Abstract
Background
Although Latinos living in the U.S. are disproportionately affected by HIV, the development, implementation, and evaluation of HIV prevention, testing, and linkage to care interventions lag behind efforts occurring in other communities. To address sociocultural barriers to testing, we developed a multilevel intervention. This study is a pilot evaluation of the individual level component of the intervention – animated video modules that address specific barriers to HIV testing common among foreign-born Latino men.
Methods
We conducted a survey assessing HIV risk and barriers to testing with a convenience sample of 104 foreign-born Latino men in Baltimore, Maryland, who had not tested for HIV within the past year. Intention to test in the next three months was measured before and after viewing an intervention module selected based on survey responses.
Results
Fifty-two (50.0%) participants had never tested for HIV. Of the participants who had previously tested for HIV, the mean time since their last test was 3.48 years (sd = 3.55). Participants’ intention to test for HIV significantly increased after watching the module (t = −8.28, p < 0.001). Increased intention to test was not associated with any sociodemographic characteristics (i.e., age, country of origin) or reported sexual behaviors (i.e., number of sex partners in past year).
Discussion
These results suggest that our culturally-sensitive, individually-tailored intervention can be an additional tool to encourage HIV testing among previously untested foreign-born Latino men, one of the demographic groups at highest risk for delayed HIV diagnosis in the U.S.
Keywords: HIV/AIDS, HIV testing, HIV-related stigma, Latino immigrant
INTRODUCTION
HIV/AIDS continues to have a disproportionate effect on Latinos compared to non-Hispanic Whites in the United States (U.S.). Among Latinos living in the U.S., rates of new HIV infections are almost three times higher than that of Whites.1-4 Additionally, Latinos are more likely to be diagnosed or present late to HIV care.5-9 Males and foreign-born Latinos in particular are more likely to have undiagnosed HIV, which is concerning given that men account for approximately 80% of all new HIV infections among Latinos.9-12
In addition to negatively affecting the health of the individual, persons with HIV who are not in treatment are more likely to transmit HIV to others.13,14 Thus, a critical component to reducing HIV transmission is early diagnosis of infection and engagement and retention in care. Mathematical models have demonstrated that universal voluntary HIV testing combined with immediate initiation of antiretroviral treatment (ART) at diagnosis (“test and treat”) could reduce HIV prevalence over the coming decades.14, 15 Additionally, locations with high ART coverage have experienced reductions in HIV incidence.16-18
Current recommendations in the U.S. advocate routine voluntary (opt-out) HIV testing as a part of normal medical practice, and ART initiation regardless of CD4 cell counts.19-21 However, many foreign-born Latinos in the U.S. have limited access to healthcare, and may not benefit from opt-out HIV testing initiatives. Structural barriers include cost and/or inadequate health insurance, undocumented status, a lack of understanding of the healthcare system, and inadequate translation services.22-26 Sociocultural barriers include stigma of HIV/AIDS and anticipated and/or experienced discrimination as a Latino immigrant.22,23
Nonclinical community-based HIV testing and counseling (HTC) has been used to address some of the limitations of accessing HIV-related services in the healthcare setting for vulnerable populations, including Latinos. Community-based HTC includes door-to-door testing (systematically offering HCT to members of homes in a specific catchment area), mobile testing for the general population or for targeted populations in community sites, self-testing, workplace HCT, and school-based HCT.27 Given the barriers faced by Latino immigrants in clinical healthcare settings, community-based HCT provides an important alternative for reaching members of this population.
Many Latino immigrants are moving to new receiving communities or new growth communities – areas without established Latino communities. Baltimore, Maryland is one of these new receiving communities; in the past decade, the Latino population has increased by 135% to 26,019 (although this is likely an underestimation of the true population) 28,29. The Baltimore City Health Department (BCHD) surveillance data shows that HIV-infected Latinos in Baltimore are more likely to be diagnosed late than any other racial/ethnic groups (defined as diagnosed with AIDS within 12 months of initial HIV diagnosis).30 To address concerns of HIV/AIDS within the growing Latino immigrant population in Baltimore, the BCHD initiated a community-based outreach, testing, and linkage to care program in 2008.
The BCHD outreach, testing, and linkage to care program is a culturally-competent HIV program staffed by bilingual Latino promotoras/es. Promotoras/es, or lay health advisors, are members of the community in which they work. They are ethnically, socioeconomically, and experientially part of the community and therefore have a deep understanding of community strengths, needs, and priorities.31,32 The promotoras/es conduct street and venue-based outreach using a mobile van where clients can get free HIV testing. Since 2008, the Latino outreach team has tested over 5000 Latino men and women, and prevalence of previous HIV testing improved from 40% to 60% within 2 years.33,34 Patients diagnosed with HIV are counseled by the outreach workers and linked to HIV care at the BCHD HIV clinic, which is staffed with bilingual clinicians and case managers. Once in care, foreign-born Latinos do well, with high rates of antiretroviral coverage and virologic suppression.7,11,35,36 However, almost 50% of foreign-born Latinos in Baltimore are still diagnosed late, often during hospital admission for an opportunistic infection.
Since the mobile testing program largely addresses structural barriers to testing, this suggests that sociocultural barriers remain a significant challenge for improving HIV testing among this population. Particularly, our research in Baltimore, which is supported by research among Latinos in other settings, suggests that HIV-related stigma poses a critical barrier to HIV testing.22,23,33,37 In focus groups with Latino immigrant men living in the U.S. for less than 10 years, participants associated HIV with “immoral” behaviors (particularly same-sex relations), creating fear of a rejection by family and/or peers (a “social death”).22 Evidence of these HIV-related stigma beliefs were further supported in a community-wide survey in Baltimore completed in 2015. Three-quarters (74.4%) of the 312 respondents agreed that people get HIV because they engage in irresponsible behavior, and half (50.0%) agreed that people living with HIV or thought to be living with HIV lose respect in the community. Controlling for education and importance of religion, male respondents were almost 3.5 times more likely than women to report 4 or more (out of 6) stigmatizing beliefs. Over one-fourth of the men (27.6%) reported hesitation in testing for HIV for fear of people's reaction if the result of the test is positive.38 Similarly, in a survey of 391 newly diagnosed HIV patients attending a public AIDS program in California, Latino immigrants presented with lower CD4 counts at diagnosis than U.S.-born patients, and in-depth interviews revealed that HIV stigma emerged as an important influence in delayed HIV testing.37
Although the Latinos living in the U.S. are disproportionately affected by HIV, the development, implementation, and evaluation of HIV prevention, testing, and linkage to care interventions lag behind efforts in other communities. Efficacious interventions that do exist, such as VOICES/VOCES39 and HoMBReS-2,40 are individual or small-group interventions that reach a small number of community members. Feedback from community partners suggested that success in reducing individual level barriers to HIV testing alone would not be as effective if community-wide HIV-related stigma was not simultaneously addressed. As a result of a desire to increase HIV testing and address sociocultural barriers to HIV testing within the Baltimore Latino immigrant community, particularly HIV-related stigma, a multilevel (individual and community level) intervention called ¡Solo Se Vive Una Vez! (You Only Live Once) was developed through a partnership between the BCHD Latino outreach team, community members and leaders, the Maryland Institute College of Art (MICA), and academic investigators from Johns Hopkins University (JHU). The intervention includes: 1) graphic animation modules (with three storylines each) targeting heterosexual-identifying Latino immigrant men that address individual-level barriers to testing as identified by our previous research and the literature, and 2) materials for a community-wide anti-stigma social marketing campaign. The objective of this study was to conduct a pilot evaluation of the individually-tailored component of the ¡Sólo Se Vive Una Vez! Intervention. A separate study was completed to assess community-wide baseline measures of HIV-related stigma for development of the community-wide anti-stigma campaign and future evaluation of the complete, multilevel intervention.38
METHODS
Development of the ¡Sólo Se Vive Una Vez! (You Only Live Once) Intervention
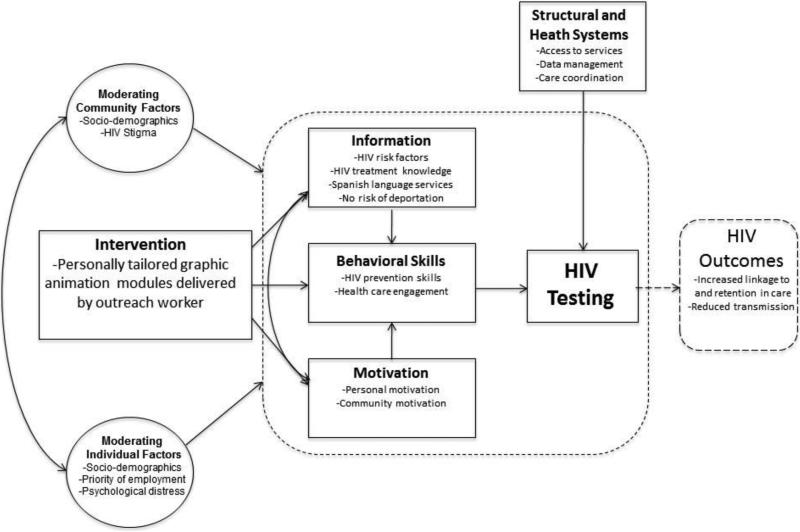
During the 2014-2015 academic year, MICA's Center for Social Design (CSD) established a yearlong practice-based studio. Students in the studio program were asked by the partners to develop an intervention to promote HIV testing in the Latino immigrant community in Baltimore with specific emphasis on foreign-born Latino men and guided by the situated Information, Motivation, Behavioral Skills framework (sIMB)41 and the Transtheoretical Model (TTM)42 (Figure 1). In this framework, relevant information, motivation, and behavioral skills interact to determine HIV testing and health seeking behaviors. These factors influence an individual's progress moving through a series of stages in their readiness to engage in HIV testing: pre-contemplation (e.g., not aware they are at risk of HIV-infection), contemplation (e.g., accurate perception of risk, knowledge of treatment, but fear of stigma), preparation (e.g., intention to test), and action (engagement in HIV testing). Our framework contextualizes and cross-culturally adapts the sIMB model to our setting through consideration of moderating personal, cultural, situational, and structural factors.
Figure 1.
situated Information, Motivation, Behavioral Skills (sIMB) framework for the ¡Solo Se Vive Una Vez! multilevel intervention. In this framework, relevant information, motivation, and behavioral skills interact to determine HIV testing and health seeking behaviors.
Prioritization on men was based on national and local characteristics of the HIV epidemic (in which Latino men are most likely to be infected) and data showing that Latino immigrant men in Baltimore are less likely to have ever tested for HIV.3,34,38 Additionally, although Latino men who have sex with men (MSM) are most at risk for HIV infection, based on community feedback, the focus on module development for heterosexually-identifying men was initially prioritized; however, we are currently working with our partners to develop modules for MSM.
Prioritization of the intervention's focus was developed through the literature, our previous research, and a nominal group technique conducted by community partners. The prioritized foci for the intervention were: 1) fear of HIV diagnosis (e.g., not knowing that HIV treatment is effective, free, and available regardless of immigration status), 2) inaccurate perception of risk (e.g., not knowing that HIV can be asymptomatic, associating HIV with homosexuality), and 3) competing priorities, especially with work, that reduce concern about HIV testing.
Working with the BCHD outreach team, JHU researchers, and a community coalition made up of eight members, students in the studio developed the intervention concept and messaging, the campaign identity design and branding direction, and the content of the individual intervention modules through a three-part process: research/immersion (where the students learned more about the specific problem to be addressed and the culture and context of the project), ideation (where the students generated as many ideas as possible for the intervention), and pitch (where the students presented ideas to the community). At each stage, the partners engaged in an iterative process of review and feedback, incorporating additional community voice through a total of 10 focus groups. Methods of information dissemination, including the development of animated video modules, were created from this iterative process of presenting multiple ideas and options to the partners and members of the community via focus groups, and then refining ideas based on the feedback. Specifically, through the focus groups with Latino immigrants details of the intervention, including the name ¡Sólo Se Vive Una Vez! (or simply ¡Vive!), design colors, fonts, module storylines, and pictures, were selected.
Through this partnership process, the multilevel (individual and community level) campaign ¡Vive! was created to reduce HIV-related stigma and increase HIV testing, particularly among foreign-born Latino men. ¡Vive! products include: 1) four graphic animation modules with three storylines each that address the identified priority areas (one addresses multiple priorities), and 2) photographs and designs for a community-wide anti-stigma social marketing campaign. Details of the intervention development are published elsewhere.43
Each animated module presents three stories of heterosexually-identifying Latino immigrant men who decide to get tested for HIV. They discuss the reasons why they have not been tested previously (i.e., they did not think they were at risk because they do not have sex with prostitutes), why they decided to get tested (i.e., they spoke to a healthcare worker who told them they could get HIV from having sex with women who were not prostitutes), and then the outcome of the test and how they feel as a result. Each animated module has one character testing positive for HIV, who then informs the viewer that his results are confidential, he takes one pill a day, he receives his medicine for free, he is healthy, and he is not at risk of deportation because of his HIV status. Each of the men's stories end with a variation of the phrase “You only live once. Get tested for HIV every 6 months.” Finally, at the end of the three stories, information for local testing sites with Spanish-language services are presented. The goal of this study was to conduct a pilot evaluation of the video modules only (available online at: https://www.youtube.com/watch?v=zIDBX6cuYaA [fear of HIV diagnosis]; https://www.youtube.com/watch?v=vYEXsQ-yCSk [inaccurate perception of risk]; and https://www.youtube.com/watch?v=2qhmiCagpks [competing priorities]).
Study Design and Sample Population
From June to August 2016, we conducted a cross sectional study to pilot the ¡Vive! modules among a convenience sample of foreign-born Latino men in Baltimore, Maryland. Trained research assistants recruited respondents at selected street- and community-based venues frequented by foreign-born Latinos, as informed by our prior work mapping and assessing locations for sampling the Latino immigrant population in Baltimore.44
Participants were eligible for inclusion if they identified as male, were 18 years of age or older, from a Spanish-speaking country in Latin America, and self-reported not testing for HIV in the past year. Research assistants approached individuals at each venue to describe the survey details (including content of questions, confidentiality, risks of participation, time required for participation, and incentive for participation) and assess eligibility. Of 295 people approached about the survey, 135 (45.8%) agreed to screen for eligibility. If eligible, the research assistant read an informed consent form and obtained oral consent from the participant before beginning the survey. The survey was completed by the participant on paper, with help from the research assistant as necessary, in an area of the street- or community-based venue that allowed privacy for the participant. The Institutional Review Board of the Johns Hopkins School of Medicine approved the study.
Survey Measures and Module Evaluation
The eligibility screener, delivered in Spanish, inquired about: 1) socio-demographics (i.e., age, country of origin, length of time in the U.S. and Baltimore, educational attainment) and 2) history of HIV testing (if ever tested, and if so date of last test). If eligible, the participant then completed the survey that inquired about: 1) relationship status (including, if in a relationship, length of the relationship, if the participant is monogamous with their partner, and if they believe their partner is monogamous); 2) recent sexual history (i.e., number of vaginal and/or anal sex partners in the past year, frequency of condom use); 3) barriers to HIV testing; 4) intention to test for HIV in the next three months (pre- and post-module viewing); 5) thoughts/feedback on the module; and 6) interest in rapid oral HIV testing. At the start of the survey, and then again after watching the module, participants were asked “How likely is it that you will be tested for HIV in the next three months?” Participants then circled a number from 1 (not probable) to 10 (very probable). Participants were asked to select the best response for why they have not recently (or ever) tested for HIV: 1) I don't want to know if I have HIV. It just means I know I will die; 2) I don't want to know if I have HIV. I don't want to take a lot of pills; 3) I don't want to know if I have HIV. I don't have insurance and could not pay for any treatments; 4) I don't know where to go to get tested; 5) I'm healthy. I'm not sick so I don't need to be tested; 6) I don't want people to see me get tested and think I have HIV; 7) I am not at risk for HIV; 8) I'm afraid that if I have HIV I will get deported; and 9) I am too busy / no time to get tested.
Participants completed a portion of the survey with the research assistant that included the socio-demographic questions, intention to test for HIV in the next three months, and the reason for not testing for HIV in the past year or ever. Based on the barrier selected, the research assistant identified the appropriate module for the participant (using pre-developed selection criteria). For example, if the participant selected “I'm healthy. I'm not sick so I don't need to be tested” they were shown the module for inaccurate perception of risk explicitly stating that a person with HIV can look and feel healthy. If the participant selected “I don't want to know if I have HIV. It just means I know I will die” then they were shown the module for fear of diagnosis which had information about current HIV treatment modalities and accessibility to all, regardless of immigration or insurance status. The research staff showed the selected module to the participant on a tablet computer. Only three modules were screened – one for each priority. For purposes of simplification, the combination module was not included in this pilot evaluation. After viewing the module, the second portion of the survey was administered by the research assistant. This second section of the survey included a question about intention to test for HIV in the next three months (post-module assessment), feedback on the module, and interest in rapid oral HIV testing. The survey, including watching the module, took approximately 10-15 minutes to complete and participants received $10 compensation.
Data Analysis
All analyses were conducted with SPSS Software Version 23.0. Descriptive analysis of all variables was conducted. Sociodemographic differences between eligible participants and persons screened but ineligible, and between participants who had ever tested and never tested for HIV, were assessed using t-test or chi-squared tests, as appropriate. A variable “at possible risk for HIV” was constructed, and participants were categorized as possibly at risk for HIV if they: 1) were sexually active, not in a mutually monogamous relationship, and reported inconsistent condom use, or 2) were in a mutually monogamous relationship and had not tested for HIV since beginning the relationship (i.e., report being in the relationship for one year and their last HIV test three years ago). Paired t-test assessed a change in intention to test for HIV within the next three months pre- and post-module viewing. Bivariate analyses assessed relationships between change in intention to test for HIV and socio-demographic variables. Effect size was calculated using the Cohen's d statistic.
RESULTS
Socio-demographic Characteristics of the Participants
Of 135 people screened, 113 (83.7%) were eligible. Almost all of those eligible, 104 (92.0%), completed the survey. No differences in age, country of origin, education, time in the U.S, or time in Baltimore were observed between those who were eligible and those who were not.
Socio-demographic characteristics of the 104 participants are presented in Table 1. The age of participants ranged from 18 to 74 years, with a mean age of 38.5 years (sd = 12.2). Participants were overwhelmingly from Central America (El Salvador [24.0%], Guatemala [12.5%], Honduras [21.2%]) and Mexico (31.7%). Participants reported low educational attainment, with 23.1% reporting never having attended school and 38.5% reporting attending school through 8th grade or less. Only 23.1% reported having a high school diploma (or equivalent). Participants had lived in the U.S. for an average of 9.9 years (sd = 6.3) and in Baltimore for 7.2 years (sd = 5.2).
Table 1.
Sociodemographic characteristics of participants in the ¡Solo Se Vive Una Vez! module pilot evaluation study and associations with ever having tested for HIV (n = 104).
| Variable | # (%) | Ever Tested for HIV | p-value |
|---|---|---|---|
| Age (mean, sd) | 38.5 (12.2) | ||
| Country of Origin | |||
| El Salvador | 25 (24.0%) | 13 (52.0%) | ns |
| Guatemala | 13 (12.5%) | 4 (30.8%) | |
| Honduras | 22 (21.2%) | 12 (54.5%) | |
| Mexico | 33 (31.7%) | 16 (48.5%) | |
| Other | 11 (10.6%) | 7 (63.6%) | |
| Education | |||
| No schooling | 24 (23.1%) | 11 (45.8%) | ns |
| 8th grade or less | 40 (38.5%) | 18 (45.0%) | |
| Some high school | 16 (15.4%) | 9 (56.3%) | |
| High school diploma/GED | 21 (20.2%) | 12 (57.1%) | |
| College degree | 3 (2.9%) | 2 (66.7%) | |
| Time in the U.S. | |||
| Less than 10 years | 49 (47.1%) | 16 (32.7%) | 0.001 |
| 10 years or more | 55 (52.9%) | 36 (65.5%) | |
| Time in the Baltimore | |||
| Less than 10 years | 73 (70.2%) | 30 (41.1%) | 0.005 |
| 10 years or more | 31 (29.8%) | 22 (71.0%) |
Sexual Behavior and HIV Testing History
Reported sexual behavior and HIV testing history of participants are provided in Table 2. In the past year, participants reported 0-20 vaginal and/or anal sex partners, with a mean of 2.1 sex partners (sd = 3.0). One-third (31.7%) of the participants reported having a romantic partner in Baltimore, although only 39.4% of these participants reported being monogamous to this partner and felt confident that their partner was monogamous as well. Almost half of the participants reported consistent condom use (43.3%). Based on reported sexual behaviors, 95 (91.3%) of the participants would be considered at possible risk for HIV infection.
Table 2.
Sexual partnerships, sexual behaviors, and HIV testing history among participants in the ¡Solo Se Vive Una Vez! module pilot evaluation study (n = 104).
| Variable | # (%) | Ever Tested for HIV | p-value |
|---|---|---|---|
| Has ever tested for HIV | 52 (50.0%) | --- | |
| Age (if ever tested); mean (sd) | 35.7 (11.6) | --- | |
| Years since last HIV test (if ever tested); mean (sd) | 3.48 (3.55) | --- | |
| Number of sex partners in the past year (mean, sd) | 2.1 (3.0) | --- | |
| Has a romantic/regular partner in Baltimore | 0.058 | ||
| Yes | 33 (31.7%) | 21 (63.6%) | |
| No | 71 (68.3%) | 31 (43.7%) | |
| Relationship is mutually monogamous (n = 33) | 0.015 | ||
| Yes | 13 (39.4%) | 5 (38.5%) | |
| No | 20 (60.6%) | 16 (80.0%) | |
| Condom Use | ns | ||
| Never | 38 (36.5%) | 18 (47.4%) | |
| Sometimes | 16 (15.4%) | 12 (75.0%) | |
| Most of the time | 5 (4.8{%) | 2 (40.0%) | |
| Always | 45 (43.3%) | 20 (44.4%) | |
| At Risk for HIVa | ns | ||
| Yes | 95 (91.3%) | 3 (33.3%) | |
| No | 9 (8.7%) | 49 (51.6%) | |
| Reason for not testing for HIV | 0.016 | ||
| I don't want to know if I have HIV. It just means I know I will die. | 3 (2.9%) | 1 (33.3%) | |
| I don't know where to go to get tested. | 10 (9.6%) | 7 (70.0%) | |
| I'm healthy. I'm not sick so I don't need to be tested. | 23 (22.1%) | 5 (21.7%) | |
| I am not at risk for HIV. | 39 (37.5%) | 20 (51.3%) | |
| I'm afraid if I have HIV I will get deported. | 1 (1.0%) | 0 (0.0%) | |
| I am too busy / no time to get tested. | 28 (26.9%) | 19 (67.9%) |
Participants were categorized as possibly at risk for HIV if they: 1) are sexually active, not in a mutually monogamous relationship, and report inconsistent condom use, or 2) are in a mutually monogamous relationship but have not tested for HIV since beginning the relationship.
Half (50.0%) of the participants had ever tested for HIV. Among those who had previously tested, the mean time since their last test was 3.48 years (sd = 3.55). Participants reporting that they had ever tested were significantly older than those who had not (41.4 years compared to 35.7 years; p = 0.015). Length of time in the U.S. and Baltimore was also associated with reporting ever having tested for HIV. Participants living in the U.S. and/or Baltimore for 10 or more years were significantly more likely to have ever received an HIV test than those living in the U.S. and Baltimore less than 10 years (Χ2 =11.2, p = 0.001 and Χ2 =7.8, p = 0.005, respectively). People in a partnership in Baltimore were more likely to have ever tested for HIV, although this association was only marginally significant (Χ2 = 3.6, p = 0.058); however, participants in a mutually monogamous relationship were significantly less likely to be tested than those with a partner but not monogamous (Χ2 = 5.88, p = 0.015).
Reasons for not testing for HIV ever or recently included believing they are not at risk for HIV (37.5%), being too busy to take the time to get tested (26.9%), testing is not needed because they are healthy (22.1%), not knowing where to get tested (9.6%), fear of death if positive (2.9%), and fear of deportation if positive (1.0%) (Χ2 = 13.88, p = 0.016). Participants reporting that they did not have time to test for HIV were more likely to have reported ever testing, although this association was only marginally significant (Χ2 = 5.46, p = 0.065).
¡Sólo Se Vive Una Vez! (You Only Live Once) Intervention Module Evaluation
At the beginning of the survey, participants were asked their likelihood of testing for HIV in the next three months before answering the additional survey items. On a scale from 1 (not likely) to 10 (very likely), the mean likelihood response was 4.9 (sd = 3.6) (Table 3). Based on the reason provided for not testing for HIV ever or in the previous year, participants watched a module addressing inaccurate perception of risk to HIV (69.2%), lack of priority of HIV testing (26.9%), and fear of HIV (3.8%). At the completion of the survey, and after watching the module selected, participants were asked again about their likelihood of testing for HIV in the next three months. The post-viewing mean was 7.0 (sd = 3.3), significantly higher than the previewing response (t = −8.28, p < 0.001). A medium effect size of the intervention was observed (d = 0.60).
Table 3.
¡Sólo Se Vive Una Vez! (You Only Live Once) intervention module evaluation findings (n = 104).
| Variable | # (%) | Ever Tested for HIV | p-value |
|---|---|---|---|
| Module Viewed | 0.065 | ||
| Inaccurate Perception of Risk | 72 (69.2%) | 32 (44.4%) | |
| Fear of HIV | 4 (3.8%) | 1 (25.0%) | |
| Not a priority | 28 (26.9%) | 19 (67.9%) | |
| Reported learning something new from the video | ns | ||
| Yes | 101 (97.1%) | 50 (49.5%) | |
| No | 3 (2.9%) | 2 (66.7%) | |
| Found the video interesting | ns | ||
| Yes | 101 (97.1%) | 50 (49.5%) | |
| No | 3 (2.9%) | 2 (66.7%) | |
| Likelihood of testing for HIV in the next 3 months | < 0.001 | ||
| Before watching the intervention module; mean (sd) | 4.9 (3.6) | --- | |
| After watching the intervention module; mean (sd) | 7.0 (3.3) | --- |
Twenty-five individuals (24.0%) rated their likelihood of testing in the next three month as a 10 prior to watching the module. Among the 79 participants reporting a likelihood less than 10, 68.4% reported an increase likelihood of testing after watching the module. Considering only those who did not report a high probability of HIV testing in the next three months prior to viewing the module (i.e., not reporting this as a 10), a large effect size was observed (d = 1.2). Reporting an increased likelihood of testing after viewing the module was not associated with any sociodemographic characteristics or reported sexual behaviors.
After watching the module, participants were also asked for feedback on the module. The majority of participants found the module interesting (97.1%) and stated that they learned something new (97.1%). Forty-two (40.4%) participants provided a response to an open-ended question requesting feedback on the module. Twenty (47.6%) of these responses included a statement regarding their need to be tested for HIV.
Interest in a Rapid Oral HIV Test
To help in the planning of the implementation of the intervention and possible linkages to services, we asked participants about the acceptability of rapid oral HIV testing. The majority of participants reported that they would be willing to take a rapid oral HIV test (86.5%). Preference for taking a rapid oral HIV test varied. Of those willing to take a rapid oral test (90 participants), 42.2% preferred to have the test administered by a healthcare worker in a clinical setting, 33.3% preferred to have the test administered by a healthcare worker in a community setting (i.e., health fair, community event, health van), and 24.4% preferred to administer the test themselves in a private setting.
DISCUSSION
Latinos are disproportionately impacted by HIV, with undocumented foreign-born men being at the highest risk for delayed diagnosis and presentation to care.5-8 Latinos in the U.S. may face significant structural and sociocultural barriers to accessing healthcare services in general, and HIV-related services in particular, and community-based HIV-related services that adequately address structural barriers must still deal with sociocultural barriers to access such as HIV-related stigma. To address continued barriers to community-based HTC in Baltimore, we worked with partners to create the multilevel (individual and community level) ¡Sólo Se Vive Una Vez! campaign. Together, this campaign seeks to individually address concerns about HIV testing and treatment by Latino immigrant men while simultaneously aiming to alter the cultural context of community beliefs about HIV. Research suggests that the use of multilevel interventions that include complementary individual and community level components can have synergistic impact on reducing HIV risk and improving testing and linkage to care.45-47 This study aimed to consider the impact of the individual intervention component as a first step to evaluating the comprehensive ¡Sólo Se Vive Una Vez! intervention.
This pilot evaluation of three animated video modules addressing key barriers to HIV testing among foreign-born Latinos in Baltimore demonstrated the potential effectiveness of this campaign component. Watching one of the three modules, individually selected based on participant response, significantly increased the participant's 0 reported likelihood of testing in the next three months. Participants reported positive feedback about the modules, and nearly 50% of those who provided a feedback statement about the module mentioned the need or desire to test for HIV.
We did not find any associations with an increased likelihood of testing after watching the module and sociodemographic characteristics or reported sexual behavior suggesting that the modules may have potential generalizability for this population (i.e., certain age groups or persons from specific countries of origin were not more likely to increase their intention to test). Although a more intensive evaluation is warranted, this potential generalizability to Latino immigrant men may be very important given the extent of the population that has not previously tested or has not tested in the past year despite risk to HIV infection. Of 135 people screened for this study, 113 (83.7%) were eligible as a result of not having been tested for HIV ever or in the past year, and of the 104 participants who enrolled, 50% had never tested for HIV.
Behavioral intentions are understood to be a critical component of many health behavior models, including the Theory of Planned Behavior and Theory of Reasoned Action, but the “intention-behavior gap” remains an important focus of research.48-50 Particularly, research has demonstrated that more vulnerable populations may be less likely to act on intention as a result of barriers faced when attempting the action.51 Therefore, the next steps for evaluating the individual component of the intervention is to determine if increased intention to test as a result of viewing the modules leads to increased testing.
To reduce the “intention-behavior gap” by removing barriers that hinder completion of the intended action, the modules could be viewed in a community setting with an option to test at that time. Partnering with local community-based organizations could allow for lay health advisors to use private space to conduct a rapid HIV test at that time, or the health advisory could immediately link the participant to existing mobile outreach and testing programming in the area. Given that participants expressed some interest in self-testing using a rapid oral HIV test, lay health advisors could also provide a testing kit at this time. However, more research on the acceptability and feasibility of at-home testing among this population is needed. Additionally, other methods of dissemination of the individual intervention component should also be considered. We used the lay health advisor model as this is a method supported by data in this population, but social network and social media dissemination methods could be explored, especially if paired with at-home HIV testing.
There are several limitations to our study. The pre-post intervention assessment design, in which all data was collected at one time, limits the ability to make causal associations related to previous HIV testing or to assess whether increased intention to test for HIV led to HIV testing among participants. In addition, the individual intervention modules were created with and for heterosexual-identifying men. Since most of the recruitment, enrollment, and survey completion took place at street venues, we elected not to ask participants about their sexuality. Thus, we are unable to know if men who do not identify as heterosexual, and who are not the targeted audience for the modules, were included in our sample. Almost a quarter of the participants reported at the start of the survey they were very likely to test for HIV in the next three months. It is possible that this was influenced by social desirability since the research assistant was often aware of their answer. The results are also limited by the relatively small sample size of this pilot study, which was not powered to fully evaluate associations between participant characteristics and prior HIV testing. Finally, this survey was conducted primarily among foreign-born Latinos living in Baltimore, and our findings may not be generalizable to Latino populations in other areas. However, our results may be relevant to other urban areas with rapidly growing Latino immigrant communities, many of which have similar community characteristics and challenges as Baltimore.
This pilot evaluation demonstrates the potential usefulness of the individual intervention component of the ¡Sólo Se Vive Una Vez! intervention. The multilevel intervention also includes a community component aimed at reducing HIV-related stigma, which was also developed in partnership with the BCHD Latino outreach team, community members and leaders, and the Maryland Institute College of Art. The next step will be to conduct an evaluation of the multilevel intervention to its impact on community-wide stigma beliefs and timely HIV testing.
Opt-out testing during routine medical care does not reach all populations at risk for HIV, particularly those with limited access to care, such as foreign-born Latinos not eligible for health insurance coverage under the Affordable Care Act. While community-based services such as HIV testing and counseling by promotoras/es, or lay health workers, in mobile testing vans address many of the structural barriers faced by the Latino community, sociocultural barriers, such as HIV-related stigma and inaccurate perception of risk, continue to cause diagnostic delays. Given the disproportionate impact of HIV on the Latino community, culturally tailored interventions to reduce HIV-related stigma and improve HIV prevention, testing, and linkage to care are needed.
ACKNOWLEDGEMENTS
This work was funded through a supplemental grant from the Johns Hopkins University Center for AIDS Research (P30AI094189). We would like to thank Mariela Pinedo and Holly Dalton for assistance in data collection and management, respectively. We would also like to acknowledge Mike Weikert, Ryan Clifford, Nate Gulledge, and the students in the Maryland Institute College of Art Center for Social Design Practice-Based Studio course of the 2014-2015 academic year.
Footnotes
MEETING AT WHICH PART OF THIS DATA WERE PRESENTED
Data on the pilot evaluation has not been presented elsewhere. Information on the development of the Sólo Se Vive Una Vez! (You Only Live Once) intervention was presented at the 142nd Annual American Public Health Association Meeting and is published in the journal Progress in Community Health Partnerships.
Grieb SMD, Flores-Miller A, Clifford R, Zelaya C, Page KR. Development of a tailored mHealth platform to improve HIV testing and linkage to care in a new immigrant receiving community. 142nd Annual American Public Health Association Meeting, New Orleans, Louisiana.
Grieb SMD, Flores-Miller A, Gulledge N, Clifford R, Page KR. ¡Vive! : Designing an Intervention to Improve Timely HIV Diagnosis Among Latino Immigrant Men. Progress in Community Health Partnerships. In press.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Contributor Information
Suzanne M. Dolwick Grieb, Johns Hopkins University School of Medicine, Center for Child and Community Health Research, 5200 Eastern Avenue, Mason F. Lord Bldg – Center Tower Suite 4200, Baltimore, Maryland 21224.
Alejandra Flores-Miller, Baltimore City Health Department, Alejandra.Flores-miller@baltimorecity.gov.
Kathleen R. Page, Johns Hopkins University School of Medicine, Division of Infection Disease, Baltimore City Health Department, kpage2@jhmi.edu.
REFERENCES
- 1.Centers for Disease Control and Prevention Monitoring selected national HIV prevention care objectives by using HIV surveillance data – United States and 6 U.S. dependent areas, 2010. HIV Surveillance Supplemental Report 2012. 2012;17(3 Part A) [Google Scholar]
- 2.Centers for Disease Control and Prevention Diagnoses of HIV infection and AIDS in the United States and Dependent areas, 2010. HIV Surveillance Report 2012. 2012:22. [Google Scholar]
- 3.Centers for Disease Control and Prevention HIV among Latinos. Available at: http://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/
- 4.Chen M, Rhodes PH, Hall IH, et al. Prevalence of undiagnosed HIV infection among persons aged ≥13 years--National HIV Surveillance System, United States, 2005-2008. MMWR. Morb Mortal Wkly Rep. 2012;61(Suppl):57–64. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Late versus early testing of HIV – 16 sites, United States, 2000-2003. MMWR. Morb Mortal Wkly Rep. 2003;52:581–586. [PubMed] [Google Scholar]
- 6.Dennis AM, Napravnik S, Sena AC, et al. Late entry to HIV care among Latinos compared with non-Latinos in a southeastern US cohort. Clin Infect Dis. 2011;53(5):480–487. doi: 10.1093/cid/cir434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poon KK, Dang BN, Davila JA, et al. Treatment outcomes in undocumented Hispanic immigrants with HIV infection. PloS one. 2013;8(3):e60022. doi: 10.1371/journal.pone.0060022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Espinoza L, Hall HI, Selik RM, et al. Characteristics of HIV infection among Hispanics, United States 2003-2006. J Acquir Immune Defic Syndr. 2008;49(1):94–101. doi: 10.1097/QAI.0b013e3181820129. [DOI] [PubMed] [Google Scholar]
- 9.Chen NE, Gallant JE, Page KR. A systematic review of HIV/AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2012;14(1):65–81. doi: 10.1007/s10903-011-9497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelley CF, Hernandez-Ramos I, Franco-Paredes C, et al. Clinical, epidemiologic characteristics of foreign-born Latinos with HIV/AIDS at an urban HIV clinic. AIDS Read. 2007;17(2):73–74, 78-80, 85-88. [PubMed] [Google Scholar]
- 11.Dennis AM, Wheeler JB, Valera E, et al. HIV risk behaviors and sociodemographic features of HIV-infected Latinos residing in a new Latino settlement area in the Southeastern United States. AIDS Care. 2013;25(10):1298–1307. doi: 10.1080/09540121.2013.764964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention Estimated Lifetime Risk for Diagnosis of HIV Infection Among Hispanics/Latinos --- 37 States and Puerto Rico, 2007. MMWR. Morb Mortal Wkly Rep. 2010;59(40):1297–1301. [PubMed] [Google Scholar]
- 13.HIV-CAUSAL Collaboration. Ray M, Logan R, et al. The effect of combined antiretroviral therapy on the overall mortality of HIV-infected individuals. AIDS. 2010;24:123–37. doi: 10.1097/QAD.0b013e3283324283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Granich RM, Gilks CF, Dye C, et al. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 15.Law MG, Prestage G, Grulich A, et al. Modelling the effect of combination antiretroviral treatments on HIV incidence. Aids. 2001;15(10):1287–1294. doi: 10.1097/00002030-200107060-00011. [DOI] [PubMed] [Google Scholar]
- 16.Das M, Chu PL, Santos GM, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5:e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang CT, Hsu HM, Twu SJ, et al. Decreased HIV transmission after a policy of providing free access to highly active antiretroviral therapy in Taiwan. J Infect Dis. 2004;190:879–85. doi: 10.1086/422601. [DOI] [PubMed] [Google Scholar]
- 18.Montaner JS, Lima VD, Harrigan PR, et al. Expansion of HAART coverage is associated with sustained decreases in HIV/AIDS morbidity, mortality and HIV transmission: the “HIV Treatment as Prevention” experience in a Canadian setting. PloS One. 2014;9(2):e87872. doi: 10.1371/journal.pone.0087872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Branson BM, Handsfield HH, Lampe MA, et al. Recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. Morb Mortal Wkly Rep. 2006;55(RR14):1–17. [PubMed] [Google Scholar]
- 20.DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. 2016 Jul 14; Available at: http://aidsinfo.nih.gov/guidelines.
- 21.World Health Organization Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2013 Jun; Available at: http://www.who.int/hiv/pub/guidelines/arv2013/en/ [PubMed]
- 22.Dang BN, Giordano TP, Kim JH. Sociocultural and structural barriers to care among undocumented Latino immigrants with HIV infection. J Immigr Minor Health. 2012;14(1):124–131. doi: 10.1007/s10903-011-9542-x. [DOI] [PubMed] [Google Scholar]
- 23.Grieb SMD, Desir F, Flores-Miller A, et al. Qualitative assessment of HIV prevention challenges and opportunities among Latino immigrant men in a new receiving city. J Immigr Minor Health. 2015;17(1):118–124. doi: 10.1007/s10903-013-9932-3. [DOI] [PubMed] [Google Scholar]
- 24.Cristancho S, Garces DM, Peters KE, et al. Listening to rural Hispanic immigrants in the Midwest: a community-based participatory assessment of major barriers to health care access and use. Qual Health Res. 2008;18(5):633–646. doi: 10.1177/1049732308316669. [DOI] [PubMed] [Google Scholar]
- 25.Ransford HE, Carrillo FR, Rivera Y. Health care-seeking among Latino immigrants: blocked access, use of traditional medicine, and the role of religion. J Health Care Poor Underserved. 2010;21(3):862–878. doi: 10.1353/hpu.0.0348. [DOI] [PubMed] [Google Scholar]
- 26.Harari N, Matthew D, Heisler M. Strangers in a strange land: health care experiences for recent Latino immigrants in Midwest communities. J Health Care Poor Underserved. 2008;19(4):1350–1367. doi: 10.1353/hpu.0.0086. [DOI] [PubMed] [Google Scholar]
- 27.Suthar AB, Ford N, Bachanas PJ, et al. Towards universal voluntary HIV testing and counseling: a systematic review and meta-analysis of community-based approaches. PLoS Med. 2013;10(8):e1001496. doi: 10.1371/journal.pmed.1001496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.United States Census Bureau State and County QuickFacts: Maryland. Available at: http://www.census.gov/quickfacts/table/PST045215/24,48321,00.
- 29.Maryland State Data Center Census 2000 data and information. Available at: http://www.mdp.state.md.us/msdc/
- 30.Maryland Department of Health and Mental Hygiene Baltimore City HIV / AIDS epidemiological profile. Available at: http://phpa.dhmh.maryland.gov/OIDEOR/CHSE/Shared%20Documents/Baltimore%20City% 20HIV%20AIDS%20Epidemiological%20Profile%2012-2011.pdf.
- 31.Ayala GX, Vaz L, Earp JA, et al. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res. 2010;25(5):815–840. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rhodes SD, Foley KL, Zometa CS, et al. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. American J Prev Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 33.Chen N, Erbelding E, Yeh HC, et al. Predictors of HIV testing among Latinos in Baltimore City. J Immgr Minor Health. 2010;12(6):867–874. doi: 10.1007/s10903-009-9297-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen NE, Meyer JP, Bollinger R, et al. HIV testing behaviors among Latinos in Baltimore City. J Immgr Minor Health. 2012;14(4):540–551. doi: 10.1007/s10903-012-9573-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McFall AM, Dowdy DW, Zelaya CE, et al. Understanding the disparity: predictors of virologic failure in women using highly active antiretroviral therapy vary by race and/or ethnicity. J Acquir Immune Defic Syndr. 2013;64(3):289–298. doi: 10.1097/QAI.0b013e3182a095e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simoni JM, Huh D, Wilson IB, et al. Racial/Ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. 2012;60(5):466–472. doi: 10.1097/QAI.0b013e31825db0bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levy V, Prentiss D, Balmas G, et al. Factors in the delayed HIV presentation of immigrants in Northern California: Implications for voluntary counseling and testing programs. J Immigr Minor Health. 2007;9:49–54. doi: 10.1007/s10903-006-9015-9. [DOI] [PubMed] [Google Scholar]
- 38.Grieb SMD, Shah H, Flores-Miller A, et al. HIV-related stigma among Spanish speaking Latinos in an emerging immigrant receiving city. J Immigrant Minor Health. 2016:e1–8. doi: 10.1007/s10903-016-0497-9. [DOI] [PubMed] [Google Scholar]
- 39.O'Donnell CR, O'Donnell L, San Doval A, et al. Reductions in STD infections subsequent to an STD clinic visit. Using video-based patient education to supplement provider interactions. Sex Transm Dis. 1998;25(3):161–8. doi: 10.1097/00007435-199803000-00010. [DOI] [PubMed] [Google Scholar]
- 40.Rhodes SD, McCoy TP, Vissman AT, et al. A randomized controlled trial of a culturally congruent intervention to increase condom use and HIV testing among heterosexually active immigrant Latino men. AIDS Behav. 2011;15(8):1764–75. doi: 10.1007/s10461-011-9903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Amico KR. A situated-Information Motivation Behavioral Skills Model of Care Initiation and Maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychol. 2011;16(7):1071–1081. doi: 10.1177/1359105311398727. [DOI] [PubMed] [Google Scholar]
- 42.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. A J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 43.Grieb SMD, Flores-Miller A, Gulledge N, et al. ¡Vive! : Designing an Intervention to Improve Timely HIV Diagnosis Among Latino Immigrant Men. Prog Comm Health Partners. 2016;10(3):365–372. doi: 10.1353/cpr.2016.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leite L, Buresh M, Rios N, et al. Cell phone utilization among foreign-born Latinos: A promising tool for dissemination of health and HIV information. J Immigr Minor Health. 2014;16:661–669. doi: 10.1007/s10903-013-9792-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coates T, Kulich M, Celentano D, et al. Effect of community-based voluntary counselling and testing on HIV incidence and social and behavioural outcomes (NIMH Project Accept; HPTN 043): a cluster-randomised trial. Lancet Glob Health. 2014;2(5):e267–277. doi: 10.1016/S2214-109X(14)70032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DiClemente RJ, Jackson JM. Towards an integrated framework for accelerating the end for the global HIV epidemic among young people. Sex Educ. 2014;14(5):609–621. doi: 10.1080/14681811.2014.901214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Beyrer C, Baral S, Kerrigan D, et al. Expanding the space: inclusion of most-at-risk populations in HIV prevention, treatment, and care services. J Acquir Immune Defic Syndr. 2011;57(Suppl 2):S96–99. doi: 10.1097/QAI.0b013e31821db944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Godin G, Conner M, Sheeran P. Bridging the intention–behaviour “gap”: The role of moral norm. Brit J Social Psychol. 2005;44:497–512. doi: 10.1348/014466604X17452. [DOI] [PubMed] [Google Scholar]
- 49.Scholz U, Schüz B, Ziegelmann JR, et al. Beyond behavioural intentions: Planning mediates between intentions and physical activity. Brit J Health Psychol. 2008;13:479–494. doi: 10.1348/135910707X216062. [DOI] [PubMed] [Google Scholar]
- 50.Sheeran P. Intention–behavior relations: A conceptual and empirical review. In: Stroebe W, Hewstone M, editors. European review of social psychology. Wiley; London: 2002. pp. 1–36. [Google Scholar]
- 51.McGarrity LA, Huebner DM. Behavioral intentions to HIV test and subsequent testing: the moderating role of sociodemographoic characteristics. Health Psychol. 2014;33(4):396–400. doi: 10.1037/a0033072. [DOI] [PubMed] [Google Scholar]