Abstract
Oropharyngeal and esophageal candidiases remain significant causes of morbidity in human immunodeficiency virus (HIV)-infected patients, despite the dramatic ability of antiretroviral therapy to reconstitute immunity. Notable advances have been achieved in understanding, at the molecular level, the relationships between the progression of HIV infection, the acquisition, maintenance, and clonality of oral candidal populations, and the emergence of antifungal resistance. However, the critical immunological defects which are responsible for the onset and maintenance of mucosal candidiasis in patients with HIV infection have not been elucidated. The devastating impact of HIV infection on mucosal Langerhans' cell and CD4+ cell populations is most probably central to the pathogenesis of mucosal candidiasis in HIV-infected patients. However, these defects may be partly compensated by preserved host defense mechanisms (calprotectin, keratinocytes, CD8+ T cells, and phagocytes) which, individually or together, may limit Candida albicans proliferation to the superficial mucosa. The availability of CD4C/HIV transgenic mice expressing HIV-1 in immune cells has provided the opportunity to devise a novel model of mucosal candidiasis that closely mimics the clinical and pathological features of candidal infection in human HIV infection. These transgenic mice allow, for the first time, a precise cause-and-effect analysis of the immunopathogenesis of mucosal candidiasis in HIV infection under controlled conditions in a small laboratory animal.
INTRODUCTION
Oropharyngeal candidiasis (OPC) is the most frequent opportunistic fungal infection among human immunodeficiency virus (HIV)-infected patients, and it has been estimated that more than 90% of HIV-infected patients develop this often debilitating infection at some time during progression of their disease (374, 375). Although the incidence of OPC in HIV infection has been significantly reduced since the introduction of highly active antiretroviral therapy (HAART) (280), it remains a common opportunistic infection in HIV-infected patients. Clinically, OPC in HIV infection has been classified as exhibiting pseudomembranous and erythematous variants, or angular cheilitis (2). The pseudomembranous form of HIV-associated OPC is characterized by the presence of multifocal smooth white papular lesions that can usually be rubbed away, leaving a red surface, and surface pseudohyphae can be readily detected. The erythematous form of OPC typically presents as diffuse and multiple foci of macular erythema involving the palate, oropharynx, buccal mucosa, and dorsal tongue, but hyphae are frequently absent. OPC is frequently complicated by esophageal candidiasis, which may limit food consumption and lead to weight loss, threatening the general health and well-being of HIV-infected patients (428). Furthermore, clinical and in vitro resistance to antifungal azoles frequently occurs in OPC when CD4+ cell counts fall to <200 cells/mm3 of blood, either by selection or acquisition of resistant strains of Candida albicans or by infection with inherently resistant species of Candida other than C. albicans (273, 332, 343, 344, 354, 380, 445). Of added concern, the full potential impact of antiretroviral therapy on the ability to reconstitute immunity (10, 21, 22, 55, 111, 292, 323, 324, 395) and therefore to reduce the incidence of OPC and esophageal candidiasis (67, 68, 470) has been hampered (362, 429) by suboptimal adherence (235, 441, 443), toxicity (125), and resistance (316, 337) to antiretrovirals, as well as the limited availability of these treatments in developing countries where most HIV-infected patients reside (104).
The leading cause of candidiasis, C. albicans, is an imperfect diploid dimorphic fungus that resides as a commensal of the mucosae and the gastrointestinal tract. Intraoral C. albicans is found in ∼40% of healthy humans (16). However, colonization often leads to opportunistic mucosal or life-threatening deep-organ infection in immunocompromised hosts. Invasion of the human gastrointestinal mucosa by C. albicans and its passage across the bowel wall into the bloodstream is an important portal of entry for this opportunistic pathogen into the neutropenic host, leading to systemic or disseminated candidiasis (114, 451). Hematogenous candidiasis is a frequent complication in the treatment of patients with acute leukemia (2, 278). In contrast, Candida fungemia is infrequent in HIV-infected patients and is confined mainly to the late stage of HIV infection (247, 333, 438).
The predisposition for OPC and esophageal candidiasis among HIV-infected patients, initially attributed to T-cell impairment, is enigmatic (72, 74, 240, 446). Colonization of oral mucosal surfaces and symptomatic disease are closely correlated with the development and progression of the cellular immunodeficiency of HIV infection (230, 311, 414). However, because Candida colonization of the keratinocyte surface occurs without invasion of the submucosa, the occurrence of this superficial fungal disease in a T-cell-poor environment has not been adequately explained. The onset of lesions depends on imbalances between Candida virulence attributes and progressively impaired host mucosal defenses in the sequential development of HIV infection, but the exact pathways leading to this imbalance are still unclear. The enhanced risk of OPC and esophageal candidiasis in HIV infection stands in striking contrast to the unenhanced incidence of vaginal candidiasis in HIV-infected women (255, 389), indicating that mucosal immune defense mechanisms and/or their perturbations which favor candidiasis in HIV infection are anatomically compartmentalized (158, 160, 250).
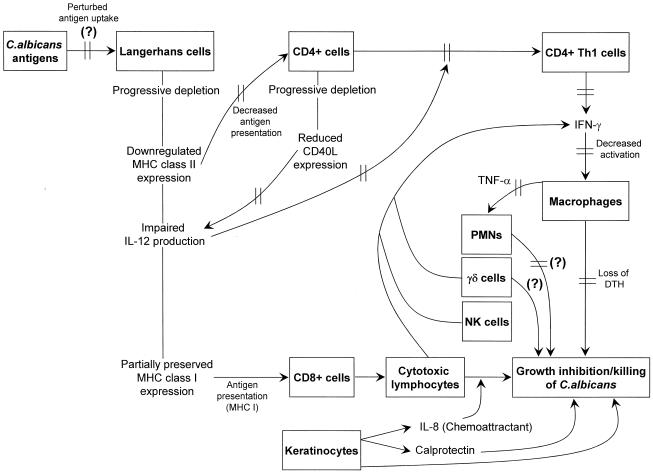
A large body of work conducted with experimentally infected intact or congenitally immunodeficient mice has provided a foundation for understanding the critical roles of Th1 CD4+ T cells, CD8+ T cells, γδ T cells, macrophages, and polymorphonuclear leukocytes (PMNs) in host defense against mucosal and systemic candidiasis (19, 29, 149, 150, 213, 446). The results of these investigations indicated that protection against mucosal candidiasis involves the recruitment and interactive collaboration of several cell populations which, together, can prevent invasion of mucosal surfaces by C. albicans in the normal host. It is thus evident that multiple, rather than single, defects in host defense mechanisms potentially underlie mucosal candidiasis in HIV-infection.
In this review, the salient clinical features of OPC and esophageal candidiasis are correlated with mucosal immune defense mechanisms against C. albicans and their perturbations in HIV infection. We also describe how a novel experimental model of oroesophageal candidiasis in transgenic (Tg) mice expressing HIV and developing an AIDS-like disease (116, 363) can be used as a new and powerful tool to investigate critical issues regarding innate and acquired immunity at the level of the oral and esophageal mucosa.
OROPHARYNGEAL AND ESOPHAGEAL CANDIDIASES IN THE SETTING OF HIV INFECTION
Clinical Features and Pathology
The pseudomembranous and erythematous variants of OPC represent the most common clinical presentations of mucosal candidiasis associated with HIV-infection (12). Further clinical variants include angular cheilitis (12), exfoliative cheilitis (360), and Candida-associated palatal papillary hyperplasia (359). Recognition of these specific forms of oral candidiasis in HIV-infected patients is facilitated by utilizing established clinical diagnostic criteria (12, 178). Symptoms may include burning pain, altered taste sensation, and difficulty swallowing liquids and solids (155). The pseudomembranous form can be easily diagnosed by demonstrating the presence of candidal yeast and pseudohyphae on wet mounts or stained smears of material obtained by swabbing the lesions and is confirmed by isolation of Candida species on culture. In the erythematous form, however, the sparse presence of Candida at the mucosal surface frequently requires a biopsy and periodic acid-Schiff staining to establish a formal diagnosis.
At least 75% of HIV-infected patients with OPC have concurrent AIDS-associated (70a) esophageal candidiasis (263) confirmed by histopathology of biopsy material obtained at endoscopic examination (355). While 30 to 43% of these patients may not have symptoms of esophageal involvement, a majority have symptoms including dysphagia and odynophagia (80, 428). For this reason, the combination of OPC and these symptoms of esophagitis is highly predictive of esophageal involvement, and these patients can receive empirical antifungal therapy without confirmation of the diagnosis by endoscopy (15, 349, 428). However, patients who fail to respond to antifungal treatment require esophageal biopsy to assess the possibility of azole-resistant Candida, other opportunistic pathogens including herpes simplex virus and cytomegalovirus, and lymphoma or Kaposi's sarcoma.
Because procurement of oral tissue samples is restricted for ethical reasons (358), only a limited number of studies have been conducted to determine the histopathologic and ultrastructural features of OPC in HIV infection (147, 357, 358, 367). In erythematous candidiasis, Candida hyphae are few while blastoconidia may be found on an atrophic epithelial surface. In contrast, hyphae are numerous and extend into the spinous cell layer in pseudomembranous candidiasis, accompanied by parakeratosis, acanthosis, and spongiosis of the infected superficial epithelium (357). Of interest, hyphae have been observed to penetrate through intercellular spaces, suggesting that Candida can engage in thigmotropism (contact guidance), a phenomenon commonly seen in plant fungi and also recognized in C. albicans in vitro (398). In some cases, hyphae are seen to traverse spinous cells and display appressoria-like appendages at their extremities, another common feature in plant fungi which enhances the strength of attachment of the exploring fungal tip (357). Intercellular penetration of hyphae is also facilitated by the detachment of epithelial cell desmosomes, presumably by C. albicans secretory aspartyl proteinases (SAPs) and/or phospholipase (357). This particular feature is also observed in non-HIV-infected patients with OPC (294). In addition to the marked contrast in penetration of the epithelium by C. albicans in pseudomembranous and erythematous candidiasis, these two forms of OPC are distinguished by the nature and intensity of the mucosal inflammatory cell response (147, 357, 358, 367). The erythematous form in both HIV-infected and uninfected patients is characterized by abundant neutrophilic microabcesses in the parakeratin layer of the epithelium, while microabcesses are rarely found in pseudomembranous candidiasis, even underneath foci of extensive hyphal colonization of the parakeratin layer (147, 358, 367). Indeed, some HIV-infected patients with pseudomembranous candidiasis have almost no epithelial inflammatory response (147, 357). In both clinical forms, however, an abundant mononuclear cell response is observed in the submucosa with no significant difference between HIV-infected and -uninfected patients with the exception of an enhanced infiltration in HIV-infected compared to HIV-uninfected patients with pseudomembranous candidiasis. Immunohistochemical analysis has demonstrated that the inflammatory response in both forms of OPC consists predominantly of CD8+ T cells and CD1a+ Langerhans cells (367). The mechanisms which govern the more intense inflammatory response in erythematous compared to pseudomembranous candidiasis remain unknown but are probably independent of HIV infection and its progression since these differences are also observed in patients who are not infected with HIV (147).
Epidemiology
The development of molecular biology-based methods for discriminating Candida strains (121) has provided a vital tool to determine the relationships between progression of HIV infection; acquisition, maintenance, and clonality of oral candidal populations; and selection of resistant C. albicans or non-albicans species of Candida following sustained treatment with antifungal azoles. Using these methods, a number of longitudinal studies have been conducted with HIV-infected patients to prospectively examine the molecular epidemiology of recurrent OPC (32, 246, 344, 354, 380, 445). The majority of patients (77 to 100%) with OPC are infected with C. albicans, while the remaining patients are infected with one or more non- albicans species of Candida, either alone or in combination with C. albicans (32, 246, 344, 354, 380, 445). A diversity of non-albicans species of Candida are found, including Candida tropicalis. Candida parapsilosis. Candida guillermondii. Candida glabrata, and Candida dubliniensis. However, among these species only C. dubliniensis has been specifically associated with and recognized as the sole cause of OPC in HIV infection (88, 246, 290, 386, 422, 445). Analysis of serial isolates has revealed that throughout each episode of OPC, the majority of patients are infected with a unique strain of C. albicans, originally present as a commensal of the oral cavity (32, 246, 269, 445). In a minority of patients, other patterns of recurrence are found, including strain replacement with a new genotype of C. albicans and species replacement with non-albicans species of Candida (344, 354, 380, 445). Fluconazole resistance may occur through acquisition of a new resistant genotype of C. albicans or by development of resistance in a previously susceptible strain (380). Surprisingly, C. albicans strains colonizing HIV-infected patients prior to the first episode of OPC and antifungal therapy exhibit an increased frequency of phenotypic switching which increases the proportion of phenotypes in the colonizing population which are resistant to fluconazole (444). After the first OPC episode, risk factors for the emergence of recurrent OPC caused by fluconazole-resistant C. albicans include lower CD4+ cell counts, a greater number of treated episodes of OPC, and a greater duration of prior fluconazole treatment (156, 273). Although colonization with azole-resistant C. glabrata increases after treatment with fluconazole (402) it is rarely if ever isolated as the sole cause of recurrent OPC (159, 273, 380, 445). In vitro resistance to fluconazole is strongly correlated with clinical failure of fluconazole treatment of OPC in HIV-infected patients (273, 354, 380) and failure to respond to fluconazole therapy in experimental OPC and esophageal candidiasis (450). The molecular mechanisms of resistance to azole antifungals in C. albicans strains isolated from HIV-infected patients are multifactorial, with a predominance of overexpression of genes (MDR1 and CDR) encoding efflux pumps, detected in 85% of all resistant isolates (332). Alterations in the gene encoding the target lanosterol 14-α-demethylase enzyme, including functional amino acid substitutions and overexpression of the gene that encodes the enzyme (ERG11), are detected in 65 and 35% of the resistant isolates, respectively (332). Overall, multiple mechanisms of resistance are combined in 75% of the isolates displaying high-level fluconazole resistance (332). Although azole-resistant C. albicans strains usually remain confined to a single patient with HIV infection and OPC, the potential for transmission of resistant isogenic strains of C. albicans among couples (33, 380) and family members including children (301) has been clearly established.
Although HIV-infected women may develop both OPC and vaginal candidiasis, the risk of OPC alone is enhanced by HIV-infection (255, 389). Molecular typing of C. albicans colonizing HIV-infected women revealed that concurrent oral and vaginal isolates were in all cases dissimilar, suggesting that the dominant strains of C. albicans colonizing these different mucosal sites are distinct (102). These differences may indicate an ability of specific genotypes of C. albicans to colonize different ecological niches or may result from interhuman transmission of different genotypes to separate mucosal sites.
Correlation with Progression of HIV Infection
OPC and esophageal candidiasis can occur at any time during the course of HIV infection, including primary HIV infection (82, 330), the chronic asymptomatic phase and overt AIDS (1, 80, 152, 177, 237, 277, 285, 329, 366, 389). During the chronic asymptomatic phase, both erythematous and pseudomembranous candidiases are predictive of progressive immunodeficiency and onset of AIDS, independently of the CD4+ cell count (129, 224, 230, 311). Oral burdens of C. albicans are augmented in HIV-infected patients even prior to the first episode of OPC (439, 445, 467), and the intensity of carriage increases significantly in the progression from asymptomatic Candida carrier to an episode of OPC (445). These observations indicate that normal defenses against Candida are perturbed early in the progression of HIV infection before any marked depletion of CD4+ cells has occurred. However, the prevalence of the pseudomembranous form of OPC (152, 237, 277, 285, 329, 445) and esophageal candidiasis (1) increases dramatically in advanced HIV disease associated with CD4+ cell counts of <200/mm3, while erythematous candidiasis and angular cheilitis are less strongly associated with late disease (152, 329, 366). The association of lower CD4+ cell counts and OPC has also been established in HIV-infected women (177, 389) and children (80). Higher HIV RNA burdens are also associated with an enhanced risk of OPC and esophageal candidiasis (1, 53, 277, 329) and inversely correlated with CD4+ cell counts, especially in the absence of treatment with HAART. Overall, these findings suggest that while depletion of CD4+ cells below a critical threshold of 200 cells/mm3 most often triggers the onset of OPC and esophageal candidiasis, other as yet unidentified perturbations of mucosal immunity against Candida appear early during the progression of HIV infection.
Impact of Antiretroviral Therapy
The introduction in 1996 of HAART including protease inhibitors dramatically reduced the prevalence of OPC (17, 68, 127, 280) and esophageal candidiasis (120, 207, 222) in HIV-infected patients. Over a period of 12 months after starting antiretroviral treatment including a protease inhibitor, significant decreases were found in the prevalence of OPC (from 30-56% to 1-9%) (17, 68, 127, 280), the number of relapses of OPC (127), the rate of asymptomatic oral carriage of C. albicans (280), and oral candidal burdens (17). An equally striking diminution in the incidence of Candida esophagitis ranging from 29 to 42% occurred during the period from 1996 to 1998 compared with the first half of the decade (pre-HAART) (120, 207, 222). A comparable decline in the incidence of esophageal candidiasis has been observed in HIV-infected children since the introduction of HAART (222).
The mechanisms underlying the dramatic impact of HAART on the incidence of OPC and esophageal candidiasis have received close attention (10, 17, 21, 39, 67, 68, 127, 292) and provide valuable insights into understanding the perturbations of mucosal defense mechanisms against C. albicans in HIV-infection. Several observations indicate that increases in CD4+ cell counts in response to HAART confer immunologic reconstitution and a decreased incidence of opportunistic infections. Episodes of OPC and esophageal candidiasis that continue to occur despite HAART have done so at low CD4+ cell counts, and patients whose CD4+ cell counts have increased in response to HAART are at lower risk (17, 127, 222, 280), establishing a correlation between CD4+ cell recovery and a decreased incidence of mucosal candidiasis. A three-phase T-cell reconstitution has been demonstrated after HAART, with an early rise in the number of memory CD4+ cells, an improved CD4+ cell reactivity to recall antigens, and a late rise in the number of naive CD4+ cells (21, 22, 292). In addition, proliferative responses to the mitogen phytohemagglutinin develop in the majority of patients in whom responses were absent at baseline (10, 292), and there is increasing interleukin-2 (IL-2), IL-12, and IL-10 production (10). It could therefore be hypothesized that HAART reduces the incidence of mucosal candidiasis by reconstituting delayed-type hypersensitivity to C. albicans antigens and a protective mucosal Th1 response to C. albicans (42, 70, 211) and rectifying the shift to a nonprotective Th2 response resulting from HIV infection (83). However, in contrast to the frequent recovery of a proliferative response to phytohemagglutinin, treatment with HAART results only in late and inconsistent recovery of anticandidal cellular immunity, as assessed either by skin test reactivity for delayed-type hypersensitivity or by a proliferative response to C. albicans antigens (17, 67, 68, 292). These findings, associated with the resolution of refractory OPC in some HAART-treated patients well before the recovery of CD4+ cell counts and response to Candida antigens (67, 68), indicate that the decreased incidence of OPC in patients receiving HAART cannot be fully accounted for by reconstitution of Candida cell-mediated immunity (67, 68). Indeed, decrease of the viral load after HAART therapy (10) may also ameliorate mucosal candidiasis by correcting a dysfunction of neutrophils induced by HIV envelope glycoprotein gp41 (143, 168, 454) or by increasing the neutrophil count in HIV-infected patients with neutropenia (127, 471). Evidence has also been presented that HAART has an early, immune reconstitution-independent inhibitory effect on C. albicans Saps in the oral cavities of HIV-infected patients (67), and that HIV protease inhibitors attenuate adherence of C. albicans to epithelial cells in vitro (39). It has been shown that C. albicans strains from HIV-infected patients with OPC have increased expression of Saps (107, 321), possibly enhanced by HIV envelope gp160 and gp41 binding to C. albicans (180). Therefore, inhibition of C. albicans Saps by HIV protease inhibitors may also contribute to the amelioration of OPC and esophageal candidiasis in HIV-infected patients treated with HAART.
HISTOLOGY OF THE ORAL MUCOSA
The oral mucosa has histological features in common with the vaginal and esophageal mucosas, including a superficial stratified squamous epithelium and an underlying lamina propria of dense collagenous connective tissue, separated by a basal membrane. However, the mucosa of the oral cavity varies in cellular layer composition, depending on the position and function (145, 369, 408). The lining mucosa, including that found on the cheeks, floor of the mouth, underside of the tongue, and soft palate, represents 60% of the surface area of the oral mucosa. The stratified squamous epithelium in these areas contains a germinating layer (stratum basale) overlying the basal membrane, a spinous layer (stratum spinosum), and a superficial granular layer (stratum granulosum) and is generally nonkeratinized and therefore similar to the esophageal epithelium. The cells undergo structural differentiation as they migrate from the stratum basale to the epithelial surface (408). The masticatory mucosa, found on the gingiva and hard palate, represents 25% of the surface area of the oral mucosa and has an additional keratinized or parakeratinized surface layer resembling that of the skin but lacking a stratum lucidum (145, 369). The specialized stratified squamous epithelium of the dorsum of the tongue (15% of the surface area of the oral mucosa) contains abundant lingual papillae differentiated into four different types: filiform, fungiform, circumvallate, and foliate. The outer surface of the papillae is covered by keratinized epithelium and thus resembles the hard palate, while the interpapillary region is covered by nonkeratinized epithelium similar to that of the lining mucosa (388). The oral epithelium thus varies in the degree of keratinization, cornification, and orthokeratinous and parakeratinous layer thickness found in areas (gingiva, hard palate, and dorsal surface of the tongue) where frictional forces created by biting, chewing, or movement of food occur. Although the thickness of the human oral stratified squamous epithelium shows regional variation ranging from 190 ± 40 μm (floor of the mouth) to 580 ± 90 μm (cheeks) (388), the width of the epithelium is three to five times less in the mouse oral mucosa at each site (197).
Keratinocyte proliferation is stimulated by epidermal growth factor, transforming growth factor α, platelet-derived growth factor, and IL-1 (408). The switch between proliferation and differentiation is modulated by extracellular calcium, phorbol esters, retinoic acid, and vitamin D3 (408). To ensure a 14- to 20-day median turnover time of oral epithelial cells (408), the keratinocytes attached to the basal membrane lose integrin expression, leading to progressive morphologic changes during migration to the mucosal surface (408). Interestingly, the turnover times of mouse palate and cheek epithelia are slightly shorter than that of tongue epithelium, and the times for all of these tissues are threefold that for epidermis (197). Keratinocytes are linked by desmosomes, which increase in number from the basal to the superficial layer of the epithelium, and by nexus-like (gap) junctions (388, 392). Polygonal and more flattened, upwardly migrating cells discharge the contents of membrane-coating granules by an exocrine process into the intercellular space, forming broad lipid lamellae containing ceramides and acylceramides which serve as a permeability barrier in the keratinized stratified squamous epithelium (399, 408, 455). In nonkeratinized epithelium, intercellular lipid is nonlamellar, contains mainly cholesterol and glycosphingolipids but no acylceramides and only small amounts of ceramide, and provides a less efficient permeability barrier (399, 408, 455). Continuous desquamation of surface keratinocytes of the oral epithelium plays a pivotal role in maintaining a healthy oral mucosa and in limiting candidal colonization and infection (378).
In several regions of the oral cavity, there are nodules of lymphoid tissue consisting of crypts formed by invagination of the epithelium into the lamina propria. These areas are extensively infiltrated by lymphocytes, which play an important role in host defense against oral infections.
ALTERATIONS IN MECHANISMS OF ORAL INNATE RESISTANCE TO C. ALBICANS IN HIV INFECTION
The skin and mucosal tissues represent the primary portal of entry for opportunistic pathogens, leading to life-threatening systemic dissemination in the immunocompromised host. In the normal host, however, several redundant immunological and nonimmunological defense mechanisms directly limit the proliferation of pathogenic microorganisms, thus reducing the burden of organisms available for binding to potential attachment sites. In the oral cavity, the flow and composition of saliva establish a dynamic equilibrium between C. albicans (361) and other members of the commensal microbiota, preventing the establishment of oral candidiasis in the normal host (37). Salivary flow protects the oral cavity by dislodging yeasts and bacteria, which are then removed by swallowing, and studies have provided evidence that this process may be facilitated by binding of C. albicans to salivary mucins (139, 140) or to a nonmucin proteoglycan (198, 199). In patients with Sjögren's syndrome, however, decreased salivary flow and buffering capacity are associated with an increased frequency of carriage of C. albicans (361) and of oral candidiasis (7). The prevalence of oral candidiasis in these patients has been estimated at about 35% (7). A similar effect is observed in patients with advanced HIV infection, in whom the salivary flow rate is reduced by 40% and is also correlated with enhanced recovery of Candida from saliva (258). The incidence of oral candidiasis is also enhanced in patients with acidic saliva (373), and a low pH increases the adherence of C. albicans to epithelial surfaces in vitro (377). Glucose supplementation of saliva augments the growth rate of C. albicans in vitro, and the resulting acidic pH provides the required environment for activity of Candida Saps, which enhance virulence by degrading a wide variety of host substrates including the mucins, which play an important role in lubrication of epithelial surfaces and host defense (89, 115, 253, 307, 363, 376, 384). The pH of the mucosa also regulates the expression of the C. albicans virulence genes PHR1 and PHR2 (108) and is thus a significant environmental signal in determining the virulence capacity of Candida and/or modulation of the host defenses (372). Finally, biofilm formation by C. albicans has been implicated in the ability of the fungus to cause persistent infection on bioprosthetic materials, including denture acrylic, as well as mucosal surfaces (75, 76). However, there were no significant quantitative differences in biofilm formation between C. albicans oral isolates from HIV-infected and noninfected patients, indicating that the biofilm-forming ability of C. albicans is unlikely to contribute to high levels of oral yeast carriage in cases of HIV infection (212).
Several salivary anticandidal proteins, including lysozyme, lactoferrin, the histatins, calprotectin, and antileukoprotease, inhibit the growth of C. albicans and its attachment to the oral epithelium. Because saliva from HIV-infected patients shows decreased anticandidal activity (258), several investigations have focused on identifying putative defects in salivary antimicrobial proteins which may favor oral candidiasis in HIV infection. Lysozyme and lactoferrin are two major nonimmunological antimicrobial proteins in saliva which possess concentration-, time-, and strain-dependent fungicidal activity against C. albicans in vitro (379, 466). Lysozyme is found at a concentration range of 1.5 to 57 μg/ml of saliva (350, 419), and its antifungal properties are thought to be mediated by the enzymatic hydrolysis of N-glycosidic linkages in the microbial cell wall and injury to the cytoplasmic membrane following direct cationic-protein binding (279). Interestingly, concentrations of salivary lysozyme are increased in HIV-infected patients with or without oral candidiasis (20, 199, 274, 467), and a trend toward progressive in vitro resistance to lysozyme has been observed in genetically similar, sequential oral C. albicans isolates from patients infected with HIV (379). Because the concentration of lysozyme is increased in HIV-infected patients while the anticandidal activity of saliva is decreased, the contribution of salivary lysozyme to limiting the proliferation of C. albicans in the oral cavity of these patients appears doubtful.
Lactoferrin is a member of the transferrin family of nonheme iron-binding glycoproteins and is found at the mucosal surface, where it functions as a prominent component of the first line of host defense against infection (452). The concentration of lactoferrin in unstimulated saliva is about 7 to 20 μg/ml (126, 371), and its fungicidal activity against C. albicans (404) has been attributed not only to sequestration of ferrous ions (284) but also to structural damage to the fungal cell wall (313) and activation of intracellular autolytic enzymes (243). Salivary concentrations of lactoferrin in patients with HIV infection have been variously reported to be increased (20, 258), unchanged (276), or decreased (266, 300). These variable results have been at least partly ascribed to the source of the saliva, because increased concentrations of lactoferrin in HIV infection have been found in submandibular but not parotid saliva (20, 258, 274). The predisposition to oral candidiasis in HIV-infected patients is thus not convincingly associated with defective production of lactoferrin. In contrast to lysozyme, serial genotypically identical oral isolates of C. albicans from HIV-infected patients did not develop progressive in vitro resistance to lactoferrin (379). The therapeutic potential of lactoferrin for the treatment of OPC has recently led to the development of mucoadhesive lactoferrin tablets with fungicidal activity against C. albicans and C. glabrata (239). This novel approach to the treatment of mucosal candidiasis will require further validation in clinical trials.
The family of salivary histatins consists of at least 12 low-molecular-weight, structurally related, histidine-rich, cationic proteins, which also contribute to nonimmunological host defense of the oral mucosa (138, 437). The histatins have broad fungicidal activity against pathogenic fungi, including C. albicans, Cryptococcus neoformans, and Aspergillus fumigatus (194), and are present at 50 to 425 μg/ml (244) in the saliva of healthy adults. Histatin 5, which exerts potent candidacidal activity (138), is internalized by C. albicans, inhibits the respiration of mitochondria, and induces the formation of reactive oxygen species leading to mitochondrial and cytoplasmic membrane damage, efflux of ATP and other nucleotides, and cell death (183, 194). The mechanism of action of the histatins is thus distinct from that of other cationic peptides such as the defensins, which can directly insert into and disrupt cell membranes because of the strongly amphipathic nature of their α-helical structures (138). The concentration of histatins in the saliva of HIV-infected patients has been determined to be increased (20) unchanged (258), or decreased (244, 274), and these seemingly discordant results may have been caused by the different stages of HIV infection among the patients under study as well as by the analytical methods employed. However, decreased concentrations of histatins appeared to correlate with an increased tendency to oral candidiasis in a subgroup of HIV-infected patients (274), suggesting that decreased histatin concentrations and/or an inability of these proteins in saliva to interact with C. albicans may contribute to the defective salivary anticandidal activity seen in HIV-infected patients (244). Interestingly, transfer of the gene encoding histatin 3 in the salivary glands of rats by using recombinant adenovirus vectors resulted in its expression at up to 1,045 μg/ml of saliva, suggesting that a gene transfer approach to overexpression of naturally occurring antifungal proteins may be potentially useful in the management of mucosal candidiasis (317).
The heterodimeric calcium- and zinc-binding protein calprotectin is produced by PMNs, monocytes, macrophages and mucosal keratinocytes (54, 73, 403). In vitro, calprotectin quantitatively inhibits the growth of C. albicans by depriving the fungus of zinc, which is essential for microbial growth (138). Salivary calprotectin concentrations and oral keratinocyte expression of calprotectin are augmented in response to oral candidiasis, in both HIV-infected and -uninfected patients (146, 231, 424). However, the results of two independent studies demonstrated that salivary concentrations of calprotectin are deficient in HIV-infected patients with oral candidiasis or high salivary Candida counts compared to those in HIV-infected patients without oral candidiasis or with low salivary Candida counts (298, 424). These results suggested that a diminution of this antimicrobial factor may predispose to oral candidiasis in HIV infection. On examination of the oral mucosa of HIV-infected patients with OPC, however, Candida hyphae were found to penetrate through the epithelial parakeratin layer yet did not extend beyond the zone of spinous-layer keratinocyte calprotectin expression (147). Further studies are required to determine whether reduced salivary calprotectin is not simply associated with but directly contributes to the predisposition to oral candidiasis in HIV-infected patients.
Antileukoprotease (436), also known as secretory leukocyte protease inhibitor (141), is produced by keratinocytes (457) and constitutes the last member of the family of antimicrobial proteins involved in nonimmunological defense against C. albicans at mucosal sites. Like other cationic antimicrobial polypeptides, the antimicrobial activity of antileukoprotease is limited to conditions of low ionic strength. In addition to its inhibition of leukocyte-derived proteinases, antileukoprotease has fungicidal activity by an unknown mode of action against C. albicans which is localized primarily in the NH2-terminal domain (436) and it may thus play an important role in the innate mucosal defense. Interestingly, antileukoprotease exhibits anti-HIV-1 activity in vitro and may contribute to the antiviral activity of saliva associated with the infrequent oral transmission of HIV-1 (287).
ORAL MUCOSAL IMMUNE SYSTEM AND HOST DEFENSES AGAINST C. ALBICANS
Cells with Immune Potential in the Oral Mucosa
The oral mucosa is continuously challenged by the resident microbial flora and occasionally by microbial pathogens; it is therefore armed with several cell populations which individually, or in association, can produce a protective innate or acquired immune response. Mucosal cell populations with immune potential include Langerhans' cells, macrophages, αβ- and γδ-T cells, keratinocytes, and PMNs. We now review the specific properties of these cell populations and their role in host defense.
Lymphoid cells.
The oral mucosal immune system possesses features in common with both the skin immune system and the mucosal immune system (442). The normal oral mucosa shares with normal skin an absence of B lymphocytes, which are present in the mucosal immune system (50, 442). In contrast to the skin, however, T lymphocytes in the normal human oral mucosa are not organized in rows around postcapillary venules of the superficial and deep vascular networks (50) but are distributed singly or in small clusters on both sides of the basal membrane (442). In addition, T lymphocytes are only rarely found in the more superficial layer of the epithelium. The oral mucosal epithelium contains about 37 times as many T lymphocytes as the epidermis of normal skin (442). The vast majority of T lymphocytes in the oral mucosa express the memory CD45R0+ phenotype (86, 340). T lymphocytes within the oral epithelium are not activated (CD25−), in contrast to CD25+ T cells in the underlying stroma (86). The conversion of T cells from the naive CD45RA+ to the memory CD45R0+ phenotype requires repeated antigenic stimulation, suggesting that apoptotic CD25−, CD45RA+ intraepithelial T cells die after unsuccessful antigen presentation by Langerhans' cells (86).
The CD4/CD8 ratio of 1:2 in the human oral epithelium and 1:4 in the skin indicates the preferential presence of the CD8+ subset in both sites, but CD4+ cells are proportionately more frequent in the oral mucosa than in the skin (442). However, a CD4/CD8 ratio of 1 within the epithelium of the normal human gingiva indicates regional variation in the oral cavity (86). In contrast to normal humans, CD4+ cells are twice as numerous as CD8+ cells in the normal murine oral mucosa (47). CD4+ T cells are required for a Th1-type protective response against oral candidiasis in mice (149) and therefore play a central role in host defense against OPC.
Of direct relevance to host defense against OPC in HIV infection, the buccal epithelium is an inductive site for the generation of cytotoxic T-lymphocyte responses mediated by major histocompatibility complex (MHC) class I-restricted CD8+ T cells, independent of CD4+ cell help (119). It has been suggested that CD8+ T lymphocytes are attracted to the epithelium by IL-8 produced by keratinocytes (267, 442). Moreover, IL-2 (but not gamma interferon [IFN-γ])-activated CD8+ cells exert direct growth inhibition against the hyphal form of C. albicans (40). However, CD8+ cells may not be in proximity to C. albicans hyphae, which are usually confined to the upper layers of the epithelium (72, 147, 357). Alternatively, CD8+ cells may produce cytokines which enhance the antimicrobial activity of macrophages and neutrophils against C. albicans. In addition, MHC class I molecules expressed constitutively on keratinocytes may represent a target for CD8+ cytotoxic T lymphocytes after internalization by keratinocytes of microbial pathogens (448).
γδ T cells represent at most 2% of the T-cell population in the human oral epithelium (331). Oral mucosal γδ T cells display ultrastructural features typical of large granular lymphocytes, also found in cytotoxic CD8+ and NK cells (267), and probably represent a first immunologic line of defense. γδ T cells are located within the epithelium in both normal and inflamed gingiva, often in close proximity to CD1a+ and/or CD1c+ Langerhans' cells and keratinocytes (268). In inflamed mucosa the γδ T cells show the phenotype of activated cells (CD45RO+, CD8+, or CD4+), whereas in normal mucosa the cells are CD4− CD8− and express CD45RA (268). In the connective tissue, under the basal membrane, Vδ2+ γδ T cells are predominant, whereas the epithelium contains mostly Vδ1+ γδ T cells (206, 331). γδ T cells participate in the immune response to microbial pathogens including C. albicans by producing cytokines such as IFN-γ (213, 267) or by direct cell-to-cell contact leading to cytotoxicity (267, 303). Increases in the numbers of γδ T cells have been found in the oral mucosa soon after mice are colonized and infected with C. albicans (71), coinciding with resolution of infection.
Finally, natural killer (NK) cells are large granular lymphocytes which represent 6 to 39% of human gingival (268) and 3% of lower lip (283) mononuclear cells. NK cells are cytotoxic in vitro to certain tumor cell lines and to virally infected cells (72) and have direct antimicrobial activity against Cryptococcus neoformans (256) but little or no effect against C. albicans hyphae in vitro (40).
Langerhans' cells.
Langerhans' cells develop from bone marrow stem cells as one of three distinct subsets of dendritic cells (DCs) which home in to selected tissues (30, 99, 448). The bone marrow stem cells appear to be common precursors of both macrophages and DCs (30). Serving as an essential link between innate and acquired immunity, dendritic cells function as antigen-presenting cells (APCs) that patrol all tissues of the body, capturing pathogens for processing and presentation to T cells in the secondary lymphoid organs. Two subsets of human DCs, Langerhans' cells and interstitial (or dermal) DCs, belong to the myeloid lineage, while the third subset is composed of lymphoid DCs (99). Culture of human CD34+ hematopoietic progenitors in the presence of granulocyte-macrophage colony-stimulating factor (GM-CSF) and tumor necrosis factor alpha (TNF-α) gives rise to CD1a+ DCs related to Langerhans' cells and CD14+ DCs closely related to interstitial DCs, which can differentiate into macrophages in the presence of M-CSF (69). DCs are thus phenotypically and functionally heterogeneous depending on their specific differentiation pathways (11, 468, 469). Serving as sentinels for pathogen entry at the epithelium of the skin and mucosa, Langerhans' cells, identified by expression of CD1a, Lag, and langerin, are localized on the basal and suprabasal layers and represent 2 to 4% of the cells in the epithelium (6, 34, 49, 59, 96, 99, 103, 216, 245, 262, 351, 356, 365, 390, 391, 442). These cells express MHC class II molecules and are also CD11b+ and CD11c+. Langerhans' cells have a pronounced dendritic shape and contain rod-shaped organelles called Birbeck granules. Immature epithelial Langerhans' cells are equipped to capture antigens by phagocytosis, macropinocytosis, and receptor-mediated absorptive endocytosis, including the macrophage mannose receptor, DEC-205, as well as Fcγ and Fcɛ receptors (30). The loose interaction of DC-specific, ICAM-3 grabbing, nonintegrin (DC-SIGN) with ICAM-3 establishes the initial contact of the Langerhans' cell with a resting T cell in the apparent absence of foreign antigen (416). To successfully present antigens for T-cell activation, Langerhans' cells must undergo a maturation process (334) triggered by whole bacteria, bacterial lipopolysaccharide, cytokines such as TNF-α and IL-1β, or the T-cell CD40 ligand (CD40L) (30, 99, 216, 458). Mature Langerhans' cells lose the ability to take up antigens but express surface molecules required for communication with T cells at the immunologic synapse (416). During maturation, Langerhans' cells express high levels of surface MHC class I and II and the costimulatory molecules CD54, CD58, and CD86 that interact with receptors on T cells to enhance adhesion (30, 99, 416). In addition, high CD40 expression on mature Langerhans' cells favors binding to CD40L on T cells, which in turn up-regulates the expression of CD80 and CD86, secretion of IL-12, and release of chemokines such as IL-8 and macrophage inflammatory proteins 1α and 1β (MIP-1α and MIP-1β) (30). Antigen presentation via MHC class II molecules in the presence of IL-12 and collaborating IL-18 induces CD4+ cells to differentiate into IFN-γ-producing Th1 cells, leading to activation of the antimicrobial properties of macrophages, and is therefore critical to the induction of a protective acquired cell-mediated immune response (30, 99, 308). Furthermore, Langerhans' cells receiving T-cell help mediated by CD40-CD40L interactions (385) can also present antigen on MHC class I molecules to cytotoxic CD8+ cells, which can be loaded through both endogenous and exogenous pathways (30, 99). More recent work, however, indicates that Langerhans' cells do not need to receive a signal from T cells to become fully mature DCs capable of stimulating CD4+ T cells and cytotoxic CD8+ T cells (110). Interestingly, the murine oral mucosa is an inductive site for priming class I-restricted CD8+ cytotoxic T cells in vivo (119). The expression of MIP-3α by TNF-α-stimulated keratinocytes in the spinous layer (77, 435) and the production of defensins (464), which both recognize the CCR6 chemokine receptor in immature DCs, may explain the positioning of Langerhans' cells in the epidermis and their ready access to microbial pathogens (99). The mobilization of Langerhans' cells and their migration via afferent lymphatics to draining lymph nodes for antigen presentation (208) is governed by the upregulation of the chemokine receptor CCR7 and the production of MIP-3β (405). In addition, IL-18 produced by Langerhans' cells and keratinocytes also contributes to the regulation of Langerhans' cell migration by a TNF-α and IL-1β-dependent mechanism (98).
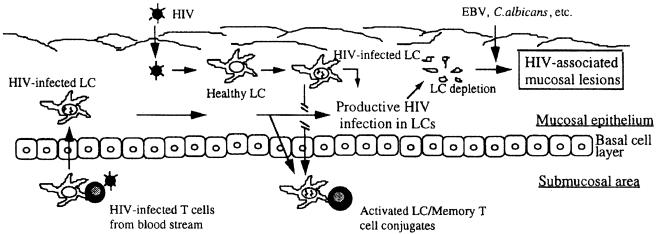
In normal humans, the density of Langerhans' cells in nonkeratinized oral mucosa is apparently the same as in the skin, but keratinized oral mucosa has fewer Langerhans' cells (96, 103, 442). Although murine palate implants are repopulated by Langerhans' cells within 2 weeks (365), the numerical densities of Langerhans' cells in old mice is reduced compared with that in young mice (364). At the ultrastructural level, murine and human Langerhans' cells in the oral mucosa exhibit no significant differences (59). In the normal human oral mucosa, however, Langerhans' cells present a highly variable morphology according to their epithelial location (391). In contrast to the upper epithelium, where CD1a+ Langerhans' cells have long dendrites forming a network, Langerhans' cells in the basal layer are more rounded and have very few short dendrites. Functionally, the well-developed dendritic morphology of Langerhans' cells in the upper epithelium could reflect optimal immune surveillance (391). Conventionalization of germfree mice with a bacterial flora results in enhanced migration of Langerhans' cells to the oral epithelium (49), and the densities of oral epithelial Langerhans' cells are increased in patients with chronic periodontitis compared to healthy controls (216), demonstrating that Langerhans' cells are recruited to the oral epithelium in response to a bacterial challenge. Purified human (35) or rat (192) oral mucosal Langerhans' cells can serve as APCs in vitro and are more efficient than skin Langerhans' cells in providing costimulatory signals to T cells (193). C. albicans-specific T-cell activation by human epidermal Langerhans' cells (85, 223) requires not only the ligation of the T-cell receptor to the antigen-MHC complex but also costimulation by the combination of adhesion molecules CD54 and CD58 with CD11a and CD2 on T cells, respectively (433). As described in further detail below, productive infection of oral mucosal Langerhans' cells by HIV-1 may contribute to their selective depletion (81) and perturb their ability to generate a primary immune response (44), which may impair protective mucosal immunity against colonization and infection by opportunistic microbial pathogens. In addition, Langerhans' cells serve as the portal of entry for HIV-1 at mucosal sites and are critical to the initiation and subsequent spread of infection to draining lymphoid tissue (340).
Keratinocytes.
Keratinocytes are of primary importance in the pathogenesis of OPC since they constitute a physical barrier after adhesion of C. albicans to the epithelial surface. In addition to their role as a mechanical barrier, epithelial keratinocytes function as fixed or immobile immunocytes and are capable of producing a number of soluble factors and expressing receptors that are involved in up-regulating and down-regulating immune responses (179, 415, 440). The major growth factors produced include basic fibroblast growth factor, platelet-derived growth factors, transforming growth factors α and β, and TNF-α. Keratinocytes also produce several cytokines including IL-1, IL-3, IL-6, IL-7, IL-8, IL-10, IL-12, IL-15, IL-18, and IL-20, and a number of CSFs such as GM-CSF, G-CSF, and M-CSF (14, 45, 179, 440, 448). Under normal conditions, most of these mediators are not constitutively produced (162), but their gene expression and release is up-regulated during inflammation by a variety of external stimuli derived from leukocytes, Langerhans' cells, and keratinocytes themselves, including IFN-γ, TNF-α and IL-17 (14, 241, 257, 282, 432, 448). Interestingly, mRNA expression of IL-1α, IL-1β, IL-8, GM-CSF, and TNF-α is up-regulated in experimental cutaneous C. albicans infection with reconstituted human epidermis, demonstrating that the fungus induces a brisk cytokine response by host keratinocytes (383). C. albicans also triggers the production of IL-1α and TNF-α (410), as well as GM-CSF (131), by primary oral epithelial cells and oral epithelial cell lines in vitro. In addition, proteolytic activation of the IL-1β precursor by C. albicans Sap (38) suggests that candidal proteinases may contribute to the activation and maintenance of the inflammatory response at the epithelial surface. IL-1, IL-8, and IL-12 possess attractant effects on PMNs, macrophages, and lymphocytes (448). In addition, some of the cytokines produced by keratinocytes (IL-1 and TNF-α) promote the maturation of DCs and therefore could differentially modify the ability of Langerhans' cells to respond to antigens (448). Keratinocyte-derived IL-7 and IL-15 are involved in epidermal T-cell trafficking (179, 448). In addition to the production of soluble factors, keratinocytes express the adhesion molecules CD54 and CD58, and CD54 expression is increased by IFN-γ (136, 448). MHC class I molecules are expressed constitutively and may be a target for CD8+ T cells (448). MHC class II molecules are not expressed constitutively but can be induced by IFN-γ produced by infiltrating T lymphocytes (448). Keratinocytes may function as accessory cells in antigen presentation and interact with lymphocytes to produce a Th2 cytokine response (448).
Of potential relevance to the fragile equilibrium between epithelial colonization and infection, IFN-γ promotes expression of the glycoprotein desquamin, a cell adhesion molecule in the stratum corneum of the human epidermis which possesses lectin-like properties for amino sugars (58), as well as trypsin-like serine proteinase (57) and RNase (393) activity. Desquamin may thus play a crucial role in desquamation and shedding of Candida from the superficial portion of the epithelium.
In addition to these indirect mechanisms, keratinocytes possess several potential antimicrobial mechanisms which may directly contribute to host defense against Candida. (i) Keratinocytes have been shown to express inducible nitric oxide synthase activity (43), and NO has been associated with candidacidal activity and resistance to mucosal candidiasis (213). (ii) Human oral keratinocytes produce numerous antimicrobial peptides, including β-defensins 1 to 3 (134, 135, 191, 261, 281, 387), cathelicidins (132, 166, 167, 182, 465), adrenomedullin (220, 221), calprotectin (54, 73, 146, 147, 231, 298, 370, 403, 424), and bactericidal/permeability-increasing protein (BPI) (61), which, as natural antibiotics, contribute to the innate immunity of the epithelium (170, 453). β-Defensins exhibit potent antimicrobial activity against Candida (387), and their expression by keratinocytes at the mRNA and protein level is enhanced by TNF-α, IL-1β, whole bacteria, and bacterial lipopolysaccharide (191, 261, 281, 387). Although epithelial injury or inflammatory disorders augment the expression and release of the human cathelicidin LL-37 from keratinocytes (132, 166), its antimicrobial activity in vitro has so far been demonstrated only against bacteria and the MBCs against Candida species are >100 μg/ml (182). In addition to their direct antimicrobial properties, human β-defensins and the cathelicidin LL-37 are chemotactic for immature DCs and neutrophils and for monocytes and T cells, respectively (465). Secretion of the vasoactive peptide adrenomedullin from oral keratinocytes is stimulated by IL-1α, IL-1β, TNF-α, LPS, and live bacteria but not by C. albicans (220, 221). Although adrenomedullin possesses antimicrobial properties, it is not yet known whether it contributes to host defense against oral candidiasis. As outlined previously in this review, oral keratinocytes also express calprotectin, a heterodimer of MRP8 and MRP14 with antimicrobial activity against C. albicans. The up-regulated expression of calprotectin by oral keratinocytes in response to infection has been investigated in vitro and appears to be independent of IL-1β (370). Finally, keratinocytes express on their cell membranes BPI, which is also an abundant constituent of PMNs (61, 170). BPI on keratinocytes contributes to the killing of gram-negative bacteria that become closely adherent to epithelial cells (61, 170). The role, if any, of BPI in limiting C. albicans colonization or infection of the oral mucosa remains to be determined. (iii) Human oral keratinocytes directly inhibit the growth of blastoconidia and/or hyphae of Candida species in vitro, with a strict requirement for cell contact (411). Growth inhibition appears to involve a carbohydrate moiety on the surface of the keratinocytes but is not mediated by phagocytosis, nitric oxide, superoxide-hydrogen peroxide pathways, or defensin and calprotectin antimicrobial peptides (412). Direct growth inhibition of Candida by oral keratinocytes appears to occur through a novel and distinct mechanism, complementary to other components of the antimicrobial armamentarium of oral keratinocytes. Oral epithelial keratinocytes are thus equipped with numerous redundant defense mechanisms, acting either directly or indirectly against the continuous microbial challenge at the oral mucosal surface. The role of keratinocytes in host protection against Candida at mucosal surfaces appears likely, since C. albicans hyphae are restricted to the upper layers of the oral epithelium in OPC and are some distance away from lymphocytes and Langerhans' cells located in deeper layers.
Macrophages and PMNs.
Macrophages and PMNs originate from monoblasts and myeloblasts, distinct populations of myeloid stem cells which differentiate into monocytes and neutrophils in the bloodstream. In the normal uninfected host, circulating monocytes differentiate into resident tissue macrophages, in contrast to PMNs, which are retained almost exclusively within the circulation. Because of their key role in the innate immune response (289), these two cell populations are critical effectors in the first line of defense against oral microbial pathogens. In the normal human oral mucosa, macrophages are located mainly in the lamina propria (86) while PMNs appear in the lamina propria and epithelium only in response to inflammation (268). Macrophages are not a homogeneous cell population but can be separated into biologically active subpopulations which appear at early, intermediate, or late stages of inflammation (185).
Oral mucosal resident macrophages express MHC class II molecules and CD11b, as well as Fc receptors that bind IgG (FcγR) (31). Like Langerhans' cells, macrophages present antigenic peptides to CD4+ T cells after induction of CD86 costimulatory molecules (112, 113). Th1 CD4+ T cells secrete IFN-γ and IL-2, which activate both macrophages (97) and CD8+ cytotoxic T cells to kill intracellular pathogens (113). After activation, macrophages produce TNF-α, which activates PMNs, further amplifying the innate immune response (19). For this reason, macrophages play a critical dual role at the crossroads of innate and acquired cell-mediated immunity. Indeed, activation of a specific T-cell response to C. albicans antigens in vitro has been found to require macrophages expressing MHC class II molecules (314).
To date, Langerhans' cells, monocytes, macrophages, and PMNs are the only cells that have been reported to be candidacidal (132a, 213, 310). Macrophages and PMNs have the ability to kill both C. albicans blastoconidia and hyphae by both oxygen-dependent and -independent mechanisms (446). Oxygen-dependent killing by PMNs is mediated by superoxide anion and the myeloperoxidase-hydrogen peroxide-halide system, with the added participation of reactive nitrogen intermediates including NO and peroxynitrite in the candidacidal activity of macrophages which lack myeloperoxidase (446). Production of IFN-γ by γδ T cells augments NO production by macrophages and enhances resistance to orogastric candidiasis, indicating that γδ T cells indirectly contribute to macrophage killing of C. albicans (213). Macrophages and PMNs are also equipped with oxygen-independent mechanisms including the cationic protein defensins (446) and calprotectin (54, 73, 403), demonstrating the use of an extensive array of oxidative and nonoxidative mechanisms to kill C. albicans blastoconidia and hyphae (446).
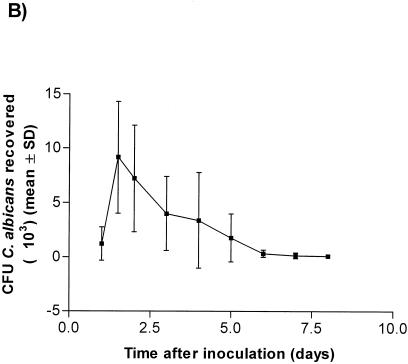
In experimental OPC in the mouse model, the early inflammatory response 24 to 48 h postinfection is composed of large numbers of PMNs migrating from the lamina propria to accumulate in the superficial epithelial layers (242). During recovery from primary infection, at 5 to 6 days postinfection, the initial influx of PMNs is replaced by a massive recruitment of macrophages in the lamina propria (71). The presence of both macrophages and PMNs in experimental candidiasis concurs with similar histologic findings in HIV-infected patients with OPC, suggesting a major role for these professional phagocytes in mucosal containment of C. albicans.
Mechanisms of Protective Cellular Immunity to C. albicans in the Oral Mucosa
A foundation for understanding the complex mechanisms critical to host defense against C. albicans at mucosal sites was provided by a large body of work conducted with experimentally infected, congenitally immunodeficient mice (26, 27, 63, 64, 209, 210, 309, 446), as well as in intact (94) or knockout (28) mice depleted of specific factors (CD4+ cells or IFN-γ). These studies demonstrated that functional T cells play a role in resistance to C. albicans colonizing or infecting mucosal surfaces and that an added defect of phagocytes is required to produce dissemination of C. albicans from the gastrointestinal tract (63, 209). Further investigation showed that, although Th1 and Th2 CD4+ cells are involved in recovery from primary gastrointestinal candidiasis in immunocompetent mice, activation of a Th1 response occurs in animals that show delayed-type hypersensitivity to Candida and protection after a second gastrointestinal inoculation (70). Studies of B-cell knockout mice demonstrated that antibodies do not play a role in protection against mucosal candidiasis or dissemination from the gastrointestinal tract (449). However, a protective role of antimannan antibodies has been demonstrated in experimental vaginal candidiasis (106, 184). Overall, these investigations have produced the current paradigm of a central role for a Th1 CD4+ response in host defense against mucosal candidiasis (42, 70, 211, 406).
In contrast to gastrointestinal and vaginal candidiasis, relatively few hypothesis-driven, cause-and-effect investigations have been conducted to specifically elucidate the mechanisms of host defense against C. albicans in the oral mucosa (157). The accumulated evidence indicates that normal host defense against OPC is the sum of individual redundant mechanisms which include several salivary anticandidal proteins, growth inhibition of C. albicans by oral keratinocytes, and the presence of T-cell-mediated delayed-type hypersensitivity to C. albicans. The evidence implicating anticandidal proteins and oral keratinocytes, described in previous sections of this review, has so far been derived solely from observations of in vitro activity against C. albicans. Although their role in host defense appears likely, no direct demonstration has been presented using compelling approaches such as their depletion, augmentation, or transfer in an experimental model of OPC. Consequently, mechanistic investigations of host defense in experimental OPC have been focused almost entirely on dissecting the precise role of an acquired cell-mediated immune response to C. albicans.
Although this has not yet been directly studied in experimental OPC, oral mucosal Langerhans' cells are most probably involved in the initiation of an acquired cell-mediated immune response to C. albicans. Both human (310) and murine (132a) DCs recognize C. albicans by the mannose-fucose receptor, can phagocytose and degrade Candida, and can subsequently present Candida antigens to T cells. Interestingly, the yeast and hyphal forms of Candida are ingested by different mechanisms and receptors. Phagocytosis of the yeast cells by DCs occurs by coiling phagocytosis, characterized by the presence of overlapping bilateral pseudopods, whereas ingestion of hyphae occurs through a more conventional zipper-type phagocytosis (132a). Human DCs kill Candida as efficiently as human monocyte-derived macrophages do, and killing appears to be mainly oxygen independent, possibly via lysosomal hydrolases (310). In contrast, killing of C. albicans yeast cells or hyphae by murine DCs is correlated with the production of NO (132a). The T-cell proliferation observed with a mixture of human DCs, Candida, and T cells most probably represents a secondary immune response, since C. albicans is a commensal in humans (310). However, analogous experiments conducted using murine DCs required the presence of IL-2 to elicit a priming response since C. albicans is not a commensal organism in mice (132a). In vitro, ingestion of the yeast form of C. albicans activated DCs for IL-12 production and priming of Th1 cells whereas ingestion of hyphae inhibited IL-12 and Th1 priming and induced IL-4 production (132a). The pivotal role of DCs in initiating the immune response to C. albicans was elegantly demonstrated by the generation of protective immunity against intravenous infection after injection of DCs ex vivo pulsed with C. albicans yeasts but not hyphae (132a). Yeast-pulsed DCs from IL-12 knockout mice primed lymphocytes for IL-4 production in vitro and were unable to confer resistance to candidiasis (132a), consistent with the lack of Th1 response development (272). Finally, work from the same group showed that murine DCs pulsed with yeast but not hyphal RNA induce protective immunity to C. albicans in allogeneic bone marrow-transplanted mice (24).
In addition to Langerhans' cells, macrophages and keratinocytes could be potentially involved in the processing and presentation of Candida antigens to CD4+ cells and could therefore also participate in the induction of an adaptive immune response to C. albicans in the oral cavity. Keratinocytes of the reproductive tract express MHC class II molecules and can function as APCs (459). In addition, expression of MHC class II molecules by epithelial keratinocytes is enhanced in patients with angular cheilitis (320) or OPC (214), possibly in response to IFN-γ produced by infiltrating T lymphocytes (18, 448). However, the ability of oral keratinocytes to engage in presentation of Candida antigens is uncertain, since these cells do not appear to have the capacity to engulf C. albicans (412), and the epithelial CD4+ cells are located above the basement membrane and therefore not in proximity to the superficial keratinocyte layer where C. albicans is localized. Although not formally demonstrated in OPC, the participation of macrophages in Candida antigen presentation is more likely, since these cells are a prominent component of the innate immune response to C. albicans and fulfill all the requirements for engulfment, killing, and presentation of C. albicans antigens to CD4+ cells (18, 173, 314). Of direct relevance to this process, the ability of human monocytes to phagocytose the yeast but not the hyphal form of C. albicans is correlated with enhanced induction of IL-12, again indicating that C. albicans yeasts are specifically involved in promoting Th1 protective immunity (79).
The initiation of the mucosal immune response to C. albicans in OPC requires the maturation and mobilization of the Langerhans' cells (30) resulting either directly from exposure to C. albicans or from cytokines produced by the T-cell response to infection (30). Maturation of DCs, including mucosal Langerhans' cells, is characterized by a strong up-regulation of MHC class II expression, secretion of IL-12, and expression of the adhesion molecules CD54, CD58 and CD86 (30). Enhancement of MHC class II expression on APCs by coculture with C. albicans or exposure to C. albicans antigens has been demonstrated in vitro (18), in accordance with the ability of microbial pathogens and their products to directly induce the maturation of DCs (30, 458). Cytokines such as IL-1, GM-CSF, and TNF-α, as well as the T-cell ligand CD40L, which binds CD40 on dendritic cells, may also contribute to maturation of Langerhans' cells in mucosal candidiasis (30). MHC class II alloantigens (173, 314, 433) and the adhesion molecules CD54 and CD58 (433) are all directly involved in Candida-specific T-cell activation by APCs and therefore most probably participate in this critical step in the afferent limb of the specific immune response in OPC.
Several lines of evidence in support of the protective role of acquired cell-mediated immunity in OPC have been presented by Ashman and colleagues, using experimentally infected mice (142, 149, 150). The differences between the colonization patterns of C. albicans in infection-resistant BALB/c mice and infection-prone DBA/2 mice following oral inoculation correlated with both Candida antigen-specific T-cell proliferation and early expression of IL-4, IFN-γ, and IL-12 in cervical lymph nodes, supporting the concept of a balanced Th1 and Th2 response in clearing OPC (142). A constitutive mixed Th1/Th2 cytokine expression (Th0) was also found in whole saliva of healthy HIV-negative individuals with (251) or without (252) Candida-associated denture stomatitis. Although associated with a Th2 response, IL-4-enhanced resistance to OPC may be mediated by the promotion of a protective Th1 response (291) and by enhanced killing of Candida by both PMNs (46) and macrophages (153). Although systemic depletion of CD4+ cells alone did not increase the severity of oral infection in immunocompetent BALB/c and CBA/CaH mice (150), reconstitution of immunodeficient BALB/c and CBA/CaH nu/nu mice with naive CD4+ but not CD8+ T cells significantly decreased oral colonization compared to that in controls and was correlated with expression of IL-12 and IFN-γ in cervical lymph nodes (149), demonstrating the direct requirement for T lymphocytes in recovery from OPC. The depletion of PMNs and the inactivation of monocytes/macrophages increased the severity of infection in immunocompetent BALB/c and CBA/CaH mice, clearly demonstrating the critical role of these professional phagocytes in the efferent limb of the immune response (150). It thus appears that the clearance of OPC is dependent on CD4+ T-cell augmentation of monocyte/macrophage and PMN functions exerted by Th1-type cytokines such as IL-12 and IFN-γ (150). A significant expansion of γ/δ T cells in the cervical lymph nodes was demonstrated after oral inoculation of C. albicans (142), and these cells may also augment the function of phagocytes by their production of IFN-γ and indirectly contribute to clearing OPC, as previously demonstrated in experimental gastrointestinal candidiasis (213).
PATHOGENESIS OF OROPHARYNGEAL AND ESOPHAGEAL CANDIDIASES IN HIV/AIDS
Evidence Implicating C. albicans Virulence Factors
The ability of C. albicans to colonize, penetrate, and damage host tissues depends on imbalances between Candida virulence attributes and specific defects in host immune defenses. C. albicans possesses a multiplicity of properties, including adhesins, dimorphism, phenotypic switching, molecular mimicry of mammalian integrins, and secretion of hydrolytic enzymes, each with a low propensity for enhancing fungal infection and none necessarily dominant, and all, even in combination, unable to fully overcome intact host defenses (319). Hydrolytic enzymes are probable virulence factors in pathogenic Candida species (reviewed in references 87, 100, 109, 202, 203 and 456). Among these, C. albicans Saps, under the control of a multigene family (SAP1 to SAP10) expressing distinct isoenzymes that are regulated differentially at the mRNA level in vitro (204, 295, 456), are implicated in the breakdown of several host substrates (202). Evidence has been presented that phospholipase B, expressed by at least two genes (PLB1 and PLB2) (249, 421), also contributes to the pathogenesis of candidiasis by the degradation of host tissues (172, 205).
Several lines of evidence implicate Saps in the pathogenesis of OPC in the setting of HIV infection. Sap antigens have been detected on the surface of blastoconidia and hyphae adhering to human oral mucosa (48), and C. albicans isolates from HIV-infected patients with OPC not only exhibited enhanced adherence to buccal epithelial cells (423) but also produced higher Sap levels in vitro than did strains isolated from an HIV-negative control group (107, 321, 462). In addition, in vivo expression of individual members of the C. albicans SAP gene family was found to be differentially regulated in a murine model of esophageal candidiasis (409), during oral infection in intact and HIV-1 Tg mice (363), and in HIV-positive and -negative patients with OPC (307). Specifically, assessment of the expression of the SAP1 to SAP6 genes by in vivo expression technology revealed that the SAP5 and SAP6 genes were strongly activated at a single time point examined during infection of the esophageal mucosa in experimentally infected, immunocompromised mice whereas only low-level expression of SAP1 to SAP4 occurred (409). A controlled sequential reverse transcription-PCR analysis of the temporal expression of individual members of the SAP gene family was conducted in a model of OPC in intact and transgenic mice that expressed HIV-1 and developed an AIDS-like disease (363). In contrast to the sustained expression of other SAP genes, SAP7 and SAP8 were conspicuously distinguished by their transient expression in both intact and transgenic mice. SAP5 and SAP9 were most strongly expressed throughout the course of infection in the transgenic mice (363). In accordance with these findings, reverse transcription-PCR analysis of the in vivo expression of the SAP1 to SAP7 genes on single samples of saliva, collected from a limited number of HIV-positive and -negative patients with OPC, revealed that SAP2 and SAP4 to SAP6 were uniformly expressed and that all seven SAP genes were simultaneously expressed in some patients (307). Expression of specific SAP genes was comparable in HIV-positive and -negative patients with OPC (307) and in immunocompetent C3H and DBA/2 mice, non-Tg controls, and HIV-1 transgenic mice (363), indicating that the HIV status does not in itself alter SAP expression. Finally, a temporal progression of SAP expression in the order SAP1 and SAP3. SAP6, and SAP2 and SAP8 was observed in an in vitro model of OPC that made use of reconstituted human epithelium (384). Taken together, these results suggest that some SAP gene products may be involved in specific steps in the onset, progression, and maintenance of OPC in HIV infection by their ability to degrade particular host substrates. This possibility is supported by the observation that although recombinant Sap1p, Sap2p, Sap3p, and Sap6p cleave peptide bonds between larger hydrophobic amino acids, substrate specificities differ among the four Sap proteins (236). Evidence implicating C. albicans Saps in the pathogenesis of OPC in HIV infection was further strengthened by studies demonstrating that the decreased prevalence of OPC in patients treated with HIV-1 protease inhibitors results not only from immune reconstitution but also from inhibition of Sap activity (65, 67, 128, 238, 304). The requirement for specific SAP genes in the pathogenesis of mucosal candidiasis may differ according to the microenvironment at individual anatomic sites, as exemplified by the loss of virulence of null sap1 to sap3 but not sap4 to sap6 mutants in an estrogen-dependent rat vaginitis model (105). In this regard, a direct role for individual C. albicans SAPs in the pathogenesis of OPC will require assessment of the virulence of targeted null mutants at this specific mucosal site.
In contrast to the substantial evidence implicating SAP genes in the pathogenesis of OPC in HIV infection, the potential role of C. albicans phospholipase at this specific mucosal site has received less attention. PLB1 mRNA transcripts were detected during the entire course of OPC, with the exception of primary infection, in Tg mice expressing HIV-1 (363). This was the first report of PLB1 expression at the mRNA level in vivo and corroborated the finding of caPlb1p secretion in the stomach (172) and kidneys (249) of experimentally infected mice. In vitro, blastoconidia, pseudohyphae, and hyphae of C. albicans expressed higher levels of PLB1 mRNA than did germ tube-forming cells, suggesting that expression of caPLB1 is regulated as a function of morphogenic transition (200). The presence of both blastoconidia and hyphae in the oral cavities of the Tg mice was therefore consistent with detection of expression of PLB1. In addition, the optimal activity of caPlb1 at pH 6.0 (172) makes it likely that the enzyme is functional in oral candidiasis. The attenuated virulence of plb1 null mutants in a hematogenous-dissemination murine model (249) and an oral-intragastric infant mouse model (172), combined with the involvement of PLB1 in the penetration and damage of host tissues (172, 249), indicates that C. albicans phospholipases also contribute to fungal virulence. However, determination of the precise role of PLB gene products in the pathogenesis of OPC in HIV-infected patients will require further analysis, including but not limited to the demonstration of attenuated virulence of plb1 null mutants in a clinically relevant model of OPC and an assessment of C. albicans phospholipase gene expression in HIV-infected patients with OPC.
Perturbed Mucosal Immune Defense Mechanisms against C. albicans in HIV-Infected Patients
Humoral immune response.
Secretory immunoglobulin A (sIgA) constitutes the predominant immunoglobulin isotype in secretions, including saliva, and is considered to be the first line of defense of the host against pathogens which colonize or invade surfaces bathed by external secretions (275). Salivary sIgA binds to a group of polydispersed heat shock mannoproteins expressed on C. albicans yeast cells and germ tubes grown at 37°C, and the highest reactivity is observed with yeast grown at pH values between 5.9 and 7.5, a range similar to that found in normal saliva (41). The possibility that specific anti-Candida sIgA antibodies may be protective was suggested by their higher concentrations in patients with oral candidiasis than in controls (144), as well as their ability to quantitatively inhibit the adherence of C. albicans to buccal epithelial cells in vitro (144, 447). However, a primary role for sIgA in protection against mucosal candidiasis remains inconsistent with the rarity of oral candidiasis in patients with selective IgA deficiency (8). In HIV infection, salivary concentrations and secretion rates of total sIgA and its subclasses have been found to be unchanged (274), increased (20, 258), or decreased (299, 425), with a lower avidity of sIgA antibodies (73, 91). In contrast, the concentration of Candida-specific salivary sIgA has been repeatedly found to be increased in HIV-infected patients despite the decreased salivary flow rate (92, 133). Furthermore, Candida-specific salivary IgA production significantly correlated with the salivary Candida load (92), suggesting that an adequate mucosal humoral immune response to C. albicans is maintained in HIV infection. It was further suggested that increased salivary C. albicans-specific sIgA antibody concentrations may be a consequence of infection instead of playing a protective role (92). In support of this interpretation, increased salivary sIgA concentrations were correlated with decreased salivary anticandidal activity in HIV-infected patients (258). More recently, a comprehensive analysis of Candida-specific antibodies in the saliva of HIV-positive patients revealed that despite changes in total immunoglobulin levels, when levels of Candida-specific antibodies were normalized to total protein or total immunoglobulin levels of the corresponding isotype, no distinct differences in IgA or sIgA were seen, regardless of the OPC status or CD4+ cell count (461). Therefore, there is no evidence of appreciable changes in levels of Candida-specific IgA in saliva that would account for the prevalence of OPC among patients infected with HIV.
Cellular immune response.
The devastating impact of HIV infection on mucosal cell populations is most probably central to the pathogenesis of mucosal candidiasis in HIV-infected patients. In several investigations, possible defects of cells with immune potential against Candida were specifically examined in the HIV setting of infection.
Oral epithelial keratinocytes play a critical role in the pathogenesis of OPC because of their close interaction with C. albicans in the superficial epithelium. Because oral epithelial keratinocytes from HIV-infected patients contain integrated HIV proviral DNA and HIV Tat/Rev RNA (347, 348), possibly acquired through contact with submucosal HIV-positive lymphocytes and/or Langerhans' cells, the anticandidal properties of these cells could be potentially impaired. However, although HIV-positive patients with OPC had a significant decrease in oral epithelial cell-mediated growth inhibition of C. albicans in vitro compared to those without OPC, there was no difference in epithelial cell activity between HIV-noninfected and -infected persons without OPC (411). Expression of IL-1 and IL-8 by keratinocytes was equivalent in HIV-positive and -negative patients with OPC, and no constitutive expression of either cytokine was found in control patients without OPC (147). As mentioned above, expression of calprotectin by keratinocytes was preserved in HIV-infected patients with OPC and appeared to serve as a keratinocyte barrier to hyphal penetration (147). Consequently, further investigation is required to firmly establish whether defects in the anticandidal mechanisms of keratinocytes contribute to the predisposition to OPC in HIV infection.
Mucosal Langerhans' cells are the initial target cells after primary mucosal contact with the virus, facilitating the transfer of HIV to CD4+ cells (81, 340, 341). Tonsils and adenoids from HIV-infected patients contain multinucleated syncytia expressing high levels of intracellular HIV Gag protein in the DC- and T-cell-rich crypt lymphoepithelium (164, 165). DCs within these areas express the viral coreceptors CD4 and CCR5 required for cell entry (217) and are selectively infected by R5 (macrophage-tropic) strains, promoting vigorous replication of HIV. DCs play two critical roles in the pathogenesis of HIV infection, first by spreading infection to and then by inducing virus-specific immune responses in draining lymph nodes (217, 340, 341). Despite being infected by HIV, oral mucosal Langerhans' cells are challenged to perform a vital task: the uptake of Candida antigens in the mucosa and their presentation to CD4+ T cells in draining lymph nodes. Several lines of evidence have now clearly demonstrated multiple defects of oral Langerhans' cells, which probably contribute to a progressive loss of protective acquired cell-mediated immune responses to C. albicans antigens in HIV infection. Numbers of both oral (81) and esophageal (78) Langerhans' cells are depleted in HIV infection, congruent with decreased numbers of cervical (368), splenic (286), and blood (36, 130, 175, 271, 322) DCs (Fig. 1). It remains unclear whether decreased DC populations result from cytopathic changes caused by productive HIV infection, cytotoxic T-cell responses resulting in lysis of targeted DCs, migration to lymph nodes where active viral replication occurs, or down-regulation of DC surface markers (36, 81). In addition, impairment of terminal differentiation of Langerhans' cells was demonstrated by decreased expression of MHC class II antigens (338, 367), as well as the presence of blunt dendrites, very limited development of organelles, and lack of Birbeck granules (367). In contrast, however, increased expression of CD40 and CD86 costimulatory molecules was observed on blood DCs from HIV-infected patients (36). HIV and its transcriptional transactivator (Tat) block the expression of MHC class II genes in HIV infection by competing with the class II transactivator (218). Expression of MHC class I antigens in APCs is also down-regulated, but to a lesser degree than expression of MHC class II molecules (218), and results from a combination of their transcriptional blockade by Tat (56, 201) and intracytoplasmic sequestration by the HIV Nef protein (176, 248). Several of the defects identified in Langerhans' cells are also present in monocytes and macrophages, including reduced expression of MHC class II and formation of MHC class II-antigen complexes (339) and altered capacity to stimulate and present antigen to CD4+ T cells (265). In addition to these defects, expression of HIV gp120 in APCs and impaired CD40L induction on CD4+ cells activated by antigens contribute to impaired IL-12 and IFN-γ production by APCs, thus preventing a protective CD4+ Th1 response as well as differentiation of CD8+ cells into cytotoxic lymphocytes (335, 420).
FIG. 1.
Hypothetical model of the role of mucosal Langerhans' cells (LC) in HIV infection. Oral mucosal Langerhans' cells serve as an initial target for HIV infection. The cytopathic changes of Langerhans' cells with a productive HIV infection contribute to selective depletion of Langerhans' cells, which may impair mucosal immunologic protection against colonization by microorganisms causing HIV-associated oral mucosal lesions. Reprinted from reference 81 with permission of the publisher.
Progressive depletion of CD8+ cells in HIV infection results from apoptosis mediated by macrophages through interaction of HIV gp120 with the chemokine receptor CXCR4 (195). Despite a progressive diminution in absolute numbers, remaining CD8+ T cells nevertheless successfully accumulate in the basal epithelial layer of the oral mucosa in HIV-infected patients with OPC, demonstrating that these cells can be actively recruited to the mucosa in response to candidiasis (305, 367). However, the precise role of CD8+ cells in mucosal containment of C. albicans in HIV infection, either by direct growth inhibition of Candida or, more likely, by an indirect mechanism, remains to be determined (157, 305).
Numbers of CD4+ T cells are strikingly reduced in the oral mucosae of HIV-infected patients with or without OPC (318, 367, 413). In addition, C. albicans-specific peripheral CD4+ cells become depleted with HIV disease progression in patients with concurrent OPC (240), but these findings have not yet been demonstrated for CD4+ cells isolated from cervical lymph nodes draining the mucosal surface. HIV-infected patients have a Th2 cytokine profile in saliva (252) consistent with the well-documented switch from Th1 to Th2 in HIV infection (83), which correlates with a loss of lymphocyte proliferation in response to Candida antigens in patients with advanced HIV infection (252, 346). However, deficiencies in Candida-specific systemic cell-mediated immunity do not solely account for susceptibility to OPC in HIV-infected patients (250). The overall evidence nevertheless suggests that the depletion and immaturity of oral Langerhans' cells may interfere with normal processing and presentation of C. albicans antigens to CD4+ cells, which are themselves depleted in HIV infection, and that perturbation of these protective mechanisms probably plays a preponderant role in the pathogenesis of OPC in HIV infection.
Potential defects of phagocytes could also predispose to OPC in patients HIV with infection. HIV-infected patients with chronically inflamed gingivae have increased numbers of mucosal macrophages and PMNs, demonstrating that HIV infection does not prevent a normal innate mucosal immune response by these cells (306). Although recruitment of phagocytes to the oral epithelium does not appear to be perturbed by HIV infection, their anticandidal properties could be impaired either directly by HIV infection or by altered stimulation by cytokines. In several investigations yielding conflicting results, phagocytosis of C. albicans by blood monocyte-derived macrophages from HIV-infected patients has been found to be either normal (312, 315) or reduced (95), possibly by HIV Nef (345). Likewise, although HIV gp41 suppresses the reduction of nitroblue tetrazolium by PMNs in vitro (168), growth inhibition of C. albicans and IL-1 and IL-6 production by PMNs were found to be preserved in HIV infection (66), while in other studies phagocytosis (143) and killing (454) of C. albicans by PMNs were impaired but without altered production of reactive oxygen intermediates (454). Interestingly, the candidacidal activity of PMNs from healthy subjects and HIV-infected patients is impaired by the Th2 cytokines IL-4 and IL-10, suggesting a role for these cytokines in mediating increased susceptibility to OPC in HIV infection (427).
In conclusion, HIV infection severely perturbs APCs and CD4+ cells, and may also reduce the function of phagocytes against C. albicans in the oral mucosa, leading to the onset of OPC. However, these critical defects may be partly compensated by preserved host defense mechanisms (calprotectin, keratinocytes, CD8+ T cells, and some activity of phagocytes), which individually or together may limit C. albicans proliferation to the superficial mucosa and prevent systemic dissemination in HIV infection.
AIDS-Like Disease in Transgenic Mice Expressing HIV-1
The above description of the numerous manifestations of HIV infection, including multiple perturbations of immune cells which express HIV as well as of the immune response to C. albicans, highlights the difficulties in studying and understanding the pathogenesis of candidiasis in the context of HIV infection. Undoubtedly, the availability of an adequate animal model would facilitate this task enormously. Unfortunately, there is no animal species in which HIV-1 can replicate and induce an AIDS-like disease. The most widely used model for AIDS remains the rhesus macaque infected with simian immunodeficiency virus (SIV) (117, 118). These primates are not widely available to researchers, the model requires the use of a virus different from HIV-1, and the tools to probe the macaque immune system, especially at the genetic level, are very limited. For studies of the immune system, the mouse has been the species of choice. Decades of research have provided a panoply of biological and molecular reagents to study virtually any cell population of the immune system. More recent advances in transgenesis and in embryonic stem cell technology, coupled with the development of efficient homologous recombination, have allowed the generation of Tg and gene-deficient mice. These technologies have been used largely for the investigation of the immune system.
Early attempts to express HIV-1 gene products in Tg mice were not totally successful in initiating an AIDS-like disease (52, 122-124, 254, 259, 381, 401, 434; for reviews, see references 51 and 232). Novel phenotypes not usually seen in HIV-1-infected individuals were observed in some of these Tg mice, while others showed either minimal or no permanent perturbation of immune cell populations, or severe immune defects, distinct from those usually associated with HIV-1 infection in human individuals. However, more recent attempts to generate a mouse model of AIDS were more successful, and the CD4C/HIV Tg mice were found to develop an AIDS-like disease very similar in its manifestations to human AIDS (186, 187).
Structure and expression of HIV-1 in CD4C/HIV Tg mice.
A key feature of the CD4C/HIV transgene is the nature of its regulatory elements (CD4C) allowing the expression of HIV-1 in a selected subset of immune cells: thymic immature CD4+ CD8+ and mature CD4+ CD8− T cells, peripheral mature CD4+ T cells, and cells of the myeloid lineage such as macrophages, DCs, and Kupffer cells. These cells represent the majority of the natural cell populations found to be infected with HIV-1 in humans (325). The CD4C regulatory elements were indeed chosen to target as faithfully as possible the expression of HIV-1 in the same cell populations as those infected in humans.
It was initially thought that the best way to achieve this selected cell tropism was to use the regulatory elements of the CD4 gene itself, which codes for the receptor of HIV-1. The human CD4 (hCD4) gene was chosen, since expression of the mouse CD4 gene is absent in most myeloid cell populations, including macrophages, while several subsets of human myeloid cells, including macrophages and DCs, express CD4 at their surface (228, 460). Using a reporter gene, the cell surface hCD4 itself and the hCD4 regulatory elements were dissected (first by generating the CD4A, CD4B, and CD4C constructs) in order to identify which sequences were required to drive expression in CD4+ T cells and macrophages and at the same time to silence the expression in CD8+ T cells, B cells, and other nonhematopoietic cells (189). An in vivo (Tg) approach was used, since initial experiments with established human cell lines in vitro appeared unreliable. Among the DNA constructs tested, the CD4C regulatory elements were found to drive the expression of the reporter gene most faithfully (Fig. 2A). These CD4C elements represent a human/mouse chimeric construct (14.4 kbp) containing the murine T-cell-specific enhancer (1.9 kbp) (382) fused to human genomic elements (12.5 kbp) representing 4.5 kbp of sequences upstream of the first noncoding exon (exon 1), intron 1 (9.9 kbp), exon 2, and part of exon 3 (189). Further work has now confirmed that intron 1 contains a silencer (repressing expression in CD8+ T cells, B cells, and nonlymphoid cells [426]) and DNA elements necessary for macrophage expression (188).
FIG. 2.
Incidence of death in CD4C/HIVMut Tg mice. (A) Structure of the CD4C/HIVMut transgenes. The mouse CD4 enhancer (mCD4enh.), the human CD4 promoter (hCD4C prom.), each of the HIV-1NL4-3 mutant genomes, and the polyadenylation sequences from simian virus 40 (SV40) were ligated. Ex1 and Ex2 are the first two untranslated exons of the hCD4 gene; 3′ LTR is part of the 3′ long terminal repeat of the HIV-1 genome. The symbol × means that the open reading frame of the indicated HIV gene was interrupted. Restriction sites: A, Aatll; Bs, BssHII; S, Sstl. (B) Cumulative incidence of death in non-Tg and CD4C/HIVMut Tg mice. The arrows show the time of death of 50% (TD50) of the Tg mice from different founders (F) for each mutant. Each point represents the death of a mouse. Symbols: n, number of animals observed. Reprinted from reference 187 with permission of the publisher.
The CD4C regulatory elements have been used in Tg mice to express the genome of wild-type HIV-1 (186), of point and deletion mutants of HIV-1 (187, 190) (Fig. 2A), of natural HIV-1 variants, of an experimental variant of HIV-1 encoding green fluorescent protein (Z. Hanna, C. Simard, and P. Jolicoeur, unpublished data), and of the wild-type SIV genome (400). They have also been used to express other nonviral genes, such as Notch1 (IC) (X. Zang, Z. Hanna, J. Poudrier, D. G. Kay, and P. Jolicoeur, unpublished data). In each case, the expression of the transgene, assessed with a very large number of Tg founder lines, has been remarkably reproducible and faithful, the major differences between lines being the levels of expression, most probably reflecting the distinct sites of transgene integration within the host genome. A variety of techniques were used to identify the cells expressing the transgene: immunohistochemistry with cell-specific markers coupled with in situ hybridization (ISH) with transgene-specific probes, cell sorting of specific populations followed by ISH or Western blot analysis, and fluorescence-activated cell sorter (FACS) analysis on cells expressing a cell surface reporter (CD4C/hCD4 Tg mice) or expressing a fluorescent reporter (CD4C/HIVGFP Tg mice). The consensus emerging from these studies is that the transgene is expressed in the same murine cell populations which have been found to express the cell surface CD4 molecules in human cells, i.e., thymic immature CD4+ CD8+ T cells and mature CD4+ CD8− T cells, peripheral CD4+ T cells, and cells of the myeloid lineage (peripheral macrophages, Kupffer cells, DCs, and microglial cells). Expression was not detectable in many cell populations which are not thought to express hCD4, notably hepatocytes, kidney epithelial cells, lung epithelial cells, cardiomyocytes, endothelial cells, intestinal epithelial cells, muscle cells, neurons, oligodendrocytes, and astrocytes.
It therefore seems that HIV-1 gene products are expressed in CD4C/HIV Tg mice in the same cell populations which are thought to be infected with HIV-1 in human individuals. This specific targeted expression of HIV-1 genes is thought to be critical for the development of the AIDS-like disease observed in these Tg mice (186, 187). However, the latency of disease was found to correlate very closely with the levels of transgene expression (187). Indeed, Tg mice from very-high-expressor lines died within weeks after birth, and these lines could not be maintained. Tg mice from medium-expressor lines survived 4 to 6 months, while Tg mice expressing low levels of HIV-1 Nef survived as long as 1 year but still developed essentially the same multiorgan phenotypes as Tg mice dying early (Fig. 2B). This feature of fast and slow disease progression in Tg mice is reminiscent of the human clinical situation.
To determine whether all or only a subset of the HIV-1 gene products were required to induce this AIDS-like disease in mice, various mutated forms of the HIV-1 genome were constructed and assessed in Tg mice (Fig. 2). It was found that only Tg mice expressing Nef developed disease, while Tg mice expressing all other HIV-1 genes or a subset of them did not develop apparent phenotypes and apparently led a disease-free life (187). This mutational analysis established that Nef was the major determinant of this AIDS-like disease in Tg mice.
Clinical and pathological features of AIDS-like disease in CD4C/HIV Tg mice.
The CD4C/HIV Tg mice, even those expressing only Nef, develop a severe AIDS-like disease whose latency correlated with the levels of Tg expression (186, 187). Clinically, these Tg mice show wasting, failure to thrive and/or weight loss, premature and sudden death, and sometimes edema and diarrhea. Wasting is a known consequence of human AIDS (90, 181, 270). The early death and edema are most probably caused by a severe renal disease (see below). The sudden deaths are probably due to a cardiac disease (see below). The Tg mice are fragile: often minor manipulations such as preparation for echocardiography will precipitate an early death. They also appear to survive better in a specific-pathogen-free environment than in non-specific-pathogen-free animal rooms. Tg females have lower fertility than non-Tg female littermates and typically give birth to fewer pups per litter. Tg males also show lower fertility, although this is not as apparent as with females. This lower fertility may reflect a general disease state or more specific problems of the autonomic nervous system.
A more detailed macroscopic and histological examination of these CD4C/HIV Tg mice showed multiorgan AIDS-like disease.
(i) Kidneys.
Smaller, atrophic, and pale kidneys with an irregular surface are the most macroscopically visible manifestation of the disease. This phenotype also has the highest penetrance (in virtually 100% of Tg mice), at least for Tg mice bred on the C3H/HeN background. This kidney disease represents a tubulointerstitial nephritis associated with tubular atrophy, interstitial mononuclear cell infiltration, and fibrosis, as well as with lumen dilatation forming cysts. In addition, glomerular changes are observed and often represent segmental glomerulosclerosis. Kidney disease such as tubulointerstitial nephritis and focal and segmental glomerulosclerosis are relatively frequent in SIV-infected macaques (417) and in AIDS patients, especially in children (352, 394, 418). The early expression of the Tg along with the specific C3H/HeN background may explain the high penetrance of this phenotype in the CD4C/HIV Tg mice.
(ii) Lungs.
A lymphocytic interstitial pneumonitis (LIP) (thickening of alveolar walls caused by infiltrating mononuclear cells) was observed in a high proportion of Tg mice bred on a mixed C3H-C57BL/6 background. The incidence of LIP decreased somewhat after inbreeding within the C3H background. LIP also develops in SIV-infected macaques (23) and is most often observed in human pediatric AIDS and constitutes an AIDS-defining condition (4, 5, 60, 215, 288). Since the CD4C/HIV transgene is expressed early in life, it is therefore not surprising to observe this phenotype in these Tg mice.
(iii) Heart.
The sudden deaths observed in these Tg mice prompted a detailed analysis of the heart. Noninvasive echocardiography revealed signs of depressed cardiac functions (increased systolic left ventricular internal dimension and decreased fractional shortening, ejection fraction, stroke volume, and cardiac output) compared to those of their non-Tg littermates (227). Cardiac disease was also observed very frequently at autopsy, especially when the animals were bred on a C3H-C57BL/6 mixed background. The hearts often appeared enlarged and dilated. After exsanguination, they become smaller, suggesting dilated cardiomyopathy. Histologically, multifocal lesions representing focal areas of myocytolysis, sometimes associated with infiltrating mononuclear cells and fibrosis, were observed. In addition, a more diffuse interstitial fibrosis compared to that in non-Tg mouse hearts was revealed by Sirius red staining. This was not always associated with focal lesions. More recently, evidence of disturbances of the cardiac rhythm was found (D. G. Kay and P. Jolicoeur, unpublished data). Analysis by ISH with HIV-1-specific probes revealed no detectable expression in cardiomyocytes of Tg mice (227), suggesting that the pathogenesis of this cardiomyopathy is indirect and reflects abnormal functions of immune cells, some of them most probably expressing the transgene. Interestingly, cardiac disease is a relatively frequent manifestation of simian (396, 397) and human (3, 9, 84, 154, 196, 225, 260, 293) AIDS, and the cardiac lesions of the CD4C/HIV Tg mice are similar to those found in individuals with AIDS.
(iv) Bones.
Often, the bones of CD4C/HIV Tg mice have a white appearance and are more fragile than those of non-Tg mice. Again the severity and penetrance of this phenotype was more apparent when these Tg mice were bred on a C3H-C57BL/6 background. These two phenotypes suggest the presence of a myelodysplasia and of osteoporosis. These phenotypes have not been extensively investigated, but preliminary FACS and X-ray analyses conducted on bone marrow cells and bones, respectively, are consistent with such anomalies (J. Caceres-Cortes, C. Simard, and P. Jolicoeur, unpublished data). Hematological abnormalities have been described in AIDS (93, 169, 297, 353).
Immune defects in CD4C/HIV Tg mice.
In addition to the various organ diseases described above, the CD4C/HIV Tg mice developed several phenotypes of the immune system involving many cell populations and structures, which are very similar to those found in human AIDS.
(i) Thymus.
The most striking macroscopic feature of the immune system is a severe thymic atrophy (186, 187). Histologically, loss of the normal thymus architecture is noted, with the cortical and medullary regions being poorly defined in contrast to the well-defined structures observed in non-Tg mice. In addition, the thymuses of the Tg mice are hypocellular. Thymocyte cell counts are close to normal at birth and during the first few weeks of life, but thereafter they progressively decrease to reach very small numbers, with loss of more than 90% of thymocytes. FACS analysis data show that the relative proportion of thymocytes is often almost normal, except for a lower proportion of mature CD4+ CD8− cells (P. Chrobak, M. C. Simard, T. Ndolo, Z. Hanna, and P. Jolicoeur, Abstr. 10th Conf. Retroviruses Opportunistic Infect., 2003). This appears to reflect a block in differentiation at the transition stage of double-positive (DP) CD4+ CD8+ to single-positive CD4+ CD8− T cells (Chrobak et al., Abstr. 10th Conf. Retroviruses Opportunistic Infect, abstr. 210, 2003). This thymic depletion appears to be cell autonomous and independent of stromal epithelial cells. It can indeed be reproduced in lethally irradiated normal non-Tg mice transplanted with bone marrow or fetal liver cells from Tg mice. Depletion of thymic cell populations is a feature of human AIDS, in both children and adults (171, 215, 229).
Phenotypically, these Tg DP CD4+ CD8+ T cells are abnormal and show a significant downregulation of the cell surface CD4 molecule (186, 187), also a characteristic of Nef-expressing human cells. In addition, DP cells from Tg mice show dysregulation of development marker expression (Chrobak et al., Abstr. 10th Conf. Retroviruses Opportunistic Infect., 2003), suggesting an impaired differentiation. Moreover, biochemical studies revealed constitutively enhanced levels of phosphotyrosine-containing proteins and further enhancement of tyrosine phosphorylation of several protein species, notably lysophospholipid:acyl-CoA acyltransferase and mitogen-activated protein kinases (ERK 1/2), on in vitro stimulation with anti-CD3 (187) compared to the situation for DP cells from non-Tg mice.
(ii) Peripheral lymphoid organs.
Macroscopic and microscopic examination of peripheral lymphoid organs (lymph nodes [LN] and spleen) from CD4C/HIV Tg mice showed that they were atrophic, in contrast to organs from control non-Tg mice (186, 187). They had lost their normal architecture and were hypocellular and often fibrotic. On stimulation with an antigen (ovalbumin), the CD4C/HIV Tg mice produced a significantly smaller number of germinal centers (GC) in their LN (342). In spleens of Tg mice, the T-cell zone was markedly decreased and the marginal zone (MZ) appeared larger and contained numerous Mac-1+ and CD11c+ cells, likely to represent macrophages and DCs (342). In addition, the follicular DC network was found to be markedly reduced in Tg mice compared to non-Tg mice (342). An atrophic follicular DC network and smaller numbers of GC were observed early during the course of the AIDS pandemic and were considered one of the pathological hallmarks of the disease (326, 336, 430, 431). The CD4C/HIV Tg mice show this phenotype. Such a phenotype, reminiscent of that found in CD40- or CD40L-deficient mice (226, 463), is likely to reflect a lack of CD4+ T-cell help (342).
(iii) CD4+ T cells.
Peripheral CD4+ T cells are present in smaller numbers in Tg mice than in non-Tg mice (186, 187, 342). At later stages of the disease, they often almost totally disappear from peripheral organs. They also show a down-regulation of the cell surface CD4 molecule. Therefore, the loss of this population is best assessed by quantitating the TcRαβ+ CD8− T-cell population, which essentially represents the entire CD4+ T-cell population, including the subpopulation which expresses no or very low levels of CD4. FACS analysis of CD4+ T cells from Tg mice revealed a lower expression of CD40L than that in cells from non-Tg mice (342). Also, an increased population of CD4+ T cells in Tg mice, compared to that in non-Tg mice, exhibit an activated/memory phenotype (CD69Hi, CD44Hi, CD25Hi, CD45RBLow, CD62LLow) (342; X. Weng, E. Priceputu, J. Poudrier, D. G. Kay, Z. Hanna, T. W. Mak, and P. Jolicoeur, unpublished data). Assessment of the division capacity of these cells carried out by in vivo bromodeoxyuridine labeling showed that a higher proportion of these CD4+ T cells from Tg mice than from non-Tg mice divided in vivo. However, in vitro, the purified CD4+ T cells appear to be restricted in their ability to divide. They also appear to die by apoptosis at a higher rate. Finally, in a mixed leukocyte reaction, they performed poorly compared to cells from non-Tg mice (Weng et al., unpublished). It therefore appears that the peripheral CD4+ T cells are functionally impaired, especially in their helper function, despite being in a state of activation.
(iv) CD8+ T cells.
The numbers of peripheral CD8+ T cells of CD4C/HIV Tg mice are proportionally increased, as in human AIDS (186, 187). At later stages of the disease, these cells are lost, along with the CD4+ T cells, as occurs in human AIDS (151, 327). Coupled with the smaller CD4+ T-cell numbers, this leads to a lower CD4/CD8 ratio, also a characteristic of human AIDS.
(v) B cells.
The proportion of B cells in lymphoid organs of CD4C/HIV Tg mice is increased compared to that in non-Tg mice (186, 187, 342). The presence of hyperglobulinemia is associated with this peripheral B-cell expansion in Tg mice. Most of the immunoglobulins are of the IgM isotype because of a failure to class switch (342). After ovalbumin immunization, most of the ova-specific antibodies (Ab) were of the IgM isotype (342). Interestingly, these Tg mice also appear to exhibit signs of autoimmunity, producing autoantibodies, notably anti-DNA Ab (342) and anti-heart Ab (227).
(vi) Macrophages.
The macrophages from the Tg mice seem to have a constitutively activated phenotype. Preliminary experiments also indicate that they can produce higher levels of NO and TNF-α on stimulation than those from non-Tg control littermates (D. Jovanovic, P. Vincent, and P. Jolicoeur, unpublished data). In addition, they were found to be more numerous in the spleen MZ (342).
(vii) Dendritic cells.
DCs express the transgene and are abnormal in CD4C/HIV Tg mice (342a). In LN, the total number of DC were found to progressively decrease and to express lower levels of MHC class II, CD40, and CD86 cell surface markers, suggesting an immature phenotype. Interestingly, a subpopulation of CD11bHi DC was found to accumulate in these lymphoid organs. LN DC also show a reduced capacity to deliver costimulatory signals to syngeneic CD4+ T cells in the presence of anti-CD3 and to stimulate a mixed leukocyte reaction in coculture with allogeneic CD4+ T cells from non-Tg mice. In addition, LN DC exhibit an impaired capacity to present antigen, both as proteins (pigeon cytochrome c [Pcc]) and as Pcc peptides. In contrast, in the spleen, DC were present in large numbers, especially in the MZ. In the thymus of Tg mice, recovery of CD8α+ DCs tended to be low compared to that in non-Tg control mice. Consistent with these findings, maturation of bone marrow-derived DCs from Tg mice was impaired and expression of MHC class II, CD86, and MHC class I cell surface proteins was lower than on DCs from non-Tg mice. Therefore, it appears that DCs from Tg mice fail to undergo full maturation. This may well affect their capacity to fully activate T cells. Also, the abnormal DC phenotypes and functions may contribute to the expanded B-cell compartment described above and the Ab production found in these Tg mice.
The number of DCs in HIV-infected individuals has been reported by some investigators to be small in the blood (130, 148, 175, 271, 322, 328), skin (302), lymphoid tissues (264), and oral mucosa (407). Also, DCs with an immature phenotype have been observed in some HIV-infected patients (137, 286, 338). In addition, reduced DC function has been detected in AIDS patients (reviewed in references 233 and 234). Although the benefit for the virus to elicit such a phenotype is unclear, it may favor viral replication. Indeed, it has been reported that HIV-1 replicates preferentially in immature DCs (25, 62, 163, 174).
This brief summary highlights the main features of the AIDS-like disease which develops in this CD4C/HIV Tg mouse model. All of the immune and organ disease phenotypes studied to date appear to be similar to human AIDS, not only pathologically but also at the cellular and molecular levels. In addition, no major phenotypes which are absent in human AIDS arise in the Tg mice. Conversely, almost all of the phenotypes found in human AIDS develop in these Tg mice. This strong similarity suggests that this murine AIDS model is relevant to the human disease and may be instrumental in understanding several manifestations of AIDS, in particular, opportunistic infections with pathogens such as C. albicans.
Oroesophageal Candidiasis in CD4C/HIV Transgenic Mice: a New Tool To Study Pathogenesis
Controlled studies of the pathogenesis of mucosal candidiasis in HIV infection have been hampered by the lack of a relevant animal model. The availability of CD4C/HIV Tg mice expressing HIV-1 in immune cells and developing an AIDS-like disease has recently provided a unique opportunity to devise a novel model of mucosal candidiasis that closely mimics the clinical and pathological features of candidal infection in human HIV infection (116). The following features of mucosal candidiasis in the Tg mice were found to be identical to those in patients with HIV infection: a sustained enhancement of oral burdens of C. albicans, becoming more manifest in the later stage of HIV disease (161, 439, 467) (Fig. 3); penetration by Candida hyphae of the stratified squamous epithelium of the oral cavity and esophagus, limited to the superficial epithelial layer (147, 357, 367) (Fig. 4); a low incidence of systemic dissemination of C. albicans (219, 296, 438); and a mononuclear inflammatory cell infiltrate of the mucosa (147, 367). In addition to closely mimicking the features of mucosal candidiasis in patients infected with HIV, the model obviates the problematic procurement of tissue samples from human patients; avoids the potentially confounding effects of antiretroviral therapy and of mixed infection by different strains of C. albicans or different Candida species, often found in HIV-infected patients (344); and allows for longitudinal observations at fixed times during the progression of HIV infection by direct comparison with non-Tg littermates. The Tg mice thus provide a novel opportunity to study the pathogenesis of mucosal candidiasis in HIV infection under controlled conditions in a small laboratory animal.
FIG. 3.
Oral burdens of C. albicans in CD4C/HIVMutA Tg mice and non-Tg controls. Mice were inoculated intraorally with 108 CFU of C. albicans LAM-1, and burdens were assessed longitudinally by sampling the oral cavity. Oral burdens were strikingly elevated in Tg mice compared to control non-Tg mice during primary infection, the 6- to 10-week carrier state, and marked terminal outgrowth preceding death. In contrast, C. albicans was rapidly cleared from oral cavities of non-Tg mice immediately after primary infection. Oral burdens during primary infection in control non-Tg (A) and intact C3H mice (B; mean and standard deviation [SD]) were not significantly different (P > 0.05). There were six Tg and six non-Tg mice in the experiment in panel A and 42 C3H mice in the experiment in panel B. Adapted from reference 116 with permission of the publisher.
FIG. 4.
Histopathology of oral candidiasis in CD4C/HIVMutA Tg mice. Candida hyphae penetrate the superficial keratin layer of the stratified squamous epithelium of the tongue (To), palate (P), and gingiva (G) surrounding the tooth (T). Stain, Gomori-Grocott methenamine silver. Magnifications: A, ×100; B, ×250; C, ×500. Adapted from reference 116 with permission of the publisher.
In accordance with the findings in humans with advanced HIV infection, the frequencies of cells expressing MHC class II antigen and CD4+ cells were markedly reduced in the oral mucosa of the Tg compared to the non-Tg mice at the time of marked terminal outgrowth of C. albicans preceding death (116). However, in the Tg mice, infection with C. albicans also resulted in a substantial increase in the frequencies of mucosal cells expressing MHC class II and a more modest enhancement in the frequencies of CD4+ cells, demonstrating the ability of the Tg mice to partially respond to mucosal infection despite the reduction in these cell populations (116).
Continuing investigation using this novel model in Tg mice is under way and is allowing, for the first time, a precise cause-and-effect analysis of the immunopathogenesis of mucosal candidiasis in HIV infection.
FUTURE DIRECTIONS AND CONCLUSION
The accumulated evidence presented in this review suggests a number of hypothetical defects which may underlie the susceptibility to mucosal candidiasis in HIV-infection (Fig. 5). Depletion of Langerhans' cells and their reduced expression of MHC class II molecules and IL-12 probably perturb the development of Candida-specific CD4+ Th1 cells which are instrumental in orchestrating a protective adaptive cell-mediated immune response to C. albicans in the oral and esophageal mucosa. The depletion of CD4+ cells and a shift in expression from Th1 to Th2 cytokines may reduce the anticandidal activity of macrophages and PMNs and thus trigger the onset of OPC. Partly preserved expression of MHC class I antigens on Langerhans' cells may allow the recruitment of a compensatory protective CD8+ T-cell response to C. albicans in the mucosa despite HIV infection; this, combined with the anticandidal activity of preserved innate defense mechanisms (calprotectin and keratinocytes), may limit the proliferation of C. albicans to the mucosa and prevent systemic dissemination to deep organs.
FIG. 5.
Hypothetical defects in host defenses against oroesophageal candidiasis in HIV infection. Progressive depletion and functional dysregulation of mucosal Langerhans' cells alters normal processing and presentation of C. albicans antigens to CD4+ cells, which are themselves depleted in HIV infection, resulting in diminished numbers of CD4+ Th1 cells and perturbed adaptive immunity to C. albicans. However, substantially preserved innate defense mechanisms (calprotectin, PMNs, and γδ T cells) and cytotoxic T lymphocytes prevent systemic dissemination.
Oral biopsy material from HIV-infected patients will continue to provide clinically relevant, descriptive information about critical alterations in mucosal host defense mechanisms which may predispose to mucosal candidiasis in HIV-infection and may also suggest a protective role for cell populations which appear in the mucosa in response to candidiasis. The specificity of these identified alterations will be strengthened by examining tissue samples from normal and infected areas of the oral cavity in HIV-infected patients with OPC in comparison to HIV- and non-HIV-infected patients without OPC. Complementary to these investigations, the novel model of mucosal candidiasis in CD4C/HIV Tg mice will for the first time allow a longitudinal assessment of the alterations in oral mucosal and cervical lymph node cell populations and their production of cytokines at the single-cell level under controlled conditions. New Tg mouse constructs and replenishment with specific cell populations and cytokines should provide the opportunity to achieve a precise cause-and-effect analysis of the immunopathogenesis of mucosal candidiasis in HIV infection. The new knowledge gained is a prerequisite to designing novel approaches to immune reconstitution.
Acknowledgments
The work on the transgenic mice was supported by the Canadian Institutes of Health Research HIV/AIDS Research Program (HOP-41544).
We thank Claire St-Onge and Sylvie Julien for expert manuscript preparation.
REFERENCES
- 1.Abgrall, S., I. Charreau, V. Joly, J. Bloch, and J. Reynes. 2001. Risk factors for esophageal candidiasis in a large cohort of HIV-infected patients treated with nucleoside analogues. Eur. J. Clin. Microbiol. Infect. Dis. 20:346-349. [DOI] [PubMed] [Google Scholar]
- 2.Abi-Said, D., E. Anaissie, O. Uzun, I. Raad, H. Pinzcowski, and S. Vartivarian. 1997. The epidemiology of hematogenous candidiasis caused by different Candida species. Clin. Infect. Dis. 24:1122-1128. [DOI] [PubMed] [Google Scholar]
- 3.Acierno, L. J. 1989. Cardiac complications in acquired immunodeficiency syndrome (AIDS): a review. J. Am. Coll. Cardiol. 13:1144-1154. [DOI] [PubMed] [Google Scholar]
- 4.Agostini, C., and G. Semenzato. 1996. Immunologic effects of HIV in the lung. Clin. Chest Med. 17:633-645. [DOI] [PubMed] [Google Scholar]
- 5.Agostini, C., R. Zambello, L. Trentin, and G. Semenzato. 1996. HIV and pulmonary immune responses. Immunol. Today 17:359-364. [DOI] [PubMed] [Google Scholar]
- 6.Ahlfors, E. E., P. A. Larsson, and P. R. Bergstresser. 1985. Langerhans cell surface densities in rat oral mucosa and human buccal mucosa. J. Oral Pathol. 14:390-397. [DOI] [PubMed] [Google Scholar]
- 7.Almstahl, A., U. Kroneld, A. Tarkowski, and M. Wikstrom. 1999. Oral microbial flora in Sjogren's syndrome. J. Rheumatol. 26:110-114. [PubMed] [Google Scholar]
- 8.Ammann, A. J., and R. Hong. 1971. Selective IgA deficiency: presentation of 30 cases and a review of the literature. Medicine (Baltimore) 50:223-236. [PubMed] [Google Scholar]
- 9.Anderson, D. W., and R. Virmani. 1990. Emerging patterns of heart disease in human immunodeficiency virus infection. Hum. Pathol. 21:253-259. [DOI] [PubMed] [Google Scholar]
- 10.Angel, J. B., A. Kumar, K. Parato, L. G. Filion, F. Diaz-Mitoma, P. Daftarian, B. Pham, E. Sun, J. M. Leonard, and D. W. Cameron. 1998. Improvement in cell-mediated immune function during potent anti-humanimmunodeficiency virus therapy with ritonavir plus saquinavir. J. Infect. Dis. 177:898-904. [DOI] [PubMed] [Google Scholar]
- 11.Anjuere, F., P. Martin, I. Ferrero, M. L. Fraga, G. M. del Hoyo, N. Wright, and C. Ardavin. 1999. Definition of dendritic cell subpopulations present in the spleen, Peyer's patches, lymph nodes, and skin of the mouse. Blood 93:590-598. [PubMed] [Google Scholar]
- 12.Anonymous. 1993. Classification and diagnostic criteria for oral lesions in HIV infection. EC-Clearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Immunodeficiency Virus. J. Oral Pathol. Med. 22:289-291. [PubMed] [Google Scholar]
- 13.Reference deleted.
- 14.Ansel, J., P. Perry, J. Brown, D. Damm, T. Phan, C. Hart, T. Luger, and S. Hefeneider. 1990. Cytokine modulation of keratinocyte cytokines. J. Investig. Dermatol. 94:101S-107S. [DOI] [PubMed] [Google Scholar]
- 15.Antinori, A., A. Antinori, A. Ammassari, R. Masetti, A. De Luca, R. Murri, E. Tamburrini, and P. Magistrelli. 1995. Presumptive clinical criteria versus endoscopy in the diagnosis of Candida esophagitis at various HIV-1 disease stages. Endoscopy 27:371-376. [DOI] [PubMed] [Google Scholar]
- 16.Arendorf, T. M., and D. M. Walker. 1980. The prevalence and intra-oral distribution of Candida albicans in man. Arch. Oral Biol. 25:1-10. [DOI] [PubMed] [Google Scholar]
- 17.Arribas, J. R., S. Hernandez-Albujar, J. J. Gonzalez-Garcia, J. M. Pena, A. Gonzalez, T. Canedo, R. Madero, J. J. Vazquez, and W. G. Powderly. 2000. Impact of protease inhibitor therapy on HIV-related oropharyngeal candidiasis. AIDS 14:979-985. [DOI] [PubMed] [Google Scholar]
- 18.Ashman, R. B. 1991. Enhancement of MHC class II antigen expression by exposure to Candida albicans. Immunol. Lett. 30:255-260. [DOI] [PubMed] [Google Scholar]
- 19.Ashman, R. B., and J. M. Papadimitriou. 1995. Production and function of cytokines in natural and acquired immunity to Candida albicans infection. Microbiol. Rev. 59:646-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atkinson, J. C., C. Yeh, F. G. Oppenheim, D. Bermudez, B. J. Baum, and P. C. Fox. 1990. Elevation of salivary antimicrobial proteins following HIV-1 infection. J. Acquir. Immune. Defic. Syndr. 3:41-48. [PubMed] [Google Scholar]
- 21.Autran, B., G. Carcelain, T. S. Li, C. Blanc, D. Mathez, R. Tubiana, C. Katlama, P. Debre, and J. Leibowitch. 1997. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science 277:112-116. [DOI] [PubMed] [Google Scholar]
- 22.Autran, B., G. Carcelaint, T. S. Li, G. Gorochov, C. Blanc, M. Renaud, M. Durali, D. Mathez, V. Calvez, J. Leibowitch, C. Katlama, and P. Debre. 1999. Restoration of the immune system with anti-retroviral therapy. Immunol. Lett. 66:207-211. [DOI] [PubMed] [Google Scholar]
- 23.Babas, T., E. Vieler, D. A. Hauer, R. J. Adams, P. M. Tarwater, K. Fox, J. E. Clements, and M. C. Zink. 2001. Pathogenesis of SIV pneumonia: selective replication of viral genotypes in the lung. Virology 287:371-381. [DOI] [PubMed] [Google Scholar]
- 24.Bacci, A., C. Montagnoli, K. Perruccio, S. Bozza, R. Gaziano, L. Pitzurra, A. Velardi, C. F. d'Ostiani, J. E. Cutler, and L. Romani. 2002. Dendritic cells pulsed with fungal RNA induce protective immunity to Candida albicans in hematopoietic transplantation. J. Immunol. 168:2904-2913. [DOI] [PubMed] [Google Scholar]
- 25.Bakri, Y., C. Schiffer, V. Zennou, P. Charneau, E. Kahn, A. Benjouad, J. C. Gluckman, and B. Canque. 1920. The maturation of dendritic cells results in postintegration inhibition of HIV-1 replication. J. Immunol. 166:3780-3788. [DOI] [PubMed] [Google Scholar]
- 26.Balish, E., H. Filutowicz, and T. D. Oberley. 1990. Correlates of cell- mediated immunity in Candida albicans-colonized gnotobiotic mice. Infect. Immun. 58:107-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Balish, E., J. Jensen, T. Warner, J. Brekke, and B. Leonard. 1993. Mucosal and disseminated candidiasis in gnotobiotic SCID mice. J. Med. Vet. Mycol. 31:143-154. [DOI] [PubMed] [Google Scholar]
- 28.Balish, E., R. D. Wagner, A. Vazquez-Torres, C. Pierson, and T. Warner. 1998. Candidiasis in interferon-gamma knockout (IFN-gamma−/−) mice. J. Infect. Dis. 178:478-487. [DOI] [PubMed] [Google Scholar]
- 29.Balish, E., T. Warner, C. J. Pierson, D. M. Bock, and R. D. Wagner. 2001. Oroesophageal candidiasis is lethal for transgenic mice with combined natural killer and T-cell defects. Med. Mycol. 39:261-268. [DOI] [PubMed] [Google Scholar]
- 30.Banchereau, J., and R. M. Steinman. 1998. Dendritic cells and the control of immunity. Nature 392:245-252. [DOI] [PubMed] [Google Scholar]
- 31.Barbeau, J., and N. Deslauriers. 1989. Phenotypic and functional analysis of oral mucosal macrophages. Reg. Immunol. 2:285-293. [PubMed] [Google Scholar]
- 32.Barchiesi, F., D. Arzeni, M. S. Del Prete, A. Sinicco, D. F. Falconi, M. B. Pasticci, L. Lamura, M. M. Nuzzo, F. Burzacchini, S. Coppola, F. Chiodo, and G. Scalise. 1998. Fluconazole susceptibility and strain variation of Candida albicans isolates from HIV-infected patients with oropharyngeal candidosis. J. Antimicrob. Chemother. 41:541-548. [DOI] [PubMed] [Google Scholar]
- 33.Barchiesi, F., R. J. Hollis, M. Del Poeta, D. A. McGough, G. Scalise, M. G. Rinaldi, and M. A. Pfaller. 1995. Transmission of fluconazole-resistant Candida albicans between patients with AIDS and oropharyngeal candidiasis documented by pulsed-field gel electrophoresis. Clin. Infect. Dis. 21:561-564. [DOI] [PubMed] [Google Scholar]
- 34.Barrett, A. W., A. T. Cruchley, and D. M. Williams. 1996. Oral mucosal Langerhans' cells. Crit. Rev. Oral. Biol. Med. 7:36-58. [DOI] [PubMed] [Google Scholar]
- 35.Barrett, A. W., D. A. Ross, and J. A. Goodacre. 1993. Purified human oral mucosal Langerhans cells function as accessory cells in vitro. Clin. Exp. Immunol. 92:158-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barron, M. A., N. Blyveis, B. E. Palmer, S. MaWhinney, and C. C. Wilson. 2003. Influence of plasma viremia on defects in number and immunophenotype of blood dendritic cell subsets in human immunodeficiency virus 1-infected individuals. J. Infect. Dis. 187:26-37. [DOI] [PubMed] [Google Scholar]
- 37.Basson, N. J. and C. W. van Wyk. 1996. The establishment of a community of oral bacteria that controls the growth of Candida albicans in a chemostat. Oral Microbiol. Immunol. 11:199-202. [DOI] [PubMed] [Google Scholar]
- 38.Beausejour, A., D. Grenier, J. P. Goulet, and N. Deslauriers. 1998. Proteolytic activation of the interleukin-1beta precursor by Candida albicans. Infect. Immun. 66:676-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bektic, J., C. P. Lell, A. Fuchs, H. Stoiber, C. Speth, C. Lass-Florl, M. Borg-von Zepelin, M. P. Dierich, and R. Wurzner. 2001. HIV protease inhibitors attenuate adherence of Candida albicans to epithelial cells in vitro. FEMS Immunol. Med. Microbiol. 31:65-71. [DOI] [PubMed] [Google Scholar]
- 40.Beno, D. W., A. G. Stover, and H. L. Mathews. 1995. Growth inhibition of Candida albicans hyphae by CD8+ lymphocytes. J. Immunol. 154:5273-5281. [PubMed] [Google Scholar]
- 41.Bikandi, J., M. D. Moragues, G. Quindos, L. Polonelli, and J. Ponton. 2000. Influence of environmental pH on the reactivity of Candida albicans with salivary IgA. J. Dent. Res. 79:1439-1442. [DOI] [PubMed] [Google Scholar]
- 42.Bistoni, F., E. Cenci, A. Mencacci, E. Schiaffella, P. Mosci, P. Puccetti, and L. Romani. 1993. Mucosal and systemic T helper cell function after intragastric colonization of adult mice with Candida albicans. J. Infect. Dis. 168:1449-1457. [DOI] [PubMed] [Google Scholar]
- 43.Blank, C., C. Bogdan, C. Bauer, K. Erb, and H. Moll. 1996. Murine epidermal Langerhans cells do not express inducible nitric oxide synthase. Eur. J. Immunol. 26:792-796. [DOI] [PubMed] [Google Scholar]
- 44.Blauvelt, A., M. Clerici, D. R. Lucey, S. M. Steinberg, R. Yarchoan, R. Walker, G. M. Shearer, and S. I. Katz. 1995. Functional studies of epidermal Langerhans cells and blood monocytes in HIV-infected persons. J. Immunol. 154:3506-3515. [PubMed] [Google Scholar]
- 45.Blumberg, H., D. Conklin, W. F. Xu, A. Grossmann, T. Brender, S. Carollo, M. Eagan, D. Foster, B. A. Haldeman, A. Hammond, H. Haugen, L. Jelinek, J. D. Kelly, K. Madden, M. F. Maurer, J. Parrish-Novak, D. Prunkard, S. Sexson, C. Sprecher, K. Waggie, J. West, T. E. Whitmore, L. Yao, M. K. Kuechle, B. A. Dale, and Y. A. Chandrasekher. 2001. Interleukin 20: discovery, receptor identification, and role in epidermal function. Cell 104:9-19. [DOI] [PubMed] [Google Scholar]
- 46.Bober, L. A., T. A. Waters, C. C. Pugliese-Sivo, L. M. Sullivan, S. K. Narula, and M. J. Grace. 1995. IL-4 induces neutrophilic maturation of HL-60 cells and activation of human peripheral blood neutrophils. Clin. Exp. Immunol. 99:129-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bolduc, C., J. D. Waterfield, and N. Deslaurlers. 1990. Tissue distribution and cytofluorometric analysis of oral mucosal T cells in the BALB/c mouse. Res. Immunol. 141:461-475. [DOI] [PubMed] [Google Scholar]
- 48.Borg, M., and R. Ruchel. 1988. Expression of extracellular acid proteinase by proteolytic Candida spp. during experimental infection of oral mucosa. Infect. Immun. 56:626-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bos, I. R., and A. Burkhardt. 1980. Interepithelial cells of the oral mucosa. Light and electron microscopic observations in germfree, specific pathogen- free and conventionalized mice. J. Oral Pathol. 9:65-81. [DOI] [PubMed] [Google Scholar]
- 50.Bos, J. D., I. Zonneveld, P. K. Das, S. R. Krieg, C. M. van der Loos, and M. L. Kapsenberg. 1987. The skin immune system (SIS): distribution and immunophenotype of lymphocyte subpopulations in normal human skin. J. Investig. Dermatol. 88:569-573. [DOI] [PubMed] [Google Scholar]
- 51.Brady, H. J., D. J. Pennington, and E. A. Dzierzak. 1994. Transgenic mice as models of human immunodeficiency virus expression and related cellular effects. J. Gen. Virol. 75:2549-2558. [DOI] [PubMed] [Google Scholar]
- 52.Brady, H. J., D. J. Pennington, C. G. Miles, and E. A. Dzierzak. 1993. CD4 cell surface downregulation in HIV-1 Nef transgenic mice is a consequence of intracellular sequestration. EMBO J. 12:4923-4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brambilla, A. M., A. Castagna, B. Nocita, H. Hasson, E. Boeri, F. Veglia, and A. Lazzarin. 2001. Relation between CD4 cell counts and HIV RNA levels at onset of opportunistic infections. J. Acquir. Immune Defic. Syndr. 27:44-48. [DOI] [PubMed] [Google Scholar]
- 54.Brandtzaeg, P., T. O. Gabrielsen, I. Dale, F. Muller, M. Steinbakk, and M. K. Fagerhol. 1995. The leucocyte protein L1 (calprotectin): a putative nonspecific defence factor at epithelial surfaces. Adv. Exp. Med. Biol. 371A:201-206. [DOI] [PubMed] [Google Scholar]
- 55.Brodt, H. R., B. S. Kamps, P. Gute, B. Knupp, S. Staszewski, and E. B. Helm. 1997. Changing incidence of AIDS-defining illnesses in the era of antiretroviral combination therapy. AIDS 11:1731-1738. [DOI] [PubMed] [Google Scholar]
- 56.Brown, J. A., T. K. Howcroft, and D. S. Singer. 1998. HIV Tat protein requirements for transactivation and repression of transcription are separable. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 17:9-16. [DOI] [PubMed] [Google Scholar]
- 57.Brysk, M. M., T. Bell, H. Brysk, P. Selvanayagam, and S. Rajaraman. 1994. Enzymatic activity of desquamin. Exp. Cell Res. 214:22-26. [DOI] [PubMed] [Google Scholar]
- 58.Brysk, M. M., T. Bell, C. Hoida, S. K. Tyring, and S. Rajaraman. 1991. Interferon-gamma modulates terminal differentiation and the expression of desquamin in cultured keratinocytes. Exp. Cell. Res. 197:140-147. [DOI] [PubMed] [Google Scholar]
- 59.Burkhardt, A. 1992. Intraepithelial lymphocytes and Langerhans cells in the oral mucosa—dynamic aspects. J. Dent. Assoc. S. Afr. 47:200-203. [PubMed] [Google Scholar]
- 60.Calvelli, T. A., and A. Rubinstein. 1990. Pediatric HIV infection: a review. Immunodefic. Rev 2:83-127. [PubMed] [Google Scholar]
- 61.Canny, G., O. Levy, G. T. Furuta, S. Narravula-Alipati, R. B. Sisson, C. N. Serhan, and S. P. Colgan. 2002. Lipid mediator-induced expression of bactericidal/ permeability-increasing protein (BPI) in human mucosal epithelia. Proc. Natl. Acad. Sci. USA 99:3902-3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Canque, B., Y. Bakri, S. Camus, M. Yagello, A. Benjouad, and J. C. Gluckman. 1999. The susceptibility to X4 and R5 human immunodeficiency virus-1 strains of dendritic cells derived in vitro from CD34+ hematopoietic progenitor cells is primarily determined by their maturation stage. Blood 93:3866-3875. [PubMed] [Google Scholar]
- 63.Cantorna, M. T., and E. Balish. 1990. Mucosal and systemic candidiasis in congenitally immunodeficient mice. Infect. Immun. 58:1093-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cantorna, M. T., and E. Balish. 1991. Role of CD4+ lymphocytes in resistance to mucosal candidiasis. Infect. Immun. 59:2447-2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cassone, A., F. De Bernardis, A. Torosantucci, E. Tacconelli, M. Tumbarello, and R. Cauda. 1999. In vitro and in vivo anticandidal activity of human immunodeficiency virus protease inhibitors. J. Infect. Dis. 180:448-453. [DOI] [PubMed] [Google Scholar]
- 66.Cassone, A., C. Palma, J. Y. Djeu, F. Aiuti, and I. Quinti. 1993. Anticandidal activity and interleukin-1 beta and interleukin-6 production by polymorphonuclear leukocytes are preserved in subjects with AIDS. J. Clin. Microbiol. 31:1354-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cassone, A., E. Tacconelli, F. De Bernardis, M. Tumbarello, A. Torosantucci, P. Chiani, and R. Cauda. 2002. Antiretroviral therapy with protease inhibitors has an early, immune reconstitution-independent beneficial effect on Candida virulence and oral candidiasis in human immunodeficiency virus-infected subjects. J. Infect. Dis. 185:188-195. [DOI] [PubMed] [Google Scholar]
- 68.Cauda, R., E. Tacconelli, M. Tumbarello, G. Morace, F. De Bernardis, A. Torosantucci, and A. Cassone. 1999. Role of protease inhibitors in preventing recurrent oral candidosis in patients with HIV infection: a prospective case-control study. J. Acquir. Immune Defic. Syndr. 21:20-25. [DOI] [PubMed] [Google Scholar]
- 69.Caux, C., C. Massacrier, B. Vanbervliet, B. Dubois, I. Durand, M. Cella, A. Lanzavecchia, and J. Banchereau. 1997. CD34+ hematopoietic progenitors from human cord blood differentiate along two independent dendritic cell pathways in response to granulocyte-macrophage colony- stimulating factor plus tumor necrosis factor alpha. II. Functional analysis. Blood 90:1458-1470. [PubMed] [Google Scholar]
- 70.Cenci, E., A. Mencacci, R. Spaccapelo, L. Tonnetti, P. Mosci, K. H. Enssle, P. Puccetti, L. Romani, and F. Bistoni. 1995. T helper cell type 1 (Th1)- and Th2-like responses are present in mice with gastric candidiasis but protective immunity is associated with Th1 development. J. Infect. Dis. 171:1279-1288. [DOI] [PubMed] [Google Scholar]
- 70a.Centers for Disease Control and Prevention. 1992. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. Morb. Mortal. Wkly. Rep. Recomm. Rep. 41:1-19. [PubMed] [Google Scholar]
- 71.Chakir, J., L. Cote, C. Coulombe, and N. Deslauriers. 1994. Differential pattern of infection and immune response during experimental oral candidiasis in BALB/c and DBA/2 (H-2d) mice. Oral Microbiol. Immunol. 9:88-94. [DOI] [PubMed] [Google Scholar]
- 72.Challacombe, S. J. 1994. Immunologic aspects of oral candidiasis. Oral Surg. Oral Med. Oral Pathol. 78:202-210. [DOI] [PubMed] [Google Scholar]
- 73.Challacombe, S. J., and S. P. Sweet. 1997. Salivary and mucosal immune responses to HIV and its co-pathogens. Oral Dis. 3(Suppl. 1):S79-S84. [DOI] [PubMed] [Google Scholar]
- 74.Challacombe, S. J., and S. P. Sweet. 2002. Oral mucosal immunity and HIV infection: current status. Oral Dis. 8(Suppl. 2):55-62. [DOI] [PubMed] [Google Scholar]
- 75.Chandra, J., D. M. Kuhn, P. K. Mukherjee, L. L. Hoyer, T. McCormick, and M. A. Ghannoum. 2001. Biofilm formation by the fungal pathogen Candida albicans: development, architecture, and drug resistance. J. Bacteriol. 183:5385-5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chandra, J., P. K. Mukherjee, S. D. Leidich, F. F. Faddoul, L. L. Hoyer, L. J. Douglas, and M. A. Ghannoum. 2001. Antifungal resistance of candidal biofilms formed on denture acrylic in vitro. J. Dent. Res. 80:903-908. [DOI] [PubMed] [Google Scholar]
- 77.Charbonnier, A. S., N. Kohrgruber, E. Kriehuber, G. Stingl, A. Rot, and D. Maurer. 1999. Macrophage inflammatory protein 3α is involved in the constitutive trafficking of epidermal langerhans cells. J. Exp. Med. 190:1755-1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Charton-Bain, M. C., B. Terris, M. C. Dauge, C. Marche, F. Walker, O. Bouchaud, L. Xerri, and F. Potet. 1999. Reduced number of Langerhans cells in oesophageal mucosa from AIDS patients. Histopathology 34:399-404. [DOI] [PubMed] [Google Scholar]
- 79.Chiani, P., C. Bromuro, and A. Torosantucci. 2000. Defective induction of interleukin-12 in human, monocytes by germ-tube forms of Candida albicans. Infect. Immun. 68:5628-5634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chiou, C. C., A. H. Groll, C. E. Gonzalez, D. Callender, D. Venzon, P. A. Pizzo, L. Wood, and T. J. Walsh. 2000. Esophageal candidiasis in pediatric acquired immunodeficiency syndrome: clinical manifestations and risk factors. Pediatr. Infect. Dis. J. 19:729-734. [DOI] [PubMed] [Google Scholar]
- 81.Chou, L. L., J. Epstein, S. A. Cassol, D. M. West, W. He, and J. D. Firth. 2000. Oral mucosal Langerhans' cells as target, effector and vector in HIV infection. J Oral Pathol. Med. 29:394-402. [DOI] [PubMed] [Google Scholar]
- 82.Cilla, G., T. E. Perez, J. R. Furundarena, E. Cuadrado, J. A. Iribarren, and F. Neira. 1988. Esophageal candidiasis and immunodeficiency associated with acute HIV infection. AIDS 2:399-400. [DOI] [PubMed] [Google Scholar]
- 83.Clerici, M. and G. M. Shearer. 1993. A TH1→TH2 switch is a critical step in the etiology of HIV infection. Immunol. Today 14:107-111. [DOI] [PubMed] [Google Scholar]
- 84.Cohen, I. S., D. W. Anderson, R. Virmani, B. M. Reen, A. M. Macher, J. Sennesh, P. DiLorenzo, and R. R. Redfield. 1986. Congestive cardiomyopathy in association with the acquired immunodeficiency syndrome. N. Engl. J. Med. 315:628-630. [DOI] [PubMed] [Google Scholar]
- 85.Cohen, P. J., and S. I. Katz. 1992. Cultured human Langerhans cells process and present intact protein antigens. J. Investig. Dermatol. 99:331-336. [DOI] [PubMed] [Google Scholar]
- 86.Colasante, A., S. Rosini, A. Piattelli, L. Artese, F. B. Aiello, and P. Musiani. 1992. Distribution and phenotype of immune cells in normal human gingiva: active immune response versus unresponsiveness. J. Oral Pathol. Med. 21:12-16. [DOI] [PubMed] [Google Scholar]
- 87.Cole, G. T. 1996. Biochemistry of enzymatic pathogenicity factors, p. 31-65. In D. H. Howard and J. D. Miller (ed.), Human and animal relationships. Springer-Verlag KG, Berlin, Germany.
- 88.Coleman, D., D. Sullivan, B. Harrington, K. Haynes, M. Henman, D. Shanley, D. Bennett, G. Moran, C. McCreary, and L. O'Neill. 1997. Molecular and phenotypic analysis of Candida dubliniensis: a recently identified species linked with oral candidosis in HIV-infected and AIDS patients. Oral Dis. 3 (Suppl. 1):S96-S101. [DOI] [PubMed] [Google Scholar]
- 89.Colina, A. R., F. Aumont, N. Deslauriers, P. Belhumeur, and L. de Repentigny. 1996. Evidence for degradation of gastrointestinal mucin by Candida albicans secretory aspartyl proteinase. Infect. Immun. 64:4514-4519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Coodley, G. O., M. O. Loveless, and T. M. Merrill. 1994. The HIV wasting syndrome: a review. J. Acquir. Immune Defic. Syndr. 7:681-694. [PubMed] [Google Scholar]
- 91.Coogan, M. M., and S. J. Challacombe. 2000. Serum and salivary antibodies to a mycobacterial 65-kDa stress protein are elevated in HIV-positive patients and modified by oral candidiasis. Oral Microbiol. Immunol. 15:284-289. [DOI] [PubMed] [Google Scholar]
- 92.Coogan, M. M., S. P. Sweet, and S. J. Challacombe. 1994. Immunoglobulin A (IgA), IgA1, and IgA2 antibodies to Candida albicans in whole and parotid saliva in human immunodeficiency virus infection and AIDS. Infect. Immun. 62:892-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Costello, C. 1988. Haematological abnormalities in human immunodeficiency virus (HIV) disease. J. Clin. Pathol. 41:711-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Côté, L. and N. Deslauriers. 1994. Intraepithelial recruitment and persistence of CD8+ T cells during experimental oral candidiasis in anti-CD4- treated mice. Immunol. Infect. Dis. 4:219-227. [Google Scholar]
- 95.Crowe, S. M., N. J. Vardaxis, S. J. Kent, A. L. Maerz, M. J. Hewish, M. S. McGrath, and J. Mills. 1994. HIV infection of monocyte-derived macrophages in vitro reduces phagocytosis of Candida albicans. J. Leukoc. Biol. 56:318-327. [DOI] [PubMed] [Google Scholar]
- 96.Cruchley, A. T., D. M. Williams, P. M. Farthing, C. A. Lesch, and C. A. Squier. 1989. Regional variation in Langerhans cell distribution and density in normal human oral mucosa determined using monoclonal antibodies against CD1, HLADR, HLADQ and HLADP. J. Oral Pathol. Med. 18:510-516. [DOI] [PubMed] [Google Scholar]
- 97.Cullell-Young, M., M. Barrachina, C. Lopez-Lopez, E. Gonalons, J. Lloberas, C. Soler, and A. Celada. 2001. From transcription to cell surface expression, the induction of MHC class II I-A alpha by interferon-gamma in macrophages is regulated at different levels. Immunogenetics 53:136-144. [DOI] [PubMed] [Google Scholar]
- 98.Cumberbatch, M., R. J. Dearman, C. Antonopoulos, R. W. Groves, and I. Kimber. 2001. Interleukin (IL)-18 induces Langerhans cell migration by a tumour necrosis factor-alpha- and IL-1beta-dependent mechanism. Immunology 102:323-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cutler, C. W., R. Jotwani, and B. Pulendran. 2001. Dendritic cells: immune saviors or Achilles' heel? Infect. Immun. 69:4703-4708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cutler, J. E. 1991. Putative virulence factors of Candida albicans. Annu. Rev. Microbiol. 45:187-218. [DOI] [PubMed] [Google Scholar]
- 101.Reference deleted
- 102.Dahl, K. M., E. J. Keath, V. J. Fraser, and W. G. Powderly. 1997. Molecular epidemiology of mucosal candidiasis in HIV-positive women. AIDS Res. Hum. Retroviruses 13:485-491. [DOI] [PubMed] [Google Scholar]
- 103.Daniels, T. E. 1984. Human mucosal Langerhans cells: postmortem identification of regional variations in oral mucosa. J. Investig. Dermatol. 82:21-24. [DOI] [PubMed] [Google Scholar]
- 104.Darbyshire, J. 2000. Therapeutic interventions in HIV infection—a critical view. Trop. Med. Int. Health 5:A26-A31. [DOI] [PubMed] [Google Scholar]
- 105.De Bernardis, F., S. Arancia, L. Morelli, B. Hube, D. Sanglard, W. Schafer, and A. Cassone. 1999. Evidence that members of the secretory aspartyl proteinase gene family, in particular SAP2, are virulence factors for Candida vaginitis. J. Infect. Dis. 179:201-208. [DOI] [PubMed] [Google Scholar]
- 106.De Bernardis, F., M. Boccanera, D. Adriani, E. Spreghini, G. Santoni, and A. Cassone. 1997. Protective role of antimannan and anti-aspartyl proteinase antibodies in an experimental model of Candida albicans vaginitis in rats. Infect. Immun. 65:3399-3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.De Bernardis, F., P. Chiani, M. Ciccozzi, G. Pellegrini, T. Ceddia, G. D'Offizzi, I. Quinti, P. A. Sullivan, and A. Cassone. 1996. Elevated aspartic proteinase secretion and experimental pathogenicity of Candida albicans isolates from oral cavities of subjects infected with human immunodeficiency virus. Infect. Immun. 64:466-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.De Bernardis, F., F. A. Muhlschlegel, A. Cassone, and W. A. Fonzi. 1998. The pH of the host niche controls gene expression in and virulence of Candida albicans. Infect. Immun. 66:3317-3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.De Bernardis, F., P. A. Sullivan, and A. Cassone. 2001. Aspartyl proteinases of Candida albicans and their role in pathogenicity. Med. Mycol. 39:303-313. [DOI] [PubMed] [Google Scholar]
- 110.De Creus, A., K. Van Beneden, T. Taghon, F. Stolz, V. Debacker, J. Plum, and G. Leclercq. 2000. Langerhans cells that have matured in vivo in the absence of T cells are fully capable of inducing a helper CD4 as well as a cytotoxic CD8 response. J. Immunol. 165:645-653. [DOI] [PubMed] [Google Scholar]
- 111.Deeks, S. G., M. Smith, M. Holodniy, and J. O. Kahn. 1997. HIV-1 protease inhibitors. A review for clinicians. JAMA 277:145-153. [PubMed] [Google Scholar]
- 112.Delves, P. J., and I. M. Roitt. 2000. The immune system. First of two parts. N. Engl. J. Med. 343:37-49. [DOI] [PubMed] [Google Scholar]
- 113.Delves, P. J., and I. M. Roitt. 2000. The immune system. Second of two parts. N. Engl. J. Med. 343:108-117. [DOI] [PubMed] [Google Scholar]
- 114.de Repentigny, L. 1992. Serodiagnosis of candidiasis, aspergillosis, and cryptococcosis. Clin. Infect. Dis. 14 (Suppl. 1):S11-S22. [DOI] [PubMed] [Google Scholar]
- 115.de Repentigny, L., F. Aumont, K. Bernard, and P. Belhumeur. 2000. Characterization of binding of Candida albicans to small-intestinal mucin and its role in adherence to mucosal epithelial cells. Infect. Immun. 68:3172-3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.de Repentigny, L., F. Aumont, J. S. Ripeau, M. Fiorillo, D. G. Kay, Z. Hanna, and P. Jolicoeur. 2002. Mucosal candidiasis in transgenic mice expressing human immunodeficiency virus type 1. J. Infect. Dis. 185:1103-1114. [DOI] [PubMed] [Google Scholar]
- 117.Desrosiers, R. C. 1990. The simian immunodeficiency viruses. Annu. Rev. Immunol. 8:557-578. [DOI] [PubMed] [Google Scholar]
- 118.Desrosiers, R. C., and D. J. Ringler. 1989. Use of simian immunodeficiency viruses for AIDS research. Intervirology 30:301-312. [DOI] [PubMed] [Google Scholar]
- 119.Desvignes, C., F. Esteves, N. Etchart, C. Bella, C. Czerkinsky, and D. Kaiserlian. 1998. The murine buccal mucosa is an inductive site for priming class I- restricted CD8+ effector T cells in vivo. Clin. Exp. Immunol. 113:386-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Detels, R., P. Tarwater, J. P. Phair, J. Margolick, S. A. Riddler, and A. Munoz. 2001. Effectiveness of potent antiretroviral therapies on the incidence of opportunistic infections before and after AIDS diagnosis. AIDS 15:347-355. [DOI] [PubMed] [Google Scholar]
- 121.Diaz-Guerra, T. M., J. V. Martinez-Suarez, F. Laguna, and J. L. Rodriguez-Tudela. 1997. Comparison of four molecular typing methods for evaluating genetic diversity among Candida albicans isolates from human immunodeficiency virus-positive patients with oral candidiasis. J. Clin. Microbiol. 35:856-861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dickie, P. 2000. Nef modulation of HIV type 1 gene expression and cytopathicity in tissues of HIV transgenic mice. AIDS Res. Hum. Retroviruses 16:777-790. [DOI] [PubMed] [Google Scholar]
- 123.Dickie, P., R. Gazzinelli, and L. J. Chang. 1996. Models of HIV type 1 proviral gene expression in wild-type HIV and MLV/HIV transgenic mice. AIDS Res. Hum. Retroviruses 12:1103-1116. [DOI] [PubMed] [Google Scholar]
- 124.Dickie, P., F. Ramsdell, A. L. Notkins, and S. Venkatesan. 1993. Spontaneous and inducible epidermal hyperplasia in transgenic mice expressing HIV-1 Nef. Virology 197:431-438. [DOI] [PubMed] [Google Scholar]
- 125.Dieleman, J. P., M. Jambroes, I. C. Gyssens, M. C. Sturkenboom, B. H. Stricker, W. M. Mulder, F. de Wolf, G. J. Weverling, J. M. Lange, P. Reiss, and K. Brinkman. 2002. Determinants of recurrent toxicity-driven switches of highly active antiretroviral therapy. The ATHENA cohort. AIDS 16:737-745. [DOI] [PubMed] [Google Scholar]
- 126.Dipaola, C., and I. D. Mandel. 1980. Lactoferrin concentration in human parotid saliva as measured by an enzyme-linked immunosorbent assay (ELISA). J. Dent. Res. 59:1463-1465. [DOI] [PubMed] [Google Scholar]
- 127.Diz, D. P., A. Ocampo, C. Miralles, I. Otero, I. Iglesias, and N. Rayo. 1999. Frequency of oropharyngeal candidiasis in HIV-infected patients on protease inhibitor therapy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 87:437-441. [DOI] [PubMed] [Google Scholar]
- 128.Diz, D. P., A. Ocampo, I. Otero, I. Iglesias, and C. Martinez. 2001. Changes in oropharyngeal colonization and infection by Candida albicans in human immunodeficiency virus-infected patients. J. Infect. Dis. 183:355-356. [DOI] [PubMed] [Google Scholar]
- 129.Dodd, C. L., D. Greenspan, M. H. Katz, J. L. Westenhouse, D. W. Feigal, and J. S. Greenspan. 1991. Oral candidiasis in HIV infection: pseudomembranous and erythematous candidiasis show similar rates of progression to AIDS. AIDS 5:1339-1343. [PubMed] [Google Scholar]
- 130.Donaghy, H., A. Pozniak, B. Gazzard, N. Qazi, J. Gilmour, F. Gotch, and S. Patterson. 2001. Loss of blood CD11c+ myeloid and CD11c− plasmacytoid dendritic cells in patients with HIV-1 infection correlates with HIV-1 RNA virus load. Blood 98:2574-2576. [DOI] [PubMed] [Google Scholar]
- 131.Dongari-Bagtzoglou, A., and H. Kashleva. 2003. Granulocyte-macrophage colony-stimulating factor responses of oral epithelial cells to Candida albicans. Oral Microbiol. Immunol. 18:165-170. [DOI] [PubMed] [Google Scholar]
- 132.Dorschner, R. A., V. K. Pestonjamasp, S. Tamakuwala, T. Ohtake, J. Rudisill, V. Nizet, B. Agerberth, G. H. Gudmundsson, and R. L. Gallo. 2001. Cutaneous injury induces the release of cathelicidin anti-microbial peptides active against group A Streptococcus. J. Investig. Dermatol. 117:91-97. [DOI] [PubMed] [Google Scholar]
- 132a.d'Ostiani, C. F., G. Del Sero, A. Bacci, C. Montagnoli, A. Spreca, A. Mencacci, P. Ricciardi-Castagnoli, and L. Romani. 2000. Dendritic cells discriminate between yeasts and hyphae of the fungus Candida albicans. Implications for initiation of T helper cell immunity in vitro and in vivo. J. Exp. Med. 191:1661-1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Drobacheff, C., L. Millon, M. Monod, R. Piarroux, E. Robinet, R. Laurent, and D. Meillet. 2001. Increased serum and salivary immunoglobulins against Candida albicans in HIV-infected patients with oral candidiasis. Clin. Chem. Lab. Med. 39:519-526. [DOI] [PubMed] [Google Scholar]
- 134.Dunsche, A., Y. Acil, H. Dommisch, R. Siebert, J. M. Schroder, and S. Jepsen. 2002. The novel human beta-defensin-3 is widely expressed in oral tissues. Eur. J. Oral Sci. 110:121-124. [DOI] [PubMed] [Google Scholar]
- 135.Dunsche, A., Y. Acil, R. Siebert, J. Harder, J. M. Schroder, and S. Jepsen. 2001. Expression profile of human defensins and antimicrobial proteins in oral tissues. J. Oral Pathol. Med. 30:154-158. [DOI] [PubMed] [Google Scholar]
- 136.Dustin, M. L., K. H. Singer, D. T. Tuck, and T. A. Springer. 1988. Adhesion of T lymphoblasts to epidermal keratinocytes is regulated by interferon gamma and is mediated by intercellular adhesion molecule 1 (ICAM-1). J. Exp. Med. 167:1323-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Eales, L. J., J. Farrant, M. Helbert, and A. J. Pinching. 1988. Peripheral blood dendritic cells in persons with AIDS and AIDS related complex: loss of high intensity class II antigen expression and function. Clin. Exp. Immunol 71:423-427. [PMC free article] [PubMed] [Google Scholar]
- 138.Edgerton, M., S. E. Koshlukova, T. E. Lo, B. G. Chrzan, R. M. Straubinger, and P. A. Raj. 1998. Candidacidal activity of salivary histatins. Identification of a histatin 5-binding protein on Candida albicans. J. Biol. Chem. 273:20438-20447. [DOI] [PubMed] [Google Scholar]
- 139.Edgerton, M., and M. J. Levine. 1992. Characterization of acquired denture pellicle from healthy and stomatitis patients. J. Prosthet. Dent. 68:683-691. [DOI] [PubMed] [Google Scholar]
- 140.Edgerton, M., F. A. Scannapieco, M. S. Reddy, and M. J. Levine. 1993. Human submandibular-sublingual saliva promotes adhesion of Candida albicans to polymethylmethacrylate. Infect. Immun. 61:2644-2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Eisenberg, S. P., K. K. Hale, P. Heimdal, and R. C. Thompson. 1990. Location of the protease-inhibitory region of secretory leukocyte protease inhibitor. J. Biol. Chem. 265:7976-7981. [PubMed] [Google Scholar]
- 142.Elahi, S., G. Pang, R. Clancy, and R. B. Ashman. 2000. Cellular and cytokine correlates of mucosal protection in murine model of oral candidiasis. Infect. Immun. 68:5771-5777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ellis, M., S. Gupta, S. Galant, S. Hakim, C. VandeVen, C. Toy, and M. S. Cairo. 1988. Impaired neutrophil function in patients with AIDS or AIDS- related complex: a comprehensive evaluation. J. Infect. Dis. 158:1268-1276. [DOI] [PubMed] [Google Scholar]
- 144.Epstein, J. B., L. H. Kimura, T. W. Menard, E. L. Truelove, and N. N. Pearsall. 1982. Effects of specific antibodies on the interaction between the fungus Candida albicans and human oral mucosa. Arch. Oral Biol. 27:469-474. [DOI] [PubMed] [Google Scholar]
- 145.Eroschenko, V. P. 2000. Atlas of histology with functional correlations. di Fiore's, Baltimore, Md.
- 146.Eversole, L. R., K. T. Miyasaki, and R. E. Christensen. 1993. Keratinocyte expression of calprotectin in oral inflammatory mucosal diseases. J. Oral Pathol. Med. 22:303-307. [DOI] [PubMed] [Google Scholar]
- 147.Eversole, L. R., P. A. Reichart, G. Ficarra, A. Schmidt-Westhausen, P. Romagnoli, and N. Pimpinelli. 1997. Oral keratinocyte immune responses in HIV-associated candidiasis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 84:372-380. [DOI] [PubMed] [Google Scholar]
- 148.Fan, Z., X. L. Huang, L. Zheng, C. Wilson, L. Borowski, J. Liebmann, P. Gupta, J. Margolick, and C. Rinaldo. 1997. Cultured blood dendritic cells retain HIV-1 antigen-presenting capacity for memory CTL during progressive HIV-1 infection. J. Immunol. 159:4973-4982. [PubMed] [Google Scholar]
- 149.Farah, C. S., S. Elahi, K. Drysdale, G. Pang, T. Gotjamanos, G. J. Seymour, R. L. Clancy, and R. B. Ashman. 2002. Primary role for CD4+ T lymphocytes in recovery from oropharyngeal candidiasis. Infect. Immun. 70:724-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Farah, C. S., S. Elahi, G. Pang, T. Gotjamanos, G. J. Seymour, R. L. Clancy, and R. B. Ashman. 2001. T cells augment monocyte and neutrophil function in host resistance against oropharyngeal candidiasis. Infect. Immun. 69:6110-6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Fauci, A. S., G. Pantaleo, S. Stanley, and D. Weissman. 1996. Immunopathogenic mechanisms of HIV infection. Ann. Intern. Med. 124:654-663. [DOI] [PubMed] [Google Scholar]
- 152.Feigal, D. W., M. H. Katz, D. Greenspan, J. Westenhouse, W. Winkelstein, Jr., W. Lang, M. Samuel, S. P. Buchbinder, N. A. Hessol, A. R. Lifson, et al. 1991. The prevalence of oral lesions in HIV-infected homosexual and bisexual men: three San Francisco epidemiological cohorts. AIDS 5:519-525. [DOI] [PubMed] [Google Scholar]
- 153.Feldman, G. M., and D. S. Finbloom. 1990. Induction and regulation of IL-4 receptor expression on murine macrophage cell lines and bone marrow- derived macrophages by IFN-gamma. J. Immunol. 145:854-859. [PubMed] [Google Scholar]
- 154.Ferguson, D. W., and B. D. Volpp. 1994. Cardiovascular complications of AIDS. Heart Dis. Stroke 3:388-394. [PubMed] [Google Scholar]
- 155.Fichtenbaum, C. J. 2003. Candidiasis, p. 531-542. In R. Dolin, H. Masur, and M. S. Saag (ed.), AIDS therapy. Churchill Livingstone, Inc., New York, N.Y.
- 156.Fichtenbaum, C. J., S. Koletar, C. Yiannoutsos, F. Holland, J. Pottage, S. E. Cohn, A. Walawander, P. Frame, J. Feinberg, M. Saag, H. C. Van der, and W. G. Powderly. 2000. Refractory mucosal candidiasis in advanced human immunodeficiency virus infection. Clin. Infect. Dis. 30:749-756. [DOI] [PubMed] [Google Scholar]
- 157.Fidel, P. L., Jr. 2002. Distinct protective host defenses against oral and vaginal candidiasis. Med. Mycol. 40:359-375. [PubMed] [Google Scholar]
- 158.Fidel, P. L., Jr., and J. D. Sobel. 1996. Immunopathogenesis of recurrent vulvovaginal candidiasis. Clin. Microbiol. Rev. 9:335-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Fidel, P. L., Jr., J. A. Vazquez, and J. D. Sobel. 1999. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin. Microbiol. Rev. 12:80-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Fidel, P. L., Jr., N. A. Wolf, and M. A. KuKuruga. 1996. T lymphocytes in the murine vaginal mucosa are phenotypically distinct from those in the periphery. Infect. Immun. 64:3793-3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Fong, I. W., M. Laurel, and A. Burford-Mason. 1997. Asymptomatic oral carriage of Candida albicans in patients with HIV infection. Clin. Investig. Med. 20:85-93. [PubMed] [Google Scholar]
- 162.Formanek, M., B. Knerer, and J. Kornfehl. 1999. Cytokine expression of human oral keratinocytes. J. Otorhinolaryngol. Relat. Spec. 61:103-107. [DOI] [PubMed] [Google Scholar]
- 163.Frank, I., L. Kacani, H. Stoiber, H. Stossel, M. Spruth, F. Steindl, N. Romani, and M. P. Dierich. 1999. Human immunodeficiency virus type 1 derived from cocultures of immature dendritic cells with autologous T cells carries T-cell-specific molecules on its surface and is highly infectious. J. Virol. 73:3449-3454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Frankel, S. S., K. Tenner-Racz, P. Racz, B. M. Wenig, C. H. Hansen, D. Heffner, A. M. Nelson, M. Pope, and R. M. Steinman. 1997. Active replication of HIV-1 at the lymphoepithelial surface of the tonsil. Am. J. Pathol. 151:89-96. [PMC free article] [PubMed] [Google Scholar]
- 165.Frankel, S. S., B. M. Wenig, A. P. Burke, P. Mannan, L. D. Thompson, S. L. Abbondanzo, A. M. Nelson, M. Pope, and R. M. Steinman. 1996. Replication of HIV-1 in dendritic cell-derived syncytia at the mucosal surface of the adenoid. Science 272:115-117. [DOI] [PubMed] [Google Scholar]
- 166.Frohm, M., B. Agerberth, G. Ahangari, M. Stahle-Backdahl, S. Liden, H. Wigzell, and G. H. Gudmundsson. 1997. The expression of the gene coding for the antibacterial peptide LL-37 is induced in human keratinocytes during inflammatory disorders. J. Biol. Chem. 272:15258-15263. [DOI] [PubMed] [Google Scholar]
- 167.Frohm, N. M., B. Sandstedt, O. Sorensen, G. Weber, N. Borregaard, and M. Stahle-Backdahl. 1999. The human cationic antimicrobial protein (hCAP18), a peptide antibiotic, is widely expressed in human squamous epithelia and colocalizes with interleukin-6. Infect. Immun. 67:2561-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Gabrilovich, D. I., A. T. Kozhich, Z. K. Suvorova, V. S. Ivanov, S. A. Moshnikov, L. D. Chikin, O. V. Kolezonkova, and V. V. Pokrovsky. 1991. Influence of HIV antigens on functional activity of neutrophilic granulocytes. Scand. J. Immunol. 33:549-552. [DOI] [PubMed] [Google Scholar]
- 169.Ganser, A. 1988. Abnormalities of hematopoiesis in the acquired immunodeficiency syndrome. Blut 56:49-53. [DOI] [PubMed] [Google Scholar]
- 170.Ganz, T. 2002. Epithelia: not just physical barriers. Proc. Natl. Acad. Sci. USA 99:3357-3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gaulton, G. N., J. V. Scobie, and M. Rosenzweig. 1997. HIV-1 and the thymus. AIDS 11:403-414. [DOI] [PubMed] [Google Scholar]
- 172.Ghannoum, M. A. 2000. Potential role of phospholipases in virulence and fungal pathogenesis. Clin. Microbiol. Rev. 13:122-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gonwa, T. A., L. J. Picker, H. V. Raff, S. M. Goyert, J. Silver, and J. D. Stobo. 1983. Antigen-presenting capabilities of human monocytes correlates with their expression of HLA-DS, an Ia determinant distinct from HLA-DR. J. Immunol. 130:706-711. [PubMed] [Google Scholar]
- 174.Granelli-Piperno, A., E. Delgado, V. Finkel, W. Paxton, and R. M. Steinman. 1998. Immature dendritic cells selectively replicate macrophagetropic (M-tropic) human immunodeficiency virus type 1, while mature cells efficiently transmit both M- and T-tropic virus to T cells. J. Virol. 72:2733-2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Grassi, F., A. Hosmalin, D. McIlroy, V. Calvez, P. Debre, and B. Autran. 1999. Depletion in blood CD11c-positive dendritic cells from HIV-infected patients. AIDS 13:759-766. [DOI] [PubMed] [Google Scholar]
- 176.Greenberg, M. E., A. J. Iafrate, and J. Skowronski. 1998. The SH3 domain-binding surface and an acidic motif in HIV-1 Nef regulate trafficking of class I MHC complexes. EMBO J. 17:2777-2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Greenspan, D., E. Komaroff, M. Redford, J. A. Phelan, M. Navazesh, M. E. Alves, H. Kamrath, R. Mulligan, C. E. Barr, and J. S. Greenspan. 2000. Oral mucosal lesions and HIV viral load in the Women's Interagency HIV Study (WIHS). J. Acquir. Immune. Defic. Syndr. 25:44-50. [DOI] [PubMed] [Google Scholar]
- 178.Greenspan, J. S., C. E. Barr, J. J. Sciubba, J. R. Winkler, and The U.S.A. Oral AIDS Collaborative Group. 1992. Oral manifestations of HIV infection. Definitions, diagnostic criteria, and principles of therapy. Oral Surg. Oral Med. Oral Pathol. 73:142-144. [DOI] [PubMed] [Google Scholar]
- 179.Grone, A. 2002. Keratinocytes and cytokines. Vet. Immunol. Immunopathol. 88:1-12. [DOI] [PubMed] [Google Scholar]
- 180.Gruber, A., E. Lukasser-Vogl, M. Borg-von Zepelin, M. P. Dierich, and R. Wurzner. 1998. Human immunodeficiency virus type 1 gp160 and gp41 binding to Candida albicans selectively enhances candidal virulence in vitro. J. Infect. Dis. 177:1057-1063. [DOI] [PubMed] [Google Scholar]
- 181.Grunfeld, C., and K. R. Feingold. 1992. Metabolic disturbances and wasting in the acquired immunodeficiency syndrome. N. Engl. J. Med. 327:329-337. [DOI] [PubMed] [Google Scholar]
- 182.Guthmiller, J. M., K. G. Vargas, R. Srikantha, L. L. Schomberg, P. L. Weistroffer, P. B. McCray, Jr., and B. F. Tack. 2001. Susceptibilities of oral bacteria and yeast to mammalian cathelicidins. Antimicrob. Agents Chemother. 45:3216-3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Gyurko, C., U. Lendenmann, E. J. Helmerhorst, R. F. Troxler, and F. G. Oppenheim. 2001. Killing of Candida albicans by histatin 5: cellular uptake and energy requirement. Antonie Leeuwenhoek 79:297-309. [DOI] [PubMed] [Google Scholar]
- 184.Han, Y., M. H. Riesselman, and J. E. Cutler. 2000. Protection against candidiasis by an immunoglobulin G3 (IgG3) monoclonal antibody specific for the same mannotriose as an IgM protective antibody. Infect. Immun. 68:1649-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Handschel, J., C. Sunderkotter, F. J. Prott, U. Meyer, B. Kruse-Losler, and U. Joos. 2001. Increase of RM3/1-positive macrophages in radiation- induced oral mucositis. J. Pathol. 193:242-247. [DOI] [PubMed] [Google Scholar]
- 186.Hanna, Z., D. G. Kay, M. Cool, S. Jothy, N. Rebai, and P. Jolicoeur. 1998. Transgenic mice expressing human immunodeficiency virus type 1 in immune cells develop a severe AIDS-like disease. J. Virol. 72:121-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hanna, Z., D. G. Kay, N. Rebai, A. Guimond, S. Jothy, and P. Jolicoeur. 1998. Nef harbors a major determinant of pathogenicity for an AIDS-like disease induced by HIV-1 in transgenic mice. Cell 95:163-175. [DOI] [PubMed] [Google Scholar]
- 188.Hanna, Z., N. Rebai, J. Poudrier, and P. Jolicoeur. 2001. Distinct regulatory elements are required for faithful expression of human CD4 in T cells, macrophages, and dendritic cells of transgenic mice. Blood 98:2275-2278. [DOI] [PubMed] [Google Scholar]
- 189.Hanna, Z., C. Simard, A. Laperriere, and P. Jolicoeur. 1994. Specific expression of the human CD4 gene in mature CD4+ CD8− and immature CD4+ CD8+ T cells and in macrophages of transgenic mice. Mol. Cell. Biol. 14:1084-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Hanna, Z., X. Weng, D. G. Kay, J. Poudrier, C. Lowell, and P. Jolicoeur. 2001. The pathogenicity of human immunodeficiency virus (HIV) type 1 Nef in CD4C/HIV transgenic mice is abolished by mutation of its SH3-binding domain, and disease development is delayed in the absence of Hck. J. Virol. 75:9378-9392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Harder, J., J. Bartels, E. Christophers, and J. M. Schroder. 2001. Isolation and characterization of human beta-defensin-3, a novel human inducible peptide antibiotic. J. Biol. Chem. 276:5707-5713. [DOI] [PubMed] [Google Scholar]
- 192.Hasseus, B., U. Dahlgren, G. Bergenholtz, and M. Jontell. 1995. Antigen presenting capacity of Langerhans cells from rat oral epithelium. J. Oral Pathol. Med. 24:56-60. [DOI] [PubMed] [Google Scholar]
- 193.Hasseus, B., M. Jontell, G. Bergenholtz, C. Eklund, and U. I. Dahlgren. 1999. Langerhans cells from oral epithelium are more effective in stimulating allogeneic T-cells in vitro than Langerhans cells from skin epithelium. J. Dent. Res. 78:751-758. [DOI] [PubMed] [Google Scholar]
- 194.Helmerhorst, E. J., R. F. Troxler, and F. G. Oppenheim. 2001. The human salivary peptide histatin 5 exerts its antifungal activity through the formation of reactive oxygen species. Proc. Natl. Acad. Sci. USA 98:14637-14642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Herbein, G., U. Mahlknecht, F. Batliwalla, P. Gregersen, T. Pappas, J. Butler, W. A. O'Brien, and E. Verdin. 1998. Apoptosis of CD8+ T cells is mediated by macrophages through interaction of HIV gp120 with chemokine receptor CXCR4. Nature 395:189-194. [DOI] [PubMed] [Google Scholar]
- 196.Herskowitz, A. 1996. Cardiomyopathy and other symptomatic heart diseases associated with HIV infection. Curr. Opin. Cardiol. 11:325-331. [DOI] [PubMed] [Google Scholar]
- 197.Hill, M. W., J. H. Berg, and I. C. Mackenzie. 1981. Quantitative evaluation of regional differences between epithelia in the adult mouse. Arch. Oral Biol. 26:1063-1067. [DOI] [PubMed] [Google Scholar]
- 198.Hoffman, M. P., and C. G. Haidaris. 1993. Analysis of Candida albicans adhesion to salivary mucin. Infect. Immun. 61:1940-1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hoffman, M. P., and C. G. Haidaris. 1994. Identification and characterization of a Candida albicans-binding proteoglycan secreted from rat submandibular salivary glands. Infect. Immun. 62:828-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Hoover, C. I., M. J. Jantapour, G. Newport, N. Agabian, and S. J. Fisher. 1998. Cloning and regulated expression of the Candida albicans phospholipase B (PLB1) gene. FEMS Microbiol. Lett. 167:163-169. [DOI] [PubMed] [Google Scholar]
- 201.Howcroft, T. K., K. Strebel, M. A. Martin, and D. S. Singer. 1993. Repression of MHC class I gene promoter activity by two-exon Tat of HIV. Science 260:1320-1322. [DOI] [PubMed] [Google Scholar]
- 202.Hube, B. 1996. Candida albicans secreted aspartyl proteinases. Curr. Top. Med. Mycol. 7:55-69. [PubMed] [Google Scholar]
- 203.Hube, B. 1998. Possible role of secreted proteinases in Candida albicans infections. Rev. Iberoam. Micol. 15:68-71. [PubMed] [Google Scholar]
- 204.Hube, B., M. Monod, D. A. Schofield, A. J. Brown, and N. A. Gow. 1994. Expression of seven members of the gene family encoding secretory aspartyl proteinases in Candida albicans. Mol. Microbiol. 14:87-99. [DOI] [PubMed] [Google Scholar]
- 205.Ibrahim, A. S., F. Mirbod, S. G. Filler, Y. Banno, G. T. Cole, Y. Kitajima, J. E. Edwards, Jr., Y. Nozawa, and M. A. Ghannoum. 1995. Evidence implicating phospholipase as a virulence factor of Candida albicans. Infect. Immun. 63:1993-1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Itohara, S., A. G. Farr, J. J. Lafaille, M. Bonneville, Y. Takagaki, W. Haas, and S. Tonegawa. 1990. Homing of a gamma delta thymocyte subset with homogeneous T-cell receptors to mucosal epithelia. Nature 343:754-757. [DOI] [PubMed] [Google Scholar]
- 207.Ives, N. J., B. G. Gazzard, and P. J. Easterbrook. 2001. The changing pattern of AIDS-defining illnesses with the introduction of highly active antiretroviral therapy (HAART) in a London clinic. J. Infect. 42:134-139. [DOI] [PubMed] [Google Scholar]
- 208.Jakob, T., J. Ring, and M. C. Udey. 2001. Multistep navigation of Langerhans/dendritic cells in and out of the skin. J. Allergy Clin. Immunol. 108:688-696. [DOI] [PubMed] [Google Scholar]
- 209.Jensen, J., T. Warner, and E. Balish. 1993. Resistance of SCID mice to Candida albicans administered intravenously or colonizing the gut: role of polymorphonuclear leukocytes and macrophages. J. Infect. Dis. 167:912-919. [DOI] [PubMed] [Google Scholar]
- 210.Jensen, J., T. Warner, and E. Balish. 1994. The role of phagocytic cells in resistance to disseminated candidiasis in granulocytopenic mice. J. Infect. Dis. 170:900-905. [DOI] [PubMed] [Google Scholar]
- 211.Jensen, J., T. Warner, C. Johnson, and E. Balish. 1996. Oral immunization of mice against candidiasis. J. Infect. Dis. 174:133-140. [DOI] [PubMed] [Google Scholar]
- 212.Jin, Y., H. K. Yip, Y. H. Samaranayake, J. Y. Yau, and L. P. Samaranayake. 2003. Biofilm-forming ability of Candida albicans is unlikely to contribute to high levels of oral yeast carriage in cases of human immunodeficiency virus infection. J. Clin. Microbiol. 41:2961-2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Jones-Carson, J., A. Vazquez-Torres, H. C. van der Heyde, T. Warner, R. D. Wagner, and E. Balish. 1995. Gamma delta T cell-induced nitric oxide production enhances resistance to mucosal candidiasis. Nat. Med. 1:552-557. [DOI] [PubMed] [Google Scholar]
- 214.Jontell, M., A. Scheynius, S. C. Ohman, and B. Magnusson. 1986. Expression of Class II transplantation antigens by epithelial cells in oral candidosis, oral lichen planus and gingivitis. J. Oral Pathol. 15:484-488. [DOI] [PubMed] [Google Scholar]
- 215.Joshi, V. V. 1994. Pathology of acquired immunodeficiency syndrome in children. Pediatr. Hematol. Oncol. 11:351-355. [DOI] [PubMed] [Google Scholar]
- 216.Jotwani, R., A. K. Palucka, M. Al Quotub, M. Nouri-Shirazi, J. Kim, D. Bell, J. Banchereau, and C. W. Cutler. 2001. Mature dendritic cells infiltrate the T cell-rich region of oral mucosa in chronic periodontitis: in situ, in vivo, and in vitro studies. J. Immunol. 167:4693-4700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Kahn, J. O., and B. D. Walker. 1998. Acute human immunodeficiency virus type 1 infection. N. Engl. J. Med. 339:33-39. [DOI] [PubMed] [Google Scholar]
- 218.Kanazawa, S., T. Okamoto, and B. M. Peterlin. 2000. Tat competes with CIITA for the binding to P-TEFb and blocks the expression of MHC class II genes in HIV infection. Immunity 12:61-70. [DOI] [PubMed] [Google Scholar]
- 219.Kao, A. S., M. E. Brandt, W. R. Pruitt, L. A. Conn, B. A. Perkins, D. S. Stephens, W. S. Baughman, A. L. Reingold, G. A. Rothrock, M. A. Pfaller, R. W. Pinner, and R. A. Hajjeh. 1999. The epidemiology of candidemia in two United States cities: results of a population-based active surveillance. Clin. Infect. Dis. 29:1164-1170. [DOI] [PubMed] [Google Scholar]
- 220.Kapas, S., A. Bansal, V. Bhargava, R. Maher, D. Malli, E. Hagi-Pavli, and R. P. Allaker. 2001. Adrenomedullin expression in pathogen-challenged oral epithelial cells. Peptides 22:1485-1489. [DOI] [PubMed] [Google Scholar]
- 221.Kapas, S., M. L. Tenchini, and P. M. Farthing. 2001. Regulation of adrenomedullin secretion in cultured human skin and oral keratinocytes. J. Investig. Dermatol. 117:353-359. [DOI] [PubMed] [Google Scholar]
- 222.Kaplan, J. E., D. Hanson, M. S. Dworkin, T. Frederick, J. Bertolli, M. L. Lindegren, S. Holmberg, and J. L. Jones. 2000. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clin. Infect. Dis. 30(Suppl. 1):S5-S14. [DOI] [PubMed] [Google Scholar]
- 223.Katou, F., H. Ohtani, A. Saaristo, H. Nagura, and K. Motegi. 2000. Immunological activation of dermal Langerhans cells in contact with lymphocytes in a model of human inflamed skin. Am. J. Pathol. 156:519-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Katz, M. H., D. Greenspan, J. Westenhouse, N. A. Hessol, S. P. Buchbinder, A. R. Lifson, S. Shiboski, D. Osmond, A. Moss, M. Samuel, et al. 1992. Progression to AIDS in HIV-infected homosexual and bisexual men with hairy leukoplakia and oral candidiasis. AIDS 6:95-100. [DOI] [PubMed] [Google Scholar]
- 225.Kaul, S., M. C. Fishbein, and R. J. Siegel. 1991. Cardiac manifestations of acquired immune deficiency syndrome: a 1991 update. Am. Heart J. 122:535-544. [DOI] [PubMed] [Google Scholar]
- 226.Kawabe, T., T. Naka, K. Yoshida, T. Tanaka, H. Fujiwara, S. Suematsu, N. Yoshida, T. Kishimoto, and H. Kikutani. 1994. The immune responses in CD40-deficient mice: impaired immunoglobulin class switching and germinal center formation. Immunity 1:167-178. [DOI] [PubMed] [Google Scholar]
- 227.Kay, D. G., P. Yue, Z. Hanna, S. Jothy, E. Tremblay, and P. Jolicoeur. 2002. Cardiac disease in transgenic mice expressing human immunodeficiency virus-1 nef in cells of the immune system. Am. J. Pathol. 161:321-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Kazazi, F., J. M. Mathijs, P. Foley, and A. L. Cunningham. 1989. Variations in CD4 expression by human monocytes and macrophages and their relationships to infection with the human immunodeficiency virus. J. Gen. Virol. 70:2661-2672. [DOI] [PubMed] [Google Scholar]
- 229.Kirschner, D. E., R. Mehr, and A. S. Perelson. 1998. Role of the thymus in pediatric HIV-1 infection. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 18:95-109. [DOI] [PubMed] [Google Scholar]
- 230.Klein, R. S., C. A. Harris, C. B. Small, B. Moll, M. Lesser, and G. H. Friedland. 1984. Oral candidiasis in high-risk patients as the initial manifestation of the acquired immunodeficiency syndrome. N. Engl. J. Med. 311:354-358. [DOI] [PubMed] [Google Scholar]
- 231.Kleinegger, C. L., D. C. Stoeckel, and Z. B. Kurago. 2001. A comparison of salivary calprotectin levels in subjects with and without oral candidiasis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 92:62-67. [DOI] [PubMed] [Google Scholar]
- 232.Klotman, P. E., J. Rappaport, P. Ray, J. B. Kopp, R. Franks, L. A. Bruggeman, and A. L. Notkins. 1995. Transgenic models of HIV-1. AIDS 9:313-324. [PubMed] [Google Scholar]
- 233.Knight, S. C. 1994. AIDS. A problem of antigen presentation? Curr. Biol. 4:1131-1134. [DOI] [PubMed] [Google Scholar]
- 234.Knight, S. C., and S. Patterson. 1997. Bone marrow-derived dendritic cells, infection with human immunodeficiency virus, and immunopathology. Annu. Rev. Immunol. 15:593-615. [DOI] [PubMed] [Google Scholar]
- 235.Knobel, H., J. Alonso, J. L. Casado, J. Collazos, J. Gonzalez, I. Ruiz, J. M. Kindelan, A. Carmona, J. Juega, and A. Ocampo. 2002. Validation of a simplified medication adherence questionnaire in a large cohort of HIV- infected patients: the GEEMA Study. AIDS 16:605-613. [DOI] [PubMed] [Google Scholar]
- 236.Koelsch, G., J. Tang, J. A. Loy, M. Monod, K. Jackson, S. I. Foundling, and X. Lin. 2000. Enzymic characteristics of secreted aspartic proteases of Candida albicans. Biochim. Biophys. Acta 1480:117-131. [DOI] [PubMed] [Google Scholar]
- 237.Kolokotronis, A., V. Kioses, D. Antoniades, K. Mandraveli, I. Doutsos, and P. Papanayotou. 1994. Immunologic status in patients infected with HIV with oral candidiasis and hairy leukoplakia. Oral Surg. Oral Med. Oral Pathol. 78:41-46. [DOI] [PubMed] [Google Scholar]
- 238.Korting, H. C., M. Schaller, G. Eder, G. Hamm, U. Bohmer, and B. Hube. 1999. Effects of the human immunodeficiency virus (HIV) proteinase inhibitors saquinavir and indinavir on in vitro activities of secreted aspartyl proteinases of Candida albicans isolates from HIV-infected patients. Antimicrob. Agents Chemother. 43:2038-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Kuipers, M. E., J. Heegsma, H. I. Bakker, D. K. Meijer, P. J. Swart, E. W. Frijlink, A. C. Eissens, H. G. Vries-Hospers, and J. J. van den Berg. 2002. Design and fungicidal activity of mucoadhesive lactoferrin tablets for the treatment of oropharyngeal candidosis. Drug Deliv. 9:31-38. [DOI] [PubMed] [Google Scholar]
- 240.Kunkl, A., L. Mortara, M. T. Valle, D. Fenoglio, M. P. Terranova, A. M. Megiovanni, A. Alessandrini, P. G. Li, G. Mazzarello, B. Del, V. A. Canessa, D. Bassetti, and F. Manca. 1998. Recognition of antigenic clusters of Candida albicans by T lymphocytes from human immunodeficiency virus-infected persons. J. Infect. Dis. 178:488-496. [DOI] [PubMed] [Google Scholar]
- 241.Kutsch, C. L., D. A. Norris, and W. P. Arend. 1993. Tumor necrosis factor- alpha induces interleukin-1 alpha and interleukin-1 receptor antagonist production by cultured human keratinocytes. J. Investig. Dermatol. 101:79-85. [DOI] [PubMed] [Google Scholar]
- 242.Lacasse, M., C. Fortier, L. Trudel, A. J. Collet, and N. Deslauriers. 1990. Experimental oral candidosis in the mouse: microbiologic and histologic aspects. J. Oral Pathol. Med. 19:136-141. [DOI] [PubMed] [Google Scholar]
- 243.Laible, N. J., and G. R. Germaine. 1985. Bactericidal activity of human lysozyme, muramidase-inactive lysozyme, and cationic polypeptides against Streptococcus sanguis and Streptococcus faecalis: inhibition by chitin oligosaccharides. Infect. Immun. 48:720-728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Lal, K., J. J. Pollock, R. P. Santarpia III, H. M. Heller, H. W. Kaufman, J. Fuhrer, and R. T. Steigbigel. 1992. Pilot study comparing the salivary cationic protein concentrations in healthy adults and AIDS patients: correlation with antifungal activity. J. Acquir. Immune Defic. Syndr. 5:904-914. [PubMed] [Google Scholar]
- 245.Lappin, M. B., I. Kimber, and M. Norval. 1996. The role of dendritic cells in cutaneous immunity. Arch. Dermatol. Res. 288:109-121. [DOI] [PubMed] [Google Scholar]
- 246.Lasker, B. A., C. M. Elie, T. J. Lott, A. Espinel-Ingroff, L. Gallagher, R. J. Kuykendall, M. E. Kellum, W. R. Pruitt, D. W. Warnock, D. Rimland, M. M. McNeil, and E. Reiss. 2001. Molecular epidemiology of Candida albicans strains isolated from the oropharynx of HIV-positive patients at successive clinic visits. Med. Mycol. 39:341-352. [DOI] [PubMed] [Google Scholar]
- 247.Launay, O., O. Lortholary, C. Bouges-Michel, B. Jarrousse, M. Bentata, and L. Guillevin. 1998. Candidemia: a nosocomial complication in adults with late-stage AIDS. Clin. Infect. Dis. 26:1134-1141. [DOI] [PubMed] [Google Scholar]
- 248.Le Gall, S., L. Erdtmann, S. Benichou, C. Berlioz-Torrent, L. Liu, R. Benarous, J. M. Heard, and O. Schwartz. 1998. Nef interacts with the mu subunit of clathrin adaptor complexes and reveals a cryptic sorting signal in MHC I molecules. Immunity 8:483-495. [DOI] [PubMed] [Google Scholar]
- 249.Leidich, S. D., A. S. Ibrahim, Y. Fu, A. Koul, C. Jessup, J. Vitullo, W. Fonzi, F. Mirbod, S. Nakashima, Y. Nozawa, and M. A. Ghannoum. 1998. Cloning and disruption of caPLB1, a phospholipase B gene involved in the pathogenicity of Candida albicans. J. Biol. Chem. 273:26078-26086. [DOI] [PubMed] [Google Scholar]
- 250.Leigh, J. E., M. Barousse, R. K. Swoboda, T. Myers, S. Hager, N. A. Wolf, J. L. Cutright, J. Thompson, J. D. Sobel, and P. L. Fidel, Jr. 2001. Candida-specific systemic cell-mediated immune reactivities in human immunodeficiency virus-positive persons with mucosal candidiasis. J. Infect. Dis. 183:277-285. [DOI] [PubMed] [Google Scholar]
- 251.Leigh, J. E., C. Steele, F. Wormley, and P. L. Fidel, Jr. 2002. Salivary cytokine profiles in the immunocompetent individual with Candida-associated denture stomatitis. Oral Microbiol. Immunol. 17:311-314. [DOI] [PubMed] [Google Scholar]
- 252.Leigh, J. E., C. Steele, F. L. Wormley, Jr., W. Luo, R. A. Clark, W. Gallaher, and P. L. Fidel, Jr. 1998. Th1/Th2 cytokine expression in saliva of HIV-positive and HIV-negative individuals: a pilot study in HIV-positive individuals with oropharyngeal candidiasis. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 1:373-380. [DOI] [PubMed] [Google Scholar]
- 253.Lenander-Lumikari, M., and I. Johansson. 1995. Effect of saliva composition on growth of Candida albicans and Torulopsis glabrata. Oral Microbiol. Immunol. 10:233-240. [DOI] [PubMed] [Google Scholar]
- 254.Leonard, J. M., J. W. Abramczuk, D. S. Pezen, R. Rutledge, J. H. Belcher, F. Hakim, G. Shearer, L. Lamperth, W. Travis, T. Fredrickson, et al. 1988. Development of disease and virus recovery in transgenic mice containing HIV proviral DNA. Science 242:1665-1670. [DOI] [PubMed] [Google Scholar]
- 255.Levine, A. M. 2002. Evaluation and management of HIV-infected women. Ann. Intern. Med. 136:228-242. [DOI] [PubMed] [Google Scholar]
- 256.Levitz, S. M., H. L. Mathews, and J. W. Murphy. 1995. Direct antimicrobial activity of T cells. Immunol. Today 16:387-391. [DOI] [PubMed] [Google Scholar]
- 257.Li, J., P. M. Farthing, G. W. Ireland, and M. H. Thornhill. 1996. IL-1 alpha and IL-6 production by oral and skin keratinocytes: similarities and differences in response to cytokine treatment in vitro. J. Oral Pathol. Med. 25:157-162. [DOI] [PubMed] [Google Scholar]
- 258.Lin, A. L., D. A. Johnson, T. F. Patterson, Y. Wu, D. L. Lu, Q. Shi, and C. K. Yeh. 2001. Salivary anticandidal activity and saliva composition in an HIV-infected cohort. Oral Microbiol. Immunol. 16:270-278. [DOI] [PubMed] [Google Scholar]
- 259.Lindemann, D., R. Wilhelm, P. Renard, A. Althage, R. Zinkernagel, and J. Mous. 1994. Severe immunodeficiency associated with a human immunodeficiency virus 1 NEF/3′-long terminal repeat transgene. J. Exp. Med. 179:797-807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Lipshultz, S. E. (ed.). 1998. Cardiology in AIDS. Chapman & Hall, New York, N.Y.
- 261.Liu, A. Y., D. Destoumieux, A. V. Wong, C. H. Park, E. V. Valore, L. Liu, and T. Ganz. 2002. Human beta-defensin-2 production in keratinocytes is regulated by interleukin-1, bacteria, and the state of differentiation. J. Investig. Dermatol. 118:275-281. [DOI] [PubMed] [Google Scholar]
- 262.Lombardi, T., C. Hauser, and E. Budtz-Jorgensen. 1993. Langerhans cells: structure, function and role in oral pathological conditions. J. Oral Pathol. Med. 22:193-202. [DOI] [PubMed] [Google Scholar]
- 263.Lopez-Dupla, M., S. P. Mora, G. Pintado, V, O. E. Valencia, P. L. Uriol, M. A. Khamashta, and A. G. Aguado. 1992. Clinical, endoscopic, immunologic, and therapeutic aspects of oropharyngeal and esophageal candidiasis in HIV-infected patients: a survey of 114 cases. Am. J. Gastroenterol. 87:1771-1776. [PubMed] [Google Scholar]
- 264.Lore, K., A. Sonnerborg, C. Brostrom, L. E. Goh, L. Perrin, H. McDade, H. J. Stellbrink, B. Gazzard, R. Weber, L. A. Napolitano, Y. van Kooyk, and J. Andersson. 2002. Accumulation of DC-SIGN+CD40+ dendritic cells with reduced CD80 and CD86 expression in lymphoid tissue during acute HIV-1 infection. AIDS 16:683-692. [DOI] [PubMed] [Google Scholar]
- 265.Louie, A. T., L. M. Wahl, I. K. Hewlett, J. S. Epstein, and S. Dhawan. 1996. Impaired antigen presentation to CD4+ T-cells by HIV-infected monocytes is related to down-modulation of CD4 expression on helper T-cells: possible involvement of HIV-induced cellular factors. FEBS Lett. 398:1-6. [DOI] [PubMed] [Google Scholar]
- 266.Lu, X. S., J. F. Delfraissy, L. Grangeot-Keros, M. T. Rannou, and J. Pillot. 1994. Rapid and constant detection of HIV antibody response in saliva of HIV-infected patients; selective distribution of anti-HIV activity in the IgG isotype. Res. Virol. 145:369-377. [DOI] [PubMed] [Google Scholar]
- 267.Lundqvist, C., V. Baranov, S. Teglund, S. Hammarstrom, and M. L. Hammarstrom. 1994. Cytokine profile and ultrastructure of intraepithelial gamma delta T cells in chronically inflamed human gingiva suggest a cytotoxic effector function. J. Immunol. 153:2302-2312. [PubMed] [Google Scholar]
- 268.Lundqvist, C., and M. L. Hammarstrom. 1993. T-cell receptor gamma delta-expressing intraepithelial lymphocytes are present in normal and chronically inflamed human gingiva. Immunology 79:38-45. [PMC free article] [PubMed] [Google Scholar]
- 269.Lupetti, A., G. Guzzi, A. Paladini, K. Swart, M. Campa, and S. Senesi. 1995. Molecular typing of Candida albicans in oral candidiasis: karyotype epidemiology with human immunodeficiency virus-seropositive patients in comparison with that with healthy carriers. J. Clin. Microbiol. 33:1238-1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Macallan, D. C. 1999. Wasting in HIV infection and AIDS. J. Nutr. 129:238S-242S. [DOI] [PubMed] [Google Scholar]
- 271.Macatonia, S. E., R. Lau, S. Patterson, A. J. Pinching, and S. C. Knight. 1990. Dendritic cell infection, depletion and dysfunction in HIV-infected individuals. Immunology 71:38-45. [PMC free article] [PubMed] [Google Scholar]
- 272.MacDonald, A. S., and E. J. Pearce. 2002. Cutting edge: polarized Th cell response induction by transferred antigen-pulsed dendritic cells is dependent on IL-4 or IL-12 production by recipient cells. J. Immunol. 168:3127-3130. [DOI] [PubMed] [Google Scholar]
- 273.Maenza, J. R., W. G. Merz, M. J. Romagnoli, J. C. Keruly, R. D. Moore, and J. E. Gallant. 1997. Infection due to fluconazole-resistant Candida in patients with AIDS: prevalence and microbiology. Clin. Infect. Dis. 24:28-34. [DOI] [PubMed] [Google Scholar]
- 274.Mandel, I. D., C. E. Barr, and L. Turgeon. 1992. Longitudinal study of parotid saliva in HIV-1 infection. J. Oral Pathol. Med. 21:209-213. [DOI] [PubMed] [Google Scholar]
- 275.Marcotte, H., and M. C. Lavoie. 1998. Oral microbial ecology and the role of salivary immunoglobulin A. Microbiol. Mol. Biol. Rev. 62:71-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Marder, M. Z., C. E. Barr, and I. D. Mandel. 1985. Cytomegalovirus presence and salivary composition in acquired immunodeficiency syndrome. Oral Surg. Oral Med. Oral Pathol. 60:372-376. [DOI] [PubMed] [Google Scholar]
- 277.Margiotta, V., G. Campisi, S. Mancuso, V. Accurso, and V. Abbadessa. 1999. HIV infection: oral lesions, CD4+ cell count and viral load in an Italian study population. J. Oral Pathol. Med. 28:173-177. [DOI] [PubMed] [Google Scholar]
- 278.Marina, N. M., P. M. Flynn, G. K. Rivera, and W. T. Hughes. 1991. Candida tropicalis and Candida albicans fungemia in children with leukemia. Cancer 68:594-599. [DOI] [PubMed] [Google Scholar]
- 279.Marquis, G., S. Montplaisir, S. Garzon, H. Strykowski, and P. Auger. 1982. Fungitoxicity of muramidase. Ultrastructural damage to Candida albicans. Lab. Investig. 46:627-636. [PubMed] [Google Scholar]
- 280.Martins, M. D., M. Lozano-Chiu, and J. H. Rex. 1998. Declining rates of oropharyngeal candidiasis and carriage of Candida albicans associated with trends toward reduced rates of carriage of fluconazole-resistant C. albicans in human immunodeficiency virus-infected patients. Clin. Infect. Dis. 27:1291-1294. [DOI] [PubMed] [Google Scholar]
- 281.Mathews, M., H. P. Jia, J. M. Guthmiller, G. Losh, S. Graham, G. K. Johnson, B. F. Tack, and P. B. McCray, Jr. 1999. Production of beta- defensin antimicrobial peptides by the oral mucosa and salivary glands. Infect. Immun. 67:2740-2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Matsuura, K., F. Otsuka, and H. Fujisawa. 1998. Effects of interferons on tumour necrosis factor alpha production from human keratinocytes. Cytokine 10:500-505. [DOI] [PubMed] [Google Scholar]
- 283.Mattsson, T., K. G. Sundqvist, A. Heimdahl, G. Dahllof, P. Ljungman, and O. Ringden. 1992. A comparative immunological analysis of the oral mucosa in chronic graft-versus-host disease and oral lichen planus. Arch. Oral Biol. 37:539-547. [DOI] [PubMed] [Google Scholar]
- 284.Mazurier, J., and G. Spik. 1980. Comparative study of the iron-binding properties of human transferrins. I. Complete and sequential iron saturation and desaturation of the lactotransferrin. Biochim. Biophys. Acta 629:399-408. [DOI] [PubMed] [Google Scholar]
- 285.McCarthy, G. M. 1992. Host factors associated with HIV-related oral candidiasis. A review. Oral Surg. Oral Med. Oral Pathol. 73:181-186. [DOI] [PubMed] [Google Scholar]
- 286.McIlroy, D., B. Autran, J. P. Clauvel, E. Oksenhendler, P. Debre, and A. Hosmalin. 1998. Low CD83, but normal MHC class II and costimulatory molecule expression, on spleen dendritic cells from HIV+ patients. AIDS Res. Hum. Retroviruses 14:505-513. [DOI] [PubMed] [Google Scholar]
- 287.McNeely, T. B., M. Dealy, D. J. Dripps, J. M. Orenstein, S. P. Eisenberg, and S. M. Wahl. 1995. Secretory leukocyte protease inhibitor: a human saliva protein exhibiting anti-human immunodeficiency virus 1 activity in vitro. J. Clin. Investig. 96:456-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.McSherry, G. D. 1996. Human immunodeficiency-virus-related pulmonary infections in children. Semin. Respir. Infect. 11:173-183. [PubMed] [Google Scholar]
- 289.Medzhitov, R., and C. Janeway, Jr. 2000. Innate immunity. N. Engl. J. Med. 343:338-344. [DOI] [PubMed] [Google Scholar]
- 290.Meiller, T. F., M. A. Jabra-Rizk, A. Baqui, J. I. Kelley, V. I. Meeks, W. G. Merz, and W. A. Falkler. 1999. Oral Candida dubliniensis as a clinically important species in HIV-seropositive patients in the United States. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 88:573-580. [DOI] [PubMed] [Google Scholar]
- 291.Mencacci, A., G. Del Sero, E. Cenci, C. F. d'Ostiani, A. Bacci, C. Montagnoli, M. Kopf, and L. Romani. 1998. Endogenous interleukin 4 is required for development of protective CD4+ T helper type 1 cell responses to Candida albicans. J. Exp. Med. 187:307-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Mezzaroma, I., M. Carlesimo, E. Pinter, C. Alario, G. Sacco, D. S. Muratori, M. L. Bernardi, R. Paganelli, and F. Aiuti. 1999. Long-term evaluation of T-cell subsets and T-cell function after HAART in advanced stage HIV-1 disease. AIDS 13:1187-1193. [DOI] [PubMed] [Google Scholar]
- 293.Michaels, A. D., R. J. Lederman, J. S. MacGregor, and M. D. Cheitlin. 1997. Cardiovascular involvement in AIDS. Curr. Probl. Cardiol. 22:109-148. [DOI] [PubMed] [Google Scholar]
- 294.Mohamed, A. M. 1975. Ultrastructural aspects of chronic oral candidosis. J. Oral Pathol. 4:180-194. [DOI] [PubMed] [Google Scholar]
- 295.Monod, M., B. Hube, D. Hess, and D. Sanglard. 1998. Differential regulation of SAP8 and SAP9, which encode two new members of the secreted aspartic proteinase family in Candida albicans. Microbiology 144:2731-2737. [DOI] [PubMed] [Google Scholar]
- 296.Morace, G., E. Tamburrini, S. Manzara, A. Antinori, G. Maiuro, and G. Dettori. 1990. Epidemiological and clinical aspects of mycoses in patients with AIDS-related pathologies. Eur. J. Epidemiol. 6:398-403. [DOI] [PubMed] [Google Scholar]
- 297.Moses, A., J. Nelson, and G. C. Bagby, Jr. 1998. The influence of human immunodeficiency virus-1 on hematopoiesis. Blood 91:1479-1495. [PubMed] [Google Scholar]
- 298.Muller, F., S. S. Froland, P. Brandtzaeg, and M. K. Fagerhol. 1993. Oral candidiasis is associated with low levels of parotid calprotectin in individuals with infection due to human immunodeficiency virus. Clin. Infect. Dis. 16:301-302. [DOI] [PubMed] [Google Scholar]
- 299.Muller, F., S. S. Froland, M. Hvatum, J. Radl, and P. Brandtzaeg. 1991. Both IgA subclasses are reduced in parotid saliva from patients with AIDS. Clin. Exp. Immunol. 83:203-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Muller, F., M. Holberg-Petersen, H. Rollag, M. Degre, P. Brandtzaeg, and S. S. Froland. 1992. Nonspecific oral immunity in individuals with HIV infection. J. Acquir. Immune. Defic. Syndr. 5:46-51. [PubMed] [Google Scholar]
- 301.Muller, F. M., M. Kasai, A. Francesconi, B. Brillante, M. Roden, J. Peter, S. J. Chanock, and T. J. Walsh. 1999. Transmission of an azole- resistant isogenic strain of Candida albicans among human immunodeficiency virus-infected family members with oropharyngeal candidiasis. J. Clin. Microbiol. 37:3405-3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Muller, H., S. Weier, G. Kojouharoff, M. Grez, S. Berger, R. Kappus, P. M. Shah, H. J. Stutte, and H. L. Schmidts. 1993. Distribution and infection of Langerhans cells in the skin of HIV-infected healthy subjects and AIDS patients. Res. Virol. 144:59-67. [DOI] [PubMed] [Google Scholar]
- 303.Munk, M. E., A. J. Gatrill, and S. H. Kaufmann. 1990. Target cell lysis and IL-2 secretion by gamma/delta T lymphocytes after activation with bacteria. J. Immunol. 145:2434-2439. [PubMed] [Google Scholar]
- 304.Munro, C. A., and B. Hube. 2002. Anti-fungal therapy at the HAART of viral therapy. Trends Microbiol. 10:173-177. [DOI] [PubMed] [Google Scholar]
- 305.Myers, T. A., J. E. Leigh, A. R. Arribas, S. Hager, R. Clark, E. Lilly, and P. L. Fidel, Jr. 2003. Immunohistochemical evaluation of T cells in oral lesions from human immunodeficiency virus-positive persons with oropharyngeal candidiasis. Infect. Immun. 71:956-963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Myint, M., S. Steinsvoll, Z. N. Yuan, B. Johne, K. Helgeland, and K. Schenck. 2002. Highly increased numbers of leukocytes in inflamed gingiva from patients with HIV infection. AIDS 16:235-243. [DOI] [PubMed] [Google Scholar]
- 307.Naglik, J. R., G. Newport, T. C. White, L. L. Fernandes-Naglik, J. S. Greenspan, D. Greenspan, S. P. Sweet, S. J. Challacombe, and N. Agabian. 1999. In vivo analysis of secreted aspartyl proteinase expression in human oral candidiasis. Infect. Immun. 67:2482-2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Nakanishi, K., T. Yoshimoto, H. Tsutsui, and H. Okamura. 2001. Interleukin-18 regulates both Th1 and Th2 responses. Annu. Rev. Immunol. 19:423-474. [DOI] [PubMed] [Google Scholar]
- 309.Narayanan, R., W. A. Joyce, and R. A. Greenfield. 1991. Gastrointestinal candidiasis in a murine model of severe combined immunodeficiency syndrome. Infect. Immun. 59:2116-2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Newman, S. L., and A. Holly. 2001. Candida albicans is phagocytosed, killed, and processed for antigen presentation by human dendritic cells. Infect. Immun. 69:6813-6822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Nielsen, H., K. D. Bentsen, L. Hojtved, E. H. Willemoes, F. Scheutz, M. Schiodt, K. Stoltze, and J. J. Pindborg. 1994. Oral candidiasis and immune status of HIV-infected patients. J. Oral Pathol. Med. 23:140-143. [DOI] [PubMed] [Google Scholar]
- 312.Nielsen, H., A. Kharazmi, and V. Faber. 1986. Blood monocyte and neutrophil functions in the acquired immune deficiency syndrome. Scand. J. Immunol. 24:291-296. [DOI] [PubMed] [Google Scholar]
- 313.Nikawa, H., L. P. Samaranayake, J. Tenovuo, K. M. Pang, and T. Hamada. 1993. The fungicidal effect of human lactoferrin on Candida albicans and Candida krusei. Arch. Oral Biol. 38:1057-1063. [DOI] [PubMed] [Google Scholar]
- 314.Nose, Y., K. Komori, H. Inouye, K. Nomura, M. Yamamura, and K. Tsuji. 1981. Role of macrophages in T lymphocyte response to Candida allergen in man with special reference to HLA-D and DR. Clin. Exp. Immunol. 45:152-157. [PMC free article] [PubMed] [Google Scholar]
- 315.Nottet, H. S., L. de Graaf, N. M. de Vos, L. J. Bakker, J. A. van Strijp, M. R. Visser, and J. Verhoef. 1993. Phagocytic function of monocyte- derived macrophages is not affected by human immunodeficiency virus type 1 infection. J. Infect. Dis. 168:84-91. [DOI] [PubMed] [Google Scholar]
- 316.O'Brien, W. A. 2000. Resistance against reverse transcriptase inhibitors. Clin. Infect. Dis. 30(Suppl. 2):S185-S192. [DOI] [PubMed] [Google Scholar]
- 317.O'Connell, B. C., T. Xu, T. J. Walsh, T. Sein, A. Mastrangeli, R. G. Crystal, F. G. Oppenheim, and B. J. Baum. 1996. Transfer of a gene encoding the anticandidal protein histatin 3 to salivary glands. Hum. Gene Ther. 7:2255-2261. [DOI] [PubMed] [Google Scholar]
- 318.Odden, K., K. Schenck, and B. Hurlen. 1995. High numbers of T cells in gingiva from patients with human immunodeficiency virus (HIV) infection. J. Oral Pathol. Med. 24:413-419. [DOI] [PubMed] [Google Scholar]
- 319.Odds, F. C. 1988. Candida and candidasis: a review and bibliography. Baillière Tindall, London, United Kingdom.
- 320.Ohman, S. C., M. Jontell, and R. Jonsson. 1989. Phenotypic characterization of mononuclear cells and class II antigen expression in angular cheilitis infected by Candida albicans or Staphylococcus aureus. Scand. J Dent. Res. 97:178-185. [DOI] [PubMed] [Google Scholar]
- 321.Ollert, M. W., C. Wende, M. Gorlich, C. G. McMullan-Vogel, M. Borg-von Zepelin, C. W. Vogel, and H. C. Korting. 1995. Increased expression of Candida albicans secretory proteinase, a putative virulence factor, in isolates from human immunodeficiency virus-positive patients. J. Clin. Microbiol. 33:2543-2549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Pacanowski, J., S. Kahi, M. Baillet, P. Lebon, C. Deveau, C. Goujard, L. Meyer, E. Oksenhendler, M. Sinet, and A. Hosmalin. 2001. Reduced blood CD123+ (lymphoid) and CD11c+ (myeloid) dendritic cell numbers in primary HIV-1 infection. Blood 98:3016-3021. [DOI] [PubMed] [Google Scholar]
- 323.Pakker, N. G., M. T. Roos, R. van Leeuwen, M. D. de Jong, M. Koot, P. Reiss, J. M. Lange, F. Miedema, S. A. Danner, and P. T. Schellekens. 1997. Patterns of T-cell repopulation, virus load reduction, and restoration of T-cell function in HIV-infected persons during therapy with different antiretroviral agents. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 16:318-326. [DOI] [PubMed] [Google Scholar]
- 324.Palella, F. J., Jr., K. M. Delaney, A. C. Moorman, M. O. Loveless, J. Fuhrer, G. A. Satten, D. J. Aschman, S. D. Holmberg, and the HIV Outpatient Study Investigators. 1998. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N. Engl. J. Med. 338:853-860. [DOI] [PubMed] [Google Scholar]
- 325.Pantaleo, G., and A. S. Fauci. 1995. New concepts in the immunopathogenesis of HIV infection. Annu. Rev. Immunol. 13:487-512. [DOI] [PubMed] [Google Scholar]
- 326.Pantaleo, G., C. Graziosi, J. F. Demarest, L. Butini, M. Montroni, C. H. Fox, J. M. Orenstein, D. P. Kotler, and A. S. Fauci. 1993. HIV infection is active and progressive in lymphoid tissue during the clinically latent stage of disease. Nature 362:355-358. [DOI] [PubMed] [Google Scholar]
- 327.Pantaleo, G., C. Graziosi, and A. S. Fauci. 1993. The role of lymphoid organs in the immunopathogenesis of HIV infection. AIDS 7(Suppl. 1):S19-S23. [PubMed] [Google Scholar]
- 328.Patterson, S., N. R. English, H. Longhurst, P. Balfe, M. Helbert, A. J. Pinching, and S. C. Knight. 1998. Analysis of human immunodeficiency virus type 1 (HIV-1) variants and levels of infection in dendritic and T cells from symptomatic HIV-1-infected patients. J. Gen. Virol. 79:247-257. [DOI] [PubMed] [Google Scholar]
- 329.Patton, L. L. 2000. Sensitivity, specificity, and positive predictive value of oral opportunistic infections in adults with HIV/AIDS as markers of immune suppression and viral burden. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 90:182-188. [DOI] [PubMed] [Google Scholar]
- 330.Pena, J. M., M. A. Martinez-Lopez, F. Arnalich, F. J. Barbado, and J. J. Vazquez. 1991. Esophageal candidiasis associated with acute infection due to human immunodeficiency virus: case report and review. Rev. Infect. Dis. 13:872-875. [PubMed] [Google Scholar]
- 331.Pepin, L. F., T. Roger, J. Morisset, and M. Seman. 1993. Preferential V delta 1 expression among TcR gamma/delta-bearing T cells in human oral epithelium. Scand. J. Immunol. 37:289-294. [DOI] [PubMed] [Google Scholar]
- 332.Perea, S., J. L. Lopez-Ribot, W. R. Kirkpatrick, R. K. McAtee, R. A. Santillan, M. Martinez, D. Calabrese, D. Sanglard, and T. F. Patterson. 2001. Prevalence of molecular mechanisms of resistance to azole antifungal agents in Candida albicans strains displaying high-level fluconazole resistance isolated from human immunodeficiency virus-infected patients. Antimicrob. Agents Chemother. 45:2676-2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Petrosillo, N., P. Viale, E. Nicastri, C. Arici, E. Bombana, A. Casella, F. Cristini, M. De Gennaro, F. Dodi, A. Gabbuti, G. Gattuso, L. Irato, P. Maggi, F. Pallavicini, A. Pan, M. Pantaleoni, and G. Ippolito. 2002. Nosocomial bloodstream infections among human immunodeficiency virus- infected patients: incidence and risk factors. Clin. Infect. Dis. 34:677-685. [DOI] [PubMed] [Google Scholar]
- 334.Pieri, L., L. Domenici, and P. Romagnoli. 2001. Langerhans cells differentiation: a three-act play. Ital. J. Anat. Embryol. 106:47-69. [PubMed] [Google Scholar]
- 335.Pietrella, D., T. R. Kozel, C. Monari, F. Bistoni, and A. Vecchiarelli. 2001. Interleukin-12 counterbalances the deleterious effect of human immunodeficiency virus type 1 envelope glycoprotein gp120 on the immune response to Cryptococcus neoformans. J. Infect. Dis. 183:51-58. [DOI] [PubMed] [Google Scholar]
- 336.Pileri, S., M. T. Rivano, E. Raise, G. Gualandi, M. Gobbi, M. Martuzzi, F. M. Gritti, J. Gerdes, and H. Stein. 1986. The value of lymph node biopsy in patients with the acquired immunodeficiency syndrome (AIDS) and the AIDS-related complex (ARC): a morphological and immunohistochemical study of 90 cases. Histopathology 10:1107-1129. [DOI] [PubMed] [Google Scholar]
- 337.Pillay, D., S. Taylor, and D. D. Richman. 2000. Incidence and impact of resistance against approved antiretroviral drugs. Rev. Med. Virol. 10:231-253. [DOI] [PubMed] [Google Scholar]
- 338.Pimpinelli, N., L. Borgognoni, R. Riccardi, G. Ficarra, M. Mori, D. Gaglioti, and P. Romagnoli. 1991. CD36(OKM5)+ dendritic cells in the oral mucosa of HIV− and HIV+ subjects. J. Investig. Dermatol. 97:537-542. [DOI] [PubMed] [Google Scholar]
- 339.Polyak, S., H. Chen, D. Hirsch, I. George, R. Hershberg, and K. Sperber. 1997. Impaired class II expression and antigen uptake in monocytic cells after HIV-1 infection. J. Immunol. 159:2177-2188. [PubMed] [Google Scholar]
- 340.Pope, M. 1999. Mucosal dendritic cells and immunodeficiency viruses. J. Infect. Dis. 179(Suppl. 3):S427-S430. [DOI] [PubMed] [Google Scholar]
- 341.Pope, M., D. Elmore, D. Ho, and P. Marx. 1997. Dendritic cell-T cell mixtures, isolated from the skin and mucosae of macaques, support the replication of SIV. AIDS Res. Hum. Retroviruses 13:819-827. [DOI] [PubMed] [Google Scholar]
- 342.Poudrier, J., X. Weng, D. G. Kay, G. Pare, E. L. Calvo, Z. Hanna, M. H. Kosco-Vilbois, and P. Jolicoeur. 2001. The AIDS disease of CD4C/HIV transgenic mice shows impaired germinal centers and autoantibodies and develops in the absence of IFN-gamma and IL-6. Immunity 15:173-185. [DOI] [PubMed] [Google Scholar]
- 342a.Poudrier, J., X. Weng, D. G. Kay, Z. Hanna, and P. Jolicoeur. 2003. The AIDS-like disease of CD4C/human immunodeficiency virus transgenic mice is associated with accumulation of immature CD11b Hi dendritic cells. J. Virol. 77:11733-11744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Powderly, W. G. 1992. Mucosal candidiasis caused by non-albicans species of Candida in HIV-positive patients. AIDS 6:604-605. [PubMed] [Google Scholar]
- 344.Powderly, W. G., K. Robinson, and E. J. Keath. 1993. Molecular epidemiology of recurrent oral candidiasis in human immunodeficiency virus- positive patients: evidence for two patterns of recurrence. J. Infect. Dis. 168:463-466. [DOI] [PubMed] [Google Scholar]
- 345.Pugliese, A., D. Torre, F. M. Baccino, G. Di Perri, C. Cantamessa, L. Gerbaudo, A. Saini, and V. Vidotto. 2000. Candida albicans and HIV-1 infection. Cell Biochem. Funct. 18:235-241. [DOI] [PubMed] [Google Scholar]
- 346.Quinti, I., C. Palma, E. C. Guerra, M. J. Gomez, I. Mezzaroma, F. Aiuti, and A. Cassone. 1991. Proliferative and cytotoxic responses to mannoproteins of Candida albicans by peripheral blood lymphocytes of HIV- infected subjects. Clin. Exp. Immunol. 85:485-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Qureshi, M. N., C. E. Barr, I. Hewlitt, R. Boorstein, F. Kong, O. Bagasra, L. E. Bobroski, and B. Joshi. 1997. Detection of HIV in oral mucosal cells. Oral Dis. 3(Suppl. 1):S73-S78. [DOI] [PubMed] [Google Scholar]
- 348.Qureshi, M. N., C. E. Barr, T. Seshamma, J. Reidy, R. J. Pomerantz, and O. Bagasra. 1995. Infection of oral mucosal cells by human immunodeficiency virus type 1 in seropositive persons. J. Infect. Dis. 171:190-193. [DOI] [PubMed] [Google Scholar]
- 349.Rabeneck, L., and L. Laine. 1994. Esophageal candidiasis in patients infected with the human immunodeficiency virus. A decision analysis to assess cost-effectiveness of alternative management strategies. Arch. Intern. Med. 154:2705-2710. [DOI] [PubMed] [Google Scholar]
- 350.Raeste, A. M., and H. Tuompo. 1976. Lysozyme activity and flow rate of mixed saliva in children, adolescents and adults. Scand. J. Dent. Res. 84:418-422. [DOI] [PubMed] [Google Scholar]
- 351.Raffaniello, R. D., and M. Roy. 1990. Immunohistological analysis of the immune cells in the normal oral mucosa of aging mice. Gerodontology 9:51-57. [DOI] [PubMed] [Google Scholar]
- 352.Rappaport, J., J. B. Kopp, and P. E. Klotman. 1994. Host virus interactions and the molecular regulation of HIV-1: role in the pathogenesis of HIV-associated nephropathy. Kidney Int. 46:16-27. [DOI] [PubMed] [Google Scholar]
- 353.Re, M. C., G. Furlini, G. Zauli, and M. La Placa. 1994. Human immunodeficiency virus type 1 (HIV-1) and human hematopoietic progenitor cells. Arch. Virol. 137:1-23. [DOI] [PubMed] [Google Scholar]
- 354.Redding, S. W., M. A. Pfaller, S. A. Messer, J. A. Smith, J. Prows, L. L. Bradley, A. W. Fothergill, and M. G. Rinaldi. 1997. Variations in fluconazole susceptibility and DNA subtyping of multiple Candida albicans colonies from patients with AIDS and oral candidiasis suffering one or more episodes of infection. J. Clin. Microbiol. 35:1761-1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Reef, S. E. and K. H. Mayer. 1995. Opportunistic candidal infections in patients infected with human immunodeficiency virus: prevention issues and priorities. Clin. Infect. Dis. 21(Suppl. 1):S99-S102. [DOI] [PubMed] [Google Scholar]
- 356.Reibel, J., E. Dabelsteen, B. Kenrad, and K. Buschard. 1985. Pattern of distribution of T lymphocytes, Langerhans cells and HLA-DR bearing cells in normal human oral mucosa. Scand. J. Dent. Res. 93:513-521. [DOI] [PubMed] [Google Scholar]
- 357.Reichart, P. A., H. P. Philipsen, A. Schmidt-Westhausen, and L. P. Samaranayake. 1995. Pseudomembranous oral candidiasis in HIV infection: ultrastructural findings. J. Oral Pathol. Med. 24:276-281. [DOI] [PubMed] [Google Scholar]
- 358.Reichart, P. A., L. P. Samaranayake, and H. P. Philipsen. 2000. Pathology and clinical correlates in oral candidiasis and its variants: a review. Oral Dis. 6:85-91. [DOI] [PubMed] [Google Scholar]
- 359.Reichart, P. A., A. Schmidt-Westhausen, L. P. Samaranayake, and H. P. Philipsen. 1994. Candida-associated palatal papillary hyperplasia in HIV infection. J. Oral Pathol. Med. 23:403-405. [DOI] [PubMed] [Google Scholar]
- 360.Reichart, P. A., D. Weigel, A. Schmidt-Westhausen, and H. D. Pohle. 1997. Exfoliative cheilitis (EC) in AIDS: association with Candida infection. J. Oral Pathol. Med. 26:290-293. [DOI] [PubMed] [Google Scholar]
- 361.Rhodus, N. L., C. Bloomquist, W. Liljemark, and J. Bereuter. 1997. Prevalence, density, and manifestations of oral Candida albicans in patients with Sjogren's syndrome. J. Otolaryngol. 26:300-305. [PubMed] [Google Scholar]
- 362.Richman, D. D. 2001. HIV chemotherapy. Nature 410:995-1001. [DOI] [PubMed] [Google Scholar]
- 363.Ripeau, J. S., M. Fiorillo, F. Aumont, P. Belhumeur, and L. de Repentigny. 2002. Evidence for differential expression of Candida albicans virulence genes during oral infection in intact and human immunodeficiency virus type 1-transgenic mice. J. Infect. Dis. 185:1094-1102. [DOI] [PubMed] [Google Scholar]
- 364.Rittman, B. R., M. W. Hill, G. A. Rittman, and I. C. Mackenzie. 1987. Age-associated changes in Langerhans cells of murine oral epithelium and epidermis. Arch. Oral Biol. 32:885-889. [DOI] [PubMed] [Google Scholar]
- 365.Rittman, B. R., I. C. Mackenzie, and G. A. Rittman. 1989. Replacement of Langerhans cells in murine palate. J. Oral Pathol. Med. 18:279-281. [DOI] [PubMed] [Google Scholar]
- 366.Robinson, P. G., S. J. Challacombe, A. Sheiham, and J. M. Zakrzewska. 1997. Is erythematous candidiasis associated with advanced HIV disease? Oral Dis. 3(Suppl 1):S116-S118. [DOI] [PubMed] [Google Scholar]
- 367.Romagnoli, P., N. Pimpinelli, M. Mori, P. A. Reichart, L. R. Eversole, and G. Ficarra. 1997. Immunocompetent cells in oral candidiasis of HIV- infected patients: an immunohistochemical and electron microscopical study. Oral Dis. 3:99-105. [DOI] [PubMed] [Google Scholar]
- 368.Rosini, S., S. Caltagirone, G. Tallini, G. Lattanzio, R. Demopoulos, M. Piantelli, and P. Musiani. 1996. Depletion of stromal and intraepithelial antigen-presenting cells in cervical neoplasia in human immunodeficiency virus infection. Hum. Pathol. 27:834-838. [DOI] [PubMed] [Google Scholar]
- 369.Ross, H., L. J. Romrell, and G. I. Kaye. 1995. Histology: a text and atlas. The Williams & Wilkins Co., Baltimore, Md.
- 370.Ross, K. F., and M. C. Herzberg. 2001. Calprotectin expression by gingival epithelial cells. Infect. Immun. 69:3248-3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Rudney, J. D., K. C. Kajander, and Q. T. Smith. 1985. Correlations between human salivary levels of lysozyme, lactoferrin, salivary peroxidaseand secretory immunoglobulin A with different stimulatory states and over time. Arch. Oral Biol. 30:765-771. [DOI] [PubMed] [Google Scholar]
- 372.Runeman, B., J. Faergemann, and O. Larko. 2000. Experimental Candida albicans lesions in healthy humans: dependence on skin pH. Acta Dermatol. Venereol. 80:421-424. [DOI] [PubMed] [Google Scholar]
- 373.Samaranayake, L. P. 1990. Host factors and oral candidosis, p. 66-103. In L. Y. Samaranayake and T. W. MacFarlane (ed.), Oral candidosis. Butterworth & Co. Ltd., London, United Kingdom.
- 374.Samaranayake, L. P. 1992. Oral mycoses in HIV infection. Oral Surg. Oral Med. Oral Pathol. 73:171-180. [DOI] [PubMed] [Google Scholar]
- 375.Samaranayake, L. P., and P. Holmstrup. 1989. Oral candidiasis and human immunodeficiency virus infection. J. Oral Pathol. Med. 18:554-564. [DOI] [PubMed] [Google Scholar]
- 376.Samaranayake, L. P., A. Hughes, D. A. Weetman, and T. W. MacFarlane. 1986. Growth and acid production of Candida species in human saliva supplemented with glucose. J. Oral Pathol. 15:251-254. [DOI] [PubMed] [Google Scholar]
- 377.Samaranayake, L. P., and T. W. MacFarlane. 1982. Factors affecting the in-vitro adherence of the fungal oral pathogen Candida albicans to epithelial cells of human origin. Arch. Oral Biol. 27:869-873. [DOI] [PubMed] [Google Scholar]
- 378.Samaranayake, Y. H., and L. P. Samaranayake. 2001. Experimental oral candidiasis in animal models. Clin. Microbiol. Rev. 14:398-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Samaranayake, Y. H., L. P. Samaranayake, E. H. Pow, V. T. Beena, and K. W. Yeung. 2001. Antifungal effects of lysozyme and lactoferrin against genetically similar, sequential Candida albicans isolates from a human immunodeficiency virus-infected southern Chinese cohort. J. Clin. Microbiol. 39:3296-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Sangeorzan, J. A., S. F. Bradley, X. He, L. T. Zarins, G. L. Ridenour, R. N. Tiballi, and C. A. Kauffman. 1994. Epidemiology of oral candidiasis in HIV-infected patients: colonization, infection, treatment, and emergence of fluconazole resistance. Am. J. Med. 97:339-346. [DOI] [PubMed] [Google Scholar]
- 381.Sawada, S., K. Gowrishankar, R. Kitamura, M. Suzuki, G. Suzuki, S. Tahara, and A. Koito. 1998. Disturbed CD4+ T cell homeostasis and in vitro HIV-1 susceptibility in transgenic mice expressing T cell line-tropic HIV-1 receptors. J. Exp. Med. 187:1439-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Sawada, S., and D. R. Littman. 1991. Identification and characterization of a T-cell-specific enhancer adjacent to the murine CD4 gene. Mol. Cell. Biol. 11:5506-5515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Schaller, M., R. Mailhammer, and H. C. Korting. 2002. Cytokine expression induced by Candida albicans in a model of cutaneous candidosis based on reconstituted human epidermis. J. Med. Microbiol. 51:672-676. [DOI] [PubMed] [Google Scholar]
- 384.Schaller, M., W. Schafer, H. C. Korting, and B. Hube. 1998. Differential expression of secreted aspartyl proteinases in a model of human oral candidosis and in patient samples from the oral cavity. Mol. Microbiol. 29:605-615. [DOI] [PubMed] [Google Scholar]
- 385.Schoenberger, S. P., R. E. Toes, E. I. van der Voort, R. Offringa, and C. J. Melief. 1998. T-cell help for cytotoxic T lymphocytes is mediated by CD40-CD40L interactions. Nature 393:480-483. [DOI] [PubMed] [Google Scholar]
- 386.Schorling, S. R., H. C. Kortinga, M. Froschb, and F. A. Muhlschlegel. 2000. The role of Candida dubliniensis in oral candidiasis in human immunodeficiency virus-infected individuals. Crit Rev. Microbiol. 26:59-68. [DOI] [PubMed] [Google Scholar]
- 387.Schroder, J. M. and J. Harder. 1999. Human beta-defensin-2. Int. J. Biochem. Cell Biol. 31:645-651. [DOI] [PubMed] [Google Scholar]
- 388.Schroeder, H. E. 1991. Oral structural biology. Thieme Medical Publishers, Inc., New York, N.Y.
- 389.Schuman, P., J. D. Sobel, S. E. Ohmit, K. H. Mayer, C. C. Carpenter, A. Rompalo, A. Duerr, D. K. Smith, D. Warren, R. S. Klein, and HIV Epidemiology Research Study (HERS) Group. 1998. Mucosal candidal colonization and candidiasis in women with or at risk for human immunodeficiency virus infection. Clin. Infect. Dis. 27:1161-1167. [DOI] [PubMed] [Google Scholar]
- 390.Seguier, S., G. Godeau, and N. Brousse. 2000. Immunohistological and morphometric analysis of intra-epithelial lymphocytes and Langerhans cells in healthy and diseased human gingival tissues. Arch. Oral Biol. 45:441-452. [DOI] [PubMed] [Google Scholar]
- 391.Seguier, S., G. Godeau, M. Leborgne, G. Pivert, and N. Brousse. 2000. Quantitative morphological analysis of Langerhans cells in healthy and diseased human gingiva. Arch. Oral Biol. 45:1073-1081. [DOI] [PubMed] [Google Scholar]
- 392.Seibel, W. 1988. Basic tissues, p. 969. In D. V. Provenza (ed.), Fundamentals of oral histology and embryology. Lea & Febiger Philadelphia, Pa.
- 393.Selvanayagam, P., G. Lei, T. Bell, S. Ram, H. Brysk, S. Rajaraman, and M. M. Brysk. 1998. Desquamin is an epidermal ribonuclease. J. Cell. Biochem. 68:74-82. [DOI] [PubMed] [Google Scholar]
- 394.Seney, F. D., Jr., D. K. Burns, and F. G. Silva. 1990. Acquired immunodeficiency syndrome and the kidney. Am. J. Kidney Dis. 16:1-13. [DOI] [PubMed] [Google Scholar]
- 395.Sepkowitz, K. A. 1998. Effect of HAART on natural history of AIDS-related opportunistic disorders. Lancet 351:228-230. [DOI] [PubMed] [Google Scholar]
- 396.Shannon, R. P. 2001. SIV cardiomyopathy in non-human primates. Trends Cardiovasc: Med. 11:242-246. [DOI] [PubMed] [Google Scholar]
- 397.Shannon, R. P., M. A. Simon, M. A. Mathier, Y. J. Geng, S. Mankad, and A. A. Lackner. 2000. Dilated cardiomyopathy associated with simian AIDS in nonhuman primates. Circulation 101:185-193. [DOI] [PubMed] [Google Scholar]
- 398.Sherwood, J., N. A. Gow, G. W. Gooday, D. W. Gregory, and D. Marshall. 1992. Contact sensing in Candida albicans: a possible aid to epithelial penetration. J. Med. Vet. Mycol. 30:461-469. [DOI] [PubMed] [Google Scholar]
- 399.Shojaei, A. H. 1998. Buccal mucosa as a route for systemic drug delivery: a review. J. Pharm. Pharm. Sci. 1:15-30. [PubMed] [Google Scholar]
- 400.Simard, M. C., P. Chrobak, D. G. Kay, Z. Hanna, S. Jothy, and P. Jolicoeur. 2002. Expression of simian immunodeficiency virus nef in immune cells of transgenic mice leads to a severe AIDS-like disease. J. Virol. 76:3981-3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Skowronski, J., D. Parks, and R. Mariani. 1993. Altered T cell activation and development in transgenic mice expressing the HIV-1 nef gene. EMBO J. 12:703-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Sobel, J. D., S. E. Ohmit, P. Schuman, R. S. Klein, K. Mayer, A. Duerr, J. A. Vazquez, and A. Rampalo. 2001. The evolution of Candida species and fluconazole susceptibility among oral and vaginal isolates recovered from human immunodeficiency virus (HIV)-seropositive and at-risk HIV-seronegative women. J. Infect. Dis. 183:286-293. [DOI] [PubMed] [Google Scholar]
- 403.Sohnle, P. G., M. J. Hunter, B. Hahn, and W. J. Chazin. 2000. Zinc- reversible antimicrobial activity of recombinant calprotectin (migration inhibitory factor-related proteins 8 and 14). J. Infect. Dis. 182:1272-1275. [DOI] [PubMed] [Google Scholar]
- 404.Soukka, T., J. Tenovuo, and M. Lenander-Lumikari. 1992. Fungicidal effect of human lactoferrin against Candida albicans. FEMS Microbiol. Lett. 69:223-228. [DOI] [PubMed] [Google Scholar]
- 405.Sozzani, S., P. Allavena, A. Vecchi, and A. Mantovani. 2000. Chemokines and dendritic cell traffic. J. Clin. Immunol. 20:151-160. [DOI] [PubMed] [Google Scholar]
- 406.Spellberg, B. and J. E. Edwards, Jr. 2001. Type 1/type 2 immunity in infectious diseases. Clin. Infect. Dis. 32:76-102. [DOI] [PubMed] [Google Scholar]
- 407.Sporri, B., J. von Overbeck, C. U. Brand, J. Schmidli, M. L. Sanchez, R. Grunow, and L. R. Braathen. 1994. Reduced number of Langerhans cells in oral mucosal washings from HIV-1 seropositives. J. Oral Pathol. Med. 23:399-402. [DOI] [PubMed] [Google Scholar]
- 408.Squier, C. A., and M. J. Kremer. 2001. Biology of oral mucosa and esophagus. J. Natl. Cancer Inst. Monogr. 29:7-15. [DOI] [PubMed] [Google Scholar]
- 409.Staib, P., M. Kretschmar, T. Nichterlein, H. Hof, and J. Morschhauser. 2000. Differential activation of a Candida albicans virulence gene family during infection. Proc. Natl. Acad. Sci. USA 97:6102-6107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Steele, C., and P. L. Fidel, Jr. 2002. Cytokine and chemokine production by human oral and vaginal epithelial cells in response to Candida albicans. Infect. Immun. 70:577-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Steele, C., J. Leigh, R. Swoboda, and P. L. Fidel, Jr. 2000. Growth inhibition of Candida by human oral epithelial cells. J. Infect. Dis. 182:1479-1485. [DOI] [PubMed] [Google Scholar]
- 412.Steele, C., J. Leigh, R. Swoboda, H. Ozenci, and P. L. Fidel, Jr. 2001. Potential role for a carbohydrate moiety in anti-Candida activity of human oral epithelial cells. Infect. Immun. 69:7091-7099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Steidley, K. E., S. H. Thompson, M. J. McQuade, S. L. Strong, M. J. Scheidt, and T. E. Van Dyke. 1992. A comparison of T4:T8 lymphocyte ratio in the periodontal lesion of healthy and HIV-positive patients. J. Periodontol. 63:753-756. [DOI] [PubMed] [Google Scholar]
- 414.Stein, D. S., J. A. Korvick, and S. H. Vermund. 1992. CD4+ lymphocyte cell enumeration for prediction of clinical course of human immunodeficiency virus disease: a review. J. Infect. Dis. 165:352-363. [DOI] [PubMed] [Google Scholar]
- 415.Steinhoff, M., T. Brzoska, and T. A. Luger. 2001. Keratinocytes in epidermal immune responses. Curr. Opin. Allergy Clin. Immunol. 1:469-476. [DOI] [PubMed] [Google Scholar]
- 416.Steinman, R. M. 2000. DC-SIGN: a guide to some mysteries of dendritic cells. Cell 100:491-494. [DOI] [PubMed] [Google Scholar]
- 417.Stephens, E. B., C. Tian, S. B. Dalton, and V. H. Gattone. 2000. Simian- human immunodeficiency virus-associated nephropathy in macaques. AIDS Res. Hum. Retroviruses 16:1295-1306. [DOI] [PubMed] [Google Scholar]
- 418.Strauss, J., C. Abitbol, G. Zilleruelo, G. Scott, A. Paredes, S. Malaga, B. Montane, C. Mitchell, W. Parks, and V. Pardo. 1989. Renal disease in children with the acquired immunodeficiency syndrome. N. Engl. J. Med. 321:625-630. [DOI] [PubMed] [Google Scholar]
- 419.Stuchell, R. N., and I. D. Mandel. 1983. A comparative study of salivary lysozyme in caries-resistant and caries-susceptible adults. J. Dent. Res. 62:552-554. [DOI] [PubMed] [Google Scholar]
- 420.Subauste, C. S., M. Wessendarp, A. G. Smulian, and P. T. Frame. 2001. Role of CD40 ligand signaling in defective type 1 cytokine response in human immunodeficiency virus infection. J. Infect. Dis. 183:1722-1731. [DOI] [PubMed] [Google Scholar]
- 421.Sugiyama, Y., S. Nakashima, F. Mirbod, H. Kanoh, Y. Kitajima, M. A. Ghannoum, and Y. Nozawa. 1999. Molecular cloning of a second phospholipase B gene, caPLB2, from Candida albicans. Med. Mycol. 37:61-67. [PubMed] [Google Scholar]
- 422.Sullivan, D., K. Haynes, J. Bille, P. Boerlin, L. Rodero, S. Lloyd, M. Henman, and D. Coleman. 1997. Widespread geographic distribution of oral Candida dubliniensis strains in human immunodeficiency virus-infected individuals. J. Clin. Microbiol. 35:960-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Sweet, S. P., S. Cookson, and S. J. Challacombe. 1995. Candida albicans isolates from HIV-infected and AIDS patients exhibit enhanced adherence to epithelial cells. J. Med. Microbiol. 43:452-457. [DOI] [PubMed] [Google Scholar]
- 424.Sweet, S. P., A. N. Denbury, and S. J. Challacombe. 2001. Salivary calprotectin levels are raised in patients with oral candidiasis or Sjogren's syndrome but decreased by HIV infection. Oral Microbiol. Immunol. 16:119-123. [DOI] [PubMed] [Google Scholar]
- 425.Sweet, S. P., D. Rahman, and S. J. Challacombe. 1995. IgA subclasses in HIV disease: dichotomy between raised levels in serum and decreased secretion rates in saliva. Immunology 86:556-559. [PMC free article] [PubMed] [Google Scholar]
- 426.Taniuchi, I., M. J. Sunshine, R. Festenstein, and D. R. Littman. 2002. Evidence for distinct CD4 silencer functions at different stages of thymocyte differentiation. Mol. Cell 10:1083-1096. [DOI] [PubMed] [Google Scholar]
- 427.Tascini, C., F. Baldelli, C. Monari, C. Retini, D. Pietrella, D. Francisci, F. Bistoni, and A. Vecchiarelli. 1996. Inhibition of fungicidal activity of polymorphonuclear leukocytes from HIV-infected patients by interleukin (IL)- 4 and IL-10. AIDS 10:477-483. [DOI] [PubMed] [Google Scholar]
- 428.Tavitian, A., J. P. Raufman, and L. E. Rosenthal. 1986. Oral candidiasis as a marker for esophageal candidiasis in the acquired immunodeficiency syndrome. Ann. Intern. Med. 104:54-55. [DOI] [PubMed] [Google Scholar]
- 429.Telenti, A., and R. G. Paolo. 2000. Limits to potent antiretroviral therapy. Rev. Med. Virol. 10:385-393. [DOI] [PubMed] [Google Scholar]
- 430.Tenner-Racz, K., and P. Racz. 1995. Follicular dendritic cells initiate and maintain infection of the germinal centers by human immunodeficiency virus. Curr. Top. Microbiol. Immunol. 201:141-159. [DOI] [PubMed] [Google Scholar]
- 431.Tenner-Racz, K., P. Racz, M. Bofill, A. Schulz-Meyer, M. Dietrich, P. Kern, J. Weber, A. J. Pinching, F. Veronese-Dimarzo, M. Popovic, et al.1986. HTLV-III/LAV viral antigens in lymph nodes of homosexual men with persistent generalized lymphadenopathy and AIDS. Am. J. Pathol. 123:9-15. [PMC free article] [PubMed] [Google Scholar]
- 432.Teunissen, M. B., C. W. Koomen, M. R. de Waal, E. A. Wierenga, and J. D. Bos. 1998. Interleukin-17 and interferon-gamma synergize in the enhancement of proinflammatory cytokine production by human keratinocytes. J. Investig. Dermatol. 111:645-649. [DOI] [PubMed] [Google Scholar]
- 433.Teunissen, M. B., H. A. Rongen, and J. D. Bos. 1994. Function of adhesion molecules lymphocyte function-associated antigen-3 and intercellular adhesion molecule-1 on human epidermal Langerhans cells in antigen-specific T cell activation. J. Immunol. 152:3400-3409. [PubMed] [Google Scholar]
- 434.Tinkle, B. T., H. Ueda, L. Ngo, P. A. Luciw, K. Shaw, C. A. Rosen, and G. Jay. 1997. Transgenic dissection of HIV genes involved in lymphoid depletion. J. Clin. Investig. 100:32-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Tohyama, M., Y. Shirakara, K. Yamasaki, K. Sayama, and K. Hashimoto. 2001. Differentiated keratinocytes are responsible for TNF-alpha regulated production of macrophage inflammatory protein 3alpha/CCL20, a potent chemokine for Langerhans cells. J. Dermatol. Sci. 27:130-139. [DOI] [PubMed] [Google Scholar]
- 436.Tomee, J. F., P. S. Hiemstra, R. Heinzel-Wieland, and H. F. Kauffman. 1997. Antileukoprotease: an endogenous protein in the innate mucosal defense against fungi. J. Infect. Dis. 176:740-747. [DOI] [PubMed] [Google Scholar]
- 437.Tsai, H., and L. A. Bobek. 1998. Human salivary histatins: promising anti- fungal therapeutic agents. Crit Rev. Oral Biol. Med. 9:480-497. [DOI] [PubMed] [Google Scholar]
- 438.Tumbarello, M., E. Tacconelli, D. K. de Gaetano, G. Morace, G. Fadda, and R. Cauda. 1999. Candidemia in HIV-infected subjects. Eur. J. Clin. Microbiol. Infect. Dis. 18:478-483. [DOI] [PubMed] [Google Scholar]
- 439.Tylenda, C. A., J. Larsen, C. K. Yeh, H. C. Lane, and P. C. Fox. 1989. High levels of oral yeasts in early HIV-1 infection. J. Oral Pathol. Med. 18:520-524. [DOI] [PubMed] [Google Scholar]
- 440.Uchi, H., H. Terao, T. Koga, and M. Furue. 2000. Cytokines and chemokines in the epidermis. J. Dermatol. Sci. 24(Suppl. 1):S29-S38. [DOI] [PubMed] [Google Scholar]
- 441.Van Dyke, R. B., S. Lee, G. M. Johnson, A. Wiznia, K. Mohan, K. Stanley, E. V. Morse, P. A. Krogstad, and S. Nachman. 2002. Reported adherence as a determinant of response to highly active antiretroviral therapy in children who have human immunodeficiency virus infection. Pediatrics 109:61. [DOI] [PubMed] [Google Scholar]
- 442.van Loon, L. A., S. R. Krieg, C. L. Davidson, and J. D. Bos. 1989. Quantification and distribution of lymphocyte subsets and Langerhans cells in normal human oral mucosa and skin. J. Oral Pathol. Med. 18:197-201. [DOI] [PubMed] [Google Scholar]
- 443.Van Wijngaerden, E., S. De, V, G. De, V, A. M. Vandamme, K. Van Vaerenbergh, H. Bobbaers, A. Deschamps, H. Ceunen, and S. De Geest. 2002. Nonadherence to highly active antiretroviral therapy: clinically relevant patient categorization based on electronic event monitoring. AIDS Res. Hum. Retroviruses 18:327-330. [DOI] [PubMed] [Google Scholar]
- 444.Vargas, K., S. A. Messer, M. Pfaller, S. R. Lockhart, J. T. Stapleton, J. Hellstein, and D. R. Soll. 2000. Elevated phenotypic switching and drug resistance of Candida albicans from human immunodeficiency virus-positive individuals prior to first thrush episode. J. Clin. Microbiol. 38:3595-3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Vargas, K. G., and S. Joly. 2002. Carriage frequency, intensity of carriage, and strains of oral yeast species vary in the progression to oral candidiasis in human immunodeficiency virus-positive individuals. J. Clin. Microbiol. 40:341-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Vazquez-Torres, A., and E. Balish. 1997. Macrophages in resistance to candidiasis. Microbiol. Mol. Biol. Rev. 61:170-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Vudhichamnong, K., D. M. Walker, and H. C. Ryley. 1982. The effect of secretory immunoglobulin A on the in-vitro adherence of the yeast Candida albicans to human oral epithelial cells. Arch. Oral Biol. 27:617-621. [DOI] [PubMed] [Google Scholar]
- 448.Wagner, D. K., and P. G. Sohnle. 1995. Cutaneous defenses against dermatophytes and yeasts. Clin. Microbiol. Rev. 8:317-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Wagner, R. D., A. Vazquez-Torres, J. Jones-Carson, T. Warner, and E. Balish. 1996. B cell knockout mice are resistant to mucosal and systemic candidiasis of endogenous origin but susceptible to experimental systemic candidiasis. J. Infect. Dis. 174:589-597. [DOI] [PubMed] [Google Scholar]
- 450.Walsh, T. J., C. E. Gonzalez, S. Piscitelli, J. D. Bacher, J. Peter, R. Torres, D. Shetti, V. Katsov, K. Kligys, and C. A. Lyman. 2000. Correlation between in vitro and in vivo antifungal activities in experimental fluconazole-resistant oropharyngeal and esophageal candidiasis. J. Clin. Microbiol. 38:2369-2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Walsh, T. J., and W. G. Merz. 1986. Pathologic features in the human alimentary tract associated with invasiveness of Candida tropicalis. Am. J. Clin. Pathol. 85:498-502. [DOI] [PubMed] [Google Scholar]
- 452.Ward, P. P., S. Uribe-Luna, and O. M. Conneely. 2002. Lactoferrin and host defense. Biochem. Cell Biol. 80:95-102. [DOI] [PubMed] [Google Scholar]
- 453.Weinberg, A., S. Krisanaprakornkit, and B. A. Dale. 1998. Epithelial antimicrobial peptides: review and significance for oral applications. Crit. Rev. Oral Biol. Med. 9:399-414. [DOI] [PubMed] [Google Scholar]
- 454.Wenisch, C., B. Parschalk, K. Zedwitz-Liebenstein, W. Graninger, and A. Rieger. 1996. Dysregulation of the polymorphonuclear leukocyte-Candida spp. interaction in HIV-positive patients. AIDS 10:983-987. [DOI] [PubMed] [Google Scholar]
- 455.Wertz, P. W., and C. A. Squier. 1991. Cellular and molecular basis of barrier function in oral epithelium. Crit. Rev. Ther. Drug Carrier Syst. 8:237-269. [PubMed] [Google Scholar]
- 456.White, T., G. A. Kohler, S. H. Miyasaki, and N. Agabian. 1995. Expression of virulence factors in Candida albicans. Can. J. Bot. 73:1058-1064. [Google Scholar]
- 457.Wingens, M., B. H. van Bergen, P. S. Hiemstra, J. F. Meis, I. M. Vlijmen-Willems, P. L. Zeeuwen, J. Mulder, H. A. Kramps, F. van Ruissen, and J. Schalkwijk. 1998. Induction of SLPI (ALP/HUSI-I) in epidermal keratinocytes. J. Investig. Dermatol. 111:996-1002. [DOI] [PubMed] [Google Scholar]
- 458.Winzler, C., P. Rovere, M. Rescigno, F. Granucci, G. Penna, L. Adorini, V. S. Zimmermann, J. Davoust, and P. Ricciardi-Castagnoli. 1997. Maturation stages of mouse dendritic cells in growth factor-dependent long- term cultures. J. Exp. Med. 185:317-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Wira, C. R., and R. M. Rossoll. 1995. Antigen-presenting cells in the female reproductive tract: influence of the estrous cycle on antigen presentation by uterine epithelial and stromal cells. Endocrinology 136:4526-4534. [DOI] [PubMed] [Google Scholar]
- 460.Wood, G. S., N. L. Warner, and R. A. Warnke. 1983. Anti-Leu-3/T4 antibodies react with cells of monocyte/macrophage and Langerhans lineage. J. Immunol. 131:212-216. [PubMed] [Google Scholar]
- 461.Wozniak, K. L., J. E. Leigh, S. Hager, R. K. Swoboda, and P. L. Fidel, Jr. 2002. A comprehensive study of Candida-specific antibodies in the saliva of human immunodeficiency virus-positive individuals with oropharyngeal candidiasis. J. Infect. Dis. 185:1269-1276. [DOI] [PubMed] [Google Scholar]
- 462.Wu, T., L. P. Samaranayake, B. Y. Cao, and J. Wang. 1996. In-vitro proteinase production by oral Candida albicans isolates from individuals with and without HIV infection and its attenuation by antimycotic agents. J. Med. Microbiol. 44:311-316. [DOI] [PubMed] [Google Scholar]
- 463.Xu, J., T. M. Foy, J. D. Laman, E. A. Elliott, J. J. Dunn, T. J. Waldschmidt, J. Elsemore, R. J. Noelle, and R. A. Flavell. 1994. Mice deficient for the CD40 ligand. Immunity 1:423-431. [DOI] [PubMed] [Google Scholar]
- 464.Yang, D., O. Chertov, S. N. Bykovskaia, Q. Chen, M. J. Buffo, J. Shogan, M. Anderson, J. M. Schroder, J. M. Wang, O. M. Howard, and J. J. Oppenheim. 1999. Beta-defensins: linking innate and adaptive immunity through dendritic and T cell CCR6. Science 86:525-528. [DOI] [PubMed] [Google Scholar]
- 465.Yang, D., O. Chertov, and J. J. Oppenheim. 2001. Participation of mammalian defensins and cathelicidins in anti-microbial immunity: receptors and activities of human defensins and cathelicidin (LL-37). J. Leukoc. Biol. 69:691-697. [PubMed] [Google Scholar]
- 466.Yeh, C. K., M. W. Dodds, P. Zuo, and D. A. Johnson. 1997. A population- based study of salivary lysozyme concentrations and candidal counts. Arch. Oral Biol. 42:25-31. [DOI] [PubMed] [Google Scholar]
- 467.Yeh, C. K., P. C. Fox, J. A. Ship, K. A. Busch, D. K. Bermudez, A. M. Wilder, R. W. Katz, A. Wolff, C. A. Tylenda, and J. C. Atkinson. 1988. Oral defense mechanisms are impaired early in HIV-1 infected patients. J. Acquir. Immune. Defic. Syndr. 1:361-366. [PubMed] [Google Scholar]
- 468.Zhang, Y., A. Harada, J. B. Wang, Y. Y. Zhang, S. Hashimoto, M. Naito, and K. Matsushima. 1998. Bifurcated dendritic cell differentiation in vitro from murine lineage phenotype-negative c-Kit+ bone marrow hematopoietic progenitor cells. Blood 92:118-128. [PubMed] [Google Scholar]
- 469.Zhang, Y., Y. Y. Zhang, M. Ogata, P. Chen, A. Harada, S. Hashimoto, and K. Matsushima. 1999. Transforming growth factor-β1 polarizes murine hematopoietic progenitor cells to generate Langerhans cell-like dendritic cells through a monocyte/macrophage differentiation pathway. Blood 93:1208-1220. [PubMed] [Google Scholar]
- 470.Zingman, B. S. 1996. Resolution of refractory AIDS-related mucosal candidiasis after initiation of didanosine plus saquinavir. N. Engl. J. Med. 334:1674-1675. [DOI] [PubMed] [Google Scholar]
- 471.Zon, L. I., C. Arkin, and J. E. Groopman. 1987. Haematologic manifestations of the human immune deficiency virus (HIV). Br. J. Haematol. 66:251-256. [DOI] [PubMed] [Google Scholar]