Abstract
Objective
In a randomized controlled trial we compared two models of community health worker (CHW)-led diabetes medication decision support for low-income Latino and African American adults with diabetes. Most outcomes were improved when CHWs used either an interactive e-Health tool or print materials. This paper investigates mediators and moderators of improved medication adherence in these two models.
Methods
Because both programs significantly improved satisfaction with medication information, medication knowledge, and decisional conflict, we examined whether improvements in each of these outcomes in turn were associated with improvements in self-reported medication adherence, and, if so, whether these improvements were mediated by improvements in diabetes self-efficacy or diabetes distress. Potential moderators of improvement included gender, race/ethnicity, age, education, insulin use, health literacy, and baseline self-efficacy, diabetes distress, and A1c.
Results
A total of 176 participants (94%) completed all assessments. After adjusting for potential confounders, only increased satisfaction with medication information w as correlated with improved medication adherence (p=0.024). Improved self-efficacy, but not diabetes distress, was associated with improvements in both satisfaction with medication information and medication adherence. However, the Sobel-Goodman Mediation test did not support improvements in self-efficacy as a mechanism by which improved satisfaction led to better adherence. None of the examined variables achieved statistical significance as moderators.
Conclusions
Improvements in satisfaction with medication information but not in medication knowledge or decision conflict were associated with improvements in medication adherence. Interventions that target low-income ethnic and racial minorities may need to focus on increasing participants’ satisfaction with information provided on diabetes medications and not just improving their knowledge about medications. Future research should explore in more depth other possible mediators and moderators of improvements in medication adherence in low -income minority populations.
Keywords: chronic disease management, tailored or targeted Interventions, computer-mediated health promotion, diabetes, health behavior, lay health workers, patient education, randomized controlled trial, self-management, community health worker, tailored, e-health
Introduction
Over 25 million people in the United States have Type 2 diabetes( Centers for Disease Control and Prevention). The demands of managing diabetes are costly, complex, and time consuming( American Diabetes Association, 2013). Patients must initiate and sustain multiple self-management behaviors between health care visits( Montori, Gafni, & Charles, 2006). Yet, patient adherence to prescribed medications and other recommended self-management behaviors is often low( Cramer, 2004), which can lead to increased rates of hospitalizations, emergency room visits(Jha, Aubert, Yao, Teagarden, & Epstein, 2012), complications, and mortality( Ho et al., 2006). Diabetic patients from ethnic minorities and of lower socio-economic status tend to have lower medication adherence( Rolnick, Pawloski, Hedblom, Asche, & Bruzek, 2013; Trinacty et al., 2009), higher risk of morbidity and mortality, and lower quality of care than white and higher SES patients( Lanting, Joung, Mackenbach, Lamberts, & Bootsma, 2005).
There is thus a pressing need to develop interventions to support and improve self-management among low-income, ethnic and racial minority diabetic patients. A growing body of evidence supports the effectiveness of interventions that are culturally tailored( Peek, Cargill, & Huang, 2007), involve one-on-one interpersonal interactions with trusted supporters such as community health workers (CHWs) (Betancourt, Duong, & Bondaryk, 2012), and are community-based( M. Shah, Kaselitz, & Heisler, 2013). CHWs both educate and provide support to patients, thereby increasing patients’ confidence and motivation to care for their diabetes (Heisler et al., 2009). Interventions using CHWs have found improvements in HbA1cand diabetes knowledge (Duggan et al., 2014) and could therefore be a powerful tool for reducing diabetes health disparities. Tailorede-Health tools also show promise for patient education and decision support, but have not been widely tested in CHW and other lay health worker interventions among populations with low health literacy.
Many factors influence whether patients take their diabetes medications as prescribed (Anderson & Funnell, 2000). Both patients’ knowledge of medications (MK)(Ahmad, Ramli, Islahudin, & Paraidathathu, 2013; Al-Qazaz et al., 2011; Munoz, Dorado, Guerrero, & Martinez, 2014; Weymiller et al., 2007)and satisfaction with information provided on their prescribed medications (SMI)( Alhewiti, 2014; Horne, Hankins, & Jenkins, 2001) have been associated with medication adherence. Medication knowledge has long been acknowledged as important in understanding of and adherence to medication regimens. However, individuals differ in their preferences for the amount of information received and means of information delivery( Horne et al., 2001). Satisfaction with medication information is thus also an important measure to assess quality of an education intervention.
In a recent randomized controlled trial (M. Heisler et al., 2014) we examined whether two CHW-led approaches would improve satisfaction with diabetes medication information, diabetes medication knowledge, and decrease medication decisional conflict among low-income Latino and African American Adults with Type 2 diabetes receiving care at a federally qualified health center in southwest Detroit. Participants were randomized to one of two groups receiving a brief community health worker (CHW)-led intervention consisting of an initial home visit and two follow-up calls. One group received the services of the CHW using the iPad decision aid (iDecide) tool, an interactive tailored e-health tool, while the other received the CHW services providing the same information through printed diabetes materials. The print materials included both information on diabetes and diabetes medications(oral and insulin )including effectiveness, cost, and side effects. The iDecide tool was designed to be more accessible to patients with low health literacy. It consisted of animations describing diabetes disease processes, graphical depictions related to the patient’s personal diabetes risk profile, and interactive options for patients to explore how their risk profile could change at different A1c levels and how they could choose a specific medication based on their preferences related to cost, effectiveness, and side effects.
Both groups achieved significant improvements in the main outcomes of satisfaction with medication information, medication knowledge, and decisional conflict three months after the intervention. Improvements in satisfaction with medication information and diabetes distress in the iDecide group were significantly greater than in the printed materials group. Tables 1 and 2 contain participant baseline screening characteristics and each measure’s means and standard deviations at baseline and 3-month follow-up, respectively.
Table 1.
Participant Baseline Screening Characteristics (N=188)
| Characteristic | iDecide (N=93) | Print Materials (N=95) | Between-Group Difference | ||
|---|---|---|---|---|---|
|
| |||||
| % or mean (SD) | N. of missing | % or mean (SD) | N. of missing | P-value | |
| Age in years | 51 (8.6) | 0 | 52 (9.4) | 0 | 0.42 |
| Female gender | 76% | 0 | 66% | 1 | 0.12 |
| Hispanic | 53% | 0 | 61% | 1 | 0.28 |
| African American | 41% | 0 | 32% | 0 | 0.19 |
| Health Literacy†: | |||||
| Confident filling forms | 2.3 (1.3) | 0 | 2.9 (1.5) | 0 | 0.003 |
Note:
Values in health literacy range from 1 to 5 (1=Always and 5=Never).
Table 2.
Summary of Main Outcome Variables and Potential Mediators
| Variable | Group | Outcome Measure in Time Point = (unadjusted) | Change over Time (adjusted) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Time 1: Baseline | Time 3: Three Months Later | Time 3 – 1: From Baseline to 3 Months | ||||||||
|
| ||||||||||
| N = 188 | Mean (SD) | Between group P-value | N = 176 | Mean (SD) | Between group P-value | Mean (95% CI) | Within Group P-value | Between group P-value | ||
| Medication Adherence (MA) | 95 | 83.9 (19.2) | 0.45 | 89 | 89.7 (11.9) | 0.86 | 5.7 (2.5 to 8.8) | <0.001 | 0.33 | |
| iDecide | 93 | 87.2 (13.7) | 87 | 90.5 (10.8) | 3.4 (0.2 to 6.6) | 0.036 | ||||
|
| ||||||||||
| MAIN OUTCOME VARIABES | ||||||||||
|
| ||||||||||
| Satisfaction with Medication Information (SMI) | 95 | 77.4 (28.7) | 0.10 | 89 | 87.6 (17.9) | 0.29 | 10.2 (4.5 to 15.9) | <0.001 | 0.007 | |
| iDecide | 93 | 68.6 (33.4) | 87 | 90.4 (17.2) | 21.5 (15.7 to 27.3) | <0.001 | ||||
| Medication Knowledge (MK) | 95 | 34.8 (17.4) | 0.93 | 89 | 45.7 (21.8) | 0.84 | 10.8 (6.4 to 15.1) | <0.001 | 0.51 | |
| iDecide | 93 | 34.8 (17.6) | 87 | 47.4 (18.5) | 12.8 (8.4 to 17.2) | <0.001 | ||||
| Decisional Conflict (DC) | 95 | 60.7 (16.2) | 0.07 | 89 | 72.3 (13.2) | 0.53 | 11.5 (8.2 to 14.8) | <0.001 | 0.3 | |
| iDecide | 93 | 56.6 (15.7) | 86 | 70.9 (13.7) | 14.1 (10.7 to 17.4) | <0.001 | ||||
|
| ||||||||||
| POTENTIAL MEDIATORS | ||||||||||
|
| ||||||||||
| Self-Efficacy (SE) | 95 | 75.0 (19.2) | 0.98 | 89 | 80.0 (16.6) | 0.05 | 4.8 (1.8 to 7.7) | 0.002 | 0.13 | |
| iDecide | 93 | 74.6 (19.3) | 87 | 83.3 (19.5) | 8.1 (5.0 to 11.1) | <0.001 | ||||
| Diabetes Distress (DD) | 95 | 68.0 (26.5) | 0.21 | 89 | 66.5 (30.7) | 0.05 | −1.6 (−6.9 to 3.7) | 0.555 | <0.001 | |
| iDecide | 93 | 62.7 (28.3) | 87 | 76.9 (22.3) | 14.1 (8.7 to 19.5) | <0.001 | ||||
Note: Means of each outcome measure at each time point are unadjusted. Means in changes in each outcome measure are estimated from linear mixed-effect models, adjusted for baseline health literacy. All self-reported scales have a range of 0–100 with more positive outcomes reflected by higher numbers (e.g., less medication decisional conflict, higher levels of self-reported medication adherence, and lower diabetes distress are closer to 100). P-values are bolded if less than 0.05.
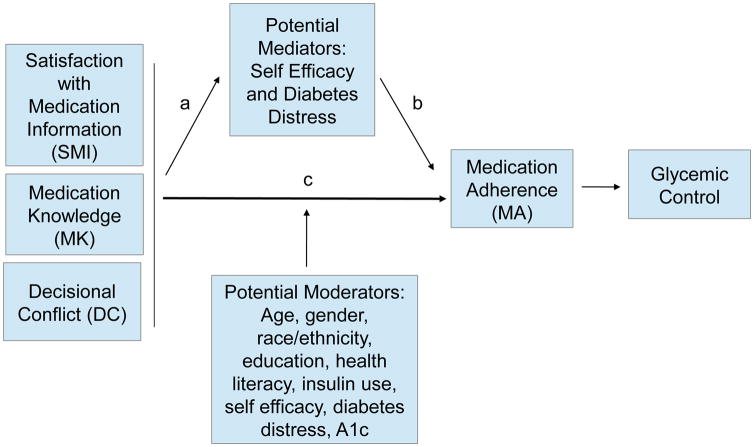
To guide the development of future interventions building on this work, it is important to understand whether the improvements observed in our primary outcomes of satisfaction with medication information, medication knowledge, and decisional conflict were in turn associated with improvements in medication adherence. In designing our decision support intervention, we hypothesized that these three outcomes would be associated with improved medication adherence. If one or more of these primary outcomes were associated with improved medication adherence, it is also important to understand the mechanisms (“mediators”) for these observed effects. Multiple studies have found strong associations between increased self-efficacy (SE) (K. R. Lorig et al., 2001; Mishali, Omer, & Heymann, 2011; Nakahara et al., 2006; K. M. Nelson, McFarland, & Reiber, 2007) and decreased diabetes distress (DD)(Aikens, 2012; Fisher, Glasgow, & Strycker, 2010; Fisher et al., 2013) with improved medication adherence and other diabetes clinical outcomes. We hypothesized that by improving participants’ satisfaction with information received on their diabetes medications, knowledge of these medications, and decisional conflict about taking these medications, our intervention might in turn increase their self-efficacy and reduce the distress associated with their diabetes, both of which could contribute to improvements in medication adherence.(see figure 1) The current study was not powered to detect differences in A1c of less than 0.5%. Medication adherence was thus our main outcome variable, but we included glycemic control in our conceptual model as a reminder that medication adherence is an important contributor to glycemic control.
Figure 1.
Conceptual Model
Equally important as identifying mediators of effects is understanding characteristics of participants who gained the most benefit from these CHW-led interventions in order to guide targeting of future similar interventions. Such baseline characteristics that show an interactive effect with intervention outcomes are called ‘moderators’ (Kraemer, Wilson, Fairburn, & Agras, 2002). In this paper, we examined potential mediators and moderators of the intervention’s effect according to the original conceptual model that informed the design of the intervention (Figure 1). Along with baseline patient characteristics such as age, gender, race/ethnicity, education level, health literacy, insulin use, and A1c, we also examined baseline self-efficacy and diabetes distress levels as potential moderators as we hypothesized participants with low self-efficacy and high diabetes distress at baseline might benefit disproportionately from the intervention—even if intervention effects were not mediated by improvements in these.
Our specific questions were:
Are improvements achieved in both intervention groups in satisfaction with diabetes medication information, medication knowledge, and decisional conflict in turn associated with improvements in medication adherence?
Are diabetes self-efficacy or diabetes distress significant mediators in the relationship between improvements in our primary outcomes and changes in medication adherence?
Do baseline characteristics of age, gender, race/ethnicity, education level, health literacy, insulin use, self-efficacy, diabetes distress or A1c moderate the relationship between change in our primary outcomes and change in medication adherence?
Methods
Setting, Recruitment, Intervention, and Measures
Details on recruitment, interventions, outcomes, and results of the RCT are described briefly above and in detail elsewhere (M. Heisler et al., 2014). Self-reported outcome measures were collected using validated surveys at baseline and 3 months. All measures were scaled from 0 to 100, with higher numbers indicating more positive outcomes (e.g., better medication adherence, lower diabetes distress). Outcome measures included the following(see Appendix A for complete measures):
-
1
Medication adherence: a validated 8-item scale of self-reported medication adherence (Morisky, Green, & Levine, 1986). Participants were asked to consider their diabetes medications in answering the questions.
-
2
Satisfaction with medication information: this 3-item scale has been used in prior diabetes medication decision tool RCT s(Mullan et al., 2009; Weymiller et al., 2007). Participants are asked to describe their satisfaction with the amount, clarity, and helpfulness of the information they had received from their health care team (including CHWs)about their “blood sugar medications ”.
-
3
Medication knowledge (MK): This consists of 11 true/false questions about the effects of diabetes medications( Weymiller et al., 2007).
-
4
Decisional conflict (DC): this scale consists of 16 questions focusing on the confidence the participant felt about key aspects of decision-making about their anti-hyperglycemic medications.(O’Connor, 1995).
Scales used to assess potential mediators and moderators were:
-
5
Diabetes Self-efficacy (SE): This 5-item scale focuses on how confident the participant feels in five key areas related to managing diabetes (A. Lorig, 1986).
-
6
Diabetes distress (DD):This is a 2-item scale assessing the extent to which the participant has been troubled over the prior month by “feeling overwhelmed by the demands of living with my diabetes” and/or“ feeling that I am often failing with my health routine.” (Polonsky et al., 2005).
-
7
Health literacy: This was measured with a single validated item: “How often do you have problems understanding written materials?” with five response options ranging from ‘Always’ to ‘Never’. (Chew, Bradley, & Boyko, 2004)
Both groups improved significantly for most outcomes over the three months(see Table 2) (M. Heisler et al., 2014). Thus, in the analysis of the current paper we examined whether the observed improvements in the outcomes in both groups were associated with medication adherence and what baseline characteristics in both groups may have moderated improvements in outcomes.
Statistical Analyses
To examine whether changes in satisfaction with medication information, medication knowledge, or decisional conflict were associated with changes in medication adherence over the course of the three-month intervention, we performed bivariate and multivariate linear regressions with each of these as the principal independent variables and change in adherence as the outcome variable. Covariates include gender, race/ethnicity, and health literacy.
We next conducted tests of whether self-efficacy or diabetes distress were mediators in the bivariate relationships between each of our three primary outcomes and medication adherence. We sequentially assessed the following relationships because for a variable to be a mediator there must be a significant relationship between each of the following (see Fig. 1 for mediation model):
Between the explanatory variable and the outcome (c);
Between the explanatory variable and the potential mediator (a);
Between the potential mediator and the outcome variable (b);
Multivariate linear regressions were used to determine the significance of each relationship. If all three relationships were significant, then Sobel-Goodman Mediation Tests were conducted to assess whether the relationship (c) decreased significantly upon the addition of the mediator to the model(Aroian, 1944; Bruin, 2006; MacKinnon & Dwyer, 1993; Mackinnon, Warsi, & Dwyer, 1995; Preacher & Hayes, 2004).
Finally, we assessed whether socio-demographic factors (sex, race/ethnicity, age) or baseline clinical and psychosocial attributes (education level, health literacy, insulin use, HbA1c, self-efficacy, diabetes distress) moderated the relationship between change in satisfaction with medication information, medication knowledge or decisional conflict and change in adherence. For this analysis we added an interaction term of each of the three explanatory variables and the potential moderator to the multivariate linear regression with change in adherence as the outcome variable. We then examined the significance of the interaction term to determine whether the relationship was significantly different for different subgroups. Finally, we examined relationships between change in each of our primary outcomes and change in medication adherence within each subgroup.
Results
Description of the Sample
A total of 176 participants (94%) completed all assessments. Relevant patient baseline characteristics are reported in Table 1. The average age was 51.5 years, 71% were women, 57% were Latino, 50% were African American, 31% were unemployed, and mean HbA1c was 8.22%.
Results of Main Relationships
Results from linear regressions showed a significant association between change in satisfaction with medication information and change in medication adherence (p=0.024). This relationship remained significant after controlling for gender, race/ethnicity, and health literacy (p=0.019). However, changes in medication knowledge and in decisional conflict were not significantly related with change in adherence (p=0.67 and p=0.14 respectively) (Table 3).
Table 3.
Main Relationships
| Outcome Variables | Outcome: Correlation with Change in Medication Adherence | |||
|---|---|---|---|---|
|
| ||||
| Bivariate | Multivariate* | |||
|
| ||||
| Coefficient | P-value | Coefficient | P-value | |
| 1) Change in Satisfaction with Medication Information | 0.084 | 0.024 | 0.092 | 0.019 |
| 2) Change in Medication Knowledge | 0.085 | 0.140 | 0.085 | 0.155 |
| 3) Change in Decisional Conflict | 0.031 | 0.674 | 0.035 | 0.646 |
Covariates include sex, race/ethnicity, and baseline health literacy level. P-values are bolded if less than 0.05.
Results of Mediator Analysis
Change in satisfaction with medication information was the only study outcome variable that was significantly associated with change in medication adherence. Therefore, we focused on the relationship between change in satisfaction and change in adherence to assess whether diabetes self-efficacy and diabetes distress were potential mediators in the relationship. As shown in Table 4, self-efficacy was significantly related with change in satisfaction with medication information (coef 0.087, p=0.022) and with change in adherence (coef 0.165, p=0.039) while diabetes distress was not. To determine the indirect effect--the amount of variation in change in adherence as explained by change in satisfaction with medication information through the mechanism of change in self-efficacy – we then performed the Sobel-Goodman Mediation tests. The test results did not support self-efficacy as a significant mediator, as the effect of change in satisfaction with medication information on change in adherence was not significantly reduced by the addition of self-efficacy to the model (indirect effect=0.012, p=0.169).
Table 4.
Results of Mediation Tests.
| Potential Mediator | Correlation with predictor and outcome* | Sobel-Goodman Mediation Test | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Change in SMI (relationship a) | Change in MA (relationship b) | |||||
|
|
||||||
| Coefficient | P-value | Coefficient | P-value | Indirect effect | P-value | |
| 1) Self-efficacy | 0.087 | 0.022 | 0.165 | 0.039 | 0.012 | 0.169 |
| 2) Diabetes Distress | 0.104 | 0.137 | - | - | - | - |
See figure 1 for mediation model. P-values are bolded if less than 0.05.
Results of Moderator Analyses
Table 5 shows the results of the moderator analyses. The group difference in the association between change in satisfaction with medication information and change in medication adherence was not statistically significant for any of the potential moderators, although there was a trend toward significance for baseline A1C level (<=7 vs >7; p=0.060). Our subgroup analyses show that the relationship was significant for those with high baseline A1c (coef 0.173, p=0.003), but not for those with lower baseline A1c (coef 0.031, p=0.543). Similarly, change in satisfaction with medication information was significantly associated with change in adherence for women (coef 0.098, p=0.033) and participants not using insulin at baseline (coef 0.133, p=0.014), with high self-efficacy (coef 0.138, p=0.014), with less than a high school education (coef 0.134, p=0.016), with identifying as African American (coef. 0.046, p=0.046) and with lower health literacy levels (coef 0.136, p=0.005). We did not find any significant relationship between change in satisfaction with medication information and change in adherence among men, or among participants using insulin, with low self-efficacy, with more than a high school education, identifying as Latin, or with higher health literacy levels.
Table 5.
Moderator Results
| Potential Moderator | Coefficient | p-value | Difference in Coefficient | p-value |
|---|---|---|---|---|
| Gender | ||||
| Female | 0.098 | 0.033 | 0.022 | 0.804 |
| Male | 0.076 | 0.317 | ||
| Race/Ethnicity | ||||
| Hispanic | 0.075 | 0.221 | H&AA: 0.036 H&O: 0.017 |
0.658 0.911 |
| African American | 0.112 | 0.046 | ||
| Other | 0.092 | 0.497 | ||
| Age | ||||
| <50 | 0.100 | 0.134 | 0.022 | 0.789 |
| ≥50 | 0.079 | 0.097 | ||
| Education Level | ||||
| < High School | 0.134 | 0.016 | 0.077 | 0.314 |
| ≥ High school | 0.056 | 0.313 | ||
| Health Literacy | ||||
| Low | 0.136 | 0.005 | 0.112 | 0.119 |
| High | 0.017 | 0.786 | ||
| Insulin Use | ||||
| Not using | 0.133 | 0.014 | 0.079 | 0.297 |
| Using | 0.055 | 0.318 | ||
| Baseline Self-efficacy | ||||
| Low | 0.023 | 0.672 | 0.116 | 0.125 |
| High | 0.138 | 0.013 | ||
| Baseline Diabetes Distress | ||||
| Low | 0.073 | 0.113 | 0.043 | 0.603 |
| High | 0.116 | 0.101 | ||
| Baseline HbA1c | ||||
| ≤ 7% | 0.031 | 0.543 | 0.142 | 0.060 |
| > 7% | 0.173 | 0.003 |
P-values are bolded if less than 0.05.
Discussion
In this sample of low-income Latino and African American adults with diabetes, improvements in satisfaction with medication information were associated with better medication adherence, but improvements in medication knowledge and decisional conflict were not. Among examined possible mechanisms by which improved satisfaction with medication information led to improved medication adherence, improved diabetes self-efficacy was associated with improvements in both satisfaction with medication information and medication adherence, but these improvements did not meet rigorous analytical standards to be considered a mediator of the improvements. Similarly, none of our examined participant characteristics met criteria to be considered moderators of the relationship between improved satisfaction with medication information and medication adherence. Thus, our principal positive finding was that satisfaction with medication information was the only study outcome independently associated with concomitant improvements in participants’ medication adherence.
This finding builds on prior research showing that, especially among historically underserved racial and ethnic groups, feeling trust in one’s health care providers and satisfaction in their communication and information provided are central to improving important health behaviors such as adherence (Salvalaggio et al., 2013; van Servellen & Lombardi, 2005). In an earlier study among diabetes patients in this same clinic population, we found that objective knowledge of one’s last A1c was associated with better diabetes care understanding but not with better diabetes care self-efficacy or reported self-management behaviors( Heisler, Piette, Spencer, Kieffer, & Vijan, 2005). Studies among ethnic and racial minority adults with diabetes or hypertension similarly have found that higher levels of trust in health care providers are associated with increased medication adherence (Elder et al., 2012), satisfaction( White et al., 2015), reduced emotional disease burden (Slean, Jacobs, Lahiff, Fisher, & Fernandez, 2012), and improved disease self-care (Bonds et al., 2004). More broadly, trust has also been correlated with self-reported health outcomes( Safran et al., 1998), patient satisfaction, continuity with the same provider, and medication adherence (Thom, Ribisl, Stewart, & Luke, 1999). Further, positive evaluations of providers’ communication and shared decision-making are associated with increased engagement in communication with providers( Lyles et al., 2013)while negative evaluations are associated with medication non-adherence(Bauer et al., 2014; Ratanawongsa et al., 2013).
Especially among populations who have experienced disproportionate levels of discrimination and poor treatment in formal institutions such as health care systems, it is not surprising that feelings of trust in and satisfaction with the information provided on their medications are such strong predictors of improved medication adherence. Since Community Health Workers (CHWs) share cultural and linguistic similarities with the population of patients they serve, they are especially well-positioned to increase trust in and satisfaction with the information they provide. This is also likely another important factor explaining the effectiveness of CHW interventions in these populations (M. Shah et al., 2013; M. K. Shah, Heisler, & Davis, 2014; Spencer et al., 2011).
Although both of our interventions effectively decreased participants’ conflict about making decisions about their anti-hyperglycemic medications, this decrease was not an independent contributor to improved medication adherence. Many decision aid developers have argued that reducing decisional conflict should be an important objective of decision aids. Yet, our findings are similar to the findings of a 2014 Cochrane Review on 115 studies of effectiveness of decision aids for people facing health treatment or screening decisions. That review concluded that although there was high-quality evidence that decision aids compared to usual care reduced decisional conflict related to feeling uninformed and unclear about their personal values, this reduction did not translate into improved adherence with the chosen option (Stacey et al., 2014, Issue 1). Moreover, while the measure we used for decisional conflict has been used repeatedly in studies on the effectiveness of decision aids, most of these have evaluated aids for decisions about one-time treatment options (e.g., breast cancer surgical options)and not for long -term treatment options. Although almost half of our study participants were eligible for our study because they voiced concerns or difficulty taking their diabetes medications, it is not clear that high decisional conflict about their medication choices was a significant factor in their difficulties. Moreover, a growing number of experts argue that decisional conflict is not necessarily a bad thing, especially in the face of the ongoing decisions that of necessity must be made about taking long-term medications in which ambivalence, revision, and changing one’s mind may be beneficial( W. L. Nelson, Han, Fagerlin, Stefanek, & Ubel, 2007). For example, Nelson et al suggest that understanding the uncertainty of outcomes can result in a high decisional conflict score, regardless of a patient’s satisfaction with her decision in the face of that uncertainty. Thus, although the interventions led on average to decreased decisional conflict, it is thus perhaps not surprising that these decreases did not in turn translate into improved medication adherence.
None of our hypothesized moderators of improvements were significant. Several prior studies of models in which lay workers or peers provide more intensive support and educational outreach to adults with diabetes have found that these interventions are especially effective in participants with low health literacy and high baseline levels of diabetes distress, poor medication adherence and self-management(Moskowitz, Thom, Hessler, Ghorob, & Bodenheimer, 2013; Piette, Resnicow, Choi, & Heisler, 2013; Rothman et al., 2004). In our sample, while there was a trend toward significantly greater effectiveness among participants with lower levels of formal education and health literacy, this did not achieve statistical significance. Of note, however, most of our study participants had relatively low health literacy, and 52% of all participants had less than a high school education. We thus had less variation in these participant characteristics than some prior studies.
Limitations
This study has several limitations. First, this study was conducted at a single federally qualified health center and thus our results may not generalize to other settings or populations. Second, low variation in several of the variables may have contributed to the limited ability to detect moderator effects. Lastly, there are also likely other potential moderators and mediators of intervention effectiveness that may be important and were not measured in this study. For example, our findings on the importance of participants’ improvements in their satisfaction with the information received on diabetes medications suggests that trust in providers might be both an important mediator and moderator of intervention effects. Another important mediator that we did not examine is participants’ level of motivation to take medications and improve medication adherence. Further research is needed to identify and understand unmeasured aspects of these interventions that contributed to their effectiveness. However, in light of the paucity of prior research on effective medication decisional support for low-income populations with low health literacy and formal education, this study points to a number of promising directions for research. In particular, future assessments should include well-validated measures of levels of trust and satisfaction with key aspects of information and service delivery, as well as on the potentially crucial role of trust in the individuals delivering interventions.
Implications for Research and Practice
Our key finding was that improvements in satisfaction with medication information were associated with increases in medication adherence. An important implication of this finding for research is the need to identify what aspects of interventions enhance satisfaction with information received. In both arms of this intervention, the intervention was delivered by trusted community health workers in home visits in which the worker took time to review information on diabetes medications and address participants’ questions. This face-to-face relationship in a home setting appeared to increase satisfaction with the information on medications provided regardless of whether the information was through an interactive, tailored e-health tool or through print materials.
Our findings suggest the importance of including measures of satisfaction with information provided in assessments of educational programs. They further suggest that decisional conflict may not be an important outcome measure in the evaluations of efforts to inform long-term and reversible decisions in the same way that it has been used for time-sensitive and irreversible decisions, such as with breast cancer treatment. Finally, we underscore the importance of further investigation into the mediators and moderators of medication adherence among low-income and minority patients. This knowledge will be invaluable to better designing and targeting future interventions to improve the health of underserved patients.
Conclusion
In conclusion, in the two models of CHW-led medication decision support we evaluated, observed improvements in satisfaction with the information received on diabetes medications, but not medication knowledge or decisional conflict, were associated with improvements in diabetes medication adherence in this study population of low-income Latino and African American adults. Interventions that target low-income ethnic and racial minorities need to focus on increasing participants’ satisfaction with the information provided on diabetes medications and not just improving their knowledge about medications.
Acknowledgments
This research was supported by a Grant from AHRQ (R18 DK078558) and by Grant Number P30DK092926 (MCDTR) from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have no conflict of interest or financial disclosures. The funding sources had no role in the study design; data collection; administration of the interventions; analysis, interpretation, or reporting of data; or decision to submit the findings for publication.
APPENDIX: Outcome Scales
A. MEDICATION ADHERENCE(MA): MORISKY MEDIC ATION ADHERENCE SCALE
| Responses: | Never | Rarely | Sometimes | Often | Always |
| |||||
B. MEDICATION KNOWLEDGE (MK)
| Responses: | True | False | Don’t Know |
| |||
C. SATISFACTION WITH MEDICATION INFORMATION
| Scale: | 1 = Too little information | to | 4 = Just the right amount of information | to | 7 = Too much information |
| |||||
| Scale: | 1 = Not at all clear | to | 4 = Somewhat clear | to | 7 = Extremely clear |
| |||||
| Scale: | 1 = Not at all helpful | to | 4 = Somewhat helpful | to | 7 = Extremely helpful |
| |||||
Note: Only #3 (satisfaction with helpfulness of medication information) was used in the present study, as these were considered to be measuring different questions.
D. DECISIONAL CONFLICT (DC): FROM O’CONNOR
| Responses: | Strongly | Disagree | Neither agree nor disagree | Agree | Strongly agree disagree |
| |||||
E. SELF-EFFICACY (SE): LORIG SELF-EFFICACY SCALE
| Scale: | 1 = Not at all confident | to | 10 = Totally confident |
| |||
F. DIABETES DISTRESS SCALE (DD)
| Responses: | Not a problem | A slight problem | A moderate problem | A somewhat serious problem | A serious problem | A very serious problem |
| ||||||
G. HEALTH LITERACY SCALE: CHEW HEALTH LITERACY SCREENING
| Responses: | Extremely | Quite a Bit | Somewhat | A Little | Not at All |
| |||||
References
- Ahmad NS, Ramli A, Islahudin F, Paraidathathu T. Medication adherence in patients with type 2 diabetes mellitus treated at primary health clinics in Malaysia. Patient Prefer Adherence. 2013;7:525–530. doi: 10.2147/PPA.S44698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aikens JE. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care. 2012;35(12):2472–2478. doi: 10.2337/dc12-0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Qazaz H, Sulaiman SA, Hassali MA, Shafie AA, Sundram S, Al-Nuri R, Saleem F. Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. Int J Clin Pharm. 2011;33(6):1028–1035. doi: 10.1007/s11096-011-9582-2. [DOI] [PubMed] [Google Scholar]
- Alhewiti A. Adherence to Long-Term Therapies and Beliefs about Medications. Int J Family Med. 2014;2014:479596. doi: 10.1155/2014/479596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2013;36(Supplement):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26(4):597–604. doi: 10.1177/014572170002600405. [DOI] [PubMed] [Google Scholar]
- Aroian LA. The probability function of the product of two normally distributed variables. Annals of Mathematical Statistics. 1944;18:265–271. [Google Scholar]
- Bauer AM, Parker MM, Schillinger D, Katon W, Adler N, Adams AS, … Karter AJ. Associations between antidepressant adherence and shared decision-making, patient-provider trust, and communication among adults with diabetes: diabetes study of Northern California (DISTANCE) J Gen Intern Med. 2014;29(8):1139–1147. doi: 10.1007/s11606-014-2845-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt JR, Duong JV, Bondaryk MR. Strategies to reduce diabetes disparities: an update. Curr Diab Rep. 2012;12(6):762–768. doi: 10.1007/s11892-012-0324-1. [DOI] [PubMed] [Google Scholar]
- Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:26. doi: 10.1186/1471-2296-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruin J. sgmediation: command to compute Sobel-Goodman mediation tests. UCLA: Statistical Consulting Group; 2006. Retrieved 1/9/2015, from http://www.ats.ucla.edu/stat/stata/faq/sgmediation.htm. [Google Scholar]
- Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta, GA: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–1224. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- Duggan C, Carosso E, Mariscal N, Islas I, Ibarra G, Holte S, … Thompson B. Diabetes prevention in Hispanics: report from a randomized controlled trial. Prev Chronic Dis. 2014;11:E28. doi: 10.5888/pcd11.130119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder K, Ramamonjiarivelo Z, Wiltshire J, Piper C, Horn WS, Gilbert KL, … Allison J. Trust, medication adherence, and hypertension control in Southern African American men. Am J Public Health. 2012;102(12):2242–2245. doi: 10.2105/AJPH.2012.300777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care. 2010;33(5):1034–1036. doi: 10.2337/dc09-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L, Hessler D, Glasgow RE, Arean PA, Masharani U, Naranjo D, Strycker LA. REDEEM: a pragmatic trial to reduce diabetes distress. Diabetes Care. 2013;36(9):2551–2558. doi: 10.2337/dc12-2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisler M, Choi H, Palmisano G, Mase R, Richardson C, Fagerlin A, … An LC. Comparison of community health worker-led diabetes medication decision-making support for low-income Latino and African American adults with diabetes using e-health tools versus print materials: a randomized, controlled trial. Ann Intern Med. 2014;161(10 Suppl):S13–22. doi: 10.7326/M13-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisler M, Choi H, Palmisano R, Mase R, Richardson C, Fagerlin A, … An LC. A Randomized Controlled Trial Comparing Community Health Worker-led Diabetes Medication Decision-making Support for Low-income Latino and African American Adults with Diabetes Using e-Health Tools versus Print Materials. Annals of Internal Medicine. 2014;161(10):S13–22. doi: 10.7326/M13-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28(4):816–822. doi: 10.2337/diacare.28.4.816. [DOI] [PubMed] [Google Scholar]
- Heisler M, Spencer M, Forman J, Robinson C, Shultz C, Palmisano G, … Kieffer E. Participants’ assessments of the effects of a community health worker intervention on their diabetes self-management and interactions with healthcare providers. Am J Prev Med. 2009;37(6 Suppl 1):S270–279. doi: 10.1016/j.amepre.2009.08.016. S0749-3797(09)00531-5 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, Magid DJ. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- Horne R, Hankins M, Jenkins R. The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Qual Health Care. 2001;10(3):135–140. doi: 10.1136/qhc.0100135... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Aubert RE, Yao J, Teagarden JR, Epstein RS. Greater adherence to diabetes drugs is linked to less hospital use and could save nearly $5 billion annually. Health Aff (Millwood) 2012;31(8):1836–1846. doi: 10.1377/hlthaff.2011.1198. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care. 2005;28(9):2280–2288. doi: 10.2337/diacare.28.9.2280. [DOI] [PubMed] [Google Scholar]
- Lorig A. Outcome Measures for Health Education and Other Health Care Interventions. London: Sage; 1986. [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, … Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Lyles CR, Sarkar U, Ralston JD, Adler N, Schillinger D, Moffet HH, … Karter AJ. Patient-provider communication and trust in relation to use of an online patient portal among diabetes patients: The Diabetes and Aging Study. J Am Med Inform Assoc. 2013;20(6):1128–1131. doi: 10.1136/amiajnl-2012-001567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- Mackinnon DP, Warsi G, Dwyer JH. A Simulation Study of Mediated Effect Measures. Multivariate Behav Res. 1995;30(1):41. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishali M, Omer H, Heymann AD. The importance of measuring self-efficacy in patients with diabetes. Fam Pract. 2011;28(1):82–87. doi: 10.1093/fampra/cmq086. [DOI] [PubMed] [Google Scholar]
- Montori VM, Gafni A, Charles C. A shared treatment decision-making approach between patients with chronic conditions and their clinicians: the case of diabetes. Health Expect. 2006;9(1):25–36. doi: 10.1111/j.1369-7625.2006.00359.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Moskowitz D, Thom DH, Hessler D, Ghorob A, Bodenheimer T. Peer coaching to improve diabetes self-management: which patients benefit most? J Gen Intern Med. 2013;28(7):938–942. doi: 10.1007/s11606-013-2367-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullan RJ, Montori VM, Shah ND, Christianson TJ, Bryant SC, Guyatt GH, … Smith SA. The diabetes mellitus medication choice decision aid: a randomized trial. Arch Intern Med. 2009;169(17):1560–1568. doi: 10.1001/archinternmed.2009.293. [DOI] [PubMed] [Google Scholar]
- Munoz EB, Dorado MF, Guerrero JE, Martinez FM. The effect of an educational intervention to improve patient antibiotic adherence during dispensing in a community pharmacy. Aten Primaria. 2014;46(7):367–375. doi: 10.1016/j.aprim.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakahara R, Yoshiuchi K, Kumano H, Hara Y, Suematsu H, Kuboki T. Prospective study on influence of psychosocial factors on glycemic control in Japanese patients with type 2 diabetes. Psychosomatics. 2006;47(3):240–246. doi: 10.1176/appi.psy.47.3.240. [DOI] [PubMed] [Google Scholar]
- Nelson KM, McFarland L, Reiber G. Factors influencing disease self-management among veterans with diabetes and poor glycemic control. J Gen Intern Med. 2007;22(4):442–447. doi: 10.1007/s11606-006-0053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson WL, Han PK, Fagerlin A, Stefanek M, Ubel PA. Rethinking the objectives of decision aids: a call for conceptual clarity. Med Decis Making. 2007;27(5):609–618. doi: 10.1177/0272989X07306780. [DOI] [PubMed] [Google Scholar]
- O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5 Suppl):101S–156S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Resnicow K, Choi H, Heisler M. A diabetes peer support intervention that improved glycemic control: mediators and moderators of intervention effectiveness. Chronic Illn. 2013;9(4):258–267. doi: 10.1177/1742395313476522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Ratanawongsa N, Karter AJ, Parker MM, Lyles CR, Heisler M, Moffet HH, … Schillinger D. Communication and medication refill adherence: the diabetes study of northern california. JAMA Intern Med. 2013;173(3):210–218. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. doi: 10.3121/cmr.2013.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, … Pignone M. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292(14):1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47(3):213–220. [PubMed] [Google Scholar]
- Salvalaggio G, Dong K, Vandenberghe C, Kirkland S, Mramor K, Brown T, … Wild TC. Enhancing screening, brief intervention, and referral to treatment among socioeconomically disadvantaged patients: study protocol for a knowledge exchange intervention involving patients and physicians. BMC Health Serv Res. 2013;13:108. doi: 10.1186/1472-6963-13-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah M, Kaselitz E, Heisler M. The role of community health workers in diabetes: update on current literature. Curr Diab Rep. 2013;13(2):163–171. doi: 10.1007/s11892-012-0359-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah MK, Heisler M, Davis MM. Community health workers and the Patient Protection and Affordable Care Act: an opportunity for a research, advocacy, and policy agenda. J Health Care Poor Underserved. 2014;25(1):17–24. doi: 10.1353/hpu.2014.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slean GR, Jacobs EA, Lahiff M, Fisher L, Fernandez A. Aspects of culturally competent care are associated with less emotional burden among patients with diabetes. Med Care. 2012;50(9 Suppl 2):S69–73. doi: 10.1097/MLR.0b013e3182641127. [DOI] [PubMed] [Google Scholar]
- Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, … Heisler M. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011;101(12):2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D, Legare F, Col NF, Bennett CL, Barry MJ, Eden KB, … Wu JHC. TC Collaboration, editor. Decision aids for people facing health treatment or screening decisions (Review) 1. 2014. [DOI] [PubMed] [Google Scholar]
- Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care. 1999;37(5):510–517. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- Trinacty CM, Adams AS, Soumerai SB, Zhang F, Meigs JB, Piette JD, Ross-Degnan D. Racial differences in long-term adherence to oral antidiabetic drug therapy: a longitudinal cohort study. BMC Health Serv Res. 2009;9:24. doi: 10.1186/1472-6963-9-24. 1472-6963-9-24 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Servellen G, Lombardi E. Supportive relationships and medication adherence in HIV-infected, low-income Latinos. West J Nurs Res. 2005;27(8):1023–1039. doi: 10.1177/0193945905279446. [DOI] [PubMed] [Google Scholar]
- Weymiller AJ, Montori VM, Jones LA, Gafni A, Guyatt GH, Bryant SC, … Smith SA. Helping patients with type 2 diabetes mellitus make treatment decisions: statin choice randomized trial. Arch Intern Med. 2007;167(10):1076–1082. doi: 10.1001/archinte.167.10.1076. [DOI] [PubMed] [Google Scholar]
- White RO, Eden S, Wallston KA, Kripalani S, Barto S, Shintani A, Rothman RL. Health communication, self-care, and treatment satisfaction among low-income diabetes patients in a public health setting. Patient Educ Couns. 2015;98(2):144–149. doi: 10.1016/j.pec.2014.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]