Abstract
Strongyloides stercoralis is a soil-transmitted helminth (STH) widespread in various part of the world. A 78-yr-old peasant diabetic female from Mazandaran Province northern Iran, was admitted to Infection Department of the Razi Hospital in city of Qaemshahr, north of Iran complaining about abdominal skin rash, pruritus, itching, anorexia, nausea, vomiting, dysuria and cough. This patient had cutaneous migration effects of S. stercoralis larvae in her abdominal skin (larva currents and urticaria). Lung CT without contrast demonstrate s bilateral diffuse ground glass opacity draws attention. Upper gastrointestinal endoscopy revealed gastro esophageal reflux with antral gastritis. Duodenal endoscopy showed unusual mucosa and a biopsy from it sent to the pathology laboratory. Histopathology of duodenal bulb and duodenum biopsy showed mild villous atrophy and S. stercoralis infection. The patient was treated with albendazole and clinical sings improved completely after treatment. Strongyloidiasis should be carefully considered by clinicians who practice in endemic areas. Clinicians must keep a high level of skepticism for patients from endemic area.
Keywords: Strongyloides stercoralis, Immunocompromise, Iran
Introduction
Strongyloides stercoralis is a soil-transmitted helminth (STH) widespread in various part of the world. Recently, it has been estimated about 370 million people are infected with this parasite (1). Strongyloides is one of the most ignored infections between the neglected tropical diseases (NTDs) (2). Data about S. stercoralis is much less than other major soil-transmitted helminths (STHs), such as Ascaris lumbricoides, Necator americanus, Ancylostoma duodenale and Trichuris trichiura (3). Strongyloides has a complex life cycle and transmission of it is usually with penetration into the skin by filariform larvae, which originating from soil or other materials contaminated by human feces (4, 5). It can also replicate inside the host as an autoinfection and causing a long-lived infection in humans for decade (6, 7). Infection with the S. stercoralis in individuals with a complete immune system is self-limited but in immunocompromised patients can be complicated and cause hyperinfection (8, 9).
The signs of strongyloidiasis varies and contains asymptom, complaints such as irritation, inflammation, and pruritus at the place of penetration of the skin, Luffer’s syndrome (larvae immigration through the lung), abdominal pain, qualm, diarrhea, and malabsorption syndrome with long-lasting strongyloidiasis (8, 9). Presence of infection with S. stercoralis in the stomach and lung is relatively rare (10–12).
We report a case of immunocompromised patient in north of Iran, that infected by S. stercoralis and involvement three organs of this patient.
Case report
A 78-yr-old peasant female was admitted to Infection Department of the Razi Hospital in city of Qaemshahr in north of Iran on April 2015 due to abdominal skin rash, dysuria and cough from two weeks ago. She had nausea and vomiting from one day ago. The rash was with pruritus. This patient was a known case of diabetes mellitus and nephrotic syndrome for one year and take 10 unit insulin NPH daily and prednisolone 12.5 mg/d. She also had edema in lower extremities until near the knee. In physical examination revealed temperature body: 36.3 °C, Blood pressure: 125/80 mmHg, Respiratory rate: 16 rr/min, Heart rate: 83 beat/min. Chest sound was normal in auscultation of abdominal examination. The skin rash was linear erythematous and migratory similar to larvae current and urticaria (Fig. 1).
Fig. 1:

Larva currents and urticarial in abdominal skin (Original)
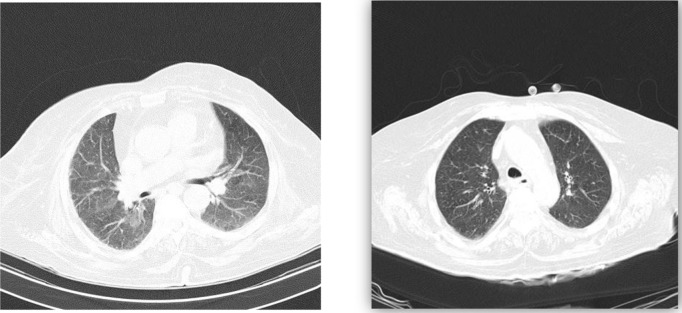
In blood examination, the ESR was normal but she had anemia with hemoglobin level 8.1 g/dl, mild thrombocytopenia 142×10 3 μ/L and normal with cell (9.8×10 3 /μd) and hyper-glycemia with 368 mg/dl blood sugar. The urea and creatinine level was high, 113 mg/dl and 1.4 mg/dl, respectively. Liver function test was impaired with SGOT: 59 IU/I, SGPT: 70 IU/I, alkaline phosphatase: 675 IU/I. In direct examination of feces parasite not observed. She underwent at upper gastrointestinal endoscopy that revealed gastroesophagus reflux with antral gastritis. Biopsy was taken and sent to pathology laboratory. A chest X ray obtained was normal but in lung CT scan without contrast bilateral diffuse ground glass opacity seen (Fig. 2).
Fig. 2:
Spiral lung CT parenchymal windows. Left-Pretreatment Right-post treatment 10 days after starting treatment
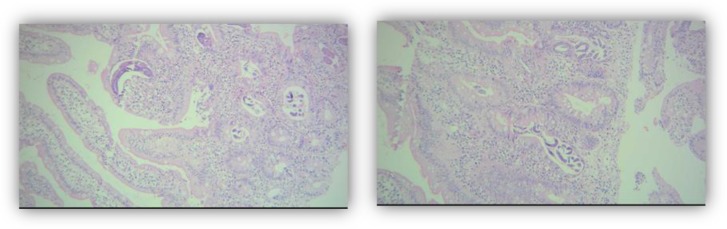
Histopathology show mild villous atrophy with Strongyloides infestation (Fig. 3).
Fig. 3:
Numerous longitudinal and cross section of S. stercoralis adult worms in duodenale mucosa are observed, H&E stain, Power 400x
The patient was treated with albendazole 400 mg doses twice daily during two weeks and discharged from Hospital after 14 days of admission. Treatment prolonged for one month. Clinical sings improved complete lately after treatment. Follow-up stool examination 14 and 40 days after beginning treatment show no S. stercoralis larva in stool.
Discussion
This is the first report of strongyloidiasis in a patient that suffering from diabetes, nephritis and gastric symptom in northern Iran.
Clinical and paraclinical inspection confirm presence of S. stercoralis in this case. This patient lived in rural area of Mazandaran Province and probably infected with this parasite when she worked barefoot in rice farm (12). In this case, the stool microscopy not identifies S. stercoralis; consequently, the diagnosis was based on biopsy. Strongyloidiasis is endemic in Southeast Asia, Latin America, sub-Saharan Africa, parts of the southeastern United States and Iran (13). Mazandaran is a province with moderate climate, in northern of Iran, at the vicinity of Alburz Mountain range and Caspian Sea. 45.9% of the population in this area was as urban inhabitants and 54.1% villagers (14). This province, located in the north of Iran and close to the sea, has the largest polar of production of rice in Iran (15). Infection with S. stercoralis in this province, that has a moderate temperature and high moisture, is endemic (16, 17). The prevalence of S. stercoralis in northern Iran is reported from 1%–10.3% (18–21).
Infection with S. stercoralis is comparatively common in north of Iran because of high humidity, kind of soil, and high exposure to mud in agriculturalists, particularly paddy field workers (22). People such as this patient who work in rice-filed are most commonly infected with this parasite (13, 23). S. stercoralis infection is a therapeutic challenge but should always be cured even in asymptomatic people. It can lead to a 60%–85% death rate in immunocompromised people (6, 8, 24–26).
Strongyloidiasis should be carefully considered by clinicians who work in medical profession in endemic areas but it is easily neglected by both the patients and physicians (12). Clinicians must be skepticism of patients from endemic areas (12, 27). Moreover, screening for strongyloidiasis infection in endemic area, particularly in corticosteroids treatment patient for example inflammatory bowel disease (IBD) is recommended (6).
Acknowledgments
The authors would like to appreciate for financial support by Vice Chancellors for Research of Mazandaran University of Medical Sciences (project number: 472). The authors declare that there is no conflict of interests.
Reference
- 1. Bisoffi Z, Buonfrate D, Montresor A, Requena-Méndez A, Muñoz J, Krolewiecki AJ, et al. Strongyloides stercoralis: a plea for action. PLoS Negl Trop Dis. 2013. ; 7 (5 ): e2214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis--the most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg. 2009. ; 103 (10 ): 967 –72. [DOI] [PubMed] [Google Scholar]
- 3. Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet. 2006; 367 ( 9521): 1521– 1532 [DOI] [PubMed] [Google Scholar]
- 4. Potter A, Stephens D, De Keulenaer B. Strongyloides hyper-infection: a case for awareness. Ann Trop Med Parasitol. 2003; 97 (8): 855– 60. [DOI] [PubMed] [Google Scholar]
- 5. Won EJ, Jeon J, Koh YI, Ryang DW. Strongyloidiasis in a diabetic patient accompaniedby gastrointestinal stromal tumor: cause of eosinophilia unresponsive to steroid therapy. Korean J Parasitol. 2015; 53 (2): 223– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moghadam KG, Khashayar P, Hashemi M. Gastrointestinal strongyloidiasis in immunocompromised patients: a case report. Acta Med Indones. 2011; 43 (3): 191– 4. [PubMed] [Google Scholar]
- 7. Siddiqui AA, Berk SL. Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis. 2001. 1; 33 (7): 1040– 7. [DOI] [PubMed] [Google Scholar]
- 8. Tabei SZ, Asadian F, Fakhar M, Safaei A. Gastrointestinal hyper infection due to Strongyloides stercoralis in a patient with Behcet’s syndrome. Comp Clin Pathol. 2009; 18: 89– 91. [Google Scholar]
- 9. Keiser PB, Nutman TB. Strongyloides stercoralis in the Immunocompromised Population. Clin Microbiol Rev. 2004; 17 (1): 208– 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Igra-Siegman Y, Kapila R, Sen P, Kaminski ZC, Louria DB. Syndrome of hyperinfection with Strongyloides stercoralis. Rev Infect Dis. 1981; 3 (3): 397– 407. [DOI] [PubMed] [Google Scholar]
- 11. Wurtz R, Mirot M, Fronda G, Peters C, Kocka F. Short report: gastric infection by Strongyloides stercoralis. Am J Trop Med Hyg. 1994; 51 (3): 339– 40. [DOI] [PubMed] [Google Scholar]
- 12. Shafaghi A, Askari K, Hajizadeh H, Mansour-Ghanaei F. Gastric strongyloidiasis as multiple small gastric nodules. Am J Case Rep. 2012; 13: 7– 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dogan C, Gayaf M, Ozsoz A, Sahin B, Aksel N, Karasu I, et al. Pulmonary Strongyloides stercoralis infection. Respir Med Case Rep. 2014; 11: 12– 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anonymus . Available at: https://en.wikipedia.org/wiki/Mazandaran_Province .
- 15. Feizabadi Y. editor. Study of rice marketing system in Iran. 85th Annual Conference of the Agricultural Economics Society Warwick University; 2011. . [Google Scholar]
- 16. Arfaa F. Medical Helminthology. Daneshpajouh 2007: (In persian).
- 17. Rokni MB. The present status of human helminthic diseases in Iran. Ann Trop Med Parasitol. 2008; 102 (4): 283– 95. [DOI] [PubMed] [Google Scholar]
- 18. Rezaiian M, Hooshyar H. The prevalence of intestinal parasitic infection in rural areas of Tonekabon, Iran. Iran J Public Health. 1996; 25 (3–4): 47– 58. [Google Scholar]
- 19. Rohani S, Kiyanian H, Athari H. Prevalence of intestinal parasities in villages of Sari (1998–99). Journal of Zanjan University of Medical Sciences and Health Services. 2001; 9 ( 34): 33– 40. [Google Scholar]
- 20. Kia E, Mahmoudi M, Zahabiun F, Meamar A. An evaluation on the efficacy of agar plate culture for detection of Strongyloides stercoralis. Iran J Parasitol. 2007; 2 (1): 29– 34. [Google Scholar]
- 21. Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G. Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg. 2012; 106 (8): 455– 9. [DOI] [PubMed] [Google Scholar]
- 22. Fakhar M, Gholami Z, Banimostafavi ES, Madjidi H. Respiratory hyperinfection caused by Strongyloides stercoralis in a patient with pemphigus vulgaris and minireview on diagnosis and treatment of strongyloidiasis. Comparative Clin Pathol. 2010; 19 (6): 621– 5. [Google Scholar]
- 23. Ardic N. An overview of Strongyloides stercoralis andits infections. Mikrobiyol Bul. 2009; 43 (1): 169– 77. [PubMed] [Google Scholar]
- 24. Grove DI. Human strongyloidiasis. Adv Parasitol. 1996; 38: 251– 309. [DOI] [PubMed] [Google Scholar]
- 25. Fardet L, Genereau T, Poirot JL, Guidet B, Kettaneh A, Cabane J. Severe strongyloidiasis in corticosteroid-treated patients :case series and literature review. J Infect. 2007; 54 (1): 18– 27. [DOI] [PubMed] [Google Scholar]
- 26. Goh SK, Chow PK, Chung AY, Tan BH, Tan PH. Strongyloides colitis in a patient with Cushing’s syndrome. Gastrointest Endosc. 2004; 59 (6): 738– 41. [DOI] [PubMed] [Google Scholar]
- 27. Newberry AM, Williams DN, Stauffer WM, Boulware DR, Hendel-Paterson BR, Walker PF. Strongyloides hyperinfection presenting as acute respiratory failure and gram-negative sepsis. Chest. 2005; 128 (5): 3681– 4. [DOI] [PMC free article] [PubMed] [Google Scholar]