Abstract
A 74 yr old woman from Gonabad, southern part of Khorasan Razavi Province of Iran was admitted to a Hospital of Gonabad, because of respiratory distress, exertional dyspnea and fever. Close contact with domestic animals, history of chronic obstructive pulmonary disease (COPD), and completely resolved pulmonary tuberculosis (TB) in remote past, were notable parts of her past medical history. Due to clinical, paraclinical and radiographic findings and because of recent hospitalization, she was admitted to internal medicine ward with the diagnosis of health care associated pneumonia (HCAP). Despite the application of broad-spectrum antibiotics and appropriate supportive care, she had a poor response to the treatment. During the daily visit in Intensive Care Unit (ICU), numerous white larvae were detected in both nostrils. Further investigation of oropharynx and tracheal tube aspiration, showed no more larvae in mentioned parts. An hour later, nasal spontaneous bleeding occurred. Otorhinolaryngology consultation was performed and led to surgical procedure. In ENT examination, there were numerous larvae and massive clot formation in both inferior meatuses and distal nasal septum perforation. Thirty-seven extracted larvae were transferred to Medical Entomology lab by vial 70% ethanol and 5 live larvae for rearing. After precise investigation by aid of light microscopy, the larvae were identified as Chrysomya bezziana. Due to discovered 2nd larvae stage and duration of hospitalization, this infestation was identified as nasal myiasis.
Keywords: Chrysomya bezziana, Septicemia, Nasal myiasis, Iran
Introduction
The larvae of flies in the nose detected as nasal myiasis (1), is an infestation of the bad nasal hygiene cavities, by Diptera of genus Chrysomia. This is more common in tropical countries. Atrophic rhinitis is one of the important factors for this problem. The maggots can cause deformities of the nose, face, ears and other organs in human or occasionally causing meningitis and death (2).
Nasal myiasis is underreported, in the world but in the India (tropical countries), is endemic due to warm and humid conditions (3). This problem can be seen more in older people, especially females, who have little ability to ward off the flies themselves. It is common, in low socioeconomic classes that are poor nasal hygienic conditions. C. bezziana, known as Old World Screwworm flies, is an obligate parasite. While the fly larvae feed on the living tissue of warm-blooded mammals, many other fly larvae feed on. This insect, belongs to the order Diptera, family Calliphoridae, and suborder Cyclorrhapha (4).
The clinical and pathological infestation of myiasis in human will depend to the genus and species of flies, the mode of invasion by the larvae, the degree and type of migration after invasion, the stage in the life cycle of the fly, including the type and number of larval molts in the host and the topographical site of invasion (5). These flies can cause disease in humans, with living on rotten tissue (maggots), or larvae crawl under the skin. (6). Myiasis treatment, according to its type, to be performed as soon as possible, with surgery or using anti-bacterial materials and removing the larvae from cavity. In the case of intestinal myiasis of hexylresorcinol is used orally (5).
Case Report
A 74-yr-old female from Gonabad - southern part of Khorasan Razavi Province of Iran – had been referred in 8 June 2015 to a Hospital of Gonabad City, because of respiratory distress, exertional dyspnea and fever. History of chronic obstructive pulmonary disease (COPD), and completely resolved pulmonary tuberculosis (TB) in remote past, were notable parts of her past medical history. Due to clinical, paraclinical and radiographic findings and because of recent hospitalization, she was admitted to internal medicine ward with the diagnosis of health care associated pneumonia (HCAP). Despite the application of broad-spectrum antibiotics and appropriate supportive care, she had a poor response to the treatment. Subsequently, a computed tomography of lung was done. Computerized tomography (CT scan) showed a consolidation in right middle lobe of the right lung with air bronchogram, a right middle lobe mass (Diameter: 3 cm), and a right middle lobe pulmonary nodule (Diameter: 1 cm). The patient’s clinical status deteriorated and in 4 th day of her admission, severe sepsis occurred and the patient was transferred to Intensive Care Unit (ICU). After 24 hours, the patient was intubated due to severe hypoxic respiratory failure and loss of consciousness. On 4 th day of her admission to ICU and during the daily visit, numerous white larvae were detected in both nostrils ( Fig. 1)
Fig. 1:

Larvae of Chrysomya bezziana in Nasal Cavities of patient
Further investigation of oropharyngeal and tracheal tube aspiration, showed no more larvae in mentioned parts. An hour later, nasal spontaneous bleeding occurred. Otorhinolaryngology consultation was performed and led to surgical procedure. In ENT examination, there were numerous larvae and massive clot formation in both inferior meatuses and distal nasal septum perforation. The larvae and clots were extracted successfully and surgical mesh was applied to reconstruct the septal defect and terminate the bleeding. Finally, after the procedure, paranasal sinus and brain CT scan were performed to identify possible further sites of myasis involvement. There was not any site of further involvement, but CT scan showed distal nasal septum perforation ( Fig. 2). Despite broad spectrum antibiotics application and intensive supportive care, the clinical course of the underlying disease worsen and severe sepsis, septic shock and finally multi organ failure, led to patient’s death in 7 th day of her ICU admission (11 th day of hospitalization).
Fig. 2:

Axial and Para nasal CT scan shows nasal septal injury and perforation
Characteristics of Chrysomya bezziana
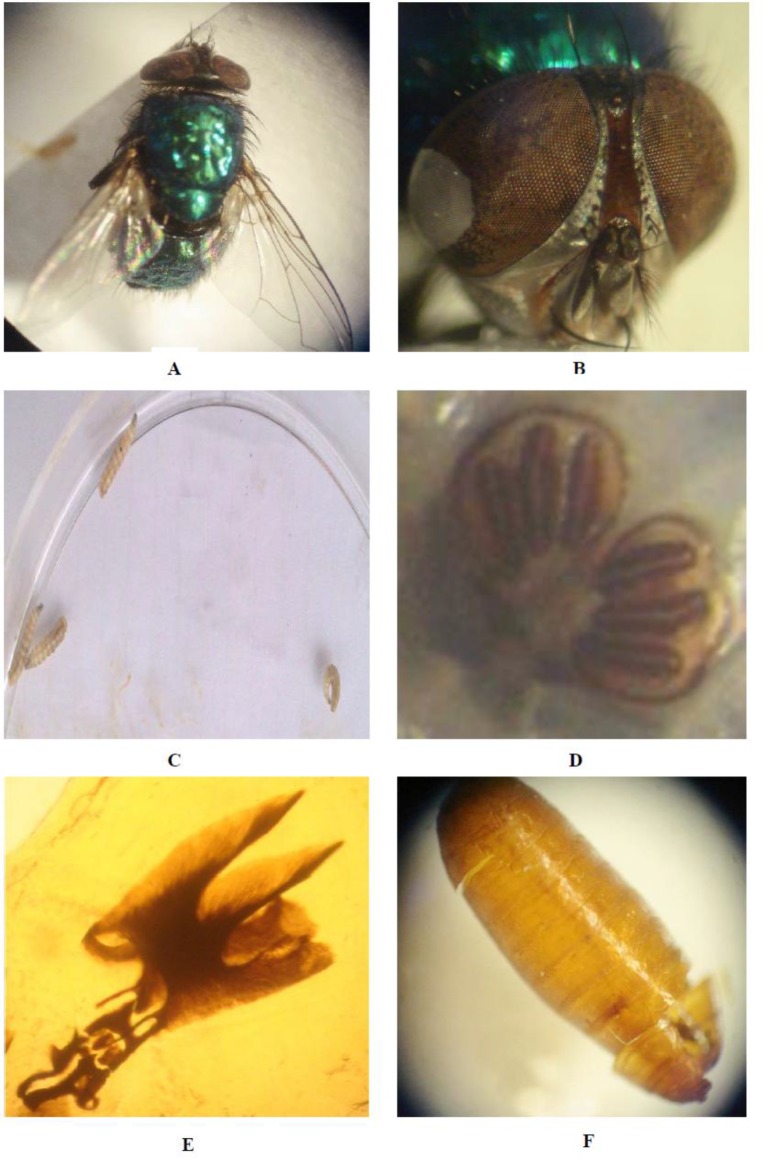
Forty-two larvae where extracted from both inferior nasal meatus and bleeding stopped successfully. Thirty-seven extracted larvae were transferred to Medical Entomology Lab by 70% ethanol vial and 5 alive larvae for rearing. After precise investigation by aid of light microscopy and used of key identification fly larvae, the larvae were detected as C. bezziana (Fig. 3).
Fig 3:
Adult form of Chrysomya bezziana found in this study (A), Head of C. bezziana (B), third stage of larvae (C)Posterior spiracle of C. bezziana in the third stage of larvae (D), Cephalopharyngeal skeleton of C. bezziana in the third larval stage(E), stage of pupa of C. bezziana (F). (Original Photos)
Discussion
Myiasis, in Greek means flies; the disease is observed more in middle age and old age. Hope for the first time, in 1840, reported contamination of humans and vertebrate animals, to the larval stages of flies that spend their life cycle on living or dead tissues (7).
C. bezziana belong to the Calliphoridae family and suborder Cyclorrhapha (8). This fly has been reported from South Asia, India, Africa, Saudi Arabia, Indonesia, the Philippines, Guinea and the Persian Gulf territory. Human infection with this type of flies was first reported by Abed- Benamara et al. from Algeria, in 1997 (9).
In this study, the mature C. bezziana had green-blue color, and 6 mm in size. The anterior spiracle is dark brown in color. The life cycle was 15 days and after 4 days, at a temperature of 30 °C and in blood agar culture, stage two larvae changed to stage three larvae, respectively. The larvae of stage two and three measured 9 and 18 mm respectively. After 4 days, larvae dropped on soil and after 3 days, become sexually mature flies. The present case is the first report of nosocomial myiasis caused by Chrysomia in Iran.
Maggots in nose are commonly seen in elderly patients with slight preponderance in females. It is common in low socioeconomic classes due to their poor nasal hygienic conditions (10).
Infestation of the nose can be extremely dangerous because of the possibility of penetration into the intracranial cavity and there is a fatality of 8% in such cases. The maggots may spread laterally and posterior to the orbit and par nasal sinuses and in a few instances may spread inferiorly and perforate the palate (11).
Nosocomial myiasis usually occurs in weak patients and with little ability (12). In our study, due to the larvae collected 4 days after patient hospitalization in the ICU, the type of myiasis is nosocomial myiasis.
Manfrim et al. reported a case of a 70-yr-old woman with nasal obstruction, nose itching and nasal/palatal myiasis after she had undergone an operation for basal cell carcinoma of the nasolabial fold (13).
A 15-yr-old girl of India presented with a chief complaint of bleeding from her nose. She had noticed that worms were emerging from her right nostril. She had a continuous dull ache on the right side of her nose, spreading over the maxillary sinus area, and on the infra-orbital margin on the same side. The maggots were reported to be C. bezziana (14). Lucilia sericata and C. bezziana has been recognized as a cause of wound myiasis (15). Recently, human cases of myiasis caused by the fly, C. Bezziana in south and southeast of Iran have been increased (16).
The first diagnosis C. bezziana in Iran was reported by the Tirgari et al. in 2002 (17). A 63-year old man was admitted to an ICU in Mashhad City of Iran. He has been in adult ICU for more than 40 days while in deep coma. On the 35 th day of hospitalization, about 100 larvae of 6–7 mm in length yellow to cream and fusiform were observed around the tracheotomy site and malodorous open wound, They were identified as second instar larvae of Lucilia genus of the family Calliphoridae (18).
Conclusion
To our knowledge, it is first case report of Nasal Nosocomial myiasis caused by C. bezziana in Iran and world.
Acknowledgements
The authors declare that there is no conflict of interests.
References
- 1. Sinha V, Shah S, Ninama M, Gupta D, Prajapati B, More Y. Nasal Myiasis. J Rhinol. 2006; 13 (2): 120– 123. [Google Scholar]
- 2. Sony NK. Endoscopy in nasal myiasis. Trop Doct. 2000; 30: 225– 7 [DOI] [PubMed] [Google Scholar]
- 3. Sharma H, Dayal D, Agrawal SP. Nasal myiasis: review of 10-year experience. J Laryngol Otol. 1989; 103 (5): 489– 91. [DOI] [PubMed] [Google Scholar]
- 4. Yaghoobi R, Bagherani N. Chrysomya bezziana infestation in a neglected squamous cell carcinoma on the face. Indian J Dermatol Venereol Leprol, 2009; 75 (1 ): 81 –82. [DOI] [PubMed] [Google Scholar]
- 5. Hubbert WT, McCulloch WF, Schnurrenberger PR. Diseases Transmitted From Animals to Man, 6th ed Springfield, 1ll : , Charles C Thomas ; , 1975. . [Google Scholar]
- 6. Süleyman Yazar Bilal Dik, Şaban Yalçin, et al. Nosocomial Oral Myiasis by Sarcophaga sp. in Turkey. Yonsei Med J. 2005; 46 (3): 431– 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robbins K, Khachemoune A. Cutaneous myiasis: a review of the common types of myiasis. Int J Dermatol. 2010. : 1; 49 (10 ): 1092 –8. [DOI] [PubMed] [Google Scholar]
- 8. Ramalingam S, Nurulhuda A, Bee LH. Urogenital myiasis caused by Chrysomya bezziana (Diptera: Calliphoridae) in peninsular Malaysia. Southeast Asian J Trop Med Public Health. 1980; 11: 405– 7. [PubMed] [Google Scholar]
- 9. Abed-Benamara M, Achir I, Rodhain F, Perez-Eid C. First Algerian case of human otomyiasis from Chrysomya bezziana. Bull Soc Pathol Exot. 1997; 90: 172– 5. [PubMed] [Google Scholar]
- 10. Kuruvilla G, Albert RRA, Job A, Ranjith VT, Selvakumar P. Pneumocephalus: a rare complication of nasal myiasis. Am J Otolaryngol 2006; 27: 133– 135. [DOI] [PubMed] [Google Scholar]
- 11. Thomas S1, Nair P, Hegde K, Kulkarni A. Nasal myiasis with orbital and palatal complications. BMJ Case Rep. 2010. ; 29 : 1 –4. 10.1136/bcr.08.2010.3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smith DR, Clevenger RR. Nosocomial nasal myiasis. Arch Pathol Lab Med. 1986; 110: 439– 40. [PubMed] [Google Scholar]
- 13. Manfrim AM, Cury A, Demeneghi P, et al. Nasal myiasis: case report and literature review. Arq Int Otorrinolaringol 2007; 11: 1– 7. [Google Scholar]
- 14. Bapna S, Kothari S, Raju S, et al. A rare case of human nasal myiasis due to the larvae of Oestrus Ovis. J Parasit Dis 2006; 30: 184– 6. [Google Scholar]
- 15. Alizadeh M1, Mowlavi G2, Kargar F, et al. A Review of Myiasis in Iran and a New Nosocomial Case from Tehran, Iran. J Arthropod Borne Dis. 2014; 8 (2): 124– 31. [PMC free article] [PubMed] [Google Scholar]
- 16. Faramarzi A, Rasekhi AR, Kalantari M, Hatam GR. Chrysomya bezziana as a causative agent of human myiasis in Fars Province, southern Iran. Iran J Arthropod-Borne Dis. 2009; 3: 60– 63. [PMC free article] [PubMed] [Google Scholar]
- 17. Tirgari S, Nateghpour M, Jahanian AH, Akbarzadeh K. Case report: First Record of Human Myiasis caused by Chrysomia bezziana (Villeneuve) in Iran (Diptera, Calliphoridae). Iran J Public Health. 2003. . 32 (3 ): 68 –70. [Google Scholar]
- 18. Najjari M, Shafiei R, Fakoorziba MR. Nosocomial myiasis with Lucilia sericata (Diptera: Calliphoridae) in an ICU patient in Mashhad, Northeastern of Iran. Arch Iran Med. 2014; 17 (7): 523– 5. [PubMed] [Google Scholar]