Abstract
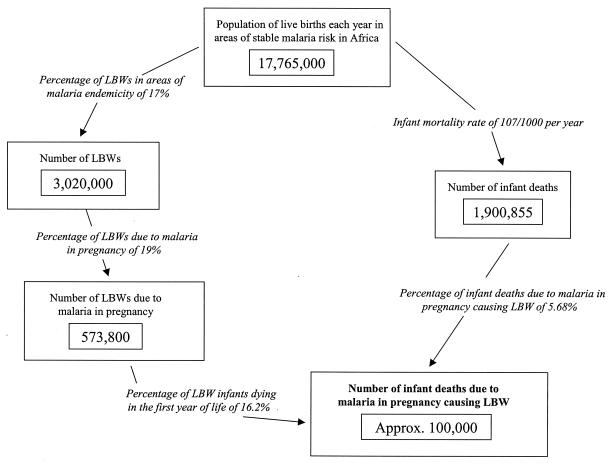
Malaria during pregnancy can result in low birth weight (LBW), an important risk factor for infant mortality. This article reviews the pathological effects of malaria during pregnancy and the implications for the newborn's development and survival. Empirical data from throughout Africa on associations between placental malaria and birth weight outcome, birth weight outcome and infant mortality, and the rates of LBW in areas with various levels of malaria transmission are evaluated to assess the increased risks of LBW and infant mortality associated with malaria. It is estimated that in areas where malaria is endemic, around 19% of infant LBWs are due to malaria and 6% of infant deaths are due to LBW caused by malaria. These estimates imply that around 100,000 infant deaths each year could be due to LBW caused by malaria during pregnancy in areas of malaria endemicity in Africa.
INTRODUCTION
It is estimated that each year over 30 million women become pregnant in malarious areas of Africa, with most living in areas of stable malaria transmission (92). Although the vast majority of women with malaria infections during pregnancy remain asymptomatic, infection increases the risk of maternal anemia and delivering a low-birth-weight (LBW) baby. LBW (<2,500 g) is an important risk factor for infant mortality, and this review focuses on the impact of malaria during pregnancy on LBW and subsequent infant mortality in sub-Saharan Africa.
There have been many papers describing the impact of malaria during pregnancy (11) and, more recently, attempts to quantify this burden (79). However, there remains a poor understanding of the effects under different levels of transmission and in different gravidity groups. It is frequently reported that primigravidae and secundigravidae are the most at risk (11), and much of the literature on the burden of malaria during pregnancy has focused on women of these gravidities. However, there is an increasing recognition that women of higher gravidities may also be at risk, particularly in areas of high transmission levels (83). The aim of this review was to investigate the impact of malaria during pregnancy on low birth weight (LBW) across all gravidities by collating data from areas in sub-Saharan Africa with various levels of malaria transmission. The present review benefits from a wealth of recently published data on malaria and LBW for all pregnant women in these areas and undertakes a novel analysis of the associations between LBW and rate of malaria transmission. A similar analysis of maternal anemia has been conducted previously (25).
PATHOPHYSIOLOGICAL PROCESS
Most malaria infections, and the most severe morbidity and mortality, are caused by Plasmodium falciparum. Most P. falciparum infections occur in sub-Saharan Africa, and the P. falciparum parasite has been shown to be more common in pregnant than nonpregnant women and to have a substantial adverse effect on pregnancy outcome (causing both prematurity [gestation of <37 weeks] and intrauterine growth retardation [IUGR]). Erythrocytes infected with P. falciparum congregate in the maternal placental vascular space, where the parasites replicate. Malaria-infected placentas are frequently observed to carry antibodies, cytokines, and macrophages, which are indicative of an active immune response (35). This immune response may stimulate early labor, though the precise effect of malaria-parasitized placentas on prematurity is not clear.
The IUGR effect appears to relate to nutrient transport to the fetus. First, a high density of parasites and chronic parasite infection in the placental blood and the associated cellular immune response may result in consumption of glucose and oxygen that would have gone to the fetus. Second, histopathological studies of infected placentas have found thickening of the cytotrophoblastic membranes, which may interfere with nutrient transport (35). However, the details of these biological processes remain uncertain given that they can be studied only after the placenta has been delivered. Malaria-associated maternal anemia may also contribute independently to IUGR (35, 89), most likely through a reduction in oxygen transport to the fetus.
Until recently, the mechanism through which parasite sequestration occurs in the placenta has been unclear. However, recent studies in Kenya and Malawi have identified certain parasite strains that are found at an increased frequency in pregnant women and have suggested that these strains may be selected for due to their ability to adhere to chondroitin sulfate A on the syncytiotrophoblast (21, 43, 63).
The observations described above relate to malaria contracted during pregnancy among women residing in areas of stable malaria transmission. The adverse effects in unstable areas may be quite different, with the effects of severe malaria, such as febrile episodes and stillbirths, becoming more apparent (55).
RISKS FOR THE LBW BABY
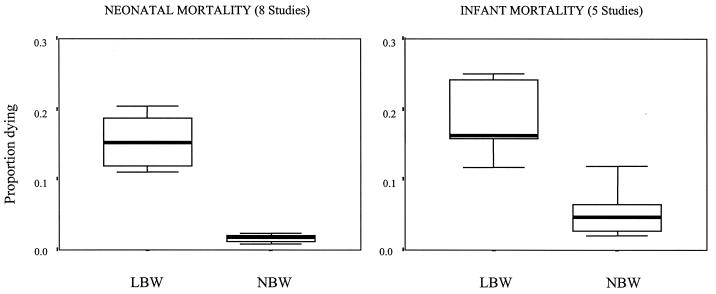
LBW is the single greatest risk factor for neonatal and infant mortality (45). Although most of the evidence arises from studies in the developed world, a recent analysis of cross-sectional data on birth weight and survival from five sites in sub-Saharan Africa showed that infant mortality is three times higher for LBW babies than for those of normal weight (Fig. 1) (26). The effects on neonatal mortality are even more marked, with a LBW baby being nine times more likely to die in the first month of life than a normal-weight baby. The risks for mortality increase steadily as the birth weight decreases to below the LBW threshold, though the data are limited. The best example is from Malawi, where the infant death rate per 1,000 live births was 650 for babies with birth weights of less than 1,500 g, 276 for babies with birth weights of 1,500 to 1,999 g, 58 for babies with birth weights of 2,000 to 2,499 g, and 24 for babies with normal birth weights (>2,499 g) (41).
FIG. 1.
Proportions of LBW and normal birth weight (NBW) babies dying in the first month and the first year of life in sub-Saharan Africa. Thick lines represent the medians, boxes represent the interquartile ranges, and I bars represent the ranges of data points. (Reprinted from reference 26 with permission of the publisher.)
LBW can be due to prematurity or IUGR. Identifying LBW cases caused by prematurity can be difficult, as many African women are not certain of their gestational age; as a result, very few studies report separately data on LBWs for preterm infants and those for infants with IUGR. It was previously thought that malaria mostly affects IUGR (11), though recent work has shown malaria to also be important in prematurity (47, 57). This finding has important implications for the impact on mortality, as preterm infants with LBW have been shown to be at a higher risk of dying than those with IUGR, at least in developed countries (34).
LBW is also a well-documented risk factor for poor neurosensory, cognitive, and behavioral development, as well as for limited school performance and academic achievement (46, 81, 82). Most of the studies concerned with these factors have been conducted in developed countries, and many have focused on very LBW (usually less than 1,001 g). However, the most vulnerable group appears to be those infants born prematurely, who will be two to four times more likely to experience failure in school than infants of normal birth weight and will need specialist support or educational services (27).
IMPORTANCE OF GRAVIDITY
Most studies find primigravidae to have a higher prevalence of P. falciparum infection than women of higher gravidities and to be at higher risk of adverse outcomes. Sera from multigravid women in their third or later pregnancy, but not sera from primigravidae, can often agglutinate parasites from the placenta, suggesting that exposure to these isolates does not occur prior to pregnancy but that variant-specific immune responses develop following exposure during pregnancy (5). The risk of placental malaria and its associated morbidity with gravidity have been exploited in the development of a birth weight nomogram (12), where malarious areas and zones of malaria transmission are based on odds ratios for an excess of LBW infants for primigravidae compared with those for multigravidae. Any outliers, i.e., sites with a low odds ratio resulting from a high risk of LBW infants for multigravidae, are assumed to occur because those residing in low transmission areas have not acquired significant antimalarial immunity or because they are exposed to a high risk of human immunodeficiency virus (HIV) (12).
Although a Cochrane meta-analysis of randomized controlled trials suggested that the benefit of preventing malaria during pregnancy is limited to primigravidae (24), a recent analysis of the approach used in that analysis suggests that this conclusion may have been incorrect (28). Other intervention studies not included in the Cochrane review have shown benefits in women of all gravidities (11, 61, 87), with protective efficacies of around 50%. There would be obvious operational problems of limiting treatment to primigravidae only, with the added concern that all women infected with HIV would benefit from treatment (83).
PLACENTAL MALARIA AND LBW
Although maternal parasitemias have been used routinely to detect malaria during pregnancy, it is recognized that peripheral parasitemias may remain below the levels of microscopic detection while parasites are harbored by the placenta (68). Histological examination of the placenta is the most sensitive indicator of maternal infection (68). Examination can show signs of active infection (presence of infected erythrocytes in the intervillous space), past or chronic infection (malarial pigment), or both.
Cross-sectional data on the associations between placental malaria infection and birth weight outcome have been collected for all gravidity groups since the late 1940s. A previous analysis showed that a baby is twice as likely to be born with a LBW if the mother has an infected placenta at delivery (26). This finding held true both for primigravidae only and for all gravidities. It was based on data from 14 studies from five countries dating from 1948 to 1998, with four of the studies excluding preterm births. Since this analysis, a number of new studies have been published; Table 1 summarizes the associations found between placental malaria and LBW in studies conducted since 1980 of random samples of births (preterm and full-term) from facilities in areas of stable malaria transmission. Data from intervention trials (14, 15, 77) and from areas of unstable malaria transmission (17, 55) were excluded. Studies that assessed infection only through maternal peripheral smears (65, 80) or did not differentiate between peripheral and placental infection (8) were also excluded. Remaining were 4 studies for primigravidae and 11 studies for all gravidities (Table 1).
TABLE 1.
Increased risk of LBW associated with placental infection in stable transmission areasa
| Parity group or aggregate studied | Prevalence of placental malaria (%) | Study area | Study author(s) (reference)b | Sample size (infected/uninfected) | Prevalence of LBW (<2,500 g) (%)
|
Prc | Infected attributable fraction (%) | Population-attributable fraction (%) | |
|---|---|---|---|---|---|---|---|---|---|
| With placental malaria | Without placental malaria | ||||||||
| Primigravidae | 26 | Freetown, Sierra Leone | Morgan (51) | 36/104 | 39 | 18 | 2.12 | 53 | 22 |
| 26 | Mombasa, Kenya | M. Parise (pers. comm.) | 23/63 | 48 | 29 | 1.67 | 40 | 35 | |
| 34 | Kisumu, Kenya | M. Parise (pers. comm.) | 58/113 | 35 | 19 | 1.86 | 46 | 22 | |
| 63 | Kilifi, Kenya | Shulman et al. (69) | 153/90 | 29 | 16 | 1.84 | 46 | 35 | |
| Median (lower to upper quartiles) | 30 (25-41) | 1.85 (1.80-1.92) | 46 (44-48) | 22 (21-26) | |||||
| All gravidities | 5 | Gambella, Ethiopia | Newman et al. (55) | 9/159 | 44 | 14 | 3.21 | 69 | 11 |
| 18 | Freetown, Sierra Leone | Morgan (51) | 142/626 | 22 | 10 | 2.35 | 58 | 20 | |
| 19 | Mombasa, Kenya | M. Parise (pers. comm.) | 41/174 | 42 | 20 | 2.06 | 51 | 17 | |
| 23 | Kisumu, Kenya | M. Parise (pers. comm.) | 107/352 | 28 | 16 | 1.79 | 44 | 16 | |
| 23 | Koupela, Burkino Faso | Sirima et al. (70) | 179/608 | 21 | 12 | 1.67 | 40 | 13 | |
| 26 | Lowlands, Madagascar | Cot et al. (17) | 90/260 | 27 | 14 | 1.92 | 48 | 19 | |
| 26 | Blantyre, Malawi | Rogerson et al. (64) | 252/705 | 24 | 11 | 2.19 | 54 | 24 | |
| 45 | Benin City, Nigeria | Ibhanesebhor and Okolo (33) | 141/171 | 26 | 22 | 1.21 | 18 | 9 | |
| 48 | Kilifi, Kenya | Shulman et al. (69) | 392/423 | 23 | 13 | 1.73 | 42 | 26 | |
| 51 | Bansang, Gambia | Okoko et al. (57) | 160/153 | 38 | 14 | 2.46 | 59 | 43 | |
| 52 | Rutshuru, Zaire | Meuris et al. (48) | 242/219 | 20 | 10 | 2.11 | 53 | 36 | |
| Median (lower to upper quartiles) | 26 (21-47) | 2.06 (1.76-2.27) | 51 (43-56) | 19 (14-25) | |||||
Studies conducted since 1980 of random samples of births (preterm and full-term) from facilities in areas of stable malaria transmission. Data from intervention trials, areas of unstable malaria transmission, and studies that assessed infection only through maternal peripheral smears or did not differentiate between peripheral and placental infection were excluded.
pers. comm., personal communication.
The prevalence ratio (Pr) is the proportion of infected women with LBW divided by the proportion of uninfected women with LBW. The infected attributable fraction is the percentage of infected women with LBW that is due to malaria [(Pr − 1/)Pr]. The population-attributable fraction is the percentage of LBW cases that are due to malaria infection; [S(Pr − 1)]/{1 + [S(Pr − 1)]} where S is the proportion with placental malaria infection.
Despite the prevalence of placental infections for women of all gravidities, ranging from 5 to 52%, the risk of LBW associated with infection was relatively consistent, with babies born to mothers with an infected placenta being twice as likely to be of LBW than those born to mothers with an uninfected placenta (median prevalence ratio, 2.06) (Table 1). The prevalence ratio appears to be unaffected by the prevalence of placental malaria, and therefore for purposes of attributable fraction analysis the median value is used. This value suggests that approximately half of the LBW cases among those infected with placental malaria are due to malaria (the infected attributable fraction). Given a median prevalence of placental malaria of 26%, the population-attributable fraction (the percentage of all LBW cases due to malaria) is estimated to be 19% (Table 1). In other words, one-fifth of the LBWs of babies born to mothers in areas where malaria is endemic are due to malarial infection of the placenta while the mother is pregnant. This compares to previous estimates of between 8 and 14% (79).
PARASITE RATE AND LBW
Although the prevalence of placental malaria infection may provide an indication of the risk of malaria transmission, a more widely used marker of malaria endemicity is the prevalence of P. falciparum infection in a given childhood population (73). This is often termed the parasite rate, and this information is available for many sites throughout sub-Saharan Africa, often from research projects undertaking community-based surveys. Independent of this information are data on the prevalence of LBW, which are often routinely collected at hospitals. The purpose of this section is to combine these independently collected data on LBWs and parasite rates for sites across the African continent.
LBW Data
A literature search was undertaken for birth weight data in sub-Saharan Africa by using MEDLINE and CAB HEALTH databases with “birthweight” and “Africa” as the search keywords. The major tropical journals were also checked for possible data sources by manual searches of issues with predigital dates. The bibliographies of all papers collected were checked for additional references. Studies were included in the analysis only if they were undertaken post-1980, as for previous burden estimates (75), and did not exclude preterm births from those sampled. Since 1976, LBW was universally classified as <2,500 g (91). However, the denominator may be variously defined. It may incorporate all births or be selected based on whether the baby is a singleton, a live birth, or full term. It has been well established that the choice of denominator can widely affect the LBW value, since twins, stillbirths, and preterm births are invariably of a lower birth weight. One study from Tanzania recorded a 17% rate of LBW for all births, a 14% rate for singletons only, and an 11% rate for live singletons only (90). For collation of LBW data for the present analysis, only data for live singletons were selected when that option was available. However, in order to be inclusive rather than exclusive, we also accepted data from eight studies that explicitly included twins and five that explicitly included stillbirths. Unpublished data for nine sites in Kenya were also included (R. Snow, personal communication).
Parasite Prevalence Data
The parasite rate has been widely used as a marker of malaria endemicity (73). Although a more reliable measure of infection risk is the entomological inoculation rate, estimates of this rate are rare across Africa (29) and the methods used often vary between studies (23). Independent data searches were used to locate time- and location-specific estimates of parasite rates for geographical areas covered by the LBW survey.
The parasite rate is simply the prevalence of P. falciparum infection in a given childhood population. Cross-sectional surveys of parasite prevalence since 1980 were included if at least 50 randomly selected children between 0 and 4 years of age or, if that sample was not available, between 0 to 15 years of age, were examined, as in previous global mortality and morbidity analyses (75). The first search for data was of the published literature or by correspondence with the authors of the LBW studies. The second search used two main sources: the thesis of J. A. Omumbo (58) for Kenya, Uganda, and Tanzania and the MARA/ARMA database (Mapping Malaria Risk in Africa/Atlas du Risque de la Malaria en Afrique, July 2002 [http://www.mara.org.za].) for the African countries.
Analysis and Main Findings
Table 2 summarizes the LBW data that were matched with a parasite rate. Overall, data from 44 LBW studies (25 for primigravidae only), representing parasite rates from 0 to 90%, were included. Recent data from the control arm of a bed net trial (83) was excluded because the authors suspected that the prevalence of LBWs in the control arm might also have decreased as the result of the mass killing of mosquitoes in the study villages.
TABLE 2.
LBWs and parasite rates for sub-Saharan Africa
| Study area | Study author(s) (reference)a | Yr(s) of survey | % LBW infants (sample size)b
|
PRc | PR source (reference) | ||
|---|---|---|---|---|---|---|---|
| All parities | Primigravidae | Multigravidae | |||||
| Addis Ababa, Ethiopia | Feleke and Enquoselassic (19) | 1996-1997 | 9.1 (4,010) | 12 (1,767) | 6.6 (2,200) | 0 | MARA/ARMA |
| Mantsonyane, Lesotho | Brabin et al. (12) | 1980-1983 | 7.5 (828) | 9.3 (259) | 6.7 (569) | 0 | Brabin et al. (12) |
| Cape Town, South Africa | Rip et al. (62) | 1982 | 12 (36,789) | NA | NA | 0 | MARA/ARMA |
| Gweru, Zimbabwe | De Muylder (18) | 1982-1984 | 18.5 (4,850) | NA | NA | 1.2 | Freeman (20) |
| Kabale, Uganda | Ndyomugyenyi and Magnussen (54) | 1997-1998 | 5.2 (2,582) | 5.6 (1,106) | 4.9 (1,476) | 1.4 | MARA/ARMA |
| Kerugoya, Kenya | R. Snow (pers. comm.) | 1996 | 8.3 (3,976) | 11 (1,478) | 6.8 (2,498) | 2.0 | Omumbo (58) |
| Highlands, Madagascar | Cot et al. (17) | 1996-1997 | 9.7 (1,255) | NA | NA | 4.2 | Cot et al. (16) |
| Hai, Tanzania | Basheke and Wandema (4) | 1988-1991 | 6.2 (1,402) | NA | NA | 4.2 | Basheke (4) |
| Midlands Province, Zimbabwe | Brabin et al. (12) | 1995 | 13 (241) | 16 (104) | 11 (137) | 7.9 | Freeman (20) |
| Accra, Ghana | Klufio et al. (40) | 1994 | 13 (866) | NA | NA | 12 | MARA/ARMA |
| Ilula, Tanzania | Moller et al. (50) | 1983-1986 | 13 (625) | NA | NA | 12 | Omumbo (58) |
| Gucha, Kenya | R. Snow (pers. comm.) | 1998-2000 | 16 (3,319) | NA | NA | 15 | Omumbo (58) |
| Bobo-Dioulasso, Burkina Faso | Mbacke and van de Walle (44) | 1981-1984 | 14 (6,091) | NA | NA | 15 | Gazin et al. (22) |
| Gambella, Ethiopia | Newman et al. (55) | 2000-2001 | 16 (168) | 21 (58) | 13 (110) | 25 | Bentiee |
| Dar-es-Salaam, Tanzania | Kazimoto (39) | 1981 | 15 (6,774) | NA | NA | 28 | Yamagata (93) |
| Niamey, Niger | Mock et al. (49) | 1980-1985 | 11 (5,097) | 18 (885) | 10 (4,177) | 30 | Julvez et al. (37) |
| Kitui, Kenya | Odala and Oheno (56) | 1987 | 20 (8,744) | NA | NA | 31 | Omumbo (58) |
| Ndala, Tanzania | Bantje (3) | 1980-1984 | 11 (4,589) | NA | NA | 31 | Omumbo (58) |
| Makueni, Kenya | R. Snow (pers. comm.) | 1996 | 12 (764) | 13 (272) | 11 (492) | 33 | Omumbo (58) |
| Makindye, Uganda | Kasumba et al. (38) | 1998 | 9 (537) | 16 (202) | 6.8 (383) | 36 | Omumbo (58) |
| Maputo, Mozambique | Bergstrom et al. (8) | 1985 | 17 (202) | NA | NA | 38 | Schapira and Da Costa (66) |
| Banfora, Burkino Faso | Cot et al. (14) | 1987-1988 | 16 (554) | NA | NA | 41 | MARA/ARMA |
| Mombasa, Kenya | Parise et al. (60) | 1996 | 25 (216) | 34 (86) | 18 (130) | 41 | Omumbo (58) |
| Kakamega, Kenya | R. Snow (pers. comm.) | 1997 | 14 (3,024) | 22 (1,158) | 8.9 (1,866) | 42 | MARA/ARMA |
| Blantyre, Malawi | Brabin et al. (12) | 1997-1999 | 15 (924) | NA | NA | 46 | Holtz et al. (32) |
| Kapsabet, Kenya | R. Snow (pers. comm.) | 1996 | 17 (1,635) | 18 (510) | 17 (1,125) | 47 | Omumbo (58) |
| Kisumu, Kenya | Parise et al. (60) | 1996 | 18 (467) | 23 (177)d | 15 (290)d | 48 | Omumbo (58) |
| Kilifi, Kenya | Shulman et al. (69) | 1996-1997 | 18 (820) | 24 (246) | 15 (574) | 49 | Snow et al. (72) |
| Lowland, Madagascar | Cot et al. (17) | 1996-1997 | 17 (354) | NA | NA | 49 | Cot et al. (16) |
| Homa Bay, Kenya | R. Snow (pers. comm.) | 1996 | 14 (2,189) | 19 (706) | 11 (1,483) | 49 | Omumbo (58) |
| Mwanza, Tanzania | Walraven et al. (90) | 1989-1990 | 11 (2,719) | NA | NA | 50 | Omumbo (58) |
| Msambweni, Kenya | R. Snow (pers. comm.) | 1996 | 21 (1,116) | 25 (501) | 17 (615) | 50 | Omumbo (58) |
| Mangochi, Malawi | Steketee et al. (77) | 1987-1990 | 17 (1,766) | 28 (602) | 11 (1,164) | 51 | Mangochi Malaria Research Project (41) |
| Bondo, Kenya | R. Snow (pers. comm.) | 1998-2000 | 16 (1,387) | NA | NA | 52 | Omumbo (58) |
| Kinshasa, Zaire | Steketee et al. (76) | 1985 | 12 (1,116) | 19 (290) | 9 (825) | 52 | Mulumba et al. (52) |
| Cotonou, Benin | Alihonou et al. (2) | 1987 | 19 (1,007) | NA | NA | 58 | Akogbeto et al. (1) |
| Bougoula, Mali | Bouvier et al. (10) | 1992 | 16 (146) | 40 (30)d | 10 (116)d | 62 | Traore (84) |
| Ashanti, Ghana | Brabin et al. (12) | 1995-1996 | 18 (9,001) | 26 (2,881) | 15 (6,120) | 65 | MARA/ARMA |
| Ebolowa, Cameroon | Salihu et al. (65) | 1997-1998 | 20 (232) | 21 (66) | 21 (156) | 65 | MARA/ARMA |
| Hoima, Uganda | Ndyomugyenyi and Magnussen (54) | 1997-1998 | 14 (3,147) | 17 (1,254) | 12 (1,893) | 67 | MARA/ARMA |
| Busia, Kenya | R. Snow (pers. comm.) | 1996 | 11 (3,147) | 16 (652) | 7.8 (1,211) | 68 | Omumbo (58) |
| Ejisu Juaben, Ghana | Brabin et al. (12) | 1995-1996 | 20 (373) | 32 (114) | 14 (2,475) | 75 | MARA/ARMA |
| Bagamoyo, Tanzania | Bantje (3) | 1982-1984 | 14 (2,475) | NA | NA | 80 | Hedman et al. (30) |
| Ifakara, Tanzania | Brabin et al. (12) | 1990-1992 | 18 (8,259) | 31 (2,173) | 13 (6,086) | 90 | Smith et al. (71) |
pers. comm., personal communication.
LBW is defined as <2,500 g. NA, not available.
Parasite rate (PR), prevalence of P. falciparum in a given childhood population.
Sample includes primigravidae and secundigravidae.
D. Bentie, Abstr. Proc. Third Cycle Local Res. Grant 1996 (http://www.telecom.net.et/∼estc/publication/proceedi.htm).
LBWs are assessed according to four broad risk categories of malaria prevalence (<25, 25 to 49, 50 to 74, and >75%) matching logarithmic increases in the entomological inoculation rate (<1, 1 to 10, 11 to 100, and >100 infective bites per adult per year) (6, 73) (Table 3). Although there is a general trend for the prevalence of LBWs to increase with increasing malaria risk, the only clear and marked difference is observed when malaria risks of greater and less than 25% are being compared. Differences in the prevalences of LBW with malaria risk at levels greater than 25% are inconclusive, partly due to the paucity of data at high malaria risk levels. Even a marked relationship may not be causal but may simply reflect the association of malaria risk and LBW with other underlying factors (such as poverty) that determine both malaria risk and LBW. However, recent data from an insecticide-treated bed net trial in Kenya has provided important evidence that a reduction in the rate of malaria transmission can reduce the prevalence of LBW, with even greater reductions expected than those observed, given the anticipated reductions in the control arm through the effects of mass killing of mosquitoes (83). The lack of a clear relationship between the independently collated data on LBW and parasite prevalence from 44 sites across Africa is not surprising given the possible variations in the parasite rate by age group and season, among other factors, and the expected heterogeneity across sites in factors which may affect LBW, such as altitude and HIV status.
TABLE 3.
Median prevalences of LBWs at different levels of malaria endemicity
| PRa | All gravidities
|
Primigravidae
|
||
|---|---|---|---|---|
| No. of studies | Prevalence of LBW (%)b | No. of studies | Prevalence of LBW (%)b | |
| <25% | 13 | 11.8 (8.32-13.3) | 5 | 11.0 (9.27-11.7) |
| 25-49% | 17 | 15.5 (13.7-17.2) | 10 | 19.8 (17.8-22.8) |
| 50-74% | 11 | 16.4 (12.7-18.9) | 8 | 19.1 (16.0-25.9) |
| >74% | 3 | 17.9 (15.8-19.1) | 2 | 31.4 (31.3-31.5) |
| All | 44 | 14.2 (11.5-17.4) | 25 | 18.4 (14.6-24.4) |
Four broad-risk categories of parasite rates (PRs) matching logarithmic increases in the entomological inoculation rate (<1, 1-10, 11-100, and >100) infective bites per adult per year (6, 73).
The median prevalences of LBW (<2,500 g) are shown; the lower- to upper-quartile ranges are in parentheses.
HIV AND MALARIA DURING PREGNANCY
The interactions between HIV and malaria during pregnancy are complex. Studies in Kenya and Malawi have shown that the prevalence and density of malaria parasites are higher in pregnant women who are also HIV positive (59, 78, 88). The risk of infants dying during the postneonatal period has also been shown to be 3.4-fold higher in children born to HIV-positive mothers with placental malaria than in those born to HIV-positive mothers without placental malaria (9). It has been demonstrated in some studies that HIV alters the patterns of malaria during pregnancy so that women of all gravidities are at the same level of risk, with the implication that prevention strategies need to be targeted to all pregnant women (86).
The current recommended preventive therapy for malaria during pregnancy is the drug sulfadoxine pyrimethamine (SP), given in two doses for intermittent preventive treatment in the second and third trimesters. However, HIV also has an impact on the efficacy of SP, and it has been suggested that at least three doses of SP may be required for HIV-positive women (59). Malaria may also worsen HIV infection, with a recent study in Blantyre, Malawi, indicating that malaria may increase the HIV load in adults (31). In addition, concerns that malaria infection of the placenta may contribute to mother-to-child HIV transmission remain (9, 13).
REDUCING INFANT MORTALITY
LBW is influenced by many factors, including genetics, multiple pregnancies, placental abnormalities, maternal nutrition, maternal age, gravidity, and history of smoking, and a range of viral, bacterial, and parasitic infections. Malaria is unique in being one of the few problems that is amenable to intervention once a woman becomes pregnant. Although the relationship between LBW and child survival has been recognized for several decades (45), surprisingly little attention has been paid to preventing LBW as a mortality reduction strategy (67). The first hurdle is to establish just how many infant deaths could be prevented. The Africa Malaria Report states that malaria during pregnancy is estimated to cause between 75,000 and 200,000 infant deaths per year (92), and other estimates (by Murphy and Breman [53]) are between 62,000 and 363,000. Using two different approaches, we estimate that around 100,000 infant deaths in areas of Africa where malaria is endemic could be due to malaria during pregnancy causing LBW (Fig. 2).
FIG. 2.
Number of infant deaths due to malaria during pregnancy in areas of stable malaria risk in sub-Saharan Africa. Population of live births refers to number of live births in areas at risk for stable endemic malaria in 2000, as estimated from maps of malaria risk and population models (74). The infant mortality rate is a summary of the rate for sub-Saharan African in 2001 (85). The percentage of infant deaths was determined by using the formula and data on mortality risks presented by Guyatt and Snow (26) with the following revised probabilities based on the new data in Table 1: 0.257 for placental malaria infection (PI), 0.262 for LBW given placental infection (qLBW; range, 0.228 to 0.309), and 0.137 for LBW given no placental infection (range, 0.117 to 0.147). It is estimated that 5.68% (range, 3.69 to 8.77%) of infant deaths are due to malaria-induced LBW. The percentage of LBW infants in areas of malaria endemicity is 17%, the median of the results of 11 studies presented in Table 1. This figure is supported by the data from 31 studies which reported a malaria risk of >25% (Table 2), with a median LBW of 16.4%. The percentage of LBW infants due to malaria during pregnancy is 19% (range, 14 to 25%), which is the population-attributable fraction from Table 1. The percentage of LBW infants dying in the first year of life is 16.2%, based on the mortality risk of 0.162 in five studies reported by Guyatt and Snow (26).
Both estimates use as their foundation the 17,765,000 live births estimated each year in areas of stable malaria risk in Africa (74). The first approach uses the model described by Guyatt and Snow (26) and revised estimates on the risks of LBW with and without placental infection, and the risks of placental infection from the data in Table 1, to determine that 5.68% (range, 3.69 to 8.77%) of infant deaths are attributable to LBW caused by malaria. Assuming that there are 1,900,855 infant deaths (from the base population of live births and an infant mortality rate of 107/1,000 births (85) (see Fig. 2) in areas of malaria endemicity in Africa suggests that 107,969 (range, 70,142 to 166,705) of the infant deaths may be attributable to malaria during pregnancy. The second estimate uses the population-attributable fraction (19% [range, 14 to 25%] of LBWs being due to malaria during pregnancy) shown in Table 1 and applies this fraction to the population of LBW infants in areas of stable malaria risk in Africa. It is estimated that 573,800 (range, 422,800 to 755,000) infants have LBWs due to malaria during pregnancy, and modifying this result with a probability of dying from a LBW in the first year of life of 0.162 (26) yields 92,956 (range, 68,494 to 122,310) infant deaths as a result of malaria-induced LBWs.
LBWs due to malaria may result from IUGR or premature delivery. In a recent review of measures for preventing child mortality, malaria during pregnancy was identified as an important factor in precipitating preterm delivery, one of the nine main causes of death in children under 5 years of age (36). Antimalarial intermittent preventive treatment during pregnancy was estimated to prevent 22,000 deaths of children under 5 years of age through reduced numbers of preterm deliveries, which is <1% of the estimated 9.7 million infant deaths each year in the 42 countries with 90% of worldwide child deaths (36). We suggest that this effective therapy would prevent many more deaths. With the effects in epidemic-prone regions and regions outside the African continent excluded and with the assumption of an efficacy rate of preventing placental malaria infection of 80% (24), the number of deaths prevented is likely to be closer to 80,000.
Acknowledgments
We thank Rose Lusinde and Judy Omumbo for help determining malaria parasite prevalences for Tanzania and Kenya, respectively.
Support was provided by the Wellcome Trust and the Kenyan Medical Research Institute. H.G. was in receipt of a Wellcome Trust Research Career Development Fellowship (055100), and R.W.S. has a Senior Research Fellowship in Basic Biomedical Science (058992).
This paper is published with the permission of the director of KEMRI.
REFERENCES
- 1.Akogbeto, M., D. Modiano, and A. Bosman. 1992. Malaria transmission in the lagoon area of Cotonou, Benin. Parassitologia 34:147-154. [PubMed] [Google Scholar]
- 2.Alihonou, E., V. Dan, B. Ayivi, E. C. Sossou, T. Gandaho, and S. Koumakpai. 1991. Mortalité néonatale au Centre National Hospitalier et Universitaire de Cotonou: incidence, causes et moyens de lutte. Med. d'Afr. Noir 38:745-751. [Google Scholar]
- 3.Bantje, H. 1987. Seasonality of births and birthweights in Tanzania. Soc. Sci. Med. 24:733-739. [DOI] [PubMed] [Google Scholar]
- 4.Basheke, M. M., and F. S. Wandema. 1989. Nutritional and health status of children in Hai District, Kilimanjaro Region: report of the baseline nutrition survey conducted during CSD campaign from September to October 1988. TFNC report 1190, p. 36. Tanzania Food and Nutrition Centre, Dar-es-Salaam, Tanzania.
- 5.Beeson, J. G., G. V. Brown, M. E. Molyneux, C. Mhango, F. Dzinjalamala, and S. J. Rogerson. 1999. Plasmodium falciparum isolates from infected pregnant women and children are each associated with distinct adhesive and antigenic properties. J. Infect. Dis. 180:465-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beier, J. C., G. F. Killeen, and J. I. Githure. 1999. Short report: entomologic inoculation rates and Plasmodium falciparum malaria prevalence in Africa. Am. J. Trop. Med. Hyg. 61:109-113. [DOI] [PubMed] [Google Scholar]
- 7.Reference deleted.
- 8.Bergstrom, S., A. Fernandes, J. Schwalbach, O. Perez, and R. Miyar. 1993. Materno-fetal transmission of pregnancy malaria: an immunoparasitological study on 202 parturients in Maputo. Gynecol. Obstet. Investig. 35:103-107. [DOI] [PubMed] [Google Scholar]
- 9.Bloland, P. B., J. J. Wirima, R. W. Steketee, B. Chilima, A. Hightower, and J. G. Breman. 1995. Maternal HIV infection and infant mortality in Malawi: evidence for increased mortality due to placental malaria infection. AIDS 9:721-726. [DOI] [PubMed] [Google Scholar]
- 10.Bouvier, P., N. Breslow, O. Doumbo, C.-F. Robert, M. Picquet, A. Mauris, A. Dolo, H. K. Dembele, V. Delley, and A. Rougemont. 1997. Seasonality, malaria and impact of prophylaxis in a West African village. II. Effect on birthweight. Am. J. Trop. Med. Hyg. 56:384-389. [DOI] [PubMed] [Google Scholar]
- 11.Brabin, B. J. 1991. The risks and severity of malaria in pregnant women. Applied field research in malaria reports no. 1. World Health Organization, Geneva, Switzerland.
- 12.Brabin, B. J., S. O. F. Agbaje, Y. Ahmed, and N. D. Briggs. 1999. A birthweight nomogram for Africa, as a malaria-control indicator. Ann. Trop. Med. Parasitol. 93:S43-S57. [PubMed] [Google Scholar]
- 13.Brahmbhatt, H., G. Kigozi, F. Wabwire-Mangen, D. Serwadda, N. Sewankambo, T. Lutalo, M. J. Wawe, C. Abramowsky, D. Sullivan, and R. Gray. 2003. The effects of placental malaria on mother-to-child HIV transmission in Rakai, Uganda. AIDS 17:2539-2541. [DOI] [PubMed] [Google Scholar]
- 14.Cot, M., A. Roisin, D. Barro, A. Yada, J. P. Verhave, P. Carnevale, and G. Breart. 1992. Report of chloroquine chemoprophylaxis during pregnancy on birth weight: result of a randomized trial. Am. J. Trop. Med. Hyg. 46:21-26. [DOI] [PubMed] [Google Scholar]
- 15.Cot, M., J. Y. Hesran, P. Miailes, M. Esveld, D. Etya'ale, and G. Breart. 1995. Increase in birth weight following chloroquine chemoprophylaxis during the first pregnancy: results of a randomized trial in Cameroon. Am. J. Trop. Med. Hyg. 53:581-585. [DOI] [PubMed] [Google Scholar]
- 16.Cot, M., L. Brutus, G. Le Goff, V. Rajaonarivelo, and A. Raveloson. 2001. The campaign against malaria in central western Madagascar: comparison of lambda-cyhalothrin and DDT house spraying. I. Parasitological and clinical study. Parasite 8:309-316. [DOI] [PubMed] [Google Scholar]
- 17.Cot, M., L. Brutus, V. Pinell, H. Ramaroson, D. Rabeson, and A. L. Rakotonjanabelo. 2002. Malaria prevention during pregnancy in unstable transmission areas: the highlands of Madagascar. Trop. Med. Int. Health 7:565-572. [DOI] [PubMed] [Google Scholar]
- 18.De Muylder, X. 1987. Maternity services in a general hospital. Part II. Perinatal data. Cent. Afr. J. Med. 33:70-74. [PubMed] [Google Scholar]
- 19.Feleke, Y., and F. Enquoselassie. 1999. Maternal age, parity and gestational age on the size of the newborn in Addis Ababa. East Afr. Med. J. 76:468-471. [PubMed] [Google Scholar]
- 20.Freeman, T. 1993. 1991 National malaria prevalence survey. Blair Research Institute, Harare, Zimbabwe.
- 21.Fried, M., and P. E. Duffy. 1996. Adherence of Plasmodium falciparum to chondroitin sulphate A in the human placenta. Science 272:1502-1504. [DOI] [PubMed] [Google Scholar]
- 22.Gazin, P., V. Robert, and P. Carnevale. 1987. Le paludisme urbain à Bobo-Dioulasso (Burkina Faso). 2. Les indices paludologiques. Cah. O. R. S. T. O. M. Sér. Entomol. Méd. Parasitol. 25:27-31. [Google Scholar]
- 23.Githeko, A. K., C. N. M. Mbogo, C. F. Curtis, J. Lines, and C. Lengeler. 1996. Entomological monitoring of large-scale vector control interventions. Parasitol. Today 12:127-128. [Google Scholar]
- 24.Gulmezoglu, A. M., and P. Garner. 1998. Malaria in pregnancy in endemic areas (Cochrane Review). The Cochrane Library, issue 2. Update Software, Liverpool, United Kingdom.
- 25.Guyatt, H. L., and R. W. Snow. 2001. The epidemiology and burden of Plasmodium falciparum-related anemia among pregnant women in sub-Saharan Africa. Am. J. Trop. Med. Hyg. 64:36-44. [DOI] [PubMed] [Google Scholar]
- 26.Guyatt, H. L., and R. W. Snow. 2001. Malaria in pregnancy as an indirect cause of infant mortality in sub-Saharan Africa. Trans. R. Soc. Trop. Med. Hyg. 95:569-576. [DOI] [PubMed] [Google Scholar]
- 27.Hack, M., N. Klein, H. G. Taylor. 1995. Long-term developmental outcomes of low-birth weight infants. Future Child 5:176-196. [PubMed] [Google Scholar]
- 28.Hahn, S., P. R. Williamson, J. L. Hutton, P. Garner, and E. V. Flynn. 2000. Assessing the potential for bias in meta-analysis due to selective reporting of subgroup analyses within studies. Stat. Med. 19:3325-3336. [DOI] [PubMed] [Google Scholar]
- 29.Hay, S. I., J. F. Toomer, D. J. Rogers, and R. W. Snow. 2000. Annual entomological inoculation rates (EIR) across Africa: literature survey, Internet access and review. Trans. R. Soc. Trop. Med. Hyg. 94:113-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hedman, P., L. Rombo, A. Björkman, J. Brohult, C. M. Kihamia, J. Potter, and J. Stenbeck. 1986. Sensitivity in vivo of Plasmodium falciparum to chloroquine and pyrimethamine/sulfadoxine in a coastal area of Tanzania. Ann. Trop. Med. Parasitol. 80:7-11. [DOI] [PubMed] [Google Scholar]
- 31.Hoffman, I. F., C. S. Jere, T. E. Taylor, P. Munthali, J. R. Dyer, J. J. Wirima, S. J. Rogerson, N. Kumwenda, J. J. Eron, S. A. Fiscus, H. Chakraborty, T. E. Taha, M. S. Cohen, and M. E. Molyneux. 1999. The effect of Plasmodium falciparum malaria on HIV-1 RNA blood plasma concentration. AIDS 13:487-494. [DOI] [PubMed] [Google Scholar]
- 32.Holtz, T. H., L. H. Marum, C. Mkandala, N. Chizani, J. M. Roberts, A. Macheso, M. E. Parise, and S. P. Kachur. 2002. Insecticide-treated bednet use, anaemia, and malaria parasitaemia in Blantyre District, Malawi. Trop. Med. Int. Health 7:220-230. [DOI] [PubMed] [Google Scholar]
- 33.Ibhanesebhor, S. E., and A. A. Okolo. 1992. Placental malaria and pregnancy outcome. Int. J. Gynaecol. Obstet. 37:247-252. [DOI] [PubMed] [Google Scholar]
- 34.Institute of Medicine. 1985. Preventing low birthweight. National Academy Press, Washington, D.C. [PubMed]
- 35.Ismail, M. R., J. Ordi, C. Menendez, P. J. Ventura, J. J. Aponte, E. Kahigwa, R. Hirt, A. Cardesa, and A. P. L. Alonso. 2000. Placental pathology in malaria: a histological, immunohistochemical, and quantitative study. Hum. Pathol. 31:85-93. [DOI] [PubMed] [Google Scholar]
- 36.Jones, G., R. W. Steketee, R. E. Black, Z. A. Bhutta, S. S. Morris, and the Bellagio Child Survival Group. 2003. How many child deaths can we prevent this year? Lancet 362:65-71. [DOI] [PubMed] [Google Scholar]
- 37.Julvez, J., J. Mouchet, A. Michault, A. Fouta, and M. Hamidine. 1997. Eco-épidemiologie du paludisme à Niamey et dans la vallée du fleuve, République du Niger, 1992-1995. Bull. Soc. Pathol. Exot. 90:94-100. [PubMed] [Google Scholar]
- 38.Kasumba, I. N., A. J. Nalunkuma, G. Mujuzi, F. S. Kitaka, R. Byaruhanga, P. Okong, and T. G. Egwang. 2000. Low birth weight associated with maternal anaemia and Plasmodium falciparum infection during pregnancy in a low endemicity peri-urban population in Uganda. Ann. Trop. Med. Parasitol. 94:7-13. [PubMed] [Google Scholar]
- 39.Kazimoto, T. P. K. 1982. Review of perinatal mortality at Muhumbili maternity block. J. Obstet. Gynecol. East Cent. Afr. 105:105-107. [Google Scholar]
- 40.Klufio, C. A., A. T. Lassey, B. D. Annan, and J. B. Wilson. 2001. Birthweight distribution at Korle-Bu teaching Hospital, Ghana. East Afr. Med. J. 78:418-423. [DOI] [PubMed] [Google Scholar]
- 41.Mangochi Malaria Research Project. 1993. Malaria prevention in pregnancy: the effects of treatment and chemoprophylaxis on placental malaria infection, low birth weight, and fetal, infant, and child survival. U.S. Agency for International Development in conjunction with Centers for Disease Control and Prevention, Atlanta, Ga.
- 42.Reference deleted.
- 43.Maubert, B., N. Fievet, G. Tami, M. Cot, C. Boudin, and P. Deloron. 1999. Development of antibodies against chondroitin sulfate A-adherent Plasmodium falciparum in pregnant women. Infect. Immun. 67:5367-5371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mbacke, C., and E. van de Walle. 1992. Socio-economic factors and use of health services as determinants of child mortality, p. 123-144. In E. van de Walle, G. Pison, and M. Sala-Diakanda (ed.), Mortality and society in sub-Saharan Africa. Clarendon Press, Oxford, United Kingdom.
- 45.McCormick, M. C. 1985. The contribution of low birth weight to infant mortality and childhood mortality. N. Engl. J. Med. 312:82-90. [DOI] [PubMed] [Google Scholar]
- 46.McCormick, M. C., J. Brooks-Gunn, K. Workman-Daniels, J. Turner, and G. J. Peckham. 1992. The health and developmental status of very low-birth-weight children at school age. JAMA 267:2204-2208. [PubMed] [Google Scholar]
- 47.Menendez, C., J. Ordi, M. R. Ismail, P. J. Ventura, J. J. Aponte, E. Kahigwa, F. Font, and P. L. Alonso. 2000. The impact of placental malaria on gestational age and birth weight. J. Infect. Dis. 181:1740-1745. [DOI] [PubMed] [Google Scholar]
- 48.Meuris, S., B. B. Piko, P. Eerens, A. Van Bellinghen, M. Dramaix, and P. Hennart. 1993. Gestational malaria: assessment of its consequences on fetal growth. Am. J. Trop. Med. Hyg. 48:603-609. [DOI] [PubMed] [Google Scholar]
- 49.Mock, N. B., D. M. Mercer, J. C. Setzer, R. J. Magnani, K. Tankari, and L. Brown. 1994. Prevalence and differentials of low birth weight in Niamey, Niger. J. Trop. Pediatr. 40:72-77. [DOI] [PubMed] [Google Scholar]
- 50.Moller, B., O. Lushino, O. Meirik, M. Gebre-Medhin, and G. Lindmark. 1989. A study of antenatal care at village level in rural Tanzania. Int. J. Gynaecol. Obstet. 30:123-131. [DOI] [PubMed] [Google Scholar]
- 51.Morgan, H. G. 1994. Placental malaria and low birthweight neonates in urban Sierra Leone. Ann. Trop. Med. Parasitol. 88:575-580. [DOI] [PubMed] [Google Scholar]
- 52.Mulumba, M. P., M. Wery, N. N. Ngimbi, K. Paluku, P. van der Stuyft, and A. de Muynck. 1990. Le paludisme de l'enfant a Kinshasa (Zaire) influence des saisons, de l'age, de l'environnement et du standing familial. Med. Trop. 50:53-64. [PubMed] [Google Scholar]
- 53.Murphy, S. C., and J. G. Breman. 2002. Gaps in the childhood malaria burden in Africa: cerebral malaria, neurological sequelae, anemia, respiratory distress, hypoglycemia, and complications of pregnancy. Am. J. Trop. Med. Hyg. 64(Suppl. 1-2):S57-S67. [DOI] [PubMed] [Google Scholar]
- 54.Ndyomugyenyi, R., and P. Magnussen. 2001. Malaria morbidity, mortality and pregnancy outcome in areas with different levels of malaria transmission in Uganda: a hospital record-based study. Trans. R. Soc. Trop. Med. Hyg. 95:463-468. [DOI] [PubMed] [Google Scholar]
- 55.Newman, R. D., A. Hailemariam, D. Jimma, A. Degifie, D. Kebede, A. E. C. Rietveld, B. L. Nahlen, J. W. Barnwell, R. W. Steketee, and M. E. Parise. 2003. Burden of malaria during pregnancy in areas of stable and unstable transmission in Ethiopia during a nonepidemic year. J. Infect. Dis. 187:1765-1772. [DOI] [PubMed] [Google Scholar]
- 56.Odala, J. E., and J. O. Oheno. 1990. Socio-economic profiles, June 1990. Ministry of Planning and National Development, Government of Kenya, Nairobi, Kenya.
- 57.Okoko, B. J., O. O. Martin, L. K. Lawrence, D. Idiong, S. N. Mkpanam, A. Avieka, W. A. S. Banya, and K. Osinusi. 2002. Influence of placental malaria infection on foetal outcome in the Gambia: twenty years after Ian McGregor. J. Health Popul. Nutr. 20:4-11. [PubMed] [Google Scholar]
- 58.Omumbo, J. A. 2004. Developing a risk map of malaria transmission in the East and Horn of Africa. Ph.D. thesis. Oxford University, Oxford, United Kingdom.
- 59.Parise, M. E., J. G. Ayisi, B. L. Nahlen, L. J. Schultz, J. M. Roberts, A. Misore, R. Muga, A. J. Oloo, and R. W. Steketee. 1998. Efficacy of sulfadoxine-pyrimethamine for prevention of placental malaria in an area of Kenya with a high prevalence of malaria and human immunodeficiency virus infection. Am. J. Trop. Med. Hyg. 59:813-822. [DOI] [PubMed] [Google Scholar]
- 60.Parise, M. E., L. S. Lewis, J. G. Ayisi, B. L. Nahlen, L. Slutsker, R. Muga, S. K. Sharif, J. Hill, and R. W. Steketee. 2003. A rapid assessment approach for public health decision-making related to the prevention of malaria during pregnancy. Bull. W. H. O. 81:316-323. [PMC free article] [PubMed] [Google Scholar]
- 61.Pertet, A. M. 1990. The effect of weekly chloroquine prophylaxis given to pregnant mothers and their respective infants on birthweight and physical growth during infancy in a rural area of Kenya. Ph.D. thesis. University of Nairobi, Nairobi, Kenya.
- 62.Rip, M. R., C. S. Keen, and D. L. Woods. 1987. Spatial variations of low birthweight in Cape Town. J. Trop. Pediatr. 33:333-335. [DOI] [PubMed] [Google Scholar]
- 63.Rogerson, S. J., S. C. Chaiyaroj, K. Ng, J. C. Reeder, and G. V. Brown. 1995. Chondroitin sulphate A is a cell surface receptor for Plasmodium falciparum infected erythrocytes. J. Exp. Med. 182:15-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rogerson, S. J., E. Chaluluka, M. Kanjala, P. Mkundika, C. Mhango, and M. E. Molyneux. 2000. Intermittent sulfadoxine-pyrimethamine in pregnancy: effectiveness against malaria morbidity in Blantyre, Malawi, in 1997-99. Trans. R. Soc. Trop. Med. Hyg. 94:549-553. [DOI] [PubMed] [Google Scholar]
- 65.Salihu, H. M., G. Tchuinguem, and R. Ratard. 2000. Effect of chloroquine prophylaxis on birthweight and malaria parasite load among pregnant women delivering in a regional hospital in Cameroon. West Indian Med. J. 49:143-147. [PubMed] [Google Scholar]
- 66.Schapira, A., and F. Da Costa. 1988. Studies on malaria prophylaxis with chlorproguanil or chloroquine in Mozambique. Cent. Afr. J. Med. 34:44-49. [PubMed] [Google Scholar]
- 67.Shrimpton, R. 2003. Reducing childhood mortality in poor countries: preventing low birthweight and reduction of child mortality. Trans. R. Soc. Trop. Med. Hyg. 97:39-42. [DOI] [PubMed] [Google Scholar]
- 68.Shulman, C. E., and E. K. Dorman. 2003. Reducing childhood mortality in poor countries. Importance and prevention of malaria in pregnancy. Trans. R. Soc. Trop. Med. Hyg. 97:30-35. [DOI] [PubMed] [Google Scholar]
- 69.Shulman, C. E., T. Marshall, E. K. Dorman, J. N. Bulmer, F. Cutts, N. Peshu, and K. Marsh. 2001. Malaria in pregnancy: adverse effects on haemoglobin levels and birthweight in primigravidae and multigravidae. Trop. Med. Int. Health 6:770-778. [DOI] [PubMed] [Google Scholar]
- 70.Sirima, S. B., R. Sawadogo, A. C. Moran, A. Konate, A. Diarra, M. Yameogo, M. E. Parise, and R. D. Newman. 2003. Failure of a chloroquine chemoprophylaxis program to adequately prevent malaria during pregnancy in Koupela District, Burkino Faso. Clin. Infect. Dis. 36:1374-1382. [DOI] [PubMed] [Google Scholar]
- 71.Smith, T. A., J. D. Charlwood, J. Kihonda, S. Mwankusye, P. Billingsley, J. Meuwissen, E. Lyimo, W. Takken, T. Teuscher, and M. Tanner. 1993. Absence of seasonal variation in malaria parasitaemia in an area of intense seasonal transmission. Acta Trop. 54:55-72. [DOI] [PubMed] [Google Scholar]
- 72.Snow, R. W., J. A. Omumbo, B. Lowe, S. M. Molyneux, J. O. Obiero, A. Palmer, M. W. Weber, M. Pinder, B. Nahlen, C. Obonyo, C. Newbold, S. Gupta, and K. Marsh. 1997. Relation between severe malaria morbidity in children and level of Plasmodium falciparum transmission in Africa. Lancet 349:1650-1654. [DOI] [PubMed] [Google Scholar]
- 73.Snow, R. W., and K. Marsh. 2002. The consequences of reducing Plasmodium falciparum transmission in Africa. Adv. Parasitol. 52:235-264. [DOI] [PubMed] [Google Scholar]
- 74.Snow, R. W., M. H. Craig, C. R. J. C. Newton, and R. W. Steketee. 2003. The public health burden of Plasmodium falciparum malaria in Africa: deriving the numbers. The Disease Control Priorities Project (DCPP) Working Paper no 11. Fogarty International Center, National Institutes of Health, Bethesda, Md.
- 75.Snow, R. W., E. L. Korenromp, and E. Gouws. Pediatric mortality in Africa: Plasmodium falciparum malaria as a cause or risk? Am. J. Trop. Med. Hyg., in press. [PubMed]
- 76.Steketee, R. W., J. G. Breman, K. M. Paluku, M. Moore, J. Roy, and M. Ma-Disu. 1988. Malaria infection in pregnant women in Zaire: the effects and the potential for intervention. Ann. Trop. Med. Hyg. 82:113-120. [DOI] [PubMed] [Google Scholar]
- 77.Steketee, R. W., J. J. Wirima, A. W. Hightower, L. Slutsker, D. L. Heymann, and J. G. Breman. 1996. The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity, and intrauterine growth retardation in rural Malawi. Am. J. Trop. Med. Hyg. 55(Suppl. 1):S33-S41. [DOI] [PubMed] [Google Scholar]
- 78.Steketee, R. W., J. J. Wirima, P. B. Bloland, B. Chilima, J. H. Mermin, L. Chitsulo, and J. G. Breman. 1996. Impairment of a pregnant woman's acquired ability to limit Plasmodium falciparum by infection with human immunodeficiency virus type-1. Am. J. Trop. Med. Hyg. 55(Suppl. 1):S42-S49. [DOI] [PubMed] [Google Scholar]
- 79.Steketee, R. W., B. L. Nahlen, M. E. Parise, and C. Menendez. 2001. The burden of malaria in pregnancy in malaria-endemic areas. Am. J. Trop. Med. Hyg. 42(Suppl. 1-2):S28-S35. [DOI] [PubMed] [Google Scholar]
- 80.Sule-Odu, A. O., A. Ogunledun, and A. O. Olatunji. 2002. Impact of asymptomatic maternal malaria parasitaemia at parturition on perinatal outcome. J. Obstet. Gynaecol. 22:25-28. [DOI] [PubMed] [Google Scholar]
- 81.Taylor, H. G., N. Klein, N. M. Minich, and M. Hack. 2000. Middle-school-age outcomes in children with very low birthweight. Child Dev. 71:1495-1511. [DOI] [PubMed] [Google Scholar]
- 82.Teplin, S. W., M. Burchinal, N. Johnson-Martin, R. Humphrey, and E. Kraybill. 1991. Neurodevelopmental, health and growth status at age 6 years of children with birth weights less than 1001 grams. J. Pediatr. 118:768-777. [DOI] [PubMed] [Google Scholar]
- 83.Ter Kuile, F. O., D. J. Terlouw, P. A. Phillips-Howard, W. A. Hawley, J. F. Friedman, S. K. Kariuki, Y. P. Shi, M. S. Kolczak, A. A. Lal, J. M. Vulule, and B. L. Nahlen. 2003. Reduction of malaria during pregnancy by permethrin-treated bed nets in an area of intense perennial malaria transmission in western Kenya. Am. J. Trop. Med. Hyg. 68(Suppl. 4):S50-S60. [PubMed] [Google Scholar]
- 84.Traore, S. 1996. Epidemiologie du Paludisme en zone de savane sud-soudanienne au Mali: le village de Pimperna dans la région de Sikasso de Juin 1992 à Septembre 1993. Thesis. University of Mali, Ecole Nationale de Médicine et de la Pharmacie (ENMP), Bamako, Mali.
- 85.UNICEF. 2002. The state of the world's children report 2003—child participation. UNICEF, New York, N.Y.
- 86.Van Ejik, A. M., J. G. Ayisi, F. O. Ter Kuile, A. O. Misore, J. A. Otieno, D. H. Rosen, P. A. Kager, R. W. Steketee, and B. L. Nahlen. 2003. HIV increases the risk of malaria in women of all gravidities in Kisumu, Kenya. AIDS 17:595-603. [DOI] [PubMed] [Google Scholar]
- 87.Verhoeff, F. H., B. J. Brabin, L. Chimsuku, P. Kazembe, W. B. Russell, and R. L. Broadhead. 1998. An evaluation of the effects of intermittent sulfadoxine-pyrimethamine treatment in pregnancy on parasite clearance and risk of low birthweight in rural Malawi. Ann. Trop. Med. Hyg. 92:141-150. [DOI] [PubMed] [Google Scholar]
- 88.Verhoeff, F. H., B. J. Brabin, C. A. Hart, L. Chimsuku, P. Kazembe, and R. L. Broadhead. 1999. Increased prevalence of malaria in HIV-infected pregnant women and its implications for malaria control. Trop. Med. Int. Health 4:5-12. [DOI] [PubMed] [Google Scholar]
- 89.Verhoeff, F. H., B. J. Brabin, S. van Buuren, L. Chimsuku, P. Kazembe, J. M. Wit, and R. L. Broadhead. 2001. An analysis of intra-uterine growth retardation in rural Malawi. Eur. J. Clin. Nutr. 55:682-689. [DOI] [PubMed] [Google Scholar]
- 90.Walraven, G. E. L., R. J. E. Mkanje, H. A. G. H. van Asten, J. van Roosmalen, P. W. J. van Dongen, and W. M. V. Dolmans. 1997. The aetiology of low birthweight in a rural area of Tanzania. Trop. Med. Int. Health 2:558-567. [DOI] [PubMed] [Google Scholar]
- 91.World Health Organization. 1977. International classification of diseases, 1975 revision, vol. 1. World Health Organization, Geneva, Switzerland.
- 92.World Health Organization/UNICEF. 2003. Africa malaria report 2003. WHO/CDS/MAL/2003.1093. World Health Organization, Geneva, Switzerland.
- 93.Yamagata, Y. 1996. Final report: malaria control in the United Republic of Tanzania, 1996. Report by Japanese International Cooperation Agency to Ministry of Health, Tanzania, October 1996. Ministry of Health, Dar-es-Salaam, Tanzania.