the question “What is your relationship to this person?” regarding each of their network members. Options included parent, sibling, other family member, health care provider, best friend, friend or acquaintance, lover or boyfriend, and ex-lover. A total of the number of different relationships represented in the network was then created, with larger numbers indicating more variety in relationship types.
Network Functions Social Support
This was calculated to refer to the availability of HIV-specific social support from network members named via the aforementioned procedure. After naming each network member, participants were asked to state whether (1) this person “would be supportive if you had HIV”; and (2) this person would go with them to get an HIV test. Responses were on a binary scale (1 = Yes, 0 = No). For each network member, a “social support” variable was created as a sum of the values for each of the two support-related questions; these were then summed for a network total and then standardized.
Perceived Stigma
Given our focus on HIV testing behavior, we created a scale that measured perceived stigma specifically in the context of help-seeking in relation to HIV/AIDS. We believed this narrow focus was important since broader manifestations of stigma such as prejudice and discrimination, often the focus of other instruments, may not have a strong impact on HIV testing behavior [90]. Our measure was based on an established measure concerning the perceived social costs of help-seeking [91] that was adapted to the HIV/AIDS context. The scale summed responses to four survey items; these concerned interactions with all members of a respondent’s personal network, including weaker ties, not just the core discussion network members identified elsewhere in the survey. Perceptions of stigmatizing attitudes were conceptualized as an indicator of social support from the broader social network since represents perceived acceptance and inclusion, or lack thereof, from others [92]. Furthermore, we reasoned that people outside of the core discussion network may be more likely to openly express stigmatizing attitudes concerning HIV/AIDS-related help-seeking, and we felt this was important to capture from a network perspective. Two items asked participants to state their level of agreement as to whether they would “make myself and the person I approached uncomfortable” if they asked another person for information about where to get tested for HIV, or what their HIV test results meant. Responses were on a 5-point scale from “Strongly disagree” to “Strongly agree”, with higher scores indicating more discomfort. The other two items also asked “how hard it would be” to discuss getting tested with someone the participant was dating or a casual partner. Responses to these questions ranged from “Very easy” to “Very hard” on a 5-point scale, with higher scales indicating more difficulty. Principal axis factor analysis with varimax rotation revealed a single factor with an Eigenvalue of 2.445 and explained 61.13 % of the variance. The values for each of these four questions were summed and standardized. The reliability of this scale was good (α = 0.783).
Descriptive Testing Norms
This measure was based on a validated scale for subjective norms in AIDS prevention [93]. The scale represented the sum of responses to two questions on the subjective norms scale: (1) “Most people who are important to me have gotten an HIV test” and (2) “Most of my male friends have gotten an HIV test”. Responses were on a 4-point scale from “Strongly Disagree” to “Strongly Agree”; these questions addressed interactions with everyone in a person’s social network (including weaker ties) and not just the core discussion network members since norms spread through weak ties as well as strong ones [32]. This scale had good reliability (α = 0.71).
Injunctive Testing Norms
This scale combined responses to two questions on the aforementioned validated subjective norms scale [93]: (1) “Most people who are important to me think that I should get tested for HIV” and (2) “Most people whose opinion I value have encouraged me to get an HIV test”. Responses were on a 4-point scale from “Strongly Disagree” to “Strongly Agree”. As above, this referred to interactions with anyone in the participant’s social network, not just core discussion network members, due to the fact that norms can be transmitted via both weak and strong ties [32]. The reliability of this scale was very good (α = 0.87).
Network-Mediated Information Acquisition
Based on extant theory and empirical research showing that HIV/ AIDS information is acquired from social networks via both purposeful and non-purposeful means [94–98], we created an original five-item scale that asked “how much you have gotten information in each of the following ways in the past 12 months”. Questions included “People give me HIV/AIDS information without me asking for it”, “I search for HIV/AIDS information with someone else” and “I ask someone else to look for HIV/AIDS information for me”. Responses were on a 4-point scale including “Never”, “A little”, “Some”, and “A lot”. We conducted a principal axis factor analysis with varimax rotation with these five items; results showed the existence of one factor with an eigenvalue of 2.72 and explained 54.31 % of the variance. Reliability was good (α = 0.78). To construct this measure, we then summed responses to these five variables. These questions concerned interactions with anyone in the participant’s social network, not only the core discussion network members. This decision was made since the existence of HIV prevention efforts directed towards MSM means that information may be obtained from health care providers, outreach workers, activists and others outside of the core discussion network. We felt that such information acquisition events were important to capture since they could influence a participant even if such information did not come from the confidantes in a core discussion network.
Data Analysis
We explored the distribution, central tendency and variance for each network-related and individual-related variable using descriptive statistics, graphs and plots (see Table 1). The internal reliability of each scale was assessed with Cronbach’s alpha and factor analyses were conducted to evaluate their construct validity.
Table 1.
Survey participant demographics, risk behavior and psychosocial characteristics (n = 194)
| Percentage | Number | Mean (SD); range | |
|---|---|---|---|
| Age | |||
| Mean (s.d.) | 20.66 (1.71); 18–24 | ||
| Racea | |||
| Black/African American | 57.2 | 111 | |
| White/European American | 38.7 | 75 | |
| Native American/Native Hawaiian/Pacific Islander | 5.2 | 10 | |
| Asian | 6.2 | 12 | |
| Other | 6.7 | 13 | |
| Hispanic/Latino | 17.5 | 34 | |
| Education | |||
| Some high school | 5.2 | 10 | |
| High school/GED | 47.4 | 92 | |
| Technical school | 1.5 | 3 | |
| Some college | 35.6 | 69 | |
| Bachelor’s/graduate degree | 9.8 | 18 | |
| Sexual identity* | |||
| Gay | 84.5 | 154 | |
| Bisexual | 13.5 | 26 | |
| Heterosexual | 3.6 | 5 | |
| Other | 3.1 | 6 | |
| Risk behavior | |||
| High-risk sexual behavior in the past 2 months | 9.3 | 18 | |
| Substance use in the past 2 months | 48.2 | 92 | |
| STI history | 13.9 | 27 | 0.22 (0.61); 0–4 |
| Internet use to seek casual partners in the past 2 months | |||
| Never | 67.0 | 130 | |
| 1–3 times per month | 19.0 | 37 | |
| 1–6 times per week | 9.8 | 19 | |
| One or more times per day | 3.0 | 6 | |
| Has main partner | 16.0 | 31 | |
| Psychosocial characteristics | |||
| Perceived risk | 2.27 (1.23); 1–6 | ||
| Perceived behavioral control re: testing | 4.12 (0.92); 1–5 | ||
| Attitude to testing | 4.44 (0.79); 1–5 | ||
| Information use | 11.73 (9.28); 0–25 | ||
| HIV testing | |||
| Has ever had an HIV test | 64.4 | 125 | |
| Repeat HIV tester | 46.4 | 90 | |
| Last HIV test in past 12 months | 43.8 | 85 | |
| HIV-positive | 11.6 | 15 |
More than one response possible
Logistic regression analyses were conducted to evaluate predictors of HIV testing behavior in the sample. Where appropriate to the measurement level of the variable, preliminary analyses were conducted to ensure no violation of the assumptions of normality and multicollinearity. Separate models were run for the three different outcome variables (ever tested, repeat testing, tested within the past 12 months). For the “ever tested” model, all participants (including those who were HIV-positive) were included. Results for the repeat testers model were unchanged when restricted to only those participants who had been tested at least once in their lifetime, and thus the full non-HIV positive sample (n = 179) was included in the final analyses. For the “tested within the past 12 months” sample, we excluded all participants who received an HIV diagnosis more than 12 months ago (n = 179), since we reasoned that these people were already diagnosed and thus diagnostic testing would take on a different significance for them.
The variables were entered into each regression in steps. Variables were initially tested for a bivariate association with the outcome variable in unadjusted models, and then entered into multivariate adjusted models. Then, in order to determine the influence of network characteristics (tie characteristics and network structure), we ran our first model (Step 1). Next, the network function variables were entered (Step 2—social support, social influence and resource-related variables). Finally, the influence of individual-level factors, including demographic covariates, risk behavior and psychosocial factors was assessed (Step 3). Given the novelty of this research, the significance level was set at p < 0.10 for all analyses.
Results
Characteristics of Participants
Survey participants’ average age was 20.66 (see Table 1). More than half of the sample (57.2 %) was Black/African American, and 18 % of participants were Hispanic/Latino. Approximately half of the sample had a high school education or less. The majority identified as gay. Fifteen participants reported that they had received an HIV-positive test result.
With regard to risk behavior, a small proportion had engaged in serodiscordant sexual activity in the previous 2 months or had a history of STIs. Two-thirds had not sought casual partners on the Internet in the past 2 months. A minority had a main partner. Almost half had used controlled substances in the previous 2 months. On average, participants perceived their risk of HIV to be moderate (Table 1). Information use levels were also moderate. Participants generally endorsed a positive attitude regarding HIV testing, and felt that it would be easy to find a nearby HIV testing site.
As Table 2 shows, participants’ mean core discussion network size was 2.89 people, suggesting that their networks for potentially discussing HIV/AIDS were generally small. Participants had only moderately homophilous networks, with somewhat more gender homophily than age homophily. On average, participants indicated that “some” of their friends were also MSM. There was considerable variance in tie closeness as measured by participants’ weekly contacts with network members, although participants were in frequent contact with them on average. Participants did not have highly cohesive core discussion networks: only 30 % of possible ties in networks were present on average, and an average of just 26 % of total network ties were strong. Networks were not characterized by large range, with a mean of 1.36 relationship types per participant. The most common relationship types were friends/acquaintances, best friends, and lover/boyfriend or ex-lover/boyfriend. Parents, siblings and other family members comprised 17 % of named members. Only 1 % of named members were health care providers.
Table 2.
Survey participant social network functions and characteristics (n = 194)
| Mean (SD); range | |
|---|---|
| Network size | 2.89 (2.64); 0–7 |
| Network characteristics | |
| Tie characteristics | |
| Homophily | |
| Age (E–I index) | 0.05 (0.40) −1 to +1 |
| Gender (E–I index) | 0.17 (0.54) −1 to +1 |
| Sexual orientation | 3.22 (1.11); 1–5 |
| Ego-alter tie strength (mean number of communications with each network member per week) | 92 (283.92); 0–2134 |
| Network characteristics | |
| Network structure | |
| Density | 0.32 (0.40); 0.00–1.00 |
| Strong tie proportion | 0.26 (0.37); 0.00–1.00 |
| Range | 1.32 (1.35); 0–5 |
| Network functions | |
| Social support | |
| Network-mediated social support | 2.54 (4.39); 0–14 |
| Perceived stigma | 8.66 (3.54); 4–19 |
| Social influence | |
| Descriptive testing norms | 5.71 (1.52); 2–8 |
| Injunctive testing norms | 5.89 (1.74); 2–8 |
| Resources | |
| Social information acquisition | 9.74 (3.55); 5–20 |
Includes texting
As for network functions, participants reported little perceived HIV-specific social support from their core discussion network members. On average, norms regarding HIV testing tended towards more support for HIV testing. HIV-related stigma was moderate, as was network-mediated information acquisition.
Prediction of HIV Testing Behavior
Ever had an HIV Test
Just under two-thirds (64.4 %) of participants had ever had an HIV test (Table 1). As shown in Table 3, network range was the only network characteristic that significantly predicted having had an HIV test. The significant effect for network range remained significant after network functions were added into the model, but ceased to be so once adjusted for individual-level correlates.
Table 3.
Logistic regression for ever having had an HIV Test (n = 194)
| Independent variables | Step 1: Network characteristics only |
Step 2: Network characteristics + network functions |
Step 3: Network characteristics + network functions + individual level |
Step 4: Final model | ||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio (CI) | p | Odds ratio (CI) | p | Odds ratio (CI) | p | Odds ratio (CI) | p | |
| Network level—characteristics | ||||||||
| Tie characteristics | ||||||||
| Network homophily | ||||||||
| Unadj. | 1.07 (0.79–1.45) | .65 | - | - | ||||
| Adj. | - | - | - | - | - | - | - | - |
| Ego-alter tie strength | ||||||||
| Unadj. | 0.97 (0.99–1.00) | .23 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network structure | ||||||||
| Network density | ||||||||
| Unadj. | 1.02 (0.76–1.38) | .89 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Strong tie proportion | ||||||||
| Unadj. | 0.92 (0.68–1.24) | .58 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network range | ||||||||
| Unadj. | 1.40 (1.02–1.94) | .04 | - | - | - | - | - | - |
| Adj. | 1.40 (1.02–1.94) | .04 | 1.72 (1.20–2.47) | .003 | 1.21 (0.73–2.01) | .46 | - | - |
| Network level—function | ||||||||
| Social support | ||||||||
| Social support | ||||||||
| Unadj. | - | - | 0.96 (0.72–1.29) | .78 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Perceived stigma | ||||||||
| Unadj. | - | - | 1.08 (0.80–1.47) | .62 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Social influence | ||||||||
| Descriptive testing norms | ||||||||
| Unadj. | - | - | 1.11 (0.83–1.49) | .48 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Injunctive testing norms | ||||||||
| Unadj. | - | - | .99 (0.74–1.39) | .97 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Resources | ||||||||
| Network-mediated information acquisition | ||||||||
| Unadj. | - | - | 1.57 (1.12–2.20) | .009 | - | - | - | - |
| Adj. | - | - | 1.84 (1.27–2.67 | .001 | 1.97 (1.16–3.36) | .01 | 1.76 (1.11–2.78) | .01 |
| Individual level | ||||||||
| Demographics | ||||||||
| Age | ||||||||
| Unadj. | - | - | 2.39 (1.65–3.47) | .000 | - | - | ||
| Adj. | - | - | 2.12 (1.27–3.55) | .004 | 2.38 (1.54–3.67) | .000 | ||
| Education level | ||||||||
| Unadj. | - | - | 0.32 (0.17–0.60) | .000 | - | - | ||
| Adj. | - | - | 0.71 (0.25–2.00) | .71 | - | - | ||
| Black/African American or Hispanic/Latino | ||||||||
| Unadj. | - | - | 0.59 (0.31–1.12) | .11 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Risk behavior | ||||||||
| High-risk sexual behavior | ||||||||
| Unadj. | - | - | 1.35 (0.34–5.40) | .67 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Substance use | ||||||||
| Unadj. | - | - | 2.06 (1.12–3.78) | .02 | - | - | ||
| Adj. | - | - | 2.50 (1.03–6.05) | .04 | 2.60 (1.15–5.90) | .02 | ||
| STI history | ||||||||
| Unadj. | - | - | 1.60 (1.02–2.50) | .04 | - | - | ||
| Adj. | - | - | 1.40 (0.65–3.02) | .39 | - | - | ||
| Internet use to seek casual partners | ||||||||
| Unadj. | - | - | 2.43 (1.45–4.06) | .001 | - | - | ||
| Adj. | - | - | 1.47 (0.73–2.95) | .28 | - | - | ||
| Psychosocial factors | ||||||||
| Perceived risk | ||||||||
| Unadj. | - | - | 1.57 (1.12–2.20) | .009 | - | - | ||
| Adj. | - | - | 1.11 (0.62–1.98) | .072 | - | - | ||
| Perceived behavioral control re: testing | ||||||||
| Unadj. | - | - | 2.85 (1.92–4.23) | .000 | - | - | ||
| Adj. | - | - | 2.75 (1.67–4.53) | .000 | 3.32 (2.04–5.42) | .001 | ||
| Attitude to testing | ||||||||
| Unadj. | - | - | 1.34 (0.99–1.83) | .06 | - | - | ||
| Adj. | - | - | 1.40 (0.91–2.15) | .13 | - | - | ||
| Information use | ||||||||
| Unadj. | - | - | 1.11 (0.83–1.49) | .48 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Nagelkerke R2 | 0.03 | 0.13 | 0.48 | 0.45 | ||||
Bold values indicate statistical significance (p < 0.10)
As for network functions, only network-mediated information acquisition predicted having had an HIV test. This relationship remained significant after adjusting for network range. Information acquisition was significant in the final model; people who reported more acquisition of HIV/AIDS-related information from others were 1.76 times more likely to have had an HIV test than those who had not (OR = 1.76, p = 0.02).
As Table 3 shows, older YMSM were more likely to have had an HIV test. Perceived behavioral control had the strongest significant association with HIV testing: men with higher perceived control were 3.32 times more likely to have had a test than men who did not (OR = 3.32, p <.001). Drug use was also a significant predictor, with men who reported using controlled substances in the past 2 months being 2.60 times more likely to have had an HIV test, although the confidence interval for this coefficient was wide (OR = 2.60, p = 0.02).
Thirteen percent of the variance in having ever had an HIV test was explained prior to adjustment for individual factors (Table 3). However, there was a 35 % increase in variance explained with the addition of individual factors. Thus, network-level related variables had much weaker predictive power than individual-level variables. Overall, the model explained a moderate amount of variance in whether participants had ever had an HIV test (Nagelkerke R2 = 0.45).
Repeat Testing
Ninety (53.6 %) participants had been tested more than once, and received their test results each time they were tested (Table 1). Of those participants, 41 (45.6 %) stated that the reason for their last test was that they “get tested regularly”.
As shown in Table 4, there were no network characteristics that significantly predicted repeat testing on either unadjusted or adjusted bases. Furthermore, network-mediated information acquisition was the only network function variable that significantly predicted repeat testing; this variable remained significant in the final model. Those who received more HIV-related information from others were 1.64 times more likely to have more than one HIV test (OR = 1.64, p = 0.01).
Table 4.
Logistic regression for repeat testing (n = 179)
| Independent variables | Step 1: Network characteristics only |
Step 2: Network characteristics + network functions |
Step 3: Network characteristics + network functions + individual level |
Step 4: Final model | ||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio (CI) | p | Odds ratio (CI) | p | Odds ratio (CI) | p | Odds ratio (CI) | p | |
| Network level-characteristics | ||||||||
| Tie characteristics | ||||||||
| Network homophily | ||||||||
| Unadj. | 1.05 (0.79–1.41) | .73 | - | - | ||||
| Adj. | - | - | - | - | - | - | - | - |
| Ego-alter tie strength | ||||||||
| Unadj. | 1.00 (0.99–1.00) | .31 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network structure | ||||||||
| Network density | ||||||||
| Unadj. | 1.07 (0.78–1.43) | .67 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Strong tie proportion | ||||||||
| Unadj. | 0.97 (0.72–1.30) | .82 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network range | ||||||||
| Unadj. | 1.21 (0.90–1.63) | .21 | - | - | - | - | - | |
| Adj. | - | - | - | - | - | - | - | - |
| Network level—function | ||||||||
| Social support | ||||||||
| Social support | ||||||||
| Unadj. | - | - | 0.92 (0.68–1.23) | .56 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Perceived stigma | ||||||||
| Unadj. | - | - | 0.90 (0.67–1.20) | .46 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Social Influence | ||||||||
| Descriptive testing norms | ||||||||
| Unadj. | - | - | 1.21 (0.90–1.63) | .22 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Injunctive testing norms | ||||||||
| Unadj. | - | - | 1.09 (0.80–1.47) | .60 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Resources | ||||||||
| Network-mediated information acquisition | ||||||||
| Unadj. | - | - | 1.67 (1.21–2.30) | .002 | - | - | - | - |
| Adj. | - | - | 1.67 (1.21–2.30) | .002 | 1.74 (1.18–2.58) | .006 | 1.64 (1.14–2.36) | .008 |
| Individual level | ||||||||
| Demographics | ||||||||
| Age | ||||||||
| Unadj. | - | - | 1.49 (1.06–1.95) | .02 | - | - | ||
| Adj. | - | - | 1.19 (0.80–1.77) | .38 | - | - | ||
| Education level | ||||||||
| Unadj. | - | - | 0.45 (0.24–0.82) | .009 | - | - | ||
| Adj. | - | - | 0.65 (0.29–1.46) | .30 | - | - | ||
| Black/African American or Hispanic/Latino | ||||||||
| Unadj. | - | - | 0.79 (0.27–2.32) | .67 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Risk behavior | ||||||||
| High-risk sexual behavior | ||||||||
| Unadj. | - | - | 0.92 (0.28–3.01) | .89 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Drug use | ||||||||
| Unadj. | - | - | 1.63 (0.90–2.96) | .11 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| STI history | ||||||||
| Unadj. | - | - | 1.11 (0.82–1.51) | .51 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Internet use to seek casual partners | ||||||||
| Unadj. | - | - | 1.51 (1.08–2.11) | .02 | - | - | ||
| Adj. | - | - | 1.50 (0.93–2.41) | 0.09 | 1.72 (1.14–2.61) | .01 | ||
| Psychosocial factors | ||||||||
| Perceived risk | ||||||||
| Unadj. | - | - | 1.32 (0.98–1.93) | .07 | - | - | ||
| Adj. | - | - | 1.13 (0.71–1.80) | .60 | - | - | ||
| Perceived behavioral control re: testing | ||||||||
| Unadj. | - | - | 2.40 (1.61–3.57) | <.001 | - | - | ||
| Adj. | - | - | 2.10 (1.34–3.30) | .001 | 2.46 (1.60–3.78) | <.001 | ||
| Attitude to testing | ||||||||
| Unadj. | - | - | 1.44 (1.03–1.99) | .03 | - | - | ||
| Adj. | - | - | 1.28 (0.88–1.85) | .20 | - | - | ||
| Information use | ||||||||
| Unadj. | - | - | 1.26 (0.94–1.70) | .13 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Nagelkerke R2 | 0.00 | 0.08 | 0.30 | 0.28 | ||||
Bold values indicate statistical significance (p < 0.10)
At an individual level, perceived behavioral control was a significant predictor of repeat testing on an adjusted basis. Specifically, those with greater perceived behavioral control were 2.46 times more likely to have obtained testing more than once (OR = 2.46, p < 0.001). Those who were older were more likely to have tested more than once; however, these effects disappeared for age in the adjusted model. Similarly, a significant negative association between education and repeat testing disappeared when other variables were taken into account. In the final model, participants who sought casual partners on the Internet were 1.72 times more likely to have an HIV test more than once (OR = 1.72, p = 0.01).
As in the previous model, a network-related variable predicted repeat testing independent of individual-level correlates. The magnitude of this influence was moderate, however: a network function predicted 8 % of the variance in repeat HIV testing, with individual-level variables adding 22 % to the predictive power of the model. The final model predicted a moderate amount of variance in the likelihood of repeat testing (Nagelkerke R2 = 0.28).
Last Test was in the Past 12 Months
Under half (43.8 %) of participants had their last HIV test in the previous 12 months (Table 1). Table 5 demonstrates that network homophily predicted recent HIV testing on both an unadjusted and adjusted basis. In the final model, people with more homophilous networks were 2.10 times more likely to have had a test in the past 12 months (OR = 2.10, p = 0.02). Other network characteristics were not significant.
Table 5.
Logistic regression for last test in past 12 months (n = 179)
| Independent variables | Step 1: Network characteristics only |
Step 2: Network characteristics + network functions |
Step 3: Network characteristics + network functions + individual level |
Step 4: Final model | ||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio (CI) | p | Odds ratio (CI) | p | Odds ratio (CI) | p | Odds ratio (CI) | p | |
| Network level—characteristics | ||||||||
| Tie characteristics | ||||||||
| Network homophily | ||||||||
| Unadj. | 1.65 (0.99–2.75) | .05 | - | - | ||||
| Adj. | 1.65 (0.99–2.75) | .05 | 2.08 (1.12–3.86) | .02 | 2.18 (1.13–4.23) | .02 | 2.10 (1.11–3.94) | .02 |
| Ego-alter tie strength | ||||||||
| Unadj. | 0.49 (0.18–1.33) | .16 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network structure | ||||||||
| Network density | ||||||||
| Unadj. | 0.81 (0.52–1.26) | .36 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Strong tie proportion | ||||||||
| Unadj. | 0.95 (0.59–1.52) | .82 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network range | ||||||||
| Unadj. | 0.76 (0.51–1.13) | .18 | - | - | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Network level—function | ||||||||
| Social support | ||||||||
| Social support | ||||||||
| Unadj. | - | - | 0.81 (0.51–1.29) | .38 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Perceived stigma | ||||||||
| Unadj. | - | - | 0.55 (0.35–0.87) | .011 | - | - | - | - |
| Adj. | - | - | 0.45 (0.26–0.79) | .006 | 0.50 (0.27–0.94) | .03 | 0.44 (0.25–0.77) | .005 |
| Social influence | ||||||||
| Descriptive testing norms | ||||||||
| Unadj. | - | - | 1.74 (1.09–2.79) | .02 | - | - | - | - |
| Adj. | - | - | 0.75 (0.37–1.55) | .44 | - | - | - | - |
| Injunctive testing norms | ||||||||
| Unadj. | - | - | 1.75 (1.11–2.74) | .02 | - | - | - | - |
| Adj. | - | - | 2.26 (1.09–4.67) | .03 | 1.23 (0.61–2.47) | .56 | - | - |
| Resources | ||||||||
| Network-mediated information acquisition | ||||||||
| Unadj. | - | - | 1.25 (0.80–1.94) | .32 | - | - | - | - |
| Adj. | - | - | - | - | - | - | - | - |
| Individual level | ||||||||
| Demographics | ||||||||
| Age | ||||||||
| Unadj. | - | - | 0.56 (0.36–0.87) | .01 | - | - | ||
| Adj. | - | - | 0.54 (0.28–1.03) | .06 | 0.43 (0.25–0.76) | .003 | ||
| Education level | ||||||||
| Unadj. | - | - | 2.38 (0.95–6.01) | .07 | - | - | ||
| Adj. | - | - | 2.04 (0.52–8.11) | .31 | - | - | ||
| Black/African American or Hispanic/Latino | ||||||||
| Unadj. | - | - | 3.60 (1.47–8.82) | .005 | - | - | ||
| Adj. | - | - | 1.69 (0.12–24.67) | .70 | - | - | ||
| Risk behavior | ||||||||
| High-risk sexual behavior | ||||||||
| Unadj. | - | - | 0.71 (0.16–3.22) | .65 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Substance use | ||||||||
| Unadj. | - | - | 0.58 (0.23–1.43) | .24 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| STI history | ||||||||
| Unadj. | - | - | 0.65 (0.45–0.94) | .02 | - | - | ||
| Adj. | - | - | 0.94 (0.59–1.50) | .79 | - | - | ||
| Internet use to seek casual partners | ||||||||
| Unadj. | - | - | 0.64 (0.45–0.91) | .01 | - | - | ||
| Adj. | - | - | 0.72 (0.40–1.28) | .26 | - | - | ||
| Psychosocial factors | ||||||||
| Perceived risk | ||||||||
| Unadj. | - | - | 0.74 (0.50–1.12) | .16 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Perceived behavioral control re: testing | ||||||||
| Unadj. | - | - | 1.55 (0.87–2.77) | .14 | - | - | ||
| Adj. | - | - | - | - | - | - | ||
| Attitude to testing | ||||||||
| Unadj. | - | - | 2.54 (1.23–5.24) | .01 | - | - | ||
| Adj. | - | - | 2.53 (0.98–6.49) | .05 | 2.44 (1.03–5.78) | .04 | ||
| Information use | ||||||||
| Unadj. | - | - | 1.53 (0.99–2.39) | .06 | - | - | ||
| Adj. | - | - | 1.72 (0.90–3.29) | .10 | - | - | ||
| Nagelkerke R2 | 0.06 | 0.26 | 0.45 | 0.37 | ||||
Bold values indicate statistical significance (p < 0.10)
Both social support and social influence-related network functions were predictive of recent testing. Specifically, greater perceived stigma was associated with a reduced likelihood of recent HIV testing on both unadjusted and adjusted bases, with those who perceived greater stigma being 56 % less likely to have had an HIV test in the prior 12 months. However, direct social support was not significantly predictive. Furthermore, both descriptive and injunctive norms significantly predicted a recent HIV test on a bivariate basis, although only injunctive norms remained significant after adjustment for network characteristics (2.23 times higher likelihood with more testing-supportive injunctive norms) (OR = 2.23, p = 0.03). However, this variable was no longer significant after adjustment for individual-level predictors.
The individual-level variables that were most predictive of recent HIV testing were age—younger men were more likely to have had a recent test—and attitudes toward testing. Those men who had more positive attitudes toward testing, i.e., that HIV testing is “the responsible thing to do”, were 2.44 times more likely to have had a recent HIV test (OR = 2.44, p = 0.04).
Other variables that significantly increased the odds of recent testing on an unadjusted basis were Black/African American or Hispanic/Latino identity and greater information use. Additionally, STI history and Internet use to seek casual partners significantly reduced the likelihood of testing in the past 12 months on an unadjusted, but not adjusted, basis.
Notably, network structure and function predicted HIV testing behavior independent of individual-level correlates. The magnitude of this influence was relatively high: network structure and function predicted 26 % of the variance in recent HIV testing, with individual-level variables adding only 19 % to the predictive power of the model. Therefore, network-related variables had stronger predictive power than individual-level variables. The final model predicted a moderate amount of variance in the likelihood of having had an HIV test in the previous 12 months (Nagelkerke R2 = 0.37).
Discussion
We explored the potential influence of a range of network-related and individual-level variables on HIV testing behavior. In a series of steps, we investigated predictors at network structure, function and individual levels for three HIV testing behaviors [ever had an HIV test, repeat testing and HIV testing in the previous 12 months (recent testing)]. One network characteristic (either tie characteristics or network structure) variable was predictive of the outcomes in two of the models. However only network homophily was significantly predictive of an outcome (recent testing) after adjustment for both network functions and individual characteristics. Network functions such as network-mediated information acquisition and perceived stigma were also significant in all three models; in each model, at least one variable remained significant after adjustment for both network characteristics and individual-level factors. Individual-level variables were predictive in all models, but the effects were strongest for ever having had an HIV test and repeat testing. In those models, age, perceived behavioral control, and positive attitudes were the most predictive variables. Overall, network structure (e.g., homophily and network range) and function (e.g., network-mediated information acquisition and perceived stigma) predicted 13, 8 and 26 % of the variance in the ever tested, repeat testing, and recent HIV testing models, respectively. In other words, networks predicted a non-negligible amount of the variance in all of the HIV testing behavior models.
A notable finding of this research lies in the fact that network-related variables predicted HIV testing independent of individual-level correlates in all three models tested. Moreover, the magnitude of the influence of network-related variables was greatest in the recent testing model: they actually predicted a larger proportion of the variance in recent testing than individual-level variables. This suggests the value of multi-level interventions that incorporate network intervention strategies and outcomes in HIV testing interventions among YMSM. Additionally, it is notable that different predictors were relevant for each aspect of HIV testing behavior; accordingly, different network intervention strategies may be needed for promoting testing in general versus regular or recent testing.
Network homophily and range significantly predicted HIV testing-related behavior on an unadjusted basis. However, only homophily remained significant after adjustment for individual factors. Theory suggests that mechanisms through which homophily may affect behavior include shared attitudes, behavioral self-evaluations and mimicry [32, 99–102]. These possibilities should be tested in future research. For example, as done in Chinese research, researchers should investigate behavioral cascades by examining the timing of network members’ HIV testing or HIV prevention activities as predictors of participants’ own testing behavior [12]. Although further research is needed, study findings nevertheless confirm the value of peer-based interventions for HIV testing.
We identified network range (relationship type diversity) as a predictor of HIV testing behavior, although this variable was no longer a significant predictor of ever having had an HIV test after individual-level variables were entered into the model. Along with findings regarding the importance of network-mediated information acquisition for both ever testing and repeat testing, this may align with theory suggesting that network range increases access to more resources, such as information and referrals [28]. Furthermore, research outside of the health field shows that information is a resource more easily acquired with greater network range, since it accords access to more diverse or potentially more valuable pools of knowledge [103–105]. These results offer the intriguing possibility that network diversification could be a network alteration intervention strategy to promote HIV testing [106].
We found that tie strength between participants and their network members was not a significant predictor of HIV testing. This is an unexpected finding in light of research showing that that strong ties influence HIV risk behavior among MSM [41]. Research with non-MSM samples of adolescents has shown that the sexual behavior of a youth’s “best friends” is associated with his or her own sexual behavior [107, 108]. There is also ample literature that shows that substance use among young people’s stronger ties is linked to their own substance use [43, 109, 110]. However, among MSM, stronger ties have also been found to moderate the effect of norms on HIV risk behavior [41] rather than having an indirect effect. While the sample size in this study did not permit such analyses, future researchers should examine the potential of moderating as well as direct effects for this variable. Additionally, although there was a great deal of variation in responses to this variable, it is possible that our focus on core discussion networks meant that named network members did not include weaker ties with whom participants spoke very rarely. If such people were included in the networks, tie strength may have been a significant predictor. To investigate this potential, future research should deliberately elicit information about both stronger and weaker ties of YMSM. Furthermore, our study differs from prior research in its consideration of multiple measures of network cohesion. Nevertheless, we did not find a relationship between network cohesion and HIV testing behavior.
Researchers have previously identified the fact that stigma can be a barrier to timely HIV testing [18, 60, 111, 112]. Similarly, we found that stigma in the context of help-seeking was a significant negative predictor of recent HIV testing. This suggests that stigma reduction strategies may be an important step towards meeting national HIV testing guidelines among MSM.
Contrary to research findings in multiple health domains that show a positive association between social support and health-enhancing behaviors [28], social support did not significantly predict HIV testing behavior. It may be that our measure of HIV-specific social support did not capture the full range of testing-relevant supportive behaviors. Future researchers are entreated to use more multidimensional measures of these constructs. Furthermore, greater variance in support measures might be captured if researchers include weaker ties in future investigations.
Results reported here revealed a relatively minor role for norms in HIV testing behavior. Although injunctive norms predicted testing in the past 12 months on an unadjusted basis, these significant relationships vanished after entering other network variables and/or individual-level variables into the model. In contrast with our findings, recent Scottish research showed that MSM who perceived strong descriptive norms in favor of HIV testing were more likely to have had a recent HIV test [10]. Furthermore, a recent study of non-MSM Mexican–American men demonstrated that descriptive norms regarding testing were associated with a stronger intention to have an HIV test [113, 114]. In the present research, however, we included network-mediated information acquisition, a variable that was a significant predictor in the final models for ever having had an HIV test and for repeat testing. Since norms might be thought of as a form of information, it is possible that norm communication was encompassed in this measure. The contribution of network-mediated information to HIV testing confirms the value of induction-based network interventions [106] that focus on prompting information sharing; such approaches are now common in HIV prevention.
The attitude that HIV testing “is the responsible thing to do” significantly predicted recent HIV testing. This has resonance with other HIV research that showed that partner protection can be a motivator for engaging in sexual risk reduction and/or HIV testing [26, 115]. In other research, MSM with both main and non-main male partners had higher rates of testing than those who had only non-main male partners [17]. This finding suggests the value of HIV testing interventions that focus on this sense of personal responsibility, although such messages should be carefully contextualized so as to avoid unintentional reinforcement of HIV stigma.
Perceived behavioral control was a significant predictor of both having ever had an HIV test and repeat testing. Indeed, this variable had the strongest association with both behaviors. However, due to the cross-sectional nature of this study, it is impossible to identify whether this perceived control preceded, or resulted from, HIV testing. Order effects seem particularly important in this case given that the ability to identify an HIV testing location nearby should be linked to having had a test in that location. Future research of a longitudinal nature should investigate these relationships.
We found that risk behavior had an inconsistent relationship with HIV testing behavior. While serodiscordant sexual activity was not a significant predictor of HIV testing behavior, casual partner-seeking on the Internet was associated with repeat testing. This research therefore finds partial resonance with prior research showing an unclear or negative relationship between risk behavior and testing [10, 12, 23, 116]. Additionally, this study showed an association between drug use and having ever had an HIV test. Such an association may have emerged because HIV testing is often recommended as part of addiction treatment programs; future work should investigate this context for testing among YMSM. Like others, we found that individual MSM’s perceptions of risk were positively associated with HIV testing [6, 15, 18, 23, 24], although this variable was not significant in any of the final models. Accordingly, there is tentative evidence that assisting YMSM in developing risk perceptions that align with federal HIV testing guidelines may provide an opportunity for HIV testing promotion.
Results of the study should be interpreted in light of several limitations. First, the study was cross-sectional, and thus it is impossible to determine order effects; for example, perceived behavioral control and attitudes could have emerged as a consequence of HIV testing rather than the reverse. Additionally, the study’s participants were recruited in part through health clinics, ASOs and health departments; YMSM recruited from these sites may have been more likely to have had an HIV test than the general population of MSM. Participants recruited at LGBT or ASOs in the area, as well as those from local bars/clubs, and online venues may have also been more connected to other YMSM than YMSM in general. Such factors may also make participants more likely to obtain testing, suggesting a potential bias in the sample towards YMSM who are likely to seek HIV testing. Furthermore, we focused the study on core discussion networks in the context of this research while creating several measures that could capture network functions not confined to core discussion network members (e.g., perceived stigma). However, given that the spread of some health behaviors (e.g., obesity [32]) are best understood at the whole network level, this research is limited in its focus on egocentric networks. In addition, our measure of tie strength was based on communication frequency. Although we felt that this approach to measurement was appropriate due to our focus on core discussion networks, some literature has argued instead that tie closeness should instead be measured as one’s subjective feelings of closeness to a network member (e.g., [40]); furthermore, this measure has not previously been used in research with MSM. Additional research is needed to determine the most appropriate measures of tie strength for MSM, and in the context of different network types. Finally, since the survey was conducted in spring 2011, HIV testing was not yet available through home testing means. Accordingly, the applicability of these findings to home testing is unknown.
Conclusions
Results of this study highlight the potential for multi-level interventions to promote HIV testing, including efforts focused on social networks. Network characteristics and functions significantly predicted three HIV testing behaviors over and above individual-level characteristics, with network variables including homophily and stigma being even more predictive than individual-level factors for recent testing. However, the relative importance of each varied by testing behavior, with individual-level factors proving more important for ever testing and repeat testing. Future research should investigate the dynamics of, and differences between, these three HIV behaviors—particularly from a network perspective. There is a significant need for novel, multi-level strategies to encourage YMSM to have their first HIV test, and to keep coming back at regular intervals.
Acknowledgments
This project was funded by the National Institutes of Health, National Center for Research Resources, Grant UL1RR024986. Dr. Bauermeister is supported by a Career Development K01 (K01-MH087242) from the National Institutes of Mental Health.
References
- 1.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas. HIV Surveillance Report. 2011:23. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men—United States. MMWR. 2013;62(47):958–962. [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. Healthy people 2020. Washington, DC: Office of Disease Prevention and Health Promotion; 2011. [Google Scholar]
- 4.Workowski KA, Berman S. Sexually transmitted diseases treatment guidelines, 2010. MMWR. 2010;59(Rr-12):1–110. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV testing among men who have sex with men—21 Cities, United States, 2008. MMWR. 2011;60(21):694–699. [PubMed] [Google Scholar]
- 6.Kellerman SE, Lehman JS, Lansky A, et al. HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. J Acquir Immune Defic Syndr. 2002;31(2):202–210. doi: 10.1097/00126334-200210010-00011. [DOI] [PubMed] [Google Scholar]
- 7.Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: the social networks demonstration project. Am J Public Health. 2009;99(6):1093–1099. doi: 10.2105/AJPH.2008.139329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amirkhanian YA. Social networks, sexual networks and HIV risk in men who have sex with men. Curr HIV/AIDS Rep. 2014;11(1):81–92. doi: 10.1007/s11904-013-0194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hickson F, Tomlin K, Hargreaves J, Bonell C, Reid D, Weatherburn P. Internet-based cohort study of HIV testing over 1 year among men who have sex with men living in England and exposed to a social marketing intervention promoting testing. Sex Transm Infect. 2014;91(1):24–30. doi: 10.1136/sextrans-2014-051598. [DOI] [PubMed] [Google Scholar]
- 10.Knussen C, Flowers P, McDaid LM. Factors associated with recency of HIV testing amongst men residing in Scotland who have sex with men. AIDS Care. 2014;26(3):297–303. doi: 10.1080/09540121.2013.824543. [DOI] [PubMed] [Google Scholar]
- 11.Scott H, Pollack L, Rebchook G, Huebner D, Peterson J, Kegeles S. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS Behav. 2014;18(5):913–920. doi: 10.1007/s10461-013-0608-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hao C, Lau JT, Zhao X, Yang H, Huan X, Yan H, et al. Associations between perceived characteristics of the peer social network involving significant others and risk of HIV transmission among men who have sex with men in China. AIDS Behav. 2014;18(1):99–110. doi: 10.1007/s10461-013-0492-2. [DOI] [PubMed] [Google Scholar]
- 13.Hussen SA, Stephenson R, del Rio C, Wilton L, Wallace J, Wheeler D. HIV testing patterns among black men who have sex with men: a qualitative typology. PLoS ONE. 2013;8(9):e75382. doi: 10.1371/journal.pone.0075382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkerson JM, Fuchs EL, Brady SS, Jones-Webb R, Rosser BR. Correlates of human immunodeficiency virus/sexually transmitted infection (HIV/STI) testing and disclosure among HIV-negative collegiate men who have sex with men. J Am Coll Health. 2014;62(7):450–460. doi: 10.1080/07448481.2014.917654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackellar DA, Hou SI, Whalen CC, et al. Reasons for not HIV testing, testing intentions, and potential use of an over-the-counter rapid HIV test in an internet sample of men who have sex with men who have never tested for HIV. Sex Transm Dis. 2011;38(5):419–428. doi: 10.1097/OLQ.0b013e31820369dd. [DOI] [PubMed] [Google Scholar]
- 16.Reisen CA, Zea MC, Bianchi FT, et al. HIV testing among MSM in Bogota, Colombia: the role of structural and individual characteristics. AIDS Educ Prev. 2014;26(4):328–344. doi: 10.1521/aeap.2014.26.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mashburn AJ, Peterson JL, Bakeman R, Miller RL, Clark LF. Influences on HIV testing among young African-American men who have sex with men and the moderating effect of the geographic setting. J Commun Psychol. 2004;32(1):45–60. [Google Scholar]
- 18.Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDS. 2013;27(11):621–627. doi: 10.1089/apc.2013.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holt M, Hull P, Lea T, et al. Comprehensive testing for, and diagnosis of, sexually transmissible infections among Australian gay and bisexual men: findings from repeated, cross-sectional behavioural surveillance, 2003–2012. Sex Transm Infect. 2014;90(3):208–215. doi: 10.1136/sextrans-2013-051294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Washington TA, Robles G, Malotte K. Factors associated with HIV-Testing history among black men who have sex with men (BMSM) in Los Angeles County. Behav Med. 2013;39(3):52–59. doi: 10.1080/08964289.2013.779565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nelson KM, Thiede H, Jenkins RA, Carey JW, Hutcheson R, Golden MR. Personal and contextual factors related to delayed HIV diagnosis among men who have sex with men. AIDS Educ Prev. 2014;26(2):122–133. doi: 10.1521/aeap.2014.26.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mimiaga MJ, Reisner SL, Bland S, et al. Health system and personal barriers resulting in decreased utilization of HIV and STD testing services among at-risk black men who have sex with men in Massachusetts. AIDS Patient Care STDS. 2009;23(10):825–835. doi: 10.1089/apc.2009.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang ZJ, He N, Nehl EJ, et al. Social network and other correlates of HIV testing: findings from male sex workers and other MSM in Shanghai, China. AIDS Behav. 2012;16(4):858–871. doi: 10.1007/s10461-011-0119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell JW, Petroll AE. Patterns of HIV and sexually transmitted infection testing among men who have sex with men couples in the United States. Sex Transm Dis. 2012;39(11):871–876. doi: 10.1097/OLQ.0b013e3182649135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meadowbrooke CC, Veinot TC, Loveluck J, Hickok A, Bauermeister JA. Information behavior and HIV testing intentions among young men at risk for HIV/AIDS. J Assoc Inf Sci Technol. 2014;65(3):609–620. doi: 10.1002/asi.23001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bell D, Atkinson J, Mosier V, Riley M, Brown V. The HIV transmission gradient: relationship patterns of protection. AIDS Behav. 2007;11(6):789–811. doi: 10.1007/s10461-006-9192-5. [DOI] [PubMed] [Google Scholar]
- 27.Wasserman S, Faust K. Social network analysis: methods and applications. Cambridge: Cambridge University Press; 1994. p. xxxi. 825. [Google Scholar]
- 28.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 29.McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annu Rev Sociol. 2001;27:415. [Google Scholar]
- 30.Centola D. An experimental study of homophily in the adoption of health behavior. Science. 2011;334(6060):1269–1272. doi: 10.1126/science.1207055. [DOI] [PubMed] [Google Scholar]
- 31.Valente TW. Social networks and health: models, methods, and applications. Oxford; New York: Oxford University Press; 2010. p. xiv. 277. [Google Scholar]
- 32.Christakis NA, Fowler JH. Connected: the surprising power of our social networks and how they shape our lives. New York: Little, Brown and Co./Hachette Book Group; 2009. p. xiii. 338. [Google Scholar]
- 33.Brechwald WA, Prinstein MJ. Beyond homophily: a decade of advances in understanding peer influence processes. J Res Adolesc. 2011;21(1):166–179. doi: 10.1111/j.1532-7795.2010.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wagner GJ, Hoover M, Green H, Tohme J, Mokhbat J. Social, relational and network determinants of unprotected anal sex and HIV testing among men who have sex with men in Beirut, Lebanon. Int J Sex Health. 2015;27(3):264–275. doi: 10.1080/19317611.2014.969467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cialdini RB. Influence: science and practice. Harlow: Pearson Education; 2009. p. xii. 260. [Google Scholar]
- 36.Shang J, Croson R. A field experiment in charitable contribution: the impact of social information on the voluntary provision of public goods. Econ J. 2009;119(540):1422–1439. [Google Scholar]
- 37.Granovetter MS. The strength of weak ties. AJS. 1973;78(6):1360–1380. [Google Scholar]
- 38.Arnaboldi V, Guazzini A, Passarella A. Egocentric online social networks: analysis of key features and prediction of tie strength in Facebook. Comput Commun. 2013;36(10–11):1130–1144. [Google Scholar]
- 39.Gilbert E, Karahalios K, Sandvig C. The network in the garden: an empirical analysis of social media in rural life; Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; Florence, Italy. 2008. pp. 1603–1612. 1357304: ACM. [Google Scholar]
- 40.Marsden PV, Campbell KE. Measuring tie strength. Soc Forces. 1984;63(2):482–501. [Google Scholar]
- 41.Choi KH, Ayala G, Paul J, Boylan R, Gregorich SE. Social network characteristics and HIV risk among African American, Asian/Pacific Islander, and Latino men who have sex with men. J Acquir Immune Defic Syndr. 2013;64(5):496–501. doi: 10.1097/QAI.0b013e3182a7ee52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haynie DL. Delinquent peers revisited: does network structure matter? AJS. 2001;106(4):1013–1057. [Google Scholar]
- 43.Cook SH, Bauermeister JA, Gordon-Messer D, Zimmerman MA. Online network influences on emerging adults’ alcohol and drug use. J Youth Adolesc. 2013;42(11):1674–1686. doi: 10.1007/s10964-012-9869-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Valente TW. Network models of the diffusion of innovations. Cresskill: Hampton Press; 1995. p. xv. 171. [Google Scholar]
- 45.Centola D. The spread of behavior in an online social network experiment. Science. 2010;329(5996):1194–1197. doi: 10.1126/science.1185231. [DOI] [PubMed] [Google Scholar]
- 46.Alonzo AA, Reynolds NR. Stigma, HIV and AIDS: an exploration and elaboration of a stigma trajectory. Soc Sci Med. 1995;41(3):303–315. doi: 10.1016/0277-9536(94)00384-6. [DOI] [PubMed] [Google Scholar]
- 47.Friedkin NE. Social cohesion. Ann Rev of Sociol. 2004;30:409–425. [Google Scholar]
- 48.Rogers EM. Diffusion of innovations. 5th. New York: Free Press; 2003. [Google Scholar]
- 49.Monge PR, Contractor NS. Theories of communication networks. Oxford: Oxford University Press; 2003. p. xxi. 406. [Google Scholar]
- 50.Friedkin NE. Horizons of observability and limits of informal control in organizations. Soc Forces. 1983;62(1):54–77. [Google Scholar]
- 51.Festinger L, Schacter S, Back KW. Social pressures in informal groups. Stanford: Stanford University Press; 1950. [Google Scholar]
- 52.Burt RS. Structural holes: the social structure of competition. Cambridge: Harvard University Press; 1992. [Google Scholar]
- 53.Lauby JL, Marks G, Bingham T, et al. Having supportive social relationships is associated with reduced risk of unrecognized HIV infection among black and Latino men who have sex with men. AIDS Behav. 2012;16(3):508–515. doi: 10.1007/s10461-011-0002-3. [DOI] [PubMed] [Google Scholar]
- 54.White K, Rudolph AE, Jones KC, et al. Social and individual risk determinants of HIV testing practices among noninjection drug users at high risk for HIV/AIDS. AIDS Care. 2013;25(2):230–238. doi: 10.1080/09540121.2012.701269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jumbe CAD. The role of social networks in the decision to test for HIV. Toronto: University of Toronto; 2011. [Google Scholar]
- 56.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 57.Galvan FH, Davis EM, Banks D, Bing EG. HIV stigma and social support among African Americans. AIDS Patient Care STDS. 2008;22(5):423–436. doi: 10.1089/apc.2007.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Takada S, Weiser SD, Kumbakumba E, et al. The dynamic relationship between social support and HIV-related stigma in rural Uganda. Ann Behav Med. 2014;48(1):26–37. doi: 10.1007/s12160-013-9576-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one’s HIV-positive status, stigma and social support. AIDS Care. 2008;20(10):1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 60.Levy M, Wilton L, Phillips G, et al. Understanding Structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014;18(5):972–996. doi: 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Awad GH, Sagrestano LM, Kittleson MJ, Sarvela PD. Development of a measure of barriers to HIV testing among individuals at high risk. AIDS Educ Prev. 2004;16(2):115–125. doi: 10.1521/aeap.16.2.115.29397. [DOI] [PubMed] [Google Scholar]
- 62.Lapinski MK, Rimal RN. An explication of social norms. Commun Theory. 2005;15(2):127–147. [Google Scholar]
- 63.Friedkin NE. Norm formation in social influence networks. Soc Netw. 2001;23(3):167–189. [Google Scholar]
- 64.van den Boom W, Stolte IG, Roggen A, Sandfort T, Prins M, Davidovich U. Is anyone around me using condoms? site-specific condom-use norms and their potential impact on condomless sex across various gay venues and websites in the Netherlands. Health Psychol. 2015;34(8):857–864. doi: 10.1037/hea0000230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rivis A, Sheeran P. Descriptive norms as an additional predictor in the theory of planned behaviour: a meta-analysis. Curr Psychol. 2003;22(3):218–233. [Google Scholar]
- 66.Latkin C, Weeks MR, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS Behav. 2010;14(Suppl 2):222–238. doi: 10.1007/s10461-010-9804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fox S. The social life of health information. Washington, DC: Pew Internet & American Life Project; 2011. [April 30, 2012] http://pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx. [Google Scholar]
- 68.Livneh H, Martz E. An introduction to coping theory and research. In: Martz E, Livneh H, Wright BA, editors. Coping with chronic illness and disability. New York: Springer; 2007. pp. 3–27. [Google Scholar]
- 69.Endler NS, Parker JDA. Assessment of multidimensional coping: task, emotion and avoidance strategies. Psychol Assess. 1994;6:50–60. [Google Scholar]
- 70.Farber EW, Mirsalimi H, Williams KA, McDaniel JS. Meaning of illness and psychological adjustment to HIV/AIDS. Psycho-somatics. 2003;44(6):485–491. doi: 10.1176/appi.psy.44.6.485. [DOI] [PubMed] [Google Scholar]
- 71.Folkman S. Coping across the life span: theoretical issues. In: Cummings EM, Greene AL, Karraker KH, editors. Life-span developmental psychology: perspectives on stress and coping. Hillsdale: Lawrence Erlbaum; 1991. pp. 3–19. [Google Scholar]
- 72.Stanton AL, Revenson TA, Tennen H. Health psychology: psychological adjustment to chronic disease. Annu Rev Psychol. 2007;58:565–592. doi: 10.1146/annurev.psych.58.110405.085615. [DOI] [PubMed] [Google Scholar]
- 73.Schaefer C, Coyne JC, Lazarus RS. The health-related functions of social support. J Behav Med. 1981;4(4):381–406. doi: 10.1007/BF00846149. [DOI] [PubMed] [Google Scholar]
- 74.Siegel K, Krauss BJ. Living with HIV: adaptive tasks of seropositive gay men. J Health Soc Behav. 1991;32(1):17–32. [PubMed] [Google Scholar]
- 75.Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216–269. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- 76.Veinot TC, Meadowbrooke CC, Loveluck J, Hickok A, Bauermeister JA. How “community” matters for how people interact with information: mixed methods study of young men who have sex with other men. J Med Internet Res. 2013;15(2):e33. doi: 10.2196/jmir.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Marsden PV. Core discussion networks of Americans. Am Sociol Rev. 1987;52(1):122–131. [Google Scholar]
- 78.McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: changes in core discussion networks over two decades. Am Sociol Rev. 2006;71(3):353–375. [Google Scholar]
- 79.Couper M. Designing effective web surveys. Cambridge: Cambridge University Press; 2008. p. xvii. 398. [Google Scholar]
- 80.Bauermeister J, Pingel E, Zimmerman M, Couper M, Carballo-Dieguez A, Strecher VJ. Data quality in web-based HIV/AIDS research: handling invalid and suspicious data. Field Methods. 2012;24(3):272–291. doi: 10.1177/1525822X12443097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Young SD, Shoptaw S, Weiss RE, Munjas B, Gorbach PM. Predictors of unrecognized HIV infection among poor and ethnic men who have sex with men in Los Angeles. AIDS Behav. 2011;15(3):643–649. doi: 10.1007/s10461-009-9653-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bauermeister J, Leslie-Santana M, Johns M, Pingel E, Eisenberg A. Mr. right, Mr. right now: romantic and casual partner-seeking online among young men who have sex with men. AIDS Behav. 2011;15(2):261–272. doi: 10.1007/s10461-010-9834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 84.Veinot TC. We have a lot of information to share with each other: understanding the value of peer-based health information exchange. Inform Res. 2010;15(4):452. [Google Scholar]
- 85.Taylor RS. Information use environments. In: Dervin B, Voigt MJ, editors. Progress sciences in communication. Norwood: Ablex Publishing; 1991. pp. 217–255. [Google Scholar]
- 86.Marsden PV. The SAGE handbook of social network analysis. Thousand Oaks: Sage; 2011. Survey methods for network data; pp. 370–388. [Google Scholar]
- 87.Krackhardt D, Stern RN. Informal networks and organizational crises: an experimental simulation. Soc Psychol Q. 1988;51(2):123–140. [Google Scholar]
- 88.Hill RA, Dunbar RIM. Social network size in humans. Human Nat. 2003;14(1):53–72. doi: 10.1007/s12110-003-1016-y. [DOI] [PubMed] [Google Scholar]
- 89.Huang G, Tausig M. Network range in personal networks. Soc Netw. 1990;12(3):261–268. [Google Scholar]
- 90.Earnshaw V, Chaudoir S. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sias PM, Wyers TD. Employee uncertainty and information-seeking in newly formed expansion organizations. Manag Commun Q. 2001;14(4):549–573. [Google Scholar]
- 92.Veinot TC. Regional HIV/AIDS information environments and information acquisition success. Inform Soc. 2013;29(2):88–112. [Google Scholar]
- 93.Fisher WA, Fisher JD, Rye BJ. Understanding and promoting AIDS-preventive behavior: insights from the theory of reasoned action. Health Psychol. 1995;14(3):255–264. doi: 10.1037//0278-6133.14.3.255. [DOI] [PubMed] [Google Scholar]
- 94.Veinot TC. Interactive acquisition and sharing: understanding the dynamics of HIV/AIDS information networks. J Am Soc Inform Sci Technol. 2009;60(11):2313–2332. [Google Scholar]
- 95.Veinot TC, Harris RM. Talking about, knowing about HIV/ AIDS in Canada: a rural-urban comparison. J Rural Health. 2011;27(3):310–318. doi: 10.1111/j.1748-0361.2010.00353.x. [DOI] [PubMed] [Google Scholar]
- 96.Veinot TC, Harris RM, Bella L, Rootman I, Krajnak J. HIV/ AIDS information exchange in rural communities: preliminary findings from a three province study. Can J Inform Libr Sci. 2006;30(3/4):271–290. [Google Scholar]
- 97.Harris RM, Veinot TC, Bella L, Rootman I, Krajnak J. Helpers, gatekeepers and the well-intentioned: the mixed blessing of HIV/AIDS informediation in rural Canada. In: Wathen N, Wyatt S, Harris RM, editors. Health information and technology: mediating health information in a changing socio-technical landscape. London: Palgrave; 2008. pp. 167–181. [Google Scholar]
- 98.Veinot TC, Campbell TR, Kruger D, Grodzinksi A, Franzen S, editors. American Medical Informatics Association (AMIA) Annual Symposium Proceedings. Washington, DC: AMIA; 2011. Drama and danger: the opportunities and challenges of promoting youth sexual health through online social networks. [PMC free article] [PubMed] [Google Scholar]
- 99.Erickson BH. The relational basis of attitudes. In: Wellman B, Berkowitz SD, editors. Social structures: a network approach. Cambridge: Cambridge University Press; 1988. pp. 99–121. [Google Scholar]
- 100.Friedkin NE. The attitude-behavior linkage in behavioral cascades. Soc Psychol Q. 2010;73(2):196–213. [Google Scholar]
- 101.Suls J, Martin R, Wheeler L. Social comparison: why, with whom, and with what effect? Curr Dir Psychol Sci. 2002;11(5):159–163. [Google Scholar]
- 102.Gino F, Shang J, Croson R. The impact of information from similar or different advisors on judgment. Organ Behav Hum Decis Process. 2009;108(2):287–302. [Google Scholar]
- 103.Tortoriello M, Reagans R, McEvily B. Bridging the knowledge gap: the influence of strong ties, network cohesion, and network range on the transfer of knowledge between organizational units. Organ Sci. 2012;23(4):1024–1039. [Google Scholar]
- 104.Lai G, Lin N, Leung S-Y. Network resources, contact resources, and status attainment. Soc Netw. 1998;20(2):159–178. [Google Scholar]
- 105.Reagans R, McEvily B. Network structure and knowledge transfer: the effects of cohesion and range. Adm Sci Q. 2003;48(2):240–267. [Google Scholar]
- 106.Valente TW. Network interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- 107.Walter HJ, Vaughan RD, Gladis MM, Ragin DF, Kasen S, Cohall AT. Factors associated with AIDS risk behaviors among high school students in an AIDS epicenter. Am J Public Health. 1992;82(4):528–532. doi: 10.2105/ajph.82.4.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Billy JO, Udry JR. The influence of male and female best friends on adolescent sexual behavior. Adolescence. 1985;20(77):21–32. [PubMed] [Google Scholar]
- 109.Alexander C, Piazza M, Mekos D, Valente T. Peers, schools, and adolescent cigarette smoking. J Adolesc Health. 2001;29(1):22–30. doi: 10.1016/s1054-139x(01)00210-5. [DOI] [PubMed] [Google Scholar]
- 110.Urberg KA, Degirmencioglu SM, Pilgrim C. Close friend and group influence on adolescent cigarette smoking and alcohol use. Dev Psychol. 1997;33(5):834–844. doi: 10.1037//0012-1649.33.5.834. [DOI] [PubMed] [Google Scholar]
- 111.Lorenc T, Marrero-Guillamon I, Llewellyn A, et al. HIV testing among men who have sex with men (MSM): systematic review of qualitative evidence. Health Educ Res. 2011;26(5):834–846. doi: 10.1093/her/cyr064. [DOI] [PubMed] [Google Scholar]
- 112.Chesney MA, Smith AW. Critical delays in HIV testing and care: the potential role of stigma. Am Behav Sci. 1999;42(7):1158–1170. [Google Scholar]
- 113.Gu J, Lau JT, Tsui H. Psychological factors in association with uptake of voluntary counselling and testing for HIV among men who have sex with men in Hong Kong. Public Health. 2011;125(5):275–282. doi: 10.1016/j.puhe.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 114.Glasman LR, Weinhardt LS, Difranceisco W, Hackl KL. Intentions to seek and accept an HIV test among men of Mexican descent in the Midwestern USA. AIDS Care. 2010;22(6):718–728. doi: 10.1080/09540120903431322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wei C, Yan H, Yang C, et al. Accessing HIV testing and treatment among men who have sex with men in China: a qualitative study. AIDS Care. 2013;26(3):372–38. doi: 10.1080/09540121.2013.824538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Phillips KA, Paul J, Kegeles S, Stall R, Hoff C, Coates TJ. Predictors of repeat HIV testing among gay and bisexual men. AIDS. 1995;9(7):769–775. doi: 10.1097/00002030-199507000-00015. [DOI] [PubMed] [Google Scholar]