Abstract
Introduction:
The positive effects of worldwide increases in enactment of legislative bans on smoking in public areas have been well documented. Relatively little is known about the effects of such bans on voluntary home smoking behavior. Meanwhile, private spaces, such as homes, have replaced public spaces as the primary milieu of secondhand smoke exposure.
Methods:
A systematic search of peer-reviewed articles was conducted using multiple databases including Cochrane Library, Cinahl, Embase, Global Health, Health Star, Joanna Briggs, MEDLINE, PsycINFO, PAIS International, PubMed, and Web of Science. We examined peer-reviewed studies that considered the impact of legislation-based public smoking bans on enactment of private home smoking restrictions.
Results:
Sixteen articles published between 2002 and 2014 were identified and included. Our results suggest overall positive effects post-legislative ban with the majority of studies demonstrating significant increases in home smoking restrictions. Studies focusing on smoking and nonsmoking samples as well as child populations are discussed in depth.
Conclusions:
Existing evidence indicates an overall significant positive effect post-legislative ban on voluntary home smoking restrictions. While disentangling these effects over space and time remains a challenge, scientific research has converged in dispelling any notion of significant displacement of smoking into the home. Policy makers, especially those in countries without existing public smoking legislation, can rest assured that these types of bans contribute to the minimization of tobacco-related harm.
Implications:
Findings converge in dispelling notions of displacement of smoking into the home as a consequence of legislative bans that prohibit smoking in public spaces. Evidence from the studies reviewed suggests that through their influence on social norms, legislative bans on smoking in public places may encourage citizens to establish voluntary home smoking restrictions, thus decreasing harm related to secondhand smoke.
Introduction
Globally, smoking tobacco accounts for approximately 6 million deaths per year, a substantial number that includes more than 600 000 nonsmokers.1 The detrimental effects of tobacco are known, as is the overwhelming cost associated with smoking, yet it remains the leading cause of preventable death worldwide.1 Legislation banning or restricting where individuals can smoke has increased steadily over the past three decades.2 One consequence of this increase has been the normalization of smoke-free public spaces such as worksites and restaurants. In turn, private venues (eg, homes and cars) have generally replaced public spaces as the primary milieu of secondhand smoke (SHS) exposure.3–7 The objective of this review has been to understand how the enactment of legislative (public) smoking bans or restrictions affect voluntary home smoking bans in private residences.
SHS, also known as passive smoke, involuntary smoke, tobacco smoke pollution, or environmental tobacco smoke, is the combination of contaminants released during the process of smoking a cigarette.8 SHS can be broken down into smoke emitted from the cigarette between puffs of burning tobacco known as “side stream smoke” (~85%)9 and smoke exhaled from the smoker known as “mainstream smoke” (the remaining 15%).10 SHS is considered the third leading cause of preventable disease, disability, and death worldwide.11 It has also long been known to be associated with adverse health effects for nonsmokers, such as cardiovascular disease, acute respiratory illness, low birth weight in babies of nonsmokers, morbidity and mortality in children, and multiple types of cancer.4,12–14 There is no safe level of SHS exposure, even minimal exposure to SHS is harmful.8,15 The negative effects of smoking within the home go beyond the immediate health risks of exposure to SHS. Children living with an adult smoker are up to twice as likely to take up smoking themselves.16,17 In contrast, smokers living in a smoke-free home exhibit increased cessation attempts, longer time to relapse, and lower consumption.18 For young adults, smoke-free homes moderate the effects of friends’ smoking on their smoking behavior and increase their likelihood of seeking smoke-free residences when leaving home.19
While research on the effectiveness of smoke-free legislation on exposure to SHS has been mostly positive, it has not always been straightforward. Published in 2010, a review paper by Callinan et al.2 consolidated 50 articles published before July 2009 and found reduced SHS exposure for a large portion of the population in public spaces. Callinan et al.2 reported no change in either the prevalence or duration of reported exposure to SHS in the home as a result of implementing legislative bans. This presents a challenge, especially given how much time is inevitably spent within private residences each day.20 However, SHS exposure in the home was only a secondary objective of the Callinan et al.2 review and only 30% of the included studies measured exposure to SHS in the home. Indeed, research concerning public smoking bans did not initially focus on the effects of bans on smoking behaviors within private residences.21 Over time, however, two main theories have been suggested to address the potential “spillover effects” of macro-environments (eg, public smoking policies) on micro-environments (eg, home smoking policies): social diffusion and displacement.7
Social diffusion posits that restricting smoking in public spaces leads to increases in voluntary home smoking bans or restrictions.22,23 This theoretical model encompasses ideas such as social norm and behavioral susceptibility theories.24–26 Social norms influence social behavior through perceptions of what is “normal” or “typical.” Smoke-free legislation may alter social norms by decreasing visibility and perceived acceptability of smoking in public venues and lead people to change their beliefs, awareness, attitudes, and practices concerning smoking.26,27 Behavioral susceptibility theory argues that if a given behavior becomes inconvenient or difficult, this behavior will gradually decline.27,28 Indeed, research demonstrates that smoking restrictions in public places inform people about current social norms toward smoking, and that greater perceived social unacceptability is associated with reduced cigarette consumption.26
A second, somewhat more pessimistic, theoretical model is that of displacement or last refuge which posits that smoking bans in public places will displace smoking behaviors to private places, like homes, and will produce undesired effects such as increased SHS exposure for nonsmoking family members.3,29 This is especially concerning for children, who are more vulnerable to the effects of SHS.5,30,31 In the United States, in 2010, approximately 98% of children living with a smoker, compared to 40% not living with a smoker, had cotinine levels (a metabolite of nicotine which has a longer half-life than nicotine) above .05ng/mL, indicating SHS exposure.32 Cotinine levels in children are predicted by the number of cigarettes smoked inside the home.32 ,33 This is particularly problematic because under most circumstances children do not have a choice as to whether or not they are exposed to SHS within their home environment.
To date, findings have been inconsistent with regard to the effects of public smoking bans on voluntary home smoking restrictions but most support a social diffusion model.2,22,23,29,34–40 Nevertheless, some findings suggest that smoking bans may have negative repercussions.4,41,42 The relationships between private and public spaces with regard to smoking bans and behavior have been found to be complex and have been said to “demand[] more consideration if interventions in public areas are meant to serve as catalysts for favorable changes in primary private spaces such as homes.”20 , p.2 This review aims to determine the overall effect of the enactment of legislative (public) smoking bans or restrictions on voluntary smoking restrictions in private residences as well as to evaluate the current status of the literature and the strength of evidence for and against diffusion and social displacement models.
Methods
Literature Search Strategy and Study Selection
In August 2014, a systematic literature search was undertaken by the lead author using keyword searches in multiple electronic databases including: Cochrane Library, Cinahl, Embase, Global Health, Health Star, Joanna Briggs, MEDLINE, PsycINFO, PAIS International, PubMed (excluding Medline), and Web of Science. The following terms and keywords were combined using database-specific search strategies: tobacco use disorder; tobacco use; tobacco consumption; adolescent smoking; parental smoking; smoking habit*; maternal smoking; paternal smoking; parental smoking; nicotine; tobacco smoke; cigarette smoking; tobacco smoke pollution; smoking; tobacco use cessation; smoking cessation; tobacco dependence; tobacco products; smokeless tobacco; indoor air pollution; passive smok*; secondhand smoke; second-hand smoke; second hand smoke; environmental tobacco smoke; involuntary smok*; anti-smoking; antismoking; smoke-free policy; legislation; legislative processes; drug laws; ban, bans; legisl*; restrict*; prohibit*; policy, policies; law, laws; household*; home, homes; condos, condominium*; dwelling*; residence*; private places. A full appendix of search terms and strategies employed for each database can be made available by the authors.
After duplicate references were removed, titles of articles were screened and references were discarded if they did not relate to public smoking bans. Both authors independently screened and reviewed the titles and abstracts of remaining references to identify whether articles were relevant and met the inclusion criteria. The full text was obtained for all articles where clarification was needed with regard to study design or outcomes of interest. This search was further supplemented by hand-searching reference lists from included studies and relevant journals such as Addiction, Nicotine and Tobacco Research, and Tobacco Control, through forward citation tracking, and through “related article” searches on Google Scholar.
Inclusion and Exclusion Criteria
We included English language peer-reviewed articles that examined the impact of legislation-based smoking bans or restrictions on enactment of private home smoking bans or restrictions. Legislative bans included those implemented at a local, regional, or national level which either banned smoking completely (comprehensive) or restricted it to designated areas (partial). Comprehensiveness of the bans was assessed using the same criteria as Callinan et al.2 whereby bans prohibiting smoking in indoor workplaces, including bars and restaurants, were categorized as comprehensive legislation, regardless of exemptions in particular settings such as prisons or mental health institutions. Partial bans are less restrictive and were categorized by legislation allowing designated smoking areas in indoor workplaces, including bars and restaurants. Articles that included setting-based bans, such as workplaces, where smoking has been partially or comprehensively restricted, though not necessarily as a result of municipal, state-level, or national legislation, were excluded. In order to ensure valid assessment of home smoking restrictions, only studies that specifically used terms such as “allowed,” “permitted,” or “restricted/restrictions” with regard to smoking in the home were included. After the abstracts were sifted, outcome variables for all potential articles were specified in a table (not shown) and compared for consistency of terminology. For studies comparing pre- and post-legislation outcomes and a control group (no legislative change), only pre- and post-legislative samples were examined. While certain study findings were derived from the same datasets, the outcomes measured differed, and as such are separately reviewed within the results section.
Given that longitudinal studies of population-based samples are one of the best ways to examine the process of change in smoking behaviors, articles were excluded if they did not include at least one pre-ban timepoint and at least one follow-up post-ban.43 Studies were not excluded on the basis of participant smoking status (ie, smokers only, nonsmokers, and both) or age (eg, child sample included). Publications were not excluded on the basis of publication date. Finally, meta-analysis was not possible due to the heterogeneity in study design, participants, outcomes, and nature of the intervention.44
Critical Appraisal of Studies
Critical appraisal of the methodology of identified studies was undertaken independently by both authors. Specifically, the validity and suitability of the methods employed, outcome measures, and risk of bias due to response rates, inadequate sample size, and potential confounding variables were assessed for each study.45 Results of the critical appraisal were compared and, when necessary, discussions between the both authors were undertaken until consensus was reached.
Results
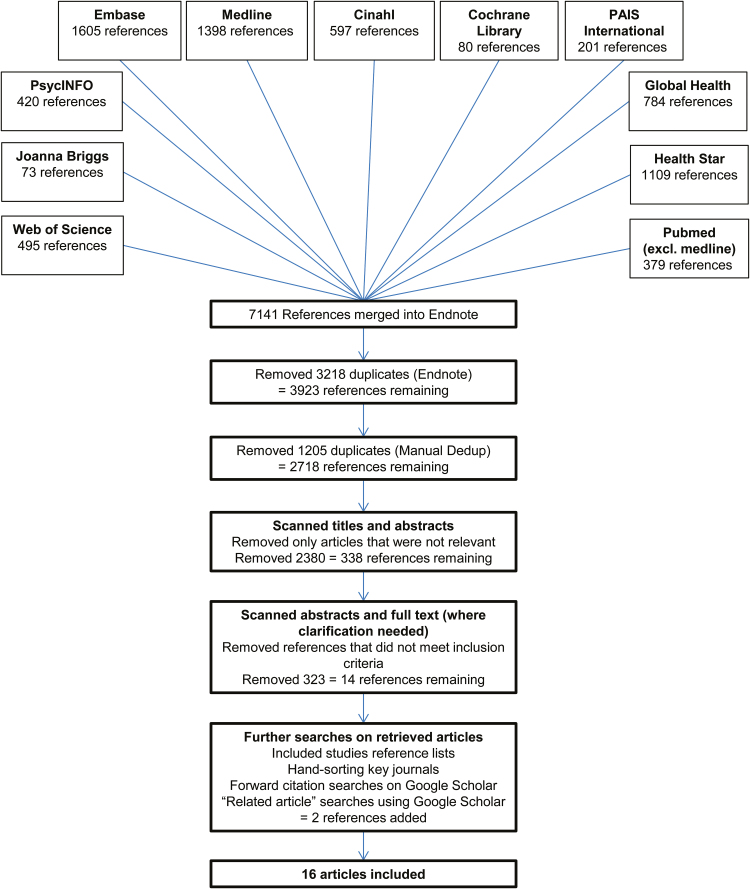
A full breakdown of the article identification and selection procedure for this review is outlined in Figure 1. The electronic database search yielded 7141 potential articles, of which 4423 were duplicates. A further 2380 were excluded on the basis of title and abstract. Full texts for the remaining 338 articles were retrieved. After evaluation of full text, 14 references remained and an additional two articles were identified through hand-searching of relevant journals and through forward citation tracking. A total of 16 studies published between 2002 and 2014 met final inclusion for this review.20,29,35–37,39,40,46–54 Supplementary Table 1 includes a description of each of the 16 selected studies, including author, publication year, country, study design, sample descriptions, date of ban(s), and a brief summary of key results/findings.
Figure 1.
Flowchart identifying study selection process.
Quality of Included Studies
All studies clearly stated a research question/objective and specified a population of interest. Each study also consistently applied inclusion and exclusion criteria, recruited participants from the same or similar populations over consistent time periods, and adjusted for key potential confounding variables.
None of the included studies demonstrated limitations which wholly compromised their results to the point where exclusion was necessary. Still, the studies included in this review are not without their limitations; all studies introduced certain risk of bias. For example, one study49 had a participation rate below 50% at the first wave data collection and another39 had participation rates below 50% at both timepoints. Low participation rates create potential risk of bias and may mislead readers to conclude (erroneously) that a sample may be generalizable when, in actuality, it does not adequately represent the target population.
Some studies did not provide sample size justifications or power descriptions within their results but in each case authors did draw attention to this specific limitation.36,40,48,49 Finally, loss to follow-up was above 20% in certain cohort studies.20,36,39,47,54 Due to these limitations, readers should be cautious in interpreting the results of some of the included studies. However, using the appraisal tool’s criteria, the quality of all of the studies was considered sufficiently high for inclusion and similar enough to be comparable.
Effects of Smoking Legislation on Home Smoking Restrictions
Six studies reported general population trends in home smoking restrictions before and after implementation of a legislative public smoking ban.30,46,49,51–53 All studies either reported overall significant positive effects post-legislative ban (ie, social diffusion) or no significant differences pre- and post-legislation.20,29,35–37,39,40,46–54 For example, a study by Guzman et al.49 reported on cross-sectional analysis of participants surveyed before and after a statewide smoke-free law enacted in the summer of 2010 and found that participants with smoking restrictions in their homes increased significantly from 74% to 79.6% (p = .04). No studies reported an overall significant decrease in home smoking restrictions (ie, displacement of smoking into the home) after legislation was enacted although some studies did report smokers who had started smoking within the home after the smoking ban.20,36 Nevertheless, these studies also reported that considerably more smokers ceased smoking within the home after the enactment of legislation. For example, a study by Biener et al.36 reported, in a generalizable sample of Massachusetts smokers, that 10.1%, 95% confidence interval (CI) [4.9, 19.4] of the sample started smoking at home but twice as many individuals (ie, 20.3%, 95% CI [12.0, 32.4]) stopped smoking at home after a ban was implemented in Boston.
Smokers versus Nonsmokers
Three studies reported results that contrasted populations of both smokers and nonsmokers.39,52,54 One of the three studies further analyzed subsamples of their nonsmoking population broken down by whether or not they lived with one or more smokers.52 Similarly, an additional study of nonsmokers compared individuals who lived in homes with and without smokers.29 Five studies looked at only nonsmoking participants,29,35,40,48,50 of which three were focused on children35,40,50 and one on mothers whose spouse was a smoker.48 Three studies specifically looked at smoking populations,36,37,47 of which one defined smokers at baseline only.36 One study included smokers and ex-smokers.20
All studies comparing smoking and nonsmoking subsamples (n = 3)39,52,54 found that smokers were less likely to have smoking restrictions before the ban and after the ban, but that regardless of smoking status, restrictions increased pre- to post-legislation. However, two studies did not specifically mention if their findings were statistically significant.39,52 Another study found that while bans on smoking in homes increased significantly for nonsmokers shortly after a first public smoking ban for workplaces was enacted, smokers only demonstrated a significant increase in home smoking bans after the second timepoint (ie, after smoking was banned from bars, taverns, gaming clubs, and bar areas of restaurants).54 Gilpin et al.52 found that after a first comprehensive statewide law mandating clean air in indoor workplaces (excluding hospitality sectors), nonsmokers and smokers reported similar increases in complete home smoking bans, but after a second comprehensive ban, smokers continued to increase in their uptake of home smoking restrictions, while nonsmokers continued to adopt home smoking restrictions but to a lesser degree than after the first ban.
Two studies included within this review compared nonsmoking populations based on whether or not they lived with one or more smokers.29,52 These studies also confirmed that homes with one or more adult smoker were less likely to have a home smoking ban prior to legislation and post-legislation (as reported by a nonsmoker within the home).52 Additionally, participants from homes where all adults smoked reported even fewer home smoking restrictions than those from homes with at least one adult who smoked. The latter also showed larger increases in home smoking bans after the first comprehensive ban was put in place (17.5%) than after the second comprehensive ban (16.3%), while children living in homes where all adults smoked showed continued large increases after the first (18.2%) and the second (20.8%) bans.52 In contrast, a study by Haw et al.31 found that, after enactment of a legislative ban, nonsmokers living in smoking homes had almost double the increase in complete home smoking bans (10.3%) compared to nonsmokers living in nonsmoking homes (5.8% increase).
Of the studies under review focusing solely on nonsmoking individuals (n = 5),29,35,40,48,50 all demonstrated significant increases in home smoking restrictions pre- to post-ban. In contrast, of the four studies that specifically concentrated on individuals who smoke (including one study that also included ex-smokers),20,36,37,47 only one reported a significant increase in home smoking restrictions post-ban.37 When contrasted to a similar (control) area without a ban, similar significant decreases were demonstrated for percentage of homes that allowed smoking pre- and post-ban.39 Moreover, the one study that combined smokers and nonsmokers but controlled for smoking status also failed to report significant findings.53
Evidence From Child Studies
Three studies specifically focused on self-reported home smoking restrictions by children and youth aged 4–15 years.35,40,50 All studies looked exclusively at nonsmoking school-aged children before and after enactment of comprehensive national level smoke-free legislation.
Regardless of parental smoking status, Akhtar et al.35 found that 10–11 months after implementation of smoke-free legislation, less students reported “no restriction” at home (pre 18.5%, 95% CI [16.0, 21.3]; post 14.2%, 95% CI [12.1, 16.5]). They also found that after adjusting for age, the type of home smoking restriction (none, partial, or complete) was associated with not only the survey year (pre- or post-legislation), but also the number of parents who smoked and family affluence. Furthermore, households with children and only a father who smoked were more likely to have a complete home smoking restriction than homes with children where only a mother smoked or where both parents smoked. In contrast, a study by Jarvis et al.40 found that while the percentage of nonsmoking households with nonsmoking parents remained stable (and ˃95%), homes with smoking parents reported significantly more smoke-free homes post-legislation than before the ban took place. This was found despite the fact the number of smoking parents pre- and post-legislative ban remained stable (ie, no statistically significant decline). Regardless of parental smoking status, the effects of the legislative ban also seemed to take some time before affecting behavior; indeed, pre- and post-ban data show a stall in increases to the number of home smoking restrictions around the time of the ban (2006 = 76.6%; 2007 [pre] = 78.1%; 2007 [post] = 77.2%; 2008 = 80.4%). When only looking at smoking parents, this makes sense given that before the ban came into place, the number of smoke-free homes was not increasing, but rather decreasing (2006 = 35.5%; 2007 [pre] = 30.5%; 2007 [post] = 40.5%; 2008 = 48.1%). Finally, a study published in 2012 by Moore et al.50 looked at pre- and post-legislative home smoking restrictions in Scotland, Wales, and Northern Ireland. Across the three regions, full restrictions in the home increased (51.9% pre to 55.1% post) and the number of homes that permitted smoking indoors decreased (16.8% pre to 12.7% post). However, among children of smokers, full smoking restrictions only increased by 1%. Decreased risk of unrestricted smoking remained significant after adjustment for parents’ smoking status in Scotland and Northern Ireland, but not in Wales where decreased risk of unrestricted smoking failed to reach significance.50
One study of adults looked at how the presence of a child in a residence affected rates of smoking restrictions in the home.52 Homes where all adults smoked had fewer restrictions than homes with at least one adult smoker or all households with children regardless of smoking status. Homes with all adults smoking increased in home smoking restrictions from 13.5% (pre-legislation concerning smoke-free workplaces) to 31.7% and again to 52.5% (after legislation was extended to include restaurants and bars), while homes with at least one adult smoker increased from 33.1% to 50.6%, and again to 66.9%, and overall homes with children increased from 59.7% to 73.9% and again (after legislation was extended) to 82.2%.
Discussion
This review both extends and refines previous work by Callinan et al.2 who summarized the general effects of public smoking legislation on SHS exposure, including, as a secondary outcome of interest, home smoking restrictions. Certain articles found within Callinan et al.2 were not included in our review due to our more stringent criteria for outcomes under consideration, which specifically focused on home smoking restrictions instead of general SHS exposure. Only five of the studies that Callinan et al. reviewed were included in the present review.29,36,37,39,52 Of the studies included in this review but not in Callinan et al.’s, 10 were published after their final literature search was conducted in July 200920,35,40,46–51,54 and one was published prior.53 Overall, the Callinan et al.2 article found no effect of legislative bans on home smoking restrictions. In contrast, this review establishes that the benefits of public smoking bans (ie, statistically significant increases in home smoking restrictions) greatly outweigh undesirable consequences.
Overall, results from the studies included in the present review revealed that the number of voluntary home smoking restrictions either increased or remained stable across all studies, thus providing support for the continued enactment of legislative public smoking restrictions. Results support the conclusion that a major anticipated drawback of smoke-free legislation (ie, displacement from public places into the home) is not occurring. Continuing to anticipate displacement of smoking into the home as a consequence of the enactment of public smoking bans might actually do more harm than good by hindering the benefits of public smoking bans such as reduced SHS in public venues and healthcare savings for governments and individuals.55
Studies contrasting smokers and nonsmokers revealed that despite the known benefits of smoke-free homes, current smokers are much more likely to allow smoking in the home both prior to and after the enactment of legislative smoking bans.39,52,54 Studies that focused specifically on smoking populations also reported fewer significant increases in the number of home smoking restrictions. While this may be unsurprising, the studies that contrasted smokers and nonsmokers also revealed that regardless of smoking status, home smoking restrictions increased after legislative bans were enacted. Findings also suggested that the progression to voluntary home smoking restrictions may vary based on smoking status: Individuals who smoke may take longer to adopt home smoking bans and may only change their behavior in response to harsher restrictions.52,54 Perhaps with time, legislative smoking bans hasten or promote normalization of negative stigma associated with smoking and SHS exposure, particularly when it comes to private residences, eventually encouraging smokers to enact these changes voluntarily within the home.
The studies under review focusing on nonsmoking individuals all demonstrated significant increases in voluntary home smoking restrictions pre- to post-ban.29,35,40,48,50 This finding, in favor of diffusion, is important given that nonsmokers are the individuals who suffer most from the health consequences of SHS exposure and are the primary concern of policy makers who seek to avoid potential displacement of smoking into the home post-legislation. Three of the five studies focused specifically on nonsmoking populations used samples of children exclusively.35,40,50 Results remain noteworthy given that, again, they confirm a lack of evidence for significant displacement of smoking into the home after legislation is enacted.
Children have been hypothesized to be the most vulnerable population affected by SHS because they do not have the same agency as adults with regard to exposure to smoke, particularly if their parents are smokers. This review found no evidence of displacement of smoking into the home within the studies focused on child samples. In fact, the studies included supported the theory of diffusion and the argument that the benefits of smoking legislation in public places is extending into the homes of children whose parents smoke. This finding was echoed in samples of adult populations where individuals living with children reported that they were more likely to establish home smoking bans after legislation had been implemented.52
This review is not without limitations. With the exception of one subsample with biochemical verification, the studies reviewed only took into consideration self-report measures which may have resulted in underestimation of smoking behaviors due to recall bias and perceived social desirability.47 Still, previous research has found self-reports of SHS exposure to be strongly correlated with other biological markers of SHS such as ambient nicotine measurements.56,57 A second limitation was that certain studies lacked clarity in reporting results (eg, not explicitly stating if results were statistically significantly different pre- and post-ban36,39,46 or relying on small figures to demonstrate differences52). Half of the studies did not mention missing data.36,40,46–49,53,54 Without transparency about missing data, there is a potential for bias and other issues of coverage and generalizability. An additional limitation of this review is the exclusion of grey literature which may have introduced possible publishing bias whereby published literature is more likely to have statistically significant results compared to grey literature.43 ,58
Changes in smoke-free legislation have occurred in parallel to an overall decline of smoking prevalence in Western societies and a corresponding rise in smoke-free homes.18,20,39 As a result, it has been suggested that this trend toward decline may explain a portion of the changes observed after a public smoking ban is enacted.36 For example, Kairouz et al.20 state that the ban under examination was one of many governmental actions being introduced concurrently meant to reduce nonsmoker exposure to SHS, any of which may have also had an effect on the results observed. Indeed, without a full understanding of the complete context in which these studies take place, it remains an ongoing challenge to tease apart changes as a result of public smoking bans from other potentially salient factors that occur over time.
Given the relatively homogenous geographic and cultural scope of the included studies (ie, mostly Western countries), investigating the consequences of legislative smoking bans on home smoking behaviors in non-Western and developing countries is an important next step. Even with a 16% increase global coverage between 2010 and 2012 alone, the World Health Organization reported that as of 2013 at least 81, mainly developing, countries have yet to see any introduction of smoke-free policy.12 Given the promising implications of findings highlighted within this review, policy makers worldwide should feel encouraged to continue pushing forward public smoking bans at a legislative level.
Future research should also examine the various pathways and progressions to voluntary home smoking restrictions in more depth. Findings from this review indicate that public smoking legislation may elicit differing responses based on individual factors (eg, smoking status) and that results may vary depending on the time frame under examination. Moving forward, studies concerning voluntary home smoking restrictions need to keep these compositional and contextual factors in mind. Furthermore, extending methodology to include biochemical markers of SHS could strengthen the reliability of literature on this topic and research should look for potential avenues to broaden areas of interest to include e-cigarettes and marijuana use. In summary, while disentangling these effects over time and space remains a challenge, existing research on home smoking restrictions following enactment of public smoking legislation indicates overall significant positive effects post-legislative ban.
Supplementary Material
Supplementary Table 1 can be found online at http://www.ntr.oxfordjournals.org
Funding
EM received the Canadian Institutes of Health Research (CIHR) Frederick Banting Doctoral Award.
Declaration of Interests
The authors have no conflicts of interest to declare.
Acknowledgments
We would like to thank Kiran McCloskey for her guidance throughout this manuscripts creation and submission. We would also like to thank Pamela Harrison who oversaw the literatures searches.
References
- 1. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2011: Warning About the Dangers of Tobacco. Geneva, Switzerland: Author; 2011. http://apps.who.int/iris/bitstream/10665/44616/1/9789240687813_eng.pdf Accessed May 25, 2016. [Google Scholar]
- 2. Callinan JE, Clarke A, Doherty K, et al. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.CD005992.pub2. [DOI] [PubMed]
- 3. Lopez MJ, Nebot M, Schiaffino A, et al. Two-year impact of the Spanish smoking law on exposure to secondhand smoke: evidence of the failure of the ‘Spanish model’. Tob Control. 2012;21:407–411. doi:10.1136/tc.2010.042275. [DOI] [PubMed] [Google Scholar]
- 4. Yao T, Lee AH, Mao Z. Potential unintended consequences of smoke-free policies in public places on pregnant women in China. Am J Prev Med. 2009;37:59–64. doi:10.1016/j.amepre.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Service USPH, Office of the Surgeon General. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2006. www.surgeongeneral.gov/library/reports/secondhandsmoke/fullreport.pdf Accessed January 1, 2015. [Google Scholar]
- 6. United States Public Health Service Office of the Surgeon General, Centers for Disease Control and Prevention Office on Smoking Health. Children and Secondhand Smoke Exposure: Excerpts From the Health Consequences of Involuntary Exposure to Tobacco Smoke. Centers for Disease Control and Prevention Office on Smoking and Health; 2007. www.cdc.gov/tobacco/data_statistics/sgr/2006/pdfs/childrens-excerpt.pdf Accessed January 1, 2015. [Google Scholar]
- 7. Martínez-Sánchez JM, Sureda X, Fu M, et al. Secondhand smoke exposure at home: assessment by biomarkers and airborne markers. Environ Res. 2014;133:111–116. doi:10.1016/j.envres.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 8. US Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease. A Report of the Surgeon General. Centers for Disease Control and Prevention (US); 2010. www.ncbi.nlm.nih.gov/pubmed/21452462 Accessed January 1, 2015. [PubMed] [Google Scholar]
- 9. Taylor AE, Johnson DC, Kazemi H. Environmental tobacco smoke and cardiovascular disease. A position paper from the Council on Cardiopulmonary and Critical Care, American Heart Association. Circulation. 1992;86(2):699–702. doi:10.1161/01.CIR.86.2.699. [DOI] [PubMed] [Google Scholar]
- 10. Dunn AJ, Satcher D, Zeise L. Health Effects of Exposure to Environmental Tobacco Smoke: The Report of the California Environmental Protection Agency. Darby, PA: DIANE Publishing; 2000. [Google Scholar]
- 11. Andersen PA, Buller DB, Voeks JH, et al. Predictors of support for environmental tobacco smoke bans in state government. Am J Prev Med. 2006;30(4):292–299. doi:10.1016/j.amepre.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization (WHO). WHO Report on the Global Tobacco Epidemic, 2013: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. Geneva, Switzerland: Author; 2003. http://apps.who.int/iris/bitstream/10665/85380/1/9789241505871_eng.pdf Accessed May 25, 2016. [Google Scholar]
- 13. DiFranza JR, Lew RA. Morbidity and mortality in children associated with the use of tobacco products by other people. Pediatrics. 1996;97:560–568. http://pediatrics.aappublications.org/content/97/4/560.full.pdf+html Accessed January 1, 2015. [PubMed] [Google Scholar]
- 14. Windham GC, Hopkins B, Fenster L, Swan SH. Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology. 2000;11(4):427–433. http://journals.lww.com/epidem/Fulltext/2000/07000/Prenatal_Active_or_Passive_Tobacco_Smoke_Exposure.11.aspx Accessed January 1, 2015. [DOI] [PubMed] [Google Scholar]
- 15. Jacobs M, Alonso AM, Sherin KM, et al. Policies to restrict secondhand smoke exposure: American College of Preventive Medicine position statement. Am J Prev Med. 2013;45(3):360–367. doi:10.1016/j.amepre.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 16. Farkas AJ, Gilpin EA, White MM, et al. Association between household and workplace smoking restrictions and adolescent smoking. JAMA. 2000;284:717–722. doi:10.1001/jama.284.6.717. [DOI] [PubMed] [Google Scholar]
- 17. Klein EG, Forster JL, Erickson DJ, et al. The relationship between local clean indoor air policies and smoking behaviours in Minnesota youth. Tob Control. 2009;18:132–137. doi:10.1136/tc.2007.024307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mills AL, Messer K, Gilpin EA, et al. The effect of smoke-free homes on adult smoking behavior: a review. Nicotine Tob Res. 2009;11:1131–1141. doi:10.1093/ntr/ntp122. [DOI] [PubMed] [Google Scholar]
- 19. Albers AB, Biener L, Siegel M, et al. Impact of parental home smoking policies on policy choices of independently living young adults. Tob Control. 2009;18:245–248. doi:10.1136/tc.2008.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kairouz S, Lasnier B, Mihaylova T, et al. Smoking restrictions in homes after implementation of a smoking ban in public places. Nicotine Tob Res. 2014;17:41–47. doi:10.1093/ntr/ntu125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brownson RC, Davis JR, Jackson-Thompson J, et al. Environmental tobacco smoke awareness and exposure: impact of a statewide clean indoor air law and the report of the US Environmental Protection Agency. Tob Control. 1995;4:132–138. doi:10.1136/tc.4.2.132. [Google Scholar]
- 22. Cheng KW, Glantz SA, Lightwood JM. Association between smokefree laws and voluntary smokefree-home rules. Am J Prev Med. 2011;41(6):566–572. doi:10.1016/j.amepre.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mons U, Nagelhout GE, Allwright S, et al. Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys. Tob Control. 2013;22(e1):e2–e9. doi:10.1136/tobaccocontrol-2011-050131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. World Health Organization. Making Cities Smoke-Free. 2010. http://whqlibdoc.who.int/publications/2011/9789241502832_eng.pdf?ua=1 Accessed January 1, 2015. [Google Scholar]
- 25. Sunstein CR, Perkins HW. Sober lemmings: the social norms approach to preventing school and college age substance abuse: a handbook for educators, counselors, and clinicians. The New Republic. 2003;228(14):34. [Google Scholar]
- 26. Hamilton WL, Biener L, Brennan RT. Do local tobacco regulations influence perceived smoking norms? Evidence from adult and youth surveys in Massachusetts. Health Educ Res. 2008;23(4):709–722. doi:10.1093/her/cym054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gritz ER, Prokhorov AV, Hudmon KS, et al. Predictors of susceptibility to smoking and ever smoking: a longitudinal study in a triethnic sample of adolescents. Nicotine Tob Res. 2003;5(4):493–506. doi:10.1080/1462220031000118568. [DOI] [PubMed] [Google Scholar]
- 28. Yang T. Tobacco Control: Theory and Implementation. Beijing, CN: People’s Health House; 2010. [Google Scholar]
- 29. Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ. 2007;335(7619):549. doi:10.1136/bmj.39315.670208.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cheraghi M, Salvi S. Environmental tobacco smoke (ETS) and respiratory health in children. Eur J Pediatr. 2009;168(8):897–905. doi:10.1007/s00431-009-0967-3. [DOI] [PubMed] [Google Scholar]
- 31. Royal College of Physicians. Passive Smoking and Children: A Report by the Tobacco Advisory Group of the Royal College of Physicians. The Royal College of Physicians; 2010. www.rcplondon.ac.uk/sites/default/files/documents/passive-smoking-and-children.pdf Accessed January 1, 2015. [Google Scholar]
- 32. Centers for Disease Control and Prevention (CDC). Vital signs: nonsmokers’ exposure to secondhand smoke—U.S., 1999–2008. MMWR Morb Mortal Wkly Rep. 2010;59:1141–1146. www.cdc.gov/mmwr/preview/mmwrhtml/mm5935a4.htm Accessed January 1, 2015. [PubMed] [Google Scholar]
- 33. Mannino DM, Caraballo R, Benowitz N, et al. Predictors of cotinine levels in US children: data from the Third National Health and Nutrition Examination Survey. Chest. 2001;120:718–24. doi:10.1378/chest.120.3.718 [DOI] [PubMed] [Google Scholar]
- 34. Akhtar PC, Currie DB, Currie CE, Haw SJ. Changes in Child Exposure to Environmental Tobacco Smoke (CHETS) study after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ. 2007;335(7619):545. doi:10.1136/bmj.39311.550197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Akhtar PC, Haw SJ, Currie DB, et al. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smokefree legislation. Tob Control. 2009;18:409–415. doi:10.1136/tc.2009.030627. [DOI] [PubMed] [Google Scholar]
- 36. Biener L, Garrett CA, Skeer M, et al. The effects on smokers of Boston’s smoke-free bar ordinance: a longitudinal analysis of changes in compliance, patronage, policy support, and smoking at home. J Public Health Manag Pract. 2007;13:630–636. doi:10.1097/01.PHH.0000296140.94670.d4. [DOI] [PubMed] [Google Scholar]
- 37. Fong GT, Hyland A, Borland R, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob Control. 2006;15(suppl 3):iii51–58. doi:10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Holliday JC, Moore GF, Moore LA. Changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales: a repeated cross-sectional study. BMC Public Health. 2009;9:430. doi:10.1186/1471-2458-9-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hyland A, Hassan LM, Higbee C, et al. The impact of smokefree legislation in Scotland: results from the Scottish ITC: Scotland/UK longitudinal surveys. Eur J Public Health. 2009;19(2):198–205. doi:10.1093/eurpub/ckn141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jarvis MJ, Sims M, Gilmore A, et al. Impact of smoke-free legislation on children’s exposure to second-hand smoke: cotinine data from the Health Survey for England. Tob Control. 2011;21:18–23. doi:10.1136/tc.2010.041608. [DOI] [PubMed] [Google Scholar]
- 41. Adda J, Cornaglia F. The effect of bans and taxes on passive smoking. Am Econ J Appl Econ. 2010;2:1–32. doi:10.1257/app.2.1.1. [Google Scholar]
- 42. Ho SY, Wang MP, Lo WS, et al. Comprehensive smoke-free legislation and displacement of smoking into the homes of young children in Hong Kong. Tob Control. 2010;19(2):129–133. doi:10.1136/tc.2009.032003. [DOI] [PubMed] [Google Scholar]
- 43. Conn VS, Valentine JC, Cooper HM, et al. Grey literature in meta-analyses. Nurs Res. 2003;52:256–261. doi:10.1097/00006199-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 44. Deeks JJ, Higgins J, Altman DG. Analysing Data and Undertaking Meta-Analyses. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; 2008:243–296. doi:10.1002/9780470712184.ch9. [Google Scholar]
- 45. National Heart Lung and Blood Institute of the United States. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort Updated March 2014. Accessed January 1, 2015. [Google Scholar]
- 46. Yang T, Abdullah AS, Li L, et al. Public place smoke-free regulations, secondhand smoke exposure and related beliefs, awareness, attitudes, and practices among Chinese urban residents. Int J Environ Res Public Health. 2013;10(6):2370–2383. doi:10.3390/ijerph10062370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cooper J, Borland R, Yong HH, Hyland A. Compliance and support for bans on smoking in licensed venues in Australia: findings from the International Tobacco Control Four-Country Survey. Aust N Z J Public Health. 2010;34(4):379–385. doi:10.1111/j.1753-6405.2010.00570.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chan SSC, Cheung YTD, Leung DYP, et al. Secondhand smoke exposure and maternal action to protect children from secondhand smoke: pre- and post-smokefree legislation in Hong Kong. PLoS One. 2014;9. doi:10.1371/journal.pone.0105781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Guzman A, Walsh MC, Smith SS, et al. Evaluating effects of statewide smoking regulations on smoking behaviors among participants in the Survey of the Health of Wisconsin. Wis Med J. 2012;111:166–171. www.wisconsinmedicalsociety.org/_WMS/publications/wmj/pdf/111/4/166.pdf Accessed January 1, 2015. [PMC free article] [PubMed] [Google Scholar]
- 50. Moore GF, Currie D, Gilmore G, et al. Socioeconomic inequalities in childhood exposure to secondhand smoke before and after smoke-free legislation in three UK countries. J Public Health (Oxf). 2012;34:599–608. doi:10.1093/pubmed/fds025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lee JT, Glantz SA, Millett C. Effect of smoke-free legislation on adult smoking behaviour in England in the 18 months following implementation. PLoS One. 2011;6(6):e20933. doi:10.1371/journal.pone.0020933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gilpin EA, Farkas AJ, Emery SL, et al. Clean indoor air: advances in California, 1990–1999. Am J Public Health. 2002;92:785–791. doi:10.2105/AJPH.92.5.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rayens MK, Hahn EJ, Langley RE, et al. Public opinion and smoke-free laws. Policy Polit Nurs Pract. 2007;8:262–270. doi:10.1177/1527154407312736. [DOI] [PubMed] [Google Scholar]
- 54. Fong GT, Craig LV, Guignard R, et al. Evaluating the effectiveness of France’s indoor smoke-free law 1 year and 5 years after implementation: findings from the ITC France Survey. PLoS One. 2013;8(6):e66692. doi:10.1371/journal.pone.0066692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hahn EJ. Smokefree legislation: a review of health and economic outcomes research. Am J Prev Med. 2010;39(6):s66–s76. doi:10.1016/j.amepre.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 56. Okoli CT, Kelly T, Hahn EJ. Secondhand smoke and nicotine exposure: a brief review. Addict Behav. 2007;32(10):1977–1988. doi:10.1016/j.addbeh.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 57. Gorber CS, Schofield-Hurwitz S, Hardt J, et al. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009;11:12–24. doi:10.1093/ntr/ntn010. [DOI] [PubMed] [Google Scholar]
- 58. Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337(8746):867–872. doi:10.1016/0140-6736(91)90201-Y. [DOI] [PubMed] [Google Scholar]