Abstract
We examined evidence on whether mobile health (mHealth) tools, including Interactive Voice Response (IVR) calls, short message service (SMS) or text messaging, and smartphones, can improve lifestyle behaviors and management related to cardiovascular diseases throughout the world. We conducted a state-of-the-art review and literature synthesis of peer-reviewed and grey literature published since 2004. The review prioritized randomized trials and studies focused on cardiovascular diseases and risk factors, but included other reports when they represented the best available evidence. The search emphasized reports on the potential benefits of mHealth interventions implemented in low- and middle-income countries (LMICs). IVR and SMS interventions can improve cardiovascular preventive care in developed countries by addressing risk factors including weight, smoking, and physical activity. IVR and SMS-based interventions for cardiovascular disease management also have shown benefits with respect to hypertension management, hospital readmissions, and diabetic glycemic control. Multi-modal interventions including web-based communication with clinicians and mHealth-enabled clinical monitoring with feedback also have shown benefits. The evidence regarding the potential benefits of interventions using smartphones and social media is still developing. Studies of mHealth interventions have been conducted in more than 30 LMICs, and evidence to date suggests that programs are feasible and may improve medication adherence and disease outcomes. Emerging evidence suggests that mHealth interventions may improve cardiovascular-related lifestyle behaviors and disease management. Next generation mHealth programs developed worldwide should be based on evidence-based behavioral theories and incorporate advances in artificial intelligence for adapting systems automatically to patients’ unique and changing needs.
Keywords: Mobile health, telehealth, care management, developing countries, preventive care, informatics
Introduction
Self-Management Support for Patients with Cardiovascular Disease
Cardiovascular disease is the leading cause of death and disease globally, responsible for 30% of all deaths worldwide.1 Improved cardiovascular outcomes depend largely on how well affected people manage these conditions between face-to-face office visits with their health care providers.2 Self-management is often challenging due to the complexity of patients’ medication regimens; the importance of self-monitoring for signs of emerging complications; and the need for lifestyle behavior changes including physical activity, healthy diet, smoking cessation, and weight loss. Especially in resource-constrained settings, health care providers have limited opportunity to interact directly with patients between in-person encounters. The effective use of patient-centered health communication technology thus represents a promising approach to extend the reach of health systems in order to provide ongoing support.
Limitations of Health Systems in Low- and Middle-Income Countries
Providing patients with the tools to take an active, participatory role in their cardiovascular disease prevention and management is particularly important in low and middle-income countries (LMICs). Patients with chronic diseases in less developed countries often face out-of-pocket healthcare costs that are prohibitive given limited household budgets.3 A WHO survey of more than 256,000 respondents in 70 countries found that healthcare accounted for 13%–32% of household expenditures, and cost barriers were a frequently cited reason for inadequate chronic illness care.4 Even when patients can afford it, health services in LMICs for lifestyle behavior change and disease management are often unavailable or of low quality.5 According to the WHO, the global deficit of health professionals exceeds 4 million, with severe shortages in 57 countries.6,7 The number of health professionals who leave LMICs to practice elsewhere has never been higher,8 and providers who stay in LMICs are often poorly trained for the growing challenge of preventing and managing cardiovascular health problems.9
Mobile Health as a Partial Solution
Innovations in mobile health technology may help to address the barriers to cardiovascular disease prevention and management.10,11 There are more than six billion mobile phone users worldwide with almost three quarters living in LMICs.12 The explosion in cell phone use represents an important resource for lifestyle behavior change and disease management, because abundant evidence has demonstrated that telephone follow-up improves the quality and outcomes of care.13–15 While most trials of telephone care have been conducted in high income countries (HICs), investigators in Chile reported that low-income diabetes patients randomized to telephone nurse counseling had better glycemic control than patients receiving usual care,16 and post-discharge telephone support for heart failure patients in Argentina significantly reduced readmission rates relative to randomized controls.17
Unfortunately, telephone care management programs often fail to demonstrate the cost savings that decision-makers look for in order to justify the investment in human capital. In a review of 15 randomized care management trials including more than 18,000 chronically-ill patients, investigators found that only two studies showed significant reductions in health care costs.18 Other studies including data on hundreds of thousands of patients receiving care management with telephone follow-up also have found that improving quality through care management while reducing costs is extremely difficult.19,20 To meet the dual goals of improving cardiovascular outcomes while minimizing the costs associated with clinician follow-up, health systems and payers increasingly look to mobile health technologies that can deliver health information and improve patient monitoring between visits, a field now widely known as mobile health or “mHealth” (a specialized offshoot of the more established field of health informatics known as “eHealth”). Prior reviews10,11,14,15,21–32 report generally positive impacts of mHealth on chronic disease treatment and outcomes, although significant barriers to implementation remain in LMICs.22,33
mHealth interventions take a variety of forms, each with its own benefits and limitations in terms of the specific modality’s reach and the richness of the information exchange (see Table 1 and Figure 1). “Interactive Voice Response” or IVR calls allow patients to receive information and communicate with others asynchronously using their mobile or landline telephone. Using IVR, patients interact with a structured series of recorded message components and respond to queries using their touch-tone keypad or voice-recognition technology. Based on their responses, patients can receive recorded messages tailored to their individual needs. Clinicians can receive automated updates based on patients’ responses during IVR calls, along with structured feedback about how to improve disease management. Patient-directed short messaging service (SMS) or text messaging interventions are designed to improve disease management primarily through reminders that improve adherence to behavioral goals such as medication taking, and through educational or supportive messages that increase motivation for changes in lifestyle behaviors or self-care. SMS messages can be triggered automatically or by clinicians, and some services use bi-directional communication with patients to increase program engagement and service impact. More recent advances in mHealth include smartphones and other mobile communication tools enabled with graphical screens, video, audio, and Internet access. An advantage of smartphones is that structured information from patients can be collected through a touchscreen or voice recognition system, thereby allowing more accurate and extensive patient reporting than is possible with SMS. Global positioning systems and physiologic sensors can be added to further tailor health communication and monitor patients’ status. The widespread and growing use of social media such as social network sites, blogs, wikis, Twitter chats, photo/video sharing services, and virtual worlds represent additional opportunities for engaging patients via their smartphone. In particular, new social media can extend the reach and impact of social networks, enable sharing of knowledge and information, and integrate real-time personal health data to leverage peer support.
Table 1.
Advantages and Disadvantages of Three Mobile Health Technologies for Improving Cardiovascular Disease Prevention and Management
| Automated Calls or IVR | Text Messaging or SMS | Smartphones and Online Tools | |
|---|---|---|---|
| Cost to the Patient | Some patients using cell phones must pay minute charges to receive a call. | Some patients using cell phones must pay to respond to text messages. | Smartphones and data plans are prohibitively expensive for some patients, especially in LMICs. |
| Literacy Requirements | Literacy not required since information is conveyed aurally. | Some reading is required although texts can be written at a low literacy level. | Some information is text, although graphics, audio, and video can be used. |
| Complexity of the Interaction | Extensive dialogues are possible. Longer messages may be cumbersome and patients cannot review information at a later time. | Only short, simple messages can be sent via SMS with very little patient-response data or dialogue. | Smartphones can send complex multi-media messages and collect detailed information via forms. |
| Other Patient Requirements | Must have good hearing and be able to respond to questions via a touch-tone phone. | May need to be able to send texts, with fine motor control and good vision. | Must be able to navigate a touch screen. Some systems also require texting. |
| Potential Reach | Can be used with all standard cell phones as well as land-line phones. | Can be used with all standard cell phones. | Limited to patients who can access and use a Smartphone. Many functions also require Internet access. |
| Evidence for Impact | Multiple studies show impacts on behaviors and some health outcomes. | Multiple studies show impacts on behaviors and some health outcomes. | Evidence base is weak for impacts on behaviors and outcomes. |
IVR: Interactive voice response/automated calls; SMS: Short messaging service or text messaging; LMIC: Low- and middle-income countries.
Figure 1. Legend. Examples of mHealth Services Targeting Three Levels of Cardiovascular Disease Prevention and Management.
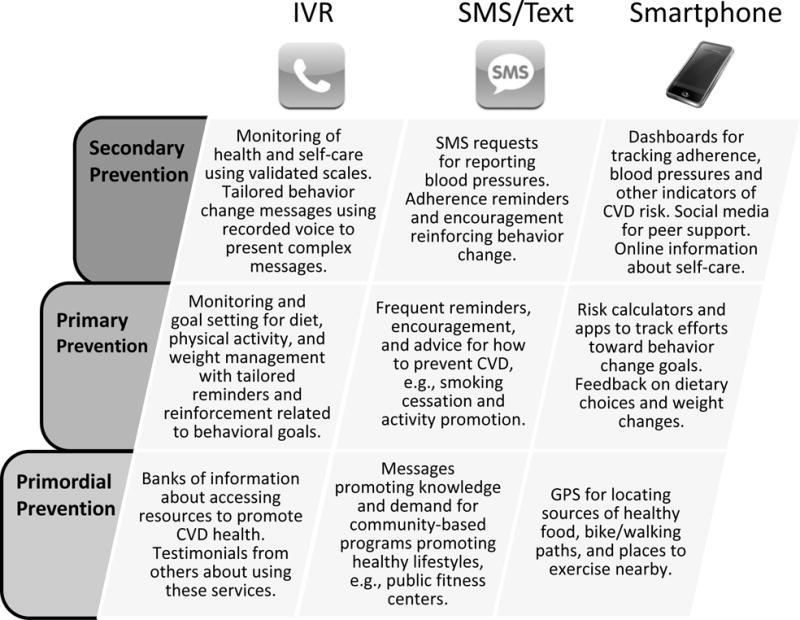
IVR: Interactive voice response/automated calls; SMS: short messaging service/text messaging; CVD: cardiovascular disease.
Scope of the Review
We conducted a state-of-the-art review and synthesis34 of the evidence regarding the potential benefits of mHealth interventions for improving the quality and outcomes of services targeting lifestyle behavior change and management of cardiovascular diseases. Key innovations are described for interventions using IVR and SMS that are accessible from almost any cell phone, as well as interventions using web-enabled communication tools such as smartphones. Given the large volume of literature in this field and limits on the length of the review, studies of interventions using specialized devices (e.g., electronic scales for assessing patients’ weight or automatically-uploading blood pressure monitors) were not included. While much less research has been conducted on the use of social networking tools to address the needs of patients with chronic diseases, we also report on the use of those approaches when evaluations have been reported in the literature. Our review of the evidence focused primarily on randomized trials, although other studies were included when they represented the strongest evidence available for an important topic. Most research on mHealth has been conducted in a small number of HICs; however, we highlight studies that have been conducted in less represented regions of the world, including LMICs.
Methods
Literature Search Methods
Using an accepted typology for reviews, we conducted a state-of-the-art review and literature synthesis. These reviews are appropriate for situations such as this one in which the purpose is to identify future areas of research in a new and rapidly evolving field of evidence.34 The literature search was conducted in March 2014 by the informationists (GKR and WT) to identify scholarly research and industry reports related to eHealth and social media interventions for cardiovascular disease lifestyle behavior change and management. A broad net was cast in order to find potentially relevant literature that could be applicable to cardiovascular disease. Discrete systematic searches were conducted in the Medline, Scopus, Embase, Global Health (CABI), and Health Policy Reference Center literature databases. Separate searches were also run in each database to identify mHealth interventions in the areas of infectious disease management and maternal health services in order to identify effective interventions that could be adapted and applied to populations affected by cardiovascular diseases. Searches used controlled vocabulary terminology and keywords representing search concepts in mHealth in LMICS, including: mHealth and social networking; cardiovascular disease and eHealth programs; eHealth strategies in vector-borne and infectious disease management; and use of eHealth/mHealth in maternal and reproductive health services. A sample Medline search strategy using the Ovid interface has been included as an Online Supplement. Additional search details are available from the authors upon request.
In order to identify “grey” or potentially unpublished literature, general web searches and searches of business resources for mobile industry-specific reports and reports from global public health organizations including the World Health Organization were conducted. Searches were limited to articles published in English in the last 10 years. Hand searching and the initial appraisal of search retrieval was conducted by the informationists, with final screening and assessment for relevance conducted by other authors. A secondary subsearch was limited to English-language randomized controlled trials (RCTs) and clinical studies published in the last 5 years. Citations of identified articles were hand-searched for relevant references.
Results
mHealth Interventions for Lifestyle Behavior Change (Table 2)
Table 2.
Trials Using mHealth Interventions for Lifestyle Behavior Change
| Authors (Year) | Sample Characteristics | Country | mHealth tool | Intervention Components | Design | Results |
|---|---|---|---|---|---|---|
| Participants Identified with CVD or Diabetes | ||||||
| Chow et al. (2012)35 | 720 adults with coronary artery disease | Australia | SMS (4 messages per week for 24 weeks) | Messages to reduce CVD risk factors: motivation to quit smoking, follow a healthy diet, and exercise | RCT: SMS versus usual care 6 month follow-up | Ongoing trial |
| Handley et al. (2008)36 | 226 adults with type 2 diabetes | USA | Weekly IVR | IVR patient education and nurse phone counseling | RCT: IVR versus usual care 12 month follow-up | Per-patient cost of $65K per QALY, 14% increase in the proportion of patients achieving vigorous activity relative to controls |
| Migneault et al. (2012)37 | 337 urban African-American adults with hypertension | USA | 32 weekly IVR counseling sessions | Patient reported health information collected on study-issued home measurement devices with motivational and behavior-change messages targeting medication adherence, physical activity, and diet | RCT: IVR versus usual care 8 month follow-up | Significant improvement in overall diet quality score (p<0.03), fiber intake (p<0.02), and energy expenditure (p=0.02) in the intervention group; no significant differences in medication adherence |
| Newton et al. (2009)38 | 78 adolescents from 4 regional diabetes services | New Zealand | Weekly SMS messages | Motivational reminder messages to wear a pedometer and be active | RCT: SMS versus usual care 12 week follow-up | No improvement in physical activity |
| Nolan et al. (2011)39 | 680 adults at high risk of CVD or with CVD diagnoses | Canada | 6 weekly 1-hour group teleconferences with lifestyle counseling sessions | Baseline advice & education for both groups plus 6 weekly 1-hour teleconference lifestyle counseling sessions | RCT: teleconferencing on lifestyle versus active control (risk factor feedback, brief advice, handouts) 6 month follow-up | Significant improvements in exercise and diet in teleconference group (p<0.001) and in systolic and diastolic BP relative to control (p<0.001) |
| Reid et al. (2007)40 | 99 adult smokers recently hospitalized with CVD | Canada | IVR post-hospital discharge calls on days 3, 14, and 30 | Questions about smoking status, confidence in staying smoke-free, use of pharmacotherapy, and self-help information with feedback to a nurse who set up phone counseling sessions for those reporting smoking-abstinence problems | RCT: IVR versus usual care 12 month follow-up | Greater proportion abstinent (odds ratio 2.34, 95% CI: 0.92–5.92; p=0.07) |
| Wong et al. (2013)41 | 105 professional drivers with pre-diabetes | Hong Kong | SMS 3 times per week for 3 months, then weekly, then monthly | Messages regarding diabetes knowledge and lifestyle modification | RCT: SMS versus usual care 24 month follow-up | Risk of DM onset 5.6% versus 16% at 12 months (RR=.35; 95% CI: .10, 1.24) but non-significant results at 24 months |
| Other Participants | ||||||
| Appel et al. (2011)42 | 415 obese adults with at least one cardiovascular risk factor | USA | Weekly website learning modules | Website learning modules (self-monitoring weight, calorie intake, exercise) with monthly e-mail messages summarizing progress | RCT: remote weight loss support, versus remote support plus in-person support, versus self-directed behavior change control group 24 month follow-up | Greater weight loss at 24 months with remote support (−4.6 kg) and remote plus in-person support (−5.1 kg) compared to control (−0.8kg, p<0.001) |
| de Niet et al. (2012)43 | 141 overweight or obese children | Nether-lands | Weekly SMS messages | Patient-reported data on exercise & diet with tailored behavior-change feedback | RCT: SMS versus usual care 12 month follow-up | No improvement in weight, eating behavior, or wellbeing |
| Estabrooks et al. (2009)44 | 22 parent-child dyads with overweight children | USA | 10 weekly IVR counseling sessions | Tailored messages regarding changes in home environment to promote activity and healthy eating | RCT: IVR versus individual workbook education versus group counseling 12 month follow-up | Greater improvement in child BMI in the IVR group than the other two groups (p<0.01) |
| Free et al. (2011)45 | 5800 adult smokers willing to make a quit attempt | United Kingdom | SMS messages (5 per day first 5 weeks, 3 per day last 26 weeks) | Motivational and behavior-change messages | RCT: SMS messages versus SMS attention control 6 month follow-up | Increase in biochemically-confirmed quit rates (10.7% versus 4.9%; p<.0001) |
| King et al. (2014)46 | 127 inactive midlife and older adults | USA | IVR counseling sessions (roughly 15 delivered over a year) | Instructional sessions emphasizing cognitive and behavioral skills, based on current stage of motivational readiness to change, for moderate-intensity physical activity adoption | RCT: IVR versus human counseling 18 month follow-up | No difference in moderate-to-vigorous physical activity levels or percentage meeting national physical activity guidelines |
| Norman et al. (2013)47 | 52 overweight or obese adults | USA | 2–5 SMS per day, with ability to tailor number and time of messages | Diet and physical activity messages (some were interactive) providing tips, suggestions, prompts, and reminders for improved weight management behaviors | RCT: SMS versus usual care 4 month follow-up | Significant improvements in fruit/vegetable intake, eating behavior scores (all p’s<0.05); weight loss 5.4 lbs compared to 1.4 in controls (p<0.05) |
| Park et al. (2012)48 | 67 post-menopausal women with abdominal obesity | South Korea | 3 SMS messages per week, 3rd message also sent via internet | Participants posted self-measured waist circumference, body weight, blood pressure, plus info about diet and exercise to website. SMS and internet messages to participants included recommendations on diet and exercise based on website postings. | Quasi-experiment with matched controls 12 week follow-up | Significantly greater improvement in waist circumference, body weight, blood pressure, total cholesterol, and LDL-C (all p’s <0.006) |
| Shapiro et al. (2012)49 | 170 overweight or obese adults | USA | SMS and MMS sent 4 times per day | Behavior change strategies targeting weight loss behaviors utilizing tips, motivational messages, requesting daily step counts and weekly weights | RCT: SMS with monthly e-newsletters versus e-newsletters alone 12 month follow-up | No difference in weight loss; SMS adherence associated with improved weight-related behaviors, increased pedometer-measured physical activity and other outcomes |
| Turner-McGrievy et al. (2011)50 | 96 overweight adults | USA | Podcasts and daily tweets delivered via mobile-devices | Both groups received 2 podcasts per week, Podcast+Mobile group instructed to interact with counselors and other participants via Twitter | RCT: podcast+Twitter versus podcast alone 6 month follow-up | No difference in weight loss |
Abbreviations: BMI Body Mass Index, BP Blood Pressure, CVD Cardiovascular Disease, DM Diabetes Mellitus, IVR Interactive Voice Response, LDL-C Low-Density Lipoprotein Cholesterol, MMS Multimedia Messaging Service, QALYs Quality-Adjusted Life Years, RCT Randomized Controlled Trial, SMS Short Message Service
Interactive Voice Response
Trials conducted in HICs have shown that IVR-based interventions can be effective in promoting: physical activity, improved dietary behavior, and smoking cessation.37,39,40,46 A trial of 337 hypertensive African Americans found that 32 weekly IVR calls improved overall dietary quality and energy expenditures relative to controls who also received a resource manual and a 20-minute in-person health education session focused on lifestyle behaviors.37 A study of an IVR-delivered intervention focused on family goal setting and changes in the home environment showed improvements in obese children’s level of physical activity, dietary behaviors, and body mass index.44 In a diverse low-income sample of diabetes patients, investigators found that an IVR service coupled with nurse care management achieved physical activity objectives at modest cost.36
Short-Message Service (SMS) or Text Messaging
With 5800 participants, the txt2stop trial sought to improve smoking cessation rates in the UK through a series of motivational messages.45 Patients were randomized to receive motivational SMS messages or messages unrelated to smoking. Txt2stop more than doubled biochemically-confirmed quit rates at six months relative to controls. Studies of SMS interventions focused on promoting a more healthy diet, weight loss, and physical activity in HICs have shown mixed results. One US trial using daily SMS messages focused on tailored dietary goal setting and showed significant improvements at four months in eating behavior and body weight.47 However, an SMS intervention incorporating pedometer step-count feedback among adolescents with diabetes did not increase physical activity.38 A trial focusing on promoting weight maintenance after a three month behavioral weight loss program through bi-directional and tailored SMS messages found no overall benefit over the subsequent nine months in weight, eating behavior, or psychological mediators of behavior change.43 Despite relatively high adherence among adult participants in an interactive and personalized weight management program, investigators found no between-group difference at 6 and 12 months in weight when comparing groups receiving SMS messages versus a monthly e-newsletter. However, SMS-group participation did increase users’ pedometer-measured physical activity levels, and greater activity and text messaging adherence were associated with greater weight loss.49 Research currently underway may further elucidate the potential of SMS for promoting meaningful lifestyle behavior changes that are important for cardiovascular risk reduction.35
Studies including SMS interventions have been conducted in over 30 countries, including several LMICs.24–26,37,51 A trial conducted in Hong Kong found that SMS messages focused on diabetes-related lifestyle modification reduced rates of progression from pre-diabetes to diabetes over 12 months.41 Many mHealth studies in LMICs have focused on HIV/AIDS; two large randomized trials in Kenya found that SMS reminders improved adherence to antiretroviral therapy, and one trial also reported reductions in viral load among patients receiving SMS adherence reminders relative to randomized controls.52,53 (See Online Supplement Table 1 for a summary of HIV/AIDS trials.52–56)
Other mHealth Approaches
Using multiple mHealth communication modalities together may improve their impact on cardiovascular disease-related lifestyle behaviors. For example, a quasi-experimental study in Korea evaluated a combined SMS plus Internet intervention among overweight and obese women and demonstrated significant reductions in waist circumference, body weight, total cholesterol, and low-density lipoprotein-cholesterol.48 In another trial, investigators found that remote weight-loss support using a combination of telephone, Internet, and email resulted in improvements in weight at 24 months comparable to what was achieved with an in-person weight loss intervention.42 Especially because of their widespread use among younger adults, social media technologies including podcasts, “apps” and Twitter represent promising channels for communicating about cardiovascular disease prevention. In one trial, overweight adults were randomized to multiple motivational podcasts per week or podcasts plus additional behavior change support via a specialized “app” on users’ smartphone and interaction via Twitter with behavioral counselors.50 While the enhanced communication group was more engaged with online health information resources, there was no incremental benefit in weight loss at six months relative to participants receiving podcasts alone.
mHealth Interventions for Cardiovascular Disease Management (Table 3)
Table 3.
Trials Using mHealth Interventions for Cardiovascular Disease Management
| Authors (Year) | SampleCharacteristics | Country | mHealth tool | Intervention Components | Design | Results |
|---|---|---|---|---|---|---|
| Participants Identified with Hypertension | ||||||
| Contreras et al. (2004)57 | 67 adults with hypertension | Spain | Twice per week SMS | Information and adherence reminders | Cluster RCT: SMS versus usual care 6 month follow-up | No significant differences in adherence to HTN therapy |
| Friedman et al. (1996)58 | 267 adults with hypertension | USA | Weekly patient-initiated IVR calls | IVR-reported BP, medication understanding, adherence, and symptoms; IVR provided education and motivation and transmitted patient reports to provider | RCT: IVR versus usual care 6 month follow-up | Significantly improved medication adherence (17.7% IVR adherence compared to 11.7% in controls, p=0.03), BP improved more in IVR group if medication adherence improved (DBP mean decrease of 5.5mmHg compared to 0.6, p=0.03) |
| Magid et al. (2011)59 | 283 adults with hypertension taking <=4 antihypertensive meds | USA | Weekly IVR | Self-reported home BP monitoring with pharmacist follow-up | RCT: IVR versus usual care 6 month follow-up | Systolic BP reductions significantly greater in intervention group (−13.1 mmHg compared to −7.1 mmHg, p=.006). |
| Margolis et al. (2013)60 | 450 hypertensive adults with uncontrolled blood pressure | USA | BP transmitted 6 times per week via modem to Tele-monitoring (TM) website | Home blood pressure telemonitoring with BP readings transmitted to pharmacist for medication adjustment | Randomized two-group cluster: TM versus usual care 12 month follow-up | Significantly more TM patients with controlled BP at follow-up (71.8% compared to 45.2% in controls, p<.001) |
| Piette et al. (2012)61 | 200 Spanish-speaking adults with systolic blood pressure >=140 mmHg (non-diabetics) or >=130 mmHg (diabetics) | Honduras Mexico | Weekly IVR | Weekly automated monitoring and behavior-change calls plus home blood pressure monitoring | RCT: IVR versus usual care 6 week follow-up | IVR significantly improved depressive symptoms, medication problems, general health, and satisfaction with care (p<=0.004), systolic BP 4.2 mmHg lower (p=0.09), improved systolic BP among patients with low literacy (−8.8 mmHg, p=0.002) |
| Participants Identified with Diabetes | ||||||
| Arora et al. (2014)62 | 128 adults with poorly controlled diabetes | USA | Daily SMS messages | Education and motivational texts plus reminders; trivia questions with answers delivered 1 hour later | RCT: SMS versus usual care 6 month follow-up | No significant difference in HbA1c improvement, although SMS group improved in medication adherence and emergency department use relative to controls |
| Homko et al. (2012)63 | 80 women at least 33 weeks gestation with gestational diabetes mellitus | USA | Up to 3 IVR reminders (a day apart) | Asynchronous 2-way communication between patients and providers plus automated patient reminders to transmit health data to providers | RCT: IVR versus usual care, duration from enrollment to delivery: average 2 months | No improvement in maternal glucose control or infant birth weight |
| Lorig et al. (2008)64 | 533 Spanish-speaking adults with diabetes | USA | Monthly IVR | IVR reinforcement calls to patients participating in a 6-week community-based peer-led program of self-management support | RCT: IVR versus usual care 18 month follow-up | Increases in glucose monitoring for patients receiving IVR (p=0.001) but no improvement in A1c, symptoms, or other outcomes |
| Nundy et al. (2014)65 | 67 adults with type 1 or type 2 diabetes | USA | 2–6 SMS messages per day | Messages provided self-management support with approximately monthly nurse calls and facilitated team-based care | Quasi-experiment with health plan members who were not enrolled serving as controls | Pre-post improvement in glycemic control (p=0.01, no glycemic change in controls), costs decreased in both groups pre/post (8.8%, p=0.02) |
| Piette et al. (2000)66,67 | 248 adults with diabetes (English or Spanish-speaking) | USA | Bi-weekly IVR | IVR behavior and symptom assessment with tailored patient feedback and telephone follow-up by a nurse care manager | RCT: IVR versus usual care 12 month follow-up | IVR increased proportion of patients with normal HbA1c by 9% (p=0.04), decreased serum glucose by 41mg/dL (p=0.002), decreased depressive symptoms and sick days (both p<0.03) |
| Piette et al. (2001)68 | 272 VA diabetes patients on hypoglycemic medication | USA | Weekly IVR | IVR assessment and self-care education with follow-up by a nurse care manager | RCT: IVR versus usual care 12 month follow-up | Increased frequency of patient monitoring of blood glucose (p=0.05) and feet inspection (p=0.05) |
| Piette et al. (2011)69 | 85 Spanish-speaking adults with diabetes | Honduras | Weekly IVR | Weekly self-management support calls with concerning patient reports forwarded to participants’ clinical team | Single-group, pre-post study with six-week follow-up | HbA1c improved from 10% at baseline to 8.9% at FU (p<0.01). High intervention satisfaction and participation in IVR calls, and improved perceived health |
| Quinn et al. (2008)70 | 32 adults with type 2 diabetes | USA | Monthly cell phone transmission via WellDoc | Cell phone software delivered real-time feedback on HbA1c levels; both groups received blood glucose monitors | RCT: Cell phone-delivered feedback versus usual care 3 month follow-up | Significant improvement in HbA1c (decrease of 2.03% compared to 0.68% in controls, p<0.02) |
| Quinn et al. (2011)71 | 126 adults with type 2 diabetes from 26 primary care practices | USA | Mobile coaching and patient/provider web portals | Automated medication mgmt. and lifestyle behavior messages in response to patient-reported blood glucose values with quarterly reports to providers | Cluster-randomized trial: 3 stepped treatment groups versus usual care 12 month follow-up | Significantly greater improvement in HbA1c in maximal treatment group at follow-up (1.9% compared to 0.7% in controls, p=0.001) |
| Schillinger et al. (2008)72 | 339 English-, Spanish-, or Cantonese-speaking adults with diabetes | USA | Weekly IVR | Evaluating the reach of self-management support strategies in two intervention groups: those receiving IVR and those in the monthly Group Medical Visit (GMV) group | Effectiveness study within RCT: IVR or GMV versus usual care 9 month follow-up | IVR arm yielded higher engagement, especially among those with limited English and literacy, than the group medical visit arm (93.8% IVR compared to 69.6% GMV) |
| Simon et al. (2010)73 | 232 adults with diabetes overdue for diabetes-related screening | USA | 3 IVR calls | IVR reminders to encourage dilated eye exams and lab tests, with offer of token gifts | RCT: IVR versus usual care 300 day follow-up | No difference in time to completion of eye exams, or testing of A1C, LDL, or microalbumin |
| Williams et al. (2012)74 | 120 adults with type 2 diabetes and HbA1c >=7.5% | Australia | Weekly IVR call-in | Assessments of patients’ health and self-care with tailored feedback; email alerts sent to study team if any concerning issues reported during the call | RCT: IVR versus usual care 6 month follow-up | Significantly improved HbA1c (IVR: 8.7% to 7.9%; controls: 8.9% to 8.7%, p=0.002); relative improvement in mental HRQL (p=0.007) |
| Participants Identified with Other/Multiple Cardiovascular Risks | ||||||
| Boriani et al. (2013)75 | 148 adults with heart failure and implanted CRT-D devices | France, Hungary, Israel, Italy, Spain, Switzer-land | Remote monitoring with alerts triggered by device | Remote follow-up and wireless automatic alerts to clinic nurses or physicians for lung fluid overload | RCT: Remote monitoring versus usual care 12 month follow-up | Significantly shorter delay in clinical FU (2 days compared to 29 days in control group, p=.004) and significantly reduced inpatient stays (p<.001) |
| Glozier et al. (2013)76 | 487 adults with depression and CVD | Australia | Weekly Internet-based CBT | Internet-based CBT (E-Couch) compared to online attention control (HealthWatch) | RCT: Internet-based CBT versus attention control 12 week follow-up | Significantly greater improvement in depression scores (p=.012), self-reported medication adherence, and health behaviors |
| Graham et al. (2012)77 | 3295 Medicare case-managed adults | USA | Weekly IVR for 30 days | Geisinger Monitoring Program (GMP) IVR protocol to reduce 30-day readmission rates with case management | Pre-post parallel quasi experimental study, GMP IVR versus matched controls 30 day follow-up | Patients in IVR monitoring plus case management were 44% less likely to have a 30-day readmission than the case management alone group (p=0.0004) |
| Park et al. (2014)78 | 90 adults with CVD | USA | At least daily SMS messages, educational messages 3 times per week | Messages to improve adherence to antiplatelet and statin medications with personalized 2-way reminders correlated with medication schedule and 1-way educational messages | RCT: SMS educational messages only, versus SMS medication reminders plus educational messages, versus usual care 30-day follow-up | SMS medication reminders improved antiplatelet medication adherence (p=0.02), and percentage of doses taken on schedule (p=0.01), no significant differences in clinical outcomes between SMS groups |
| Santamore et al. (2008)79 | 464 adults with heightened 10-year risk of CVD | USA | Telemedicine System (Internet Server with database) | Both groups were given BP monitors, Telemedicine Group (TG) entered their BP readings weekly which were downloaded at clinic visits | RCT: TG versus usual care 8 month follow-up | Significantly more blood pressure monitoring (92% compared to 49% in controls, p<0.0001), readings accurate compared to office BP measurements |
| Sherrard et al. (2009)80 | 331 adults post cardiac surgery | Canada | IVR post- discharge calls at 1, 2, 3, 4, 5, 6, 8, 10, 12, 16, 20, and 24 weeks | Questions addressed medication compliance and reporting of adverse events, and provided medication information and general medication safety tips | RCT: IVR versus usual care 6 month follow-up | Significantly greater medication adherence with no adverse events (51% versus 38% in controls, p=0.04) |
| Stacy et al. (2009)81 | 497 adults with hyperlipidemia who recently filled a statin prescription | USA | Up to 3 IVR calls | Motivational messages and tailored feedback reinforcing adherence/persistence with meds; enhanced usual care controls received one IVR call with message to contact doctor if they had questions | RCT: IVR versus enhanced usual care 6 month follow-up | Significantly greater persistence in taking statins (67% compared to 37% in controls, p<0.05) |
| Vernooij et al. (2012)82 | 330 adults with vascular disease | Nether-lands | Website with bi-weekly participant submission of weight, blood pressure, smoking status, and cholesterol | Internet-based, nurse-led treatment program with website personalized for participant based on risk factors | RCT: Internet-based nurse mgmt. versus usual care 12 month follow-up | Small non-significant improvement in CVD risk. Relative change of −14% in Framingham heart risk score, compared to control group (95% CI−25% to −2%) |
Abbreviations: BP Blood Pressure, CBT Cognitive Behavioral Therapy, CRT-D Cardiac Resynchronization Therapy Device, CVD Cardiovascular Disease, DBP Diastolic Blood Pressure, FU Follow Up, GMV Group Medical Visits, HbA1c Glycosylated Hemoglobin, HRQL Health-Related Quality of Life, HTN Hypertension, IVR Interactive Voice Response, LDL Low-Density Lipoprotein, RCT Randomized Controlled Trial, SMS Short Message Service
Interactive Voice Response
IVR monitoring can provide reliable and valid information about patients’ status between outpatient encounters,83 including information about socially stigmatizing behaviors.84,85 Non-English speaking patients are willing and able to use IVR as part of their disease management.66,72,86 In a study of 464 underserved patients with home blood pressure monitors, patients were able to accurately report their blood pressure values via IVR, obviating the need for more costly automatically-uploading blood pressure devices.79
IVR-based interventions can improve outcomes for patients with chronic illnesses. In a quasi-randomized study including more than 3000 Medicare patients, IVR-supported post-discharge care management was associated with a 44% reduction in 30-day readmission rates compared to care management without IVR support.77 Other studies using IVR to improve adherence to self-care plans have shown improvements in outcomes for patients post cardiac surgery or with hypercholesterolemia.80,81 One trial among patients with poorly controlled hypertension showed improvements in diastolic blood pressures and medication adherence at six months.58 A separate hypertension trial demonstrated greater improvements in systolic blood pressures among patients receiving IVR-supported care management than randomized controls.59
A number of trials have demonstrated benefits of IVR-supported diabetes care. In a trial of lower-income diabetes patients in the US,66,67 participants receiving IVR calls with nurse follow-up experienced significant improvements at 12 months relative to randomized controls in glycemic control, self-care behaviors, and patient-centered outcomes such as depressive symptoms. A similar intervention among patients receiving care in the US Department of Veterans Affairs health system had similar 12-month findings.68 Intervention patients receiving IVR-supported diabetes management in Australia had improvements at six months in glycemic control and mental health functioning relative to randomized controls.74
Not all trials of IVR-supported diabetes care have shown benefit. One trial of women with gestational diabetes found no impact on maternal blood glucose levels.63 A trial of IVR use to promote diabetes-related retinopathy testing among 1,200 health plan members showed low uptake of the intervention and no improvement in testing rates relative to randomized controls.73 Finally, a US trial of IVR augmentation to a successful peer-support model for promoting care management among Spanish-speakers with diabetes found no incremental benefit of the IVR booster intervention.64
To our knowledge, only two published studies have examined the impact of IVR-supported disease management in LMICs. In one pre-post study, investigators tested the feasibility of delivering IVR diabetes management calls delivered to patients in Honduras using a cloud computing approach with the IVR infrastructure maintained in the US, and calls sent using Voice over IP.69 Despite very low levels of educational attainment, at the 6-week follow-up, participants reported high levels of intervention satisfaction and improvements in their self-care. A1c levels improved significantly, and patients reported improvements in their perceived health. In a randomized trial, 200 patients with poorly controlled hypertension were enrolled in clinics in Honduras and Mexico.61 Intervention patients received weekly IVR monitoring and self-care support calls, and structured notifications based on patients’ IVR-reported information were sent automatically to the clinical team. At follow-up, intervention patients had systolic blood pressures that were on average 4.2 mmHg lower than control patients, and in a pre-planned subgroup analysis among patients with high information needs, intervention patients had an average 8.8 mmHg reduction in systolic blood pressure relative to controls. Intervention patients at follow-up also had fewer depressive symptoms, fewer medication problems, better overall perceived health, and greater satisfaction with their hypertension care. Because literacy rates are lower in LMICs, patients may prefer IVR to SMS adherence reminders.27,55 However, IVR call completion rates are lower in LMICs than they are in more developed countries, particularly among older adults.56,69
Short-Message Service (SMS) or Text Messaging
A 2012 Cochrane review evaluating the evidence on SMS messaging for facilitating chronic disease self-management found only four randomized trials that met their quality criteria (two diabetes trials, one hypertension trial, and one asthma trial).87 The authors cautiously concluded that there were some indications across all the studies that mobile phone messaging interventions may improve chronic disease self-management. However, they also noted significant information gaps regarding long-term effects, acceptability, costs, and the possible risks of such interventions.
A recent quasi-experimental study found that SMS program participation resulted in improved glycemic control, high patient satisfaction with care, and a net cost saving of 8.8% compared with the same time period prior to the program.65 Over 6 months, adults with diabetes received automated text messages, including educational modules on diabetes self-care and prompts to engage in specific behaviors (e.g., “Do you need refills of any of your medications?”). Patients were asked to respond to messages via a reply text, and patient reports exceeding predefined thresholds triggered a response from a nurse. To increase patient engagement and message relevance, the contents of the messages were modified every two weeks based on users’ interactions with the system. With program costs estimated at $375 per patient, net cost savings in outpatient, emergency department and inpatient care were $437 per patient. In another US trial among English- and Spanish-speaking diabetes patients presenting to a safety net emergency department, the intervention group received two daily SMS messages and had improvements in medication adherence and decreased emergency department use over the subsequent 6-month period. Intervention effects were particularly pronounced among Spanish-speakers.62
A 2014 trial78 examined antiplatelet and statin medication adherence among recently discharged patients hospitalized for a myocardial infarction or cardiac procedure. Patients were randomized to usual care or either: (1) daily SMS medication reminders and self-care educational messages, with messages asking patients to confirm receipt; or (2) three times a week one-way educational SMS messages only. Both groups had significantly higher anti-platelet medication adherence 30 days post discharge compared to randomized controls. Patients randomized to the bi-directional SMS messages had high rates of engagement with the messaging system but there were no significant differences between the two SMS intervention groups in clinical outcomes.
Several of the abovementioned trials suggest that SMS disease management may be particularly effective if the messages are personally tailored and include a mechanism for patients to be actively engaged in the communication. In contrast, a 2012 trial found that generic motivational one-way SMS messages sent weekly to HIV-positive adults in Cameroon did not improve adherence to antiretroviral therapy over 6 months relative to usual care.54 Similarly, a multicenter, randomized cluster study of 26 primary care health centers in Spain examined the impact of SMS messages and reminders sent twice per week over four months to adults with hypertension. Messages were not tailored to the individual and required no response; no improvements in blood pressure-related outcomes or adherence were observed at six months.57
A 2010 systematic review of behavior change interventions for chronic disease management and prevention delivered through SMS examined nine studies that were sufficiently powered to detect a difference in the specific characteristics of the intervention.28 Eight of the nine studies found evidence to support text messaging as a tool for behavior change. Noting that prior research has shown that messaging interventions designed based on behavioral theory are more likely to be successful, the authors observed that few studies they reviewed specified a theoretical rationale for the intervention design. In a 2011 systematic review of mobile health intervention trials, Riley and colleagues also found that most studies did not report on whether the intervention was informed by behavioral theories.88
Smartphone and Internet-Enabled Applications
A large body of evidence has demonstrated the effectiveness of remote monitoring of clinical parameters for cardiovascular diseases including heart failure, hypertension, and diabetes.60,75,89 In one trial of adults with diabetes,70 investigators evaluated a cell phone-based software system with web-based data analytics and therapy optimization tools. The application provided real-time feedback to patients on their blood glucose levels, displayed the patient’s medications, and prompted patients for additional information useful for feedback on their diabetes management. The system also sent computer-generated trend reports to the patient’s provider team along with suggested modifications to the treatment plan. The intervention group had significantly improved glycemic control and medication adjustments at three months compared to randomized controls. In addition to improving diabetes patients’ glycemic control, such applications show promise for enabling more effective monitoring of other cardiovascular risk factors such as blood pressure, physical activity, and weight.
A 2012 review of diabetes self-management interventions using mobile monitoring technologies reported that 10 of the 13 reviewed studies led to improved glycemic control compared to usual care.29 Similarly, a 2012 review of mobile health in diabetes management30 reviewed 28 intervention studies, most of which included specialized features designed for use with smartphones or other communication tools that have graphical displays. The focus of those communication tools included electronic trend reports about data such as blood pressures, blood glucose, or physical activity; reminders; and tailored information for the patient. Eighty-five percent of studies with A1c as an outcome reported improvements. Forty-eight percent of the studies reported on patient satisfaction, and 90% of those trials reported high satisfaction with the mobile disease management support.
Several studies, including a recent meta-analysis, have shown that Internet-based interventions can be effective and most of the features used could be adapted for mobile phones or tablets.82,90 A number of these trials have used multiple modalities to reach patients and provide a more flexible platform for monitoring and self-care education. A trial conducted in Australia evaluated an Internet-delivered cognitive behavioral therapy intervention among patients at high risk for cardiovascular disease who had comorbid depression and found improvements relative to randomized controls in psychological symptoms, self-reported medication adherence, and health behaviors.76 In a 2011 cluster-randomized trial among 26 primary care practices, investigators evaluated a mobile- and web-based self-management program for diabetes patient coaching and provider decision support.71 Patients received automated real-time educational and behavior change messages in response to their reported blood glucose values, with messages focusing on medication management and lifestyle behaviors. Providers received quarterly reports summarizing patients’ glycemic control, medication management, lifestyle behaviors, and evidence-based treatment options. At the 12-month follow-up, mean A1c levels declined relative to baseline in the intervention group more than twice as much as among patients randomized to usual care.
Over the past decade there has been an explosion of new social media sites offering users opportunities to interact virtually with peers and health professionals, sharing written information, graphical displays, videos, photographs, and other forms of communication. Online community resources include social networking sites such as Facebook, blogs, wikis, Twitter chats, photo and video sharing sites, and virtual worlds. A number of interventions are being evaluated that seek to leverage social media for improving chronic disease management. However, so far few results from such intervention trials have been published. One 2013 review examined studies on social media use by adults with chronic disease,91 including cardiovascular disease. The most salient finding was the paucity of rigorous studies and the variability of study methodologies. Only 3 of the 19 studies reviewed were randomized trials, and only seven reported on social media with web 2.0 platforms. While highlighting the potential of this growing and diverse set of tools for cardiovascular lifestyle behavior change and disease management, the review drew no conclusions about the effectiveness of different approaches to improving health outcomes.
Discussion
Summary of Findings
Although not all studies have had positive outcomes, a number of randomized controlled trials, including 2 studies from LMIC, have shown that IVR interventions can improve lifestyle risk factors for cardiovascular disease as well as disease management. An advantage of IVR self-management support programs is that they can be used with any standard cell or landline phone. Because no reading or writing is required, IVR interactions are accessible to low-literacy populations as well as those with vision problems. Patients can use IVR to report detailed information about their status and receive tailored feedback about their health and self-care. However, IVR interactions typically require patients to participate when the call is placed or to call-in to the system. While patients sometimes can specify when they are likely to be available, changes in their schedule may be difficult to accommodate. Unlike texts, images, or website links sent to patients via a smartphone, patients using IVR cannot review information after the fact. Unfortunately, because of the diversity of study populations, outcomes, and IVR system designs, we still cannot identify the characteristics of interventions that are associated with greater behavior change and health improvements.
Evidence also is growing about the effectiveness of SMS interventions in improving behavioral risk factors and cardiovascular disease management, especially interventions enabling real-time feedback, exchange, and support. Most randomized trials of SMS interventions for chronic disease behavior change have been conducted in HICs, however, and little work to date has examined different behavioral approaches to intervention design or content development. Also, there is little known about the optimal dosing, frequency and content of text messages, the duration of interventions, or the individual and group characteristics that may identify patients most likely to benefit. An advantage of SMS interventions is that they can be used with almost all mobile phones, and they take advantage of the widespread use of texting both in HICs and LMICs.28,31,32 However, SMS services are difficult for individuals with limited vision, dexterity, or literacy, all of which are more common in poor communities. SMS self-care supports tend to be less interactive than counseling by a clinician, but when patients are asked to confirm receipt of texts, interventions may have increased engagement and impact. More complex two-way SMS messages may boost engagement and effectiveness, but this may require a clinician or other “live” person to be in the loop, since computers are challenged by the non-standard spelling and grammar from patients’ texts.
Newer mHealth interventions hold considerable promise, but the research base on interventions delivered via smartphones or social media is still small. In the next few years, results from ongoing trials will help to develop the evidence in this important area.
Challenges and Future Directions
Given this rapidly evolving field with heterogeneous intervention characteristics, populations, and study endpoints, it was not possible to conduct a definitive, “systematic review” with clearly defined questions regarding whether mHealth “works” for cardiovascular behavior change and disease management. Similarly, this field is still too new to allow definitive conclusions about which components of successful interventions most contribute to their effectiveness. As such, in this review we have sought to highlight major advances and suggest important unanswered questions for moving the field forward (Table 4). For example, the content of mHealth messages is unstandardized across studies (see examples in Tables 5–6). While this may be appropriate given the state-of-the-science, it currently makes it impossible to say with certainty whether differences in content, mode of delivery (e.g., IVR versus SMS) or other factors are responsible for variation in intervention effects across studies.
Table 4.
Gaps in Knowledge and Future Directions for Research
| Gaps in Knowledge | Next Steps |
|---|---|
|
Technology | |
| Best combinations of features for monitoring and self-care behavior change support (animations, graphics, video, text-to-speech), given the varying levels of literacy and technology access in LMICs | Process studies and trials examining what features best promote engagement and effectiveness for different behaviors and patients |
| Optimal duration of interventions and frequency of patient contacts | Compare different durations and frequencies of contact, both in traditional randomized trials and patient-preference trials |
| Relative advantages of different types of end-user participation (e.g., required user responses to messages and bidirectional interaction with providers) | Usability testing and qualitative interviews, plus trials comparing levels and types of end-user active participation within and across cultures |
| When and how to integrate mHealth interventions with electronic health records or patient portals | Testing of different models of integration, including studies of the budget impact and cost-effectiveness of greater integration |
| Optimal balance between automated communication and self-management support delivered by community health workers and other providers | Comparative effectiveness trials of different levels of “live” versus mHealth support |
| Use of adaptive techniques in the field of artificial intelligence to design more patient-centered systems | Lab-based engineering studies to determine when and how mHealth services can adapt to patients’ characteristics and changing context. Trials comparing adapted to more regimented message delivery strategies in “real-world” LMIC settings |
|
Behavior Change | |
| Best ways to mobilize social networks and online communities for behavior change | Network analysis of “influencers” in social media networks. Studies to better understand what information patients are willing to share in networks given their sociodemographics and cultural context. |
| What patient characteristics to use in tailoring messages (e.g., level of self-efficacy, source of motivation, values/life goals, demographic characteristics) for behavior change | Fractional factorial studies examining most effective tailoring approaches for behavior change |
| Most effective behavioral theories to underpin intervention design | Fractional factorial studies and careful analysis of mediators of intervention effects to refine behavioral theory |
|
Settings and Populations | |
| Most effective approaches to adapt technologies found effective in high-income settings for LMIC settings and for populations in which low health literacy and limited electronic literacy are common | Development processes incorporating input from end-users in different settings and careful piloting of mHealth interventions for feasibility and acceptability in various populations and LMICs |
| Most effective behavioral theories to underpin different interventions | Include mediator analyses in evaluations of mHealth interventions to test mechanisms by which the interventions influence outcomes |
| Explicitly outline behavioral theories motivating different intervention components and messages | |
| Characteristic of populations that benefit most from various mHealth approaches | Include moderator analyses (specifically focusing on variation in culture and socioeconomic status within and across countries) in evaluations of interventions |
Table 5.
Examples of Message Content for Interventions Targeting Disease Prevention
| Reference | IVR Examples | |
|---|---|---|
| Estabrooks (2009)44 | “Be consistent in limiting the amount of television your child watches this week to 2 hours/day.” “Clear the kitchen cupboards of unhealthy snacks.” “Set a goal to take your family to a new park or trail that you haven’t visited before.” | |
| de Neit (2012)43 | “Well done with your exercise! Keep going! Find distractions when you cannot resist unhealthy food. Good luck, you can do it!” “Hi Bart! Well done with your exercise! Keep going! Great that you exercised with your friends! Find distractions when you cannot resist unhealthy food.” | |
| Reference | SMS Examples | |
| Free (2011)45 | “Why not write an action list of your reasons why you want to quit [smoking]. Use it as your inspiration.” “TXT2STOP: Think you’ll put on weight when you quit? We’re here to help - We’ll TXT weight control and exercise tips, recipes, and motivation tips.” “Cravings last less than 5 minutes on average. To help distract yourself, try sipping a drink slowly until the craving is over.” | |
| Norman (2013)47 | “Writing down what you ate and how you felt when you ate it will help you stay on track with your goals.” “Organize your pantry so that healthier foods are facing forward and less healthier items are in the back and out of sight.” “Find friends who share similar weight loss goals and support each other. It’s fun to exchange healthy recipes too!” | |
| Shapiro (2012)49 | “Here’s a tip: put your work-out clothes in front of your door this evening so you don’t forget to work out tomorrow.” “Remember to weigh yourself tomorrow morning.” “Peaches are a great source of carotenes, potassium, and flavonoids. Try one for 70 calories and 2.6 grams of fiber.” | |
| Chow (2012)35 | “Are you taking daily aspirin? If not discuss it with your doctor.” “Try steaming, baking or BBQ to reduce the need for excess oil when cooking.” “If you crave a cigarette, try and distract yourself by going for a walk or doing something creative.” |
|
| Wong (2013)41 | “Diabetic complications include eye problems and feet problems.” “Should choose lean meat with skin and fat trimmed off.” “Smoking is old fashioned, quit smoking is the trend.” | |
| Reference | Other Examples (i.e. SmartPhone) | |
| Park (2012)48 | Web based diary with recommendations on diet and exercise through cell phone and internet | “New week is beginning, let’s exercise.” “Walking as aerobic exercise can reduce abdominal fat.” |
| Turner-McGrievy (2011)50 | Social network posts via Twitter | “Got an insulated lunch bag? Sure helps w/healthy eating at work. Good lunch bags are available at kitchen stores at the mall.” |
Table 6.
Examples of Message Content for Interventions Targeting Disease Management.
| Reference | IVR Examples | |
|---|---|---|
| Sherrard (2009)80 | “Did you fill the prescriptions given to you at discharge?” | |
| Reid (2007)40 | “Have you smoked any cigarettes, even a puff, since you left the hospital?” “On a scale of 1–10, with 10 being the most confident, how confident are you that you will remain a non-smoker?” | |
| Piette (2011)69 | “During the past week, did you have any symptoms of low blood sugar? This is sometimes called a ‘hypoglycemic reaction and can cause symptoms such as sweating or trembling. Another symptom may be feeling weak to the point that a person feels like they’re going to fall down or does fall down.” | |
| Reference | SMS Examples | |
| Nundy (2014)65 | “Time to check your blood sugar.” “Do you need refills of any of your medications?” | |
| Arora (2014)62 | “Having diabetes can lead to a heart attack or stroke—but it doesn’t have to.” “Medication reminder! Don’t leave home without your medications.” “Challenge! Don’t drink any soda or juice today. Only drink water or milk.” | |
| Park (2014)78 | “John, take Plavix 75 mg at 9:00 AM. Respond with 1.” ‘Remember to see your cardiologist and/or primary physician 1–2 weeks after your hospitalization.” | |
| Mbuagbaw (2012)54 | “You are important to your family. Please remember to take your medication. You can call us at this number: xxx-xxx-xxxx.” | |
| Pop-Ecleches (2011)53 | “This is your reminder.” “This is your reminder. Be strong and courageous, we care about you.” | |
| Contreras (2004)57 | “Always take your blood pressure pill when you get up in the morning.” “A little exercise each day will help make your treatment more effective.” “A healthy, balanced diet is the best guarantee for controlling your blood pressure.” | |
| Reference | Other Examples (i.e. SmartPhone) | |
| Sidney (2012)55 | IVR & SMS | “Did you take all of the doses of your medication yesterday? Press ‘1’ for ‘yes’ and ‘2’ for ‘no’.” |
| Haberer (2010)56 | IVR & SMS | “How many doses of medicine did your child miss in the past 7 days?” |
Problems in the dissemination of mHealth services within LMICs mirror those seen in LMIC medical care, i.e., services are limited in scope, unevenly distributed across geographic areas, and of variable quality when they are available. In a systematic review of health data quality in LMICs, investigators identified multiple critical weaknesses, including missing data, unreliable clinical information entered into electronic records, problems with timeliness, and limited accessibility.92 One important challenge to the development of scalable, sustainable mHealth services is the limited infrastructure for training and supporting the workforce in LMICs with skills in health informatics.93 Several programs for building the needed human capital have been launched, with support by the US Fogarty International Center, the Bill and Melinda Gates Foundation, and the American Medical Informatics Association.94 Web-based distance learning programs will be important, and multiple models have been described.95 Internationally shared platforms such as the Virtual Campus of Public Health supported by the Pan America Health Organization also will facilitate the transfer of knowledge from HICs to LMICs.
The mHealth Alliance is an international leader in promoting research and dissemination on effective models of mHealth globally, through work on strategies for sustainable funding, the development of supportive governmental policies, and workforce development. In 2013, the Alliance published an important review with recommendations on standards and interoperability for mHealth services in LMICs.96 The report found that investment in standards for compatibility of systems is among the greatest challenges, although systems currently in use in some LMICs could serve as models for scaling programs transnationally.96 Alignment of market incentives to promote pooling of resources and expertise will be critical to establishing mHealth systems as tools for cardiovascular disease prevention and management around the globe.97
Next Generation Systems
Regardless of whether communication is via IVR, SMS, Internet-enabled devices, or a combination of these modalities, almost all automated mHealth patient interactions use algorithms for determining what information to “push out” to patients, what information to request, and how to determine what additional actions should be taken based on patients’ responses (e.g., feedback to the clinical team). Those algorithms typically reflect decisions made by experts that are codified in tree-structured protocols for identifying problems and giving advice. Regardless of the rigor of the development process and the complexity of the underlying conversation map, interactions based on expert systems inevitably represent developers’ best guess regarding the information exchanges that will be most useful in supporting patients’ self-management. Limited experience with users can mean that, on average, patients’ needs are different than what the experts expected. Even if the system targets an average patient well, variations around that average can result in a poor fit between individual messages and users’ unique needs and learning styles. Unpredictable changes in a patient’s health status or self-management support needs, e.g., a recent cardiovascular event, cannot be accommodated easily given that the underlying structure is often limited in its ability to “listen” to patients and adapt to important events. Finally, as patients’ health declines or they master a given self-management task, their need for information support will evolve, and an expert system that worked in the past may become increasingly unhelpful after multiple interactions. Because expert systems often do a poor job of adapting to individual patients’ needs, they can lack the credibility that patients and clinicians expect in order to adopt and maintain an mHealth service over the long term.
Well-established informatics strategies are available for improving on these deterministic mHealth programs so that they can provide a more patient-centered experience and adapt to users’ unique learning styles, preferences, and needs. Many of these strategies have been developed for use through Web-based applications such as Amazon.com, Netflix, or Pandora.com. These “intelligent” systems automatically learn from users what works for them, adapt to users’ preferences (e.g., by watching what they buy on-line), and recommend options based on the ways in which one user is similar in their behavior to others. More adaptive mHealth systems using artificial intelligence and machine learning principles may represent a substantial improvement in our ability to monitor patients’ status and provide relevant behavior change messages related to cardiovascular disease prevention and management.98,99
Other Issues
Just as no physician should rely on only one drug and dosing for all patients with hypertension, health systems should develop a portfolio of mHealth tools, and tailor their use to the needs of individual patients and problems. Regardless of the type of service employed, between-visit monitoring systems that result in more frequent patient contact run the risk of increasing health service use and cost, because relatively crude data streams may compel clinicians to follow-up on a greater number of minor or self-limiting conditions. Thus, great care needs to be taken in developing the content of these interactions, as well as the ways in which mHealth services fit with the work flow in patients’ systems of care.
More evidence is needed on the impacts of mHealth in LMICs. Development of mobile health services for language minority patients, e.g., the many indigenous communities in Latin America, is an important priority. Highly controlled studies fail to answer questions about the reach of mHealth in vulnerable communities or whether such systems can be adopted, scaled, and maintained outside of the environments in which they are originally tested. New approaches to implementation science, emphasizing both qualitative and quantitative methods, community-based participatory research, and organizational theory can complement controlled trials and ensure that mHealth systems are relevant and flexible enough to adapt to multiple environments.100
Traditionally-designed large multi-site trials are expensive and can take years to produce information. Investment in such studies should be carefully weighed against funding larger numbers of smaller and innovative (albeit less definitive) studies of solutions adapted to different cultures and settings. As this field matures, more focused, systematic reviews and meta-analyses will be possible in order to determine whether specific intervention type improve clearly defined outcomes across multiple studies. Given the current state of the science and the heterogeneity of interventions, intervention targets, and populations, that type of review currently is not possible, particularly with respect to the efficacy of mHealth solutions in LMICs. Finally, to overcome the field’s “pilot-itis” (chronic proliferation of small, short-term studies without a clear path toward scalability and sustainability), future research will need to address financing and examine the cost-effectiveness of different mHealth interventions from the perspective of large payers.
Conclusions
People with cardiovascular diseases and their risk factors – like the rest of the societies in which they live – are increasingly mobile, and mobile patients require mobile health support to meet their ongoing needs for assistance with self-management. A solid body of evidence has shown that targeted telehealth delivered by trained clinicians can improve cardiovascular outcomes, but cost constraints will continue to limit the availability of these services. mHealth tools could fill the gap between what patients need and what their health systems can provide given cost constraints. IVR, SMS, smartphones, and social media each provide a unique platform for developing mHealth services, and a variety of trials indicate that such tools may provide a low-cost and effective solution to the challenges of providing ongoing patient care at a distance. Research on new models of mHealth should emphasize creative approaches to addressing the epidemic of cardiovascular diseases in LMICs. In addition, researchers should develop new systems that take advantage of advances in artificial intelligence as well as behavioral theory to ensure that mHealth services are as personalized and effective as possible.
Supplementary Material
Acknowledgments
Jenny Chen and Nicolle Marinec provided invaluable support in the preparation of the manuscript and evaluation of studies reviewed.
Funding Sources: John Piette is a Department of Veterans Affairs Senior Career Scientist. John Piette and Michele Heisler also received support from grant number P30DK092926 from NIH. Justin List and Michele Heisler received support from the Robert Wood Johnson Foundation Clinical Scholars Program.
Footnotes
Journal Subject Codes: [117] Behavioral/psychosocial – treatment; [119] Compliance/Adherence; [26] Exercise/exercise testing/rehabilitation; [121] Primary prevention; [122] Secondary prevention; [190] Type 2 diabetes
Disclosures: None
References
- 1.World Health Organization. Global status report on noncommunicable diseases. 2010 http://whqlibdoc.who.int/publications/2011/9789240686458_eng.pdf.
- 2.World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. 2003 http://whqlibdoc.who.int/publications/2003/9241545992.pdf.
- 3.McIntyre D, Thiede M, Dahlegren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Social Science and Medicine. 2006;62:858–65. doi: 10.1016/j.socscimed.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Wagner AK, Graves AJ, Reiss SK, LeCates R, Zhang F. Access to care and medicines, burden of health care expenditures, and risk protection: Results from the World Health Survey. Health Policy. 2011;100:151–8. doi: 10.1016/j.healthpol.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Berendes S, Heywood P, Oliver S, Garner P. Quality of private and public ambulatory care in low and middle income countries: systematic review of comparitive studies. PLOS Medicine. 2011 doi: 10.1371/journal.pmed.1000433. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. The World Health Report 2006: Working Together for Health. Geneva: WHO; 2006. [Google Scholar]
- 7.World Health Organization. and the Global Health Workforce Alliance The Kampala Delcaration and Agenda for Global Action. Geneva: WHO; 2008. [Google Scholar]
- 8.Stilwell B, Diallo K, Zurn P, Vujicic M, Adams O, Dal Poz M. Migratnion of health-care workers from developing countries: strategic approaches to its management. Bulletin of the World Health Organization. 2004;82:595–600. [PMC free article] [PubMed] [Google Scholar]
- 9.Ruelas E, Gómez-Dantés O, Leatherman S, Fortune T, Gay-Molina JG. Strenthening the quality agenda in health care in low- and middle-income countries: Questions to consider. International Journal of Quality in Health Care. 2012;24:553–7. doi: 10.1093/intqhc/mzs061. [DOI] [PubMed] [Google Scholar]
- 10.Blaya JA, Fraser HSF, Holt B. E-Health technologies show promise in developing countries. Health Affairs (Millwood) 2010;29:244–51. doi: 10.1377/hlthaff.2009.0894. [DOI] [PubMed] [Google Scholar]
- 11.Piette JD, Lun KC, Moura LA, Fraser HS, Mechael PN, Powell J, Khoja SR. Impacts of eHealth on outcomes of care in low and middle-income countries: where do we go from here? WHO Bulletin. 2012;90:366–72. doi: 10.2471/BLT.11.099069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The World in 2010: ICT Facts and Figures. International Telecommunication Union; 2010. at http://www.itu.int/ITU-D/ict/material/FactsFigures2010.pdf.) [Google Scholar]
- 13.Clark RA, Inglis SC, McAlister FA, Cleland JGF, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. British Medical Journal. 2007;334:942–50. doi: 10.1136/bmj.39156.536968.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abudagga A, Resnick HE, Alwan M. Impact of blood pressure telemonitoring on hypertension outcomes: A literature review. Telemedicine and e-Health. 2010;16:830–8. doi: 10.1089/tmj.2010.0015. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal R, Bills JE, Hecht TJW, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57:29–38. doi: 10.1161/HYPERTENSIONAHA.110.160911. [DOI] [PubMed] [Google Scholar]
- 16.Lange I, Campos S, Urrutia J, Bastamante C, Alcayaga C, Piette JD. Efecto de un modelo de apoyo telefonico en el auto-manejo y control metabolico de la diabetes tipo 2, en un centro de atencion primaria, Santiago, Chile [Effect of a telephone support model on self-management and metabolic control among type 2 diabetes patients in primary care, Santiago Chile] Revista de Medicina de Chile. 2010;138:229–37. doi: 10.4067/s0034-98872010000600010. [DOI] [PubMed] [Google Scholar]
- 17.GESICA Investigators. Long-term results after a telephone intervention in chronic heart failure: DIAL (randomized trial of phone intervention in chronic heart failure) follow-up. Journal of the American College of Cardiology. 2010;56:372–8. doi: 10.1016/j.jacc.2010.03.049. [DOI] [PubMed] [Google Scholar]
- 18.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301:603–18. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 19.Bott DM, Kapp MC, Johnson LB, Magno LM. Disease management for chronically ill beneficiaries in traditional Medicare. Health Affairs. 2009;28:86–98. doi: 10.1377/hlthaff.28.1.86. [DOI] [PubMed] [Google Scholar]
- 20.Whitten PS, Mair FS, Haycox A, May CR, Williams TL, Hellmich S. Systematic review of cost-effectiveness studies of telemedicine interventions. British Medical Journal. 2002;324:1434–37. doi: 10.1136/bmj.324.7351.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beratarrechea A, Lee AG, Willner JM, Jahangir E, Ciapponi A, Rubinstein A. The impact of mobile health interventions on chronic disease outcomes in developing countries: a systematic review. Journal of Telemedicine and e-Health. 2014;20:75–83. doi: 10.1089/tmj.2012.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Esterson YB, Carey M, Piette JD, Thomas N, Hawkins M. A systematic review of innovative diabetes care models in low- and middle-income countries (LMICs) Journal of Healthcare for the Poor and Underserved. 2014;25:72–93. doi: 10.1353/hpu.2014.0037. [DOI] [PubMed] [Google Scholar]
- 23.Neubeck L, Redfern J, Fernandez R, Briffa T, Bauman A, Freedman SB. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. European journal of cardiovascular prevention and rehabilitation. 2009;16:281–9. doi: 10.1097/HJR.0b013e32832a4e7a. [DOI] [PubMed] [Google Scholar]
- 24.Deglise C, Suggs LS, Odermatt P. Short Message Service (SMS) applications for disease prevention in developing countries. Journal of Medical Internet Research. 2012;14:e3+. doi: 10.2196/jmir.1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bastawrous A, Armstrong MJ. Mobile health use in low- and high-income countries: an overview of the peer-reviewed literature. Journal of the Royal Society of Medicine. 2013;106:130–42. doi: 10.1177/0141076812472620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change communication interventions in developing countries: a systematic review of the literature. Journal of health communication. 2012;17(Suppl 1):82–104. doi: 10.1080/10810730.2011.649160. [DOI] [PubMed] [Google Scholar]
- 27.Davey S, Davey A. Mobile-health technology: Can it strengthen and improve public health systems of other developing countries as per Indian strategies? A systematic review of the literature. International Journal of Medicine and Public Health. 2014;4:40–5. [Google Scholar]
- 28.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews. 2010;32:56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baron J, McBain H, Newman S. The impact of mobile monitoring techniologies on glycosylated hemoglobin in diabetes: a systematic review. Journal of Diabetes Science & Technology. 2012;6:1185–96. doi: 10.1177/193229681200600524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemedicine Journal & E-Health. 2012;18:175–84. doi: 10.1089/tmj.2011.0119. [DOI] [PubMed] [Google Scholar]
- 31.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemedicine and e-Health. 2009;15:231–40. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 32.Fjeldsoe B, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-messaging service. American Journal of Preventive Medicine. 2009;36:165–73. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 33.Mechael P, Batavia H. Barriers and gaps affecting mHealth in low and middle-income countries: Policy white paper. 2010 http://www.globalproblems-globalsolutions-files.org/pdfs/mHealth_Barriers_White_Paper.pdf.
- 34.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information and Libraries Journal. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 35.Chow CK, Redfern J, Thiagalingam A, Jan S, Whittaker R, Hackett M, Graves N, Mooney J, Hillis GS. Design and rationale of the tobacco, exercise and diet messages (TEXT ME) trial of a text message-based intervention for ongoing prevention of cardiovascular disease in people with coronary disease: a randomised controlled trial protocol. BMJ open. 2012;2:e000606. doi: 10.1136/bmjopen-2011-000606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Handley MA, Shumway M, Schillinger D. Cost-effectiveness of automated telephone self-management support with nurse care management among patients with diabetes. Annals of Family Medicine. 2008;6:512–8. doi: 10.1370/afm.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, Rudd P, Friedman RH. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: A randomized controlled trial. Annals of Behavioral Medicine. 2012;43:62–73. doi: 10.1007/s12160-011-9319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009;32:813–5. doi: 10.2337/dc08-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nolan RP, Upshur RE, Lynn H, Crichton T, Rukholm E, Stewart DE, Alter DA, Chessex C, Harvey PJ, Grace SL, Picard L, Michel I, Angus J, Corace K, Barry-Bianchi SM, Chen MH. Therapeutic benefit of preventive telehealth counseling in the Community Outreach Heart Health and Risk Reduction Trial. The American journal of cardiology. 2011;107:690–6. doi: 10.1016/j.amjcard.2010.10.050. [DOI] [PubMed] [Google Scholar]
- 40.Reid RD, Pipe AL, Quinlan B, Oda J. Interactive voice response telephony to promote smoking cessation in patients with heart disease: a pilot study. Patient Education and Counseling. 2007;66:319–26. doi: 10.1016/j.pec.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Wong CK, Fung CS, Siu SC, Lo YY, Wong KW, Fong DY, Lam CL. A short message service (SMS) intervention to prevent diabetes in Chinese professional drivers with pre-diabetes: a pilot single-blinded randomized controlled trial. Diabetes Research and Clinical Practice. 2013;102:158–66. doi: 10.1016/j.diabres.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 42.Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, Miller ER, Dalcin A, Jerome GJ, Geller S, Noronha G, Pozefsky T, Charleston J, Reynolds JB, Durkin N, Rubin RR, Louis TA, Brancati FL. Comparative effectiveness of weight-loss interventions in clinical practice. New England Journal of Medicine. 2011;365:1959–68. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Niet J, Timman R, Bauer S, van den Akker E, Buijks H, de Klerk C, Kordy H, Passchier J. The effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: a randomized controlled trial. Pediatric obesity. 2012;7:205–19. doi: 10.1111/j.2047-6310.2012.00048.x. [DOI] [PubMed] [Google Scholar]
- 44.Estabrooks PA, Shoup JA, Gattshall M, Dandamudi P, Shetterly S, Xu S. Automated telephone counseling for parents of overweight children: a randomized controlled trial. American Journal of Preventive Medicine. 2009;36:35–42. doi: 10.1016/j.amepre.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 45.Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, Rodgers A, Cairns J, Kenward MG, Roberts I. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. The Lancet. 2011;378:49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.King AC, Hekler EB, Castro CM, Buman MP, Marcus BH, Freidman RH, Napolitano MA. Exercise advice by humans versus computers: maintenance effects at 18 months. Health Psychology. 2014;33:192–6. doi: 10.1037/a0030646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Norman GJ, Kolodziejczyk JK, Adams MA, Patrick K, Marshall SJ. Fruit and vegetable intake and eating behaviors mediate the effect of a randomized text-message based weight loss program. Preventive medicine. 2013;56:3–7. doi: 10.1016/j.ypmed.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Park MJ, Kim HS. Evaluation of mobile phone and Internet intervention on waist circumference and blood pressure in post-menopausal women with abdominal obesity. International journal of medical informatics. 2012;81:388–94. doi: 10.1016/j.ijmedinf.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 49.Shapiro JR, Koro T, Doran N, Thompson S, Sallis JF, Calfas K, Patrick K. Text4Diet: a randomized controlled study using text messaging for weight loss behaviors. Preventive medicine. 2012;55:412–7. doi: 10.1016/j.ypmed.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 50.Turner-McGrievy G, Tate D. Tweets, Apps, and Pods: Results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. Journal of Medical Internet Research. 2011;13:e120. doi: 10.2196/jmir.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.mHealth for development: The opportunity of mobile technology for healthcare in the developing world. Washington; USA: United Nations Foundation; 2009. [Google Scholar]
- 52.Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Jack W, Habyarimana J, Sadatsafavi M, Najafzadeh M, Marra CA, Estambale B, Ngugi E, Ball TB, Thabane L, Gelmon LJ, Kimani J, Ackers M, Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. The Lancet. 2010;376:1838–45. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 53.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, MacKeen L, Haberer J, Kimaiyo S, Sidle J, Ngare D, Bangsberg DR. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–34. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lester RT, Mills EJ, Smieja M, Dolovich L, Kouanfack C. The Cameroon Mobile Phone SMS (CAMPS) trial: a randomized trial of text messaging versus usual care for adherence to antiretroviral therapy. PLoS One. 2012;7:E46909. doi: 10.1371/journal.pone.0046909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sidney K, Antony J, Rodrigues R, Arumugam K, Krishnamurthy S, D’souza G, De Costa A, Shet A. Supporting patient adherence to antiretrovirals using mobile phone reminders: Patient responses from South India. AIDS Care. 2012;24:12–617. doi: 10.1080/09540121.2011.630357. [DOI] [PubMed] [Google Scholar]
- 56.Haberer JE, Kiwanuka J, Nansera D, Wilson IB, Bangsberg DR. Challenges in using mobile phones for collection of antiretroviral therapy adherence data in a resource-limited setting. AIDS and Behavior. 2010;14:1291–301. doi: 10.1007/s10461-010-9720-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Contreras EM, de la Figuera von Wichmann M, Gil-Guillen V, Ylla-Catalá A, Figueras M, Balaña M, Naval J. Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert) Atencion Primaria. 2004;34:399–405. doi: 10.1016/S0212-6567(04)78922-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Friedman RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, Carey K. A telecommunications system for monitoring and counseling patients with hypertension: impact on medication adherence and blood pressure control. American Journal of Hypertension. 1996;9:285–92. doi: 10.1016/0895-7061(95)00353-3. [DOI] [PubMed] [Google Scholar]
- 59.Magid DJ, Ho PM, Olson KL, Brand DW, Welch LK, Snow KE, Lambert-Kerzner AC, Plomondon ME, Havranek EP. A multimodal blood pressure control intervention in 3 healthcare systems. American Journal of Managed Care. 2011;17:e96–e103. [PubMed] [Google Scholar]
- 60.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O’Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310:46–56. doi: 10.1001/jama.2013.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Piette JD, Datwani H, Gaudioso S, Foster SM, Westphal J, Perry W, Rodríguez-Saldaña J, Mendoza-Avelares MO, Marinec N. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle income countries. Telemedicine and e-Health. 2012;18:613–20. doi: 10.1089/tmj.2011.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Arora S, Burner E, Lam J, De Santos R, Meeks A, Menchine M. Trial to examine text-message based mhealth in ed patients with diabetes (TExT-MED) Academic Emergency Medicine. 2014;20:S180. doi: 10.1016/j.annemergmed.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 63.Homko CJ, Deeb LC, Rohrbacher K, Mulla W, Mastrogiannis D, Gaughan J, Santamore WP, Bove AA. Impact of a telemedicine system with automated reminders on outcomes in women with gestational diabetes mellitus. Diabetes Technology and Therapeutics. 2012;14:624–9. doi: 10.1089/dia.2012.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lorig K, Ritter PL, Villa F, Piette JD. Spanish diabetes self-management with and without automated telephone reinforcement: two randomized trials. Diabetes Care. 2008;31:408–14. doi: 10.2337/dc07-1313. [DOI] [PubMed] [Google Scholar]
- 65.Nundy S, Dick JJ, Chou CH, Nocon RS, Chin MH, Peek ME. Mobile phone diabetes project led to iproved glycemic control and net savings for Chicago plan participants. Health Affairs. 2014;33:265–72. doi: 10.1377/hlthaff.2013.0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: A randomized, controlled trial. Medical Care. 2000;38(2):218–230. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 67.Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? The American Journal of Medicine. 2000;108:20–7. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 68.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs health care system: a randomized controlled trial. Diabetes Care. 2001;24:202–8. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 69.Piette JD, Mendoza-Avelares MO, Ganser M, Mohamed M, Marinec N, Krishnan S. A preliminary study of a cloud-computing model for chronic illness self-care support in an underdeveloped country. American Journal of Preventive Medicine. 2011;40:629–32. doi: 10.1016/j.amepre.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technology & Therapeutics. 2008;10:160–8. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 71.Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes care. 2011;34:1934–42. doi: 10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schillinger D, Hammer H, Wang F, Palacios J, McLean I, Tang A, Youmans S, Handley M. Seeing in 3-D: Examining the reach of diabetes self-management support strategies in a public health care system. Health Education and Behavior. 2008;35:664–82. doi: 10.1177/1090198106296772. [DOI] [PubMed] [Google Scholar]
- 73.Simon SR, Trinacty CM, Soumerai SB, Piette JD, Meigs JB, Shi P, Ensroth A, Ross-Degnan D. Improving diabetes care among patients overdue for recommended testing: a randomized controlled trial of automated telephone outreach. Diabetes Care. 2010;33:1452–3. doi: 10.2337/dc09-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Williams ED, Bird D, Forbes AW, Russell A, Ash S, Friedman R, Scuffham PA, Oldenburg B. Randomised controlled trail of an automated, interactive telephone intervention (TLC Diabetes) to improve type 2 diabetes management: baseline findings and six-month outcomes. BMC Public Health. 2012:1471+. doi: 10.1186/1471-2458-12-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boriani G, Da Costa A, Ricci RP, Quesada A, Favale S, Iacopino S, Romeo F, Risi A, Mangoni di S Stefano L, Navarro X, Biffi M, Santini M, Burri H, MORE-CARE Investigators The Monitoring Resynchronization dEvices and CARdiac patiEnts (MORE-CARE) randomized controlled trial: phase 1 results on dynamics of early intervention with remote monitoring. Journal of Medical Internet Research. 2013;15:e167. doi: 10.2196/jmir.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Glozier N, Christensen H, Naismith S, Cockayne N, Donkin L, Neal B, Mackinnon A, Hickie I. Internet-delivered cognitive behavioural therapy for adults with mild to moderate depression and high cardiovascular disease risks: a randomised attention-controlled trial. PLoS One. 2013;8:e59139. doi: 10.1371/journal.pone.0059139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Graham J, Tomcavage J, Salek D, Sciandra J, Davis DE, Stewart WF. Postdischarge monitoring using interactive voice response system reduces 30-day readmission rates in a case-managed Medicare population. Medical care. 2012;50:50–7s. doi: 10.1097/MLR.0b013e318229433e. [DOI] [PubMed] [Google Scholar]
- 78.Park LG, Howie-Esquivel J, Chung ML, Dracup K. A text messaging intervention to promote medication adherence for patients with coronary heart disease: A randomized controlled trial. Patient education and counseling. 2014;94:261–8. doi: 10.1016/j.pec.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 79.Santamore WP, Homko CJ, Kashem A, McConnell TR, Menapace FJ, Bove AA. Accuracy of blood pressure measurements transmitted through a telemedicine sysutem in underserved populations. Telemedicine and E-Health. 2008;14:333–8. doi: 10.1089/tmj.2007.0063. [DOI] [PubMed] [Google Scholar]
- 80.Sherrard H, Struthers C, Kearns SA, Wells G, Chen L, Mesana T. Using technology to create a medication safety net for cardiac surgery patients: a nurse-led randomized control trial. Canadian Journal of Cardiovascular Nursing. 2009;19:9–15. [PubMed] [Google Scholar]
- 81.Stacy JN, Schwartz SM, Ershoff D, Shreve MS. Incorporating tailored interactive patient solutions using interactive voice response technology to improve statin adherence: Results of a randomized clinical trail ina managed care setting. Population Health Management. 2009;12:241–54. doi: 10.1089/pop.2008.0046. [DOI] [PubMed] [Google Scholar]
- 82.Vernooij WP, Kaasjager HAH, Van Der Graaf Y, Wierdsma J, Grandjean HM, Hovens MM, de Wit GA, Visseren FL, SMARTStudy Group Internet based vascular risk factor management for patients with clinically manifest vascular disease: Randomised controlled trial. BMJ (Online) 2012;344 doi: 10.1136/bmj.e3750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Piette JD. Interactive voice response systems in the diagnosis and management of chronic disease. American Journal of Managed Care. 2000;6:817–27. [PubMed] [Google Scholar]
- 84.Schroder KE, Johnson CJ. Interactive voice response technology to measure HIV-related behavior. Current HIV/AIDS Reports. 2009;6:210–6. doi: 10.1007/s11904-009-0028-6. [DOI] [PubMed] [Google Scholar]
- 85.Tucker JA, Foushee HR, Black BC, Roth DL. Agreement between prospective interactive voice response self-monitoring and structured retrospective reports of drinking and contextual variables during natural resolution attempts. Journal of Studies on Alcohol and Drugs. 2007;68:538–42. doi: 10.15288/jsad.2007.68.538. [DOI] [PubMed] [Google Scholar]
- 86.Brodey BB, Rosen CS, Brodey IS, Sheetz B, Unutzer J. Reliability and acceptability of automated telephone surveys among Spanish- and English-speaking mental health services recipients. Mental Health Services Research. 2005;7:181–4. doi: 10.1007/s11020-005-5786-1. [DOI] [PubMed] [Google Scholar]
- 87.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. The Cochrane Database of Systematic Reviews. 2012;12:CD007459. doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Translational Behavioral Medicine. 2011;1:53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Acosta-Lobos A, Riley JP, Cowie MR. Current and future technologies for remote monitoring in cardiology and evidence from trial data. Future Cardiology. 2012;8:425–37. doi: 10.2217/fca.12.7. [DOI] [PubMed] [Google Scholar]
- 90.Liu S, Dunford SD, Leung YW, Brooks D, Thomas SG, Eysenbach G, Nolan RP. Reducing blood pressure with Internet-based interventions: a meta-analysis. The Canadian journal of cardiology. 2013;29:613–21. doi: 10.1016/j.cjca.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 91.Merolli M, Gray K, Martin-Sanchez F. Health outcomes and related effects of using social media in chronic disease management: A literature review and analysis of affordances. Journal of Biomedical Informatics. 2013;46:957–69. doi: 10.1016/j.jbi.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 92.Ndabarora E, Chipps JA, Uys L. Systematic review of health data quality management and best practices at community and district levels in LMIC. Information Development. 2013 [Google Scholar]
- 93.Cabieses B, Faba G, Espinoza M, Santorelli G. The link between information and communication technologies and global public health: Pushing forward. Telemedicine and E-Health. 2013;19:879–87. doi: 10.1089/tmj.2012.0232. [DOI] [PubMed] [Google Scholar]
- 94.Hersh W, Margolis A, Quirós F, Otero P. Building a health informatics workforce in developing countries. Health Affairs. 2010;29:275–8. doi: 10.1377/hlthaff.2009.0883. [DOI] [PubMed] [Google Scholar]
- 95.Frehywot S, Vovides Y, Talib Z, Mikhail N, Ross H, Wohltjen H, Bedada S, Korhumel K, Koumare AK, Scott J. E-learning in medical education in resource constrained low- and middle-income countries. Human Resources for Health. 2013;11:1–15. doi: 10.1186/1478-4491-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Payne JD. The state of standards and interoperability for mHealth. White Paper by the mHealth Alliance. 2013 http://www.mhealthalliance.org/images/content/state_of_standards_report_2013.pdf.
- 97.Marcelo A, Adejumo A, Luna D. Health informatics for development: a three-pronged strategy of partnerships, standards, and mobile health. Contribution of the IMIA Working Group on Health Informatics for Development. Yearbook of Medical Informatics. 2011:96–101. [PubMed] [Google Scholar]
- 98.Piette JD, Farris KB, Newman S, Sussman J, Singh SB. The potential impact of intelligent systems for mobile self-management support: A Monte Carlo simulation of text messaging for medication adherence. Annals of Behavioral Medicine. 2014 doi: 10.1007/s12160-014-9634-7. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Piette JD, Aikens JE, Rosland AM, Sussman J. Re-thinking the frequency of between-visit monitoring for patients with diabetes. Medical Care. 2014;52(6):511–518. doi: 10.1097/MLR.0000000000000131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science. 2009;4:50–64. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


