Abstract
AIM
To explore primary care physicians’ perspectives on possible barriers to the use of insulin.
METHODS
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Eight electronic databases were searched (between January 1, 1994 and August 31, 2014) for relevant studies. A search for grey literature and a review of the references in the retrieved studies were also conducted. Studies that focused on healthcare providers’ perspectives on possible barriers to insulin initiation with type 2 diabetic patients were included, as well as articles suggesting solutions for these barriers. Review articles and studies that only considered patients’ perspectives were excluded.
RESULTS
A total of 19 studies met the inclusion criteria and were therefore included in this study: 10 of these studies used qualitative methods, 8 used quantitative methods and 1 used mixed methods. Studies included a range of different health care settings. The findings are reported under four broad categories: The perceptions of primary care physicians about the barriers to initiate insulin therapy for type 2 diabetes patients, how primary care physicians assess patients prior to initiating insulin, professional roles and possible solutions to overcome these barriers. The barriers described were many and covered doctor, patient, system and technological aspects. Interventions that focused on doctor training and support, or IT-based decision support were few, and did not result in significant improvement.
CONCLUSION
Primary care physicians’ known delay in insulin initiation is multifactorial. Published reports of attempts to find solutions for these barriers were limited in number.
Keywords: Diabetes, Insulin, Initiation, Delay, Barriers, Primary care physicians
Core tip: There are several barriers to primary care physicians in initiating insulin therapy when it is required for type 2 diabetes patients. The main purpose of this systematic review is to explore these barriers in depth. Published reports of attempts to find solutions to these barriers were limited in number. Given the increasing burden of this chronic disease, and the need to optimize and standardize management, it is expected research in this area will remain intense. The research that remains patient-centered and takes a system approach can be expected to yield best results.
INTRODUCTION
Diabetes is a major world health problem. The most recent report from the International Diabetes Federation estimates that 415 million people have diabetes worldwide (8.8% of the adult population). Of these, 193 million people have undiagnosed diabetes, which allows the disease to progress untreated causing many complications. In 2015, diabetes was responsible for 11.6% of total global adult health expenditure and yet there were 5 million deaths from this disease. In addition, the number of people with diabetes is expected to increase to more than 642 million by 2040[1].
Type 2 diabetes is characterized by defects in both insulin secretion (due to a progressive decline in beta cell functioning), and insulin resistance. It is aggravated by obesity and sedentary lifestyle. Untreated hyperglycemia increases the risk of mortality and morbidity, via a higher risk of macro-vascular and micro-vascular complications[2-4].
With already high numbers of patients and a relatively small number of diabetes specialists worldwide, 90% of patients receive care for their diabetes from primary care physicians (PCPs)[5,6].
Several trials[7,8] have shown that improving glycemic control, via lifestyle modifications and the use of medications, reduces micro-vascular and possibly macro-vascular complications and mortality related to diabetes. However, over time, the progressive nature of beta cell dysfunction results in the inability of oral hypoglycemic agents to control hyperglycemia and achieve HbA1c targets[9]. This gradual loss in beta cell function would indicate that insulin therapy is almost always required at some point to treat diabetic patients[10].
Although most PCPs believe that the initiation of insulin therapy is an essential component in the management of type 2 diabetes, many still consider it to be the “last option” and indicate that their patients are reluctant to accept this therapy. In the seminal Diabetes Attitudes, Wishes, and Needs (DAWN) study, Peyrot et al[11] reported that approximately 50% of healthcare professionals delay insulin initiation until it is “absolutely necessary”.
Similarly, the SOLVE™ (Study of Once Daily Levemir), a multicenter observational study that involved over 17374 patients with type 2 diabetes in 10 countries (Europe, Asia and North America), showed that insulin initiation is generally delayed until an average HbA1c level of approximately 9%[12]. Several other studies across many countries have confirmed that there is significant delay in the initiation of insulin therapy[13-15]. This reluctance to initiate insulin treatment may be related to patient, provider or system factors.
Reported patient-related barriers include a sense of personal failure, a negative impact on social life, injection phobia, myths and misconceptions about the drug, the permanence of the therapy, difficulties in fulfilling responsibilities at home and at work, limited insulin self-management training, inadequate provider explanation about the risks and benefits of the intervention - and concerns over weight gain and hypoglycemia[16-21]. Most of these negative attitudes and perceptions are described in the literature under the term “psychological insulin resistance”. Studies in Various countries have found variable rates of such resistance amongst patients - from 5.9% to nearly 50% of patients[17-25].
System barriers to the use of insulin therapy may include a lack of resources (e.g., staff and materials), a lack of continuity of care, as well as the workload and time constraints of PCPs[26].
As for the providers, part of the problem has been attributed to “therapeutic or clinical inertia; a recognition (by the PCP) of a lack of glycemic control - but a failure to act”[27-29]. These PCPs blame (perceived) patient reluctance, language barriers, their concern for patients’ comorbidities and their own lack of training[26].
A few systematic reviews have been published related to patients’ perspectives on the delay in insulin initiation or to psychological insulin resistance[30-33]. This study focuses on PCP’s perspectives on their barriers to initiating insulin therapy in primary care/general practice. It will also explore the literature for possible solutions.
MATERIALS AND METHODS
This literature search was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines[34]. As this research doesn’t involve experiments on humans or animals, ethical approval is not required.
A variety of scholarly databases (PubMed, EMBASE, Psychinfo, Cinahl, Ovid, Scopus, ProQuest and the Cochrane library) were searched. The search was conducted using a combination of medical subject headings and text words: Insulin, physician, general practitioner, general practice, primary care, health care, professional, provider, psychological, clinical inertia, attitude, delay, refusal, refuse, perception, postpone, worry, initiation, compliance, knowledge, fear, belief and barrier.
A search in Google and Google Scholar engines were then conducted to look for “grey” literature and the bibliographies of the retrieved articles were also reviewed to identify further relevant studies.
Studies that satisfied the following selection criteria were included: Only original articles, quantitative or qualitative methods, descriptive or analytical, written in English and published between January 1, 1994 and August 31, 2014.
This review was restricted to studies that focused on PCP’s perspectives to the barriers they faced regarding the initiation of insulin for type 2 diabetic patients. Articles suggesting solutions for these barriers were also included. Review articles or studies that only explored patients’ perspectives were excluded.
The screening and selection of the studies were done independently by the two authors, and the final number of the studies used for this review was reached by consensus between them. The authors assessed the methods used in the various studies: The Critical Appraisal Skills Program checklist[35] was used for the qualitative studies, the STROBE checklist[36] was used for the observational studies, the Mixed Methods Appraisal Tool[37] was used for the mixed-methods studies and the Centre for Evidence-Based Medicine tool[38] was used for the randomized control trials.
The authors had to be in agreement for an article to be included in the systematic review. Both authors also collaborated to extract the data from each article. These are summarized in table form according to authors’ name, year of publication, aim of the study, sample size, the setting, instruments used, results and conclusion (Table 1).
Table 1.
Summary of the articles included in this study
| Ref. | Design | Study aims | Sample and setting | Tools and outcome measures | Results and conclusions |
| Hayat et al[39] (2010) | Qualitative | To explore barriers and myths regarding initiating insulin therapy in poorly controlled type 2 diabetic patients in primary care centres in Hyderabad District, Pakistan | 6 to 20 medical officers per each focus group and 12 medical officers for semi-structured interviews Conducted in primary care centres in the Hyderabad District, Pakistan | 6 focus group discussions 12 semi-structured individual interviews | Patients barriers: Mistaken beliefs about insulin; fear of needles and excessive belief in traditional healers Doctors’ barriers: Skill and knowledge deficiencies, language barriers and fear of hypoglycaemia and obesity risks System’s barriers: High workload, insufficient consultation time, lack of continuity of care and financial barriers |
| Manski-Nankervis et al[51] (2014) | Qualitative | To study the effect of communications and relationships between health care professionals in general practice toward the issue of insulin initiation and to clarify how multidisciplinary teams work in practice | 21 GPs, practice nurses, diabetes nurse educators and specialist physicians Conducted in Melbourne, Victoria, Australia | Semi-structured interviews face-to-face or via the telephone | Barriers for initiating insulin aren’t solely due to medical or training issues; communication and relationships among health care professionals also have a strong influence 4 themes identified from the study: Uncertain roles, unreliable competency, relationships and communication between healthcare workers and the development of trust and respect |
| Grant et al[46] (2007) | Cross-sectional | To study physicians’ considerations and preference when selecting medications for patients with type 2 diabetes | 886 academic generalists and specialists Conducted in the United States | Questionnaire-based survey | The major considerations for academic generalists when staring insulin are the patient’s HbA1c level, adherence and motivation, health assessment and glucose level patterns Major barriers to beginning insulin for generalists are patient derived (patients’ fear and preferences), while the specialists didn’t specify any major barriers |
| Yoshioka et al[48] (2013) | Cross-sectional | To identify differences in the perceptions of patients and their physicians regarding insulin initiation (using data from the DAWN Japan study) | 148 patients with type 2 diabetes and 68 physicians Conducted in Japan | Questionnaire-based survey | There are perceptions gaps regarding insulin initiation between patients and physicians, especially regarding its social impact Physicians tend to overestimate the barrier of the injections being painful and patients’ fear and to underestimate its social impact |
| Peyrot et al[11] (2005) | Cross-sectional | To study patients’ and healthcare professionals’ (physicians and nurses) attitudes toward insulin therapy and its correlation with delaying insulin therapy initiation | 2061 type 2 diabetic patients and 1109 providers (physicians and nurses) Conducted in 13 countries in Asia, Australia, Europe and North America | Structured interviews conducted face-to-face or over the telephone | Most healthcare professionals (50%-55%) delay insulin initiation until it is absolutely required Delay in insulin initiation is significantly less likely when providers consider that their patients are adherent to appointments and medication regimens Delay of starting oral hypoglycaemic drugs is the strongest correlation with insulin therapy initiation |
| Lee et al[47] (2014) | Qualitative | To determine how healthcare professionals assess their patients when initiating insulin therapy for type 2 diabetic patients | 41 health care professionals (physicians, nurses, diabetic educators and pharmacists) Conducted in Malaysia | 4 focus group discussions and 10 individual interviews | Healthcare professionals’ assessment of diabetic patients when considering insulin initiation are based on their perceptions rather than objective evaluation of patients’ backgrounds, knowledge and abilities |
| Ratanawongsa et al[43] (2012) | Cross-sectional | To explore primary care physicians’ perceptions about barriers of initiating insulin for patients with type 2 diabetes | 83 primary care physicians Conducted in United States (Indiana, New jersey and California) | Structured interviews that contained open-ended questions | Participants reported that at least 10% of their patients would reject to start insulin 64% of the clinicians believed that their patients’ reluctance was the cause of delaying insulin initiation; 43% believed it was due to their patients’ poor self-management skills 97% of physicians thought that fear of the injections was the cause of their patients’ resistance to starting insulin |
| Patel et al[40] (2012) | Qualitative | To identify healthcare professionals’ perspectives on delaying insulin initiation for type 2 diabetic patients in a multi-ethnic setting | 14 healthcare professionals (general practitioners, specialists and nurses) Conducted in the United Kingdom | Semi-structured, face-to-face, interviews | Barriers for initiating insulin therapy for South Asian diabetic patients could be over-accentuated by the presence of language barrier and the lack of patients’ understanding about the disease and its therapy South Asian patients seem to be more likely to be negatively influenced by observations and experiences about insulin treatment within their community |
| Lee et al[41] (2012) | Qualitative | To explore healthcare professionals’ opinions on barriers of initiating insulin therapy in Malaysian multi-ethnic patients with type 2 diabetes | 38 healthcare professionals (general practitioners, family medicine specialists, medical officers, policy makers, diabetes educators and endocrinologists) Conducted in Malaysia | Focus group discussions and semi-structured interviews | Patients’ barriers: Patients’ fear and misconceptions about insulin, lack of knowledge and self-efficacy Healthcare professionals’ barriers: Negative attitude toward insulin; lack of training, motivation and confidence System barriers: Lack of continuity of care, shortage of resources and language barriers |
| Lee et al[52] (2012) | Qualitative | To explore the strategies suggested by healthcare professionals to improve insulin initiation in the Malaysian dual-sector (public-private) healthcare system | 38 healthcare professionals (general practitioners, family medicine specialists, medical officers, policy makers, diabetes educators and endocrinologists) Conducted in Malaysia | Focus group discussions and semi-structured interviews | Developing an integrated system for patients’ referral from the private sector to the public health sector for insulin initiation services Involving nongovernmental organisations, the media and pharmaceutical industry in supporting insulin initiation Establishing multidisciplinary teams |
| Lakkis et al[44] (2013) | Cross-sectional | To investigate family physicians’ attitudes towards insulin therapy in type 2 diabetic patients in Middle Eastern Arab countries | 122 family physicians Conducted in Middle Eastern Arab countries | Online questionnaire-based survey | 73.6% of family physicians chosen to delay insulin initiation until it is absolutely necessary 64% of family physicians reported hesitancy to start insulin mostly due to apparent patient reluctance |
| Referral to endocrinologists for initiating insulin therapy was correlated with a lack of experience and concerns about risks, mainly with elderly patients | |||||
| Nakar et al[49] (2007) | Case-control study | To study the barriers that delay a shift to insulin from the perspectives of type 2 diabetic patients and family physicians | Study group: 92 patients who needed insulin Control group: 101 patients who had begun insulin 157 family physicians Conducted in Israel | Telephone interviews with participating patients Written questionnaire obtained from the physicians | A clear perception gap regarding the insulin initiation barriers between patients and physicians Physicians exaggerate the importance of patients’ physical fear of pain associated with injections and blood tests, while patient barriers seem to be related more to their concept of the illness |
| Furler et al[50] (2011) | Qualitative | To describe barriers and facilitators to insulin initiation in general practice | 14 healthcare professionals (general practitioners and diabetes nurse educators) and 12 type 2 diabetic patients Conducted in Australia | Semi-structured interviews | Insulin initiation could be influenced by the way patients and healthcare professionals Interact There was a disagreement and uncertainty about the healthcare workers’ role in initiating insulin |
| Hayes et al[45] (2008) | Cross-sectional | To explore primary care physicians’ attitudes toward insulin initiation for type 2 diabetic patients and to determine the areas where there is a clear lack of consensus between them | 505 primary care physicians Conducted in the United States | Online questionnaire-based survey | Highest consensus was attitudes related to risk and benefits of insulin therapy, positive experiences of diabetic patients on insulin and patient worries about insulin initiation Clear lack of consensus was seen in attitudes related to the metabolic effects of insulin, the necessity for insulin therapy, the duration needed for training and the fear of hypoglycaemia risk especially in elderly patients |
| Tan et al[42] (2011) | Qualitative | To explore the barriers to insulin initiation for diabetic patients managed in primary care polyclinics in Singapore | 18 healthcare professionals (physicians and nurses) and 11 type 2 diabetic patients Conducted in Singapore | Focus group discussions | Patient barriers to insulin initiation were denial the need for insulin therapy, perception of social stigma, inconvenience, worries of needles pain, fear from side effects and complications Physician attitude and experience with insulin therapy were also a possible barrier |
| Haque et al[26] (2005) | Qualitative | To explore the barriers to initiating insulin therapy for type 2 diabetic patients in public-sector primary health care centres in Cape Town, South Africa | 46 medical officers working at community health centres Conducted in Cape Town, South Africa | 5 focus group discussions and 10 individual semi-structured interviews | Physician barriers: Lack of knowledge and experience, language barriers and exaggerated fear of hypoglycaemia Patient barriers: False beliefs about insulin, poor compliance, lack of understanding of the disease, belief in traditional herbs, fear of injections and poor socioeconomic status System barriers: Time limitations, lack of continuity of care and financial restraints |
| Sunaert et al[53] (2014) | Qualitative | Related to a program supporting the initiation of insulin therapy in primary care in Belgium, this study determined factors influencing the general practitioners to be involved in insulin therapy initiation and explored factors relevant for future program development | 9 general practitioners for focus group discussions 20 general practitioners for individual interviews 10 type 2 diabetic patients for individual interview Conducted in Belgium | Focus group discussions Individual semi-structured interviews | General practitioners whom engaged in insulin initiation program differ from those not engaged in: Attitude, subjective norm and perceived behavioural control regarding insulin initiation Factors to consider include: Job boundaries between the diabetes nurse educators and general practitioners, job boundaries between general practitioners and specialists and protocol adherence |
| Burden et al[54] (2007) | Mixed | To evaluate the "Insulin For Life" training course for general practitioners and practice nurses in the Heart of Birmingham Teaching Primary Care Trust by exploring the attitudes of the patients, nurses and GPs toward initiating insulin therapy | 39 type 2 diabetic patients using a questionnaire 3 to 6 mo after starting insulin 17 general practitioners and practice nurse surveyed using a questionnaire after course completion 37 GPs and practice nurses attended focus group discussions Conducted in Birmingham, United Kingdom | Questionnaire-based survey Focus group discussion | Post-course completion: Type 2 diabetic patients reported that starting insulin in general practice is acceptable and were confident and self-management Most general practitioners and practice nurses were confident about initiating insulin |
| Harris et al[55] (2013) | Randomised control trial | To determine the effectiveness of an insulin initiation strategy utilising a diabetes specialist and community retail pharmacy support to increase family physician insulin-prescribing rates | 73 family physicians in the intervention group were provided with diabetes specialists/educators consultation support for 12 mo and community retail pharmacist support 78 family physicians in the control group had usual care Conducted at 15 sites across Canada | Primary outcome was insulin-prescribing rate (IPR) per physician defined as the number of insulin starts of insulin-eligible patients during the 12-mo period | No significant differences were found between the two groups: Mean IPR of 2.28 compared to 2.29 for Intervention group physicians and the control group physicians, respectively. And an estimated adjusted RR (95%CI) of 0.99 (0.80 to 1.24); P = 0.96 An insulin initiation support program utilising support from diabetes specialists, diabetic educators and community retail pharmacists to improve insulin prescribing in family practice was unsuccessful |
DAWN: Diabetes Attitudes, Wishes, and Needs
RESULTS
The initial search process resulted in 9757 studies. After removing any duplicates and adding articles by searching the cross-references and grey literature, this number dropped to 6683 studies. Titles and abstracts of these studies were then screened, and the two authors narrowed the results down to 132 articles for full-text assessment (78 articles were then excluded because they looked only at patients’ perspectives, and a further 32 were excluded because they were review studies).
The remaining 22 articles were critically appraised by the two authors, and three more articles were excluded because of their poor overall quality. Thus, a total of 19 articles were included in the final analysis. Figure 1 is a flow diagram of this process.
Figure 1.
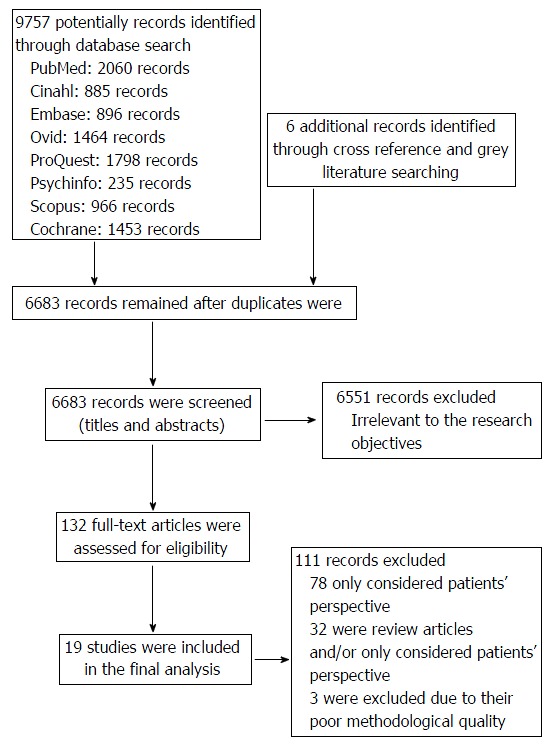
Flow diagram of the studies included in this analysis.
Characteristics of the studies
The publication dates of the final 19 studies ranged from 2005 to 2014 and included 10 qualitative studies, 7 observational studies, 1 mixed-method studies and 1 randomised controlled trial.
One study was international and multicentre; three studies were conducted in both the United States and Malaysia; two studies were conducted in the United Kingdom and Australia; and one study was conducted in each of the following countries: Japan, Pakistan, Singapore, South Africa, Israel, Belgium, Canada and Middle Eastern Arab countries. These articles are summarized in Table 1.
The perceptions of primary care physicians
Several researchers tried to explore PCP’s barriers to initiating insulin therapy using qualitative methods (e.g., focus group discussions or semi-structured interviews). Hayat et al[39], Patel et al[40], Lee et al[41], Tan et al[42] and Haque et al[26] conceptualized that the decision to initiate insulin therapy can be influenced by three types of barriers: Physician barriers, patient barriers and system barriers.
From these studies we can say that PCP’s barriers may include: A lack of knowledge, training and experience by the PCP; language barriers between PCP and patient; accentuated concern by the PCP about the risk of hypoglycemia and weight gain; and PCP concerns about patient noncompliance.
In one of the DAWN studies, Peyrot et al[11] found that a delay in beginning insulin therapy is significantly less frequent among specialists in comparison to PCPs and that healthcare providers (PCPs, specialists and nurses) usually underestimate a patient’s feelings of self-blame and personal failure when insulin is needed.
In another study, Ratanawongsa et al[43] reported that 64% of PCPs cited patients’ resistance as the major cause for delaying insulin initiation, and 97% of these physicians believed that this resistance was due to a fear of injections.
In Arab countries, 73% of PCPs prefer to delay insulin therapy until it is “absolutely essential”[44]; this percentage is higher than the data from the DAWN report (i.e., 50% to 55%)[11].
In an earlier study in the United States, Hayes et al[45] explored the attitudes of 505 PCPs in the United States regarding initiation of insulin. Most reported that initiation of insulin is the most difficult part of managing type 2 diabetes, due to the need for injections.
How PCPs assess patients prior to initiating insulin
The way in which PCPs assess their diabetic patients could highly impact their decision to start insulin. Grant et al[46] surveyed 886 academic PCPs and specialists in the United States. They reported that when initiating insulin, PCPs usually consider their patients’ HbA1c levels, adherence, motivation to improve, overall health assessments and blood glucose level patterns. Patients’ age, weight and hospital protocol or guidelines had less impact on their decisions. They appeared to consider patient concerns in their assessments of barriers, whereas few specialists pointed to any major barriers in insulin initiation at all[46].
In a similar approach a qualitative study conducted in Malaysia of over PCPs explored what assessment they made of patients requiring insulin. They concluded that the decision to start insulin therapy was influenced by assessments of their patients’ characteristics, not just their HbA1C or pattern of random glucose readings[47].
Two studies discussed the existence of a perception gap between physicians and patients when initiating insulin. Physicians tend to underestimate the social issues related to insulin usage, they also tend to underestimate patients’ understanding of the illness, including concerns that the disease will worsen, self-blame and feelings of personal failure in controlling disease progression. Rather, physicians seemed to overestimate patients’ fear and concerns that the injections will be painful[48,49].
Professional roles
The initiation of insulin could be influenced by the way that patients and healthcare providers interact. The impact of roles, communication and the relationships between healthcare professionals and their patients was explored in two qualitative studies conducted in Australia.
Furler et al[50] interviewed 14 general practice healthcare providers and 12 patients with type 2 diabetes and concluded that there was uncertainty regarding whose role it was to initiate insulin, e.g., the patients were unclear if the diabetes nurse or diabetes educators were allowed to initiate insulin therapy or whether they only had support roles. The study concluded that there were differing perceptions of what is to be done, who does it, how it is done, and how it is supported. To quote: “…initiating insulin for the treatment of diabetes in the setting of general practice is a complex social intervention”.
Manski-Nankervis et al[51] interviewed 21 PCPs, practice nurses, diabetes nurse educators and specialists. Both specialists and PCPs agreed that insulin initiation can be undertaken by general practitioners supported by diabetes educators, with specialists backing them up for the complicated cases. They found (again) concerns regarding the ambiguous roles and involvement of nurses (especially practice nurses vs diabetes nurse educators) in insulin initiation. However, there was a general feeling that nurses could play a vital role by providing specific training and education[51].
Possible solutions
Our review found four studies that explored solutions to the barriers to insulin initiation. In one study, healthcare professionals and health policy makers in Malaysia were interviewed and participated in focus group discussions. The participants concluded that there is a need to establish multidisciplinary teams and to develop an integrated system for collaboration between the private and public sectors, particularly regarding insulin initiation programs, to decrease the workload (especially of the public sector). The participants also emphasized the importance of the involvement of nongovernmental organizations, the media and the pharmaceutical industry in insulin initiation programs through the provision of training, education and financial support[52].
In another qualitative study conducted in Belgium, PCPs were invited to attend a support program addressing barriers to insulin initiation; this program involved education and specialist coaching. Comparing PCPs who participated with those who did not, the authors analyzed their findings in terms of the theory of planned behavior. This social cognition model includes consideration of attitude, subjective norm and perceived behavioral control when exploring determinants of professional behavior. Compared to PCPs who did not participate in the program, PCPs who participated noticed the following changes in their behaviors: They were more satisfied with their jobs, more interested in becoming involved in insulin initiation, felt strengthened by the appreciation of their patients and had higher self-esteem levels due to their roles in diabetes care being acknowledged by health policy makers[53].
Similarly, a 2007 study conducted in the United Kingdom to partially evaluate a training course for insulin initiation found that most of the healthcare providers thought that the course was useful and made them more confident in dealing with diabetic patients[54].
Finally, Harris et al[55] in 2013 reported a randomized controlled trial of over 151 PCPs in 15 locations across Canada to determine the effectiveness of a 12-mo insulin initiation strategy within primary care. This strategy included diabetes specialists and community retail pharmacists supporting PCPs in their initiation of insulin therapy. The primary outcome they measured was insulin prescribing rates. Surprisingly, their results showed no significant difference when using this strategy; the mean insulin prescribing rates for the intervention group PCPs and the control group PCPs were 2.28 and 2.29 respectively. The authors suggested these results might be influenced by some factors: It may be underpowered by having a smaller than estimated sample size, or the possibility of contamination (although it was limited) or the delay of recruitment and participation of the pharmacists. In addition, they considered the “Hawthorne” effect could be operating (where physicians tend to improve their behavior in response to their knowledge of being observed); and that this could explain some of the lack of difference between the two groups.
DISCUSSION
To the best of our knowledge, the present study is the first systematic review of published work that has explored primary care physicians’ points of view regarding the noticeable delay in insulin therapy initiation in primary care settings.
This clinical inertia affects approximately one-third of patients with type 2 diabetes, and this failure of PCPs to act, coupled with patients’ prolonged exposure to hyperglycemia, leads to a higher risk of chronic complications and mortality[28].
Our review finds that PCPs report many barriers to the initiation of insulin and these range across doctor, patient and system issues. Others have also pointed to this complexity[26,39,41,51]. Table 2 listed the main barriers reported by PCPs to initiate insulin as found in this review.
Table 2.
Barriers reported by primary care physicians to initiate insulin
| Physicians’ related barriers |
| PCP’s lack of knowledge, training and experience |
| Language barriers between PCP and patient |
| PCP’s concern over the risk of hypoglycemia and weight gain |
| Perceived patient resistance - esp. fear of injections |
| PCP’s concern about patient noncompliance |
| System barriers |
| Lack of resources (e.g., staff and materials) |
| Lack of continuity of care |
| The workload and time constraints of PCPs |
| Ambiguity of roles in the primary care team |
PCP: Primary care physician.
Clearly, the knowledge, training and experience of the PCP is an important factor, and must affect patient management in more domains than just insulin initiation[11]. This factor may also overlap with an over-concern (by the PCP) about their patient’s ability to cope with injections or about possible patient side-effects such as weight-gain and hypoglycemia[26,39,42-44].
Less obviously connected to training and experience is the finding that PCPs under-estimate their patient’s feelings of guilt and personal failure when faced with insulin initiation. About 40% of diabetic patients report poor psychological well-being; guilt and self-blame may well be included in this[56].
And PCPs may assess their insulin-requiring diabetic patients in ways different to their specialist colleagues - considering patient adherence and motivation (as well as general health status, HbA1C and blood glucose levels)[46,47]; thus delaying insulin initiation. Yet a concern for this wider assessment seems to miss relevant patient concerns such as the impacts (of insulin use) on their social, marital, occupational or financial situations, as well as causing inconvenience and social stigma. Patients also report lack of understanding of the illness and the role of insulin[48,49]. Perhaps PCPs hear this patient reluctance and assume it is mainly about the use of injections.
Counter to this is the reassuring findings of two studies that suggest patients’ negative attitudes toward insulin are mostly temporary and improve after they begin using insulin[57,58]. Perhaps patients need education and reassurance earlier in their diabetic journey; that insulin will most probably be needed at some stage, despite their best efforts, and that this is part of the natural history of the disease - not a sign of their poor management and certainly not a reason for self-blame.
There have been various opinions and suggestions for improving the timeliness of insulin initiation. These have included better delineation of roles within the primary health care team, better integration of health care services, improved communications within the health care setting, improved education of patients (including in groups), wider use of nursing staff, decision support for PCPs, or harnessing new technologies[52-55]. These are all consistent with the suggested approach captured within the Chronic Care Model[59].
Some of the above ideas have attracted intervention studies, with varying success and/or methodological rigor: Some interventions have targeted the PCP (including how to deal with barriers to insulin initiation) but there are few in the literature that report clinically positive effects. Two have evaluated such interventions and found that PCPs reported “increased confidence” in using insulin therapy[53,54].
But with a definite clinical outcome measure (HbA1C over three years), Dale et al[60] demonstrated a sustained effect from a brief training course on insulin initiation for healthcare professionals. The training involved “presentations, small group work, case studies and practical demonstrations”.
On the other hand, Harris et al[55] (in a randomized controlled trial) could not demonstrate any clinical effect from an intervention that provided external expert consultation support to PCPs by community pharmacists and specialists.
Another controlled trial used a decision-support tool aimed at helping PCPs make decisions about insulin therapy. They found no difference in insulin initiation between control and intervention groups - though physicians were allowed not to consult the decision support tool[61].
Clearly, interventions aimed at the PCP will need further refinement, especially if they are to be scaled up for the future increasing numbers of diabetic patients.
Of course technology may change the discourse about clinical inertia or psychological insulin resistance in other ways. For example prefilled insulin pens could reduce the time needed for patient education and training. This method is associated with increased patient convenience and persistence[62]. Other technical developments can also be expected. Table 3 listed the possible solutions for insulin initiation delay proposed in the literature.
Table 3.
Possible solutions for insulin initiation delay proposed in literature
| Establish multidisciplinary teams and an integrated system for insulin initiation programs |
| Involve non-governmental organisations through provision of training and education for both patients and healthcare workers |
| Reinforce healthcare workers skills and knowledge through training courses and workshops |
| Consider Involving clinical pharmacists and specialists in insulin initiation programs as kind of support or backup |
| Consider using the aid of electronic decision-support tool |
| Adopting technology like prefilled insulin pens |
Limitations
This systematic review concentrated only on studies of Primary Care Physicians.
It integrates the findings from a variety of research designs; thus a meta-analysis couldn’t be used. Sampling varied greatly amongst the studies: Some included patients as well as healthcare providers (even health policy experts), and some didn’t report how the subjects were recruited. Moreover, the research was restricted by the use of articles written in English, which could miss some studies related to this review subject.
In conclusion, PCPs’ known delay in insulin initiation is multifactorial, but our understanding of these is getting better, e.g., perceptions of PCPs about patient reluctance may be missing important details such as patient guilt and self-blame. Upskilling of PCPs remains an attractive approach, while the particular elements of teamwork, clinic processes, clinic resources and decision support will need further study and refinement.
ACKNOWLEDGMENTS
We gratefully acknowledge Dr. Peter Schattner for conducting a final review before official submission of the manuscript.
COMMENTS
Background
The reluctance of many general practitioners to initiate insulin treatment could be related to patient, provider and/or system factors. The purpose of this study is to explore general practitioners’ perspectives on possible barriers to the use of insulin therapy and to look for solutions to this dilemma in the current literature.
Research frontiers
A few systematic reviews have been published previously related to patients’ perspective on the delay in insulin initiation or to psychological insulin resistance. What is unique in this study is the focus on primary healthcare providers’ perspectives on barriers to the initiation of insulin therapy in primary care/general practice, and the investigation of possible solutions.
Innovations and breakthroughs
There are several barriers to primary care physicians initiating insulin therapy when it is required. Of these, patients’ perceived reluctance seems to be a prominent factor, though it is only one of many aspects of this complex issue.
Applications
Published reports of attempts to find solutions to these barriers were limited in number. Given the increasing burden of this chronic disease, and the need to optimize and standardize management, it is expected research in this area will remain intense. The research that remains patient-centered and takes a systems approach can be expected to yield best results.
Terminology
Clinical inertia could be defined as the failure of healthcare provider to initiate or intensify therapy when it is clinically required.
Peer-review
In this systematic review, the authors tried to explore primary care physicians’ perspectives on possible barriers to the use of insulin therapy and to look for solutions to this dilemma in the current literature. The authors concluded that primary care physicians’ known delay in insulin initiation is multifactorial. Published reports of attempts to find solutions for these barriers were limited in number. This is an interesting systematic review.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Endocrinology and metabolism
Country of origin: Saudi Arabia
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The authors declare that there is no conflict of interest.
Data sharing statement: No additional data are available.
Peer-review started: June 6, 2016
First decision: July 5, 2016
Article in press: October 18, 2016
P- Reviewer: Liu SH, Mitra A, Miller S S- Editor: Kong JX L- Editor: A E- Editor: Li D
References
- 1.International Diabetes Federation. IDF Diabetes Atlas, 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Google Scholar]
- 2.Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–647. doi: 10.1016/S2213-8587(14)70102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arai K, Hirao K, Matsuba I, Takai M, Matoba K, Takeda H, Kanamori A, Yamauchi M, Mori H, Terauchi Y. The status of glycemic control by general practitioners and specialists for diabetes in Japan: a cross-sectional survey of 15,652 patients with diabetes mellitus. Diabetes Res Clin Pract. 2009;83:397–401. doi: 10.1016/j.diabres.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 6.Jaakkimainen L, Shah BR, Kopp A. Sources of physician care for people with diabetes. Vol. 6. Diabetes in Ontario: an ICES practice atlas; 2003. pp. 161–192. [Google Scholar]
- 7.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 8.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005–2012. doi: 10.1001/jama.281.21.2005. [DOI] [PubMed] [Google Scholar]
- 10.U.K. prospective diabetes study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. U.K. Prospective Diabetes Study Group. Diabetes . 1995;44:1249–1258. [PubMed] [Google Scholar]
- 11.Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, Landgraf R, Kleinebreil L. Resistance to insulin therapy among patients and providers: results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care. 2005;28:2673–2679. doi: 10.2337/diacare.28.11.2673. [DOI] [PubMed] [Google Scholar]
- 12.Khunti K, Damci T, Meneghini L, Pan CY, Yale JF. Study of Once Daily Levemir (SOLVE™): insights into the timing of insulin initiation in people with poorly controlled type 2 diabetes in routine clinical practice. Diabetes Obes Metab. 2012;14:654–661. doi: 10.1111/j.1463-1326.2012.01602.x. [DOI] [PubMed] [Google Scholar]
- 13.Davis TM, Davis Cyllene Uwa Edu Au WA, Bruce DG. Glycaemic levels triggering intensification of therapy in type 2 diabetes in the community: the Fremantle Diabetes Study. Med J Aust. 2006;184:325–328. doi: 10.5694/j.1326-5377.2006.tb00264.x. [DOI] [PubMed] [Google Scholar]
- 14.Kostev K, Rathmann W. Changes in time to insulin initiation in type 2 diabetes patients: a retrospective database analysis in Germany and UK (2005-2010) Prim Care Diabetes. 2013;7:229–233. doi: 10.1016/j.pcd.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Nichols GA, Koo YH, Shah SN. Delay of insulin addition to oral combination therapy despite inadequate glycemic control: delay of insulin therapy. J Gen Intern Med. 2007;22:453–458. doi: 10.1007/s11606-007-0139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karter AJ, Subramanian U, Saha C, Crosson JC, Parker MM, Swain BE, Moffet HH, Marrero DG. Barriers to insulin initiation: the translating research into action for diabetes insulin starts project. Diabetes Care. 2010;33:733–735. doi: 10.2337/dc09-1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan H, Lasker SS, Chowdhury TA. Prevalence and reasons for insulin refusal in Bangladeshi patients with poorly controlled Type 2 diabetes in East London. Diabet Med. 2008;25:1108–1111. doi: 10.1111/j.1464-5491.2008.02538.x. [DOI] [PubMed] [Google Scholar]
- 18.Larkin ME, Capasso VA, Chen CL, Mahoney EK, Hazard B, Cagliero E, Nathan DM. Measuring psychological insulin resistance: barriers to insulin use. Diabetes Educ. 2008;34:511–517. doi: 10.1177/0145721708317869. [DOI] [PubMed] [Google Scholar]
- 19.Nur Azmiah Z, Zulkarnain A, Tahir A. Psychological insulin resistance (PIR) among Type 2 diabetes patients at public health clinics in Federal Territory of Malaysia. Int Med J Malaysia. 2011;10:7–12. [Google Scholar]
- 20.Polonsky WH, Fisher L, Guzman S, Villa-Caballero L, Edelman SV. Psychological insulin resistance in patients with type 2 diabetes: the scope of the problem. Diabetes Care. 2005;28:2543–2545. doi: 10.2337/diacare.28.10.2543. [DOI] [PubMed] [Google Scholar]
- 21.Wong S, Lee J, Ko Y, Chong MF, Lam CK, Tang WE. Perceptions of insulin therapy amongst Asian patients with diabetes in Singapore. Diabet Med. 2011;28:206–211. doi: 10.1111/j.1464-5491.2010.03195.x. [DOI] [PubMed] [Google Scholar]
- 22.Cefalu WT, Mathieu C, Davidson J, Freemantle N, Gough S, Canovatchel W. Patients’ perceptions of subcutaneous insulin in the OPTIMIZE study: a multicenter follow-up study. Diabetes Technol Ther. 2008;10:25–38. doi: 10.1089/dia.2008.0249. [DOI] [PubMed] [Google Scholar]
- 23.Machinani S, Bazargan-Hejazi S, Hsia SH. Psychological insulin resistance among low-income, U.S. racial minority patients with type 2 diabetes. Prim Care Diabetes. 2013;7:51–55. doi: 10.1016/j.pcd.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayet L, Naidoo S. An evaluation of insulin therapy initiation among patients with type 2 diabetes attending a public health facility in South Africa. South African Family Practice. 2012;54:525–530. [Google Scholar]
- 25.Polonsky WH, Hajos TR, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27:1169–1174. doi: 10.1185/03007995.2011.573623. [DOI] [PubMed] [Google Scholar]
- 26.Haque M, Emerson SH, Dennison CR, Navsa M, Levitt NS. Barriers to initiating insulin therapy in patients with type 2 diabetes mellitus in public-sector primary health care centres in Cape Town. S Afr Med J. 2005;95:798–802. [PubMed] [Google Scholar]
- 27.Khunti K, Wolden ML, Thorsted BL, Andersen M, Davies MJ. Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care. 2013;36:3411–3417. doi: 10.2337/dc13-0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mata-Cases M, Benito-Badorrey B, Roura-Olmeda P, Franch-Nadal J, Pepió-Vilaubí JM, Saez M, Coll-de-Tuero G. Clinical inertia in the treatment of hyperglycemia in type 2 diabetes patients in primary care. Curr Med Res Opin. 2013;29:1495–1502. doi: 10.1185/03007995.2013.833089. [DOI] [PubMed] [Google Scholar]
- 29.Harris SB, Kapor J, Lank CN, Willan AR, Houston T. Clinical inertia in patients with T2DM requiring insulin in family practice. Can Fam Physician. 2010;56:e418–e424. [PMC free article] [PubMed] [Google Scholar]
- 30.Brod M, Kongsø JH, Lessard S, Christensen TL. Psychological insulin resistance: patient beliefs and implications for diabetes management. Qual Life Res. 2009;18:23–32. doi: 10.1007/s11136-008-9419-1. [DOI] [PubMed] [Google Scholar]
- 31.Gherman A, Veresiu I, Sassu R, Schnur J, Scheckner B, Montgomery G. Psychological insulin resistance: a critical review of the literature. Practical Diabetes International. 2011;28:125–128d. [Google Scholar]
- 32.Stotland NL. Overcoming psychological barriers in insulin therapy. Insulin. 2006;1:38–45. [Google Scholar]
- 33.Wang HF, Yeh MC. Psychological resistance to insulin therapy in adults with type 2 diabetes: mixed-method systematic review. J Adv Nurs. 2012;68:743–757. doi: 10.1111/j.1365-2648.2011.05853.x. [DOI] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Critical Appraisal Skills Programme (CASP) 2014. 10 questions to help you make sense of qualitative research. Available from: http://www.bettervaluehealthcare.net/wp-content/uploads/2015/07/CASP-Qualitative-Research-Checklist-19.02.15.pdf. [Google Scholar]
- 36.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 37.Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, Boardman F, Gagnon M, Rousseau M. 2011. Proposal: A mixed methods appraisal tool for systematic mixed studies reviews. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com. [Google Scholar]
- 38.Centre for evidence based medicine. Oxford: University of Oxford;; 2005. Randomised clinical trial critical appraisal sheet. [Google Scholar]
- 39.Hayat A, Shaikh N. Barriers and myths to initiate insulin therapy for type 2 diabetes mellitus at primary health care centers of Hyderabad district. World Applied Sci. 2010;8:66–72. [Google Scholar]
- 40.Patel N, Stone MA, Chauhan A, Davies MJ, Khunti K. Insulin initiation and management in people with Type 2 diabetes in an ethnically diverse population: the healthcare provider perspective. Diabet Med. 2012;29:1311–1316. doi: 10.1111/j.1464-5491.2012.03669.x. [DOI] [PubMed] [Google Scholar]
- 41.Lee YK, Lee PY, Ng CJ. A qualitative study on healthcare professionals’ perceived barriers to insulin initiation in a multi-ethnic population. BMC Fam Pract. 2012;13:28. doi: 10.1186/1471-2296-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tan AM, Muthusamy L, Ng CC, Phoon KY, Ow JH, Tan NC. Initiation of insulin for type 2 diabetes mellitus patients: what are the issues? A qualitative study. Singapore Med J. 2011;52:801–809. [PubMed] [Google Scholar]
- 43.Ratanawongsa N, Crosson JC, Schillinger D, Karter AJ, Saha CK, Marrero DG. Getting under the skin of clinical inertia in insulin initiation: the Translating Research Into Action for Diabetes (TRIAD) Insulin Starts Project. Diabetes Educ. 2012;38:94–100. doi: 10.1177/0145721711432649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lakkis NA, Maalouf GJ, Mahmassani DM, Hamadeh GN. Insulin therapy attitudes and beliefs of physicians in Middle Eastern Arab countries. Fam Pract. 2013;30:560–567. doi: 10.1093/fampra/cmt022. [DOI] [PubMed] [Google Scholar]
- 45.Hayes RP, Fitzgerald JT, Jacober SJ. Primary care physician beliefs about insulin initiation in patients with type 2 diabetes. Int J Clin Pract. 2008;62:860–868. doi: 10.1111/j.1742-1241.2008.01742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grant RW, Wexler DJ, Watson AJ, Lester WT, Cagliero E, Campbell EG, Nathan DM. How doctors choose medications to treat type 2 diabetes: a national survey of specialists and academic generalists. Diabetes Care. 2007;30:1448–1453. doi: 10.2337/dc06-2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee PY, Lee YK, Khoo EM, Ng CJ. How do health care professionals assess patients when initiating insulin therapy? A qualitative study. Prim Care Diabetes. 2014;8:49–55. doi: 10.1016/j.pcd.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 48.Yoshioka N, Ishii H, Tajima N, Iwamoto Y. Differences in physician and patient perceptions about insulin therapy for management of type 2 diabetes: the DAWN Japan study. Curr Med Res Opin. 2014;30:177–183. doi: 10.1185/03007995.2013.855187. [DOI] [PubMed] [Google Scholar]
- 49.Nakar S, Yitzhaki G, Rosenberg R, Vinker S. Transition to insulin in Type 2 diabetes: family physicians’ misconception of patients’ fears contributes to existing barriers. J Diabetes Complications. 2007;21:220–226. doi: 10.1016/j.jdiacomp.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 50.Furler J, Spitzer O, Young D, Best J. Insulin in general practice - barriers and enablers for timely initiation. Aust Fam Physician. 2011;40:617–621. [PubMed] [Google Scholar]
- 51.Manski-Nankervis JA, Furler J, Blackberry I, Young D, O’Neal D, Patterson E. Roles and relationships between health professionals involved in insulin initiation for people with type 2 diabetes in the general practice setting: a qualitative study drawing on relational coordination theory. BMC Fam Pract. 2014;15:20. doi: 10.1186/1471-2296-15-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee PY, Lee YK, Ng CJ. How can insulin initiation delivery in a dual-sector health system be optimised? A qualitative study on healthcare professionals’ views. BMC Public Health. 2012;12:313. doi: 10.1186/1471-2458-12-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sunaert P, Willems S, Feyen L, Bastiaens H, De Maeseneer J, Jenkins L, Nobels F, Samyn E, Vandekerckhove M, Wens J, et al. Engaging GPs in insulin therapy initiation: a qualitative study evaluating a support program in the Belgian context. BMC Fam Pract. 2014;15:144. doi: 10.1186/1471-2296-15-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Burden M, Burden A. Attitudes to starting insulin in primary care. Practical Diabetes International. 2007;24:346–350. [Google Scholar]
- 55.Harris SB, Gerstein HC, Yale JF, Berard L, Stewart J, Webster-Bogaert S, Tompkins JW. Can community retail pharmacist and diabetes expert support facilitate insulin initiation by family physicians? Results of the AIM@GP randomized controlled trial. BMC Health Serv Res. 2013;13:71. doi: 10.1186/1472-6963-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22:1379–1385. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 57.Chen CC, Chang MP, Hsieh MH, Huang CY, Liao LN, Li TC. Evaluation of perception of insulin therapy among Chinese patients with type 2 diabetes mellitus. Diabetes Metab. 2011;37:389–394. doi: 10.1016/j.diabet.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 58.Hermanns N, Mahr M, Kulzer B, Skovlund SE, Haak T. Barriers towards insulin therapy in type 2 diabetic patients: results of an observational longitudinal study. Health Qual Life Outcomes. 2010;8:113. doi: 10.1186/1477-7525-8-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 60.Dale J, Martin S, Gadsby R. Insulin initiation in primary care for patients with type 2 diabetes: 3-year follow-up study. Prim Care Diabetes. 2010;4:85–89. doi: 10.1016/j.pcd.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 61.Sáenz A, Brito M, Morón I, Torralba A, García-Sanz E, Redondo J. Development and validation of a computer application to aid the physician’s decision-making process at the start of and during treatment with insulin in type 2 diabetes: a randomized and controlled trial. J Diabetes Sci Technol. 2012;6:581–588. doi: 10.1177/193229681200600313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xie L, Zhou S, Pinsky BW, Buysman EK, Baser O. Impact of initiating insulin glargine disposable pen versus vial/syringe on real-world glycemic outcomes and persistence among patients with type 2 diabetes mellitus in a large managed care plan: a claims database analysis. Diabetes Technol Ther. 2014;16:567–575. doi: 10.1089/dia.2013.0312. [DOI] [PubMed] [Google Scholar]


