Abstract
Background
To improve the quality of antimicrobial stewardship (AMS) interventions the application of behavioural sciences supported by multidisciplinary collaboration has been recommended. We analysed major UK scientific research conferences to investigate AMS behaviour change intervention reporting.
Methods
Leading UK 2015 scientific conference abstracts for 30 clinical specialties were identified and interrogated. All AMS and/or antimicrobial resistance(AMR) abstracts were identified using validated search criteria. Abstracts were independently reviewed by four researchers with reported behavioural interventions classified using a behaviour change taxonomy.
Results
Conferences ran for 110 days with >57,000 delegates. 311/12,313(2.5%) AMS-AMR abstracts (oral and poster) were identified. 118/311(40%) were presented at the UK’s infectious diseases/microbiology conference. 56/311(18%) AMS-AMR abstracts described behaviour change interventions. These were identified across 12/30(40%) conferences. The commonest abstract reporting behaviour change interventions were quality improvement projects [44/56 (79%)]. In total 71 unique behaviour change functions were identified. Policy categories; “guidelines” (16/71) and “service provision” (11/71) were the most frequently reported. Intervention functions; “education” (6/71), “persuasion” (7/71), and “enablement” (9/71) were also common. Only infection and primary care conferences reported studies that contained multiple behaviour change interventions. The remaining 10 specialties tended to report a narrow range of interventions focusing on “guidelines” and “enablement”.
Conclusion
Despite the benefits of behaviour change interventions on antimicrobial prescribing, very few AMS-AMR studies reported implementing them in 2015. AMS interventions must focus on promoting behaviour change towards antimicrobial prescribing. Greater focus must be placed on non-infection specialties to engage with the issue of behaviour change towards antimicrobial use.
Electronic supplementary material
The online version of this article (doi:10.1186/s13756-017-0170-7) contains supplementary material, which is available to authorized users.
Keywords: Antimicrobial Resistance, Stewardship, Quality improvement, Cross-specialty, Infection
Background
In the United Kingdom (UK), about one third of all hospital inpatients receive antimicrobials during their admission with a significant proportion of these identified as inappropriate [1–3]. This accounts for a large amount of unnecessary antimicrobial exposure. Antimicrobial resistance (AMR) is a leading patient safety issue that requires urgent interventions to curb its exponential growth. One target of interventions to address the problem of AMR is the promotion of the appropriate use of antimicrobials in humans, which is thought to be a leading driver for the growth of AMR [4].
To address this and promote the appropriate use of antimicrobial agents a number of national and international antimicrobial stewardship (AMS) initiatives have been implemented [5–8]. A key facet of these interventions targets improving and sustaining individual prescribing behaviours. Implementation of AMS programmes have been demonstrated to reduce rates of AMR and improve health and economic outcomes [9–11]. However, despite these positive steps forward, several challenges appear to remain in promoting the sustainable use of antimicrobials across clinical practice [12].
Firstly, there is a growing body of evidence to describe the cultural and social factors that influence antimicrobial prescribing across healthcare settings as well as qualitative data that supports the role of behaviour change interventions in improving antimicrobial prescribing [13–16]. Despite this, very little evidence exists to describe the current landscape of behaviour change interventions being implemented within this field [12, 13, 15–20]. Secondly, despite evidence to support engagement of infection specialists with the AMS-AMR agenda, there appears to be poorer engagement across other clinical specialties in terms of formal training and awareness at state-of-the-art scientific conferences [21–23]. Finally, although there are described frameworks and taxonomy’s available from which to begin mapping behaviour change methods [24, 25], very little data is currently available to describe the appropriateness of these specifically for AMS interventions.
In this cross-sectional study we aimed to explore antimicrobial stewardship interventions reported at major cross specialty UK state-of-the-art scientific conferences in 2015, which contained behaviour change interventions. We aimed to determine the number and type of behaviour change interventions reported by different specialties and compare these to currently available behaviour change taxonomies to identify potential gaps and highlight potential targets for future interventions.
Methods
Abstract identification & screening
All major medical specialties recognised by the Royal College of Physicians, London, UK, were identified and included alongside major surgical specialties identified by the intercollegiate surgical curriculum programme. Psychiatric, paediatric, and obstetrics and gynaecology specialties were also included. UK specialists (specialist trainees or consultants) in each of the defined fields were consulted by email to determine the largest clinical scientific/research conference within the UK in 2015. Two specialists from each field, who were based in the North West London area were contacted for their opinions. Where there was disagreement, the authors opted for the conference with the largest attendance. Educational, continuing professional development and sub-specialty conferences were not considered for inclusion given their often focused agendas, which may have biased our findings.
Each major conference per specialty was identified and abstract booklets extracted and interrogated. Conference characteristics collated included; location, conference dates, estimated attendance and total number of abstracts accepted (either as oral, poster or publication only). Accepted conference abstracts (invited, oral, poster and publication only) were then identified and interrogated using a previously validated search criterion to identify all abstracts relating to AMS and AMR. [21, 22] All identified oral, poster, or published only abstracts from the search were then anonymously reviewed by two out of three authors (TMR, AMT, & AT). Abstracts were included if they were deemed to be describing an aspect of AMS [26] or AMR [27] in terms of direct effect on patients. In vitro studies with no translational benefit to individual patients were excluded. For the purpose of our investigation we focused on bacterial resistance and stewardship, abstracts relating solely to antiviral, antifungal, antiprotozoal or antimycobacterial resistance were excluded. This focus was selected given that anti-bacterial agents make up over 93% of all antimicrobials prescribed for systemic use [28]. Furthermore, the large variation in prescribing of other antimicrobial classes across different specialties may have influenced our results. When there was disparity between the opinions of reviewers’ a fourth independent reviewer (LSPM) was consulted to reach consensus.
Characterising behaviour change interventions
Once all AMS-AMR abstracts had been identified the rates of AMS-AMR coverage between specialty conferences was assessed. Abstracts were then re-read by at least two of four researchers (TMR, AMT, AT, & LSPM) and categorised into types of intervention reported in the abstracts. To categorise the types of interventions reported a modified version of intervention and policy framework definitions provided by Michie and colleagues for the construction of their behaviour change wheel were used (Additional file 1: Table S1) [25]. In the original behaviour change wheel, three layers (policy, intervention, and behaviour systems are described). Within the classification used in this study, behaviour systems were not included (capability, opportunity, motivation, and behaviour; COM-B) as reported interventions were focused on the two levels of the framework above this, which aim to directly influence COM-B [25]. Researchers attempted, where possible, to categorise reported behaviour change interventions into one or more of the sixteen functions (split into policies and interventions) described within this framework. Although the framework is designed to provide flexibility and accommodate multiple interventions/policy combinations, researchers attempted to strictly categorise reported interventions into the fewest number of categories possible. When there was discrepancy the group discussed these issues until consensus was reached. Descriptive statistics was performed in SPSS 22.0 (IBM, Chicago, IL) with Chi-squared with Yates correction. Ethics approval was not required for this observational study.
Results
AMS-AMR coverage at UK state-of-the-art scientific conferences in 2015
Thirty specialty state-of-the-art scientific conferences abstract booklets were identified and extracted for analysis. These conferences ran over >110 days with >57,000 delegates estimated to of attended them in 2015 (Table 1). In total, 12,313 abstracts were extracted for analysis with 311 (2.5%) identified as related to AMS-AMR (Fig. 1). Of these, 118/311 (38%) were presented at the UK’s infectious diseases/microbiology conference [29]. This made up 38% (144/375) of all conference abstracts reported at this conference. Genitourinary medicine [30] had the second highest coverage with 9% (26/299), orthopaedics [31] third and plastic surgery [32] fourth with 8% of abstracts related to AMS-AMR each (8/96 & 6/78, respectively). All other specialty’s had <5% AMS-AMR coverage with neurology [33], emergency medicine [34], psychiatry [35], geriatrics [36], and endocrinology [37] not having any AMS-AMR related coverage at their 2015 conferences. Compared to published data on conference coverage in the UK in 2014 [21] there was no significant difference in the level of AMS-AMR reporting (311/12,313, 2.5%, in 2015 & 221/7843, 2.8%, in 2014; p = 0.22). Infection/microbiology had a significantly larger proportion of AMS-AMR abstracts compared to all other specialties reviewed within this study (p < 0.01).
Table 1.
UK state-of-the-art scientific conference summary
| Speciality | City | Date commenced | No Days | No delegates | No abstracts accepted |
|---|---|---|---|---|---|
| Anaesthetics [44] | Edinburgh | 23/09/2015 | 3 | 800 | 161 |
| Breast Surgery [45] | Bournemouth | 15/06/2015 | 2 | 870 | 221 |
| Cardiology [46] | Manchester | 08/06/2015 | 3 | 2448 | 235 |
| Dermatology [47] | Manchester | 06/07/2015 | 4 | 1200 | 372 |
| Emergency Medicine [34] | Manchester | 28/09/2015 | 3 | 650 | 69 |
| Endocrinology [37] | Edinburgh | 02/11/2015 | 3 | 1000 | 526 |
| Gastroenterology [48] | London | 22/06/2015 | 4 | 4500 | 1240 |
| Primary Care [38] | Glasgow | 01/10/2015 | 3 | 1600 | 450 |
| General Surgery [49] | Manchester | 22/04/2015 | 3 | 1500 | 1065 |
| Surgery (ASiT) [50] | Glasgow | 27/02/2015 | 3 | 700 | 602 |
| Genitourinary Medicine [30] | Glasgow | 01/06/2015 | 3 | 500 | 299 |
| Geriatrics [36] | Brighton | 14/10/2015 | 3 | 500 | 76 |
| Haematology [51] | Edinburgh | 20/04/2015 | 3 | 1000 | 257 |
| Infection/Microbiology [29] | Glasgow | 21/11/2015 | 3 | 1000 | 375 |
| Intensive Care [52] | London | 07/12/2015 | 3 | 1250 | 154 |
| Nephrology [43] | London | 28/05/2015 | 4 | 8190 | 1945 |
| Neuro surgery [53] | York | 09/09/2015 | 3 | 200 | 139 |
| Neurology [33] | Harrogate | 20/05/2015 | 3 | 600 | 194 |
| Obstetrics & Gynaecology [54] | Brisbane | 12/04/2015 | 4 | 2300 | 770 |
| Ophthalmology [55] | Liverpool | 18/05/2015 | 4 | 1700 | 228 |
| Orthopaedics [31] | Liverpool | 15/09/2015 | 4 | 1600 | 96 |
| Paediatric surgery [56] | Cardiff | 22/07/2015 | 3 | 346 | 83 |
| Paediatrics [57] | Birmingham | 28/04/2015 | 3 | 2000 | 546 |
| Plastic surgery [32] | Birmingham | 25/11/2015 | 3 | 400 | 78 |
| Psychiatry [35] | Birmingham | 29/06/2015 | 4 | 2500 | 79 |
| Respiratory [58] | London | 02/12/2015 | 3 | 2200 | 460 |
| Rheumatology [59] | Manchester | 28/04/2015 | 3 | 2000 | 677 |
| Transplant surgery [60] | Bournemouth | 11/03/2015 | 3 | 700 | 382 |
| Urology [61] | Manchester | 15/06/2015 | 4 | 1200 | 161 |
| Vascular surgery [62] | Bournemouth | 11/11/2015 | 3 | 800 | 373 |
Fig. 1.
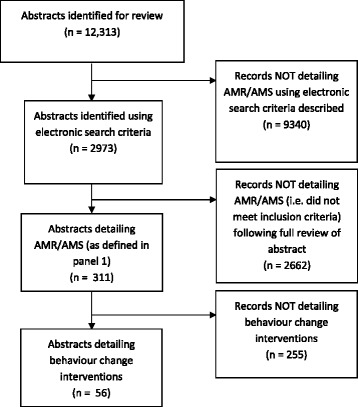
Selection method to identify antimicrobial stewardship/antimicrobial resistance abstracts among state-of-the-art conferences in 2015
Reported behaviour change interventions for antimicrobial prescribing
Of the 311 AMS-AMR abstracts identified 56 (18%) described behaviour change interventions (Table 2). Of these, 28/56 (50%) were reported at the infection/microbiology conference with general surgery conferences reporting the second largest proportion with 7/56 (13%). In total, behaviour change interventions were reported across 12/30 (40%) specialty state-of-the-art conferences with infection/microbiology reporting a significantly greater amount that all other conferences (p < 0.01). The commonest abstracts reporting behaviour change interventions were quality improvement projects accounting for 44/56 (79%) of all reported behaviour change interventions. However, this represented a minority of all AMS-AMR quality improvement projects identified with 80/124 (65%) either not reporting any intervention or not reporting a specific behaviour change intervention. The remainder of behaviour change interventions included were found to be reported within observational studies (12/56; 21%). This also represented a minority of observational studies reporting AMS-AMR topics across clinical specialties (12/54; 22%).
Table 2.
Outline of behavioural interventions reported per UK specialty
| Education | Persuasion | Incentivise | Coercion | Training | Restriction | Environmental restructure | Modelling | Enablement | Communication | Guidelines | Fiscal | Regulation | Legislation | Environmental | Service provision | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Endocrinology | ||||||||||||||||
| Geriatrics | ||||||||||||||||
| Psychiatry | ||||||||||||||||
| Emergency Medicine | ||||||||||||||||
| Neurology | ||||||||||||||||
| Cardiology | ||||||||||||||||
| Ophthalmology | ||||||||||||||||
| Paediatric surgery | ||||||||||||||||
| Paediatrics | 1 | |||||||||||||||
| Anaesthetics | ||||||||||||||||
| Breast Surgery | ||||||||||||||||
| Vascular surgery | ||||||||||||||||
| Obstetrics & Gynaecology | ||||||||||||||||
| Intensive Care | 1 | |||||||||||||||
| Neurosurgery | 1 | |||||||||||||||
| Transplant Surgery | ||||||||||||||||
| Dermatology | 1 | |||||||||||||||
| Haematology | ||||||||||||||||
| Urology | 1 | 1 | ||||||||||||||
| Plastic Surgery | ||||||||||||||||
| Gastroenterology | 1 | |||||||||||||||
| Respiratory | ||||||||||||||||
| Orthopaedics | 1 | 1 | ||||||||||||||
| Rheumatology | ||||||||||||||||
| General Surgery (ASiT) | 1 | 1 | 1 | 1 | ||||||||||||
| Primary Care | 2a | 2a | 1a | 1 | 1 | 2a | ||||||||||
| Nephrology | 1 | 1 | ||||||||||||||
| Genitourinary Medicine | ||||||||||||||||
| General Surgery | 2 | 1 | 2 | 1 | 1 | |||||||||||
| Infection/Microbiology | 3a | 5a | 1 | 1 | 5a | 5 | 2a | 6a | 1 | 2a | 8a |
Legend: aInterventions may have been part of a bundle of interventions reported in one abstract
NB. One behaviour change intervention has been excluded as the full nature of the intervention was not clearly defined
In total, 71 unique behaviour change functions were identified across the 56 abstracts reported behaviour change interventions (Table 2). Eight abstracts were deemed to describe multiple behaviour change interventions with six of these being reported at the infectious diseases/microbiology conference [29] and two at the primary care conference [38]. Policy categories; “guidelines” (16/71) and “service provision” (11/71) were the most frequently reported. Intervention functions; “education” (6/71), “persuasion” (7/71), “enablement” (9/71), and environmental restructuring (9/71) were also common. Intervention categories “incentivisation” and “coercion” and policy categories “fiscal” and “legislation” were not reported in any interventions. However, only infection/microbiology and primary care tended to report a broad variety of interventions, with the majority of interventions reported in the remaining ten specialties tending to focus on enablement (intervention) and guidelines or service provision (policy). The types of functions reported in abstracts that described multiple behaviour change interventions (8/56; 14%) are highlighted in Table 3. In abstracts reporting multiple behaviour change intervention functions there was a mix of policy and intervention targets with guidelines featuring in 6/8 (75%), environmental restructuring, education and persuasion all featuring in 4/8 (50%), and service provision in 3/8 (38%) of the abstracts.
Table 3.
Outline of intervention functions reported in abstracts reporting multiple behaviour change interventions
| Primary Care | 1. | Guideline, persuasion, & modelling |
| 2. | Education, persuasion & environmental restructuring | |
| Infection/Microbiology | 3. | Guideline, persuasion & environmental |
| 4. | Guideline, persuasion & service provision | |
| 5. | Guideline, environmental restructuring, education, communication | |
| 6. | Guideline, education, service provision, environmental restructure | |
| 7. | Guideline & service provision | |
| 8. | Education & environmental restructuring |
Discussion
Clinical state-of-the-art conferences provide an opportunity for medical professionals to participate in research and reporting. They also allow us to gain an insight into different levels of research being undertaken within the field; from small scale research undertaken at the local level, to large scale studies being performed by key opinion leaders and organisations. This provides a window into the activities within specialties that is less influenced by publication bias than can often be observed through systematically reviewing peer-reviewed publications. Within this study, we observed a low rate of behaviour change intervention reporting across the majority of specialty state-of-the-art conferences in 2015. Infection specialties reported a significantly greater number and broader variety of AMS-AMR interventions with the majority of interventions reported by non-infection specialties falling into a narrow band of intervention and policy based functions.
These observations are concerning given the recent focus placed upon the need for cross-specialty engagement with AMS-AMR and behaviour change interventions. This has been supported broadly in the literature [4, 13, 16, 21, 22, 39]; by national organisations including Public Health England (PHE) [18], the British Society for Antimicrobial Chemotherapy (BSAC), and government [40]; and major international governments and organisations [6, 7]. These findings highlight the need to broaden the focus of AMS campaigns beyond infection specialties to promote leadership from within cohorts, which can drive behaviour change towards antimicrobial use.
This must be supported by clear and defined tools to help specialties engage and design AMS-AMR behaviour change interventions and assess the impact of these on patient outcomes. Whilst the use of behaviour change taxonomies allows content of interventions to be coded and categorised, facilitating the analysis of behaviour change interventions [24, 41], they are not appropriate for determining the effectiveness of interventions. Furthermore, for the field of AMS-AMR there remains no definition on what an appropriate behaviour change intervention is. This makes evaluating behaviour change challenging as certain functions of any framework used may be irrelevant or actually have a negative impact on behaviours within this context. [24, 41, 42] Kok and colleagues argue that as behavioural determinants are often specific to behaviours, populations, and contexts characterisations should thus be individualised and tailored for such [24, 41]. This will require engagement and drive from within clinical specialties to review current practices, define the context in which AMS-AMR interventions need to be implemented, and then tailor behaviour change interventions to optimise their effect within their local environment.
Finally, in a previous study “high risk” specialties were identified that currently use large amounts of antimicrobials and also experience high levels of healthcare associated infections [21]. This study reported that certain “high risk” specialties such as infection and intensive care had relatively high levels of engagement with AMS-AMR, whilst other specialties such as haematology and nephology tended to have a low apparent engagement at scientific conferences [21]. Within this study, we have observed an overall low rate of behaviour change interventions across all high risk specialties reported previously with only infection [29] and nephrology [43] reporting any behaviour change interventions in 2015. Furthermore, specialties with relatively high coverage of AMS-AMR at scientific conferences, such as Genitourinary Medicine, failed to report on behaviour change interventions despite having 9% coverage of AMS-AMR topics in 2015. This highlights the need for greater pan-specialty promotion of behaviour change interventions for AMS-AMR given the significant lack of focus on reporting such interventions currently.
There are several limitations to this study. Firstly, we only selected one leading state-of-the-art conference for each major clinical specialty in the UK. This makes our findings difficult to generalise across other countries and also may have introduced bias through excluding smaller, conferences and meetings, where specialties may have had more of an AMS-AMR focus. However, this method was selected as we aimed to generate a representative picture of current behaviour change interventions and the importance placed upon this by different specialties. By selecting leading state-of-the-art conferences we hoped that this would reflect the current overall importance of this subject within the specialty as well as allow for a more representative view of work being undertaken in the field. Secondly, we did not review invited talks and seminars provided by conferences given that they often were not presenting original data or results. Furthermore, as the taxonomy used to describe behaviour change does not allow for evaluation of the effectiveness of interventions it is not possible to evaluate whether interventions described were “appropriate” for the context in which they were described. Finally, as only a relatively small number of specialists from a specific geographical area were contacted to seek opinions on defining the largest UK conference in their field this may have introduced bias in our conference selection. To address this we ensured that two specialists from each field were contacted for their opinions. When there was discrepancy in responses from the individuals, conference attendance size was considered as the determinant with the conference with the largest attendance selected.
Conclusion
In conclusion, despite evidence to support the role of behaviour change interventions for improving antimicrobial prescribing, very few studies reported implementing them at UK state-of-the-art conferences in 2015. Future research must focus on providing appropriate frameworks and mechanisms to allow clinical specialties to engage with AMS-AMR and design and evaluate the impact of behaviour change interventions within their specific contexts.
Acknowledgements
The authors would like to thank members of Imperial College NHS Healthcare Trust who participated in the study. The authors would also like to acknowledge the National Institute of Health Research Imperial Biomedical Research Centre and the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Healthcare Associated Infection and Antimicrobial Resistance at Imperial College London in partnership with Public Health England and the NIHR Imperial Patient Safety Translational Research Centre. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the UK Department of Health.
Funding
This report is independent research funded by the National Institute for Health Research Invention for Innovation (i4i) programme, Enhanced, Personalized and Integrated Care for Infection Management at Point of Care (EPIC IMPOC), II-LA-0214-20008.
Availability of data and materials
Datasets analysed during the current study are available from the corresponding author (TMR tmr07@ic.ac.uk) on reasonable request, as long as this meets local ethics and research governance criteria.
Authors’ contributions
TMR, LSPM, & AH conceived the study design. TMR, EC, ANT, AT, & LSMP extracted and analysed the data. TMR drafted the initial manuscript. All authors (TMR, LSPM, EC, AT, ANT, MG, & AH) reviewed and contributed significantly to revision of the manuscript, agreeing on the final format for submission to ARIC.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
No ethics or consent was required from this study using publically available data.
Additional file
Behaviour change taxonomy used for classification of interventions reported in state-of-the-art scientific conference abstracts in 2015. (DOC 36 kb)
Contributor Information
T. M. Rawson, Phone: 02033132732, Email: tmr07@ic.ac.uk, Email: timothy.rawson07@imperial.ac.uk
L. S. P. Moore, Email: l.moore@imperial.ac.uk
A. M. Tivey, Email: ann.tivey14@imperial.ac.uk
A. Tsao, Email: adam.tsao14@imperial.ac.uk
M. Gilchrist, Email: mark.gilchrist@imperial.nhs.uk
E. Charani, Email: e.charani@imperial.ac.uk
A. H. Holmes, Email: alison.holmes@imperial.ac.uk
References
- 1.English surveillance programme for antimicrobial utilisation and resistance (ESPAUR). 2014. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/362374/ESPAUR_Report_2014__3_.pdf. Accessed 3 Oct 2016.
- 2.ESPAUR. English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) 2010 to 2014 Report 2015 About Public Health England. 2015.
- 3.Raveh D, Levy Y, Schlesinger Y, Greenberg A, Rudensky B, Yinnon AM. Longitudinal surveillance of antibiotic use in the hospital. QJM. 2001;94:141–52. doi: 10.1093/qjmed/94.3.141. [DOI] [PubMed] [Google Scholar]
- 4.Holmes AH, Moore LSP, Sundsfjord A, et al. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet. 2015;6736: Available at: http://linkinghub.elsevier.com/retrieve/pii/S0140673615004730. [DOI] [PubMed]
- 5.Dellit TH, Owens RC, McGowan JE, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Clin Infect Dis. 2007;44:159–77. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 6.Cruickshank M. Antimicrobial stewardship in Australian hospitals. 2011. Available at: http://www.safetyandquality.gov.au/wp-content/uploads/2011/01/Antimicrobial-stewardship-in-Australian-Hospitals-2011.pdf.
- 7.Core Elements of Hospital Antibiotic Stewardship Programs. 2014: 1–25. Available at: http://www.cdc.gov/getsmart/healthcare/implementation/core-elements.html. Accessed 3 Oct 2016.
- 8.ESPAUR SSTF Implementation subgroup . Start Smart - Then Focus Antimicrobial Stewardship Toolkit for English Hospitals. 2015. [Google Scholar]
- 9.Macdougall C, Polk RE, Campus V. Antimicrobial Stewardship Programs in Health Care Systems. Clin Microbiol Rev. 2005;18:638–56. doi: 10.1128/CMR.18.4.638-656.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts RR, Hota B, Ahmad I, et al. Hospital and societal costs of antimicrobial-resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin Infect Dis. 2009;49:1175–84. doi: 10.1086/605630. [DOI] [PubMed] [Google Scholar]
- 11.Raymond DP, Pelletier SJ, Crabtree TD, et al. Impact of a rotating empiric antibiotic schedule on infectious mortality in an intensive care unit. Crit Care Med. 2001;29:1101–8. doi: 10.1097/00003246-200106000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Charani E, Cooke J, Holmes A. Antibiotic stewardship programmes-what’s missing? J Antimicrob Chemother. 2010;65:2275–7. doi: 10.1093/jac/dkq357. [DOI] [PubMed] [Google Scholar]
- 13.Charani E, Edwards R, Sevdalis N, et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis. 2011;53:651–62. doi: 10.1093/cid/cir445. [DOI] [PubMed] [Google Scholar]
- 14.Rawson TM, Charani E, Moore LSP, et al. Mapping the decision pathways of acute infection management in secondary care among UK medical physicians: A qualitative study. BMC Med. 2016;14:1–10. doi: 10.1186/s12916-015-0545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charani E, Castro-Sanchez E, Sevdalis N, et al. Understanding the determinants of antimicrobial prescribing within hospitals: The role of ‘prescribing etiquette’. Clin Infect Dis. 2013;57:188–96. doi: 10.1093/cid/cit212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davey P, Brown E, Charani E, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2013. Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003543.pub3/full. [DOI] [PubMed]
- 17.Skodvin B, Aase K, Charani E, Holmes A, Smith I. An antimicrobial stewardship program initiative: a qualitative study on prescribing practices among hospital doctors. Antimicrob Resist Infect Control. 2015;4:24. doi: 10.1186/s13756-015-0065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Public Health England, Department of Health. Behaviour change and antibiotic prescribing in healthcare settings Literature review and behavioural analysis. 2015. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/405031/Behaviour_Change_for_Antibiotic_Prescribing_-_FINAL.pdf.
- 19.Teixeira Rodrigues A, Roque F, Falcão A, Figueiras A, Herdeiro MT. Understanding physician antibiotic prescribing behaviour: A systematic review of qualitative studies. Int J Antimicrob Agents. 2013;41:203–12. doi: 10.1016/j.ijantimicag.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Teixeira Rodrigues A, Ferreira M, Piñeiro-Lamas M, Falcão A, Figueiras A, Herdeiro MT. Determinants of physician antibiotic prescribing behaviour: a 3-year cohort study in Portugal. Curr Med Res Opin. 2016;7995:1–24. doi: 10.1185/03007995.2016.1154520. [DOI] [PubMed] [Google Scholar]
- 21.Rawson TM, Moore LSP, Gilchrist MJ, Holmes AH. Antimicrobial stewardship: are we failing in cross-specialty clinical engagement? J Antimicrob Chemother. 2015;dkv337: Available at: http://www.jac.oxfordjournals.org/lookup/doi/10.1093/jac/dkv337. [DOI] [PMC free article] [PubMed]
- 22.Rawson TM, Butters TP, Moore LSP, Castro-Sánchez E, Cooke FJ, Holmes AH. Exploring the coverage of antimicrobial stewardship across UK clinical postgraduate training curricula. J Antimicrob Chemother. 2016;dkw280: Available at: http://www.jac.oxfordjournals.org/lookup/doi/10.1093/jac/dkw280. [DOI] [PMC free article] [PubMed]
- 23.Castro-Sánchez E, Drumright LN, Gharbi M, Farrell S, Holmes AH. Mapping antimicrobial stewardship in undergraduate medical, dental, pharmacy, nursing and veterinary education in the United Kingdom. PLoS One. 2016;11:1–10. doi: 10.1371/journal.pone.0150056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kok G, Gottlieb NH, Peters G-JY, et al. A Taxonomy of Behavior Change Methods; an Intervention Mapping Approach. Health Psychol Rev. 2015;31:1–32. doi: 10.1080/17437199.2015.1077155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pope SD, Dellit TH, Owens RC, Hooton TM. Results of survey on implementation of Infectious Diseases Society of America and Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Infect Control Hosp Epidemiol. 2009;30:97–8. doi: 10.1086/592979. [DOI] [PubMed] [Google Scholar]
- 27.WHO. Antimicrobial Resistance Global Report on Surveillance 2014. World Heal Organ 2014. Available at: http://www.who.int/drugresistance/documents/surveillancereport/en/.
- 28.European Surveillence of Antimicrobial Consumption. Report on Point Prevalence Survey of Antimicrobial Prescription in European Hospitals, 2009. 2009. Available at: http://ecdc.europa.eu/en/activities/surveillance/ESAC-Net/publications/Documents/report_survey_antimicrobial_prescriptions_eu_hospitals_2009.pdf. Accessed 3 Oct 2016.
- 29.Federation of Infection Society, Glasgow, 2015. In: Federation of Infection Society annual conference 2015. 2015
- 30.BASHH Spring Conference 2015 Abstract Presentations 1–3 June 2015 Royal Concert Halls, Glasgow, Scotland. In: Sexually Transmitted Infections (STI). Vol 91, 2015; A1–104. Available at: https://www.bashh.org/documents/Final%20BASHH%202015%20Abstract%20book.pdf/. Accessed 3 Oct 2016.
- 31.British Orthopaedic Association Annual Congress 2015, 15–18 September - ACC Liverpool. In: British Orthopaedic Association. Liverpool, 2015
- 32.Winter Scientific Meeting 25–17 November 2015, The Vox Conference Centre, Resorts World Birmingham. In: British Association of Plastic Reconstructive and Aesthetic Surgeons. Birmingham, 2015
- 33.ABN Annual Meeting 2015 19–22 May 2015 - Harrogate International Centre, Harrogate. Assoc Br Neurol 2015. Available at: http://www.theabn.org/events/abn-events/harrogate.html. Accessed 3 Oct 2016.
- 34.Abstracts from UK EM 2015. Emerg Med J 2015; 32. Available at: http://emj.bmj.com/lookup/doi/10.1136/emermed-2015-205511. Accessed 3 Oct 2016.
- 35.The Royal College of Psychiatrists’ International Congress 29 June - 2 July 2015 Birmingham, 2015. Available at: http://www.rcpsych.ac.uk/pdf/Full%20Programme%20web%20v56.pdf.
- 36.British Geriatrics Society. Abstracts of work presented at the 2015 BGS Autumn Meeting: Promoting better health in old age, Brighton, 2015. Available at: http://www.bgs.org.uk/pdf_cms/admin_archive/2015_autumn_abstracts.pdf.
- 37.Endocrine Abstracts. In: Society for Endocrinology BES 2015. Vol 38., 2015
- 38.Expanding horizons of care. In: Annual Primary Care Conference 2015., 2015
- 39.Ashiru-oredope D, Sharland M, Charani E, McNulty C, Cooke J. Improving the quality of antibiotic prescribing in the nhs by developing a new antimicrobial stewardship programme: Start smart-then focus. J Antimicrob Chemother. 2012;67:i51–63. doi: 10.1093/jac/dks202. [DOI] [PubMed] [Google Scholar]
- 40.O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations the Review on. 2016. Available at: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf.
- 41.Kok G, Gottlieb NH, Peters G-JY, et al. Tables and Figure for: A Taxonomy of Behavior Change Methods; an Intervention Mapping Approach. Health Psychol Rev. 2015;31:1–32. Available at: http://dx.doi.org/10.1080/17437199.2015.1077155. [DOI] [PMC free article] [PubMed]
- 42.Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev. 2016;7199:1–39. [DOI] [PMC free article] [PubMed]
- 43.53rd ERA-EDTA Congress Abstracts2ViewTM. Eur Ren Assoc Conf 2015. Available at: http://www.abstracts2view.com/era/. Accessed 3 Oct 2016.
- 44.Abstracts of the AAGBI Annual Congress, 23–25 September 2015, Edinburgh, UK. Anaesthesia. 2015;70(4 Suppl):1–91. doi:10.1111/anae.13223. [DOI] [PubMed]
- 45.ABS Conference Annual Meeting - 2015. In: Association of Breast Surgery., 2015. Available at: http://www.associationofbreastsurgery.org.uk/abs-events/past-meetings/abs-conference-agm-2015/. Accessed 3 Oct 2016.
- 46.BCS annual conference, ‘Hearts and Genes’ June 8–10, Manchester, UK, 2015. Heart 2015; 101. Available at: http://heart.bmj.com/content/101/Suppl_4.toc#Clinical. Accessed 3 Oct 2016.
- 47.British Association of Dermatologists Annual Meeting, 2015, Manchester. Br J Dermatol 2015; 173: 1–2. Available at: http://doi.wiley.com/10.1111/bjd.13800. Accessed 3 Oct 2016 [DOI] [PubMed]
- 48.2nd Digestive Disorders Federation Conference 22–25 June 2015 Abstracts. Gut 2015. Available at: http://gut.bmj.com/content/64/Suppl_1.toc. Accessed 3 Oct 2016.
- 49.ASGBI abstracts. Br J Surg 2015; 102: 88–177. Available at: http://doi.wiley.com/10.1002/bjs.9941. Accessed 3 Oct 2016.
- 50.The Association of Surgeons in Training Conference: #ASiT2015 Glasgow. Int J Surg 2015; 23: S1–4. Available at: http://linkinghub.elsevier.com/retrieve/pii/S1743919115012935. [DOI] [PubMed]
- 51.Abstracts of the 55th Annual Scientific Meeting of the British Society for Haematology, 20–22 April 2015, Edinburgh, UK. In: British Journal of Haematology. Vol 169., 2015; 1–104. Available at: http://doi.wiley.com/10.1111/bjh.13350. Accessed 3 Oct 2016. [DOI] [PubMed]
- 52.State of the Art Scientific Abstracts. J Intensive Care Soc 2015; 16. Available at: http://inc.sagepub.com/lookup/doi/10.1177/1751143715615276. Accessed 3 Oct 2016
- 53.Proceedings of the Society of British Neurological Surgeons: 58th Meeting. In: Journal of Neurology, Neurosurgery & Psychiatry. 2015. Available at: http://jnnp.bmj.com/cgi/doi/10.1136/jnnp.22.1.77. Accessed 3 Oct 2016.
- 54.Abstracts of the RCOG World Congress 2015, 12–15 April, Brisbane, Queensland, Australia. In: Royal College of Obstetrics & Gynaecology. Vol 122., 2015; 1–414. Available at: http://onlinelibrary.wiley.com/doi/10.1111/1471-0528.13365/abstract. Accessed 3 Oct 2016. [DOI] [PubMed]
- 55.Annual Congress 2015, 19–21 May 2015 - The ACC Liverpool. In: The Royal College of Ophthalmologists. 2015
- 56.BAPS Papers. In: Journal of Pediatric Surgery. Vol 51., 2016. Available at: http://www.sciencedirect.com/science/journal/00223468/51/2. Accessed 4 Oct 2016.
- 57.Royal College of Paediatrics and Child Health, Abstracts of the Annual Conference, 28–30 April 2015, The ICC, Birmingham. 2015. Available at: http://adc.bmj.com/content/100/Suppl_3.toc. Accessed 3 Oct 2016.
- 58.British Thoracic Society Winter Meeting, The Queen Elizabeth II Centre Broad Sanctuary Westminster London SW1P 3EE 2 to 4 December 2015 Programme and Abstracts. In: Thorax., 2015; Vol 70; Suppl 3. Available at: http://thorax.bmj.com/content/70/Suppl_3.toc.
- 59.Rheumatology 2015 Abstracts. In: Rhematology., 2015; Volume 54 suppl 1. Available at: http://rheumatology.oxfordjournals.org/content/54/suppl_1.toc. Accessed 3 Oct 2016.
- 60.British Transplantation Society and Nederlandse Transplantatie Vereniging Joint Congress 2015. In: British Transplantation Society. Bournemouth, 2015. Available at: http://www.btscongress.com/abstracts.html.
- 61.BAUS 2015 Annual Scientific Meeting. Br Assoc Urol Surg 2015. Available at: http://baus.multilearning.com/baus/#!*menu = 6*browseby = 7*sortby = 1*media = 3*ce_id = 822.
- 62.Special Issue: VSGBI abstracts from The Vascular Societies’ Annual Scientific Meeting, 11–13 November 2015. Br J Surg 2016; 103: 1–30. Available at: http://doi.wiley.com/10.1002/bjs.10271. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets analysed during the current study are available from the corresponding author (TMR tmr07@ic.ac.uk) on reasonable request, as long as this meets local ethics and research governance criteria.


