Abstract
BACKGROUND
In SPRINT (Systolic Blood Pressure Intervention Trial), a systolic blood pressure (SBP) goal of <120 mm Hg resulted in lower cardiovascular disease (CVD) risk compared with an SBP goal of <140 mm Hg.
OBJECTIVES
The purpose of this study was to estimate the prevalence, number, and characteristics of U.S. adults meeting SPRINT eligibility criteria and determine the broader population to whom SPRINT could be generalized.
METHODS
We conducted a cross-sectional, population-based study using data from the National Health and Nutrition Examination Survey, 2007 to 2012. The SPRINT inclusion criteria were age ≥50 years, SBP 130 to 180 mm Hg depending on the number of antihypertensive medication classes being taken, and high CVD risk (history of coronary heart disease, estimated glomerular filtration rate of 20 to 59 ml/min/1.73 m2, 10-year CVD risk ≥15%, or age ≥75 years). Exclusion criteria were diabetes, history of stroke, >1 g in 24 h of proteinuria daily, heart failure, estimated glomerular filtration rate <20 ml/min/1.73 m2, or receiving dialysis. Treated hypertension was defined by self-reported use of medication to lower blood pressure with ≥1 class of antihypertensive medication identified through a pill bottle review.
RESULTS
Overall, 7.6% (95% confidence interval [CI]: 7.0% to 8.3%) or 16.8 million (95% CI: 15.7 to 17.8 million) U.S. adults, and 16.7% (95% CI: 15.2% to 18.3%) or 8.2 million (95% CI: 7.6 to 8.8 million) adults with treated hypertension met the SPRINT eligibility criteria. Among both the overall U.S. population and adults with treated hypertension, the percentage meeting SPRINT eligibility criteria increased with older age, was higher among males than females, and was higher among non-Hispanic whites compared with non-Hispanic blacks or Hispanics. Of U.S. adults eligible for SPRINT, 51.0% (95% CI: 47.8% to 54.1%) or 8.6 million (95% CI: 8.0 to 9.1 million) were not treated for hypertension.
CONCLUSIONS
A substantial percentage of U.S. adults meet the eligibility criteria for SPRINT.
Keywords: control, hypertension, population health, systolic blood pressure, treatment
The SPRINT (Systolic Blood Pressure Intervention Trial) tested whether lowering systolic blood pressure (SBP) to <120 mm Hg versus <140 mm Hg results in reduced cardiovascular disease (CVD) risk (1). Between 2010 and 2013, SPRINT enrolled 9,361 adults age ≥50 years who had SBP 130 to 180 mm Hg and were at high risk for CVD. Individuals were not eligible if they had diabetes, had a history of stroke, had >1 g in 24 h of proteinuria, had heart failure, were on dialysis, or had an estimated glomerular filtration rate (eGFR) <20 ml/min/1.73 m2 (1). On September 11, 2015, the National Institutes of Health issued a press release stating that SPRINT was being stopped early due to an approximately 30% relative risk reduction in CVD events and 25% relative risk reduction in mortality among participants randomized to the SBP goal <120 mm Hg compared with the SBP goal <140 mm Hg (2).
SPRINT enrolled a diverse population, and therefore, its results may be relevant to a large percentage of U.S. adults (1). Characterizing U.S. adults who are potentially eligible for antihypertensive treatment initiation or intensification to achieve an SBP <120 mm Hg may help the health care and scientific community understand the relevance and effect of the findings from SPRINT. We, therefore, estimated the prevalence, number, and characteristics of U.S. adults who meet the SPRINT eligibility criteria and may be candidates for an SBP goal of <120 mm Hg. As clinicians often need to generalize results beyond the population examined in a clinical trial, we also estimated the size of the broader sample of U.S. adults with SBP ≥120 mm Hg who are free of SPRINT exclusion criteria.
METHODS
STUDY POPULATION
The National Health and Nutrition Examination Survey (NHANES) is conducted by the National Center for Health Statistics. The data and information on the design and conduct of NHANES are available on the Centers for Disease Control and Prevention website (3). NHANES uses a multistage stratified probability sampling approach to identify potential participants. Multiple cycles can be pooled together to provide stable estimates in population subgroups (4). We pooled data from the 2007 to 2008, 2009 to 2010, and 2011 to 2012 NHANES cycles for the current analyses. Analyses were restricted to participants who were ≥20 years of age and completed a medical evaluation at the NHANES mobile examination center (n = 17,085). We excluded participants who did not have SBP and diastolic blood pressure (DBP) measurements taken during their NHANES medical evaluation (n = 803) or were missing self-reported information on the use of prescription antihypertensive medication (n = 22), leaving 16,260 participants in the current analyses. The National Center for Health Statistics institutional review board approved each NHANES cycle, and all participants provided written informed consent.
DATA COLLECTION
Data for each NHANES cycle were collected through participant interviews and a medical evaluation. Data collected during the interview included age; race/ethnicity; sex; smoking status; a prior diagnosis of comorbid conditions including hypertension, diabetes, heart failure, myocardial infarction, angina, coronary heart disease (CHD), and stroke; receipt of dialysis in the past 12 months; and use of antihypertensive and diabetes medication.
During the NHANES medical evaluation, height and weight were measured and used to calculate body mass index. Serum glucose, serum creatinine, and hemoglobin A1c were measured from a blood sample collected during the study visit. Diabetes mellitus was defined by a prior diagnosis, excluding during pregnancy, with concurrent use of insulin or oral hypoglycemic medication, or by a fasting glucose ≥126 mg/dl, nonfasting glucose ≥200 mg/dl, or a hemoglobin A1c ≥6.5%. eGFR was calculated using the Modification of Diet in Renal Disease equation (5). Urine albumin and creatinine were measured using random spot urine samples.
BLOOD PRESSURE MEASUREMENT
Blood pressure was measured by a trained physician using a mercury sphygmomanometer and an appropriately sized cuff. Readings were obtained after 5 min of seated rest. The mean of 3 blood pressure measurements obtained at 1-min intervals during the medical evaluation was used to define SBP and DBP.
PILL BOTTLE REVIEW
Participants were asked to bring all prescription medications taken in the past 2 weeks to the NHANES medical evaluation. Pill bottles were reviewed, and medication names were recorded and coded into medication classes based on their generic equivalents. Single-pill combinations were classified into their component classes. We coded the following antihypertensive medication classes: angiotensin-converting enzyme inhibitors (ACEIs), alpha blockers, aldosterone receptor antagonists, angiotensin receptor blockers, beta-blockers, calcium-channel blockers, central-acting agents, loop diuretic agents, potassium-sparing diuretic agents (not including spironolactone and eplerenone), thiazide diuretic agents, renin inhibitors, and direct vasodilators.
SPRINT ELIGIBILITY
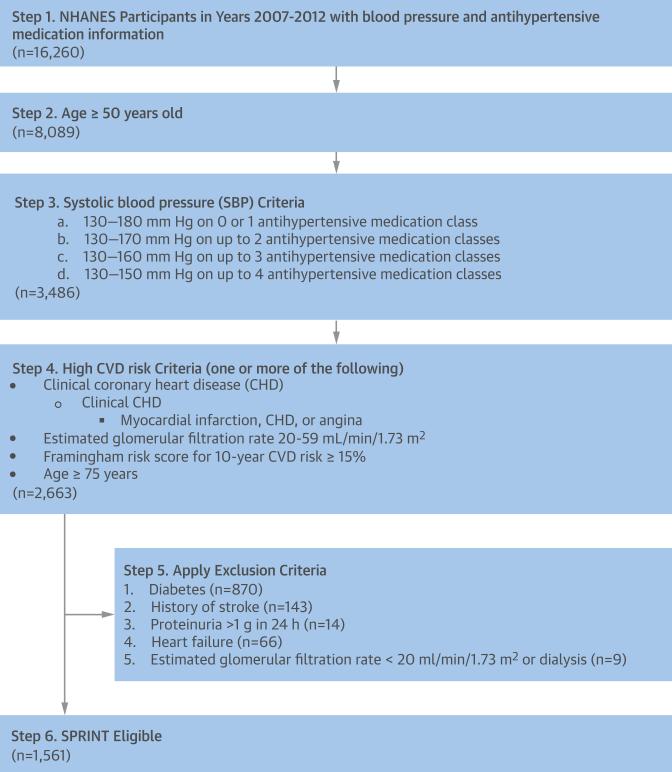
Potential eligibility for SPRINT was determined using a multistep algorithm (Figure 1). The population was restricted based on age (≥50 years), SBP (130 to 180 mm Hg on 0 or 1 antihypertensive medication class, 130 to 170 mm Hg on up to 2 classes, 130 to 160 mm Hg on up to 3 classes, and 130 to 150 mm Hg on up to 4 classes), and the presence of 1 or more high CVD risk conditions. High CVD risk conditions included history of CHD (defined in NHANES as self-report of a prior diagnosis of myocardial infarction, angina, or CHD), eGFR of 20 to 59 ml/min/1.73 m2, 10-year risk for CVD ≥15% calculated using the Framingham risk score for general clinical practice (6), and age ≥75 years. Participants were not eligible if they had any of the following exclusion criteria: diabetes, a history of stroke, >1 g in 24 h of proteinuria, heart failure, on dialysis, or an eGFR <20 ml/min/1.73 m2.
FIGURE 1. Flowchart Showing the Eligibility Criteria for SPRINT Applied to NHANES, 2007 to 2012.
CHD = coronary heart disease; CVD = cardiovascular disease; NHANES = National Health and Nutrition Examination Survey; SBP = systolic blood pressure; SPRINT = Systolic Blood Pressure Intervention Trial.
STATISTICAL ANALYSIS
Among the overall population and participants with and without treated hypertension, we calculated the percent and number of U.S. adults meeting each sequential SPRINT eligibility criterion (Figure 1). Percentages were calculated overall and within subgroups defined by age (50 to 59, 60 to 74, and ≥75 years), sex (male and female), race-ethnicity (non-Hispanic white, non-Hispanic black, and Hispanic), and SBP (130 to 139 and ≥140 mm Hg). Treated hypertension was defined by self-reported use of medication to lower BP with 1 or more classes of antihypertensive medication identified through the pill bottle review. The percentages were also calculated for participants with and without hypertension, defined by self-reported use of antihypertensive medication or SBP/DBP ≥140/90 mm Hg. For the overall population and those with treated hypertension, we also calculated the percentage and number of U.S. adults meeting SPRINT eligibility criteria in subgroups defined by: 1) age ≥50 years; 2) SBP ≥130 mm Hg; 3) any high CVD risk condition; 4) age ≥50 years and SBP ≥130 mm Hg; and 5) age ≥50 years, SBP ≥130 mm Hg, and any high CVD risk condition.
Next, demographic and clinical characteristics of U.S. adults meeting the SPRINT eligibility criteria were calculated. We also calculated the number of antihypertensive medication classes taken by U.S. adults meeting the SPRINT eligibility criteria. Additionally, the use of ACEIs, angiotensin receptor blockers, beta-blockers, calcium-channel blockers, and thiazide diuretic agents was calculated. As <10% of U.S. adults were taking other antihypertensive medication classes, these are not reported individually. For comparison, we calculated the demographic and clinical characteristics and antihypertensive medication use for all U.S. adults ≥50 years of age and those with treated hypertension.
In a secondary analysis, we calculated the percentage and number of U.S. adults with SBP ≥120 mm Hg who also did not have any SPRINT exclusion criteria, overall and who also had: 1) age ≥50 years; 2) high CVD risk; and 3) age ≥50 years and had high CVD risk. The secondary analysis was also conducted for U.S. adults overall and with and without treated hypertension, and separately with and without hypertension. All analyses were performed using SUDAAN 10.1 (Research Triangle Institute, Research Triangle Park, North Carolina), accounting for the complex sampling design of NHANES. Sampling weights, recalibrated based on the proportion of participants missing data by age, sex, and race-ethnicity, were applied to all calculations to obtain U.S. nationally representative prevalence estimates. Recalibration of the sampling weights corrects for differences in missing data across sex and race-ethnicity strata and assumes that data within strata are missing randomly (7). We calculated 95% confidence intervals (CIs) using Taylor-series variance estimation (8).
RESULTS
In 2007 to 2012, 7.6% (95% CI: 7.0% to 8.3%) of U.S. adults, 16.7% (95% CI: 15.2% to 18.3%) of those with treated hypertension, and 5.0% (95% CI: 4.5% to 5.6%) without treated hypertension met the SPRINT eligibility criteria (Table 1). The percentage eligible for SPRINT was greater at older age, among males versus females, among non-Hispanic whites compared with non-Hispanic blacks or Hispanics, and among those with SBP 140 mm Hg versus SBP of 130 to 139 mm Hg. Among U.S. adults with hypertension, 20.0% (95% CI: 18.6% to 21.5%) met the SPRINT eligibility criteria compared with 2.0% (95% CI: 1.7% to 2.4%) without hypertension (Online Table 1).
TABLE 1.
Percentage of U.S. Adults Meeting Each Sequential SPRINT Eligibility Criterion, Overall and in Subgroups
| U.S. Adults (Millions) | Age ≥50 yrs | + SBP Criteria | + High CVD Risk Condition | + No Exclusion Criteria | |
|---|---|---|---|---|---|
| Overall population | |||||
| Overall | 219.4 | 43.3 (41.5–45.3) | 17.0 (16.1–18.0) | 12.0 (11.3–12.9) | 7.6 (7.0–8.3) |
| Age group, yrs | |||||
| 50–59 | 40.8 | 100 | 29.2 (26.8–31.7) | 13.6 (11.6–15.8) | 9.0 (7.3–10.9) |
| 60–74 | 37.5 | 100 | 43.6 (41.4–45.8) | 31.5 (29.6–33.5) | 19.5 (17.8–21.3) |
| ≥75 | 16.7 | 100 | 54.2 (51.2–57.2) | 54.2 (51.2–57.2) | 34.6 (31.4–38.0) |
| Male | 105.6 | 41.9 (39.8–44.0) | 15.9 (14.8–17.0) | 13.4 (12.4–14.4) | 8.8 (8.1–9.7) |
| Female | 113.8 | 44.7 (42.7–46.7) | 18.1 (16.9–19.4) | 10.8 (10.0–11.7) | 6.5 (5.8–7.4) |
| Race-ethnicity | |||||
| Non-Hispanic white | 149.1 | 48.4 (46.2–50.6) | 18.7 (17.6–19.9) | 13.5 (12.5–14.4) | 9.0 (8.3–9.9) |
| Non-Hispanic black | 24.9 | 37.8 (35.0–40.7) | 16.9 (15.1–18.8) | 10.3 (9.1–11.8) | 4.8 (3.9–5.8) |
| Hispanic | 30.1 | 26.6 (24.2–29.1) | 10.7 (9.4–12.2) | 8.0 (6.9–9.2) | 4.3 (3.5–5.1) |
| SBP, mm Hg | |||||
| 130–139 | 26.6 | 66.2 (63.1–69.2) | 65.9 (62.7–68.9) | 39.7 (37.1–42.3) | 24.6 (22.1–27.3) |
| ≥140 | 29.1 | 78.8 (76.5–81.0) | 68.0 (65.4–70.4) | 54.4 (51.5–57.3) | 35.0 (32.1–38.0) |
| Treated hypertension | |||||
| Overall | 49.2 | 80.9 (78.7–82.9) | 36.7 (34.8–38.5) | 29.5 (27.7–31.3) | 16.7 (15.2–18.3) |
| Age group, yrs | |||||
| 50–59 | 11.8 | 100 | 38.1 (33.1–43.4) | 21.2 (16.9–26.4) | 12.5 (9.2–16.7) |
| 60–74 | 17.8 | 100 | 44.9 (41.9–47.9) | 36.2 (33.2–39.2) | 20.0 (17.4–22.8) |
| ≥75 | 10.2 | 100 | 54.5 (51.2–57.7) | 54.5 (51.2–57.7) | 31.3 (27.7–35.1) |
| Male | 21.8 | 78.7 (75.1–82.0) | 33.1 (30.4–36.0) | 31.0 (28.3–33.8) | 18.5 (16.6–20.5) |
| Female | 27.4 | 82.6 (80.4–84.5) | 39.4 (36.6–42.4) | 28.3 (25.8–30.9) | 15.3 (13.3–17.6) |
| Race-ethnicity | |||||
| Non-Hispanic white | 35.9 | 82.9 (80.2–85.4) | 37.6 (35.2–40.1) | 30.5 (28.2–32.9) | 18.8 (16.8–20.9) |
| Non-Hispanic black | 7.2 | 70.9 (67.5–74.1) | 31.4 (28.8–34.1) | 22.2 (20.1–24.5) | 8.5 (6.8–10.6) |
| Hispanic | 3.8 | 79.1 (74.9–82.8) | 37.6 (34.1–41.2) | 32.4 (28.8–36.3) | 14.2 (11.2–17.9) |
| SBP, mm Hg | |||||
| 130–139 | 9.3 | 86.5 (82.5–89.7) | 85.4 (81.4–88.7) | 62.9 (57.7–67.8) | 34.8 (29.7–40.2) |
| ≥140 | 14.2 | 87.6 (84.8–89.9) | 71.2 (68.0–74.2) | 61.0 (57.2–64.7) | 35.2 (31.3–39.2) |
| Without treated hypertension | |||||
| Overall | 170.2 | 32.5 (30.8–34.2) | 11.4 (10.5–12.2) | 7.0 (6.4–7.7) | 5.0 (4.5–5.6) |
| Age group, yrs | |||||
| 50–59 | 29.0 | 100 | 25.6 (23.1–28.3) | 10.5 (8.7–12.5) | 7.5 (6.0–9.4) |
| 60–74 | 19.7 | 100 | 42.4 (38.7–46.1) | 27.3 (24.7–30.0) | 19.0 (16.6–21.7) |
| ≥75 | 6.5 | 100 | 53.8 (49.5–58.2) | 53.8 (49.5–58.2) | 39.9 (35.8–44.1) |
| Male | 83.8 | 32.3 (30.1–34.5) | 11.4 (10.4–12.4) | 8.8 (8.0–9.7) | 6.3 (5.7–7.1) |
| Female | 86.4 | 32.7 (30.9–34.6) | 11.3 (10.3–12.5) | 5.3 (4.6–6.1) | 3.8 (3.1–4.6) |
| Race-ethnicity | |||||
| Non-Hispanic white | 113.2 | 37.5 (35.3–39.7) | 12.7 (11.6–13.8) | 8.0 (7.2–8.9) | 5.9 (5.2–6.7) |
| Non-Hispanic black | 17.8 | 24.4 (22.1–26.9) | 11.0 (9.5–12.8) | 5.6 (4.6–6.8) | 3.3 (2.6–4.1) |
| Hispanic | 26.3 | 18.9 (17.3–20.7) | 6.8 (5.8–8.0) | 4.4 (3.6–5.3) | 2.8 (2.2–3.5) |
| SBP, mm Hg | |||||
| 130–139 | 17.3 | 55.4 (51.3–59.4) | 55.4 (51.3–59.4) | 27.3 (24.4–30.3) | 19.2 (16.5–22.2) |
| ≥140 | 15.0 | 70.5 (67.6–73.3) | 64.9 (61.8–67.9) | 48.2 (44.6–51.8) | 34.9 (31.4–38.5) |
Values are % (95% confidence interval) unless otherwise specified. Treated hypertension was defined by self-reported use of antihypertensive medication with 1 or more classes of antihypertensive medication identified through the pill bottle review. SBP criteria include: 130–180 mm Hg on 0 or 1 antihypertensive medication class; 130 to 170 mm Hg on up to 2 classes; 130 to 160 mm Hg on up to 3 classes; and 130 to 150 mm Hg on up to 4 classes. Criteria for high CVD risk condition include: history of CHD (defined in NHANES as self-report of a prior diagnosis of myocardial infarction, angina, or CHD), eGFR of 20 to 59 ml/min/1.73 m2, 10-year risk for CVD ≥15% calculated using the Framingham risk score for general clinical practice (6), and age ≥75 years. Exclusion criteria include diabetes, history of stroke, >1 g in 24 h of proteinuria, heart failure, eGFR <20 ml/min/1.73 m2, or dialysis treatment in the past year.
CHD = coronary heart disease; CVD = cardiovascular disease; eGFR = estimated glomerular filtration rate; NHANES = National Health and Nutrition Examination Survey; SBP = systolic blood pressure; SPRINT = Systolic Blood Pressure Intervention Trial.
Overall, 16.8 million (95% CI: 15.7 to 17.7 million) U.S. adults met the SPRINT eligibility criteria: 6.6 million (95% CI: 6.0 to 7.1 million) U.S. adults with SBP of 130 to 139 mm Hg and 10.2 million (95% CI: 9.5 to 10.9 million) with SBP ≥140 mm Hg (Figure 2, Online Table 2). Less than one-half of U.S. adults meeting the SPRINT eligibility criteria had treated hypertension (8.2 million [95% CI: 7.6 to 8.8 million]: 3.2 million [95% CI: 2.9 to 3.5 million] with SBP of 130 to 139 mm Hg and 5.0 million [95% CI: 4.6 to 5.4 million] with SBP ≥140 mm Hg) (Online Table 3). There were 8.5 million (95% CI: 8.0 to 9.1 million) U.S. adults not treated for hypertension who met the SPRINT eligibility criteria: 3.3 million (95% CI: 3.0 to 3.6 million) with SBP of 130 to 139 mm Hg and 5.2 million (95% CI: 4.8 to 5.6 million) with SBP ≥140 mm Hg.
FIGURE 2. Number of U.S. Adults Meeting SPRINT Eligibility Criteria, Overall and Among Those With Treated Hypertension.
See Online Table 2 for the numbers and 95% confidence intervals in the figure. Abbreviations as in Figure 1.
SPRINT eligibility criteria were met by 17.6% (95% CI: 16.4% to 18.9%) of U.S. adults ≥50 years of age, 30.0% (95% CI: 28.0% to 32.2%) of those with SBP ≥130 mm Hg, and 28.5% (95% CI: 26.7% to 30.4%) of those with any high CVD risk condition (Table 2). Additionally, 41.3% (95% CI 38.8% to 43.8%) of U.S. adults ≥50 years of age with SBP ≥130 mm Hg met the SPRINT eligibility criteria. Of U.S. adults who also had a high CVD risk condition, 56.9% (95% CI: 53.8% to 60.0%) met the SPRINT eligibility criteria.
TABLE 2.
Percentage of U.S. Adults, Overall and With Treated Hypertension, Meeting the SPRINT Eligibility Criteria in Select Populations
| All Adults |
With Treated Hypertension |
|||
|---|---|---|---|---|
| U.S. Adults (Millions) | Percentage (95% CI) Meeting SPRINT Eligibility Criteria | U.S. Adults (Millions) | Percentage (95% CI) Meeting SPRINT Eligibility Criteria | |
| Age ≥50 yrs | 95.1 | 17.6 (16.4–18.9) | 39.8 | 20.7 (18.8–22.6) |
| SBP ≥130 mm Hg | 55.8 | 30.0 (28.0–32.2) | 23.5 | 35.0 (31.9–38.3) |
| Any high CVD risk condition | 55.8 | 28.5 (26.7–30.4) | 30.7 | 26.8 (24.6–29.1) |
| History of CHD | 10.3 | 15.9 (12.7–19.7) | 6.2 | 18.3 (13.8–23.8) |
| eGFR 20 to 59 ml/min/1.73 m2 | 16.8 | 23.1 (20.4–26.0) | 10.0 | 24.2 (20.1–28.8) |
| Framingham risk score ≥15% | 45.0 | 31.9 (29.6–34.2) | 25.1 | 28.9 (26.3–31.6) |
| Age ≥50 yrs and SBP ≥130 mm Hg | 40.6 | 41.3 (38.8–43.8) | 20.5 | 40.2 (36.8–43.6) |
| Age ≥50 yrs and SBP ≥130 mm Hg with any high CVD risk condition | 29.4 | 56.9 (53.8–60.0) | 16.8 | 49.0 (45.2–52.9) |
Criteria for high CVD risk condition include: history of CHD (defined in NHANES as self-report of a prior diagnosis of myocardial infarction, angina, or CHD), eGFR of 20 to 59 ml/min/1.73 m2, 10-year risk for CVD ≥15% calculated using the Framingham risk score for general clinical practice (6), and age ≥75 yrs.
CI = confidence interval; other abbreviations as in Table 1.
Compared with all U.S. adults ≥50 years of age, those eligible for SPRINT were older and more likely to be male and to be non-Hispanic white versus non-Hispanic black or Hispanic (Table 3). Among U.S. adults who met the SPRINT eligibility criteria, 39.1% (95% CI: 35.5% to 42.9%) had an SBP between 130 and 139 mm Hg, 39.3% (95% CI: 34.1% to 44.7%) among those with treated hypertension.
TABLE 3.
Characteristics of U.S. Adults ≥50 Years of Age Overall and With Treated Hypertension, Overall and Among Those Eligible for SPRINT
| U.S. Population Age ≥50 yrs |
U.S. Population Age ≥50 yrs With Treated Hypertension |
|||
|---|---|---|---|---|
| Overall (n = 95.1 Million) | SPRINT Eligible (n = 16.8 Million) | Overall (n = 39.8 Million) | SPRINT Eligible (n = 8.2 Million) | |
| Age, yrs | ||||
| 50–59 | 42.9 (41.6–44.3) | 21.8 (18.5–25.5) | 29.6 (27.4–32.0) | 17.9 (13.5–23.3) |
| 60–74 | 39.5 (38.1–40.9) | 43.7 (39.6–47.8) | 44.8 (42.6–46.9) | 43.3 (37.9–48.9) |
| ≥75 | 17.6 (16.4–18.8) | 34.5 (31.1–38.1) | 25.6 (23.8–27.5) | 38.8 (34.6–43.1) |
| Female | 53.5 (52.4–54.6) | 44.4 (41.6–47.2) | 56.9 (54.9–58.9) | 51.0 (47.1–55.0) |
| Race/ethnicity | ||||
| Non-Hispanic white | 75.9 (72.0–79.5) | 80.3 (76.2–83.8) | 74.9 (70.4–78.9) | 82.3 (77.9–85.9) |
| Non-Hispanic black | 9.9 (8.0–12.3) | 7.1 (5.5–9.2) | 12.8 (10.2–15.8) | 7.4 (5.4–10.2) |
| Hispanic | 8.4 (6.4–11.0) | 7.6 (5.5–10.5) | 7.6 (5.5–10.5) | 6.6 (4.5–9.6) |
| Current smoker | 15.5 (14.4–16.7) | 16.5 (14.4–18.8) | 11.4 (10.1–12.9) | 9.0 (7.0–11.5) |
| Body mass index, kg/m2 | ||||
| Underweight | 2.6 (2.2–3.0) | 1.7 (1.2–2.4) | 2.8 (2.3–3.5) | 1.7 (1.0–2.9) |
| Normal weight | 24.9 (23.6–26.2) | 27.0 (24.1–30.1) | 16.2 (14.5–18.0) | 23.5 (19.9–27.6) |
| Overweight | 35.4 (33.9–36.8) | 38.1 (35.2–41.1) | 32.9 (30.6–35.2) | 40.0 (35.7–44.5) |
| Obese | 37.2 (35.3–39.1) | 33.2 (30.0–36.6) | 48.2 (45.4–50.9) | 34.8 (31.0–38.8) |
| History of CHD | 9.5 (8.8–10.2) | 9.8 (7.9–12.1) | 14.4 (13.3–15.6) | 13.4 (10.4–18.0) |
| eGFR 20–59 ml/min/1.73 m2 | 15.8 (14.7–17.0) | 23.1 (20.4–26.0) | 24.3 (22.3–26.4) | 29.5 (25.1–34.3) |
| 10-yr CVD risk ≥15% | 44.5 (42.7–46.2) | 85.6 (82.8–88.1) | 60.2 (57.5–62.7) | 88.1 (84.2–91.2) |
| Mean 10-yr CVD risk | 18.3 (17.8–18.9) | 25.0 (24.2–25.7) | 23.7 (22.9–24.6) | 26.6 (25.0–28.1) |
| Systolic blood pressure, mm Hg | ||||
| <130 | 57.3 (55.5–59.1) | 0 | 48.6 (46.3–48.6) | 0 |
| 130–139 | 18.5 (17.4–19.7) | 39.1 (35.5–42.9) | 20.2 (18.9–21.6) | 39.3 (34.1–44.7) |
| 140–149 | 12.0 (11.0–13.0) | 31.3 (28.0–34.8) | 14.7 (13.4–16.2) | 32.4 (27.8–37.3) |
| 150–159 | 5.8 (5.1–6.6) | 16.7 (14.6–19.0) | 7.8 (6.8–9.0) | 16.4 (13.4–19.9) |
| ≥160 | 6.4 (5.5–7.4) | 12.9 (10.4–16.0) | 8.7 (7.4–10.1) | 12.0 (8.5–16.6) |
Values are % or mean (95% confidence interval). Body mass index: underweight <18.5 kg/m2; normal weight 18.5 to 24.9 kg/m2; overweight 25.0 to <30.0 kg/m2; and obese ≥30.0 kg/m2. 10-year CVD risk was calculated by the Framingham risk score for general clinical practice (6).
Abbreviations as in Table 1.
Among U.S. adults who met the SPRINT eligibility criteria, 51.0% (95% CI: 47.8% to 54.1%) were not treated for hypertension (Table 4). Of those eligible for SPRINT, 43.4% (95% CI: 40.3% to 46.5%) did not have any antihypertensive medication identified during their pill bottle review and 7.6% (95% CI: 6.3% to 9.1%) had 1 or more classes of antihypertensive medication identified, but reported not taking the medication to lower their blood pressure. The most common antihypertensive medication classes being taken were ACE-Is, beta-blockers, and thiazide diuretic agents.
TABLE 4.
Antihypertensive Medication Use Among U.S. Adults ≥50 Years of Age and With Treated Hypertension, Overall and Among Those Eligible for SPRINT
| U.S. Population Age ≥50 yrs |
U.S. Population Age ≥50 yrs With Treated Hypertension |
|||
|---|---|---|---|---|
| Overall (n = 95.1 Million) | SPRINT Eligible (n = 16.8 Million) | Overall (n = 39.8 Million) | SPRINT Eligible (n = 8.2 Million) | |
| Number of classes | ||||
| 0* | 58.2 (56.2–60.2) | 51.0 (47.8–54.1) | 0 | 0 |
| 1 | 14.5 (13.4–15.7) | 20.7 (18.1–23.6) | 34.7 (32.4–37.0) | 42.3 (37.1–47.6) |
| 2 | 14.7 (13.7–15.8) | 18.1 (15.1–21.5) | 35.2 (33.1–37.4) | 36.9 (31.4–42.7) |
| ≥3 | 12.6 (11.3–14.1) | 10.2 (8.0–13.0) | 30.1 (27.4–32.9) | 20.9 (16.4–26.2) |
| Classes | ||||
| ACE inhibitor | 20.1 (18.9–21.4) | 18.1 (16.1–20.2) | 42.3 (40.0–44.6) | 33.7 (29.7–38.0) |
| Angiotensin receptor blocker | 12.3 (11.2–13.6) | 12.7 (10.6–15.2) | 27.4 (25.1–29.7) | 24.5 (20.7–28.8) |
| Beta-blocker | 21.0 (19.4–22.7) | 22.9 (20.0–26.2) | 41.5 (38.9–44.1) | 43.1 (38.0–48.4) |
| Calcium-channel blocker | 12.8 (11.6–14.2) | 15.3 (13.2–17.7) | 28.2 (25.6–30.9) | 27.6 (23.8–31.7) |
| Thiazide diuretic agent | 16.8 (15.6–18.1) | 17.9 (15.4–20.8) | 37.6 (35.1–40.2) | 33.8 (29.0–39.0) |
Values are % (95% confidence interval). Number of antihypertensive medication classes included: ACE inhibitors, alpha blockers, aldosterone receptor antagonists, angiotensin-receptor-blockers, beta-blockers, calcium-channel blockers, central-acting agents, loop diuretic agents, potassium-sparing diuretic agents, thiazide diuretic agents, renin inhibitors, and direct acting vasodilators.
U.S. population ≥50 years of age with 0 classes includes adults self-reporting not taking antihypertensive medication and those with no classes of antihypertensive medication identified during the pill bottle review. Of those eligible for SPRINT, 43.4% (95% confidence interval: 40.3% to 46.5%) had no classes of antihypertensive medication and 7.6% (95% confidence interval: 6.3% to 9.1%) had 1 or more classes of antihypertensive medication but reported not taking medication to lower their blood pressure.
ACE = angiotensin-converting enzyme; SPRINT = Systolic Blood Pressure Intervention Trial.
GENERALIZABILITY OF SPRINT TO A BROADER POPULATION
Overall, 38.6% (95% CI: 37.1% to 40.2%) or 84.7 million (95% CI: 81.3 to 88.2 million) U.S. adults had an SBP ≥120 mm Hg and did not have any SPRINT exclusion criteria (Table 5). The percentage of U.S. adults with SBP ≥120 mm Hg, without any SPRINT exclusion criteria, and: 1) ≥50 years of age was 20.9% (95% CI 19.8% to 22.0%); 2) with a high CVD risk was 12.6% (95% CI: 11.9% to 13.3%); and 3) both ≥50 years of age and with high CVD risk was 11.6% (95% CI: 10.9% to 12.3%).
TABLE 5.
Percentage and Number of U.S. Adults With Systolic Blood Pressure ≥120 mm Hg Without SPRINT Exclusion Criteria
| Overall | With Treated Hypertension | Without Treated Hypertension | Hypertension | No Hypertension | |
|---|---|---|---|---|---|
| Percentage (95% CI) | |||||
| Among all U.S. adults | 38.6 (37.1–40.2) | 45.3 (42.5–48.0) | 36.7 (35.3–8.1) | 54.9 (52.3–57.5) | 31.3 (30.0–32.5) |
| Limited to age ≥50 yrs | 20.9 (19.8–22.0) | 36.4 (33.9–38.6) | 16.5 (15.5–7.3) | 39.9 (37.7–41.9) | 12.3 (11.5–13.1) |
| Limited to high CVD risk | 12.6 (11.9–13.3) | 26.4 (24.8–28.3) | 8.6 (8.0–9.0) | 28.8 (27.2–30.5) | 5.2 (4.8–5.6) |
| Limited to age ≥50 yrs and high CVD risk | 11.6 (10.9–12.3) | 25.2 (23.6–27.0) | 7.6 (7.2–8.1) | 27.2 (25.7–28.9) | 4.5 (4.2–4.8) |
| Number in Millions (95% CI) | |||||
| Among all U.S. adults | 84.7 (81.3–88.2) | 22.3 (20.9–23.6) | 62.5 (60.0–64.9) | 37.6 (35.8–39.4) | 47.2 (45.2–49.1) |
| Limited to age ≥50 yrs | 45.8 (43.4–48.3) | 17.9 (16.7–19.0) | 28.0 (26.4–29.5) | 27.3 (25.8–28.7) | 18.6 (17.4–19.8) |
| Limited to high CVD risk | 27.6 (26.1–29.1) | 3.0 (12.2–13.9) | 14.6 (13.7–15.4) | 19.7 (18.6–20.9) | 7.9 (7.3–8.4) |
| Limited to age ≥50 yrs and high CVD risk | 25.5 (24.0–26.9) | 12.4 (11.6–13.3) | 13.0 (12.3–13.8) | 18.7 (17.6–19.8) | 6.8 (6.3–7.3) |
DISCUSSION
In the current analysis, we estimated that 7.6% or 16.8 million U.S. adults meet the SPRINT eligibility criteria and, therefore, might benefit from an SBP goal <120 mm Hg (Central Illustration). Among U.S. adults with treated hypertension, 16.7% or 8.2 million U.S. adults meet the SPRINT eligibility criteria and may benefit from more intensive treatment. Subgroups that were more likely to meet the SPRINT eligibility criteria included older adults, males, and non-Hispanic whites.
CENTRAL ILLUSTRATION. Number of U.S. Adults Meeting Each Sequential SPRINT Eligibility Criterion.
The circles are proportional to the population sizes. CI = confidence interval; CVD = cardiovascular disease; SBP = systolic blood pressure; SPRINT = Systolic Blood Pressure Intervention Trial.
SPRINT enrolled adults taking antihypertensive medication with SBP between 130 and 139 mm Hg. Current hypertension guidelines do not recommend intensification of antihypertensive medication for this population (9). In our analyses, 34.8% of U.S. adults with treated hypertension and an SBP of 130 to 139 mm Hg met the SPRINT eligibility criteria. Also, SPRINT included adults with an SBP of 130 to 139 mm Hg not taking antihypertensive medication. We estimated 19.2% of the U.S. population in this group met the SPRINT eligibility criteria. Current guidelines recommend lifestyle modification for these individuals (10). Although many types of lifestyle modification, including weight loss, reduced alcohol consumption, sodium reduction, and increased physical activity, have been shown to lower blood pressure and reduce the incidence of hypertension, these approaches remain underutilized (11–14). Although there was not a pre-specified subgroup for participants not taking antihypertensive medication prior to SPRINT randomization, these individuals may benefit from lowering SBP to <120 mm Hg using antihypertensive medication.
The 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults recently recommended an SBP threshold of 150 mm Hg for treatment initiation and goal attainment in adults 60 years of age and older without diabetes or chronic kidney disease (9). In our analysis, 19.5% and 34.6% of U.S. adults age 60 to 74 years and ≥75 years, respectively, met the SPRINT eligibility criteria. Age ≥75 years is an a priori defined subgroup in SPRINT. The results from SPRINT may have a substantial effect on the management of hypertension among older U.S. adults.
In the current analysis, only 4.8% of non-Hispanic blacks met the SPRINT eligibility criteria compared with 9.0% of non-Hispanic whites. Reasons for the low percentage of non-Hispanic blacks in the U.S. meeting the SPRINT eligibility criteria include a high percentage of non-Hispanic blacks <50 years of age with SBP ≥130 mm Hg, and a high prevalence in this population of diabetes, stroke, heart failure, and severe chronic kidney disease (15,16). Hispanics were also less likely to meet the SPRINT eligibility criteria compared with non-Hispanic whites. In the current study, Hispanics were more likely to be <50 years of age and, among those treated for hypertension, have SPRINT exclusion criteria (e.g., diabetes, history of stroke) compared with non-Hispanic whites. Disparities in eligibility for SPRINT were also present by sex. Males were more likely to meet the SPRINT eligibility criteria compared with females, due to the lower likelihood of having a high CVD risk condition in females. SPRINT enrolled a substantial number of black (n = 2,802; 29.9% of SPRINT participants), Hispanic (n = 984; 10.5%), and female (n = 3,331; 35.6%) participants. Although race and sex are a priori defined subgroups in SPRINT, given the low number of non-Hispanic blacks, Hispanics, and females in the United States meeting the SPRINT eligibility criteria, consideration of the generalizability of SPRINT results beyond those individuals who strictly meet the eligibility criteria is warranted.
With the completion of SPRINT, an important challenge will be to interpret the generalizability of its results to the broader population of U.S. adults with SBP ≥120 mm Hg. It is neither possible nor practical to repeat large randomized trials in every unstudied group. Clinicians are often encountered with decisions that require extrapolation of trial results beyond the enrolled population. We estimated that 84 million U.S. adults have SBP ≥120 mm Hg and do not have any SPRINT exclusion criteria. The majority of these adults have low CVD risk (i.e., they are <50 years of age or do not have a high-risk CVD condition as defined in SPRINT). Therefore, using antihypertensive medication to lower SBP to <120 mm Hg in this group may not yield substantial CVD benefits. A more appropriate estimate of a population to whom the SPRINT results may be generalizable is the estimated 25.5 million U.S. adults ≥50 years of age with SBP ≥120 mm Hg who are at high CVD risk and who do not have any of the SPRINT exclusion criteria.
Treating hypertension to an SBP <120 mm Hg may not be beneficial and could even potentially be harmful (e.g., medication intolerance, falls, bradyarrhythmias, and hypokalemia and hyperkalemia among other potential adverse effects) in some subgroups (17). Given their low CVD risk, the bene-fits of lowering SBP to <120 mm Hg in adults <50 years of age or in adults ≥50 years of age without high CVD risk may yield less benefit than treating adults meeting the SPRINT eligibility criteria. Extrapolation of SPRINT results to adults outside of those meeting the trial entry criteria should be done with caution.
The cost-effectiveness of lowering SBP to <120 mm Hg is not known. The SPRINT investigators are testing the hypothesis that treating to an SBP goal of <120 mm Hg compared with <140 mm Hg will be cost effective (at ≤$100,000 per quality-adjusted life year gained) (18). This analysis will provide additional information on the benefits and costs of applying the SPRINT results to clinical practice.
STUDY STRENGTHS AND LIMITATIONS
NHANES is designed to provide estimates for the U.S. population and enrolled a large sample size, which allowed us to conduct several subgroup analyses. There are several potential limitations. NHANES did not have information on the presence of reduced left ventricular ejection fraction or subclinical CVD (i.e., coronary calcium score, ankle brachial index, or left ventricular hypertrophy), which were a component of the SPRINT eligibility criteria. Also, NHANES does not have information on other SPRINT exclusion criteria including a history of medication nonadherence.
CONCLUSIONS
Traditionally, an SBP goal of <140 mm Hg has been used as a threshold to guide antihypertensive medication initiation and intensification in adults. SPRINT is a landmark trial with wide-reaching implications for the management of hypertension in adults. The current study suggests that a substantial percentage of U.S. adults meet the eligibility criteria for SPRINT and may derive benefit from an SBP goal of <120 mm Hg.
Supplementary Material
PERSPECTIVES.
COMPETENCY IN SYSTEMS-BASED PRACTICE: In contrast to current clinical practice standards that treat hypertension to an SBP <140 mm Hg, data from the SPRINT trial show that a goal of <120 mm Hg may be beneficial in patients without diabetes or a history of stroke. It is estimated that 16.8 million adults in the United States may be eligible for initiation or intensification of antihypertensive treatment based on these criteria, challenging available resources and systems of care.
TRANSLATIONAL OUTLOOK: Additional analyses are needed to assess the effect of more aggressive blood pressure lowering on neurological and renal function and quantify the medical and economic implications of implementing this more aggressive goal for blood pressure control across the population.
Acknowledgments
This work was supported by the National Institutes of Health (K24-HL125704, Shimbo-PI), from the National Heart, Lung, and Blood Institute, Bethesda, Maryland.
ABBREVIATIONS AND ACRONYMS
- ACEI
angiotensin-converting enzyme inhibitors
- BMI
body mass index
- CHD
coronary heart disease
- DBP
diastolic blood pressure
- eGFR
estimated glomerular filtration rate
- SBP
systolic blood pressure
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
APPENDIX For supplemental tables, please see the online version of this article.
REFERENCES
- 1.Ambrosius WT, Sink KM, Foy CG, et al. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials. 2014;11:532–46. doi: 10.1177/1740774514537404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Heart, Lung, and Blood Institute [September 19, 2015];Landmark NIH study shows intensive blood pressure management may save lives. Available at: http://www.nhlbi.nih.gov/news/press-releases/2015/landmark-nih-study-shows-intensive-blood-pressure-management-may-save-lives.
- 3.Centers for Disease Control and Prevention [September 10, 2015];National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation. Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 4.Mirel LB, Mohadjer LK, Dohrmann SM, et al. National Health and Nutrition Examination Survey: estimation procedures, 2007–2010. Vital Health Stat. 2013;159:1–17. [PubMed] [Google Scholar]
- 5.Levey AS, Bosch JP, Lewis JB, et al. Modification of Diet in Renal Disease Study Group A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999;130:461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 6.D'Agostino RB, Sr., Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 7.Coresh J, Astor BC, McQuillan G, et al. Calibration and random variation of the serum creatinine assay as critical elements of using equations to estimate glomerular filtration rate. Am J Kidney Dis. 2002;39:920–9. doi: 10.1053/ajkd.2002.32765. [DOI] [PubMed] [Google Scholar]
- 8.LaVange LM, Stearns SC, Lafata JE, et al. Innovative strategies using SUDAAN for analysis of health surveys with complex samples. Stat Methods Med Res. 1996;5:311–29. doi: 10.1177/096228029600500306. [DOI] [PubMed] [Google Scholar]
- 9.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 10.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 11.Neter JE, Stam BE, Kok FJ, et al. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 12.Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 13.Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–7. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 14.Sacks FM, Svetkey LP, Vollmer WM, et al. DASH-Sodium Collaborative Research Group Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 15.Hertz RP, Unger AN, Cornell JA, et al. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 16.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 17.Group AS, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. [October 18, 2015];Systolic Blood Pressure Intervention Trial (SPRINT) protocol version 4.0. Available at: https://www.sprinttrial.org/public/Protocol_Current.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.