Abstract
There is research suggesting that binge eating may serve an affect regulation function. However, experimental evidence supporting this model in adults is sparse and studies have been mixed regarding whether negative affect impacts objective energy intake. This study examined the impact of a real-time interpersonal stressor on laboratory test meal intake between individuals endorsing recent objective binge eating (≥1x/week) and those denying disordered eating. Generalized linear modeling was used to compare individuals with recent binge eating (BE group; n = 52) to those denying recent eating pathology (HC group; n = 51) on test meal intake following a stressor (stressful condition) or neutral stimulus (non-stressful condition). Moderated mediation analyses were used to examine whether negative affect mediated the impact of condition on intake differently between BE and HC groups. The BE group did not have significantly higher energy intake than the HC group in the stressful verses non-stressful condition. However, the BE group was more likely to engage in extreme intake (i.e., over- or under-consumption) than the HC group in the stressful versus non-stressful condition (p = .02). Changes in negative affect did not significantly mediate the relationship between condition and intake extremes for the BE group. The results indicate that both over- and under-consumption are triggered by stress among individuals with recent binge eating. Continued research investigating both binge eating and restriction as a means of affect regulation in binge-eating samples is encouraged.
Keywords: binge eating, dietary restriction, affect regulation, test meal
Binge eating is characterized by eating an objectively large amount of food in a short period of time while experiencing a sense of loss of control over food consumption (American Psychiatric Association, 2013). Individuals who engage in binge eating episodes often experience a range of negative health effects, significant psychiatric co-morbidity, and decreased quality of life (American Psychiatric Association, 2013; Bulik, Sullivan, & Kendler, 2002; Winkler et al., 2014). While existing treatments can produce significant decreases in binge eating (Brownley, Berkman, Sedway, Lohr, & Bulik, 2007; Shapiro et al., 2007), approximately half of patients with binge eating remain symptomatic after receiving evidenced-based treatment. Development of more effective treatments may be restricted by limited knowledge of the mechanisms driving binge-eating behaviors. While multiple theoretical models pertaining to the risk for and maintenance of binge eating have been proposed (Pearson, Wonderlich, & Smith, 2015), there have been relatively few direct tests of such models (Stice, 2002).
The role of affect regulation has been increasingly acknowledged in risk and maintenance models of disorders characterized by binge eating, such as bulimia nervosa (BN) and binge eating disorder (BED) (Pearson et al., 2015; Wonderlich et al., 2008), based on research indicating that binge episodes are frequently precipitated by affective difficulties (Greeno, Wing, & Shiffman, 2000; Heatherton & Baumeister, 1991). Additionally, studies using ecological momentary assessment to examine the relationship between affect and binge eating in real-time have found negative affect to significantly increase before and decrease after binge eating (Berg et al., 2015; Smyth et al., 2007) and to mediate the relationship between stressful events and binge eating (Goldschmidt et al., 2014). Although these prior studies implicate an affect regulation function of binge eating, they have primarily relied on self-report methods (Lavender et al., 2015), which may be problematic, as individuals with disordered eating are often inaccurate in their report of eating habits (Mitchell, Crow, Peterson, Wonderlich, & Crosby, 1998; Tanofsky-Kraff, Haynos, Kotler, Yanovski, & Yanovski, 2007).
Test meal studies examining eating behavior in a controlled, laboratory can be used to effectively assess objective binge eating (Anderson, Williamson, Johnson, & Grieve, 2001), while reducing the potential for self-report bias (Mitchell et al., 1998; Tanofsky-Kraff et al., 2007). A recent meta-analysis of laboratory meal studies concluded that negative affect significantly predicts over-consumption across clinical and non-clinical samples (Cardi, Leppanen, & Treasure, 2015). However, this review only included two publications involving binge-eating samples. Indeed, few studies have experimentally examined the relationship between stress, affect, and test meal eating behavior among binge-eating adult samples (Lavender et al., 2015) and those that have report conflicting findings (Aubie & Jarry, 2009; Laessle & Schulz, 2009; Telch & Agras, 1996). Of the extant experimental studies, two have found that negative mood manipulations increased the experience of loss of control and eating rate, but not objective energy consumption among individuals meeting DSM-IV criteria for BED (Laessle & Schulz, 2009; Telch & Agras, 1996). Another found that mood manipulation through weight-related teasing vignettes was associated with increased test snack consumption among individuals with binge eating; however, vignettes portraying other teasing-related scenarios did not trigger increased consumption (Aubie & Jarry, 2009). Thus, the evidence suggests that manipulation of negative affect among binge-eating samples impacts the feeling of loss of control, which is one key facet of binge eating, as well as other aspects of the eating experience; however, the findings are mixed regarding whether negative affect promotes objectively greater consumption in a laboratory setting.
Although prior experimental studies provide important initial information about the role of affect in binge eating, several limitations should be noted. First, these studies have utilized vignettes or films to induce negative mood, which may not closely resemble the real-life stressors associated with binge eating. Research suggests that interpersonal stressors are especially powerful triggers for binge eating in the natural environment (Goldschmidt, Wonderlich, et al., 2014; Ivanova et al., 2015). Therefore, a mood induction involving a real-time interpersonal stressor could provide a more ecologically-valid negative affect manipulation. Second, nearly all of these studies have been conducted with individuals meeting DSM-IV criteria for BED, excluding a large number of individuals who binge eat at a lower severity or who also purge. However, there is growing interest in examining problem behaviors dimensionally in order to identify common mechanisms across a range of severity and presentation (Morris & Cuthbert, 2012), and therefore, a need to examine mechanisms of binge eating across diagnostic groups. Third, the existing studies have not used advanced statistical analyses to conduct modeling (e.g., mediation analyses) of the relationship between stress, affect, and test meal intake among individuals who binge eat.
Another potential limitation is that these studies have utilized energy intake as the outcome measure in order to specifically investigate over-consumption. Although it would be expected that higher energy intake would represent more disordered outcomes (i.e., over-consumption likely due to binge eating) in binge-eating samples, there are data indicating that individuals who binge eat also frequently engage in pronounced under-consumption (i.e., dietary restriction) (Elran-Barak et al., 2015; Polivy & Herman, 1985). Therefore, important findings may be masked by only examining elevated energy consumption if some the individuals in these studies engage in dietary restriction, in addition to binge eating, in response to negative affect. In a recent experimental study investigating the impact of a stressor on test meal intake of individuals with anorexia nervosa (Wildes, Marcus, Bright, & Dapelo, 2012), researchers examined the variable of extreme intake, or consuming significantly more or less (1 SD above or below) than the group average, as an outcome measure to account for patterns of both over- and under-consumption. This variable has not been examined within binge-eating samples. Examination of extreme intake in addition to overall energy intake could allow for a more thorough investigation of the association between negative affect and disordered eating in binge-eating populations.
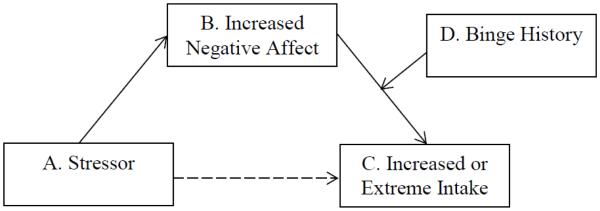
Therefore, this study examined the effects of a real-time interpersonal induction of distress (Shenk & Fruzzetti, 2011) (stressful condition) versus a non-stressful stimulus (neutral condition) on laboratory test meal intake, comparing individuals with recent binge eating (BE group) with individuals not reporting recent disordered eating (HC group). The primary aim was to test the role of negative affect in over-consumption among a dimensional sample with recent binge eating. We hypothesized that individuals in the BE group would consume more food in the stressful versus neutral condition compared to the HC group. We also conducted moderated mediation analyses consistent with the model in Figure 1. We hypothesized that the association between a stressor (i.e., stressful versus neutral condition) (1a) and energy intake (1c) would be mediated by increases in negative affect (i.e., baseline to pre-meal) (1b) for individuals who endorsed recent binge eating (i.e., BE versus HC group) (1d). As an exploratory aim, we investigated the role of negative affect in extreme intake (i.e., over- or under-consumption) by repeating all analyses with extreme intake as the outcome variable.
Figure 1.
Proposed study moderated mediation model
Materials and Methods
Participants
Participants were females ≥ 18 years old who either endorsed binge eating (n = 52; BE group) or no significant disordered eating (n = 52; HC group) within the prior month. The sample size of 104 participants was identified using G-Power software (Faul, Erdfelder, Lang, & Buchner, 2007), assuming sufficient power (80%) to detect a large effect size (d = 0.80) between groups at α = 0.05. Inclusion criteria required self-reported BMI ≥ 18.5 kg/m2 to avoid any confounding effects of starvation. Exclusion included: 1) pregnancy; 2) use of medications with known effects on appetite (e.g., stimulants) within two weeks of participation; and 3) history of bariatric surgery.
Further, inclusion in the BE sample required endorsement of engaging in objective bulimic episodes (i.e., binge eating) ≥ 1x/week on average within the prior month on the Eating Disorder Examination Questionnaire (EDE-Q) (Fairburn & Beglin, 1994). Although engaging in binge eating ≥ 1x/week corresponds with DSM-5 criteria (American Psychiatric Association, 2013), we did not require any eating disorder diagnosis for inclusion. Inclusion in the HC sample required a report of no objective bulimic episodes within the prior month on the EDE-Q. Further, the EAT-26 was used to rule out other (non-binge eating) eating pathology in the HC group because this measure has established cutoffs to detect possible disordered eating (Garner & Garfinkel, 1979). A score of < 10 on the Eating Attitudes Test (EAT-26) was required for inclusion in the HC group to rule out alternate eating disorder symptoms.
Procedures
Recruitment and screening
The local Institutional Review Board approved study procedures. Participants were recruited at a mid-size university through community and campus advertisements. Interested individuals participated in screening online or by telephone, during which they completed the demographics and eligibility form, EDE-Q, and EAT-26 to establish eligibility. Once eligibility was determined, participants were invited to attend the laboratory portion of the study.
Consent and baseline procedures
The laboratory portion of the study was conducted in the morning and participants were instructed to refrain from eating for four hours prior to participation to control for baseline hunger levels. Fasting status was verified by research staff upon participant arrival. These procedures are consistent with prior laboratory meal studies (e.g., Anderson et al., 2001; Latner, Rosewall, & Chisholm, 2008). Participants completed informed consent procedures, which indicated that the study was examining the impact of stress on the sensory experiences of consumption (e.g., taste, texture). Although participants were informed of all relevant procedures, they were not told the true purpose of the study, or that intake would be measured and stress level would be experimentally manipulated, in order to reduce the potential for reactivity. Participants then completed baseline questionnaires.
Experimental manipulation
After consent and baseline procedures, participants were randomly assigned according to a block design to the stressful or neutral condition. Participants were instructed to complete ten mental arithmetic tasks, each within 40 seconds. After the third, sixth, and ninth arithmetic task, participants were asked to describe their emotional experience and subsequently received interpersonal feedback from the experimenter regarding their reaction to the tasks. The stressful and neutral conditions differed in the difficulty of the math tasks and the nature of the interpersonal feedback in order to evoke differing affective states.
The stressful condition utilized a previously validated manipulation designed to elicit negative affect (Shenk & Fruzzetti, 2011). In this condition, the mental arithmetic tasks were challenging and designed so that most participants would be unable to complete them within the allotted time. Further, the interpersonal feedback provided by experimenters was unsupportive regarding the participant’s emotional experience (e.g., “I don’t understand why you feel that way,” “This is addition and subtraction; your reaction seems extreme”). This procedure has been previously found to elicit increases in self-reported negative affect and physiological arousal (Shenk & Fruzzetti, 2011).
The neutral condition was designed to parallel the procedures of the stressful condition, while supporting maintenance of baseline affect. In this condition, the mental arithmetic tasks were simple and piloted to establish that participants would be able to answer within the allotted time. Further, the interpersonal feedback was supportive regarding the participant’s emotional experience (e.g., “Your feelings make sense,” “How you are feeling is similar to how others have reacted”).
Test meal
Following the mood manipulation, participants were administered the single-item test meal, consisting of 946g (32 fl oz.; 1,000 kcal) of an Ensure® nutrition milkshake. The milkshake was presented in a large, opaque container to conceal the total quantity. Participants were instructed to use a straw to drink the milkshake and to otherwise avoid manipulating the container. Participants were read standardized instructions that indicated that they should drink as much as they would like, but should consume enough to answer subsequent questions about the sensory qualities of the milkshake and to have these questions be unaffected by extreme hunger levels. This instruction was provided to ensure that participants consumed some amount of milkshake. Participants ate alone in the laboratory for ten minutes before research staff re-entered and collected the container with the remaining quantity of the milkshake. The container holding the contents of the milkshake was weighed discretely out of participant sight pre- and post-test meal to calculate the amount consumed. These procedures are similar to those described in prior laboratory meal experiments (Sysko, Walsh, Schebendach, & Wilson, 2005; Walsh & Boudreau, 2003).
Debriefing
Following the test meal, participants were debriefed regarding the purpose of the study and were informed that the math tasks and interpersonal feedback were designed to manipulate mood. Participants were compensated in the form of extra credit in a psychology course (for those for whom this applied) or $15 cash compensation.
Measures
Eating Disorder Examination Questionnaire
(Fairburn & Beglin, 1994). The EDE-Q is a widely used self-report measure of eating behaviors and cognitions over the previous month. The measure provides a Global and four subscale scores (Restraint, Eating Concern, Shape Concern, and Weight Concern) and count data regarding instances of objective binge eating and purging. The EDE-Q was used to establish BE and HC eligibility, as well as to provide a baseline measure of eating disorder symptoms. In this sample, the reliability of the EDE-Q Global scores, as measured by Cronbach’s α, was .97. For the subscales, reliability ranged between .86 (Restraint) and .94 (Shape Concern).
Eating Attitudes Test
(Garner & Garfinkel, 1979). The EAT-26 is another widely used measure that assesses eating disordered thoughts and behaviors with sound psychometric characteristics (Garner & Garfinkel, 1979). EAT-26 scores range from 0 to 78, with higher scores indicating greater eating pathology. The EAT-26 was additionally used for screening out non-binge eating disordered eating in the HC group, since clinical cutoff scores have been established for this measure. Scores ≥ 20 on the EAT-26 have been found to signify elevated risk of eating pathology (Patton, Johnson-Sabine, Wood, Mann, & Wakeling, 1990). Therefore, the < 10 cutoff point for inclusion in the HC group signified low probability of significant disordered eating. The reliability of the EAT-26 in this sample, as measured by Cronbach’s α, was .91.
Positive and Negative Affect Schedule (PANAS)
(Watson, Clark, & Tellegen, 1988). The PANAS is a measure that assesses affective states, with higher scores indicating greater affective intensity. The PANAS has strong internal consistency and concurrent validity (Crawford & Henry, 2004; Watson et al., 1988). The PANAS negative affect scale was administered on the day of the laboratory visit at baseline, pre-test meal (immediately following the mood manipulation), and post-test meal. The PANAS was used as a manipulation check to establish that the mood manipulation evoked differing negative affect between conditions. PANAS pre-meal negative affect change was calculated as the difference between pre-meal and baseline negative affect for the moderated mediation analyses. The reliability of the PANAS negative affect scale in this sample, as measured by Cronbach’s α, ranged from .85 (baseline) to .86 (post-meal).
Visual Analogue Scales
Visual analogue scales, ranging from 1-100, were used to measure hunger pre- and post-meal and enjoyment of the shake post-meal. Previous studies have utilized similar measures to assess variables relevant to the test meal (Sysko et al., 2005; Walsh & Boudreau, 2003).
Data Analytic Plan
Independent t-tests and chi-square analyses were conduct to examine differences between groups on baseline characteristics. To establish whether the mood manipulation was successful, repeated measure ANOVAs were used to examine changes in PANAS negative affect over time (baseline, pre-meal, and post-meal), with condition, group, and the condition × group interaction included as between-subjects factors.
Generalized linear models were used to examine the impact of condition, group, and the condition × group interaction on test meal energy intake and extreme intake. Extreme intake was calculated at > 1 SD above (505.36 kilocalories or kcal) or below (47.70 kcal) the sample mean, consistent with the previous study using this metric (Wildes et al., 2012). Test meal energy intake was skewed and extreme intake was categorical; therefore, gamma with log link and binomial logistic distributions, respectively, were used for these analyses. Analyses were repeated including several potential covariates (i.e., age, race, BMI, purging status, EDE restraint, pre-meal hunger, and shake enjoyment). However, none of these covariates significantly altered the results; therefore, only the original model is reported. Moderated mediation analyses were conducted using the PROCESS macro for SPSS (Hayes, 2013). Analyses were conducted such that condition was the predictor variable, baseline to pre-meal change in negative affect the mediator, group the moderator, and either energy intake or extreme intake the outcome variable. Analyses used 5,000 bootstraps and the 95% confidence intervals were set at a p < .05.
Results
Baseline Demographic and Clinical Characteristics
Baseline characteristics are listed in Table 1. Participants were primarily college-aged and White. As expected, groups differed significantly in BMI and EDE-Q scores, with the BE group demonstrating higher values on these indices. The BE group reported binge eating 2x/week on average (M = 8.02, SD = 4.58, Range = 4 to 24 episodes/month). Over one-third of the BE sample also reported purging at approximately the same rate as binge eating (M = 8.95, SD = 9.25, Range = 1 to 28 episodes/month). The BE participants with recent purging had higher scores than those without recent purging on EDE Global (t(102) = 6.39, p < .001), Restraint (t(102) = 6.26, p < .001), Eating Concern (t(102) = 6.04, p < .001), Shape Concern (t(102) = 5.62, p < .001), and Weight Concern (t(102) = 5.56, p < .001) scales, indicating greater eating disorder psychopathology, but did not differ significantly on age, race, BMI, or baseline hunger. One HC participant endorsed six episodes of purging through laxatives within the prior month, despite meeting HC group inclusion criteria. Therefore, this participant was removed from all analyses. Both the BE and HC groups reported comparably moderate baseline hunger, indicating that the pre-experiment fasting successfully controlled hunger levels.
Table 1.
Baseline demographic and clinical characteristics of the binge eating and healthy control samples
| Dependent Variable | Total sample (n = 103) Mean (SD) |
Binge eating group (n = 52) Mean (SD) |
Healthy control (n = 51) Mean (SD) |
df | t / χ2 | 95% CI | p | Cohen’s d |
|---|---|---|---|---|---|---|---|---|
| Age (years) | 20.49 (5.34) | 21.10 (6.24) | 19.86 (4.20) | 101 | −1.17 | −3.32, 0.85 | .24 | 0.24 |
| Race (% Caucasian) | 68.93% | 69.23% | 68.63% | 1 | 0.00 | ----- | 1.00 | ----- |
| Body Mass Index (kg/m2) | 24.32 (4.87) | 25.90 (5.68) | 22.70 (3.20) | 101 | −3.48 | −5.03, -1.38 | .001* | 0.70 |
| EDE Restraint Score | 1.93 (1.48) | 3.07 (1.25) | 0.94 (0.82) | 101 | −10.26 | −2.55, −1.72 | <.001* | 2.03 |
| EDE Eating Concern Score | 1.69 (1.57) | 2.93 (1.21) | 0.44 (0.59) | 101 | −13.21 | −2.86, −2.10 | <.001* | 2.63 |
| EDE Shape Concern Score | 3.16 (1.78) | 4.61 (0.86) | 1.68 (1.15) | 101 | −14.69 | −3.33, −2.34 | <.001* | 2.92 |
| EDE Weight Concern Score | 2.95 (1.74) | 4.32 (0.93) | 1.56 (1.17) | 101 | −13.29 | −3.17, −2.35 | <.001* | 2.64 |
| EDE Global Score | 2.46 (1.54) | 3.73 (0.86) | 1.15 (0.83) | 101 | −15.46 | −2.91, −2.25 | <.001* | 3.08 |
| Purging (% endorsing) | 18.45% | 36.54% | 0.00% | 1 | 21.05 | ----- | <.001* | ----- |
| Pre-meal hunger | 53.40 (27.04) | 51.88 (29.16) | 54.92 (24.93) | 100 | 0.57 | −7.62, 13.70 | 0.57 | 0.11 |
Note: EDE = Eating Disorder Examination;
p < .05
Manipulation Check
There was a significant interaction between time and condition on negative affect (F(2,98) = 25.06, p < .001). In the stressful condition, negative affect significantly increased from baseline (M = 12.87, SE = 0.58) to pre-meal (M = 19.77, SE = 0.73) and decreased post-meal (M = 14.40, SE = 0.64). In contrast, in the neutral condition, negative affect remained stable at baseline (M = 13.95, SE = 0.58), pre-meal (M = 13.91, SE = 0.74), and post-meal (M = 12.92, SE = .65). The interaction between group, condition, and time was not significant (F(2,98) = 1.89, p = .16), indicating that the mood manipulation functioned similarly for individuals in the BE and HC groups.
Test Meal Intake
Test meal intake ranged from 13 to 981 kcal (M = 276.53, SD = 228.83). There were no significant differences in energy intake (F(1,102) = 1.39, p = .24) or extreme intake (χ2(1) = 0.85, p = 1.00) according to purging status. Enjoyment of the shake was, on average, moderate (M = 46.41, SD = 28.23), but ranged considerably (Range = 0 to 100), and did not vary according to group (F(1,97) = 0.03, p = .86), condition (F(1,97) = 2.92, p = .09), or the group × condition interaction (F(1,97) = 0.81, p = .37).
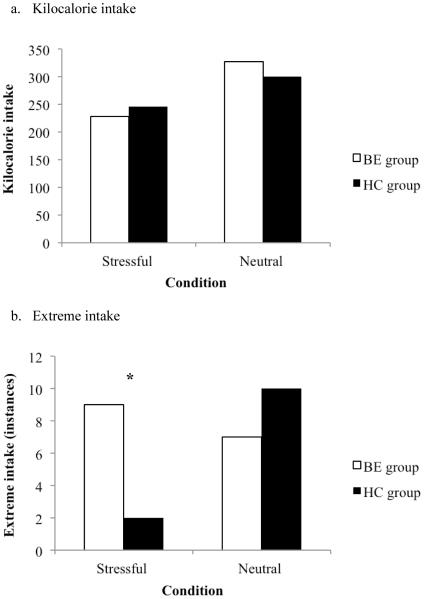
The results of the generalized linear models are detailed in Table 2 and Figure 2. Contrary to expectations, there was no significant effect of group, condition, or the group × condition interaction on energy intake. A different pattern emerged for extreme intake. Although there were no significant main effects of group or condition, there was a significant group × condition interaction (p = .02). In the stressful condition, a greater percentage of the BE group engaged in extreme intake compared to the HC group (p = .01; See Figure 2). Among those in the BE group who engaged in extreme intake in the stressful condition, 55.6% (n = 5) engaged in under-consumption and 44.4% (n = 4) engaged in over-consumption. In comparison, only two subjects in the HC group engaged in extreme intake in the stressful condition, one of which engaged in under-consumption and one of which engaged in over-consumption. In the neutral condition, there were no differences in extreme intake between the BE and HC groups.
Table 2.
Generalized linear models examining the impact of condition, group, and condition x group interactions on test meal intake
| Dependent Variable | Independent Variables | Wald χ2 | B | SE | p |
|---|---|---|---|---|---|
| Kilocalorie intake | Condition | 3.21 | 0.36 | 0.23 | 0.07 |
| Group | 0.00 | 0.08 | 0.23 | 0.98 | |
| Condition × Group | 0.20 | −0.15 | 0.32 | 0.65 | |
|
| |||||
| Extreme intake | Condition | 2.75 | 0.36 | 0.61 | 0.10 |
| Group | 1.47 | 1.85 | 0.84 | 0.23 | |
| Condition × Group | 5.56 | −2.44 | 1.04 | 0.02* | |
p < .05
Figure 2.
Test meal intake by group (binge eating, healthy control) and condition (stressful, neutral)
Note: BE = binge eating; HC = healthy control; *p < .05
Further, individuals in the HC group were significantly more likely to engage in extreme intake in the neutral versus stressful condition (p = .01). Among the HC participants who engaged in extreme intake in the neutral condition, 70.0% (n = 7) engaged in over-consumption, while 30.0% (n = 3) engaged in under-consumption. Similarly, among the BE participants who engaged in extreme intake in the neutral condition, 70.0% (n = 5) engaged in over-consumption, while 30.0% (n = 2) engaged in under-consumption.
Moderated Mediation Analyses
The index of moderated mediation was not significant for test meal energy intake (B = − 27.72, SE = 40.22, 95% CI: −108.96, 48.61), but was significant for extreme intake (B = 1.88, SE = 1.17, 95% CI: 0.43, 4.49). The conditional indirect effect of negative affective changes on extreme intake was significant for the HC group (B = −1.47, SE = 1.16, 95% CI: −4.54, −0.20), but not the BE group (B = 0.41, SE = 0.48, 95% CI: −0.36, 1.48). For the HC group, changes in negative affect significant mediated the relationship between condition and extreme intake, such that less change in negative affect accounted for greater likelihood of extreme intake in the neutral condition.
Discussion
We investigated the affect regulation model of binge eating by comparing the effects of a mood manipulation on laboratory test meal intake of individuals endorsing recent binge eating versus individuals denying recent disordered eating. In line with the affect regulation model, we hypothesized that the BE group would consume more under stressful conditions. In contrast to our expectations, but in line with prior investigations (Laessle & Schulz, 2009; Telch & Agras, 1996), individuals in the BE group did not consume significantly more energy than the HC group in the stressful condition. However, a greater portion of the BE group (9 out of 26 participants) engaged in extreme intake compared to the HC group (2 out of 26 participants) in the stressful condition. This provides initial evidence that individuals with recent binge eating may respond to stress by both over- and under-eating.
One potential interpretation of these results is that both binge eating and dietary restriction may serve as strategies to manage reactions to stressful stimuli in this population. Theory and research in binge-eating samples have focused primarily on binge eating (and purging, when relevant) as a response to stressful experiences (Aubie & Jarry, 2009; Laessle & Schulz, 2009; Telch & Agras, 1996; Wonderlich et al., 2008). However, research suggests that individuals who binge eat also frequently restrict (Elran-Barak et al., 2015; Polivy & Herman, 1985). This study illuminates the need to further investigate whether both dietary restriction and binge eating may function to manage stress or negative affect among individuals who binge eat. An alternative interpretation is that under-eating among the BE group in the stressful condition may have represented a temporary suppression of binge eating. Binge episodes typically take place when an individual is at home or alone (Goldschmidt, Crosby, et al., 2014; Stein et al., 2007). Therefore, some in the BE group may have momentarily reduced consumption with the intention of binge eating later in a different context. Future experimental studies of affect regulation and consumption would benefit from longer follow-up periods and from investigation of whether certain contextual variables (i.e., social context) promote or discourage different disordered eating behaviors.
We further examined the affect regulation model by testing whether changes in negative affect accounted for effects of condition on intake differently between groups. We expected that greater pre-meal increases in negative affect in the stressful condition would account for greater energy and/or extreme intake for individuals in the BE group. Contrary to expectations and prior research (Goldschmidt et al., 2014), changes in negative affect did not mediate the effect of the stressor on intake for the BE group. This result could indicate that the effect of the stressor on extreme intake was mediated by another putative mechanism (e.g., impulsivity, eating expectancies, self-control depletion) besides negative affect. Alternatively, this study may have been limited by using self-report of affect, which may be unreliable among individuals with disordered eating (Lavender et al., 2015), and may have been impacted by demand characteristics in the experimental setting. More objective measures of affective arousal (e.g., psychophysiology, neuroimaging) could have provided more accurate data by which to test our models. Further, there was an unexpected mediation effect of negative affect in the HC group, such that an increased likelihood of extreme intake in the neutral condition among HC individuals could be accounted for by fewer changes in negative affect. Future research on the affect regulation model of binge eating would benefit from testing multiple mediators across units of analysis and from further exploring the relationship between stress, affect, and extreme intake in HC samples.
There were several study strengths. The experimental design and test meal outcome allowed for a controlled, objective examination of the impact of affect on intake. Additionally, the sample varied across binge eating severity and diagnostic group, rather than focusing narrowly on a BN or BED sample, thus increasing the generalizability of results. Further, use of a real-time interpersonal mood manipulation was novel and may have more closely resembled social experiences that trigger binge eating in the naturalistic environment than prior manipulations. Finally, this study went beyond prior experimental studies by examining extreme intake, allowing for an initial investigation of whether individuals who binge eat utilize both under- and over-consumption to manage affect.
There are also study limitations. The first set of limitations pertains to measurement and procedural concerns. First, this study relied on self-report questionnaires to determine eating disorder status of participants. Interview measures may have more accurately identified eating disorder symptoms. However, there is evidence that individuals may be more likely to disclose sensitive information such as binge eating through questionnaire, rather than an interview, due to relative anonymity (Keel, Crow, Davis, & Mitchell, 2002), suggesting an advantage of questionnaires. Second, binge eating was only assessed for one month before the study and, therefore, may not have reflecting the larger pattern of an individual’s eating habits. Third, we did not measure the experience of loss of control, which is a required criterion for a binge episode, in the experimental portion of the study. Therefore, while objective over-consumption can provide a proxy for binge eating, it remains unclear whether consuming more food in this study reflected binge eating or overeating. Fourth, the experimental task combined interpersonal and cognitive stressors to elicit negative emotion; therefore, it was not possible to determine differential effects of either type of stressor. Finally, the milkshake in this study was rated only as moderately palatable on average. While controlling for test meal enjoyment did not alter results, the test meal may not have been representative of binge foods and, therefore, over-consumption may have increased if the test meal had been more enjoyable. Future studies would benefit from including more stringent measures of disordered eating, assessing loss of control, utilizing experimental tasks that differentiate between social and cognitive stressors, and presenting alternate test meal items.
There are also sample issues that warrant consideration. This was primarily an undergraduate sample recruited through psychology courses; therefore, the participants may not have been comparable to a more clinical sample. Further, although the use of a cross-diagnostic sample is a strength because it increases generalizability, this approach could have had added extraneous variability masking effects of the mood manipulation on eating behavior. Finally, symptoms and diagnoses related to other current or past Axis-I disorders, including those that may have impacted reactions to an interpersonal stressor (e.g., social anxiety), and lifetime history of eating disorder, were not assessed. Therefore, individuals in the HC group may have had current or past psychological concerns that would have impacted their data. Future samples would benefit from inclusion of more demographic diversity, more clear differentiation between diagnostic samples, and greater control over co-morbidity and prior eating disorder history.
Conclusions
This study provides evidence suggesting that both over-and under-eating are triggered by stress among individuals with recent binge eating. The results highlight the need for continued research investigating dietary restriction as a response to stress and examining momentary pathways to different disordered eating patterns. Such research could assist the development of interventions more effectively targeting multiple forms of disordered eating in binge-eating populations.
Acknowledgements
Research reported in this publication was supported by pre-doctoral training fellowship F31MH097450 and post-doctoral training fellowship T32MH082761 awarded by the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. 5th American Psychiatric Publishing; Washington, D.C: 2013. [Google Scholar]
- Anderson DA, Williamson DA, Johnson WG, Grieve CO. Validity of test meals for determining binge eating. Eating Behaviors. 2001;2(2):105–112. doi: 10.1016/s1471-0153(01)00022-8. doi:10.1177/0145445503259851. [DOI] [PubMed] [Google Scholar]
- Aubie CD, Jarry JL. Weight-related teasing increases eating in binge eaters. Journal of Social and Clinical Psychology. 2009;28(7):909–936. doi:10.1521/jscp.2009.28.7.909. [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, et al. Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders. 2015;48:641–653. doi: 10.1002/eat.22401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. The International Journal of Eating Disorders. 2007;40(4):337–348. doi: 10.1002/eat.20370. doi:10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Kendler KS. Medical and psychiatric morbidity in obese women with and without binge eating. The International Journal of Eating Disorders. 2002;32(1):72–78. doi: 10.1002/eat.10072. doi:10.1002/eat.10072. [DOI] [PubMed] [Google Scholar]
- Cardi V, Leppanen J, Treasure J. The effects of negative and positive mood induction on eating behaviour: A meta-analysis of laboratory studies in the healthy population and eating and weight disorders. Neuroscience and Biobehavioral Reviews. 2015;57:299–309. doi: 10.1016/j.neubiorev.2015.08.011. [DOI] [PubMed] [Google Scholar]
- Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. The British Journal of Clinical Psychology. 2004;43:245–265. doi: 10.1348/0144665031752934. Pt 3. doi:10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- De Young KP, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, Mitchell JE, et al. Bidirectional associations between binge eating and restriction in anorexia nervosa. An ecological momentary assessment study. Appetite. 2014;83:69–74. doi: 10.1016/j.appet.2014.08.014. doi:10.1016/j.appet.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elran-Barak R, Sztainer M, Goldschmidt AB, Crow SJ, Peterson CB, Hill LL, Le Grange D. Dietary restriction behaviors and binge eating in anorexia nervosa, bulimia nervosa and binge eating disorder: Trans-diagnostic examination of the restraint model. Eating Behaviors. 2015;18:192–196. doi: 10.1016/j.eatbeh.2015.05.012. doi:10.1016/j.eatbeh.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. 1 The Guilford Press; New York: 2008. [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? The International Journal of Eating Disorders. 1994;16(4):363–370. [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Garner DM, Garfinkel PE. The Eating Attitudes Test: an index of the symptoms of anorexia nervosa. Psychological Medicine. 1979;9(2):273–279. doi: 10.1017/s0033291700030762. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Crosby RD, Cao L, Engel SG, Durkin N, Beach HM, et al. Ecological momentary assessment of eating episodes in obese adults. Psychosomatic Medicine. 2014;76(9):747–752. doi: 10.1097/PSY.0000000000000108. doi:10.1097/PSY.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Wonderlich SA, Crosby RD, Engel SG, Lavender JM, Peterson CB, et al. Ecological momentary assessment of stressful events and negative affect in bulimia nervosa. Journal of Consulting and Clinical Psychology. 2014;82(1):30–39. doi: 10.1037/a0034974. doi:10.1037/a0034974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. Journal of Consulting and Clinical Psychology. 2000;68(1):95–102. [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; New York: 2013. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Ivanova IV, Tasca GA, Hammond N, Balfour L, Ritchie K, Koszycki D, Bissada H. Negative affect mediates the relationship between interpersonal problems and binge-eating disorder symptoms and psychopathology in a clinical sample: a test of the interpersonal model. European Eating Disorders Review: The Journal of the Eating Disorders Association. 2015;23(2):133–138. doi: 10.1002/erv.2344. doi: 10.1002/erv.2344. [DOI] [PubMed] [Google Scholar]
- Keel PK, Crow S, Davis TL, Mitchell JE. Assessment of eating disorders: Comparison of interview and questionnaire data from a long-term follow-up study of bulimia nervosa. Journal of Psychosomatic Research. 2002;53:1043–1047. doi: 10.1016/s0022-3999(02)00491-9. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Schulz S. Stress-induced laboratory eating behavior in obese women with binge eating disorder. The International Journal of Eating Disorders. 2009;42(6):505–510. doi: 10.1002/eat.20648. doi:10.1002/eat.20648. [DOI] [PubMed] [Google Scholar]
- Latner JD, Rosewall JK, Chisholm AM. Energy density effects on food intake, appetite ratings, and loss of control in women with binge eating disorder and weight-matched controls. Eating Behaviors. 2008;9(3):257–266. doi: 10.1016/j.eatbeh.2007.09.002. doi:10.1016/j.eatbeh.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. doi:10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JE, Crow S, Peterson CB, Wonderlich S, Crosby RD. Feeding laboratory studies in patients with eating disorders: a review. The International Journal of Eating Disorders. 1998;24(2):115–124. doi: 10.1002/(sici)1098-108x(199809)24:2<115::aid-eat1>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Morris SE, Cuthbert BN. Research Domain Criteria: cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience. 2012;14(1):29–37. doi: 10.31887/DCNS.2012.14.1/smorris. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Johnson-Sabine E, Wood K, Mann AH, Wakeling A. Abnormal eating attitudes in London schoolgirls--a prospective epidemiological study: outcome at twelve month follow-up. Psychological Medicine. 1990;20(2):383–394. doi: 10.1017/s0033291700017700. [DOI] [PubMed] [Google Scholar]
- Pearson CM, Wonderlich SA, Smith GT. A risk and maintenance model for bulimia nervosa: From impulsive action to compulsive behavior. Psychological Review. 2015;122(3):516–535. doi: 10.1037/a0039268. doi:10.1037/a0039268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Dieting and binging. A causal analysis. The American Psychologist. 1985;40(2):193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- Safer DL, Lively TJ, Telch CF, Agras WS. Predictors of relapse following successful dialectical behavior therapy for binge eating disorder. The International Journal of Eating Disorders. 2002;32(2):155–163. doi: 10.1002/eat.10080. doi:10.1002/eat.10080. [DOI] [PubMed] [Google Scholar]
- Shapiro JR, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik CM. Bulimia nervosa treatment: a systematic review of randomized controlled trials. The International Journal of Eating Disorders. 2007;40(4):321–336. doi: 10.1002/eat.20372. doi:10.1002/eat.20372. [DOI] [PubMed] [Google Scholar]
- Shenk CE, Fruzzetti AE. The impact of validating and invalidating responses on emotional reactivity. Journal of Social and Clinical Psychology. 2011;30(2):163–183. doi:10.1521/jscp.2011.30.2.163. [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–38. doi: 10.1037/0022-006X.75.4.629. doi:10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder?: A prospective examination of precursors and consequences. The International Journal of Eating Disorders. 2007;40(3):195–203. doi: 10.1002/eat.20352. doi:10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological Bulletin. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh BT, Schebendach J, Wilson GT. Eating behavior among women with anorexia nervosa. The American Journal of Clinical Nutrition. 2005;82(2):296–301. doi: 10.1093/ajcn.82.2.296. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Haynos AF, Kotler LA, Yanovski SZ, Yanovski JA. Laboratory-based studies of eating among children and adolescents. Current Nutrition and Food Science. 2007;3(1):55–74. doi: 10.2174/1573401310703010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch CF, Agras WS. Do emotional states influence binge eating in the obese? International Journal of Eating Disorders. 1996;20(3):271–279. doi: 10.1002/(SICI)1098-108X(199611)20:3<271::AID-EAT6>3.0.CO;2-L. doi:10.1002/(SICI)1098-108X(199611)20:3<271::AID-EAT6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Thomas JG, Doshi S, Crosby RD, Lowe MR. Ecological momentary assessment of obesogenic eating behavior: combining person-specific and environmental predictors. Obesity (Silver Spring, Md.) 2011;19(8):1574–1579. doi: 10.1038/oby.2010.335. doi:10.1038/oby.2010.335. [DOI] [PubMed] [Google Scholar]
- Walsh BT, Boudreau G. Laboratory studies of binge eating disorder. The International Journal of Eating Disorders. 2003;34(Suppl):S30–38. doi: 10.1002/eat.10203. doi:10.1002/eat.10203. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wildes JE, Marcus MD, Bright AC, Dapelo MM, Psychol MC. Emotion and eating disorder symptoms in patients with anorexia nervosa: an experimental study. The International Journal of Eating Disorders. 2012;45(7):876–882. doi: 10.1002/eat.22020. doi:10.1002/eat.22020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler LA-D, Christiansen E, Lichtenstein MB, Hansen NB, Bilenberg N, Støving RK. Quality of life in eating disorders: a meta-analysis. Psychiatry Research. 2014;219(1):1–9. doi: 10.1016/j.psychres.2014.05.002. doi:10.1016/j.psychres.2014.05.002. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Crosby RD, Joiner T, Peterson CB, Bardone-Cone A, Klein M, et al. Personality subtyping and bulimia nervosa: psychopathological and genetic correlates. Psychological Medicine. 2005;35(5):649–657. doi: 10.1017/s0033291704004234. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Engel SG, Peterson CB, Robinson MD, Crosby RD, Mitchell JE, et al. Examining the conceptual model of integrative cognitive-affective therapy for BN: Two assessment studies. The International Journal of Eating Disorders. 2008;41(8):748–754. doi: 10.1002/eat.20551. doi:10.1002/eat.20551. [DOI] [PubMed] [Google Scholar]