Abstract
Soluble TLR2 levels are elevated in infective and inflammatory conditions, but its diagnostic value with sepsis-induced multi-organ failure has not been evaluated. 37 patients with a diagnosis of severe sepsis/septic shock (sepsis) and 27 patients with organ failure without infection (SIRS) were studied. Median (IQR) plasma sTLR2 levels were 2.7 ng/ml (1.4–6.1) in sepsis and 0.6 ng/ml (0.4–0.9) in SIRS p < 0.001. sTLR2 showed good diagnostic value for sepsis at cut-off of 1.0 ng/ml, AUC:0.959. We report the ability of sTLR2 levels to discriminate between sepsis and SIRS within 12 h of ICU admission in patients with multi-organ failure.
Findings
The diagnosis of sepsis in ICU patients with organ failure is fraught with difficulty since both clinical signs and current diagnostic tests may be equivocal. Source control and timely antibiotic administration are crucial; thus, diagnostic tests that might enable early exclusion or positive identification of an infective etiology of critical illness are the focus of intensive research [1].
Toll-like receptor 2 (TLR2) is a member of a family of immune receptors which trigger pro-inflammatory responses following recognition of a range of microorganisms such as bacteria, viruses, and fungi. TLR2 is mainly expressed by myeloid cells and a soluble form (sTLR2), capable of down-modulating TLR-mediated pro-inflammatory responses, is released in response to microbial challenges [2]. Plasma levels of sTLR2 are elevated in a number of infective and inflammatory conditions [3] but its diagnostic value in ICU patients with sepsis-induced multi-organ failure has not been evaluated.
Following ethical approval by the South East Wales Research Ethics Committee (reference number 10WSE/421, June 2011) registration with the UK Clinical Research Network (UKCRN; cellular and biochemical investigations in sepsis, ID 11231) and written consent, 37 patients presenting to the Royal Glamorgan Hospital 10-bedded mixed medical/surgical ICU between January 2011 and March 2014 with a diagnosis of severe sepsis or septic shock according to the ESICM/SCCM consensus criteria [4] were enrolled within 24 h of the presumed onset of their illness, together with a cohort of 27 patients with organ failure due to dysregulated host response of non-infective origin (SIRS group). Patients in the SIRS group were enrolled when fulfilled two or more SIRS criteria, had documented organ dysfunction, but were not treated with antimicrobials for known or presumed infection. Blood was drawn within 12 h of ICU admission and plasma sTLR2 and C-reactive protein levels were determined by ELISA methods following the manufacturer’s instructions (R&D Systems, Minneapolis, MN, sTLR2 in normal serum: 0.575 ± 0.140 ng/ml; range 0.296–0.880).
For statistical analysis, chi-square test and Mann-Whitney U test—when the Kruskal-Wallis test rejected the null hypothesis of no differences between medians—was used as appropriate. We assessed correlations between parameters using the Spearman Rho’s correlation test. A result was considered to be significant at p < 0.05. Receiver operating characteristic (ROC) curves were plotted and the respective areas under the curve were calculated. Statistics were performed using the Statistical Program for Social Sciences (SPSS®) 20.0 software for Mac (Chicago, IL, USA).
Clinical characteristics of the patients in the sepsis and SIRS groups are presented in Table 1. Five patients in the sepsis group had culture-proven Gram-positive infection (four blood culture and one sputum), four had Gram-negative infection (all blood culture), and one had fungal infection (blood culture). Median (interquartile range) plasma sTLR2 levels were 2.7 ng/ml (1.4–6.1) in patients with severe sepsis and septic shock and 0.6 ng/ml (0.4–0.9) in patients with SIRS (p < 0.001 by Mann-Whitney U test, Fig. 1a). With a cut-off value of 1.0 ng/ml, sTLR2 showed good diagnostic value for sepsis, as it had a sensitivity of 90%, a specificity of 91%, and an AUC of 0.959 (Fig. 1b).
Table 1.
Characteristics of patients in the sepsis and SIRS groups
| Sepsis n = 37 | SIRS n = 27 | p value | |
|---|---|---|---|
| Age | 63 (55–72) | 63 (48–69) | 0.298 |
| Sex (M/F) | 17/20 | 20/7 | 0.040 |
| Admission SOFA | 16 (14–19) | 14 (13–17) | 0.080 |
| White cell count (109/L) | 15 (11–22) | 13 (8–17) | 0.169 |
| Mean arterial pressure (mmHg) | 78 (67–87) | 79 (72–91) | 0.445 |
| PEEP (cm H2O) | 8 (5–8) | 7 (5–9) | 0.892 |
| SpO2 (%) | 98 (95–100) | 99 (98–100) | 0.131 |
| FiO2 | 0.5 (0.4–0.6) | 0.4 (0.35–0.5) | 0.326 |
| Peak inspiratory pressure (cm H2O) | 22 (19–25) | 24 (16–29) | 0.528 |
| Creatinine (μmol/L) | 158 (86–259) | 88 (66–168) | 0.010 |
| Urea (mmol/L) | 13.2 (8.6–18.3) | 6.2 (4.2–10) | <0.001 |
| Albumin (g/L) | 20 (16–25) | 31 (22–34) | <0.001 |
| CRP (mg/L) | 218 (129–340) | 84 (40–168) | 0.001 |
| ICU stay (days) | 10 (5–15) | 4 (3–8) | 0.016 |
| Ventilated days | 5 (2–9) | 3 (1–4) | 0.133 |
| Shock days | 3 (2–4) | 0 (0–3) | 0.002 |
| Renal support days | 0 (0–5) | 0 (0–0) | 0.011 |
| In-hospital mortality | 12 (32%) | 11 (41%) | 0.142 |
Data are presented as medians, with the interquartile ranges in brackets. For statistical analysis, Mann-Whitney U test and chi-square test were used to test differences between the sepsis and SIRS groups
Fig. 1.
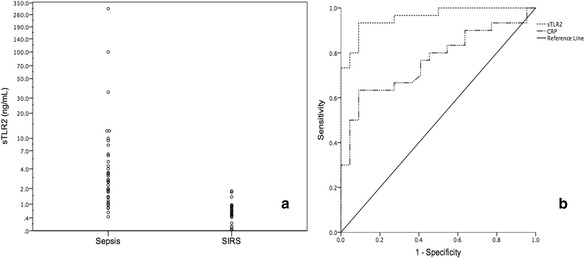
Individual sTLR2 levels in the sepsis and SIRS groups (a) and receiver operating characteristic curve (ROC) for the ability of sTLR2 and CRP levels to diagnose sepsis (b). Area under the curve (AUC) for sTLR2 0.959; 95% CI 0.912–1.000; AUC for CRP 0.764; 95% CI 0.635–0.894
In this feasibility pilot study, we report the ability of sTLR2 levels to discriminate between sepsis and SIRS within 12 h of ICU admission in a well-balanced group of patients with multi-organ failure. sTLR2 constitutes an important first-line negative regulatory mechanism to avoid harmful inflammatory responses [2]. The observed higher levels of plasma sTLR2 in sepsis (irrespective of the causative organism) than in SIRS patients suggest that this negative feedback mechanism is rapidly and preferentially activated upon infection. Notably, we found that sTLR2 has better specificity and sensitivity for sepsis than C-reactive protein, the most commonly used marker in the ICU (Fig. 1b, AUC - sTLR2 0.959; CRP - 0.764). It is encouraging that sTLR2 levels below 1 ng/mL had good ability to rule out sepsis whether it is secondary to bacterial or fungal infection within the first 12 h of ICU stay, when clinical parameters and traditional markers of infection are often equivocal. While sTLR2 levels on their own appear to be good markers of sepsis within the first 12 h of ICU admission, it is likely that they might perform even better as part of a biomarker panel [5]. Given the small sample size of our study, these promising findings warrant a larger confirmatory trial before sTLR2 levels can be introduced in the routine clinical practice.
Acknowledgements
The authors would like to thank Ms. Kelly Lewis, Mrs. Caroline Hamilton, and Dr. Matt Morgan for their invaluable help in recruiting the patients and maintaining the clinical database.
Funding
This work was supported by grants from The Wellcome Trust UK; I3 Interdisciplinary Research Group, Cardiff University, Cardiff, UK; National Institute of Social Care and Health Research (NISCHR)/Wales Office of Research and Development for Health and Social Care (to MOL); NISCHR Fellowship (to A-CR); the Wales Clinical Academic Track programme of the Welsh Assembly Government and Cardiff University (to BH); and NISCHR Clinical Research Fellowship (to TSz) and the UK Clinical Research Network Study Portfolio.
Authors’ contributions
BH, A-CR, and VH performed the laboratory analysis. TSz and KD recruited the patients and collected clinical data. MOL and JEH designed the study and secured funding. BH and TSz performed the statistical analysis. BH and TSz drafted the manuscript. TSz, A-CR, VH, KD, and MOL revised it for important intellectual content. All authors approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Tamas Szakmany, Phone: +44(0)2920743110, Email: szakmanyt1@cardiff.ac.uk.
Mario O. Labéta, Phone: +44(0)2920687019, Email: Labeta@cardiff.ac.uk
References
- 1.Cohen J, Vincent JL, Adhikari NK, et al. Sepsis: a roadmap for future research. Lancet Infect Dis. 2015;15:581–614. doi: 10.1016/S1473-3099(15)70112-X. [DOI] [PubMed] [Google Scholar]
- 2.Raby A-C, Le Bouder E, Colmont C, et al. Soluble TLR2 reduces inflammation without compromising bacterial clearance by disrupting TLR2 triggering. J Immunol. 2009;183:506–17. doi: 10.4049/jimmunol.0802909. [DOI] [PubMed] [Google Scholar]
- 3.Henrick BM, Yao X-D, Taha AY, German JB, Rosenthal KL. Insights into soluble Toll-like receptor 2 as a downregulator of virally induced inflammation. Front Immunol. 2016;7:291. doi: 10.3389/fimmu.2016.00291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29:530–8. doi: 10.1007/s00134-003-1662-x. [DOI] [PubMed] [Google Scholar]
- 5.Kempsell KE, Ball G, Szakmany T. Issues in biomarker identification, validation and development for disease diagnostics in public health. Expert Rev Mol Diagn. 2016;16:383–6. doi: 10.1586/14737159.2016.1133300. [DOI] [PubMed] [Google Scholar]


