Abstract
Purpose
Biliary cancer is a highly malignant neoplasm with poor prognosis and most patients need to undergo palliative chemotherapy, however major clinical problem associated with the use of chemotherapy is chemoresistance. So far, we aimed at investigating clinical implications of apurinic/apyrimidinic endodeoxyribonuclease 1 (APEX1) and Jagged1 as chemoresistance factors in biliary tract cancer.
Methods
We used 5 human biliary tract cancer cell lines (SNU-245, SNU-308, SNU-478, SNU-1079, and SNU-1196), and investigated the chemosensitivity of APEX1 and Jagged1 through 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay and Western blot. Alternately, the 10 patients of advanced biliary cancer consist of 2 group according to the chemotherapy response examined by immunohistochemistry using APEX1 and Jagged1 antibody, and protein expression level was scored for staining intensity and percent positive cell.
Results
The result of MTT assay after APEX1 knockdown showed that strong coexpression of APEX1 and Jagged1 cell line (SNU-245, SNU-1079, and SNU-1196) showed a greater decrease in IC50 of chemotherapeutic agent (5-fluorouracil, gemcitabine and cisplatin). The Western blot analysis of APEX1 and Jagged1 expression in biliary cancer cell lines after APEX1 knockdown definitively demonstrated decreased Jagged1 expression. The APEX1 and Jagged1expression level of immunohistochemistry represented that chemorefractory patients had higher than chemoresponsive patients.
Conclusion
These results demonstrate that simultaneous high expression of APEX1 and Jagged1 is associated with chemoresistance in biliary cancer and suggest that is a potential therapeutic target for chemoresistance in advanced biliary cancer.
Keywords: APEX1 protein, Jagged1 protein, 5-FU, Gemcitabine, Cisplatin
INTRODUCTION
Biliary cancer is uncommon, accounting for approximately 10% of primary liver cancer cases and 3% of all gastrointestinal neoplasms. Biliary cancer is a primary malignancy of the epithelial lining of the biliary tree, and is a histologically heterogeneous group that includes the intrahepatic and extrahepatic biliary trees and the gallbladder [1]. Biliary dysplasia and subsequent malignant transformation are caused by local inflammation in the biliary tree due to risk factors such as age, primary sclerosing cholangitis, hepatolithiasis, hepatitis, and liver flukes [2].
Gemcitabine, cisplatin, and 5-fluorouracil (5-FU) have shown therapeutic efficacy in advanced biliary cancer [3,4,5]; the gemcitabine plus cisplatin combination is currently the standard chemotherapeutic regimen [6].
The major clinical problem of chemotherapeutic treatment is primary or acquired resistance, and many theories regarding resistance mechanisms have been proposed. Among them, enhanced DNA repair is the most commonly proposed theory and is believed to involve the DNA base excision repair (BER) pathway. Apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) is the main enzyme involved in the BER pathway, and several studies have shown that APEX1 expression levels correlate with radio- and chemo-resistance in cancer cells; an elevated APEX1 protein level has also been found to be associated with poor clinical outcome in various cancers [7,8,9].
Many studies on the molecular mechanisms involved in the progression of biliary cancer have been performed, and there exists a clinical need to identify more effective biomarkers as therapeutic targets. However, no definitive biomarker has been identified for biliary cancer [10].
In this study, we assess the clinical implications of APEX1 in biliary cancer and analyze the relationship between APEX1 and chemoesistance to effective chemotherapeutic agent (5-FU, gemcitabine, and cisplatin) in advanced biliary cancer.
METHODS
Cell cultures
Five human biliary tract cancer cell lines (SNU-245, SNU-308, SNU-478, SNU-1079, and SNU-1196) were procured from the Korea Cell Line Bank (Seoul, Korea). Cell lines were cultured in Rosewell Park Memorial Institute 1640 medium supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin. Cells maintained in 5% CO2-humidified atmosphere at 37℃.
Preparation of drug solutions for in vitro assays
Aqueous solutions of all the drugs were prepared in distilled water and were stored at deep freezer (CLN-51U).
Cisplatin was obtained from JW Pharmaceutical Corp. (Seoul, Korea) in aqueous from 10 mg in 20 mL. 5-FU was obtained from JW Pharmaceutical Corp. in aqueous from 250 mg in 5 mL. Gemcitabine was obtained in powder from Sigma (St. Louis, MO, USA) 10 mg/mL.
MTT assay
Cell viability was determined by a 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay. The MTT assay was performed per a standard protocol. After treatment, 10 µL of MTT (1 mg/mL) in phosphate buffered saline (PBS) was incubated with cells in a 96-well plate for 4 hours at 37℃. Subsequently, medium containing MTT was removed, and 100 µL of dimethyl sulfoxide was added. Cells were incubated for an additional 10 minutes at 37℃ with gentle shaking. Absorbance was read on an enzyme-linked immunosorbent assay plate reader using a 540-nm filter.
siRNA-based experiments
Cells were transfected with small interfering RNA (siRNA) using RNAiMAX (Invitrogen, Carlsbad, CA, USA). Target sequences were as follows: APEX1, 5′-AAGTCTGGTACGACT GGAGTA-3′; for control siRNA, a nontargeting scrambled sequence was cloned into psilencer 2.1-U6. Biliary cancer cells were transfected with APEX1 siRNA or scrambled control siRNA using Lipofectamine 2000 (Invitrogen) and cultured in selection medium containing 400-µg/mL hygromycin for 4–5 weeks.
Immunoblotting
Cells were washed with 1× PBS and lysed in lysis buffer (20mM HEPES [N-2-hydroxyethylpiperazine-N-2-ethanesulfonic acid], pH 7.4; 2mM EGTA [ethyleneglycol-bis-(b-aminoethylether)-N,N,N′,N′-tetraacetic acid]; 50mM glycerol phosphate; 1% Triton X-100; 10% glycerol; 1mM Dithiothreitol; 1mM phenylmethylsulfonyl fluoride; 10-µg/mL leupeptin; 10-µg/mL aprotinin; 1mM Na3VO4; and 5mM NaF). Protein content was determined using a dye-binding microassay (Bio-Rad, Hercules, CA, USA), and 10- to 50-µg protein per lane was electrophoresed on 8%–12% sodium dodecyl sulfate polyacrylamide gels. Proteins were transferred onto Hybond ECL membranes (Amersham Pharmacia Biotech, Piscataway, NJ, USA), and immunoblotting was performed using the following antibodies: mouse anti-APEX1 (sc-17774), rabbit anti-Jagged1 (sc-8303), and mouse anti–α-tubulin (sc-23948) from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Four protein ladders (PM1001, SM0671, P8500, and P8502) were used for molecular weight determination (Thermo Fisher Scientific, Waltham, MA, USA). The blotted proteins were detected using an enhanced chemiluminescence detection system (iNtRON Biotechnology, Seongnam, Korea).
Immunohistochemistry
Chemosensitive and chemoresistant biliary cancer tissue samples were obtained from the Chosun University Department of Pathology tissue bank. Slides were stained with mouse anti-APEX1 (sc-17774; 1:500; Santa Cruz Biotechnology) or rabbit anti-Jagged1 (sc-8303; 1:200; Santa Cruz Biotechnology) antibodies. For immunohistochemistry, a biotinylated goat anti-mouse or rabbit antibody (Vector Laboratories, Burlingame, CA, USA) followed by horseradish peroxidase–conjugated streptavidin (Vector Laboratories) was used. After immuno-labeling, specimens were briefly counterstained with hematoxylin. Immunolabeled images were captured using an Olympus C-4040Z digital camera and an Olympus BX-50 microscope (Olympus Corp., Tokyo, Japan). Protein expression was scored in the nucleus for APEX1 and in the cytoplasmic membrane and cytoplasm for Jagged1. APEX1 and Jagged1 immunoreactivity was determined by scoring for staining intensity (0, none; 1, weak; 2; moderate; 3, strong) and percent positive cells (0, <5%; 1, 6%–25%; 2, 26%–50%; 3, 50%–75%; 4, >76%), and is expressed as the product of both scores.
Statistical analyses
Data in all experiments are represented as mean ± standard deviation. Statistical comparisons were carried out using two-tailed paired t-test. We considered P < 0.05 as significant. Analyses were carried out with Excel. Correlation between APEX1 expression and Jagged1 levels was assessed using a Pearson correlation test with a P-value; a P-value of 0.01 or less was considered statistically significant.
RESULTS
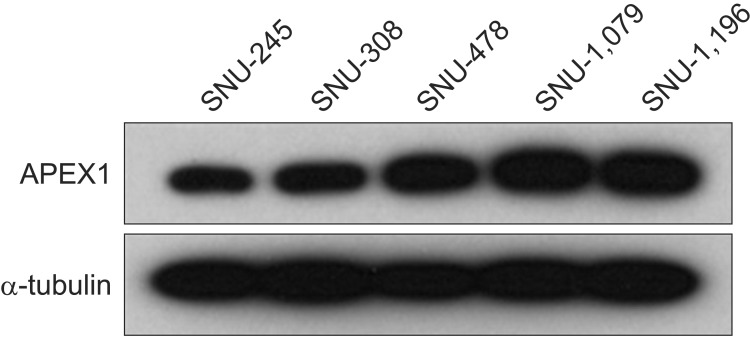
Western blot analysis of APEX1 expression in biliary cancer cell lines
First, we evaluated APEX1 expression in five biliary cancer cell lines, such as SNU-245, SNU-308, SNU-478, SNU-1079, and SNU-1196. Western blot analysis revealed that all of the biliary cancer cell lines exhibited high levels of APEX1 expression (Fig. 1).
Fig. 1. All biliary cancer cell lines showed apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) expression by western blot. APEX1 protein expression was detected by western blot analysis with α-tubulin as a loading control.
MTT assay for chemotherapeutic drugs (5 FU, gemcitabine, and cisplatin)
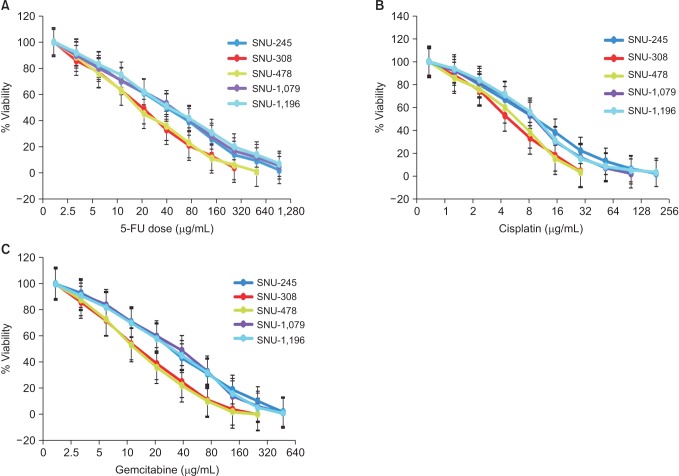
An MTT assay was performed to assess the sensitivity of the biliary cancer cell lines to 3 well-known effective chemotherapeutic agents: 5-FU, gemcitabine, and cisplatin (Fig. 2). Three of the cell lines (SNU-245, SNU-1079, and SNU-1196) were more resistant to all chemotherapeutic agents (5-FU, gemcitabine, and cisplatin) than the others (SNU-308, SNU-478). Additionally, the IC50 values of the three resistant cell lines were higher than those of the sensitive cell lines (Table 1). According to these results, the examined biliary cancer cell lines were divided into 2 groups: the group with relatively higher resistance (SNU-245, SNU-1079, and SNU-1196) and the more sensitive group (SNU-308 and SNU-478).
Fig. 2. MTT assay for chemotherapeutic drugs (A: 5-FU, B: cisplatin, C: gemcitabine) in biliary cancer cells. Cell plated in 96-well plate were treated cisplatin, 5-FU, or gemcitabine and the MTT assay was carried out on day three of the treatments. Result are shown as means ± standard deviation (n = 3). 5-FU, 5-fluorouracil; MTT, 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide.
Table 1. MTT assay for chemotherapeutic drugs (5-FU, gemcitabine, and cisplatin) in biliary cancer cells.
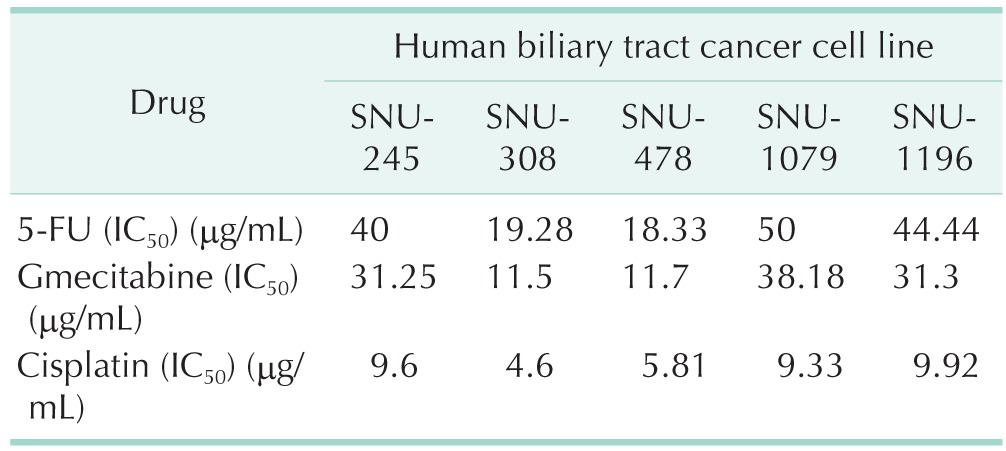
Drug concentrations which lead to a 50% inhibition of cell growth (IC50) were determined for each cell line using 3 chemotherapeutic drugs.
5-FU, 5-fluorouracil; MTT, 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide.
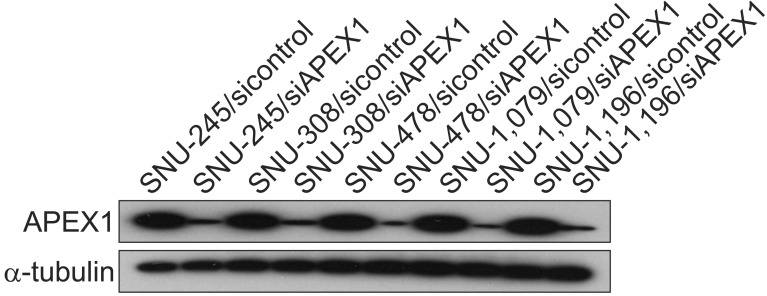
MTT assay after APEX1 knockdown
We next investigated the change in drug sensitivity of each cell line after APEX1 knockdown. APEX1 is believed to be involved in cisplatin chemoresistance by causing enhanced DNA repair. To perform these experiments, control siRNA or APEX1-specific siRNA were transfected into SNU-245, SNU-308, SNU-478, SNU-1079, and SNU-1196 cells. Western blot analysis showed that when APEX1 siRNA was transfected into biliary cancer cells, the endogenous APEX1 protein level was knocked down by 80% compared with the level in control siRNA-transfected cells (Fig. 3). After APEX1 knockdown, an MTT assay in the chemosensitive cell lines (SNU-308 and SNU-478) showed only a minimal decrease in IC50 (around 10%) for each chemotherapeutic agent; however, the chemoresistant group (SNU-245, SNU-1079, and SNU-1196) showed a greater decrease in IC50 (Table 2), and these results suggest that APEX1 is minimally related to chemoresistance in biliary cancer; however, that cell survival after chemotherapy (5-FU, gemcitabine, or cisplatin) showed greater improvement in the chemoresistant group after APEX1 knockdown suggests that some factor or pathway that is only present in these cell lines (SNU-245, SNU-1079, and SNU-1196) is affected by APEX1, leading to resistance to chemotherapeutic agents. Thus, our next step was to identify signaling molecules that may enhance resistance to chemotherapeutic agents.
Fig. 3. Western blot analysis of apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) expression in biliary cancer cell lines after APEX1 knockdown. SNU-245, SNU-308, SNU-478, SNU-1079, and SNU-1196 cells were transfected with control or APEX1-targeted siRNAs. Forty-eight hours after transfection, whole cell lysates were probed with antibodies specific for APEX1 and α-tubulin.
Table 2. APEX1-speciifc siRNA-transfected biliary cancer cells were treated with chemotherapeutic drugs (5-FU, gemcitabine, and cisplatin, and MTT assay was performed).
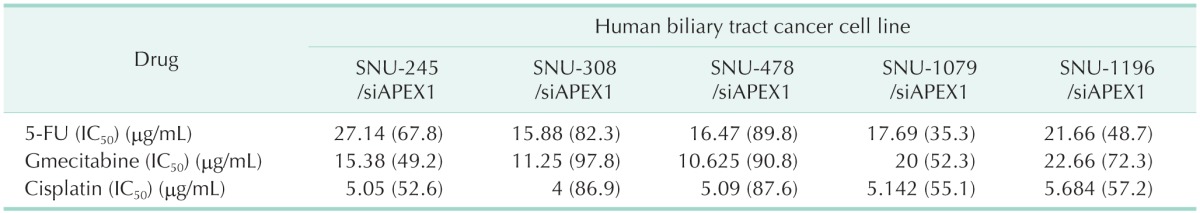
Values are presented as drug concentration (%).
Drug concentrations which lead to a 50% inhibition of cell growth (IC50) were determined for each cell line using 3 chemotherapeutic drugs.
APEX1, apurinic/apyrimidinic endodeoxyribonuclease1; 5-FU, 5-fluorouracil; MTT, 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide.
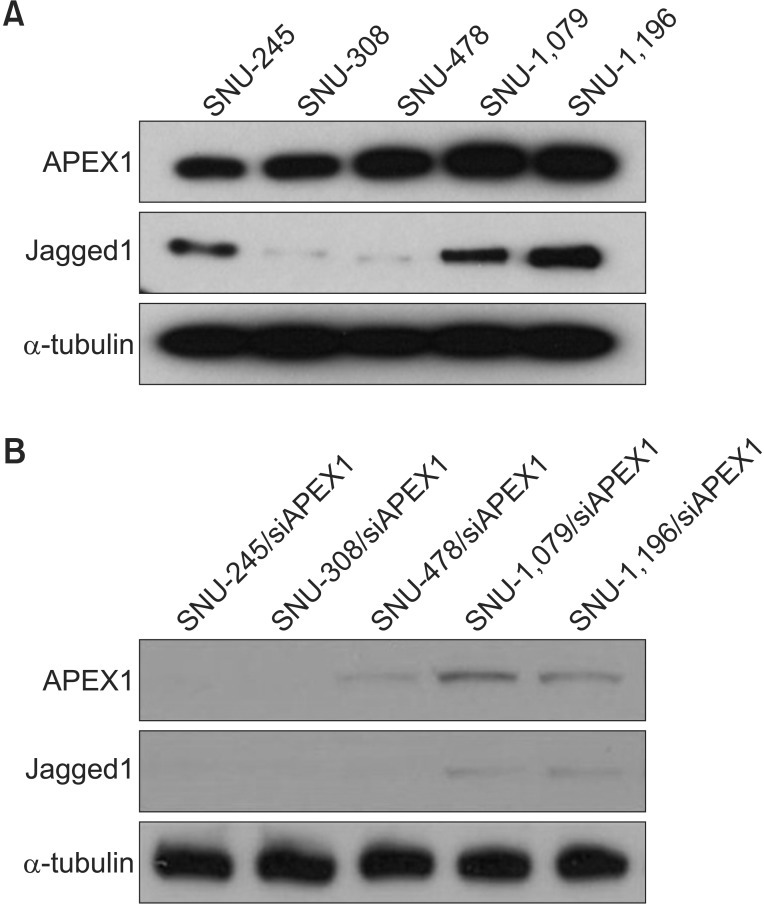
Western blot analysis of Jagged1 expression in biliary cancer cell lines
Recently, colon cancer progression was reported to be driven by APEX1-mediated upregulation of Jagged1/Notch activity, but there have been no reports on the association between APEX1 and Jagged1 in biliary cancer [11]. Given that biliary cells may belong to the gastrointestinal tract, we performed western blotting to analyze Jagged1 activity in biliary cancer cell lines, and surprisingly, we found that the chemoresistant group (SNU-245, SNU-1079, and SNU-1196) showed strong APEX1 and Jagged1 expression simultaneously, but the chemosensitive group (SNU-308 and SNU-478) showed only APEX1 expression (Fig. 4A), indicating that Jagged1 expression may be a poor response factor for chemotherapy. We next performed Western blot analysis of APEX1 and Jagged1 expression in biliary cancer cell lines after APEX1 knockdown. The result definitively showed decreased Jagged1 expression after APEX1 knockdown (Fig. 4B). These results suggest that Jagged1 activation by APEX1 is a chemoresistance factor for gemcitabine, 5-FU and cisplatin in biliary cancer.
Fig. 4. (A) All biliary cancer cell line showed apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) and Jagged1 expression by Western blot. APEX1 and Jagged1 protein expression was detected by western blot analysis with α-tubulin as a loading control. (B) Western blot analysis of APEX1 and Jagged1 expression in biliary cancer cell lines after APEX1 knockdown. Western blot of all biliary cancer cells treated with APEX1 siRNA. Samples were collected 48 hours after APEX1-siRNA treatment, and Western blot was done with APEX1 antibody and reproved with α-tubulin antibody as a loading control.
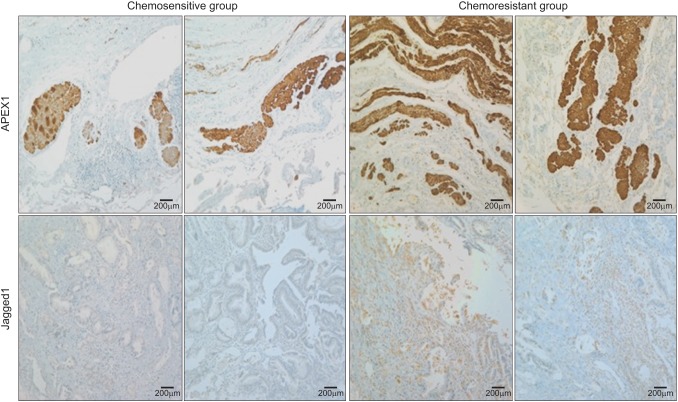
Immunohistochemistry of advanced biliary cancer patient tissues
We next directly assessed the clinical significant of APEX1 and Jagged1 in cancer tissues obtained from advanced biliary cancer patients. We aimed to investigate the clinical relationship between APEX1 and Jagged1 expression and response to chemotherapy among these patients. Biliary cancer is generally known to be unresponsive to chemotherapy, with a chemotherapeutic response of only approximately 20%.
This study was approved by ethics committee of Chosun University Hospital, and ten patients with advanced biliary cancer treated with chemotherapy were identified from the Chosun University Hospital registry. The ten patients consisted of 2 groups according to the initial chemotherapy response (chemoresponsive patients; partial response vs. chemorefractory patients; progressive disease). Chemotherapeutic regimens were all cisplatin-based combination regimens. The chemoresponsive group included four patients treated with gemcitabine plus cisplatin and one with 5-FU plus cisplatin; the chemorefractory group included three patients treated with gemcitabine plus cisplatin and two with 5-FU plus cisplatin.
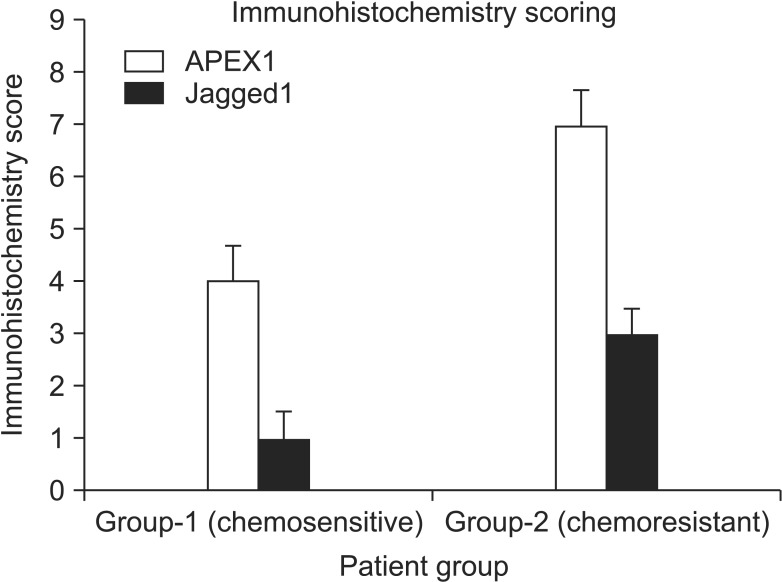
We performed immunohistochemistry on paraffin-embedded chemo native cancer tissues of all patients, with results determined by scoring for staining intensity (Fig. 5, Table 3). The results demonstrated that chemorefractory patients had higher scores (APEX1, 7; Jagged1, 3) than chemoresponsive patients (APEX1, 4; Jagged1, 1) (Fig. 6). These data indicate that coexpression of APEX1 and Jagged1 is poor prognostic factor for chemotherapeutic response in advanced biliary cancer.
Fig. 5. Immunohistochemistry of advanced biliary cancer patients. Correlation between apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) and Jagged1 expression in biliary cancer patients. APEX1 and Jagged1 proteins in biliary cancer patients are shown by immunohistochemistry with anti-APEX1 and anti-Jagged1 antibodies. Brown staining indicates positive APEX1 or Jagged1 staining (P < 0.01, Pearson correlation test. Scale bars, 200 µm).
Table 3. The characteristic of ten biliary cancer patients.
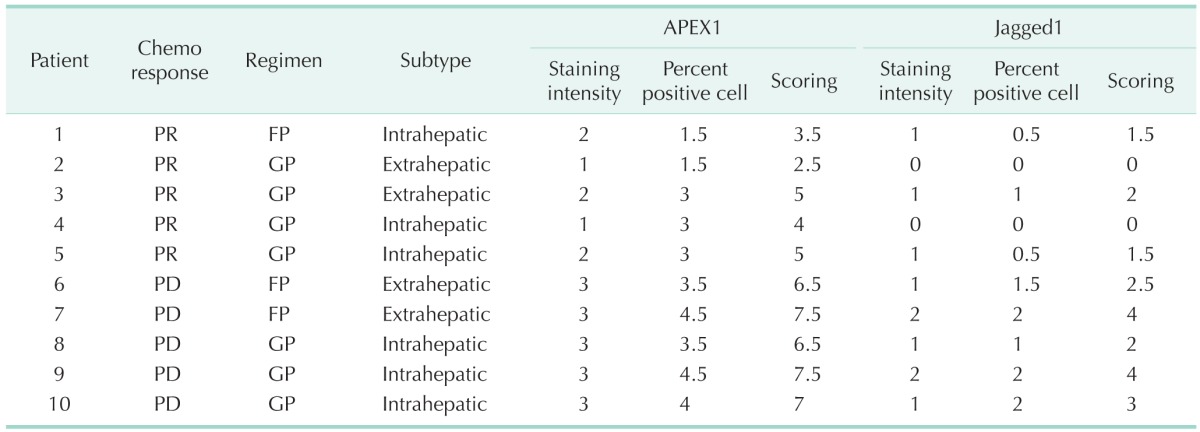
Apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) and Jagged1 expression levels assessed by immunohistochemistry scoring (see METHODS section). The 10 patients consisted of 2 groups according to the initial chemotherapy response (chemoresponsive patients; partial response [PR] vs. chemorefractory patients; progressive disease [PD]). FP; 5-FU plus cisplatin; GP, gemcitabine plus cisplatin.
Fig. 6. Immunohistochemistry scoring of advanced biliary cancer patients. Apurinic/apyrimidinic endodeoxyribonuclease1 (APEX1) and Jagged1 expression levels assessed by immunohistochemistry scoring (see METHODS section).
DISCUSSION
The only effective treatment for biliary cancer is surgical resection in the early stages. However, most cases are diagnosed only in locally advanced or metastatic stages and patients do not undergo surgery. Even if the patients undergo successful surgical resection, the recurrence rate of biliary cancer is very high. Furthermore, it is well known that biliary cancer is refractory to conventional chemotherapy. Therefore, the overall prognosis of biliary cancer patients is poor, with a 5-year survival rate of approximately 25%. Patients with unresectable biliary cancer generally survive for less than 12 months after diagnosis. However, most patients with unresectable or recurrent biliary cancer undergo palliative chemotherapy despite the tendency of biliary cancer to be refractory [1,10,12].
Since the 2000s, gemcitabine, cisplatin, and 5-FU have shown therapeutic efficacy in advanced biliary cancer; in particular, a gemcitabine plus cisplatin combination regimen has been the standard form of chemotherapy since the results of the ABC-02 trial were published in 2009 [1,3,4,5,6].
Chemotherapeutic practice in the field of oncology has changed drastically in the last decade with the introduction of targeted therapies. Therapies targeting receptors or signaling cascades associated with tumor growth or tumor growth suppression have improved chemotherapeutic responses and survival in cancer patients. This therapeutic option was developed by understanding the genetic profile and pathogenesis of specific cancers such as non-small cell lung cancer, colon cancer, and breast cancer. However, targeted therapy for biliary cancer has seen little progress, and no well-known markers for biliary cancer have been identified to date [10,11,12]. Therefore, our study aimed at investigating molecular factors (APEX1) for chemoresistance (especially cisplatin) in biliary cancer cells at first.
Many studies have focused only on gemcitabine as an effective chemotherapeutic drug for biliary cancer; however, in the ABC-02 trial, gemcitabine and cisplatin combination chemotherapy was shown to be better than gemcitabine therapy alone, prolonging the survival of patients by about 3.6 months. This result indicates that the role of cisplatin in biliary cancer is very important; therefore, firstly, we investigated the molecular mechanism underlying cisplatin chemoresistance in biliary cancer [6]. Cisplatin has been known to be a highly potent DNA-damaging chemotherapeutic agent for the past 30 years. Repair of DNA damage is important for maintaining genomic stability and enhancing cell survival. Therefore, decreasing DNA repair capabilities in cancer cells may increase chemotherapy-induced cytotoxicity. Moreover, the upregulation of DNA repair enzymes can induce resistance to chemotherapy, which would allow cancer cells to repair DNA and thus escape the toxic effects of chemotherapy [13]. One such DNA repair enzyme is APEX1. APEX1 is a multifunctional protein that is essential for BER. The relationship between APEX1 and chemoresistance (especially cisplatin) has been reported previously, however, no such studies have been conducted in biliary cancer cells [7,8,9]. The data from the present study elucidated the molecular mechanism of cisplatin chemoresistance in biliary cancer in some degree.
However, during the investigation, we found two rather unexpected results. One was that biliary cancer cell lines could be divided in 2 groups according to sensitivity to the evaluated chemotherapeutic agents (gemcitabine, cisplatin, and 5-FU). The other finding was that the chemoresistant group contained some factors or pathways responsible for resistance to chemotherapeutic agents, and that these pathways or factors were affected by APEX1. We further investigated this factor and found one molecule, Jagged1, which may be involved in the chemoresistance we observed in biliary cancer cell lines [11].
Jagged1 is one of five Notch receptor ligands expressed by mammalian cells. Jagged1-induced Notch activation plays a critical mechanistic role in various aspects of tumor biology, such as tumor growth through maintaining cancer stem cell populations, promoting cell survival, inhibiting apoptosis, and driving cell proliferation and metastasis. It affects not only cancer cells, but also tumor microenvironment components, and high expression of Notch-1 and its ligand Jagged1 is well-known as a poor prognostic factor in various cancers such as breast cancer, bladder cancer, leukemia, prostate cancer, and biliary cancer, too [14,15,16]. Moreover, it has recently been reported that Jagged1-stimulated Notch pathway activity is involved in chemoresistance [17,18]. However, no investigation on its role in chemoresistance in biliary cancer has been thus far undertaken, and no report has been made regarding the relationship between chemoresistance, Jagged1, and APEX1.
Although we demonstrated that Jagged1 is activated by APEX1, and that Jagged1 activation by APEX1 is a chemoresistance factor in biliary cancer, we need a smore research point. A direct proof to indicate that Jagged1 activation was driven by APEX1 needs to be searched for in future studies, in addition, the main pathway involving Notch, Hedgehog, Wnt, and Jagged1 for chemoresistance remains to be elucidated. The main Notch pathway among the various notch signaling pathways (1, 2, 3, 4) responsible for such chemoresistance should be further investigated, too. Finally, more cases clinical study should be evaluated for the cutoff level between chemosensitive and resistance, and more important molecular target between APEX1 and Jagged1 affecting survival benefit.
However, our results show that simultaneous expression of Jagged1 and APEX1 is generally associated with chemoresistance in biliary cancer, suggesting that APEX1 and Jagged1 are predictive of chemoresponse, and predictor may be an important tool to select a therapeutic strategy for neoadjuvant chemotherapy of borderline resectable biliary cancer patients. Furthermore, it may also be a potential therapeutic target for overcoming chemoresistance in advanced biliary cancer.
ACKNOWLEDGEMENTS
This study was supported by research fund from Chosun University, 2015. This work is supported by the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT, and Future Planning [NRF-2015R1A5A2009070].
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Khan SA, Davidson BR, Goldin RD, Heaton N, Karani J, Pereira SP, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: an update. Gut. 2012;61:1657–1669. doi: 10.1136/gutjnl-2011-301748. [DOI] [PubMed] [Google Scholar]
- 2.Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54:173–184. doi: 10.1002/hep.24351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glimelius B, Hoffman K, Sjoden PO, Jacobsson G, Sellstrom H, Enander LK, et al. Chemotherapy improves survival and quality of life in advanced pancreatic and biliary cancer. Ann Oncol. 1996;7:593–600. doi: 10.1093/oxfordjournals.annonc.a010676. [DOI] [PubMed] [Google Scholar]
- 4.Ducreux M, Van Cutsem E, Van Laethem JL, Gress TM, Jeziorski K, Rougier P, et al. A randomised phase II trial of weekly high-dose 5-fluorouracil with and without folinic acid and cisplatin in patients with advanced biliary tract carcinoma: results of the 40955 EORTC trial. Eur J Cancer. 2005;41:398–403. doi: 10.1016/j.ejca.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 5.Kornek GV, Schuell B, Laengle F, Gruenberger T, Penz M, Karall K, et al. Mitomycin C in combination with capecitabine or biweekly high-dose gemcitabine in patients with advanced biliary tract cancer: a randomised phase II trial. Ann Oncol. 2004;15:478–483. doi: 10.1093/annonc/mdh096. [DOI] [PubMed] [Google Scholar]
- 6.Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Wang J, Xiang D, Wang D, Xin X. Alterations in the expression of the apurinic/apyrimidinic endonuclease-1/redox factor-1 (APE1/Ref-1) in human ovarian cancer and indentification of the therapeutic potential of APE1/Ref-1 inhibitor. Int J Oncol. 2009;35:1069–1079. [PubMed] [Google Scholar]
- 8.Madhusudan S, Smart F, Shrimpton P, Parsons JL, Gardiner L, Houlbrook S, et al. Isolation of a small molecule inhibitor of DNA base excision repair. Nucleic Acids Res. 2005;33:4711–4724. doi: 10.1093/nar/gki781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fishel ML, Kelley MR. The DNA base excision repair protein Ape1/Ref-1 as a therapeutic and chemopreventive target. Mol Aspects Med. 2007;28:375–395. doi: 10.1016/j.mam.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Schweitzer N, Vogel A. Systemic therapy of cholangiocarcinoma: from chemotherapy to targeted therapies. Best Pract Res Clin Gastroenterol. 2015;29:345–353. doi: 10.1016/j.bpg.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Kim MH, Kim HB, Yoon SP, Lim SC, Cha MJ, Jeon YJ, et al. Colon cancer progression is driven by APEX1-mediated upregulation of Jagged. J Clin Invest. 2013 Jul 01; doi: 10.1172/JCI65521. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet. 2005;366:1303–1314. doi: 10.1016/S0140-6736(05)67530-7. [DOI] [PubMed] [Google Scholar]
- 13.Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014;740:364–378. doi: 10.1016/j.ejphar.2014.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Penton AL, Leonard LD, Spinner NB. Notch signaling in human development and disease. Semin Cell Dev Biol. 2012;23:450–457. doi: 10.1016/j.semcdb.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steg AD, Katre AA, Goodman B, Han HD, Nick AM, Stone RL, et al. Targeting the notch ligand JAGGED1 in both tumor cells and stroma in ovarian cancer. Clin Cancer Res. 2011;17:5674–5685. doi: 10.1158/1078-0432.CCR-11-0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoon HA, Noh MH, Kim BG, Han JS, Jang JS, Choi SR, et al. Clinicopathological significance of altered Notch signaling in extrahepatic cholangiocarcinoma and gallbladder carcinoma. World J Gastroenterol. 2011;17:4023–4030. doi: 10.3748/wjg.v17.i35.4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li D, Masiero M, Banham AH, Harris AL. The notch ligand JAGGED1 as a target for anti-tumor therapy. Front Oncol. 2014;4:254. doi: 10.3389/fonc.2014.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Z, Li Y, Ahmad A, Azmi AS, Banerjee S, Kong D, et al. Targeting Notch signaling pathway to overcome drug resistance for cancer therapy. Biochim Biophys Acta. 2010;1806:258–267. doi: 10.1016/j.bbcan.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]