Abstract
Background
The sodium-glucose co-transporter-2 (SGLT-2) inhibitors have been reported to increase both low-density lipoprotein (LDL) and high-density lipoprotein (HDL)-cholesterol (C). This study aimed to determine how SGLT-2 inhibitors affect LDL and HDL-C subspecies.
Methods
This single center, open-label, randomized, prospective study included 80 patients with type 2 diabetes taking prescribed oral hypoglycemic agents. Patients were allocated to receive dapagliflozin (n = 40) or sitagliptin (n = 40) as add-on treatment. Fasting blood samples were collected before and 12 weeks after this intervention. Small dense (sd) LDL-C, large buoyant (lb) LDL-C, HDL2-C, and HDL3-C levels were determined using our established homogeneous assays. Statistical comparison of blood parameters before and after treatment was performed using the paired t test.
Results
Dapagliflozin and sitagliptin comparably decreased HbA1c (0.75 and 0.63%, respectively). Dapagliflozin significantly decreased body weight, systolic blood pressure, plasma triglycerides and liver transaminases, and increased adiponectin; sitagliptin did not alter these measurements. LDL-C and apolipoprotein (apo) B were not significantly changed by dapagliflozin, whereas HDL-C and apo AI were increased. Dapagliflozin did not alter concentrations of LDL-C, but sd LDL-C decreased by 20% and lb LDL-C increased by 18%. Marked elevation in lb LDL-C (53%) was observed in individuals (n = 20) whose LDL-C was elevated by dapagliflozin. However, sd LDL-C remained suppressed (20%). Dapagliflozin increased HDL2-C by 18% without affecting HDL3-C. Sitagliptin did not alter plasma lipids or lipoprotein subspecies.
Conclusions
A SGLT-2 inhibitor, dapagliflozin suppresses potent atherogenic sd LDL-C and increased HDL2-C, a favorable cardiometabolic marker. Although LDL-C levels are elevated by treatment with dapagliflozin, this was due to increased concentrations of the less atherogenic lb LDL-C. However, these findings were not observed after treatment with dipeptidyl peptidase-4 inhibitor, sitagliptin.
Trial registration UMIN Clinical Trials Registry (UMIN000020984)
Electronic supplementary material
The online version of this article (doi:10.1186/s12933-016-0491-5) contains supplementary material, which is available to authorized users.
Keywords: Dapagliflozin, Sodium-glucose co-transporter-2 inhibitor, Small dense low-density lipoprotein-cholesterol, High-density lipoprotein 2-cholesterol, Lipoprotein subspecies
Background
Recently, sodium-glucose co-transporter-2 (SGLT-2) inhibitors have been developed as novel therapeutic agents for the treatment of type 2 diabetes [1–3]. These drugs inhibit the reabsorption of glucose in the proximal tubules of the kidney, leading to increased urinary excretion of glucose and decreased levels of blood glucose in diabetic patients [1–3]. In addition, use of SGLT-2 inhibitors results in decreased body weight and visceral fat mass, and reduced blood pressure. These factors are expected to suppress adverse cardiovascular outcomes [1–3]. In a secondary prevention study (the EMPA-REG OUTCOME® trial), empagliflozin successfully suppressed composite adverse cardiovascular outcomes [4]. However, it remains unclear whether SGLT-2 inhibitors prevent cardiovascular events in cardiovascular disease-free diabetic patients. Several clinical studies have revealed that SGLT-2 inhibitors decrease plasma triglyceride (TG) levels and increase high-density lipoprotein (HDL)-cholesterol (C) (HDL-C) levels, but also increase low-density lipoprotein (LDL)-C (LDL-C) levels [5, 6]. LDL-C is the most powerful determinant of cardiovascular events in patients with type 2 diabetes [7, 8], thus, the increased levels of LDL-C associated with SGLT-2 inhibitor use might increase cardiovascular risk.
LDL-C can be fractionated into large buoyant (lb) and small dense (sd) particles based on size and density. An abundance of clinical evidence has shown that sd LDL-C particles are more atherogenic than lb LDL-C particles, and that the predominance of sd LDL-C confers a threefold increased risk for coronary artery disease [9], as sd LDL-C forms a good substrate for oxidized LDL-C in the arterial wall [10]. LDL size is inversely regulated by plasma TG levels [11] and insulin resistance [12]. There is a preponderance of sd LDL-C particles in individuals with hypertriglyceridemia, metabolic syndrome [13], and type 2 diabetes [14].
We established a homogeneous assay for the direct measurement of serum sd LDL-C concentrations [15]. This assay has been used in well-known, large cohort studies which revealed that sd LDL-C concentrations more sensitively predicted cardiovascular events than did LDL-C or lb LDL-C concentrations [16–18]. We hypothesized that SGLT-2 inhibitors decrease the levels of potent atherogenic sd LDL-C particles by decreasing TG levels and enhancing insulin sensitivity [1, 2]. If so, an increase in LDL-C by SGLT-2 inhibitors may be attributable to increases in less atherogenic lb LDL-C particles. Hence, we investigated the effect on plasma concentrations of LDL-C subspecies in type 2 diabetic patients treated with the SGLT-2 inhibitor, dapagliflozin, compared with patients treated with the dipeptidyl peptidase-4 (DPP-4) inhibitor, sitagliptin.
HDL-C also has subspecies, namely HDL2-C and HDL3-C. Large, cholesterol-rich HDL2-C is inversely associated with plasma TG and insulin resistance, whereas small, cholesterol-poor HDL3-C is not [19]. We established a homogeneous assay for the direct measurement of HDL3-C serum concentrations. Subtracting the concentration of HDL3-C from HDL-C gives the serum concentration of HDL2-C [20]. The second aim of the present study was to determine how the use of SGLT-2 inhibitor affects HDL-C subspecies in patients with type 2 diabetes.
Methods
Study design and subjects
This study was a single center, open-label, randomized, prospective study. Dapagliflozin (5 mg) or sitagliptin (50 mg) was administered once daily for 12 weeks as add-on therapy to established oral hypoglycemic drug treatment (sulfonylureas, metformin, or an α-glucosidase inhibitor). The study was conducted in patients diagnosed with type 2 diabetes whose blood glucose was inadequately controlled despite combined treatment with diet/exercise and an oral hypoglycemic drug for more than 12 weeks prior to screening. The main inclusion criteria were: (1) age ≥20 years and ≤65 years, (2) diagnosis of type 2 diabetes at least 3 months prior to screening, and (3) HbA1c of ≥6.5% [48 mmol/mol] and ≤9.4% [79 mmol/mol] whilst on treatment. The main exclusion criteria were: (1) previous stroke or ischemic heart disease, (2) insulin use, (3) current or potential pregnancy, (4) an estimated glomerular filtration rate of <60 mL/min/1.73 m2 at the beginning of the run-in period, (5) a TG level of ≥600 mg/dL on the day of screening, and (6) users of omega-3 fatty acids. No drugs were changed during the study period.
Measurements
Overnight fasting blood samples were obtained before and 12 weeks after the administration of dapagliflozin or sitagliptin. LDL-C and HDL-C were measured by conventional direct methods. Both sd LDL-C and HDL3-C concentrations were measured using the homogeneous methods we established [15, 20]. Non HDL-C was estimated by subtracting the HDL-C from the total-C concentration. Concentrations of lb LDL-C and HDL2-C were estimated by subtracting the sd LDL-C from the LDL-C or subtracting the HDL3-C from the HDL-C, respectively [15, 20]. We have previously reported excellent correlations (coefficient of correlation: r > 0.90, p < 0.0001) between measurements obtained using our homogeneous and the standard ultracentrifugation methods of measuring LDL-C and HDL-C sub-fraction concentrations [15, 20]. In addition, the validity of our homogeneous methods has been evaluated by other researchers [21]. Remnant-like particle-cholesterol (RLP-C) was measured by the direct homogeneous method (MetaboRead, Kyowa Medex Co., Ltd., Tokyo, Japan). Total adiponectin was determined by immunoassay (Denka Seiken., Co., Ltd., Tokyo, Japan).
Statistical analysis
Data were expressed as mean ± standard deviation (SD), number and percentage, or percent changes after treatment. Statistical analyses were performed using JMP 11.0 (SAS Institute., Cavy, NC, USA). The unpaired t-test (for continuous variables) or Fisher’s exact test (for categorical variables) was used for statistical analysis of differences in the baseline clinical parameters of participants in the dapagliflozin and sitagliptin groups. Comparison of plasma parameters before and after treatment was performed using the paired t-test, and for intergroup comparisons, the unpaired t-test was used for normally distributed data, the Mann–Whitney U test for data with skewed distributions. Correlations between 2 variables, the Pearson correlation coefficient was used for data with normal distribution pattern, whereas the Spearman rank-correlation coefficient was used for data with a non-normal distribution. Differences were considered statistically significant at values of p < 0.05.
Results
The study included 80 participants, 62 men and 18 women, who were randomly allocated to receive dapagliflozin (n = 40) or sitagliptin (n = 40). Additional file 1: Table S1 lists baseline general characteristics and blood biochemical measurements, Additional file 1: Table S2 lists blood lipid levels. There were no significant differences in general characteristics, blood biochemistry results, or lipid profiles between the dapagliflozin and sitagliptin group at baseline. Both groups exhibited hyperglycemia, mild obesity (BMI = 28 kg/m2), and mild liver dysfunction. The majority of patients had normal total cholesterol, LDL-C, and HDL-C levels and mild hypertriglyceridemia.
Table 1 lists general characteristics and blood biochemical measurements and lipid levels at 12 weeks after treatment with dapagliflozin or sitagliptin, and how these changed from baseline measurements. Dapagliflozin significantly reduced body weight (by 2.2 kg) (p < 0.001) and systolic blood pressure (by 4 mmHg) (p = 0.022), whereas these changes were not observed with sitagliptin. HbA1c levels decreased 0.75% in the dapagliflozin group vs. 0.63% in the sitagliptin group. Fasting blood glucose levels decreased by 23.5 and 18.7 mg/dL in the dapagliflozin and sitagliptin groups, respectively. These results are consistent with the results reported in previous clinical trials. Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were significantly (p < 0.001) decreased by dapagliflozin, while the liver function remained unchanged by sitagliptin treatment. Hemoglobin, hematocrit and blood urea nitrogen were significantly increased in the dapagliflozin group (p < 0.001), while this remained unchanged in the sitagliptin group. Dapagliflozin significantly increased the plasma level of adiponectin from 6.0 ± 3.4 to 7.6 ± 4.2 ng/mL (p < 0.001), whereas sitagliptin had no effect on plasma adiponectin levels. Thus, there were significantly differences between two treatment groups in terms of changes in ALT, AST, hemoglobin, hematocrit and adiponectin (p < 0.01).
Table 1.
Clinical parameters before and after administration of dapagliflozin or sitagliptin
| Dapagliflozin (n = 40) | Sitagliptin (n = 40) | p valueb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre treatment | Post treatment | % change | p valuea | Pre treatment | Post treatment | % change | p valuea | ||
| BW (kg) | 78.4 ± 14.3 | 76.2 ± 1.8 | −2.8 | <0.001* | 77.6 ± 11.6 | 77.7 ± 11.6 | 0.1 | 0.089 | 0.042* |
| SBP (mmHg) | 130.7 ± 15.8 | 126.5 ± 12.7 | −3.2 | 0.022* | 133.2 ± 17.8 | 131.0 ± 13.3 | −1.7 | 0.611 | 0.031* |
| DBP (mmHg) | 86.9 ± 10.7 | 82.3 ± 16.0 | −5.3 | 0.188 | 88.1 ± 9.5 | 84.4 ± 11.0 | −4.2 | 0.024* | 0.242 |
| HR (bpm) | 82.5 ± 10.4 | 81.6 ± 13.9 | −1.1 | 0.300 | 81.5 ± 10.3 | 77.1 ± 10.8 | −5.4 | 0.056 | 0.344 |
| Hb (mg/dL) | 14.4 ± 1.2 | 15.1 ± 1.4 | 4.9 | <0.001* | 14.2. ± 1.4 | 14.5 ± 1.5 | 2.1 | 0.088 | <0.001* |
| Ht (%) | 41.9 ± 3.5 | 44.5 ± 4.0 | 6.2 | <0.001* | 41.4 ± 4.3 | 41.9 ± 4.2 | 1.2 | 0.297 | <0.001* |
| AST (IU/L) | 34.5 ± 19.4 | 26.8 ± 12.8 | −22.3 | <0.001* | 33.2 ± 9.8 | 35.4 ± 14.9 | 6.6 | 0.089 | <0.001* |
| ALT (IU/L) | 46.6 ± 37.0 | 33.5 ± 24.9 | −28.1 | <0.001* | 42.8 ± 15.0 | 44.9 ± 18.4 | 4.9 | 0.202 | <0.001* |
| γGTP (IU/L) | 53.2 ± 43.0 | 42.3 ± 47.2 | −20.5 | 0.109 | 50.9 ± 18.1 | 52.2 ± 22.0 | 2.6 | 0.729 | 0.107 |
| BUN (mg/dL) | 14.6 ± 4.3 | 16.8 ± 5.0 | 15.1 | <0.001* | 13.5 ± 4.5 | 15.3 ± 4.6 | 13.3 | 0.115 | 0.367 |
| Cre (mg/dL) | 0.72 ± 0.17 | 0.74 ± 0.23 | 2.8 | 0.173 | 0.77 ± 0.17 | 0.81 ± 0.18 | 5.2 | 0.110 | 0.757 |
| eGFR (mL/min/1.73 m2) | 86.2 ± 18.4 | 83.6 ± 23.2 | −3.0 | 0.230 | 83.5 ± 22.7 | 79.2 ± 21.4 | −5.1 | 0.003* | 0.545 |
| FPG (mg/dL) | 145.8 ± 47.8 | 122.3 ± 24.9 | −16.1 | 0.002* | 144.9 ± 57.9 | 126.2 ± 43.9 | −12.9 | 0.043* | 0.673 |
| HbA1c (%) | 7.61 ± 1.15 | 6.86 ± 0.81 | −9.9 | <0.001* | 7.55 ± 1.64 | 6.92 ± 1.20 | −8.3 | 0.006* | 0.378 |
| C-peptide (ng/mL) | 2.79 ± 1.39 | 2.40 ± 1.56 | −14.0 | 0.018* | 2.70 ± 1.25 | 2.78 ± 1.48 | 3.0 | 0.633 | 0.190 |
| Adiponectin (ng/mL) | 6.0 ± 3.4 | 7.6 ± 4.2 | 26.7 | <0.001* | 6.2 ± 5.3 | 6.2 ± 3.8 | 0 | 0.899 | 0.002* |
Data are expressed as mean ± standard deviation or percent changes after the treatment
BW body weight, SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate, Hb hemoglobin, Ht hematocrit, AST aspartate aminotransferase, ALT alanine aminotransferase, γGTP γ-glutamyltranspeptidase, BUN blood urea nitrogen, Cre creatinine, eGFR estimated glomerular filtration rate, FPG fasting plasma glucose
ap values for the intragroup comparison (pre vs. post treatment values in dapagliflozin or sitagliptin group, * p < 0.05)
bp values for intergroup comparison (dapagliflozin vs. sitagliptin group in the changes from pre to post treatment, * p < 0.05)
Total-C, LDL-C, and apolipoprotein (apo) B were unchanged in both groups (Table 2). In the dapagliflozin group, the concentration of sd LDL-C decreased significantly (20%, p < 0.01), whereas that of lb LDL-C increased significantly (18%, p < 0.05) (Fig. 1a). These changes were not observed in sitagliptin group. HDL-C, HDL2-C, apo AI, apo AII were significantly increased in dapagliflozin group (p < 0.05) (Fig. 2a); these changes were not observed in sitagliptin group (Fig. 2b). Thus, there were significantly differences between two treatment groups in terms of changes in sd LDL-C, lb LDL-C, HDL-C, HDL2-C and apo AI (Table 2) (p < 0.05).
Table 2.
Lipid parameters before and after administration of dapagliflozin or sitagliptin
| Dapagliflozin (n = 40) | Sitagliptin (n = 40) | p valueb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre treatment | Post treatment | % change | p valuea | Pre treatment | Post treatment | % change | p valuea | ||
| Total-C (mg/dL) | 193.5 ± 36.6 | 198.4 ± 45.9 | 2.5 | 0.863 | 192.5 ± 58.2 | 195.5 ± 38.9 | 1.6 | 0.720 | 0.102 |
| TG (mg/dL) | 152.6 ± 63.7 | 133.7 ± 75.8 | −12.4 | 0.145 | 150.2 ± 85.2 | 144.6 ± 87.2 | −3.7 | 0.245 | 0.928 |
| HDL-C (mg/dL) | 48.4 ± 11.1 | 53.5 ± 13.0 | 10.5 | <0.001* | 50.3 ± 9.25 | 50.3 ± 11.1 | 0 | 0.948 | 0.003* |
| LDL-C (mg/dL) | 118.2 ± 32.1 | 118.8 ± 39.7 | 0.5 | 0.875 | 120.2 ± 35.1 | 114.7 ± 33.1 | −4.6 | 0.257 | 0.323 |
| Non HDL-C (mg/dL) | 145.1 ± 36.0 | 144.9 ± 439 | −0.1 | 0.947 | 142.2 ± 57.3 | 145.1 ± 38.4 | 2.9 | 0.717 | 0.328 |
| Apo AI (mg/dL) | 133.5 ± 21.6 | 143.5 ± 22.6 | 7.5 | 0.002* | 134.9 ± 25.2 | 128.8 ± 30.7 | −4.5 | 0.135 | 0.002* |
| Apo AII (mg/dL) | 29.7 ± 4.5 | 30.9 ± 5.0 | 4.0 | 0.022* | 30.5 ± 7.2 | 30.5 ± 7.2 | 0 | 0.945 | 0.148 |
| Apo B (mg/dL) | 100.1 ± 24.5 | 100.8 ± 28.1 | 0.7 | 0.777 | 102.3 ± 27.7 | 97.4 ± 26.5 | −4.8 | 0.123 | 0.131 |
| Apo CII (mg/dL) | 4.8 ± 1.7 | 4.9 ± 2.2 | 2.1 | 0.362 | 5.4 ± 2.8 | 5.1 ± 2.6 | −5.6 | 0.197 | 0.105 |
| Apo CIII (mg/dL) | 10.5 ± 3.2 | 11.4 ± 4.3 | 8.6 | 0.021* | 10.1 ± 4.5 | 9.6 ± 4.0 | −5.0 | 0.335 | 0.028* |
| Apo E (mg/dL) | 4.4 ± 1.2 | 4.4 ± 1.5 | 0 | 0.530 | 4.3 ± 1.5 | 4.1 ± 1.0 | −4.7 | 0.296 | 0.216 |
| RLP-C (mg/dL) | 6.8 ± 4.3 | 6.4 ± 5.1 | −5.9 | 0.620 | 6.9 ± 8.0 | 6.1 ± 5.7 | −11.6 | 0.303 | 0.750 |
| HDL2-C (mg/dL) | 26.1 ± 8.2 | 30.8 ± 10.8 | 18.0 | <0.001* | 26.6 ± 7.9 | 27.5 ± 8.4 | 3.4 | 0.334 | 0.013* |
| HDL3-C (mg/dL) | 22.2 ± 3.9 | 22.7 ± 5.0 | 2.3 | 0.527 | 23.3 ± 5.2 | 22.2 ± 5.3 | −4.7 | 0.132 | 0.130 |
| sd LDL-C (mg/dL) | 54.4 ± 24.6 | 43.6 ± 24.4 | −19.9 | 0.005* | 54.0 ± 22.5 | 50.4 ± 22.4 | −6.7 | 0.368 | 0.003* |
| lb LDL-C (mg/dL) | 63.8 ± 27.6 | 75.1 ± 34.1 | 17.7 | 0.026* | 66.2 ± 26.3 | 64.3 ± 24.1 | −2.9 | 0.671 | 0.029* |
Data are expressed as mean ± standard deviation or percent changes after the treatment
Total-C total-cholesterol, TG triglycerides, HDL-C high-density lipoprotein-cholesterol, LDL-C low-density lipoprotein-cholesterol, Apo apolipoprotein, RLP-C remant-like particles-cholesterol, sd LDL-C small dense LDL-cholesterol, lb LDL-C large buoyant LDL-cholesterol, HDL2-C high-density lipoprotein 2-cholesterol, HDL3-C high-density lipoprotein 3-cholesterol
ap values for the intragroup comparison (pre vs. post treatment values in dapagliflozin or sitagliptin group, * p < 0.05)
bp values for intergroup comparison (dapagliflozin vs. sitagliptin group in the changes from pre to post treatment, * p < 0.05)
Fig. 1.
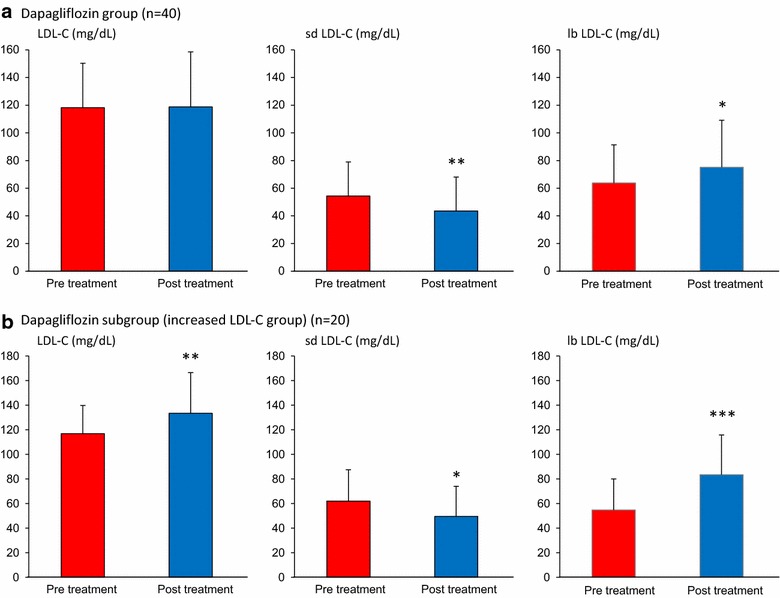
Effects of dapagliflozin on LDL-C and its subspecies. Data are expressed as mean ± standard deviation. LDL-C and its subspecies values in the dapagliflozin group (a) or subgroup whose LDL-C was increased by dapagliflozin treatment (b) were compared between before and after the treatment. *p < 0.05, **p < 0.01, ***p < 0.001 (pre vs. post treatment values). LDL-C low-density lipoprotein-cholesterol, sd LDL-C small dense LDL-cholesterol, lb LDL-C large buoyant LDL-cholesterol
Fig. 2.
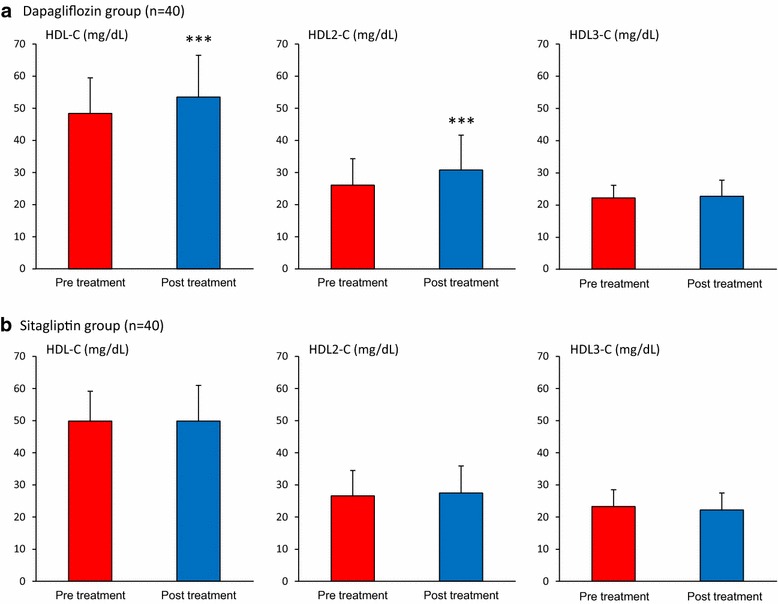
Effects of dapagliflozin and sitagliptin on HDL-C and its subspecies. Data are expressed as mean ± standard deviation. HDL-C and its subspecies values in the dapagliflozin group (a) or sitagliptin group (b) were compared between before and after the treatment. ***p < 0.001 (pre vs. post treatment values). HDL-C high-density lipoprotein-cholesterol, HDL2-C high-density lipoprotein 2-cholesterol, HDL3-C high-density lipoprotein 3-cholesterol
The correlation between the changes in LDL-C subspecies, HDL-C subspecies and changes in clinical and lipid profile after 12 weeks of treatment with either dapagliflozin or sitagliptin was analyzed in Tables 3 and 4, respectively. Dapagliflozin-mediated changes in LDL-C (r = 0.894, p < 0.001) and lb LDL-C (r = 0.665, p < 0.001) correlated with changes in apo B levels, while changes in sd LDL-C was negatively correlated with only changes in lb LDL-C (r = −0.690, p < 0.001). Sitagliptin-mediated changes in LDL-C (r = 0.909, p < 0.001), sd LDL-C (r = 0.467, p < 0.01) and lb LDL-C (r = 0.377, p < 0.05) were correlated with changes in apo B levels. Sitagliptin-mediated changes in sd LDL-C were also correlated with changes in apo CIII level (r = 0.451, p < 0.01).
Table 3.
Correlation between the changes of LDL-C subspecies, HDL-C subspecies and the changes of clinical parameters
| Dapagliflozin | Sitagliptin | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔLDL-C (mg/dL) | Δsd LDL-C (mg/dL) | Δlb LDL-C (mg/dL) | ΔLDL-C (mg/dL) | Δsd LDL-C (mg/dL) | Δlb LDL-C (mg/dL) | |||||||
| r | p | r | p | r | p | r | p | r | p | r | p | |
| ΔBW (kg) | 0.042 | 0.795 | −0.191 | 0.241 | 0.174 | 0.287 | 0.088 | 0.588 | −0.084 | 0.607 | 0.017 | 0.917 |
| ΔHbA1c (%) | 0.109 | 0.506 | −0.118 | 0.472 | 0.168 | 0.305 | 0.217 | 0.190 | −0.025 | 0.088 | 0.280 | 0.087 |
| ΔC-peptide (ng/mL) | 0.208 | 0.229 | 0.130 | 0.455 | 0.055 | 0.750 | 0.516 | 0.023* | −0.133 | 0.586 | 0.648 | 0.002* |
| ΔAST (IU/L) | 0.008 | 0.957 | −0.019 | 0.906 | −0.019 | 0.906 | 0.188 | 0.388 | 0.286 | 0.195 | −0.138 | 0.527 |
| ΔALT (IU/L) | 0.038 | 0.816 | 0.167 | 0.308 | −0.097 | 0.555 | 0.026 | 0.906 | 0.232 | 0.297 | −0.210 | 0.334 |
| ΔγGTP (IU/L) | 0.220 | 0.176 | 0.186 | 0.256 | 0.020 | 0.900 | 0.291 | 0.177 | 0.465 | 0.029* | −0.267 | 0.217 |
| ΔHDL-C (mg/dL) | ΔHDL2-C (mg/dL) | ΔHDL3-C (mg/dL) | ΔHDL-C (mg/dL) | ΔHDL2-C (mg/dL) | ΔHDL3-C (mg/dL) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | r | p | |
| ΔBW (kg) | −0.189 | 0.247 | −0.208 | 0.203 | 0.002 | 0.986 | 0.107 | 0.509 | −0.098 | 0.545 | −0.221 | 0.169 |
| ΔHbA1c (%) | −0.046 | 0.780 | −0.073 | 0.656 | 0.036 | 0.826 | 0.263 | 0.109 | 0.329 | 0.043* | 0.148 | 0.378 |
| ΔC-peptide (ng/mL) | −0.074 | 0.671 | −0.165 | 0.342 | 0.127 | 0.463 | 0.095 | 0.698 | 0.255 | 0.291 | −0.300 | 0.211 |
| ΔAST (IU/L) | 0.220 | 0.178 | 0.220 | 0.177 | 0.029 | 0.860 | −0.394 | 0.062 | −0.347 | 0.104 | 0.072 | 0.742 |
| ΔALT (IU/L) | 0.164 | 0.316 | 0.168 | 0.306 | 0.017 | 0.915 | −0.289 | 0.180 | −0.263 | 0.225 | 0.052 | 0.810 |
| ΔγGTP (IU/L) | 0.197 | 0.227 | 0.153 | 0.350 | 0.095 | 0.563 | 0.201 | 0.570 | −0.180 | 0.395 | 0.222 | 0.308 |
r coefficient of correlation, BW body weight, AST aspartate aminotransferase, ALT alanine aminotransferase, γGTP γ-glutamyltranspeptidase, LDL-C low-density lipoprotein-cholesterol, sd LDL-C small dense LDL-cholesterol, lb LDL-C large buoyant LDL-cholesterol, HDL-C high-density lipoprotein-cholesterol, HDL2-C high-density lipoprotein 2-cholesterol, HDL3-C high-density lipoprotein 3-cholesterol
* p < 0.05
Table 4.
Correlation between the changes of LDL-C subspecies, HDL-C subspecies and the changes of lipid parameters
| Dapagliflozin | Sitagliptin | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔLDL-C (mg/dL) | Δsd LDL-C (mg/dL) | Δlb LDL-C (mg/dL) | ΔLDL-C (mg/dL) | Δsd LDL-C (mg/dL) | Δlb LDL-C (mg/dL) | |||||||
| r | p | r | p | r | p | r | p | r | p | r | p | |
| ΔTG (mg/dL) | 0.085 | 0.604 | 0.008 | 0.959 | 0.055 | 0.736 | 0.125 | 0.430 | 0.155 | 0.345 | −0.009 | 0.953 |
| ΔLDL-C (mg/dL) | 0.080 | 0.625 | 0.665 | <0.001* | 0.425 | 0.006* | 0.507 | 0.001* | ||||
| Δsd LDL-C (mg/dL) | 0.080 | 0.625 | −0.690 | <0.001* | 0.425 | 0.006* | −0.324 | 0.043* | ||||
| Δlb LDL-C (mg/dL) | 0.665 | <0.001* | −0.690 | <0.001* | 0.507 | 0.001* | −0.324 | 0.043* | ||||
| Δapo AI (mg/dL) | 0.320 | 0.046* | 0.280 | 0.084 | 0.022 | 0.890 | 0.301 | 0.073 | 0.044 | 0.795 | 0.013 | 0.938 |
| Δapo AII (mg/dL) | 0.466 | 0.002* | 0.270 | 0.095 | 0.135 | 0.410 | 0.584 | <0.001* | 0.241 | 0.150 | 0.198 | 0.238 |
| Δapo B (mg/dL) | 0.894 | <0.001* | 0.078 | 0.639 | 0.592 | <0.001* | 0.909 | <0.001* | 0.467 | 0.003* | 0.377 | 0.021* |
| Δapo CIII (mg/dL) | 0.316 | 0.049 | 0.247 | 0.128 | 0.044 | 0.787 | 0.287 | 0.084 | 0.451 | 0.005* | −0.135 | 0.422 |
| ΔHDL-C (mg/dL) | ΔHDL2-C (mg/dL) | ΔHDL3-C (mg/dL) | ΔHDL-C (mg/dL) | ΔHDL2-C (mg/dL) | ΔHDL3-C (mg/dL) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | r | p | |
| ΔTG (mg/dL) | −0.156 | 0.341 | −0.125 | 0.446 | −0.069 | 0.674 | −0.176 | 0.277 | −0.074 | 0.646 | −0.228 | 0.155 |
| ΔLDL-C (mg/dL) | 0.295 | 0.067 | 0.167 | 0.306 | 0.239 | 0.142 | 0.555 | <0.001* | 0.254 | 0.113 | 0.307 | 0.053 |
| Δsd LDL-C (mg/dL) | 0.183 | 0.262 | −0.066 | 0.688 | 0.411 | 0.009* | 0.192 | 0.240 | −0.036 | 0.825 | 0.392 | 0.013* |
| Δlb LDL-C (mg/dL) | 0.760 | 0.641 | 0.171 | 0.297 | −0.134 | 0.413 | 0.288 | 0.071 | 0.561 | <0.001* | 0.307 | 0.053 |
| Δapo AI (mg/dL) | 0.890 | <0.001* | 0.697 | <0.001* | 0.450 | 0.004* | 0.808 | <0.001* | 0.516 | 0.002* | 0.489 | 0.003* |
| Δapo AII (mg/dL) | 0.647 | <0.001* | 0.394 | 0.012* | 0.500 | 0.001* | 0.633 | <0.001* | 0.354 | 0.034* | 0.446 | 0.007* |
| ΔapoB (mg/dL) | 0.283 | 0.080 | 0.240 | 0.141 | 0.105 | 0.522 | 0.368 | 0.019* | 0.135 | 0.406 | 0.230 | 0.153 |
| ΔapoCIII (mg/dL) | 0.309 | 0.055 | 0.234 | 0.149 | 0.156 | 0.340 | 0.132 | 0.415 | 0.026 | 0.871 | 0.100 | 0.538 |
r coefficient of correlation, TG triglycerides, LDL-C low-density lipoprotein-cholesterol, sd LDL-C small dense LDL-cholesterol, lb LDL-C large buoyant LDL-cholesterol, Apo apolipoprotein, HDL-C high-density lipoprotein-cholesterol, HDL2-C high-density lipoprotein 2-cholesterol, HDL3-C high-density lipoprotein 3-cholesterol
* p < 0.05
Dapagliflozin-mediated changes in HDL-C and HDL2-C were significantly correlated with changes in apo AI and apo AII levels (p < 0.05). Sitagliptin-mediated changes in HDL-C was correlated with change in LDL-C (r = 0.555, p < 0.001), apo B (r = 0.368, p < 0.05), apo AI (r = 0.808, p < 0.001) and apo AII concentrations (r = 0.633, p < 0.001). Sitagliptin-mediated changes in HDL2-C concentrations were significantly correlated with changes in HbA1c (r = 0.329, p < 0.05) and lb LDL-C (r = 0.561, p < 0.001) (Tables 3 and 4).
Tables 5 and 6 lists the general characteristics and blood lipid levels associated with dapagliflozin use in patients, stratified according to ΔLDL-C (> 0 vs. ≤ 0 mg/dL). In the increased LDL-C subgroup in which LDL-C concentrations increased by 14% (p < 0.01), sd LDL-C decreased significantly (20%, p < 0.05), while lb LDL-C concentrations increased significantly by 53% (p < 0.001) (Fig. 1b). In the decreased LDL-C subgroup in which LDL-C concentrations decreased, both sd LDL-C and lb LDL-C levels decreased significantly by 19 and 10%, respectively (p < 0.05). We compared baseline parameters between the increased LDL-C and the decreased LDL-C groups. In the increased LDL-C group, ages were significantly younger, baseline TG and sd LDL-C levels were significantly higher, and baseline apo AI, HDL2-C and lb LDL-C levels were significantly lower than the decreased LDL-C group (p < 0.05) (Tables 5 and 6).
Table 5.
Clinical parameters with dapagliflozin in increased LDL-C and decreased LDL-C subgroup
| Increased LDL-C group (n = 20) | Decreased LDL-C group (n = 20) | p valuesb | p valuesc | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre treatment | Post treatment | % change | p valuesa | Pre treatment | Post treatment | % change | p valuesa | |||
| Age (years) | 51.6 ± 8.2 | 56.9 ± 7.8 | 0.047* | |||||||
| BW (kg) | 78.8 ± 14.3 | 76.8 ± 15.4 | −2.5 | 0.002* | 78.0 ± 14.7 | 75.5 ± 14.5 | −3.2 | 0.001* | 0.853 | 0.394 |
| AST (IU/L) | 36.1 ± 22.3 | 29.4 ± 15.9 | −18.6 | <0.001* | 32.7 ± 16.3 | 24.1 ± 7.7 | −26.3 | 0.002* | 0.596 | 0.622 |
| ALT (IU/L) | 52.5 ± 46.1 | 39.9 ± 31.9 | −24.0 | 0.032* | 40.4 ± 23.6 | 26.7 ± 11.7 | −33.9 | 0.030* | 0.312 | 0.874 |
| γGTP (IU/L) | 51.0 ± 40.5 | 50.3 ± 62.6 | −1.4 | 0.930 | 55.5 ± 46.5 | 34.0 ± 20.4 | −38.7 | 0.030* | 0.750 | 0.119 |
| BUN (mg/dL) | 14.1 ± 3.8 | 16.3 ± 4.3 | 15.6 | 0.013* | 15.1 ± 4.9 | 17.3 ± 5.8 | 14.6 | 0.010* | 0.470 | 0.996 |
| Cre (mg/dL) | 0.71 ± 0.15 | 0.72 ± 0.17 | 1.4 | 0.700 | 0.72 ± 0.19 | 0.77 ± 0.29 | 6.9 | 0.170 | 0.964 | 0.258 |
| eGFR (mL/min/1.73 m2) | 89.0 ± 18.8 | 88.0 ± 17.6 | −1.1 | 0.661 | 83.3 ± 18.1 | 81.7 ± 22.1 | −1.9 | 0.507 | 0.342 | 0.861 |
| FPG (mg/dL) | 152 ± 46 | 127 ± 27 | −16.4 | 0.006* | 138 ± 50.1 | 116 ± 21 | −15.9 | 0.040* | 0.382 | 0.815 |
| HbA1c (%) | 7.51 ± 1.1 | 6.92 ± 0.94 | −7.9 | 0.002* | 7.72 ± 1.1 | 6.81 ± 0.67 | −11.8 | <0.001* | 0.575 | 0.225 |
| CPR index | 2.77 ± 15.2 | 2.35 ± 1.28 | −15.2 | 0.008* | 2.82 ± 1.28 | 2.44 ± 1.82 | −13.4 | 0.243 | 0.922 | 0.486 |
| Adiponectin (ng/mL) | 5.5 ± 3.8 | 7.2 ± 5.4 | 30.9 | 0.002* | 6.5 ± 2.8 | 8.0 ± 2.6 | 23.1 | 0.001* | 0.383 | 0.675 |
Data are expressed as mean ± standard deviation or percent changes after the treatment. Clinical and laboratory parameters in the subgroup whose LDL-C was increased or decreased by dapagliflozin treatment were analyzed
BW body weight, AST aspartate aminotransferase, ALT alanine aminotransferase, γGTP γ-glutamyltranspeptidase, BUN blood urea nitrogen, Cre creatinine, FPG fasting plasma glucose, LDL-C low-density lipoprotein-cholesterol
ap values for the intragroup comparison (pre vs. post treatment values in each subgroup, * p < 0.05)
bp values for intergroup comparison (increased LDL-C vs. decreased LDL-C group in the pre treatment values, * p < 0.05)
cp values for intergroup comparison (increased LDL-C vs. decreased LDL-C group in the changes from pre to post treatment, * p < 0.05)
Table 6.
Lipid parameters with dapagliflozin in increased LDL-C and decreased LDL-C subgroup
| Increased LDL-C group (n = 20) | Decreased LDL-C group (n = 20) | p valuesb | p valuesc | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre treatment | Post treatment | % change | p valuesa | Pre treatment | Post treatment | % change | p valuesa | |||
| Total-C (mg/dL) | 188.9 ± 31.3 | 211.4 ± 43.1 | 11.9 | <0.001* | 198.4 ± 41.8 | 184.8 ± 45.8 | −6.9 | 0.002* | 0.428 | <0.0001* |
| TG (mg/dL) | 161.3 ± 69.5 | 151.6 ± 89.4 | −6.0 | 0.440 | 123.0 ± 51.8 | 114.8 ± 54.6 | −6.7 | 0.360 | 0.029* | 0.920 |
| HDL-C (mg/dL) | 45.4 ± 8.5 | 52.0 ± 9.7 | 14.5 | 0.001* | 51.5 ± 12.7 | 55.1 ± 16.0 | 7.0 | 0.070 | 0.082 | 0.242 |
| LDL-C (mg/dL) | 116.8 ± 23.0 | 133.4 ± 33.1 | 14.2 | 0.002* | 119.8 ± 40.1 | 103.5 ± 41.0 | −13.6 | <0.001* | 0.771 | <0.0001* |
| Apo AI (mg/dL) | 126.1 ± 17.8 | 140.4 ± 18.4 | 11.3 | <0.001* | 141.4 ± 22.9 | 146.8 ± 26.4 | 3.8 | 0.230 | 0.025* | 0.145 |
| Apo AII (mg/dL) | 29.5 ± 4.8 | 32.3 ± 5.1 | 9.5 | <0.001* | 29.9 ± 4.3 | 29.5 ± 4.6 | −1.3 | 0.530 | 0.798 | 0.001* |
| Apo B (mg/dL) | 100.9 ± 17.6 | 111.8 ± 22.3 | 10.8 | <0.001* | 99.3 ± 30.0 | 85.0 ± 34.7 | −14.4 | 0.014* | 0.846 | <0.0001* |
| Apo CII (mg/dL) | 4.8 ± 1.8 | 5.4 ± 2.5 | 12.5 | 0.057 | 4.7 ± 1.6 | 4.5 ± 1.8 | −4.3 | 0.270 | 0.855 | 0.029* |
| Apo CIII (mg/dL) | 10.7 ± 3.6 | 12.0 ± 4.8 | 12.1 | 0.035* | 10.2 ± 2.8 | 10.7 ± 3.8 | 4.9 | 0.340 | 0.698 | 0.240 |
| Apo E (mg/dL) | 4.3 ± 1.1 | 4.6 ± 1.7 | 7.0 | 0.280 | 4.4 ± 1.2 | 4.3 ± 1.3 | −2.3 | 0.420 | 0.904 | 0.193 |
| RLP-C (mg/dL) | 7.6 ± 5.0 | 7.8 ± 2.5 | 2.6 | 0.870 | 5.7 ± 3.3 | 5.0 ± 3.3 | −12.3 | 0.090 | 0.136 | 0.809 |
| HDL2-C (mg/dL) | 23.5 ± 5.1 | 29.1 ± 7.8 | 23.8 | <0.001* | 28.8 ± 10.03 | 32.5 ± 13.3 | 12.8 | 0.080 | 0.043* | 0.437 |
| HDL3-C (mg/dL) | 21.8 ± 4.0 | 22.8 ± 4.9 | 4.6 | 0.410 | 22.6 ± 3.6 | 22.5 ± 5.2 | −0.4 | 0.890 | 0.476 | 0.450 |
| sd LDL-C (mg/dL) | 62.0 ± 25.5 | 49.5 ± 24.5 | −20.2 | 0.048* | 46.3 ± 21.4 | 37.3 ± 23.2 | −19.4 | 0.015* | 0.046* | 0.655 |
| lb LDL-C (mg/dL) | 54.7 ± 25.3 | 83.5 ± 32.3 | 52.7 | <0.001* | 73.4 ± 27.3 | 66.1 ± 34.4 | −9.9 | 0.010* | 0.033* | <0.0001* |
| sd LDL-C/LDL-C | 0.53 ± 0.18 | 0.37 ± 0.17 | −30.2 | 0.003* | 0.38 ± 0.00 | 0.35 ± 0.17 | −7.9 | 0.250 | 0.005* | 0.021* |
Data are expressed as mean ± standard deviation or percent changes after the treatment. Clinical and laboratory parameters in the subgroup whose LDL-C was increased or decreased by dapagliflozin treatment were analyzed
Total-C total-cholesterol, TG triglycerides, HDL-C high-density lipoprotein-cholesterol, LDL-C low-density lipoprotein-cholesterol, Apo apolipoprotein, RLP-C remant-like particles-cholesterol, HDL2-C high-density lipoprotein 2-cholesterol, HDL3-C high-density lipoprotein 3-cholesterol, sd LDL-C small dense LDL-cholesterol, lb LDL-C large buoyant LDL-cholesterol
ap values for the intragroup comparison (pre vs. post treatment values in each subgroup, * p < 0.05)
bp values for intergroup comparison (increased LDL-C vs. decreased LDL-C group in the pre treatment values, * p < 0.05)
cp values for intergroup comparison (increased LDL-C vs. decreased LDL-C group in the changes from pre to post treatment, * p < 0.05)
Discussion
Changes in LDL-C and its subspecies after SGLT-2 inhibitor treatment
Several phase III studies of SGLT-2 inhibitors—with larger sample sizes—have demonstrated that SGLT-2 inhibitors elevate LDL-C levels [5, 6]. Increased LDL-C might increase atherogenic risk in patients treated with SGLT-2 inhibitors. Conversely, the majority of studies have demonstrated that SGLT-2 inhibitors reduce TG and increase HDL-C levels, which reduce atherogenic risk [2, 22]. TG-lowering agents, such as fibrates and omega-3 fatty acids, have a tendency to increase LDL-C [23, 24] probably because of reduced lipid transfer between TG-rich lipoprotein (TRL)-TG and LDL-C [25]. Therefore, it is not surprising that reduced levels of TG associated with SGLT-2 inhibitor use resulted in suppressed generation of cholesterol-poor LDL particles. Another possible mechanism for increases in LDL-C concentrations induced by SGLT-2 inhibitors is an amelioration of insulin resistance by reducing body weight and glucose toxicity [1, 2]. Enhanced insulin sensitivity increases lipoprotein lipase activity, stimulating conversion from very-low-density lipoprotein-C to LDL-C [26]. It is of interest that an insulin sensitizer, pioglitazone, increases LDL-C levels by stimulating LDL-C production—most likely because of enhanced lipoprotein lipase activity [27, 28]. Very recently, Briand et al. [29] reported that empagliflozin reduced LDL receptor-mediated LDL clearance by the liver in hamsters fed atherogenic diets. Taken together, the possible mechanisms for increased LDL-C levels are: (1) increased LDL-C production by enhanced lipoprotein lipase activity, (2) suppressed conversion from cholesterol-rich lb LDL-C to cholesterol-poor sd LDL-C, and (3) impaired LDL-C catabolism by reduced LDL receptors.
We did not observe associated increases in LDL-C levels with the use of dapagliflozin treatment in this study. The individuals whose LDL-C levels were elevated after dapagliflozin treatment had higher TG levels than those whose LDL-C levels were declined, suggesting critical role of TG in SGLT2 inhibitor-induced elevation of LDL-C. In addition, there were significantly differences in sd LDL-C, HDL-C, HDL2-C and lb LDL-C levels between the increased LDL-C and decreased LDL-C subgroups. Higher TG, higher sd LDL-C and lower large sized HDL-C levels are usually observed in the patients who have more visceral obesity [30]. It is known that East Asian type 2 diabetes is characterized by generally lesser obesity and higher insulin sensitivity compared with Caucasians [31]. Therefore, our study is not unusual, and a report from Asian country has also shown that SGLT2 inhibitor unchanged LDL-C concentrations [32].
Despite unchanged levels of LDL-C, dapagliflozin markedly decreased the levels of potent atherogenic sd LDL-C and increased levels of the less atherogenic lb LDL-C. Lb LDL-C levels were further elevated in the subset of patients whose LDL-C levels were increased during dapagliflozin treatment. This would be due to decreased LDL-C catabolism in these patients [29]. Our results imply that lb LDL-C is the sole contributor to rising LDL-C levels in patients using SGLT-2 inhibitors. Even though lb LDL-C is less atherogenic than sd LDL-C, an increase in lb LDL-C could increase cardiovascular risk. However, the Quebec Cardiovascular study revealed that increased lb LDL-C was not positive risk factor but, in fact, a negative risk factor for cardiovascular death [33]. We failed to demonstrate a significant association between changes in TG and changes in LDL-C subspecies during dapagliflozin treatment. However, TG levels fluctuate over the course of a day and postprandial TG levels also influence LDL-C size [34]. Thus, it is possible that dapagliflozin suppresses postprandial TG levels, which affect LDL-C subspecies more strongly than fasting TG levels do. Consistent with previous reports [35, 36], dapagliflozin decreased body weight and liver transaminase levels, and increased adiponectin concentrations. Non-alcoholic fatty liver disease (NAFLD) is the most common cause of elevated liver transaminase levels. NAFLD covers a spectrum, ranging from simple stenosis in the absence of inflammation to non-alcoholic steatohepatitis (NASH). Many large population-based studies have convincingly demonstrated that an elevated serum level of liver transaminase, especially ALT, is a common laboratory surrogate marker for NAFLD and NASH [37]. Patients who have NAFLD or NASH with increased concentrations of sd LDL-C [38, 39] and decreased concentrations of adiponectin [40], carry an additional cardiovascular risk. In this study, average liver transaminase levels were significantly decreased after the administration of dapagliflozin. In addition, AST was reduced in 65%, and ALT was reduced in 73% of patients. This suggests that the protective effects of dapagliflozin on atherogenic fatty liver disease including NAFLD or NASH, occurred concomitantly with type 2 diabetes. We failed to observe a significant correlation between changes in clinical parameters and changes in the LDL-C subspecies. A decrease in sd LDL-C mediated by SGLT-2 inhibitors would be involved in multiple ameliorations of insulin resistance, hypertriglyceridemia, and liver steatosis, which synergistically contribute to suppressed generation of this potent atherogenic lipoprotein.
Changes in HDL-C and its subspecies after SGLT-2 inhibitor treatment
It is well documented that SGLT-2 inhibitors increase HDL-C levels [2], but so far no study has explored the changes in HDL-C subspecies. The present study has, for the first time, revealed that dapagliflozin specifically increased HDL2-C without affecting HDL3-C. It remains to be proven which HDL2-C or HDL3-C particles are more atheroprotective. Nevertheless, it is known that, while HDL2-C levels are sensitive to and decreased by increases in plasma TG levels [19], adiposity [41], insulin resistance, and are associated with a low risk for incident of type 2 diabetes [42], HDL3-C levels remain fairly constant. Therefore, HDL2-C inversely reflects metabolic burden leading to the development of atherosclerosis. Selective increases in HDL2-C by dapagliflozin may imply ameliorations of hypertriglyceridemia, overweight and insulin resistance, which are also implicated as possible mechanisms for reduced sd LDL-C concentrations.
Recently, a meta-analysis of 21 phase 2b/3 dapagliflozin clinical trials indicated no increased risk for major adverse cardiovascular events with dapagliflozin [43]. Recent report also indicate that dapagliflozin treatment for up to 104 weeks was well tolerated in older patients [44], who are included in a high-risk population for cardiovascular diseases. Additionally, dapagliflozin treatment was associated with reduction of oxidative stress in patients with type 2 diabetes, which may benefit the cardiovascular system [45]. The favourable or neutral effects of dapagliflozin on the cardiovascular diseases risk found in this study may be associated with blood lipid profiles after dapagliflozin treatment.
Changes in lipid profiles after sitagliptin treatment
We evaluated the effect of a DPP-4 inhibitor, sitagliptin, on plasma lipids and subspecies of LDL-C and HDL-C. Nakamura et al. [46] reported that 25, 50, 100 mg/day of sitagliptin treatment did not change the TG and LDL-C levels. Conversely, the treatment significantly reduced HDL-C levels for 12 months. Our present study showed that sitagliptin exhibited neutral effect on lipids and the subspecies of lipoproteins, which is in keeping with previous reports [47, 48]. Interestingly, Matikainen et al. reported that vildagliptin suppressed postprandial increases in TG [49], and that this suppression was associated with an increase in LDL-C particle diameter [50]. The conflicting result may be in part due to the amount of sitagliptin administrated. We used 50 mg/day of sitagliptin as a standard dose for Japanese patients, while 100 mg/day is the standard dose of sitagliptin in Western countries. Nevertheless, the results obtained from the sitagliptin-treated group may strengthen the validity of the results that dapagliflozin powerfully alters LDL-C and HDL-C subspecies.
Study limitations
Limitations of this study included the small number of study patients and short treatment period. Therefore, further studies are needed to verify the findings in this study.
Conclusions
In conclusion, an SGLT-2 inhibitor, dapagliflozin suppressed potent atherogenic sd LDL-C and increased HDL2-C. Although LDL-C was elevated by treatment with dapagliflozin, this increase was solely attributable to elevations in levels of the less atherogenic lb LDL-C. However, these findings were not observed after treatment with DPP-4 inhibitor, sitagliptin. Therefore, the use of new type of glucose-lowering agent, SGLT-2 inhibitor is unlikely to increase atherogenic risk.
Authors’ contributions
TH and TH developed the study concept and design. TH mainly implemented the study. TH, TF, NN, SY, MT, AO, MO, TY and TH registered the study patients and performed physical examination and medical treatments. YI was responsible for measuring plasma lipid parameters. TH and TH drafted the manuscript. TH performed statistical analyses. TH, TF, NH, MT, AO, MO, TY, YI and TH interpreted data and critically revised and completed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Kyoko Nohtomi and Hiroko Takeuchi for their technical assistance in this study. The authors also thank for the medical writing support provided by Interscience Co., Ltd.
Competing interests
This study was financially supported by AstraZeneca K.K., Astellas Pharma Inc., MSD K.K., and Ono Pharmceutical Co., Ltd, and medical writing support fee was funded from Ono Pharmaceutical Co., Ltd. and AstraZeneca K.K. The author, Y.I. is an employee of Denka Seiken Co., Ltd.
Availability of data and materials
The datasets analyzed during the current study are not publicly available due to some relevant ongoing studies, but may be available from the corresponding authors of this article on reasonable request.
Ethics approval and consent to participate
The study was approved by the institutional review board at Showa University School of Medicine, and written informed consent was obtained from all participating patients before the initiation of the study.
Funding
As indicated above, this study and the medical writing were financially supported by AstraZeneca K.K., Astellas Pharma Inc., MSD K.K., and Ono Pharmceutical Co., Ltd. The funders had no role in this study.
Abbreviations
- SGLT-2
sodium-glucose co-transporter-2
- TG
triglyceride
- HDL-C
high-density lipoprotein-cholesterol
- HDL2-C
high-density lipoprotein 2-cholesterol
- HDL3-C
high-density lipoprotein 3-cholesterol
- LDL-C
low-density lipoprotein-cholesterol
- lb LDL-C
large buoyant low-density lipoprotein-cholesterol
- sd LDL-C
small dense low-density lipoprotein-cholesterol
- DPP-4
dipeptidyl peptidase-4
- RLP-C
remnant-like particle-cholesterol
- AST
aspartate aminotransferase
- ALT
alanine aminotransferase
- apo
apolipoprotein
- TRL-TG
triglyceride-rich lipoprotein- triglyceride
- NASH
non-alcoholic steatohepatitis
- NAFLD
non-alcoholic fatty liver disease
Additional file
Footnotes
Toshiyuki Hayashi and Tsutomu Hirano have equal authorship
Contributor Information
Toshiyuki Hayashi, Phone: +81-3-3784-8947, Email: t-hayashi@med.showa-u.ac.jp.
Tomoyasu Fukui, Email: tomoyasufk@yahoo.co.jp.
Noriko Nakanishi, Email: nori-nnori@hotmail.co.jp.
Saki Yamamoto, Email: sakichakko@gmail.com.
Masako Tomoyasu, Email: goodnews0911@yahoo.co.jp.
Anna Osamura, Email: annatoku@gmail.com.
Makoto Ohara, Email: s6018@nms.ac.jp.
Takeshi Yamamoto, Email: tak3105@aol.com.
Yasuki Ito, Email: y_ito@denka-seiken.co.jp.
Tsutomu Hirano, Phone: +81-3-3784-8947, Email: hirano@med.showa-u.ac.jp.
References
- 1.Scheen AJ. Pharmacodynamics, efficacy and safety of sodium-glucose co-transporter type 2 (SGLT2) inhibitors for the treatment of type 2 diabetes mellitus. Drugs. 2015;75:33–59. doi: 10.1007/s40265-014-0337-y. [DOI] [PubMed] [Google Scholar]
- 2.Inzucchi SE, Zinman B, Wanner C, Ferrari R, Fitchett D, Hantel S, Espadero RM, Woerle HJ, Broedl UC, Johansen OE. SGLT-2 inhibitors and cardiovascular risk: proposed pathways and review of ongoing outcome trials. Diab Vasc Dis Res. 2015;12:90–100. doi: 10.1177/1479164114559852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fioretto P, Giaccari A, Sesti G. Efficacy and safety of dapagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, in diabetes mellitus. Cardiovasc Diabetol. 2015;14:142. doi: 10.1186/s12933-015-0297-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 5.Ptaszynska A, Hardy E, Johnsson E, Parikh S, List J. Effects of dapagliflozin on cardiovascular risk factors. Postgrad Med. 2013;125:181–189. doi: 10.3810/pgm.2013.05.2667. [DOI] [PubMed] [Google Scholar]
- 6.Hach T, Gerich J, Salsali A, Kim G, Hantel S, Woerle H, Broedl UC. Empagliflozin improves glycemic parameters and cardiovascular risk factors in patients with type 2 diabetes (T2DM): pooled data from four pivotal phase III trials. Diabetologie und Stoffwechsel. 2014;9:p142. doi: 10.1055/s-0034-1374999. [DOI] [Google Scholar]
- 7.Turner RC, Millns H, Neil HA, Stratton IM, Manley SE, Matthews DR, Holman RR. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23) BMJ. 1998;316:823–828. doi: 10.1136/bmj.316.7134.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Araki A, Iimuro S, Sakurai T, Umegaki H, Iijima K, Nakano H, Oba K, Yokono K, Sone H, Yamada N, Japanese Elderly Intervention Trial Research Group Non-high-density lipoprotein cholesterol: an important predictor of stroke and diabetes-related mortality in Japanese elderly diabetic patients. Geriatr Gerontol In. 2012;12:18–28. doi: 10.1111/j.1447-0594.2011.00809.x. [DOI] [PubMed] [Google Scholar]
- 9.Austin MA, Breslow JL, Hennekens CH, Buring JE, Willett WC, Krauss RM. Low-density lipoprotein subclass patterns and risk of myocardial infarction. JAMA. 1988;260:1917–1921. doi: 10.1001/jama.1988.03410130125037. [DOI] [PubMed] [Google Scholar]
- 10.Griffin BA. Lipoprotein atherogenicity: an overview of current mechanisms. Proc Nutr Soc. 1999;58:163–169. doi: 10.1079/PNS19990022. [DOI] [PubMed] [Google Scholar]
- 11.Boizel R, Benhamou PY, Lardy B, Laporte F, Foulon T, Halimi S. Ratio of triglycerides to HDL cholesterol is an indicator of LDL particle size in patients with type 2 diabetes and normal HDL cholesterol levels. Diabetes Care. 2000;23:1679–1685. doi: 10.2337/diacare.23.11.1679. [DOI] [PubMed] [Google Scholar]
- 12.Duez H, Lamarche B, Uffelman KD, Valero R, Cohn JS, Lewis GF. Hyperinsulinemia is associated with increased production rate of intestinal apolipoprotein B-48-containing lipoproteins in humans. Arterioscler Thromb Vasc Biol. 2006;26:1357–1363. doi: 10.1161/01.ATV.0000222015.76038.14. [DOI] [PubMed] [Google Scholar]
- 13.Kathiresan S, Otvos JD, Sullivan LM, Keyes MJ, Schaefer EJ, Wilson PW, D’Agostino RB, Vasan RS, Robins SJ. Increased small low-density lipoprotein particle number: a prominent feature of the metabolic syndrome in the Framingham Heart Study. Circulation. 2006;113:20–29. doi: 10.1161/CIRCULATIONAHA.105.567107. [DOI] [PubMed] [Google Scholar]
- 14.Krauss RM. Lipids and lipoproteins in patients with type 2 diabetes. Diabetes Care. 2004;27:1496–1504. doi: 10.2337/diacare.27.6.1496. [DOI] [PubMed] [Google Scholar]
- 15.Ito Y, Fujimura M, Ohta M, Hirano T. Development of a homogeneous assay for measurement of small dense LDL cholesterol. Clin Chem. 2011;57:57–65. doi: 10.1373/clinchem.2010.149559. [DOI] [PubMed] [Google Scholar]
- 16.Arai H, Kokubo Y, Watanabe M, Sawamura T, Ito Y, Minagawa A, Okamura T, Miyamato Y. Small dense low-density lipoproteins cholesterol can predict incident cardiovascular disease in an urban Japanese cohort: the suita study. J Atheroscler Thromb. 2013;20:195–203. doi: 10.5551/jat.14936. [DOI] [PubMed] [Google Scholar]
- 17.Tsai MY, Steffen BT, Guan W, McClelland RL, Warnick R, McConnell J, Hoefner DM, Remaley AT. New automated assay of small dense low-density lipoprotein cholesterol identifies risk of coronary heart disease: the multi-ethnic Study of atherosclerosis. Arterioscler Thromb Vasc Biol. 2014;34:196–201. doi: 10.1161/ATVBAHA.113.302401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoogeveen RC, Gaubatz JW, Sun W, Dodge RC, Crosby JR, Jiang J, Couper D, Virani SS, Kathiresan S, Boerwinkle E. Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: the atherosclerosis risk in communities (ARIC) study. Arterioscler Thromb Vasc Biol. 2014;34:1069–1077. doi: 10.1161/ATVBAHA.114.303284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calabresi L, Franceschini G, Sirtori M, Gianfranceschi G, Werba P, Sirtori CR. Influence of serum triglycerides on the HDL pattern in normal subjects and patients with coronary artery disease. Atherosclerosis. 1990;84:41–48. doi: 10.1016/0021-9150(90)90006-5. [DOI] [PubMed] [Google Scholar]
- 20.Ito Y, Satoh N, Ishii T, Kumakura J, Hirano T. Development of a homogeneous assay for measurement of high-density lipoprotein-subclass cholesterol. Clin Chim Acta. 2014;427:86–93. doi: 10.1016/j.cca.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Ashmaig M, Gupta S, McConnell JP, Warnick GR. Valiation of a novel homogenous assay for HDL3-C maeasurement. Clin Chim Acta. 2013;425:37–41. doi: 10.1016/j.cca.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Nauck MA. Update on developments with SGLT2 inhibitors in the management of type 2 diabetes. Drug Des Devel Ther. 2014;8:1335–1380. doi: 10.2147/DDDT.S50773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirose T, Teramoto T, Abe K, Taneyama T, J-BENEFIT study group Determinant of bezafibrate-induced improvements in LDL cholesterol in dyslipidemic patients with diabetes. J Atheroscler Thromb. 2015;22:676–684. doi: 10.5551/jat.27425. [DOI] [PubMed] [Google Scholar]
- 24.von Schacky C. A review of omega-3 ethyl esters for cardiovascular prevention and treatment of increased blood triglyceride levels. Vasc Health Risk Manag. 2006;2:251–262. doi: 10.2147/vhrm.2006.2.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43:1363–1379. doi: 10.1194/jlr.R200004-JLR200. [DOI] [PubMed] [Google Scholar]
- 26.Annuzzi G, De Natale C, Iovine C, Patti L, Di Marino L, Coppola S, Del Prato S, Riccardi G, Rivellese AA. Insulin resistance is independently associated with postprandial alterations of triglyceride-rich lipoproteins in type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol. 2004;24:2397–2402. doi: 10.1161/01.ATV.0000146267.71816.30. [DOI] [PubMed] [Google Scholar]
- 27.Schernthaner G, Matthews DR, Charbonnel B, Hanefeld M, Brunetti P, Quartet [corrected] Study Group Efficacy and safety of pioglitazone versus metformin in patients with type 2 diabetes mellitus: a double-blind, randomized trial. J Clin Endocrinol Metab. 2004;89:6068–6076. doi: 10.1210/jc.2003-030861. [DOI] [PubMed] [Google Scholar]
- 28.Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefèbvre PJ, Murray GD, PROactive Investigators et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366:1279–1289. doi: 10.1016/S0140-6736(05)67528-9. [DOI] [PubMed] [Google Scholar]
- 29.Briand F, Mayoux E, Brousseau E, Burr N, Urbain I, Costard C, Mark M, Sulpice T. Empagliflozin, via switching metabolism towards lipid utilization, moderately increases LDL-cholesterol levels through reduced LDL catabolism. Diabetes. 2016;65:2032–2038. doi: 10.2337/db16-0049. [DOI] [PubMed] [Google Scholar]
- 30.Okazaki M, Usui S, Ishigami M, Sakai N, Nakamura T, Matsuzawa Y, Yamashita S. Identification of unique lipoprotein subclasses for visceral obesity by component analysis of cholesterol profile in high-performance liquid chromatography. Arterioscler Thromb Vasc Biol. 2005;25:578–584. doi: 10.1161/01.ATV.0000155017.60171.88. [DOI] [PubMed] [Google Scholar]
- 31.Yabe D, Seino Y, Fukushima M, Seino S. β cell dysfunction versus insulin resistance in the pathogenesis of type 2 diabetes in East Asians. Curr Diab Rep. 2015;15:602. doi: 10.1007/s11892-015-0602-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaku K, Kiyosue A, Inoue S, Ueda N, Tokudome T, Yang J, Langkilde AM. Efficacy and safety of dapagliflozin monotherapy in Japanese patients with type 2 diabetes inadequately controlled by diet and exercise. Diabetes Obes Metab. 2014;16:1102–1110. doi: 10.1111/dom.12325. [DOI] [PubMed] [Google Scholar]
- 33.St-Pierre AC, Cantin B, Dagenais GR, Mauriège P, Bernard PM, Després JP, Lamarche B. Low-density lipoprotein subfractions and the long-term risk of ischemic heart disease in men, 13-year follow-up data from the Québec cardiovascular study. Arterioscler Thromb Vasc Biol. 2005;25:553–559. doi: 10.1161/01.ATV.0000154144.73236.f4. [DOI] [PubMed] [Google Scholar]
- 34.Tsunoda F, Koba S, Hirano T, Ban Y, Iso Y, Suzuki H, Geshi E, Katagiri T. Association between small dense low-density lipoprotein and postprandial accumulation of triglyceride-rich remnant-like particles in normotriglyceridemic patients with myocardial infarction. Circ J. 2004;68:1165–1172. doi: 10.1253/circj.68.1165. [DOI] [PubMed] [Google Scholar]
- 35.Bolinder J, Ljunggren Ö, Kullberg J, Johansson L, Wilding J, Langkilde AM, Sugg J, Parikh S. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab. 2012;97:1020–1031. doi: 10.1210/jc.2011-2260. [DOI] [PubMed] [Google Scholar]
- 36.Wilding JP, Woo V, Soler NG, Pahor A, Sugg J, Rohwedder K, Parikh S, Dapagliflozin 006 Study Group Long-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial. Ann Intern Med. 2012;156:405–415. doi: 10.7326/0003-4819-156-6-201203200-00003. [DOI] [PubMed] [Google Scholar]
- 37.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 38.Siddiqui MS, Sterling RK, Luketic VA, Puri P, Stravitz RT, Bouneva I, Boyett S, Fuchs M, Sargeant C, Warnick GR, et al. Association between high-normal levels of alanine aminotransferase and risk factors for atherogenesis. Gastroenterology. 2013;145(6):1271–1279. doi: 10.1053/j.gastro.2013.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Siddiqui MS, Fuchs M, Idowu MO, Luketic VA, Boyett S, Sargeant C, Stravitz RT, Puri P, Matherly S, Sterling RK, et al. Severity of nonalcoholic fatty liver disease and progression to cirrhosis are associated with atherogenic lipoprotein profile. Clin Gastroenterol Hepatol. 2015;13(5):1000–1008. doi: 10.1016/j.cgh.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Musso G, Gambino R, Durazzo M, Biroli G, Carello M, Fagà E, Pacini G, De Michieli F, Rabbione L, Premoli A, et al. Adipokines in NASH: postprandial lipid metabolism as a link between adiponectin and liver disease. Hepatology. 2005;42(5):1175–1183. doi: 10.1002/hep.20896. [DOI] [PubMed] [Google Scholar]
- 41.Ostlund RE, Jr, Staten M, Kohrt WM, Schultz J, Malley M. The ratio of waist-to-hip circumference, plasma insulin level, and glucose intolerance as independent predictors of the HDL2 cholesterol level in older adults. N Engl J Med. 1990;322:229–234. doi: 10.1056/NEJM199001253220404. [DOI] [PubMed] [Google Scholar]
- 42.Hwang YC, Hayashi T, Fujimoto WY, Kahn SE, Leonetti DL, McNeely MJ, Boyko EJ. Differential association between HDL subclass and the development of type 2 diabetes in prospective study of Japanese Americans. Diabetes Care. 2015;38:2100–2105. doi: 10.2337/dc15-0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sonesson C, Johansson PA, Johnsson E, Gause-Nilsson I. Cardiovascular effects of dapagliflozin in patients with type 2 diabetes and different risk categories: a meta-analysis. Cardiovasc Diabetol. 2016;15:37. doi: 10.1186/s12933-016-0356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fioretto P, Mansfield TA, Ptaszynska A, Yavin Y, Johnsson E, Parikh S. Long-term safety of dapagliflozin in older patients with type 2 diabetes mellitus: a pooled analysis of phase IIb/III studies. Drugs Aging. 2016;33(7):511–522. doi: 10.1007/s40266-016-0382-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li FF, Gao G, Li Q, Zhu HH, Su XF, Wu JD, Ye L, Ma JH. Influence of dapagliflozin on glycemic variations in patients with newly diagnosed type 2 diabetes mellitus. J Diabetes Res. 2016. [DOI] [PMC free article] [PubMed]
- 46.Nakamura T, Iwanaga Y, Miyaji Y, Nohara R, Ishimura T, Miyazaki S, Sitagliptin Registry Kinki Cardiologists’ Study (SIRKAS) Investigators Cardiovascular efficacy of sitagliptin in patients with diabetes at high risk of cardiovascular disease: a 12-month follow-up. Cardiovasc Diabetol. 2016;15:54. doi: 10.1186/s12933-016-0371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Horton ES, Silberman C, Davis KL, Berria R. Weight loss, glycemic control, and changes in cardiovascular biomarkers in patients with type 2 diabetes receiving incretin therapies or insulin in a large cohort database. Diabetes Care. 2010;33(8):1759–1765. doi: 10.2337/dc09-2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Monami M, Vitale V, Ambrosio ML, Bartoli N, Toffanello G, Ragghianti B, Monami F, Marchionni N, Mannucci E. Effects on lipid profile of dipeptidyl peptidase 4 inhibitors, pioglitazone, acarbose, and sulfonylureas: meta-analysis of placebo-controled trials. Adv Ther. 2012;29:736–746. doi: 10.1007/s12325-012-0045-5. [DOI] [PubMed] [Google Scholar]
- 49.Matikainen N, Mänttäri S, Schweizer A, Ulvestad A, Mills D, Dunning BE, Foley JE, Taskinen MR. Vildagliptin therapy reduces postprandial intestinal triglyceride-rich lipoprotein particles in patients with type 2 diabetes. Diabetologia. 2006;49:2049–2057. doi: 10.1007/s00125-006-0340-2. [DOI] [PubMed] [Google Scholar]
- 50.Matikainen N, Taskinen MR. The effect of vildagliptin therapy on atherogenic postprandial remnant particles and LDL particle size in subjects with type 2 diabetes. Diabet Med. 2013;30:756–757. doi: 10.1111/dme.12094. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are not publicly available due to some relevant ongoing studies, but may be available from the corresponding authors of this article on reasonable request.


